Abstract
Background
We compared cardiovascular (CV) risk factors (CVRFs) of community-based participatory research (CBPR) participants with the community population to better understand how CBPR participants relate to the population as a whole.
Methods
GoodNEWS participants in 20 African-American churches in Dallas, Texas were compared with age/sex-matched African-Americans in the Dallas Heart Study (DHS), a probability-based sample of Dallas County residents. DHS characteristics were sample-weight adjusted to represent the Dallas County population.
Results
Despite having more education (college education: 75 versus 51%, P< 0.0001), GoodNEWS participants were more obese (mean body mass index: 34 versus 31 kg/m2, P< 0.001) and had more diabetes (23 versus 12%, P< 0.001) and hyperlipidemia (53 versus 14%, P< 0.001) compared with African-Americans in Dallas County. GoodNEWS participants had higher rates of treatment and control of most CVRFs (treated hyperlipidemia: 95 versus 64%, P< 0.001; controlled diabetes: 95 versus 21%, P< 0.001; controlled hypertension: 70 versus 52%, P= 0.003), were more physically active (233 versus 177 metabolic equivalent units-min/week, P< 0.0001) and less likely to smoke (10 versus 30%, P< 0.001).
Conclusions
Compared with African-Americans in Dallas County, CBPR participants in church congregations were more educated, physically active and had more treatment and control of most CVRFs. Surprisingly, this motivated population had a greater obesity burden, identifying them as a prime target for CBPR-focused obesity treatment.
Keywords: African–Americans, cardiovascular risk factors, community-based participatory research, obesity
Introduction
Cardiovascular disease (CVD) is the leading cause of death in the USA, with over 36% of all yearly deaths attributed to CVD.1 CV risk factors (CVRFs), including hypertension, hyperlipidemia, diabetes and obesity disproportionately affect African-American populations, contributing to a higher burden of CVD.2,3 Physical activity and dietary changes can significantly improve CVRFs and serve as CVD prevention targets, with interventions that leverage social determinants of health such as social support having greater sustainability.4–6 Community-based interventions in faith-based organizations (FBOs) of African-American communities, build on established social networks to promote lifestyle changes,5 may be effective at improving CVRFs,7,8 and are endorsed by organizations such as the American Heart Association.9
While recent studies have focused on design and implementation of community-based interventions for treatment of CVRFs,7,10–13 little is known about how the individuals recruited for CBPR programs reflect the community at large. Detailed comparisons of intervention groups and the population they represent can provide a better understanding of the social context in which a community-based intervention occurs, and insight into the capability of interventions to impact those most in need and most likely to benefit from the intervention. In addition, comparative results can potentially identify future targets for interventions. Thus, we sought to compare demographics, anthropometrics and CVRF prevalence, awareness, treatment and control between participants in the GoodNEWS Trial, an intervention promoting lifestyle changes in predominantly African-American churches in Dallas, Texas with age- and sex-matched African-Americans in Dallas County using data from the Dallas Heart Study (DHS), a multi-ethnic, population-based sample of Dallas County residents. As a secondary aim, we evaluated the association between frequency of church attendance and CVRFs within the DHS population to provide further insight into the association between church attendance and CVRFs given the focus on avid church participants in GoodNEWS.
Methods
Study design and population
A cross-sectional analysis was done comparing baseline data from all GoodNEWS participants and Dallas County African-Americans using DHS data. The GoodNEWS trial is a CBPR study aiming to reduce CVRF burden among African-Americans, using a lay health promoter (LHP) approach by training church members to serve as health educators in the FBO setting. At baseline, 392 GoodNEWS participants, aged 18–70, completed a self-administered survey which included demographics, achieved education, medical and medication history, the Diet History Questionnaire and 7-day physical activity recall (PAR), underwent blood testing for fasting lipids and blood glucose, and completed blood pressure and anthropometric measurements in 2008. Individuals with complete baseline data for demographics, physical activity, CVRFs and anthropometrics were included in this analysis (n= 357). The GoodNEWS trial was approved by the Institutional Review Board of UT Southwestern Medical Center and all participants provided written informed consent to participate in the study.
