Abstract
Background
Although the DSM-IV provides explicit criteria for the diagnosis of BP-I disorder, this is a complex diagnosis that requires high levels of clinical expertise. Previous work shows children with a unique profile of the CBCL of high scores (2SD) on the Attention Problems (AP), Aggressive Behavior (AGG), and Anxious-Depressed (AD) (A-A-A) subscales are more likely than other children to meet criteria for BP-I disorder in both epidemiological and clinical samples. However, since not all BP-I disorder children have a positive profile questions remain as to its informativeness, particularly in the absence of an expert diagnostician.
Methods
Analyses were conducted comparing personal and familial correlates of BP-I disorder in 140 youth with a structured interview and an expert clinician based DSM-IV diagnosis of BP-I disorder with (N=80) and without (N=60) a positive CBCL- Severe Dysregulation profile, and 129 controls of similar age and sex without ADHD or a mood disorder. Subjects were comprehensively assessed with structured diagnostic interviews and wide range of functional measures. We defined the CBCL-Severe Dysregulation profile as an aggregate cut-off score of ≥210 on the A-A-A scales.
Results
BP-I probands with and without a positive CBCL-Severe Dysregulation profile significantly differed from Controls in patterns of psychiatric comorbidity, psychosocial and psychoeducational dysfunction, and cognitive deficits, as well as in their risk for BP-I disorder in first degree relatives.
Limitations
Because the sample was referred and largely Caucasian, findings may not generalize to community samples and other ethnic groups.
Conclusion
A positive CBCL-Severe Dysregulation profile identifies a severe subgroup of BP-I disorder youth.
Keywords: Mood disorders, Severity of illness index, screening instrument
INTRODUCTION
An emerging pediatric literature documents that pediatric bipolar disorder (BP) is a prevalent and highly morbid disorder worldwide. Merikangas et al. (2010) reported a 2.9% prevalence of bipolar disorder in a large epidemiological sample of over 10,000 adolescents in the US. A meta-analysis of international epidemiological studies estimated the prevalence of pediatric BP and bipolar spectrum disorder to be 1.8% and found no significant difference in prevalence between the United States and other countries (Van Meter et al., 2011).
Although the DSM-IV provides explicit criteria for the diagnosis of BP-I disorder, this is a complex diagnosis that requires high levels of clinical expertise not readily available in clinical practice. This state of affairs calls for easy to use, cost-effective methods to aid in the identification of such children in clinical practice, and particularly in the primary care setting.
Because of its empirical nature, its excellent psychometric properties and its ease of use as a paper and pencil instrument, the Child Behavior Checklist (CBCL) (Achenbach, 1991) has been examined as a potential tool to aid in the identification of children at high risk for BP-I disorder (Althoff et al., 2006; Faraone et al., 2005; Hudziak et al., 2005; Mick et al., 2003). Several groups have shown that children with a unique profile of the CBCL of high scores (2SD) on the Attention Problems (AP), Aggressive Behavior (AGG), and Anxious-Depressed (AD) (A-A-A) subscales are more likely than other children to meet DSM-based diagnosis of BP-I disorder in both epidemiological and clinical samples (Achenbach, 1991; Carlson and Kelly, 1998; Geller et al., 1998; Hazell et al., 1999; Mick et al., 2003; Wals et al., 2001). This profile has been variedly referred to as the CBCL-pediatric bipolar disorder profile or CBCL-Severe Dysregulation profile (Mick et al., 2003) (henceforth referred to as CBCL-Severe Dysregulation profile).
Using conditional probability analysis, we recently documented that children with as clinical and structured interview diagnosis of BP-I disorder were significantly more likely than both control (Odds Ratio (OR): 173.2; 95% Confidence Interval (CI): 21.2, 1413.8; p<0.001) and ADHD children (OR:14.6; 95% CI: 6.2, 34.3; p<0.001) to have a positive CBCL-Severe Dysregulation profile (A-A-A scores of ≥210) (Positive Predictive Power: 99%; false positive rate:< 0.2%) (Biederman et al., submitted). However, this study also showed that a sizeable number of children with a documented diagnosis of BP-I disorder did not have a positive profile thereby raising questions as to the general informativeness of this profile.
One approach to shed light on this important issue would be to examine whether the subgroup of BP-I disorder children with a positive CBCL-Severe Dysregulation profile would have external correlates of BP-I disorder such as patterns of psychiatric comorbidity and dysfunction and familial rates of BP-I disorder in first degree relatives. We reasoned that for a positive CBCL profile to be informative in clinical practice it should be associated with meaningful correlates of BP-I disorder.
