Abstract
Purpose
Information about the influence of delayed surgery on infectious wound complications is ambiguous. A clinical audit was performed to test the hypothesis that early surgery lowers the rate of infectious wound complications. Secondly we looked at the influence of surgical delay and complications on patient reported functional outcome.
Methods
All consecutive, closed distal fibular fractures treated surgically with a plate were included and retrospectively analysed for the delay in operation and wound complications. In a second cohort of patients with a AO-Weber B-type ankle fracture outcome was measured using the Olerud-Molander ankle score (OMAS), the American Orthopaedic Foot and Ankle Society score (AOFAS) and a visual analog score (VAS) for overall satisfaction.
Results
Patients treated within one day experienced no wound complications (zero out of 60), whereas in the delayed group 11 % (16/145) did (p = 0.004). A similar significant difference was found for the patients treated within one week (2/98) versus after one week (14/107). A systematic review of the literature showed a difference in wound complications of 3.6 % (early) versus 12.9 % (late) (p < 0.0001). After 43 months, the median AOFAS was 11.5 points lower in the complication group, the OMAS 10 points, and the VAS 0.5 points, with all differences being statistically significant.
Conclusions
Every effort should be made to operate on closed ankle fractures as soon as reasonably possible. A delay in surgery is associated with a significant rise in infectious wound complications, which significantly lowers outcome and patient satisfaction. These fractures should preferably be treated within the first day.
Introduction
Ankle fractures represent approximately 10 % of all fractures and are among the most frequently encountered surgically treated fractures [10]. The incidence of ankle fractures has increased up to 300 % in the last 30 years, especially in the elderly population [3, 16]. With increasing rates of comorbidities a concomitant rise in fragility fractures can be expected, which in turn may increase the risk of complications. Surgical treatment of ankle fractures may be accompanied by several complications such as nonunion, malunion, implant failure, and wound complications [12]. The most frequently encountered complications are wound complications, of which infection may have the most devastating effect.
Wound complications that may occur include wound edge necrosis, wound dehiscence, superficial infection, and deep infection (osteomyelitis), and are caused by surgeon, fracture, and patient characteristics. The surgeon characteristics included the timing of surgery [13], placement of the incision, soft tissue handling [23], type of implant [19, 26], and the aftertreatment [31]. The fracture characteristics include, for example, the severity of the fracture and the presence of a breach of skin integrity. The related patient characteristics include, among others, age [18, 20], obesity [9], smoking habits [4], substance abuse [32], peripheral vascular disease [28], and diabetes [11, 34].
Information about the influence of delayed surgery on infectious wound complications is ambiguous. We therefore performed a clinical audit to test the hypothesis that early surgery lowers the rate of infectious wound complications. Secondly we looked at the influence of surgical delay and complications on patient reported functional outcome. This study is a continuation of an investigation in which a series of ankle fractures from the period 2004 to 2009 were studied [26, 33].
Material and methods
This is a retrospective study of all consecutive patients, between January 1, 2004 and December 31, 2009, in which plating of the fibula in a closed ankle fracture was performed [26]. All patients received antibiotic prophylaxis according to hospital protocol (third generation cephalosporin). The use of a tourniquet was based on surgeon’s preferences. Fracture approach, reduction and fixation were according to AO standards as published previously [26]. Closure was performed in two layers, no suction-drains were used.
Delay until operation and wound complications were recorded from the patient files, operation reports, and the picture archiving and communication system (PACS).
Infectious wound complications and the need for elective hardware removal were scored. Wound infection was further separated into superficial or minor and deep or major infectious complications by applying the criteria of the Centres for Disease Control and Prevention (CDC) for defining a surgical site infection [21]. Minor complications were defined as a superficial infection treatable with conservative management such as oral antibiotics only, without the need for intervention or re-admission. Major complications were defined as a deep infection in need of intervention or re-admission, such as intravenous antibiotics, removal of hardware, and wound debridement with or without vacuum assisted closure [26]. The differentiation between superficial and deep infection was made by the surgeon or attending physician.