The DHS is a probability sample of Dallas County residents aged 18–65 (n= 6101) designed to study CVD with data collected from 2000 to 2002. Details of study design and variable definitions have been published previously.14 To allow extrapolation of DHS prevalence data to the general population of Dallas County, sample weights were calculated for each participant reflecting the probability of selection for DHS based on ethnicity, age, gender and geographic stratum. Sample-weighted DHS data allowed the comparison of the GoodNEWS cohort with African-Americans in Dallas County. The study was approved by the Institutional Review Board of UT Southwestern Medical Center and all participants provided written informed consent. To prevent confounding of CVRF prevalence due to age- and sex-distribution differences between the cohorts, four African-American participants from DHS (n= 1104) were matched with each GoodNEWS participant (n= 357) based on age and sex. If four controls were not available for a GoodNEWS participant, three or fewer controls were matched to maximize the number of DHS participants in the study and provide a more representative sample of Dallas County African-American adults. 78% (n= 279) of GoodNEWS participants were matched to four DHS controls.
Baseline measurements in the GoodNEWS trial
Blood pressure was measured using an established protocol,15 and the average of two blood pressure measurements was taken with a recently calibrated automatic blood pressure cuff (Welch Allyn, Inc., Series 52000). If the first two blood pressure measurements varied by >20 mmHg systolic or 10 mmHg diastolic, a third measurement was performed and the average recorded. Fingerstick capillary blood was drawn for analysis of plasma lipids and glucose (Cholestech LDX) after a 12-h fast. LDL-c was estimated by using Friedewald Equation. Anthropometrics included weight, height, body mass index (BMI), waist circumference (WC), hip circumference (HC) and waist-to-hip ratio (WHR). Weight was measured using a calibrated digital scale (Detecto Platform Balance Scales, Webb City, MO, for weights ≤300 lbs and Health-O-Meter Model 320 KL, Alsip, IL, for ≥300 lbs). Height was measured using a stadiometer (Seca Portable Stadiometer, Ontario, CA). BMI was then calculated as weight (kg)/height2(m)2. WC and HC were measured according to guidelines developed by a National Heart, Lung and Blood Institute Expert Panel.16
Each participant completed a 7-day PAR. This questionnaire measures intensity, frequency and type of activity within the previous 7 days and is established as a reliable and validated instrument.17 Energy expenditure was estimated by asking the participants to recall how much time was spent in: (i) sleep, (ii) moderate activity, (iii) hard activity and (iv) very hard activity. Total metabolic equivalent units (METS) were calculated by multiplying time in each category by a standard conversion for metabolic equivalent units18 and summing the total of activity categories 3 and 4, excluding the reported sleep and moderate activity time given that these categories were not included in the physical activity metric for DHS.
Prevalent CVRFs were defined using standard cut-points,15,19,20 self-reported personal medical history and self-reported medication use. Hypertension was defined as blood pressure ≥140/90 mmHg, history of hypertension or antihypertensive medication. Hyperlipidemia was defined as LDL-c ≥160 mmol/dl, history of hyperlipidemia or lipid-lowering medication. Diabetes was defined as fasting glucose ≥126 mmol/dl, history of diabetes, or anti-diabetic medication. Tobacco use was based on self-report from the participant survey.
Participants with a CVRF were considered ‘aware’ if they self-reported the risk factor. Participants who were aware of a risk factor were considered ‘treated’ if they reported medication use targeting the risk factor. Participants were classified as having a ‘controlled’ risk factor if the risk factor was treated to clinically accepted target levels (i.e. blood pressure <140/90 mmHg, LDL-c <160 mmol/dl and fasting glucose <126 mmol/dl).15,19,20
Baseline measurements in the DHS
Methods for DHS baseline measurements have been described previously.14 Visit 1 for DHS involved a home visit for collecting demographic and survey data and anthropometrics, including BMI, WC and HC, by a trained DHS employee. Visit 2 involved collecting fasting blood and urine samples. Baseline measurements in DHS (i.e. BMI, WC, HC, fasting lipids and glucose, tobacco use and achieved education) were completed in a similar manner as in the GoodNEWS trial. In DHS, awareness, treatment and control of prevalent hypertension, hyperlipidemia and diabetes were defined as described above for GoodNEWS. However, there were differences in the measurement of blood pressure and physical activity in DHS compared with methods described for GoodNEWS. In DHS, five sequential blood pressure measurements were taken and the average of the final three blood pressure measurements were recorded and used in analyses. In DHS, self-reported leisure-time physical activity was converted into METs based on the activity type and length in minutes, using a validated conversion scale for the intensity of the activity into METs.18 Exercise dose was calculated as the sum of METs multiplied by minutes of physical activity for all activity occurring over a week. Finally, church attendance, which was only surveyed in DHS, was defined as self-reported frequency of weekly attendance of church or religious activities.
Statistical analysis
Continuous data are presented as means (standard error of the mean) and categorical data as proportions. Statistical testing comparing the cohorts was performed using the Student's t-test or Wilcoxon rank-sum test, as appropriate, for continuous variables and the chi-square test for categorical variables. All DHS prevalence data were sample-weight adjusted and thus the reported proportions reflect those in the Dallas County population, not the study population. Sample-weighted regression models were used to assess trends in CVRF prevalence across categories of church attendance in the African-American DHS population. Logistic regression analysis was used to determine the association between prevalent obesity and church attendance independent of age and sex among African-Americans in the DHS. Two-sided P-values of ≤0.05 were considered statistically significant. All analyses were performed with SAS 9.2 Software.
Results
Demographic and clinical characteristics for the study populations are presented in Table 1. The proportion of individuals attaining at least some college education was higher in the GoodNEWS cohort than in African-American adults in Dallas County (75 versus 51%, P< 0.01), while marital status was similar between the populations (52 versus 50%, P= NS). GoodNEWS participants had a significantly lower prevalence of current smoking than Dallas County residents (10 versus 30%, P< 0.01). Blood pressure was slightly yet statistically significantly lower for GoodNEWS participants than that for African-Americans in Dallas County (systolic blood pressure: 126.0 ± 1.0 versus 129.6 ± 1.0 mmHg, P< 0.05; diastolic blood pressure: 79.5 ± 0.5 versus 81.1 ± 0.5 mmHg, P< 0.05).
Table 1.
Demographics, socioeconomic status and CVRFs—DHS (2001) and GoodNEWS (2008) populations
| Variable | DHS (n= 1104) | GoodNEWS (n= 357) | P-value |
|---|---|---|---|
| Age (years)a | 46.0 (0.5) | 47.0 (0.6) | 0.2 |
| Male (n, %) | 275 (25) | 78 (22) | 0.3 |
| Education | |||
| <College (n, %) | 630 (49) | 86 (25) | <0.01 |
| College + (n, %) | 474 (51) | 264 (75) | <0.01 |
| Marital status (married; n, %) | 369 (50) | 184 (52) | 0.7 |
| CVRFs | |||
| Current smoking (n, %) | 362 (30) | 31 (10) | <0.01 |
| Systolic blood pressure (mmHg)a | 129.6 (1.0) | 126.0 (1.0) | 0.01 |
| Diastolic blood pressure (mmHg)a | 81.1 (0.5) | 79.5 (0.5) | 0.03 |
| Total cholesterol (mg/dl)a | 181.1 (2.4) | 179.1 (2.3) | 0.6 |
| LDL-C (mg/dl)a | 106.4 (2.1) | 109.0 (2.3) | 0.4 |
| HDL-C (mg/dl)a | 53.9 (1.0) | 48.3 (0.9) | <0.01 |
| Triglycerides (mg/dl)a | 108.1 (6.1) | 123.7 (4.5) | 0.04 |
| Fasting glucose (mg/dl)a | 105.6 (2.4) | 102.6 (2.0) | 0.4 |
| BMI (kg/m2)a | 30.9 (0.5) | 34.1 (0.44) | <0.01 |
| WC (cm)a | 100.3 (1.0) | 105.1 (0.9) | 0.01 |
| Waist/hip ratioa | 0.89 (0.01) | 0.87 (0.00) | 0.08 |
| Physical activity (METS min)/weekb | 177 (0, 540) | 233 (227, 247) | <0.01 |
aMean (standard error).
bMedian (interquartile range).