The main aim of the present work was to further investigate the informativeness of the CBCL-Severe Dysregulation profile to aid in the identification of children with a suspected diagnosis of BP-I disorder. To this end, we compared personal (symptom profile, psychiatric comorbidity and psychosocial dysfunction) and familial correlates (rates of familiality of BP-I disorder), in BP-I disorder children with and without a positive CBCL-Severe Dysregulation profile and Controls. We hypothesized the positive profile will be associated with a picture compatible with a diagnosis of BP-I disorder.
METHODS
Subjects
Detailed study methods have been previously described (Wozniak et al. 2012 submitted). Briefly, children with BP-I disorder 6–17 years of age of both sexes were recruited and assessed at the Clinical and Research Program in Pediatric Psychopharmacology at the Massachusetts General Hospital based on the presence of a diagnosis of bipolar-I disorder in the proband youth by structured diagnostic interview and clinical assessment (Wozniak et al., 2005; Wozniak et al., 2010). Comparators were youth with and without ADHD without BP-I disorder of similar age and sex (Biederman et al., 1992; Biederman et al., 1999; Biederman et al., 2006a; Biederman et al., 2006b). We recruited 239 BP-I probands. From families participating in our case-control ADHD studies we randomly selected 136 non-ADHD control probands without mood disorders (BP-I or MDD full or subthreshold) so that the age and gender distribution was similar to that of the BP-I probands. All studies used the same assessment methodology regardless of the disorder used to classify probands as cases with the exception that children with structured interview diagnosis of BP-I disorder were also assessed buy an expert clinician to confirm the diagnosis (Wozniak et al., 2003). All study procedures were reviewed and approved by the subcommittee for human subjects of our institution. All subjects’ parents or guardians signed written informed consent forms and children older than 7 years of age signed age appropriate written assent forms.
Ascertainment Method
Potential BP-I probands were ascertained from our clinical service, referrals from local clinicians or self-referral in response to advertisements. Subjects were administered a phone screen reviewing symptoms of DSM-IV BP-I disorder and, if criteria were met, were scheduled for a face-to-face structured diagnostic interview. In addition to the structured diagnostic interview, an expert clinician (J.W.) met with each BP-I proband and his or her parents for a clinical interview in order to confirm the diagnosis of BP-I disorder using the Schedule for Affective Disorders and Schizophrenia for School-Age Children-Epidemiological version (KSADS-E) mania module. We have published data on the convergence of these clinical interviews with our structured interview diagnosis on the first 69 cases. We reported 97% agreement between the structured interview and clinical diagnosis in this analysis of 69 children (Wozniak et al., 2003). As previously reported (Biederman et al., 1992; Biederman et al., 1999; Wozniak et al., 2010), controls were ascertained from out-patients referred for routine physical examinations to pediatric medical clinics and from computerized records as not having ADHD and screening for not having ADHD.
Diagnostic Procedures
Psychiatric assessments of subjects < 18 years of age relied on the KSADS-E (epidemiologic version) (Orvaschel, 1994) and for subjects ≥18 years on the SCID supplemented with modules from the K-SADS-E to capture childhood disorders. Diagnoses of youth were based on independent interviews with mothers and direct interviews with children older than 12 years of age. Data were combined such that endorsement of a diagnosis by either report resulted in a positive diagnosis.
All interviews were conducted by extensively trained and supervised psychometricians with undergraduate degrees in psychology. This training involved several weeks of classroom instruction of interview mechanics, diagnostic criteria and coding algorithms. They also observed interviews by experienced raters and clinicians and were observed while conducting interviews during the final training period. In addition, all diagnoses were reviewed by a sign-off committee of experienced board-certified child and adolescent psychiatrists or clinical psychologists. The committee members were blind to the subjects’ ascertainment status, ascertainment site, and data collected from other family members. We computed kappa coefficients of agreement by having experienced clinicians diagnose subjects from audio-taped interviews made by the assessment staff. Based on 500 interviews, the median kappa coefficient between raters and clinicians was 0.99. For individual diagnoses the kappas were ADHD (0.88), conduct disorder (1.0), major depression (1.0), mania (0.95), separation anxiety (1.0), agoraphobia (1.0), panic (0.95), substance use disorder (1.0), and tics/Tourette’s (0.89). The median agreement between individual clinicians and the clinical review committee was 0.87 and for individual diagnoses was ADHD (1.0), CD (1.0), major depression (1.0), bipolar (0.78), separation anxiety (0.89), agoraphobia (0.80), panic (0.77), substance use disorder (1.0), and tics/Tourette’s (0.68).