In a second series of consecutive patients aged between 16 and 65 years with an AO-Weber B type ankle fracture, treated between January 2004 and July 2009 [33], the influence of infectious wound complications on the overall outcome was investigated. Only the Weber-B type fractures were included in order to obtain a more homogenous population. Minimum follow-up was six months. Patient characteristics (i.e., age, gender, diabetes, and smoking habits), fracture characteristics (i.e., fracture side and number of malleoli involved) were recorded. Outcome was measured using standard questionnaires, which consisted of the Olerud-Molander ankle score (OMAS), the American Orthopaedic Foot and Ankle Society ankle-hindfoot score (AOFAS), and a single question visual analog scale (VAS) for patient satisfaction with outcome. Two patients with a complication other than a wound infection were excluded (n = 2; one complex regional pain syndrome and one deep venous thrombosis) in order to compare patients with versus without infectious complications.
Literature search
A literature search was conducted in order to identify studies in which ankle fractures were treated surgically. The electronic databases up to December 1, 2011 of the Cochrane Library, Pubmed Medline, EMbase, and Google Scholar were explored using the combination of the following search terms and Boolean operators: ankle OR fibula AND complication OR infection OR timing. No restriction in language and publication date was applied. In addition, a comprehensive search of reference lists of all identified articles was conducted in order to find additional studies. An article was found eligible when it concerned (1) the surgical treatment of an ankle fracture, (2) reporting of the number of wound complications, and (3) reporting on two groups treated early or delayed. Abstracts from scientific meetings were included in the review, when sufficient data could be extracted on functional outcome or complication rate. The cut-off point for early and delayed surgery, the group sizes, and the number of wound complications were extracted from these publications.
Data analysis
The statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) version 16.0 (SPSS, Chicago, IL). The Kolmogorov-Smirnov test was used to test for normality of the data. The Levene’s test was applied to assess homogeneity of variance between groups. Since most numeric variables did not show normal distribution or equal variance, all items were regarded as nonparametric for the statistical analysis. A Mann–Whitney U-test (numeric data), chi-square analysis or Fisher's exact test (categorical data) was performed in order to assess statistical significance of difference between the number of complications in the early and delayed treated patients, and to test for difference in outcome between groups with and without complications. A p-value <0.05 was taken as level of statistical significance. Numeric data are expressed as medians with P25–P75; categorical data are shown as numbers with percentages.
Results
Influence of surgical delay on complications
A total of 205 ankle fractures were treated surgically in the six-year study period. All received plating of the fibula. The number of fractured malleoli was as follows: 117 unimalleolar, 57 bimalleolar, and 31 trimalleolar. There were 26 fracture-dislocations. The median surgical delay was seven days for the entire population (P25–P75 1–11 days).
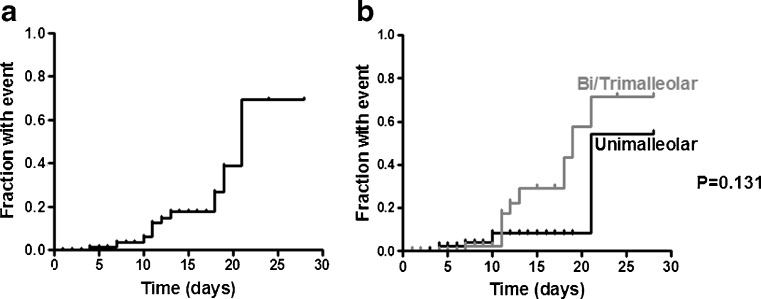
In the unimalleolar group 22.2 % was treated within the first day (24 h) and in the bi- or trimalleolar group this percentage was 38.6 % (p = 0.013). None of the 60 ankle fractures treated within one day developed an infectious wound complication, whereas in the group treated after day one 11 % (16 out of 145) did develop an infectious wound complication (p = 0.004). Ten were minor and six were major complications (Fig. 1a).
Fig. 1.
Kaplan-Meier plot of complications in relation to delay. Cumulative number of patients with an infectious wound complication in relation to surgical delay for the total study sample (a), and the difference in events in unimalleolar and bi- or trimalleolar fractures (b)
When taking one week as the cut-off point for early treatment 43.6 % of the unimalleolar fractures were treated early versus 53.4 % of the bi- or trimalleolar fractures (p = 0.204). Two percent of the patients treated within six days experienced a complication (two out of 98), which were both major complications. Patients treated from day seven experienced an infectious wound complication in 13.1 % of cases (14 out of 107; ten minor and four major), which was a significant difference (p = 0.003).
