Abstract
Purpose
Individual physiological knee kinematics are highly variable in normal knees and are altered following cruciate-substituting (PS) and cruciate-retaining (CR) total knee arthroplasty (TKA). We wanted to know whether knee kinematics are different choosing two different knee designs, CR and PS TKA, during surgery using computer navigation.
Methods
For this purpose, 60 consecutive TKA were randomised, receiving either CR (37 patients) or PS TKA (23 patients). All patients underwent computer navigation, and kinematics were assessed prior to making any cuts or releases and after implantation. Outcome measures were relative rotation between femur and tibia, measured medial and lateral gaps and medial and lateral condylar lift-off.
Results
We were not able to demonstrate a significant difference in femoral external rotation between either group prior to implantation (7.9° CR vs. 7.4° PS) or after implantation (9.0° CR vs. 11.3° PS), both groups showed femoral roll-back. It significantly increased pre- to postoperatively in PS TKA. In the CR group both gaps increased, the change of the medial gap was significantly attributable to medial release. In the PS group both gaps increased and the change of the medial and of the lateral gap was significant. Condylar lift-off was observed in the CR group during 20° and 60° of flexion.
Conclusion
This study did not reveal significant differences in navigation-based knee kinematics between CR and PS implants. Femoral roll-back was observed in both implant designs, but significantly increased pre- to postoperatively in PS TKA. A slight midflexion instability was observed in CR TKA. Intra-operative computer navigation can measure knee kinematics during surgery before and after TKR implantation and may assist surgeons to optimise knee kinematics or identify abnormal knee kinematics that could be corrected with ligament releases to improve the functional result of a TKR, whether it is a CR or PS design. Our intra-operative finding needs to be confirmed using fluoroscopic or radiographic 3D matching after complete recovery from surgery.
Introduction
Total knee arthroplasty (TKA) is one of the most successful operative procedures over the last decades in orthopaedic surgery. Nevertheless, we have to deal with a relatively high number of unsatisfied TKA patients. Bourne et al. [1] indicate a proportion of 11 % to 18 %. Different reasons are held responsible for this: direct patient-dependent coefficiencies, as for example body mass index, activity level and preoperative expectations [2, 3] on one hand; and patient-independent factors including surgical technique [4] and implant design [5] on the other hand.
Preoperative and postoperative knee kinematics of osteoarthritic knees have shown a wide variety of results, such as mostly paradoxical forward slide of the femur during flexion [6, 8, 9], whereas normal knee kinematics describe an asymmetrical femoral roll-back mechanism during flexion, predominantly of the lateral femoral condyle [10, 12]. Using a magnetic resonance imaging (MRI) technique in cadaver and living knees, Hill [11] described a pattern of no anteroposterior movement medially, but a lateral roll-back combined with sliding laterally during flexion. After TKR using 3D matching techniques, Fitz et al. [13] detected tibial internal rotation during knee flexion using a new gap-balancing technique with a more anatomical restoration of the distal and posterior medial femoral condyle. In knees with standard TKR, they predominantly found tibial external rotation during flexion [13].
The purpose of this prospective, randomised study was to describe intra-operative knee kinematics using computer assisted kinematic software. Our hypothesis was that there are different knee kinematics between cruciate-retaining (CR) and cruciate-substituting (PS) TKR designs; specifically, (1) different femoral external rotation with flexion, (2) different gaps and (3) different lift-off. Furthermore, we postulated that there were no kinematic differences prior to implantation or any differences in clinical outcome measures (Knee Society Score [KSS], Western Ontario and McMaster Universities Osteoarthritis Index [WOMAC]) prior to and after the latest follow-up between both groups.
Materials and methods
In this prospective study, we recruited 60 patients with primary osteoarthritis of the knee designated for total knee arthroplasty within a three months period. Patients older than 85 years of age, patients with secondary osteoarthritis of the knee, severe varus or valgus deformity (> 15 degrees) requiring a hinged implant, or patients not willing to participate were excluded from the study. Eleven patients out of the total had to be excluded due to the reasons mentioned above.
Patients provided informed consent to this study, which was approved by the ethical committee of our Institute (Ethic Committee Approv. Number: 10-101-0240).
All 60 patients received a standard, cemented condylar prosthesis with fixed platform (PFC Sigma, DePuy, Warsaw, IN), either cruciate-retaining (CR, 37 knees, group 1) or cruciate-substituting (PS, 23 knees, group 2) depending on computerised randomisation or stability needs. Two patients randomised to the cruciate-retaining group received a cruciate-substituting implant due to an insufficient posterior cruciate ligament. No patella replacements were used. All of the operations were performed under the direction of the senior author using a standard medial parapatellar approach. After exposing the knee, two passive optical reference arrays were attached on the medial distal femur and the medial proximal tibia. After approval of the centre of the hip joint by circumduction, the required anatomical landmarks (femoral epicondyles, anterior femoral cortex, medial and lateral malleolus, tibal plateau magnitude and anterior tibial cortex) were acquired. The following kinematic test included passive range of motion (ROM) from maximum extension to maximum flexion, during which the relative orientation between femur and tibia was displayed in real-time. The relative position of both condyles relative to the tibia were measured to see whether the condyles moved backward with increased flexion. Furthermore, the height of the medial and lateral gap was recorded, measuring the deepest points of the medial and lateral condyles in relationship to the tibial component. The difference between medial and lateral measurements was considered to represent condylar lift-off if it was greater than one millimetre. The gaps were analysed every ten degrees between 0° and 130° of flexion.