Children and adolescents were diagnosed with BP-I disorder according to DSM-IV criteria. The DSM-IV requires subjects to meet criterion A for a distinct period of extreme and persistently elevated, expansive or irritable mood lasting at least 1 week, plus criterion B, manifested by three (four if the mood is irritable only) of seven symptoms during the period of mood disturbance. To ensure that the B criterion symptoms were concurrent with A criterion mood disturbance, subjects were directed to focus on the worst or most impairing episode of mood disturbance while being assessed for the presence of the confirmatory B criterion symptoms. That is, the subject was asked to consider the time during which the screen was at its worst for the purpose of determining whether the remaining symptoms were also evident at the same as the screening item. Also recorded was the onset of first episode, the number of episodes, offset of last episode, and total duration of illness. Any subject meeting criteria for BP-II or BP-NOS was not included in this study. To gauge a distinct episode, our interviewers asked for ‘a distinct period (of at least 1 week) of extreme and persistently elevated, expansive or irritable mood’ and further required that the irritability endorsed in this module is ‘super’ and ‘extreme.’
Child Behavior Checklist
The parent (usually the mother) of each participant completed the 1991 version of the Child Behavior Checklist for ages 4 to 18 years (CBCL/4-18). The CBCL is an affordable pencil and paper test completed by the child’s caregiver, requiring no administration by a physician or rater. The CBCL queries the parent about the child’s behavior in the past six months and aggregates this data into behavioral problem T-scores (Achenbach, 1991). A computer program calculates the T-scores for each scale. Raw scores are converted to gender and age standardized scores (T-scores having a mean = 50 and SD = 10). A minimum T-score of 50 is assigned to scores that fall at midpoint percentiles of ≤50 on the syndrome scales to permit comparison of standardized scores across scales. As described previously, the CBCL-Severe Dysregulation profile (Biederman et al., 2009) was defined as positive by a score of ≥210 (2SDs) on the sum of the Attention, Aggression, and Anxious/Depressed CBCL scales (AAA profile). An intermediate or subsyndromal emotional dysregulation profile was defined as positive by a score of ≥180 (≥ 60 on average on each scale) but <210 (average T-score of ≥60 and <70 on AAA scales). This intermediate profile has been previously termed the CBCL-deficient emotional self regulation or DESR profile (Spencer et al., 2011).
Statistical analysis
Differences in demographics and clinical characteristics were assessed using ANOVA for continuous outcomes, Pearson’s χ2 for binary outcomes, and Kruskal Wallis for SES. Pairwise comparisons were made between the three groups using logistic regression for binary outcomes and linear regression for continuous outcomes. Data are expressed as mean ± standard deviation (SD) unless otherwise specified. All tests were two-tailed, and our alpha level was set at 0.05 for all analyses. We calculated all statistics using STATA, version 12.0.
RESULTS
Our analyses compared BP-I probands with and without a positive CBCL-Severe Dysregulation profile with Control probands without ADHD or a mood disorder. As shown in Table 1, there were no meaningful differences between the groups in the age and sex distributions. However, there were small, but statistically significant differences in the socioeconomic backgrounds of the families. Probands with a positive CBCL profile had a lower SES. Accordingly, all subsequent tests were adjusted for SES.
Table 1.