BMI and WC were both significantly higher for GoodNEWS participants than African-Americans in Dallas County. The average BMI for GoodNEWS participants was 34.0 ± 0.4 kg/m² compared with 30.9 ± 0.5 kg/m² in Dallas County residents (P< 0.01). Triglycerides were also higher (123.7 ± 4.5 versus 108.1 ± 6.1 mmol/L, P< 0.01) and HDL-c was significantly lower (P= 0.04) in the GoodNEWS group than that the Dallas County population; however, total cholesterol and LDL-c were similar between the two groups (P= NS for each).
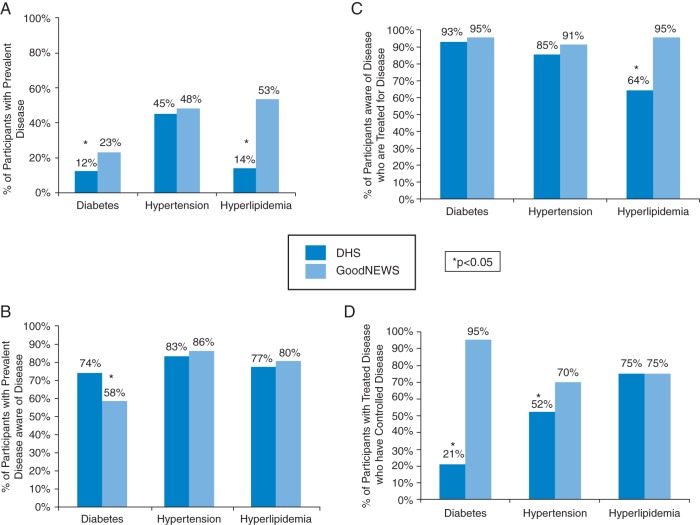
The prevalence of diabetes and hyperlipidemia was also significantly higher in the GoodNEWS population than that in African-American adults in Dallas County (Fig. 1A). While awareness of prevalent diabetes was lower in the GoodNEWS population, awareness of prevalent hypertension and hyperlipidemia was not statistically different between the groups (Fig. 1B). However, treatment and control rates of these CVRFs were higher among the GoodNEWS population (Fig. 1C and D). Over 90% of GoodNEWS participants aware of prevalent diabetes, hypertension and hyperlipidemia reported treatment for these diseases (P< 0.05 for diabetes and hyperlipidemia treatment as compared with Dallas County adults). Finally, GoodNEWS participants treated for CVRFs were significantly more likely to have control of diabetes (95 versus 21%, P< 0.05) and hypertension (70 versus 52%, P< 0.05) than African-American adults in Dallas County. Although obesity was more prevalent in the GoodNEWS population, participants in this study reported significantly higher rates of weekly physical activity than in the Dallas County population.
Fig. 1.
The prevalence (A), awareness (B), treatment (C) and control (D) of diabetes, hypertension and hyperlipidemia—GoodNEWS (2008) versus DHS (2001) population.
When comparing prevalent CVRFs based on self-reported monthly church attendance in the Dallas County population, there were no differences in prevalent diabetes, hypertension or hyperlipidemia; however, those with the most frequent church attendance had a significantly lower prevalence of current smoking (Supplementary data, Table S1). Among African-Americans in Dallas County, individuals who reported going to church four or more times per month had significantly greater BMI and WC than those who went to church less frequently (P < 0.05 for each; Fig. 2A and B). Frequent church attendance (≥4 times per month) was associated with prevalent obesity (BMI ≥30 kg/m2), independent of age and sex as compared with those who reported no church attendance (odds ratio (OR): 1.26, 95% confidence interval (CI) = 1.05–1.52, P= 0.01; Table 2).