This first kinematic test was performed before cutting the anterior cruciate ligament.
The surgical technique was navigation-based, using a tibia first approach according to the navigation target (postoperative leg axis). After the tibal cut, all osteophytes were removed and a medial (varus knees) or lateral (valgus knees) release was performed. Next, a tensiometer with metric scale to match extension and flexion gap with a distraction force of 90 N was inserted and gaps recorded. The distal femoral cut was then performed according to the navigation target. According to flexion and extension gap, the anterior and posterior femoral cuts were performed.
After implantation of the prosthesis the kinematic test was repeated.
The kinematic elaboration was based on the analysis of passive ROM. For each patient, the combination of movements was registered three times.
Intraoperative passive kinematics were measured by the BrainLab surgical navigation system [Knee 2.1 BrainLab, Feldkirchen, Germany] and analysed by the corresponding software. The system includes an optoelectronic localiser, two removable reference arrays (fixed on the femur and tibia using 7-mm Schanz screws), and a probe, all equipped with passive optical markers. The software allows anatomical and kinematic data acquisitions and provides real-time display of knee alignment during surgery (Fig. 1) and standard kinematic evaluations.
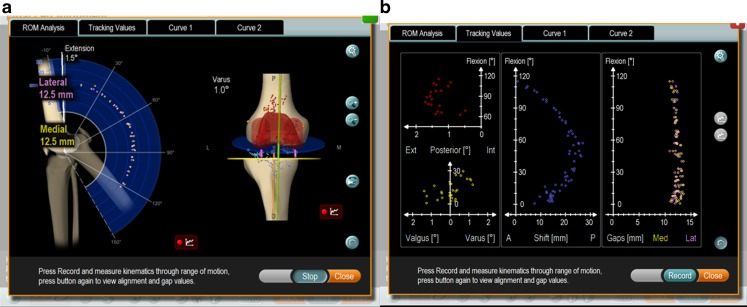
Fig. 1.
Intraoperative kinematics. a shows the medial and lateral gap width during knee flexion and extension. b shows the gaps and the femoral shift during knee movement
All kinematic analyses were recorded after temporarily occlusion of the joint capsule by clamping jaws. We used an electric leg holder for extension and flexion of the knee.
The patients were evaluated preoperatively and six months postoperatively, according to the Knee Society Clinical rating system [14] and the WOMAC rating system [15]. The results were assessed in the outpatient clinic by an independent blinded investigator. No patient was lost during follow-up.
Statistical analysis: we used the Sigma Plot statistical software version (Systat Software Inc., San Jose, USA). For within-group comparisons, we performed a paired t-test or a Wilcoxon signed rank test. A p(robability) value < 0.05 was considered to be of statistical significance.
Results
Demographic data
The patient population consisted of 26 women and 34 men with an average age of 70.0 years (range, 52–82 years). The average follow-up was six months (range, five to eight months).
Both groups were comparable with regard to age, gender and outcome measures, such as KSS and WOMAC score. The preoperative range of motion for both groups was also equal preoperatively (average of extension/flexion of 0° - 6° - 108° in group 1, average of extension/flexion of 0° - 8° - 104° in group 2) and postoperatively at six months (average of extension/flexion of 0° - 3° - 111° in group 1, average of extension/flexion of 0° - 1° - 108° in group 2). (Table 1).
Table 1.
Demographic data and range of motion (ROM)
| CR group | PS group | p-value | |
|---|---|---|---|
| Age at index operation | 70.5 Min: 56, Max: 82 | 69.0 Min: 50, Max: 82 | > 0.05 |
| ROM preoperatively | 0°/6°/108° (min: 0° extension, max: 115° flexion) | 0°/8°/104° (min: 0° extension, max: 112° flexion) | > 0.05 |
| ROM 6 months postoperatively | 0°/3°/111° (min: 0° extension, max: 130° flexion) | 0°/1°/108° (min: 0° extension, max: 125° flexion) | > 0.05 |
CR cruciate-retaining; PS cruciate-substituting
Knee society score
Overall postoperative knee score and function score showed a significant improvement compared to preoperative scores (p< 0.05) (Table 2).
Table 2.
Knee Society Score
| CR group | PS group | p-value | |
|---|---|---|---|
| Knee Score preop | 52.2 (min: 24, max: 64) | 54.0 (min: 8, max: 75) | > 0.05 |
| Knee Score 6 months | 83.6 (min: 50, max: 110) | 79.4 (min: 49, max. 88) | > 0.05 |
| Function Score preop | 54.8 (min: 0 max: 80) | 55.3 (min: 20, max: 80) | > 0.05 |
| Function Score 6 month | 76.0 (min: 40, max: 100) | 74.0 (min: 20, max: 100) | > 0.05 |
CR cruciate-retaining; PS cruciate-substituting
The average preoperative knee score was 52.9 points (range, 24–75), the function score was 55.0 points (range, 0–80). The average postoperative knee score was 82.0 points (range, 49–110), the function score was 75.2 points (range, 20–100)
WOMAC scores
The postoperative WOMAC score showed a significant improvement compared to preoperative scores (p< 0.05) (Table 3).
Table 3.
Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) Score
| WOMAC total | CR group | PS group | p-value |
|---|---|---|---|
| preop | 41.8 (min: 29, max: 60) | 40.2 (min: 27, max: 60) | > 0.05 |
| 6 months | 26.8 (min: 12, max: 51) | 25.8 (min: 11, max: 46) | > 0.05 |
CR cruciate-retaining; PS cruciate-substituting
The average preoperative WOMAC score was 41.2 points (range, 27–60), the average postoperative WOMAC score was 26.4 points (range, 11–51)
Scores were comparable between both groups.
Complications
Three patients (5 %) suffered from complications during the postoperative period. Reoperation for haematoma was necessary in two knees (3 %).
One patient suffered from deep vein thrombosis. After wound healing, the heparin injections were converted to oral anticoagulation medication.
Kinematics
Femoral rotation/roll-back
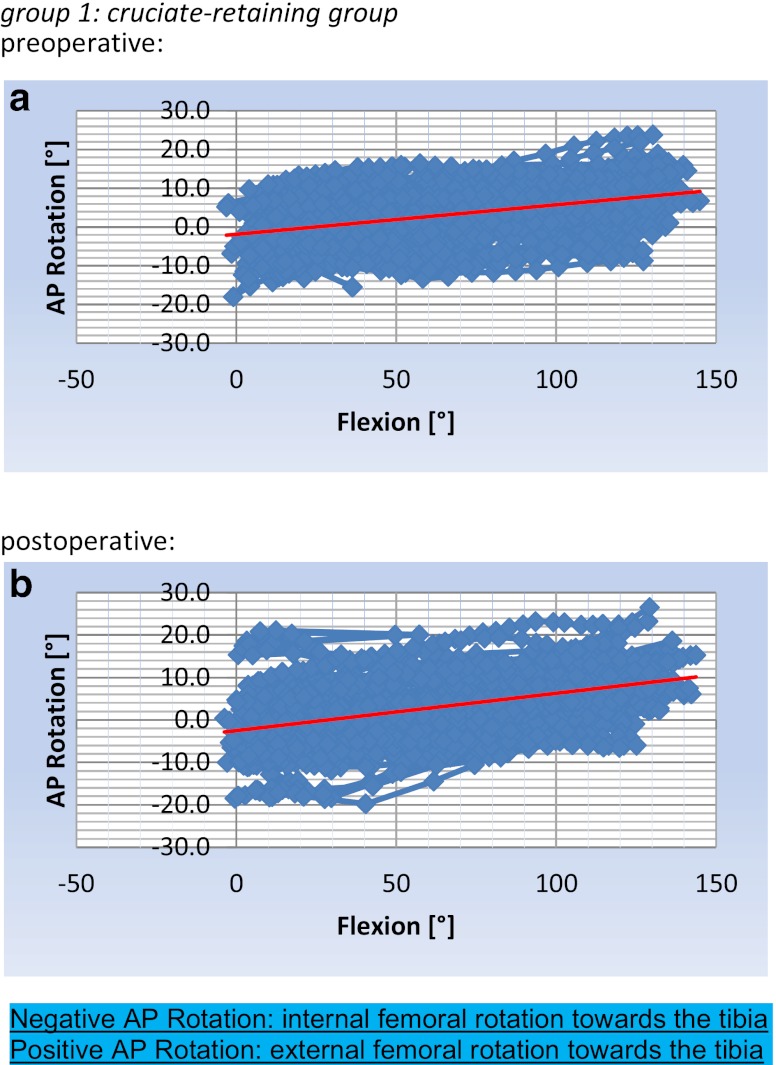
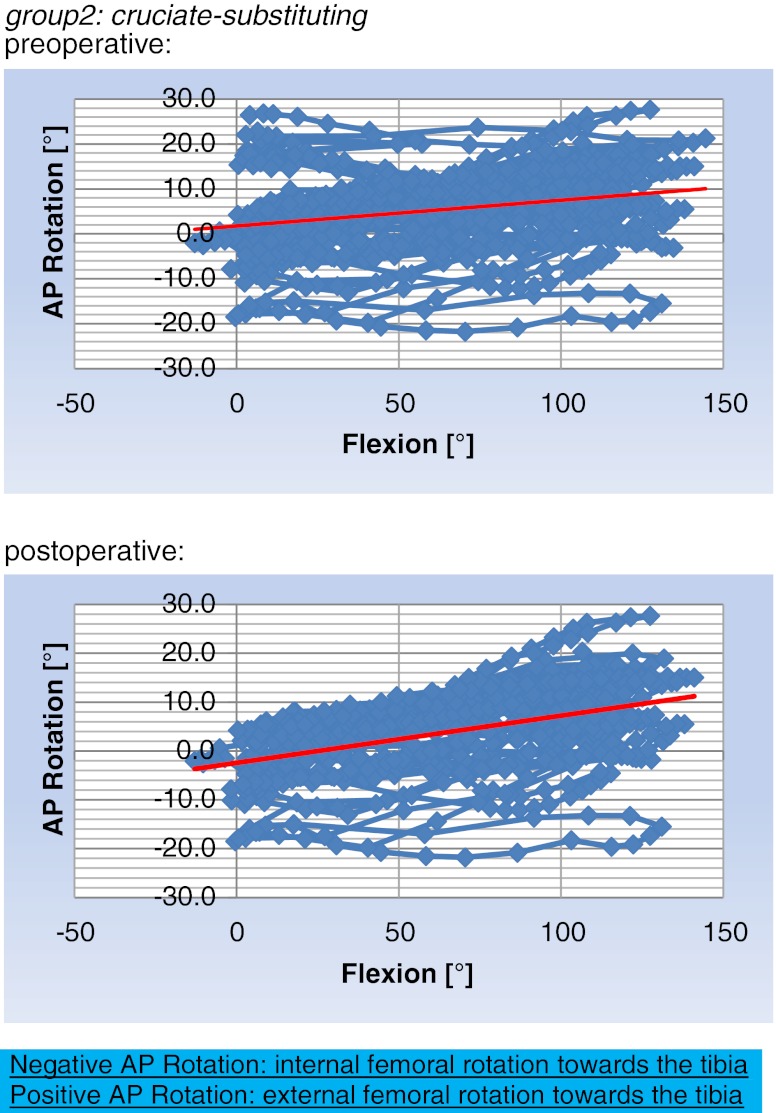
Preoperatively, there were no differences with regard to femoral external rotation during flexion in either group. Postoperatively, femoral external rotation during knee flexion showed a slight external rotational movement in both groups (Figs. 2 and 3). The change in femoral external rotation pre-implantation to post-implantation, however, was only significant in the PS group (p<0.05).
Fig. 2.
Movement pattern of the femoral bone towards the tibia during knee flexion in group 1, as shown by the trendline. a shows tibiofemoral kinematics preimplantation;b shows the kinematics postimplantation
Fig. 3.
Movement pattern of the femoral bone towards the tibia during knee flexion in group 2, as shown by the trendline. a shows tibiofemoral kinematics preimplantation; b shows the kinematics postimplantation
CR group
Preoperatively, the femoral rotation during knee flexion increased from 1.9° (SD 2.0°) internal rotation at 0° of flexion to 7.9° (SD 3.3°) external rotation at 130° of flexion.
Postoperatively, the femoral rotation during knee flexion increased from 2.5° (SD 1.4°) internal rotation at 0° of flexion to 9.0° (SD 3.1°) external rotation at 130° of flexion.
PS group
Preoperatively, the femoral rotation during knee flexion increased from 1.7° (SD 1.7°) internal rotation at 0° of flexion to 7.4° (SD 4.1°) external rotation at 130° of flexion.
Postoperatively, the femoral rotation during knee flexion increased from 0.1° (SD 0.3°) external rotation at 0° of flexion to 11.3° (SD 3.8°) external rotation at 130° of flexion. The flexion angle where cam-post engagement was observed was between 80° (5.3° external rotation) and 100° (8.1° external rotation) of flexion.
The within group comparison showed no significance between the CR and the PS group before and after implantation of the prosthesis. Both groups showed femoral external rotation with flexion and differences were not significantly different.
Gaps
In our CR cohort, the medial gap increased from 7.3 mm (± 1.1 mm) to 10.9 mm (± 0.4 mm) after the implantation attributable to medial release. The change of the medial gap was significant (p< 0.05). The lateral gap changed from 11.4 mm (± 1.0 mm) to post implantation 11.9 mm (± 0.3 mm). The change was not significant (p= 0.09).
In our PS cohort, the medial gap increased from 7.9 mm (± 1.3 mm) to 12.2 mm (± 0.3 mm) after the implantation attributable to medial release. The change of the medial gap was significant (p< 0.05). The lateral gap changed from 11.8 mm (± 1.5 mm) to post implantation 12.8 mm (± 0.4 mm). The change of the lateral gap was significant (p< 0.05).
Condylar lift-off
Comparing the gaps at different degrees of flexion and extension, we found a lateral condylar lift-off in patients with the CR implants, but not in the PS group, between 20° and 60° of flexion after the implantation. The average difference between medial and lateral gap was 1.1 mm between this range of motion and 1.0 mm or below at full extension and deep flexion (Table 4). The difference was significant (p<0.05).
Table 4.
Condylar lift-off during knee flexion in the cruciate-retaining (CR) group
| cruciate-retaining: | |||||
| average | |||||
| GAPS | pre | post | |||
| MedGap | LatGap | MedGap | LatGap | ||
| degree of | |||||
| flexion | Condylar lift off | ||||
| 0° | 7.4 | 10.2 | 10.2 | 11 | 0.8 |
| 10° | 7.2 | 11.2 | 10.4 | 11.5 | 0.8 |
| 20° | 7.5 | 11.1 | 10.6 | 11.7 | 1.1 |
| 30° | 7.6 | 11 | 10.7 | 11.8 | 1.1 |
| 40° | 7.3 | 11.1 | 10.7 | 11.8 | 1.1 |
| 50° | 6.9 | 11.1 | 10.7 | 11.9 | 1.2 |
| 60° | 6.6 | 11.1 | 10.9 | 12 | 1.1 |
| 70° | 6.3 | 10.9 | 11.1 | 12.1 | 1 |
| 80° | 6.1 | 10.8 | 11.1 | 12 | 0.9 |
| 90° | 6.3 | 11 | 11.2 | 12 | 0.8 |
| 100° | 6.7 | 11.3 | 11.3 | 12 | 0.7 |
| 110° | 7.6 | 12.2 | 11.3 | 12.1 | 0.8 |
| 120° | 8.9 | 13.1 | 11.3 | 12.1 | 0.8 |
| 130° | 10.1 | 14.1 | 11.4 | 12.2 | 0.8 |
In patients with the cruciate-substituting implant, no condylar lift-off after the implantation was detected (Table 5).
Table 5.
Condylar lift-off during knee flexion in the cruciate-substituting (PS) group
| cruciate-substituting: | |||||
| average | |||||
| GAPS | pre | post | |||
| MedGap | LatGap | MedGap | LatGap | ||
| degree of | |||||
| flexion | Condylar lift off | ||||
| 0° | 9.5 | 11.2 | 12.3 | 13.2 | 0.9 |
| 10° | 8.1 | 11.4 | 11.7 | 12.7 | 1 |
| 20° | 7.1 | 10.8 | 11.8 | 12.5 | 0.7 |
| 30° | 7.4 | 10.8 | 12 | 12.6 | 0.6 |
| 40° | 7.3 | 10.7 | 12 | 12.5 | 0.5 |
| 50° | 7.2 | 10.8 | 12 | 12.5 | 0.5 |
| 60° | 6.9 | 10.9 | 12 | 12.4 | 0.4 |
| 70° | 6.8 | 10.8 | 12.1 | 12.4 | 0.3 |
| 80° | 6.7 | 11.1 | 12.2 | 12.4 | 0.2 |
| 90° | 6.9 | 11.5 | 12.5 | 12.9 | 0.4 |
| 100° | 7.3 | 12.1 | 12.3 | 12.7 | 0.4 |
| 110° | 8.2 | 13.3 | 12.4 | 12.9 | 0.5 |
| 120° | 9.7 | 14.9 | 12.6 | 13.1 | 0.5 |
| 130° | 11 | 15.2 | 13 | 13.7 | 0.7 |
Discussion
Knee kinematics has become the focus of attention in total knee arthroplasty, as more physiological movement patterns might correlate with better postoperative knee function [16].
The main research method is in vivo fluoroscopic or gait analysis. Studies involved normal knees [17], cruciate ligament-deficient knees [18–20], and knees with a unicondylar [21] or bicondylar total knee arthroplasty [6, 21–23].
Normal knee kinematics show a roll-back of the femur, especially of the lateral femoral condyle, concomitant with tibial internal rotation during knee flexion [17].
Anterior cruciate ligament-deficient knees, however, show a marked posterior translation of the medial condyle compared to normal knees, where the posterior femoral translation of the lateral condyle remains dominant [20].
Studies of knee joints with a total knee arthroplasty revealed a variety of kinematic patterns from almost physiological sequences up to paradoxical anterior slide of the femoral condyles during flexion and opposite axial rotation [24]. Compared to healthy knees, the range of motion is diminished in almost all total resurfaced knees.
So far, little is known about intraoperative kinematics of TKA and the influence of cruciate-substituting or cruciate-sacrificing implants.
Some studies claim a more physiological kinematic pattern with a greater range of motion for posterior stabilised total knee arthroplasties compared to cruciate-retaining total knee arthroplasties [25, 26]. However, measurements under weightbearing conditions revealed a reduction of the observed range of motion and showed similar kinematic patterns of posterior stabilised and cruciate-retaining total knee arthroplasties in early flexion activities such as gait [22].
Banks [7] described similar axial rotation and condylar translation of knees after TKA with retention of the bony insertion of the posterior-cruciate ligament compared to normal and anterior cruciate-deficient knees. Axial rotations and condylar translations decreased when the PCL was recessed, which describes the cam-post mechanism.
The hypothesis of our study was that there are different knee kinematics between CR and PS TKR designs; specifically, (1) different femoral external rotation with flexion, (2) different gaps and (3) different lift-off.
As regards intraoperative navigation based knee kinematics between CR and PS TKR designs specifically, we found overlap and differences: both types of implants revealed an increased external rotation of the femur towards the tibia (femoral roll-back) during knee flexion.
A significant difference of femoral roll-back during knee flexion comparing preimplantation and postimplantational kinematics of the prosthesis could only be detected in the PS group of patients (from 7.4° to 11.3° of external rotation at 130° of knee flexion). A reason for this could be a more abnormal kinematic pattern preoperatively because of an insufficient posterior cruciate ligament. Furthermore, our results confirm the cam-post mechanism [29], with posterior femoral roll-back during flexion being more consistent with normal knees.
Although the trendline in the diagrams shown above (Figs. 2 and 3) indicates an approach to normal knee kinematics with lateral femoral roll-back and tibial internal rotation during flexion, we asked how physiological this combination of movements is. Our results confirm published results of highly variable knee kinematics with a wide range of internal-external femoral and tibial rotation. This variable movement pattern was also detected in several in vitro studies. Li G et al. [30] found in 13 cadaveric human knees a posterior translation of the lateral femoral condyle of 6.7 mm (± 6.2 mm) at 90 degrees of knee flexion after total knee arthroplasty. Compared to intact knees, the lateral roll back mechanism was significantly lower than the mean of 13.8 mm (± 7.0 mm). The same group [29] detected a significantly lower posterior translation of both femoral condyles in knees after a total knee arthroplasty compared to native knees. They found out that the cam-post engagement of PS implants occurred between 60 and 90 degrees of flexion followed by an increase in femoral roll-back of both condyles.
After implantation of the prosthesis the posterior translation of the femoral condyles increased. Femoral external rotation during knee flexion was higher in the PS group compared to the CR group (11.3° compared to 9.0°). Taking into account the results of other kinematic studies, a femoral roll-back mechanism during knee flexion after total knee arthroplasty is described predominantly [16, 27, 28].
We found balanced medial and lateral gaps in flexion and extension as suggested by implantation technique post implantation contrary to the hypothesis of different gaps and condylar lift-off for CR and PS TKR. However, a slight condylar lift-off was detected in the early stage of flexion (“midflexion”) in patients with the CR implant. There was no condylar lift-off in patients with the PS implant. This might be attributed to a more constrained conduction in the medial-lateral axis. Furthermore a too tight or too loose PCL might have contributed to lift-off. Previous studies observed lift-off up to 50 %–86 % of cruciate-retaining total knee arthroplasties [27, 31, 32]. The average amount of condylar lift-off was 0.87 mm, which is low compared to other study groups [27, 31] where an average lift-off between one and two millimetres is described. However these authors based their measurements on weight-bearing activities under fluoroscopic analysis. Furthermore Schnurr et al. [33] observed that a release or resection of the posterior cruciate ligament increases the flexion/extension gap ratio, but with no prediction on the individual effect.
We could confirm our hypothesis that there were no kinematic differences prior to implantation or any differences in clinical outcome measures (KSS, WOMAC) prior to and after latest follow-up between both groups.
There are several limitations of our study. First of all, the follow-up period was only six months.
Second, we document intraoperative kinematics, but we do not know whether the intra-operative kinematic pattern persists during recovery. After rehabilitation, knee kinematics may change again. To assess our findings, a CAS software enabling a single analysis of the medial and of the lateral femoral condyle would be helpful, and has been implemented by us in a new prospective study recently.
Third, our kinematic results are recorded under passive ROM and not weightbearing. This needs to be shown in either gait analysis or 3D matching using radiographic examinations after complete rehabilitation and recovery. Most published kinematic analysis is based on weight-bearing films, making it difficult to compare our findings. Johal et al. [12] compared tibiofemoral movement in ten weightbearing and nonweightbearing Caucasian knees using MRI. They found tibial internal rotation during flexion in both groups; however, with a earlier and greater magnitude of rotation in the weightbearing group.
Furthermore, we would advise caution comparing the condylar lift-off results with other study groups [19, 27, 28]. Different measuring techniques from the distance of the lowest point of the medial and lateral condyle to the closest point on the tibial PE insert or to the tibial plateau are described.
However, to our best knowledge, this is the first study comparing intra-operative kinematics between CR and PS implant designs so far.
This study did not reveal significant differences in navigation-based knee kinematics between CR and PS implants. Femoral roll-back was observed in both implant designs, but significantly increased from preoperatively to postoperatively solely in PS TKA. A slight midflexion instability was observed in CR TKA. Intra-operative computer navigation can measure knee kinematics during surgery before and after TKR implantation, and may assist surgeons to optimise knee kinematics or identify abnormal knee kinematics, which could be corrected with ligament releases to improve the functional result of a TKR, whether it is a CR or PS design. Further research is necessary; specifically, whether our intra-operatively observed knee kinematics are preserved after rehabilitation.
Acknowledgments
We would like to thank Mr Sven Buhk for his support and great convenience and work throughout the study.
References
- 1.Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KDJ. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468:57–63. doi: 10.1007/s11999-009-1119-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lopez-Olivo MA, Landon GC, Siff SJ, Edelstein D, Pak C, Kallen MA, Stanley M, Zhang H, Robinson KC, Suarez-Almazor ME. Psychosocial determinants of outcomes in knee replacement. Ann Rheum Dis. 2011;70:1775–1781. doi: 10.1136/ard.2010.146423. [DOI] [PubMed] [Google Scholar]
- 3.Culliton SE, Bryant DM, Overend TJ, Macdonald SJ, Chesworth BM (2011) The Relationship Between Expectations and Satisfaction in Patients Undergoing Primary Total Knee Arthroplasty. J Arthroplasty [DOI] [PubMed]
- 4.Clarke HD, Scuderi GR. Flexion instability in primary total knee replacement. J Knee Surg. 2003;16:123–128. [PubMed] [Google Scholar]
- 5.Liu Y-L, Chen W-C, Yeh W-L, McClean CJ, Huang C-H, Lin K-J, Cheng C-K. Mimicking anatomical condylar configuration into knee prosthesis could improve knee kinematics after TKA - A computational simulation. Clinical Biomechanics. Bristol: Avon; 2011. [DOI] [PubMed] [Google Scholar]
- 6.Bellemans J, Banks S, Victor J, Vandenneucker H, Moemans A. Fluoroscopic analysis of the kinematics of deep flexion in total knee arthroplasty. Influence of posterior condylar offset. J Bone Joint Surg Br. 2002;84:50–53. doi: 10.1302/0301-620X.84B1.12432. [DOI] [PubMed] [Google Scholar]
- 7.Banks SA, Markovich GD, Hodge WA. In vivo kinematics of cruciate-retaining and -substituting knee arthroplasties. J Arthroplasty. 1997;12:297–304. doi: 10.1016/S0883-5403(97)90026-7. [DOI] [PubMed] [Google Scholar]
- 8.Massin P, Boyer P, Sabourin M (2011) Less femorotibial rotation and AP translation in deep-dished total knee arthroplasty. An intraoperative kinematic study using navigation. Knee Surg Sports Traumatol Arthrosc Off J ESSKA [DOI] [PubMed]
- 9.Yue B, Varadarajan KM, Rubash HE, Li G. In vivo function of posterior cruciate ligament before and after posterior cruciate ligament-retaining total knee arthroplasty. Int Orthop. 2012;36:1387–1392. doi: 10.1007/s00264-011-1481-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Freeman MAR, Pinskerova V. The movement of the normal tibio-femoral joint. J Biomech. 2005;38:197–208. doi: 10.1016/j.jbiomech.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 11.Hill PF, Vedi V, Williams A, Iwaki H, Pinskerova V, Freeman MA. Tibiofemoral movement 2: the loaded and unloaded living knee studied by MRI. J Bone Joint Surg Br. 2000;82:1196–1198. doi: 10.1302/0301-620X.82B8.10716. [DOI] [PubMed] [Google Scholar]
- 12.Johal P, Williams A, Wragg P, Hunt D, Gedroyc W. Tibio-femoral movement in the living knee. A study of weight bearing and non-weight bearing knee kinematics using “interventional” MRI. J Biomech. 2005;38:269–276. doi: 10.1016/j.jbiomech.2004.02.008. [DOI] [PubMed] [Google Scholar]
- 13.Fitz W, Sodha S, Reichmann W, Minas T. Does a modified gap-balancing technique result in medial-pivot knee kinematics in cruciate-retaining total knee arthroplasty? A pilot study. Clin Orthop Relat Res. 2012;470:91–98. doi: 10.1007/s11999-011-2121-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14 [PubMed]
- 15.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 16.Suggs JF, Hanson GR, Park SE, Moynihan AL, Li G. Patient function after a posterior stabilizing total knee arthroplasty: cam-post engagement and knee kinematics. Knee Surg Sports Traumatol Arthrosc. 2008;16:290–296. doi: 10.1007/s00167-007-0467-9. [DOI] [PubMed] [Google Scholar]
- 17.Komistek RD, Dennis DA, Mahfouz M (2003) In vivo fluoroscopic analysis of the normal human knee. Clin Orthop Relat Res 69–81 [DOI] [PubMed]
- 18.Mahfouz MR, Komistek RD, Dennis DA, Hoff WA. In vivo assessment of the kinematics in normal and anterior cruciate ligament-deficient knees. J Bone Joint Surg Am. 2004;86-A(Suppl 2):56–61. doi: 10.2106/00004623-200412002-00009. [DOI] [PubMed] [Google Scholar]
- 19.Dennis DA, Mahfouz MR, Komistek RD, Hoff W. In vivo determination of normal and anterior cruciate ligament-deficient knee kinematics. J Biomech. 2005;38:241–253. doi: 10.1016/j.jbiomech.2004.02.042. [DOI] [PubMed] [Google Scholar]
- 20.Li G, Moses JM, Papannagari R, Pathare NP, DeFrate LE, Gill TJ. Anterior cruciate ligament deficiency alters the in vivo motion of the tibiofemoral cartilage contact points in both the anteroposterior and mediolateral directions. J Bone Joint Surg Am. 2006;88:1826–1834. doi: 10.2106/JBJS.E.00539. [DOI] [PubMed] [Google Scholar]
- 21.Casino D, Martelli S, Zaffagnini S, Lopomo N, Iacono F, Bignozzi S, Visani A, Marcacci M. Knee stability before and after total and unicondylar knee replacement: in vivo kinematic evaluation utilizing navigation. J Orthop Res. 2009;27:202–207. doi: 10.1002/jor.20746. [DOI] [PubMed] [Google Scholar]
- 22.Dennis DA, Komistek RD, Mahfouz MR, Walker SA, Tucker A (2004) A multicenter analysis of axial femorotibial rotation after total knee arthroplasty. Clin Orthop Relat Res 180–189 [DOI] [PubMed]
- 23.Sumino T, Gadikota HR, Varadarajan KM, Kwon Y-M, Rubash HE, Li G. Do high flexion posterior stabilised total knee arthroplasty designs increase knee flexion? A meta analysis. Int Orthop. 2011;35:1309–1319. doi: 10.1007/s00264-011-1228-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dennis DA, Komistek RD, Mahfouz MR, Haas BD, Stiehl JB (2003) Multicenter determination of in vivo kinematics after total knee arthroplasty. Clin Orthop Relat Res 37–57 [DOI] [PubMed]
- 25.Dennis DA, Komistek RD, Colwell CE Jr, Ranawat CS, Scott RD, Thornhill TS, Lapp MA (1998) In vivo anteroposterior femorotibial translation of total knee arthroplasty: a multicenter analysis. Clin Orthop Relat Res 47–57 [DOI] [PubMed]
- 26.Victor J, Banks S, Bellemans J. Kinematics of posterior cruciate ligament-retaining and -substituting total knee arthroplasty: a prospective randomised outcome study. J Bone Joint Surg Br. 2005;87:646–655. doi: 10.1302/0301-620X.87B5.15602. [DOI] [PubMed] [Google Scholar]
- 27.Bertin KC, Komistek RD, Dennis DA, Hoff WA, Anderson DT, Langer T. In vivo determination of posterior femoral rollback for subjects having a NexGen posterior cruciate-retaining total knee arthroplasty. J Arthroplasty. 2002;17:1040–1048. doi: 10.1054/arth.2002.35793. [DOI] [PubMed] [Google Scholar]
- 28.Schmidt R, Komistek RD, Blaha JD, Penenberg BL, Maloney WJ (2003) Fluoroscopic analyses of cruciate-retaining and medial pivot knee implants. Clin Orthop Relat Res 139–147 [DOI] [PubMed]
- 29.Li G, Most E, Otterberg E, Sabbag K, Zayontz S, Johnson T, Rubash H (2002) Biomechanics of posterior-substituting total knee arthroplasty: an in vitro study. Clin Orthop Relat Res 214–225 [DOI] [PubMed]
- 30.Li G, Zayontz S, DeFrate LE, Most E, Suggs JF, Rubash HE. Kinematics of the knee at high flexion angles: an in vitro investigation. J Orthop Res. 2004;22:90–95. doi: 10.1016/S0736-0266(03)00118-9. [DOI] [PubMed] [Google Scholar]
- 31.Moynihan AL, Varadarajan KM, Hanson GR, Park S-E, Nha KW, Suggs JF, Johnson T, Li G. In vivo knee kinematics during high flexion after a posterior-substituting total knee arthroplasty. Int Orthop. 2010;34:497–503. doi: 10.1007/s00264-009-0777-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dennis DA, Komistek RD, Walker SA, Cheal EJ, Stiehl JB. Femoral condylar lift-off in vivo in total knee arthroplasty. J Bone Joint Surg Br. 2001;83:33–39. doi: 10.1302/0301-620X.83B1.10632. [DOI] [PubMed] [Google Scholar]
- 33.Schnurr C, Eysel P, König DP. Is the effect of a posterior cruciate ligament resection in total knee arthroplasty predictable? Int Orthop. 2012;36:83–88. doi: 10.1007/s00264-011-1295-6. [DOI] [PMC free article] [PubMed] [Google Scholar]