Descriptive Statistics (N=269)
| Demographics | Control | BP-I without Profile | BP-I with Profile | Statistical Analysis | |
|---|---|---|---|---|---|
|
| |||||
| N=129 | N=60 | N=80 | Test statistic | p-value | |
|
| |||||
| Baseline age | 10.8 ± 3.1 | 10.7 ± 3.3 | 9.8 ± 2.8 | F(2, 266)=2.55 | 0.08 |
|
| |||||
| Sex (% male) | 97 (75) | 47 (78) | 57 (71) | χ2(2)=0.94 | 0.63 |
|
| |||||
| Race | |||||
|
| |||||
| Caucasian | 125 (96) | 56 (93) | 74 (92) | χ2(6)=11.4 | 0.07 |
|
| |||||
| African American | 2 (2) | 0 (0) | 2 (3) | ||
|
| |||||
| More than 1 | 0 (0) | 4 (7) | 4 (5) | ||
|
| |||||
| Unknown | 2 (2) | 0 (0) | 0 (0) | ||
|
| |||||
| Socioeconomic status (SES) | 1.5 ± 0.7 | 1.8 ± 0.9 | 1.9 ± 0.9 | χ2(2) =7.6 | 0.02 |
|
| |||||
| Clinical Characteristics | Control | BP-I without profile | BP-I with profile | Statistical Analysis | |
|
| |||||
| N=129 | N=60 | N=80 | Test statistic | p-value | |
|
| |||||
| BP-I Onset | n/a | 7.0 ± 3.7 | 5.5 ± 3.2 | t=−2.6 | 0.01 |
|
| |||||
| BP-I Total Symptom Count | n/a | 5.5 ± 1.0 | 5.9 ± 1.3 | t=1.9 | 0.6 |
|
| |||||
| BP-I Total Number of Episodes | n/a | 15.5 ± 41.0 | 16.6 ± 39.6 | t=0.1 | 0.9 |
|
| |||||
| BP-I Impairment | |||||
| Minimum | n/a | 0 (0) | 0 (0) | z=1.0 | 0.3 |
| Moderate | 25 (42) | 27 (34) | |||
| Severe | 35 (58) | 53 (66) | |||
|
| |||||
| Mania Onset Before Depression* | n/a | 14 (61) N=41 | 24 (51) N=71 | z=−0.6 | 0.5 |
|
| |||||
| Mixed State* | n/a | 36 (88) N=41 | 67 (94) N=71 | z=1.2 | 0.2 |
|
| |||||
| Treatment | |||||
| None | 39 (30) | 2 (3)a | 0 (0)a | exact: 43.3 | <0.001 |
| Any Counseling | 13 (10) | 4 (7) | 3 (4) | exact: 2.9 | 0.24 |
| Medication | 0 (0) | 6 (10)a | 2 (3) | exact: 14.2 | <0.001 |
| Both Counseling and Medication | 0 (0) | 33 (57)a | 42 (54)a | exact: 95.6 | <0.001 |
| Hospitalization | 0 (0) | 13 (23)a | 30 (39)a | exact: 52.4 | <0.001 |
15 BP-I probands without the profile and 7 BP-I probands with the profile did not have a diagnosis of Depression. Among all BP-I probands with both Mania and Depression (N=118), 4 BP-I probands without the profile and 2 BP-I probands with the profile reported the same onset for both mania and depression.
p<0.05 vs. control
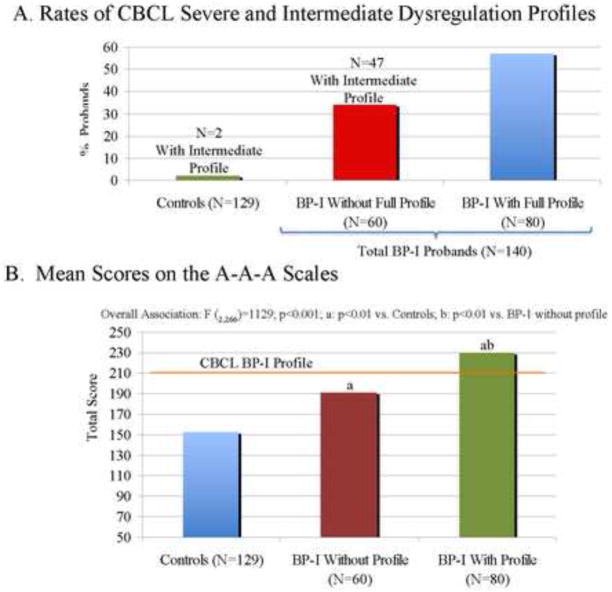
As shown in Figure 1, although only 62% of BP-Probands had a positive CBCL-Severe Dysregulation profile, 80% of profile negative BP-I probands profile had the intermediate (≥180<210) A-A-A compared to only 2% of Controls (Fig 1A). This issue of profile negative subjects being subsyndromal in this profile is further illustrated in Figure 1B showing that while BP-I probands with a positive CBCL profile had the highest mean scores on the A-A-A scales, both profile positive and negative BP-I proband differed significantly from controls on the severity of these scales (both p-values <0.01) (Fig 1A).
Figure 1.
CBCL Severe Dysregulation Profile
Clinical Characteristics
BP-I probands with a positive CBCL profile were more likely to have an earlier onset of BP-I disorder compared to negative BP-I probands. Although the rate of psychiatric hospitalization was almost twice as large in the profile positive BP-I proband group than in the profile negative one, the difference failed to reach our a priori threshold for statistical significance (p=0.066). We found no significant differences between the groups for total BP symptoms count, number of episodes, associated impairment, having mania before depression, and having a mixed state (Table 1).
With two exceptions, there were no differences in the symptoms of mania between profile positive and profile negative BP-I probands; the exceptions were that profile positive BP-I probands were more likely to have irritability and less likely to have increased social activity compared to those with a negative profile.
Patterns of Psychiatric Comorbidity and Dysfunction
As shown in Table 2, CBCL positive BP-I probands had higher rates of most psychiatric comorbidities assessed compared with CBCL negative profile BP-I probands, particularly major depression, ODD, social phobia, panic disorder and GAD.
Table 2.
Comorbid Disorders (Lifetime)
| Control | BP-I without profile | BP-I with profile | |||
|---|---|---|---|---|---|
| N=129 | N=60 | N=80 | Test statistic | p-value | |
| Major Depression | 9 (7) | 41 (68)a | 71 (89)ab | χ2(3)=174.4 | <0.001 |
| Psychosis | 2 (2) | 12 (20)a | 28 (35)a | χ2(3)=49.2 | <0.001 |
| Disruptive Disorders | |||||
| Conduct Disorder | 2 (2) | 20 (33)a | 37 (46)a | χ2(3)=791. | <0.001 |
| Oppositional Defiant Disorder | 8 (6) | 47 (78)a | 76 (95)ab | χ2(3)=220.3 | <0.001 |
| ADHD | n/a | 43 (72) | 67 (84) | z=−1.6 | 0.1 |
| Anxiety Disorders | |||||
| Multiple Anxiety Disorders (>=2) | 7 (5) | 37 (62)a | 61 (76)a | χ2(3)=138.3 | <0.001 |
| Avoidance Disorder | 2 (2) | 10 (17)a | 17 (21)a | χ2(3)=27.2 | <0.001 |
| Separation Anxiety Disorder | 10 (8) | 32 (53)a | 53 (66)a | χ2(3)=93.8 | <0.001 |
| Post Traumatic Stress Disorder | 1 (1) | 1 (2) | 2 (3) | χ2(3)=1.0 | 0.8 |
| Agoraphobia | 3 (2) | 20 (33)a | 36 (45)a | χ2(3)=68.5 | <0.001 |
| Simple Phobia | 8 (6) | 24 (40)a | 37 (46)a | χ2(3)=55.8 | <0.001 |
| Social Phobia | 3 (2) | 13 (22)a | 38 (48)ab | χ2(3)=67.9 | <0.001 |
| Panic Disorder | 1 (1) | 3 (5) | 16 (20)ab | χ2(3)=29.6 | <0.001 |
| Generalized Anxiety Disorder | 2 (2) | 21 (35)a | 43 (54)ab | χ2(3)=91.7 | <0.001 |
p<0.05 vs. control
p<0.05 vs. BP-I without profile
CBCL Positive BP-I probands also had higher rates of special help in school, lower IQs, digit span, oral arithmetic scores, and GAF scores than CBCL negative profile BP-I probands (Table 3).
Table 3.
Academic, Cognitive, and Global Functioning
| Control | BP-I without Profile | BP-1 with Profile | Statistical Analsyis | ||
|---|---|---|---|---|---|
| N=129 | N=60 | N=80 | Test Statistic | p-value | |
| Academic Function | |||||
| Repeated grade | 9 (7) | 7 (12) | 11 (14) | χ2(3)=19.5 | <0.001 |
| Special Class | 3 (2) | 18 (30)a | 25 (32)a | χ2(3)=55.2 | <0.001 |
| Extra Help | 27 (21) | 31 (52)a | 58 (73)ab | χ2(3)=62.1 | <0.001 |
| Cognitive Functioning | |||||
| Vocabulary SS* | 12.6 ± 2.8 | 11.2 ± 3.1a | 10.2 ± 3.7a | χ2(3)=17.2 | <0.001 |
| Digit Span SS | 10.7 ± 2.8 | 10.3 ± 3.0 | 9.2 ± 2.5ab | χ2(3)=8.8 | <0.001 |
| Oral arithmetic SS | 12.1 ± 2.9 | 10.9 ± 3.2a | 9.4 ± 3.0ab | χ2(3)=14.6 | <0.001 |
| Digit symbol SS | 12.1 ± 2.6 | 7.5 ± 3.5a | 7.3 ± 3.1a | χ2(3)=59.8 | <0.001 |
| Full Scale IQ | 115.9 ± 11.4 | 106.5 ± 13.0a | 101.4 ± 15.4ab | χ2(3)=29.2 | <0.001 |
| Global Functioning | |||||
| GAF Score | 70.5 ± 8.6 | 43.1 ± 4.5a | 40.0 ± 6.1ab | χ2(3)=372.5 | <0.001 |
Scaled Score
p<0.05 vs. control
p<0.05 vs. BP-I without profile
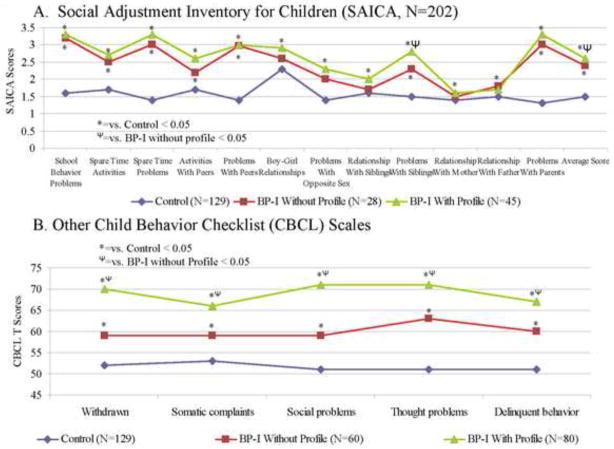
As shown in Figure 2, compared to controls, both BP-I proband groups were more likely to manifest more impaired scores for most of the SAICA items including school behavior problems, problems with peers, and problems with siblings (Figure 2A). As shown in Figure 2B, BP-I probands with a positive profile were more likely than profile negative BP-I probands to have more impaired scores on all other CBCL scales including withdrawn, social problems, and delinquent behavior.
Figure 2.
Psychosocial Functioning
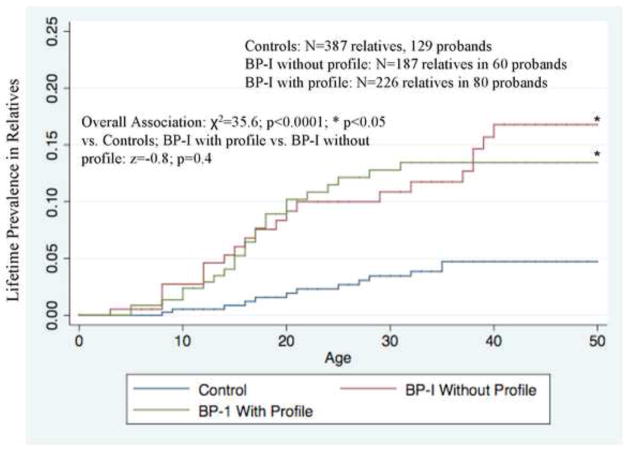
Familial Risk Analysis
The age-dependent cumulative, lifetime prevalence risk of BP-I disorder in relatives is illustrated in Figure 3. First-degree relatives of BP-I probands with and without the profile were significantly more likely than first-degree relatives of control probands to have BP-I disorder (Hazard Ratio (HR): 2.55; 95% Confidence Interval (CI): 1.29, 5.06; p=0.007; HR: 3.3; 95% CI: 1.66, 6.41, p=0.001; respectively). We found no significant difference between first-degree relatives of BP-I probands with the profile and first-degree relatives of BP-I without the profile (HR: 0.78; 95% CI: 0.43, 1.44; p=0.43).
Figure 3.
Familial Risk of Bipolar I Disorder in First-Degree Relatives
DISCUSSION
Our results show that BP-I probands with and without a positive CBCL-Severe Dysregulation profile significantly differed from Controls in patterns of psychiatric comorbidity, psychosocial and psychoeducational dysfunction, cognitive deficits as well as in their risk for BP-I disorder in first degree relatives. These results add to the emerging evidence for the utility of CBCL-Severe Dysregulation to help identify children very likely to receive a diagnosis of pediatric BP-I disorder if they were to be seen clinically.
Our results also showed that CBCL-positive BP-I probands consistently had more severe correlates on BP-I disorder relative to profile negative probands including earlier age of onset of BP-I disorder, higher rates of psychiatric hospitalization, higher rates of major depression, oppositional defiant disorder, social anxiety, panic disorder, and generalized anxiety disorder. Our results also showed that the overwhelming majority of BP-I disorder children with a negative CBCL Severe Dysregulation profile had an intermediate or subsyndromal emotional dysregulation profile previously termed CBCL-Deficient Emotional Self Regulation (DESR) profile (Spencer et al., 2011). Taken together these results indicate that the CBCL-Severe Dysregulation profile identifies BP-I children with a more severe and dysfunctional form of BP-I disorder.
Although the CBCL-Severe Dysregulation profile has been previously shown to have high diagnostic efficiency to predict a current (Faraone et al., 2005) and future (Biederman et al., 2009) diagnoses of pediatric BP-I disorder in the context of ADHD and of BP-I disorder (Biederman et al., 2012a; Biederman et al., 2012b), and has been replicated across multiple age groups, multiple treatment settings, and multiple cultures (Biederman et al., 1995; Carlson and Kelly, 1998; Dienes et al., 2002; Geller et al., 1998; Hazell et al., 1999; Wals et al., 2001), it has not always been associated with a diagnosis of BP-I disorder. However, even in negative studies, the CBCL-Severe Dysregulation profile has been shown to predict subsequent major depression, conduct disorder, poor psychosocial outcomes, and psychiatric hospitalization in children with ADHD (Biederman et al., 2009), all of which are correlates of pediatric BP-I disorder (Akiskal et al., 1995; Biederman et al., 1997; Goldstein et al., 2009; Wozniak et al., 2004). In the Volk et al. (2007) population based twin study, children with a positive CBCL-Severe Dysregulation profile had more oppositional defiant disorder (ODD), conduct disorder (CD), and ADHD and more frequently endorsed suicidal behaviors, which are also correlates of pediatric BP-I disorder. Moreover, in this latter study the CBCL-Severe Dysregulation profile study was found to be heritable and associated with the number of dopamine transporter (DAT1) 9-repeat 3′ untranslated region alleles in a region recently associated with pediatric BP-I disorder (Mick et al., 2008). Likewise, in the negative study by McGough et al. (2008), the CBCL-Severe Dysregulation profile was associated with generalized anxiety disorder, ODD, and CD, conditions also frequently associated with pediatric BP-I disorder. Finally, the negative study by Youngstrom et al. (2005), relied on archival data from a large sample from six urban community mental health centers (N=3086) with limited emphasis on operationalized diagnostic algorithms for defining pediatric BP-I disorder. Thus, differing diagnostic approaches and ascertainment strategies could account for the different findings of studies at various institutions.
Despite its potential utility, a positive CBCL-Severe Dysregulation profile should only be considered as a useful tool to help identify children at risk for BP-I disorder and in no way should it be viewed as synonymous with or a replacement for a clinical diagnosis of BP-I disorder (Biederman et al., 2009). Instead, it should be viewed in the same way as elevated blood pressure, smoking, or elevated levels of cholesterol are viewed in the primary care setting as risks for adverse medical outcomes and not as the adverse outcomes themselves.
Without any doubt, the diagnosis of pediatric BP-I disorder is a complicated and nontrivial matter. It requires careful examination of the child, parental reporting of the child’s history and high level of clinical expertise and acumen. No screening test can substitute for the judgment of well-trained clinicians in making the diagnosis. Unfortunately, highly trained child mental health clinicians with expertise in making a diagnosis of bipolar disorder in a child are not widely available in many regions of the country, leaving the primary care physician with the responsibility to determine which children in their practices are at high risk for very serious adverse mental health problems. Considering the well documented high morbidity and disability associated with pediatric BP-I disorder, identifying such cases can facilitate appropriate referrals and focus limited societal resources towards a subgroup of children at very high risk for compromised outcomes.
Our findings need to be viewed in light of some methodological limitations. Although highly selected, trained and supervised raters administered the structured diagnostic interviews, they were not clinicians. Although lay interviewers may not elicit the same quality of information as clinician interviewers, we documented very good kappa coefficients of agreement between lay interviewers and expert clinicians (see Methods). Moreover, the diagnosis of BP-I disorder in probands relied also on a clinical assessment by an experienced clinician with expertise in pediatric BP-I disorder (J.W.). Because the sample was referred and largely Caucasian, findings may not generalize to community samples and other ethnic groups.
Despite these limitations, our work suggests that children with a positive CBCL-Severe Dysregulation profile have a pattern of personal and familial correlates highly consistent with a diagnosis of BP-I disorder and even higher levels of clinical severity and dysfunction than other children with BP-I disorder with a negative profile. While the CBCL remains an attractive tool for screening children at risk for adverse outcomes in clinical settings due to its ease of administration, brevity, and reliability (Achenbach, 1991), we emphasize that clinicians should not use the CBCL Severe Dysregulation to make a diagnosis of bipolar disorder.
Acknowledgments
This work was supported by NIH grants K08MH001503 and R01MH066237 to Dr Wozniak and R01MH050657 and R01HD036317 to Dr Biederman. This work was also supported by a grant from the Heinz C. Prechter Bipolar Research Fund, the support of members of the MGH Pediatric Psychopharmacology Council, and the Susan G. Berk Endowed Fund for Juvenile Bipolar Disorder.
ROLE OF FUNDING SOURCE
The study sponsors had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript.
ABBREVIATIONS
- ADHD
Attention-deficit/hyperactivity disorder
- CBCL
Child Behavior Checklist
- BP-I
Bipolar-I Disorder
Footnotes
CONFLICT OF INTEREST
Dr. Joseph Biederman is currently receiving research support from the following sources: Elminda, Janssen, McNeil, and Shire. In 2012, Dr. Joseph Biederman received an honorarium from the MGH Psychiatry Academy for a tuition-funded CME course. In 2011, Dr. Joseph Biederman gave a single unpaid talk for Juste Pharmaceutical Spain, received honoraria from the MGH Psychiatry Academy for a tuition-funded CME course, and received an honorarium for presenting at an international scientific conference on ADHD. He also received an honorarium from Cambridge University Press for a chapter publication. Dr. Biederman received departmental royalties from a copyrighted rating scale used for ADHD diagnoses, paid by Eli Lilly, Shire and AstraZeneca; these royalties are paid to the Department of Psychiatry at MGH. In 2010, Dr. Joseph Biederman received a speaker’s fee from a single talk given at Fundación Dr.Manuel Camelo A.C. in Monterrey Mexico. Dr. Biederman provided single consultations for Shionogi Pharma Inc. and Cipher Pharmaceuticals Inc.; the honoraria for these consultations were paid to the Department of Psychiatry at the MGH. Dr. Biederman received honoraria from the MGH Psychiatry Academy for a tuition-funded CME course. In previous years, Dr. Joseph Biederman received research support, consultation fees, or speaker’s fees for/from the following additional sources: Abbott, Alza, AstraZeneca, Boston University, Bristol Myers Squibb, Celltech, Cephalon, Eli Lilly and Co., Esai, Fundacion Areces (Spain), Forest, Glaxo, Gliatech, Hastings Center, Janssen, McNeil, Medice Pharmaceuticals (Germany), Merck, MMC Pediatric, NARSAD, NIDA, New River, NICHD, NIMH, Novartis, Noven, Neurosearch, Organon, Otsuka, Pfizer, Pharmacia, Phase V Communications, Physicians Academy, The Prechter Foundation, Quantia Communications, Reed Exhibitions, Shire, the Spanish Child Psychiatry Association, The Stanley Foundation, UCB Pharma Inc., Veritas, and Wyeth.
In the past year, Dr. Stephen Faraone received consulting income and research support from Shire, Otsuka and Alcobra and research support from the National Institutes of Health (NIH). In previous years, he received consulting fees or was on Advisory Boards or participated in continuing medical education programs sponsored by: Shire, McNeil, Janssen, Novartis, Pfizer and Eli Lilly. Dr. Faraone receives royalties from books published by Guilford Press: Straight Talk about Your Child’s Mental Health and Oxford University Press: Schizophrenia: The Facts.
In the last three years Dr. Thomas Spencer has received research support from or has been an Advisor or on an Advisory Board of the following sources: Alcobra, Shire Laboratories, Inc, Eli Lilly & Company, Janssen Pharmaceutical, McNeil Pharmaceutical, Novartis Pharmaceuticals, Cephalon, the National Institute of Mental Health and the Department of Defense. Dr. Spencer receives research support from Royalties and Licensing fees on copyrighted ADHD scales through MGH Corporate Sponsored Research and Licensing. Dr. Spencer has a US Patent Application pending (Provisional Number #61/233,686), through MGH corporate licensing, on a method to prevent stimulant abuse.
Janet Wozniak MD is a speaker for Primedia/MGH Psychiatry Academy, and receives research support from McNeil, Shire, Janssen, and Johnson & Johnson. Her spouse, John Winkelman MD, PhD, is a consultant/advisory board for Impax Laboratories, Pfizer, UCB, