Abstract
Purpose
The number of candidates for a total hip arthroplasty (THA) is steadily increasing, while the average patient age is decreasing for primary THA. The rise in THA is mainly due to excellent clinical outcomes and the extended longevity of modern implants. Short stem arthroplasties with predominantly metaphyseal fixation such as the Metha® stem are suggested for young patients. It is hypothesised that the more physiological load transfer of these devices reduces stress shielding, which in turn may reduce the risk of aseptic loosening. However, patients with femoral deformities often require a deviation of the resection height. To this end, our aim was to evaluate how resection height influences strain patterns in order to characterise possible limits for short stem implantation.
Methods
Biomechanical testing using ten strain gauges on synthetic bone illustrated the strain patterns of three different resection heights (0, +5 and +10 mm) for the Metha stem.
Results
The greatest differences in strains were displayed at the “high” (most proximal) resection height (+10 mm) when compared to the non-implanted strain pattern. At the medial calcar, the strain was 143 % for +10 mm, 96 % for +5 mm and 94 % for 0 mm. Overall, discrepancies were less for deeper resections.
Conclusions
The deeper the resection, the more similar the strain patterns are when compared to a non-implanted synthetic bone. Changes in strain patterns are induced by variation in the varus/valgus positioning of the implant and by different offsets.
Introduction
Short stem total hip arthroplasty (THA) based on a metaphyseal anchorage appears to be an encouraging alternative hip replacement for young patients with osteoarthritis [3, 7, 9, 12, 19, 21]. The primary aims of implants of this type are better preservation of bone stock and a supposed reduction of stress shielding due to periprosthetic bone remodelling following cementless THA, which induces an alteration of physiological strains. Aseptic loosening is considered as a possible consequence of stress shielding. Thus, modern THA designs aim to induce a proximal load transfer to the proximal femur [1]. During the last decade, many different designs of short stem arthroplasty have been developed. Based on a publication of good results of the Mayo stem, the pioneering short stem implant which displayed a 94 % survival rate after 6.2 years [19], more short stem THA designs followed based on similar loading principles [12]. Investigations based on clinical [3, 7, 8, 12, 19, 22], biomechanical [10, 23, 24] and dual-energy X-ray absorptiometry (DXA) data [2, 16, 17] revealed promising outcomes with good bony ingrowth. Still the biomechanical loading patterns of these implant designs are relatively uncharacterised.
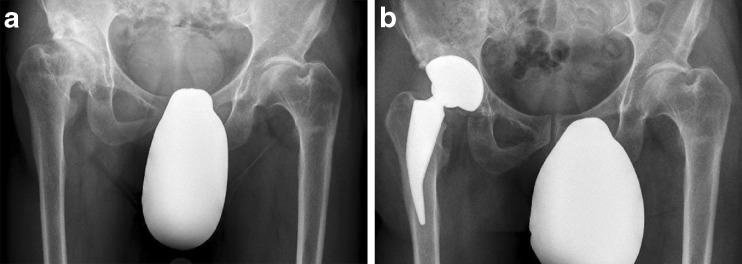
The implantation of such short stem THAs is currently recommended for patients with physiologically shaped proximal femora [3, 19]. However, the indication for THA in young patients is often given due to secondary osteoarthritis. In many of these cases, the anatomy is non-physiological (Fig. 1a). Thus, deformities of the proximal femur may lead to unconventional implantation of short stem THAs (Fig. 1b). For fixation of short stem implants such as the Metha® stem (Aesculap, Tuttlingen, Germany), a cortical ring of about 5 mm is recommended for primary metaphyseal fixation. However, in secondary coxarthrosis with femoral deformities, a lower resection height may be necessary (Fig. 1b) to reconstruct the offset and set the limb length. Nevertheless, according to our experience these cases reveal good clinical outcomes. It remains unclear how different resection heights affect load transfer and stress shielding patterns, which are generally thought to have a considerable effect on aseptic loosening.
Fig. 1.
a, b X-ray of a hip joint before (a) and after (b) implantation of the Metha short stem; due to the non-physiological anatomy a lower resection height was necessary to restore biomechanics and limb length
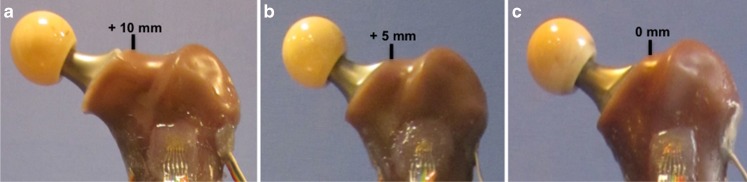
The aim of this study was to determine the influence of resection height (Fig. 2a–c) on strain patterns after implantation of the Metha short stem using strain gauges in synthetic bone in order to acquire details of load transfer. The results should lead to an improved understanding of stress shielding.
Fig. 2.
a–c Anterior view of three synthetic femora after implantation of the Metha short stem with different resection heights: +10 mm (a), + 5 mm (b) and 0 mm (c) compared to the notch of the femoral neck
Materials and methods
The femoral component of a size 4 short stem THA system (Metha, Aesculap, Tuttlingen, Germany) with a caput-collum-diaphyseal (CCD) angle of 130° was implanted in three synthetic femora (fourth-generation left adult composite femur, length 485 mm, Sawbones Europe, Malmö, Sweden). This implant is a short cementless hip prosthesis stem, which is anchored directly within the closed ring of the femoral neck and metaphysis. A special device was manufactured to fix the femora in a metal cylinder 120 mm in height and 70 mm in diameter. After resection of the femoral condyles, the distal segment was embedded in this standardised position (sagittal and frontal plane at 0°) using methylmethacrylate (Technovit 4004, Heraeus Kulzer GmbH, Wehrheim, Germany). The distance extending from proximal potting to the notch of the neck was 300 mm. Testing was first conducted on non-implanted, synthetic femora, after which testing was conducted with the stem implanted at a high resection height (+10 mm compared to the notch of the femoral neck), a median (+5 mm) and low (0 mm) resection height in one of the three femora (Fig. 2a–c).
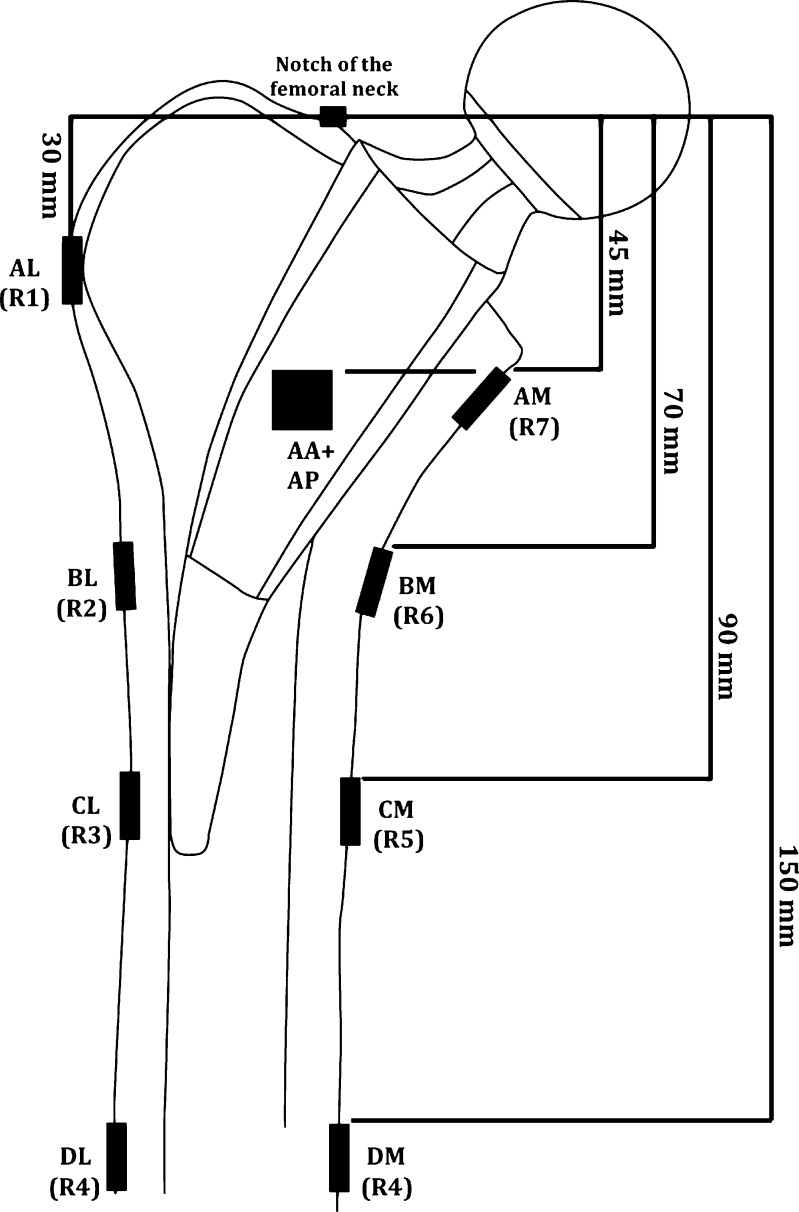
For the strain measurement ten prewired strain gauges [3/350 RY91, Hottinger Baldwin Messtechnik GmbH (HBM), Darmstadt, Germany] were bonded to four levels of each of the three femora (A–D) 45, 70, 90 and 150 mm distally to the notch of the femoral neck. The gauges were placed in specific locations to enable a comparison of the strain patterns corresponding to the Gruen zones from typical DXA scans [11]. One strain gauge was placed medially and laterally at each of the four levels. In addition at level A two gauges were placed in the anterior and posterior regions at the most proximal level A. At level A, the lateral strain gauge was located 15 mm more proximal compared to the level of the medial, anterior and posterior strain gauges to the region of the greater trochanter (Fig. 3). The positions of level A were chosen to represent the regions of the greater trochanter and the calcar, respectively. Level C was chosen to be around the distal tip of the Metha stem, while level B was directly in between levels A and C. The strain gauges at level D had a considerable distance from the distal tip of the implant so that they would not be affected by it. Thus, the read-outs of these gauges showed whether identical loading conditions were applied to intact and implanted femur [5].
Fig. 3.
Vertical levels of the strain gauges on the proximal femur with an implanted Metha short stem. The corresponding Gruen zones are in parentheses
Before mounting the strain gauges the bone surfaces were smoothed with fine sandpaper (#280), carefully cleaned and degreased with ethanol followed by a cleanser (RMS1, HBM, Darmstadt, Germany). An optical tracking system based on infrared marker tracking (Polaris P4, Northern Digital Inc., Waterloo, ON, Canada) was used to ensure perpendicular alignment to the longitudinal axis of the femur as well as precise positioning of strain gauges on each femur. The strain gauges were bonded with a two-component polymethylmethacrylate adhesive (X60, HBM) and covered with a protective polyurethane coating (PU 120, HBM). A quarter Wheatstone bridge was used per gauge. Strain gauge data were obtained using an amplifier module (CA1030, HBM) connected to a CANHEAD base module (CB1014, HBM) and recorded using catman®EASY software (Version 3.1, HBM). To avoid excessive heating of the gauges, a bridge excitation voltage of 0.5 V was selected. Data were obtained at a frequency of 100 Hz, with a low-pass filter cut-off frequency of 10 Hz.
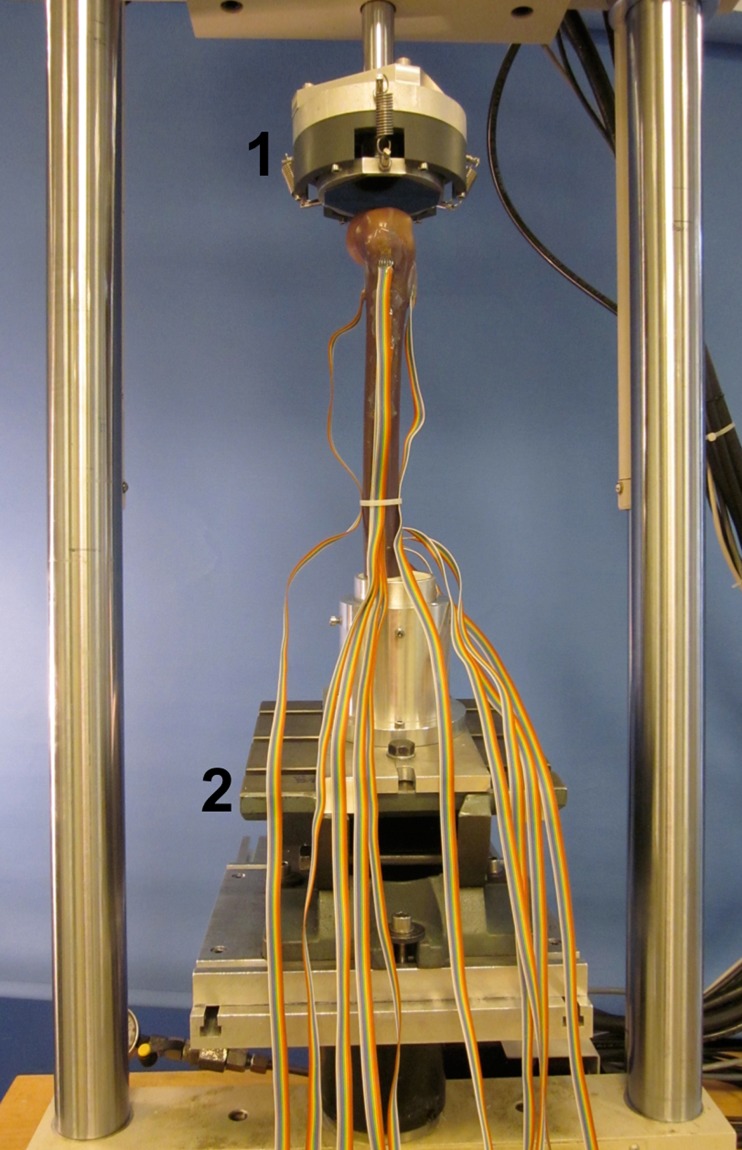
Load application and measurement protocol
The femur was placed on a 15 kN load cell on a materials testing system (MTS Mini Bionix 858, MTS Systems Corporation, Eden Prairie, MN, USA) using a custom-made jig. A floating bearing was attached to the MTS to avoid undesireable horizontal force components and moments at the point of load application (Fig. 4). Using a platform that allowed rotation of the femora at different angles, a loading configuration was chosen that simulated the single-leg stance (8° adduction, 0° flexion). After zeroing the load cell and strain gauges the femur was loaded in a ramp profile up to an axial force of 800 N at a rate of 10 N/s. Using load control during the axial force of 800 N was kept constant for 90 seconds to reduce the influence of a creep effect. After 30 seconds, an interval during which creep was observed in preliminary experiment, strains were recorded for a following 60 seconds. The measurement procedure was repeated five times, and the synthetic femur was allowed to elastically recover for eight minutes between repetitions. In order to verify material and geometric linearity, a further measurement was performed where strains were recorded at 100 N loading increments to a maximum load of 800 N. At each level the load was held for ten seconds to avoid creep effects and the strains were then measured for 30 seconds.
Fig. 4.
Experimental set-up within the MTS including the floating bearing to eliminate horizontal forces (1) and the platform that allowed rotation of the femora at an angle of 8° adduction (2)
Statistical analysis
The mean value of the principal strains and the angles of the principal strains over the five test repetitions were determined for the intact as well as for the implanted models [14], and the coefficient of variance (CoV) was computed for the major principal strains. In order to illustrate the changes in strain patterns for the Metha stem with different resection heights compared to the non-implanted intact femora, the strains for the implanted femur were expressed as a percentage of the strains in the identical, intact femur. Due to the fact that only one synthetic femur per resection height was used, no statistical testing regarding resection height was possible.
Strain read-outs from the load application, where strains were recorded in 100-N increments, were assessed in terms of linearity between force and strain by linear regression. The correlation was expressed by the coefficient of linear regression R2.
Results
Quality of strain measurement
The CoV of the principal strains within the five repetitions, under the same loading configuration, was always less than 1 % (average 0.33 %). Thus, measurement repeatability was excellent. The relationship between applied load and experimental strain was highly linear, with R2 greater than 0.995 for all strain gauges on the three femora in the non-implanted and implanted condition. This additionally proved that the strain gauges were bonded with a high quality.
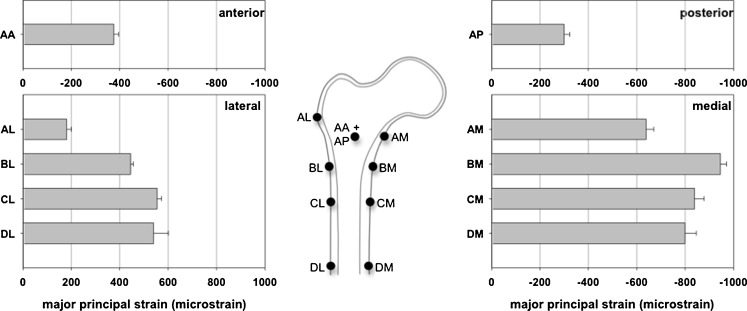
Strain patterns in the intact femora
The strain values varied between the locations in the non-implanted femora (Fig. 5). The highest compressive strain values were observed on the medial aspect of level B (946, SD 20 microstrains), while the highest tensile strains were on the lateral aspect of level C (554, SD 14 microstrains). The lowest compressive strains on the medial aspect and the lowest tensile strains on the lateral aspect were both observed at level A (653, SD 53 microstrains for strain gauge position AM and 181, SD 15 microstrains for strain gauge position AL, respectively). The compressive strains on the anterior and posterior aspects at level A were even lower (375, SD 16 microstrains and 300, SD 20 microstrains, respectively).
Fig. 5.
Major principal strains at ten different locations on the non-implated femora—tensile for the lateral and compressive for the medial, anterior and posterior aspects. Averages and standard deviations between the three femora are reported
As expected, the orientations of the major principal strains were within a few degrees from the axis of the femora on the lateral aspect and nearly perpendicular to this axis on the medial aspect.
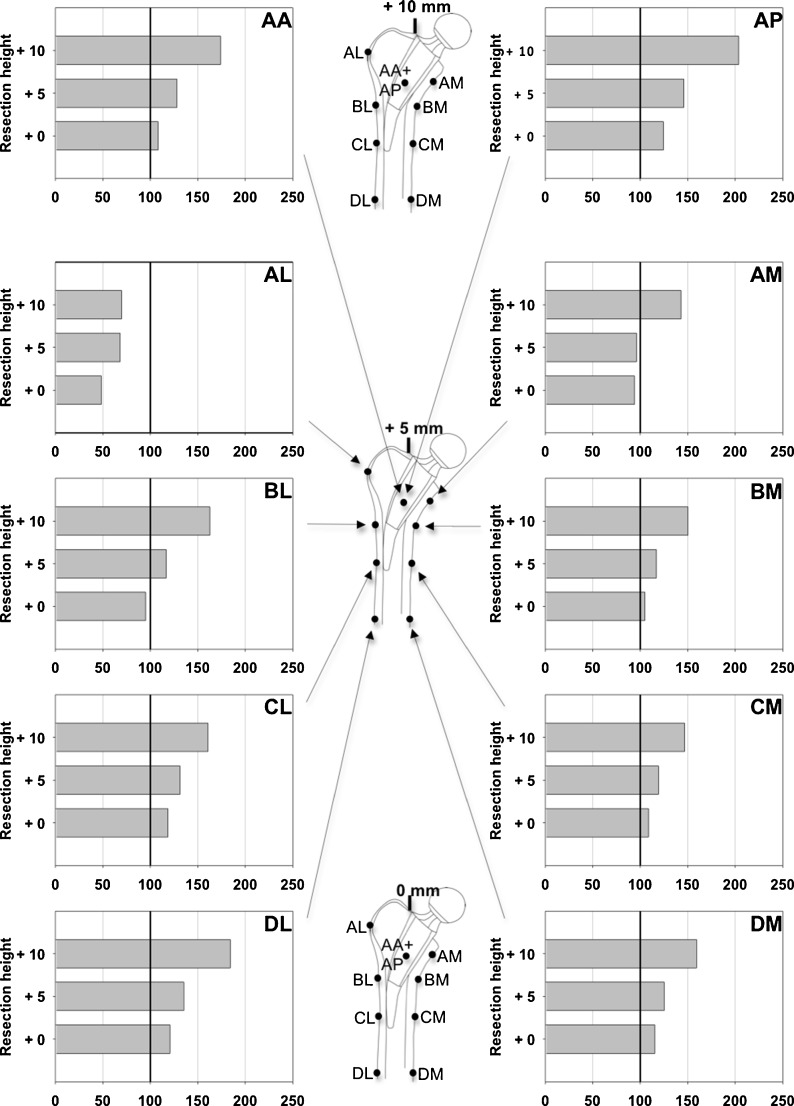
Strain patterns after insertion of stems
Implantation of the Metha stem led to only small changes in the largest principal strains for the two lower resection heights when compared with the non-implanted femora, with the exception of strains recorded at strain gauge AL (Fig. 6). At all other strain gauge locations, the strain in the implanted femur only differed from the physiological condition by between −6 and +24 % for the lowest, most distal resection (0 mm) and between −10 and +46 % for the medium resection (+5 mm). Results from the highest, most proximal resection height revealed only increased strains compared to the physiological condition, by between +43 and +104 %.
Fig. 6.
Major principal strain values at ten different locations after implantation of the Metha short stem with three different resection heights (+10, + 5 and 0 mm) expressed as a percentage of the strains in the corresponding intact femur—tensile for the lateral and compressive for the medial, anterior and posterior aspects
In the region of the greater trochanter, represented by strain gauge AL, there were decreases in strain by 30, 32 and 52 % for the high, medium and low resection height, respectively.
The low, most distal resection height displayed strain levels that were the most consistent with the condition of the non-implanted femora, at all measurement locations along the proximal femur except measurement location AL. Strains at measurement location AM (medial Gruen zone 7) were only decreased by 4 % and 6 % for the low and medium resection heights, respectively. At this location, there was a strain increase of 43 % for the high resection height. For the strain gauges at levels B, C and D, similar patterns with small differences between the three levels could be observed. More precisely, the averages of the medial strain gauges from levels B, C and D were 152 % (SD 5) for the high, 120 % (SD 3) for the medium and 111 % (SD 4) for the low resection height. For the lateral strain gauges the corresponding averages were 169 % (SD 10), 128 % (SD 8) and 112 % (SD 12).
Discussion
The aim of this biomechanical testing was to illustrate whether a divergence of the recommended resection height induces any deviation in the strain patterns after implantation of the Metha short stem. The biomechanical data revealed for a lower resection more similar strain patterns to that of a non-implanted, model. A lower, more distal resection reduces the offset and varus position of the stem. Thus, less load is transferred to the region of the calcar and the region around the distal tip of the stem. However, the simulation of the advised resection height with preservation of a 5-mm cortical ring of the femoral neck showed only small differences. Compared to the lower resection situation, the Metha stem is positioned in a slightly more varus position. For the highest resection simulation the varus position of the Metha stem is even greater. This change in stem positioning results in a greater offset in turn leading to increased strain in the medial part of the proximal femur and the region around the distal tip of the stem. For all simulated situations, there was only an obvious strain decrease in the region of the greater trochanter. Because the strain patterns matched well to that of the non-implanted model, the problem of stress shielding seems to be negligible for the different settings. Thus, as long as a cortical ring is preserved, the strain patterns after implantation of the Metha short stem remain similar to that of non-implanted pattern. Clinically, it can be inferred that, depending on the anatomy and possible deformity of the proximal femur, a lower osteotomy seems to be possible in order to reconstruct the offset and the limb length without major changes in strain patterns. As long as a cortical ring of the femoral neck is preserved and the size of the stem is chosen correctly with the proximal rim of the stem exceeding the osteotomy, implantation of the Metha stem seems suitable even in secondary osteoarthritis.
To date only one imaging study exists analysing the influence of the resection height for the Metha stem on the offset and CCD angle [18]. These data agree with the findings of our study; the final position of the Metha stem and the CCD angle were reported to be significantly higher with the lowest neck resection and the offset was lower in this position compared to more proximal resections (20). However, this study did not provide any information about strain patterns. Only Fottner et al. have reported biomechanical data regarding the Metha stem; they compared the in vitro primary stability of the thrust plate prosthesis with the Mayo short stem and the modular Metha short stem using cone adapters with 130 and 140° neck shaft angles [10]. For all tested prostheses, the micromotions did not exceed the critical value for osseointegration of 150 μm.
There are several published studies that involve biomechanical testings of different THA stems. Unfortunately, conclusive comparisons between these studies are difficult due to differing testing set-ups. Different studies on biomechanical testings determined changes in strain patterns for individual customised stems and traditional stems in cadaveric femora [1, 15, 20]. They revealed more physiological patterns of strain in the proximal femur after implantation of a customised stem compared to a standard stem. The measurements of strain revealed that both types of stems induced a reduction in axial strain in the bone adjacent to the proximal half of the stem, but the changes in cortical strain were significantly less pronounced for the customised implants. Decking et al. compared the strain patterns after implantation for the stemless ESKA CUT prosthesis and two full stem THA prostheses (Zweymüller and OPTAN stems) in a biomechanical set-up of cadaveric femora [6]. Both conventional long stem THAs led to decreases in longitudinal strain in the proximal femur, while the femoral neck-preserving CUT prosthesis mainly induced a strain increase on the lateral side of the greater trochanter. Medial strains were closer to the physiological values in the “stemless” CUT prosthesis when compared to the full stem prostheses.
The main limitation of this study was that strain gauges reflect deformation of the external bone surface only at the selected strain gauge positions. Using different femora a repeatable positioning is therefore highly relevant. This was ensured by applying a well-defined reference system including an optical tracking system. Thus, this device accounts for very little variability between the femora.
Prior to this study we were aware that synthetic femora cannot perfectly replicate in vivo conditions. However, cadaveric bone suffers from wide interspecimen variability regarding bone geometry and mechanical properties, which directly affects the results of strain measurement. Therefore, using synthetic bones, whose strong resemblance in mechanical properties to native bone with interspecimen variability of only between 2.6 and 3.1 % for the axial and bending load was proved in previous studies [13], was a good alternative because femora with identical geometry and material properties could be used.
Muscles and forces provided by other soft tissue were not simulated during biomechanical testing. However, it has been reported [4] that studies, in which the testing set-up did not feature muscles [4, 5], can reliably analyse the strain patterns of the proximal femur.
In conclusion, this study revealed similar strain patterns for the cementless Metha short stem arthroplasty with three different resection heights. Strain patterns depend on the varus/valgus position of the stem. An obvious decrease in strain occurred only around the greater trochanter, for all tested simulations. The clinical relevance of this work becomes apparent in the insight that a lower resection is possible as long as a cortical ring is preserved, the Metha stem exceeds the cortical ring and the stem is large enough. The results indicate a small influence of different resection heights on stress shielding. Thus, the Metha short stem may also be used for treatment of secondary osteoarthritis, where only a deep resection is necessary to restore physiological biomechanics. In order to overcome the limitations of strain studies relating to clinical relevance, remodelling around the THA should be more closely observed by DXA measurements and/or investigated in a long-term clinical follow-up study.
Acknowledgments
The study was kindly supported by the “Hochschulinterne Leistungsförderung (HiLF)” of the MHH and by Aesculap who provided the implants for the biomechanical testing.
Conflict of interest
Three of the authors (T. Floerkemeier, H. Windhagen and G. von Lewinski) are paid instructors for the company B. Braun Aesculap, Tuttlingen, Germany.
References
- 1.Aamodt A, Lund-Larsen J, Eine J, Andersen E, Benum P, Husby OS. Changes in proximal femoral strain after insertion of uncemented standard and customised femoral stems. An experimental study in human femora. J Bone Joint Surg Br. 2001;83(6):921–929. doi: 10.1302/0301-620X.83B6.9726. [DOI] [PubMed] [Google Scholar]
- 2.Albanese CV, Santori FS, Pavan L, Learmonth ID, Passariello R. Periprosthetic DXA after total hip arthroplasty with short vs. ultra-short custom-made femoral stems: 37 patients followed for 3 years. Acta Orthop. 2009;80(3):291–297. doi: 10.3109/17453670903074467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Braun A, Lazovic D, Zigan R. Modular short-stem prosthesis in total hip arthroplasty: implant positioning and the influence of navigation. Orthopedics. 2007;30(10 Suppl):S148–S152. [PubMed] [Google Scholar]
- 4.Cristofolini L, Juszczyk M, Taddei F, Field RE, Rushton N, Viceconti M. Stress shielding and stress concentration of contemporary epiphyseal hip prostheses. Proc Inst Mech Eng H. 2009;223(1):27–44. doi: 10.1243/09544119JEIM470. [DOI] [PubMed] [Google Scholar]
- 5.Cristofolini L, Juszczyk M, Taddei F, Viceconti M. Strain distribution in the proximal human femoral metaphysis. Proc Inst Mech Eng H. 2009;223(3):273–288. doi: 10.1243/09544119JEIM497. [DOI] [PubMed] [Google Scholar]
- 6.Decking R, Puhl W, Simon U, Claes LE. Changes in strain distribution of loaded proximal femora caused by different types of cementless femoral stems. Clin Biomech (Bristol, Avon) 2006;21(5):495–501. doi: 10.1016/j.clinbiomech.2005.12.011. [DOI] [PubMed] [Google Scholar]
- 7.Ettinger M, Ettinger P, Lerch M, Radtke K, Budde S, Ezechieli M, Becher C, Thorey F. The NANOS short stem in total hip arthroplasty: a mid term follow-up. Hip Int. 2011;21(5):583–586. doi: 10.5301/HIP.2011.8658. [DOI] [PubMed] [Google Scholar]
- 8.Fink B, Wessel S, Deuretzbacher G, Protzen M, Ruther W. Midterm results of “thrust plate” prosthesis. J Arthroplasty. 2007;22(5):703–710. doi: 10.1016/j.arth.2006.12.041. [DOI] [PubMed] [Google Scholar]
- 9.Floerkemeier T, Tscheuschner N, Calliess T, Ezechieli M, Floerkemeier S, Budde S, Windhagen H, von Lewinski G. Cementless short stem hip arthroplasty METHA® as an encouraging option in adults with osteonecrosis of the femoral head. Arch Orthop Trauma Surg. 2012;132(8):1125–1131. doi: 10.1007/s00402-012-1524-5. [DOI] [PubMed] [Google Scholar]
- 10.Fottner A, Schmid M, Birkenmaier C, Mazoochian F, Plitz W, Volkmar J. Biomechanical evaluation of two types of short-stemmed hip prostheses compared to the trust plate prosthesis by three-dimensional measurement of micromotions. Clin Biomech (Bristol, Avon) 2009;24(5):429–434. doi: 10.1016/j.clinbiomech.2009.02.007. [DOI] [PubMed] [Google Scholar]
- 11.Gruen TA, McNeice GM, Amstutz HC (1979) “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res 141:17–27 [PubMed]
- 12.Gulow J, Scholz R, Freiherr von Salis-Soglio G. Short-stemmed endoprostheses in total hip arthroplasty. Orthopade. 2007;36(4):353–359. doi: 10.1007/s00132-007-1071-x. [DOI] [PubMed] [Google Scholar]
- 13.Heiner AD, Brown TD. Structural properties of a new design of composite replicate femurs and tibias. J Biomech. 2001;34(6):773–781. doi: 10.1016/S0021-9290(01)00015-X. [DOI] [PubMed] [Google Scholar]
- 14.Hoffmann K. An introduction of measurements using strain gauges. Darmstadt: Hottinger Baldwin Messtechnik; 1989. [Google Scholar]
- 15.Kim YH, Kim JS, Cho SH. Strain distribution in the proximal human femur. An in vitro comparison in the intact femur and after insertion of reference and experimental femoral stems. J Bone Joint Surg Br. 2001;83(2):295–301. doi: 10.1302/0301-620X.83B2.10108. [DOI] [PubMed] [Google Scholar]
- 16.Lerch M, von der Haar-Tran A, Windhagen H, Behrens BA, Wefstaedt P, Stukenborg-Colsman CM. Bone remodelling around the Metha short stem in total hip arthroplasty: a prospective dual-energy X-ray absorptiometry study. Int Orthop. 2011;36(3):533–538. doi: 10.1007/s00264-011-1361-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Logroscino G, Ciriello V, D’Antonio E, De Tullio V, Piciocco P, Magliocchetti LG, Santori FS, Albanese CV. Bone integration of new stemless hip implants (proxima vs. nanos). A DXA study: preliminary results. Int J Immunopathol Pharmacol. 2011;24(1 Suppl 2):113–116. doi: 10.1177/03946320110241S221. [DOI] [PubMed] [Google Scholar]
- 18.Mihalko WM, Saleh KJ, Heller MO, Mollard B, König C, Kammerzell S. Femoral neck cut level affects positioning of modular short-stem implant. Orthopedics. 2009;32(10 Suppl):18–21. doi: 10.3928/01477447-20090915-53. [DOI] [PubMed] [Google Scholar]
- 19.Morrey BF, Adams RA, Kessler M. A conservative femoral replacement for total hip arthroplasty. A prospective study. J Bone Joint Surg Br. 2000;82(7):952–958. doi: 10.1302/0301-620X.82B7.10420. [DOI] [PubMed] [Google Scholar]
- 20.Østbyhaug PO, Klaksvik J, Romundstad P, Aamodt A. An in vitro study of the strain distribution in human femora with anatomical and customised femoral stems. J Bone Joint Surg Br. 2009;91(5):676–682. doi: 10.1302/0301-620X.91B5.21749. [DOI] [PubMed] [Google Scholar]
- 21.Rometsch E, Bos PK, Koes BW (2012) Survival of short hip stems with a “modern”, trochanter-sparing design—a systematic literature review. Hip Int 22:344–354. doi:10.5301/HIP.2012.9472 [DOI] [PubMed]
- 22.Schmidutz F, Grote S, Pietschmann M, Weber P, Mazoochian F, Fottner A, Jansson V. Sports activity after short-stem hip arthroplasty. Am J Sports Med. 2012;40(2):425–432. doi: 10.1177/0363546511424386. [DOI] [PubMed] [Google Scholar]
- 23.Steinhauser E, Ellenrieder M, Gruber G, Busch R, Gradinger R, Mittelmeier W. Influence on load transfer of different femoral neck endoprostheses. Z Orthop Ihre Grenzgeb. 2006;144(4):386–393. doi: 10.1055/s-2006-942127. [DOI] [PubMed] [Google Scholar]
- 24.Westphal FM, Bishop N, Honl M, Hille E, Püschel K, Morlock MM. Migration and cyclic motion of a new short-stemmed hip prosthesis–a biomechanical in vitro study. Clin Biomech (Bristol, Avon) 2006;21(8):834–840. doi: 10.1016/j.clinbiomech.2006.04.004. [DOI] [PubMed] [Google Scholar]