Fig. 2.
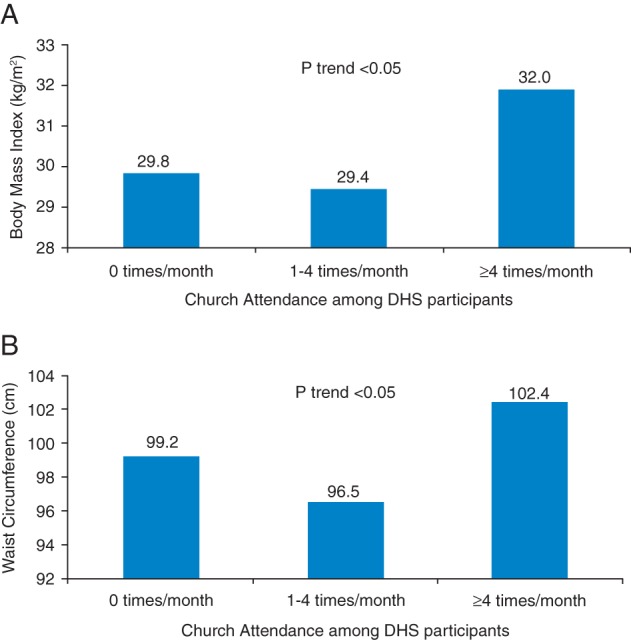
The mean BMI (A) and the mean WC (B) in the DHS stratified by monthly church attendance (attendance groups: 0, 1–4 and ≥4 per month), 2001.
Table 2.
Odds of obesity by church attendance in the African-American DHS population (2001): unadjusted and adjusted for age and sex
| Variable |
Unadjusted model |
Adjusted model |
||
|---|---|---|---|---|
| OR (95% CI) | P-value | OR (95% CI) | P-value | |
| Age (years)a | — | — | 1.02 (1.01–1.02) | <0.01 |
| Female sex | — | — | 2.09 (1.80–2.43) | <0.01 |
| Attendance 1–4 times per monthb | 1.14 (0.94–1.40) | 0.2 | 1.06 (0.86–1.29) | 0.6 |
| Attendance ≥4 times per monthb | 1.62 (1.36–1.93) | <0.01 | 1.26 (1.05–1.52) | 0.01 |
aAge as a continuous variable in logistic regression models.
bReferent category—church attendance 0 times per month.
Discussion
Main findings of this study
Comparing the GoodNEWS cohort with African-Americans in Dallas County provides unique insights into differences between those recruited for a church-based intervention and the general community population. In addition, the comparison highlights potential methods in future projects to reduce CV risk in the African-American community through church-based interventions. We have identified the GoodNEWS cohort as an at-risk population with a higher prevalence of obesity and downstream obesity-related risk factors (including diabetes, low HDL and high triglycerides), as compared with African-Americans of similar ages and sex in Dallas County. In contrast, GoodNEWS participants exercised more, smoked less and were more likely to undergo pharmacologic treatment with the control of CVRFs than the general population. These findings about GoodNEWS participants, a population of frequent churchgoers, were supported by analyses within DHS, where more frequent church attendance was associated with obesity and a lower probability of smoking.
These data provide important insights regarding the potential role of the African-American church as a site for community-based interventions. On the one hand, the church-based population appears more educated and motivated to engage in several healthy behaviors, including avoidance of smoking and treatment and control of existing risk factors. On the other hand, obesity rates are actually higher in those with more frequent church attendance. This finding highlights a ‘disconnect’ between obesity and other preventable CVRFs. It suggests that the pervasive factors contributing to obesity in modern society overwhelm the usual benefits of greater education and engagement with the health-care system that is demonstrated among those with more frequent church attendance.
These findings suggest that the most pressing needs in the GoodNEWS population are targeting obesity treatment through lifestyle modification as opposed to improving awareness, treatment and control of prevalent diabetes, hypertension and hyperlipidemia. The GoodNEWS participants also report more physical activity than the African-American Dallas County population, suggesting that they may need specific tools emphasizing appropriate intensity and proper form for physical activity that promotes weight loss. The relationship between frequent church attendance and obesity confirmed in the DHS population also emphasizes that linking church activities with lifestyle interventions for obesity treatment in African-American populations may be ideal. Moreover, developing a physical and social environment within African-American churches that is conducive to physical activity and healthy eating may also be important. Impacting obesity within the African-American church community may potentially impact the obesity epidemic in the overall African-American population.
What is already known on this topic
Previous work advocates for the church as a focus for community-based interventions given the church's role in providing social support and social networks that can reinforce necessary changes in health behavior,21–23 but little has been known about who may actually be recruited by these church-based interventions. These data support the hypothesis that church-based interventions can identify and target an at-risk population.
What this study adds
Our study is one of the first to systematically compare a church-based intervention cohort to the overall representative community from which the participants originate, providing insights for future interventions. Thus, targeting weight loss as a part of the GoodNEWS church-based intervention may serve as an important method for secondary prevention and treatment of CVRFs in this population.24
GoodNEWS participants appear to be motivated for lifestyle changes as evidenced by their increased physical activity as compared with the Dallas County population; therefore, the GoodNEWS population may need training about exercise that promotes weight loss or improvement in CVD risk factors. Moreover, they likely also need comprehensive dietary education. Prior studies suggest that church-based interventions can promote weight loss in African-American church communities using LHPs or a combination of LHPs and health professionals as program facilitators.11,13,25 In addition, weight loss interventions may need to incorporate a spiritual component that serves as a motivational tool in the church-going population.10,13 In the Love, Inspiration, Feedback and Education program, African-American women in the spirituality-based educational program had significant reductions in weight, BMI and SBP as compared with the women in the non-spiritual intervention.13
Data from DHS regarding the association between church attendance and obesity support prior studies that show evidence of a relationship between religiosity and obesity.26,27 Prior work suggests that this link between church attendance or religiosity and obesity may be related to a lack of encouragement in religious settings to avoid overeating as opposed to other vices, such as smoking.28 The higher prevalence of obesity with lower prevalence of current smoking among GoodNEWS participants suggests that these individuals are similar to those who attend church four or more times per month in the DHS population. Given that those who frequently attend church are more likely to be obese, incorporating exercise into the church activities through the GoodNEWS intervention may be essential. Our group's previous study also suggests that incorporating physical activity into the GoodNEWS program may decrease the prevalence of metabolic syndrome in this population.29 Finally, future studies may investigate targeting the physical and social environment in the African-American church to improve access to physical activity and appropriate nutrition and to reduce obesity.
Thus, our research shows African-Americans from church congregations recruited to participate in a community-based lifestyle intervention have a higher prevalence of obesity and obesity-related CVRFs than the general population. However, these participants had higher education, higher treatment and control of CVRFs, lower tobacco abuse and higher weekly exercise levels compared with the general population. This suggests African-American church-goers recruited for a CBPR program are at risk for CVD, yet are knowledgeable, utilize the healthcare system and are motivated to implement lifestyle changes. Therefore, the African-American church-based population appears to be a prime target for community interventions for obesity treatment and CVD prevention.
Limitations of this study
Important strengths of DHS include the cohort size and sample weighting, which allows the extrapolation of findings to the overall Dallas County population. There are, however, limitations to this work. The data for the cohorts are cross-sectional; therefore, no inferences of causality can be made in associations between church attendance and prevalent CVRFs. Differences in survey administration methods and physical activity and blood pressure measurements may contribute to differences between the groups; however, these methodological differences are unlikely to significantly impact study findings. Additionally, physical activity was self-reported, subjecting it to misclassification bias. The DHS cohort was enrolled between 2000 and 2002, whereas the GoodNEWS cohort was formed in 2008. The time difference may have contributed in part to differences in obesity rates, although this small time difference is unlikely to explain the full differences between groups. Sample-weighted DHS data, which is only available from 2000 to 2002, provided an opportunity to compare the GoodNEWS cohort to Dallas County African-Americans, likely improving the validity of the findings. The GoodNEWS population consists of volunteers for the study who may not be representative of all church-going Dallas County African-Americans. However, this cohort likely represents African-Americans who would volunteer in similar church-based lifestyle interventions throughout Dallas County.
Supplementary data
Supplementary data are available at the Journal of Public Health online.
Funding
This work was supported by the National Heart, Lung and Blood Institute, National Institutes of Health [RO1 HL087768]. Funding support for the Dallas Heart Study was provided by the Donald W. Reynolds Foundation (Las Vegas, NV) and the United States Public Health Service General Clinical Research Center grant [#MO1-RR00633] from the National Institutes of Health/National Center Research Resources-Clinical Research. Funding support for Dr Powell-Wiley and Dr Banks-Richard was provided by the Ruth Kirschstein National Research Service Award from the National Institutes of Health [#2-T32-HL007360-31]. Dr Powell-Wiley is currently funded by the Division of Intramural Research (DIR) of the National Heart, Lung and Blood Institute (NHLBI) of the National Institutes of Health.
Authors' contributions
T.M.P-W and K.B-R countributed equally to this project and share primary authorship of this manuscript.
Supplementary Material
Acknowledgements
We would like to thank Ms Anissa Carbajal-Diaz for her assistance in manuscript preparation and the DHS and GoodNEWS participants for all of their efforts as participants in these projects.
References
- 1.Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics—2011 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2011;123(4):e18–209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) CDC health disparities and inequalities report—United States, 2011. MMWR Suppl. 2011;60(1):1–116. [PubMed] [Google Scholar]
- 3.Poirier P, Giles TD, Bray GA, et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2006;113(6):898–918. doi: 10.1161/CIRCULATIONAHA.106.171016. [DOI] [PubMed] [Google Scholar]
- 4.Artinian NT, Fletcher GF, Mozaffarian D, et al. Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: a scientific statement from the American Heart Association. Circulation. 2010;122(4):406–41. doi: 10.1161/CIR.0b013e3181e8edf1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Green L, Kreuter M. Health Promotion Planning: An Educational and Environmental Approach. 2nd edn. Mountain View: Mayfield Publishing C; 1991. [Google Scholar]
- 6.Benjamin EJ, Smith SC, Jr, Cooper RS, et al. Task force #1—magnitude of the prevention problem: opportunities and challenges. 33rd Bethesda Conference. J Am Coll Cardiol. 2002;40(4):588–603. doi: 10.1016/s0735-1097(02)02082-x. [DOI] [PubMed] [Google Scholar]
- 7.Yanek LR, Becker DM, Moy TF, et al. Project Joy: faith based cardiovascular health promotion for African American women. Public Health Rep. 2001;116(Suppl. 1):68–81. doi: 10.1093/phr/116.S1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thompson E, Berry D, Nasir L. Weight management in African-Americans using church-based community interventions to prevent type 2 diabetes and cardiovascular disease. J Natl Black Nurses Assoc. 2009;20(1):59–65. [PubMed] [Google Scholar]
- 9.Kumanyika SK, Obarzanek E, Stettler N, et al. Population-based prevention of obesity: the need for comprehensive promotion of healthful eating, physical activity, and energy balance: a scientific statement from American Heart Association Council on Epidemiology and Prevention, Interdisciplinary Committee for Prevention (formerly the expert panel on population and prevention science) Circulation. 2008;118(4):428–64. doi: 10.1161/CIRCULATIONAHA.108.189702. [DOI] [PubMed] [Google Scholar]
- 10.Fitzgibbon ML, Stolley MR, Ganschow P, et al. Results of a faith-based weight loss intervention for black women. J Natl Med Assoc. 2005;97(10):1393–402. [PMC free article] [PubMed] [Google Scholar]
- 11.Kim KH, Linnan L, Campbell MK, et al. The WORD (wholeness, oneness, righteousness, deliverance): a faith-based weight-loss program utilizing a community-based participatory research approach. Health Educ Behav. 2008;35(5):634–50. doi: 10.1177/1090198106291985. [DOI] [PubMed] [Google Scholar]
- 12.Whitt-Glover MC, Kumanyika SK. Systematic review of interventions to increase physical activity and physical fitness in African-Americans. Am J Health Promot. 2009;23(6):S33–56. doi: 10.4278/ajhp.070924101. [DOI] [PubMed] [Google Scholar]
- 13.Parker VG, Coles C, Logan BN, et al. The LIFE project: a community-based weight loss intervention program for rural African American women. Fam Community Health. 2010;33(2):133–43. doi: 10.1097/FCH.0b013e3181d594d5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Victor RG, Haley RW, Willett DL, et al. The Dallas Heart Study: a population-based probability sample for the multidisciplinary study of ethnic differences in cardiovascular health. Am J Cardiol. 2004;93(12):1473–80. doi: 10.1016/j.amjcard.2004.02.058. [DOI] [PubMed] [Google Scholar]
- 15.Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289(19):2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 16.Services UDoHaH. Washington D.C: Government Printing Office; 1998. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: executive summary. Expert Panel on the Identification, Evaluation, and Treatment of Overweight in Adults. [Google Scholar]
- 17.Sloane R, Snyder DC, Demark-Wahnefried W, et al. Comparing the 7-day physical activity recall with a triaxial accelerometer for measuring time in exercise. Med Sci Sports Exerc. 2009;41(6):1334–40. doi: 10.1249/MSS.0b013e3181984fa8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(9 Suppl.):S498–504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 19.National Cholesterol Education Program. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143–421. [PubMed] [Google Scholar]
- 20.American Diabetes Association. Standards of medical care in diabetes—2010. Diabetes Care. 2010;33(Suppl. 1):S11–61. doi: 10.2337/dc10-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thomas SB, Quinn SC, Billingsley A, et al. The characteristics of northern black churches with community health outreach programs. Am J Public Health. 1994;84(4):575–9. doi: 10.2105/ajph.84.4.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chatters LM, Levin JS, Ellison CG. Public health and health education in faith communities. Health Educ Behav. 1998;25(6):689–99. doi: 10.1177/109019819802500602. [DOI] [PubMed] [Google Scholar]
- 23.Baskin ML, Resnicow K, Campbell MK. Conducting health interventions in black churches: a model for building effective partnerships. Ethn Dis. 2001;11(4):823–33. [PubMed] [Google Scholar]
- 24.Kumanyika SK, Gary TL, Lancaster KJ, et al. Achieving healthy weight in African-American communities: research perspectives and priorities. Obes Res. 2005;13(12):2037–47. doi: 10.1038/oby.2005.251. [DOI] [PubMed] [Google Scholar]
- 25.McNabb W, Quinn M, Kerver J, et al. The PATHWAYS church-based weight loss program for urban African-American women at risk for diabetes. Diabetes Care. 1997;20(10):1518–23. doi: 10.2337/diacare.20.10.1518. [DOI] [PubMed] [Google Scholar]
- 26.Lapane KL, Lasater TM, Allan C, et al. Religion and cardiovascular disease risk. J Religion Health. 1997;36(2):155–63. [Google Scholar]
- 27.Feinstein M, Liu K, Ning H, et al. Burden of cardiovascular risk factors, subclinical atherosclerosis, and incident cardiovascular events across dimensions of religiosity: the multi-ethnic study of atherosclerosis. Circulation. 2010;121(5):659–66. doi: 10.1161/CIRCULATIONAHA.109.879973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cline KMC, Ferraro KF. Does religion increase the prevalence and incidence of obesity in adulthood? J Sci Study Religion. 2006;45(2):269–81. doi: 10.1111/j.1468-5906.2006.00305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shuval K, DeVahl J, Tong L, et al. Anthropometric measures, presence of metabolic syndrome, and adherence to physical activity guidelines among African American church members, Dallas, Texas, 2008. Prev Chronic Dis. 2011;8(1):A18. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.