The complication rate in the unimalleolar group was 5.1 % (three minor and three major out of 107 fractures) and in the bi- or trimalleolar group this number was 11.4 % (seven minor and three major out of 88 fractures). This difference was not statistically significant (Fig. 1b; p = 0.118). Using a post hoc power analysis the groups needed to be three times the size in order to detect a significant difference (with 80 % power, two-sided testing, and an alpha of 0.05).
Systematic review influence delay on complications
Including the results of our study, 11 publications were included in the literature review (Table 1). Considering wound complications and the effect of early versus delayed surgical treatment six showed a significant increase when surgery was delayed, two showed a trend for increased complications, and three studies did not find a difference between early and delayed surgery. In the early treatment group 24 events occurred in 673 patients (3.6 %) and in the delayed group 66 events occurred in 513 patients (12.9 %). This difference was statistically significant (P < 0.0001).
Table 1.
Literature overview showing influence of timing of ankle fracture surgery and wound complications
| Study (year) | Cut-off point | Wound complications | Conclusion | |
|---|---|---|---|---|
| Early | Delayed | |||
| Breederveld (1988 )[6] | 24 h | 3/72 (2 in open#) | 2/20 | No significant difference |
| Caragee (1991) [8] | 4 daysa | 17.9 % | 39.5 % | P = 0.008 all complications |
| Caragee (1993) [7] | Same day | 3/43 | 10/34 | P < 0.001 |
| Konrath (1995) [17] | 5 days | 5/105 | 6/97 | No significant difference |
| Hoiness (2000) [13] | < 8 h or >5 days | 5/67 | 7/17 | P = 0.0018 |
| Singh (2005) [27] | 24 h | 0/24 | 6/38 | Trend (P = 0.07) |
| Pietzik (2006) [24] | 48 h | 0/62 | 1/21 | No significant difference |
| Adamson (2009) [1] | 24 h | 1/67 | 8/84 | P = 0.04 |
| Saithna (2009) [25] | 6 days | 2/56 | 6/29 | P = 0.01 |
| Sukeik (2010) [30] | 24 h | 5/117 | 4/28 | Trend (P = 0.07) |
| Present study | 24 h | 0/60 | 16/145 | P = 0.004 |
| Combinedc | 24/673 (3.6 %) | 66/513 (12.9 %) | P < 0.0001 | |
aCombination of all types of complications (infection, reduction, other) reported
bWound infection and wound edge necrosis
cCaragee (1991) [8] not included, 2-sided Fisher's exact test
Influence delay and complications on outcome
The second series was complied of 101 patients with a Weber-B fracture, of which 14 experienced an infectious wound complication. With a median follow-up of 43 (P25–P75: 29–60) months the overall outcome was significantly influenced by the development of an infectious wound complication. The median AOFAS was 11.5 points lower in the complication group, the OMAS 10 points, and the VAS 0.5 points (Table 2). With the exception of gender the two groups of Weber-B fractures were comparable considering age, BMI, number of fractured malleoli, fracture dislocation, smoking, and diabetes.
Table 2.
Demographics and outcome of surgically treated Weber-B ankle fracture with or without infectious wound complication
| Parameter | Total group (n = 101) | Without complication (n = 87) | With complications (n = 14) | p value |
|---|---|---|---|---|
| Gender (% male) | 40 (39.6 %) | 30 (34.5 %) | 10 (71.4) | 0.016a |
| Age (years) | 50.7 (40.9–60.7) | 51.7 (41.5–60.7) | 46.7 (22.1–63.3) | 0.814b |
| BMI (kg/m2) | 25.9 (23.8–29.2) | 25.9 (23.5–28.9) | 25.9 (24.1–29.6) | 0.734b |
| Unimalleolar % | 69 (68.3 %) | 60 (69.0) | 9 (64.3 %) | 0.115a |
| Fracture dislocation (%) | 12 (11.9 %) | 9 (10.3 %) | 3 (21.4 %) | 0.366a |
| Smoking (%) | 21 (20.8 %) | 17 (19.5 %) | 4 (28.6 %) | 0.482a |
| Diabetic (%) | 6 (5.9 %) | 5 (5.7 %) | 1 (7.1 %) | 1.000a |
| AOFAS | 97 (82–100) | 97 (84–100) | 85.5 (65–98.5) | 0.036b |
| OMAS | 90 (80–100) | 90 (80–100) | 80 (66.3–90) | 0.012b |
| VAS | 8 (7–9) | 8 (7–9.1) | 7.5 (6–8) | 0.027b |
Data are shown as number with percentages, or as median with P25–P75. Values in bold are statistically significant
BMI body mass index, AOFAS American Orthopaedic Foot Ankle Society hindfoot score, OMAS Olerud Molander ankle score, VAS visual analogue scale
aFisher's exact test
bMann-Whitney U test
Patients with a delay of one day to surgery showed no difference in AOFAS and VAS, but a significant five point reduction in the median OMAS (90 versus 85 points). This five point difference in the OMAS was also present when comparing the groups with a delay of one week, but not significant (p = 0.057). The AOFAS and VAS did not differ between these groups.
Discussion
This study shows a significant difference in infectious wound complications for patients treated after a delay for a closed ankle fracture. Independent of the cut-off point of 24 hours or one week the chance of an infection is at least a factor six higher in the delayed group. This difference was also noted in the systematic review where 3.6 % of infectious wound complications occurred compared with 12.9 % in the delayed group. More important this increase in complications has a direct negative effect on functional outcome as measured with three renowned scoring systems.
Previous studies on early versus delayed surgical treatment mainly focus on the length of stay and the concomitant increase in costs (up to 1250 Euro per case) with a longer hospital stay [6, 15, 24]. Others have pointed out an improved rate of anatomical reductions in early management [7, 8].
Avoiding wound complications is of paramount importance and should receive a high priority. Timing of the surgical stabilisation appears to be a controllable factor to achieve lower complication rates. Another factor that can be influenced is the choice of implant, e.g., thinner plates [26] or fibular nailing [2] in fragility fractures or in patients with comorbidities.
The effect of wound complications in general on outcome has been noted in one previous study with an almost identical duration of follow-up as our study [14]. In that study the major infectious complications (n = 2) especially were associated with a worse outcome; however, the exact difference in outcome scores was not reported. Surgical delay was not associated with a poorer outcome in the study by Hoiness et al. [14], which is in concurrence with a more recent publication [5]. Our results on the other hand show a lower OMAS in fractures treated after a surgical delay.
Other factors, different than trauma and surgical characteristics, which have been identified as negatively influencing outcome are obesity, smoking, alcohol abuse, and a lower level of education [5, 29]. These parameters were not assessed in our study.
A limitation of our study is its retrospective design, as were the studies included in the systematic review. The reasons for postponing the surgical repair were not recorded. In our study it was the policy to plan the fractures electively and to wait for approximately one week to let the swelling settle, which is not uncommon practice [22]. In some cases a conservative treatment was initiated, but because of secondary dislocation a change to surgery was made. In these patients the delay was longer than one week. The percentage of bi- and trimalleolar fractures treated early was higher than the unimalleolar fractures. Thus, the more complex fractures were apparently not postponed more frequently because of soft-tissue problems.
Open fractures form a completely different entity as an orthopaedic emergency and were not included in this study. In case of a fracture-dislocation (n = 26) a closed reduction was tried first, which resulted in an early surgical intervention if not successful. If fracture-dislocations were removed from the analyses the difference in complications with cut-off point of one day remained (0/46 vs 14/133; p = 0.022), as did the difference with cut-off point of one week (2/81 vs 12/98; p = 0.023).
In conclusion, every effort should be made to operate closed ankle fractures as soon as reasonably possible. A delay of more than one week gives a significant rise in infectious wound complications, which significantly lowers functional outcome and patient satisfaction. The fractures should preferably be treated within the first day. Published data also support the view that early operative treatment gives a significant reduction in wound complications and a concomitant improved functional outcome for the patients.
Acknowledgments
Conflicts of interest and source of funding
No conflict of interest or funding is declared by any of the authors.
References
- 1.Adamson SP, Trickett R, Hodgson P, Mohanty K. Ankle fractures: impact of timing of surgery. Inj Extra. 2009;40:224. doi: 10.1016/j.injury.2009.06.274. [DOI] [Google Scholar]
- 2.Appleton PT, McQueen MM, Court-Brown CM. The fibula nail for treatment of ankle fractures in elderly and high risk patients. Tech Foot Ankle Surg. 2006;5:204–208. doi: 10.1097/01.btf.0000221100.31792.c2. [DOI] [Google Scholar]
- 3.Bengner U, Johnell O, Redlund-Johnell I. Epidemiology of ankle fracture 1950 and 1980. Increasing incidence in elderly women. Acta Orthop Scand. 1986;57:35–37. doi: 10.3109/17453678608993211. [DOI] [PubMed] [Google Scholar]
- 4.Berkes M, Obremskey WT, Scannell B, Ellington JK, Hymes RA, Bosse M (2010) Maintenance of hardware after early postoperative infection following fracture internal fixation. J Bone Joint Surg Am 92:823–828 [DOI] [PubMed]
- 5.Bhandari M, Sprague S, Ayeni OR, Hanson BP, Moro JK. A prospective cost analysis following operative treatment of unstable ankle fractures: 30 patients followed for 1 year. Acta Orthop Scand. 2004;75:100–105. doi: 10.1080/00016470410001708200. [DOI] [PubMed] [Google Scholar]
- 6.Breederveld RS, van Straaten J, Patka P, van Mourik JC. Immediate or delayed operative treatment of fractures of the ankle. Injury. 1988;19:436–438. doi: 10.1016/0020-1383(88)90142-8. [DOI] [PubMed] [Google Scholar]
- 7.Carragee EJ, Csongradi JJ. Increased rates of complications in patients with severe ankle fractures following interinstitutional transfers. J Trauma. 1993;35:767–771. doi: 10.1097/00005373-199311000-00020. [DOI] [PubMed] [Google Scholar]
- 8.Carragee EJ, Csongradi JJ, Bleck EE. Early complications in the operative treatment of ankle fractures. Influence of delay before operation. J Bone Joint Surg Br. 1991;73:79–82. doi: 10.1302/0301-620X.73B1.1991782. [DOI] [PubMed] [Google Scholar]
- 9.Chaudhry S, Egol KA. Ankle injuries and fractures in the obese patient. Orthop Clin N Am. 2011;42:45–53. doi: 10.1016/j.ocl.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 10.Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37:691–697. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 11.Flynn JM, Rodriguez-del Rio F, Piza PA. Closed ankle fractures in the diabetic patient. Foot Ankle Int. 2000;21:311–319. doi: 10.1177/107110070002100407. [DOI] [PubMed] [Google Scholar]
- 12.Hess F, Sommer C. Minimally invasive plate osteosynthesis of the distal fibula with the locking compression plate: first experience of 20 cases. J Orthop Trauma. 2011;25:110–115. doi: 10.1097/BOT.0b013e3181d9e875. [DOI] [PubMed] [Google Scholar]
- 13.Hoiness P, Stromsoe K. The influence of the timing of surgery on soft tissue complications and hospital stay. A review of 84 closed ankle fractures. Ann Chir Gynaecol. 2000;89:6–9. [PubMed] [Google Scholar]
- 14.Hoiness P, Engebretsen L, Stromsoe K. The influence of perioperative soft tissue complications on the clinical outcome in surgically treated ankle fractures. Foot Ankle Int. 2001;22:642–648. doi: 10.1177/107110070102200805. [DOI] [PubMed] [Google Scholar]
- 15.James LA, Sookhan N, Subar D. Timing of operative intervention in the management of acutely fractured ankles and the cost implications. Injury. 2001;32:469–472. doi: 10.1016/S0020-1383(00)00254-0. [DOI] [PubMed] [Google Scholar]
- 16.Kannus P, Palvanen M, Niemi S, Parkkari J, Jarvinen M. Increasing number and incidence of low-trauma ankle fractures in elderly people: Finnish statistics during 1970-2000 and projections for the future. Bone. 2002;31:430–433. doi: 10.1016/S8756-3282(02)00832-3. [DOI] [PubMed] [Google Scholar]
- 17.Konrath G, Karges D, Watson JT, Moed BR, Cramer K. Early versus delayed treatment of severe ankle fractures: a comparison of results. J Orthop Trauma. 1995;9:377–380. doi: 10.1097/00005131-199505000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Koval KJ, Zhou W, Sparks MJ, Cantu RV, Hecht P, Lurie J. Complications after ankle fracture in elderly patients. Foot Ankle Int. 2007;28:1249–1255. doi: 10.3113/FAI.2007.1249. [DOI] [PubMed] [Google Scholar]
- 19.Lamontagne J, Blachut PA, Broekhuyse HM, O’Brien PJ, Meek RN. Surgical treatment of a displaced lateral malleolus fracture: the antiglide technique versus lateral plate fixation. J Orthop Trauma. 2002;16:498–502. doi: 10.1097/00005131-200208000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Lynde MJ, Sautter T, Hamilton GA, Schuberth JM. Complications after open reduction and internal fixation of ankle fractures in the elderly. Foot Ankle Surg. 2012;18:103–107. doi: 10.1016/j.fas.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 21.Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control. 1999;27:97–132. doi: 10.1016/S0196-6553(99)70088-X. [DOI] [PubMed] [Google Scholar]
- 22.Miller AG, Margules A, Raikin SM. Risk factors for wound complications after ankle fracture surgery. J Bone Joint Surg Am. 2012;94:2047–2052. doi: 10.2106/JBJS.K.01088. [DOI] [PubMed] [Google Scholar]
- 23.Ovaska M, Lindahl J, Mäkinen T, Madanat R, Pulliainen L, Kiljunen V, Hirvensalo E, Tukiainen E. Postoperative infection after closed and open ankle fractures. Suomen Orthop Traumatol. 2011;34:30–33. [Google Scholar]
- 24.Pietzik P, Qureshi I, Langdon J, Molloy S, Solan M. Cost benefit with early operative fixation of unstable ankle fractures. Ann R Coll Surg Engl. 2006;88:405–407. doi: 10.1308/003588406X106504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saithna A, Moody W, Jenkinson E, Almazedi B, Sargeant I. The influence of timing of surgery on soft tissue complications in closed ankle fractures. Eur J Orthop Surg Traumatol. 2009;19:481–484. doi: 10.1007/s00590-009-0455-5. [DOI] [Google Scholar]
- 26.Schepers T, Van Lieshout EMM, De Vries MR, Van der Elst M. Increased rates of wound complications with locking plates in distal fibular fractures. Injury. 2011;42:1125–1129. doi: 10.1016/j.injury.2011.01.009. [DOI] [PubMed] [Google Scholar]
- 27.Singh BI, Balaratnam S, Naidu V. Early versus delayed surgery for ankle fractures: a comparison of results. Eur J Orthop Surg Traumatol. 2005;15:23–27. doi: 10.1007/s00590-004-0171-0. [DOI] [Google Scholar]
- 28.SooHoo NF, Krenek L, Eagan MJ, Gurbani B, Ko CY, Zingmond DS. Complication rates following open reduction and internal fixation of ankle fractures. J Bone Joint Surg Am. 2009;91:1042–1049. doi: 10.2106/JBJS.H.00653. [DOI] [PubMed] [Google Scholar]
- 29.Still GP, Atwood TC. Operative outcome of 41 ankle fractures: a retrospective analysis. J Foot Ankle Surg. 2009;48:330–339. doi: 10.1053/j.jfas.2009.02.005. [DOI] [PubMed] [Google Scholar]
- 30.Sukeik M, Qaffaf M, Ferrier G. Ankle fractures: impact of swelling on timing of surgery, length of hospital stay and the economic burden. Inj Extr. 2010;41:133. doi: 10.1016/j.injury.2010.07.419. [DOI] [Google Scholar]
- 31.Thomas G, Whalley H, Modi C. Early mobilization of operatively fixed ankle fractures: a systematic review. Foot Ankle Int. 2009;30:666–674. doi: 10.3113/FAI.2009.0666. [DOI] [PubMed] [Google Scholar]
- 32.Tonnesen H, Pedersen A, Jensen MR, Moller A, Madsen JC. Ankle fractures and alcoholism. The influence of alcoholism on morbidity after malleolar fractures. J Bone Joint Surg Br. 1991;73:511–513. doi: 10.1302/0301-620X.73B3.1670461. [DOI] [PubMed] [Google Scholar]
- 33.Van Schie-Van der Weert EM, Van Lieshout EMM, De Vries MR, Van der Elst M, Schepers T (2012) Determinants of outcome in operatively and non-operatively treated Weber-B ankle fractures. Arch Orthop Trauma Surg 132:257–263 [DOI] [PMC free article] [PubMed]
- 34.Wukich DK, Kline AJ. The management of ankle fractures in patients with diabetes. J Bone Joint Surg Am. 2008;90:1570–1578. doi: 10.2106/JBJS.G.01673. [DOI] [PubMed] [Google Scholar]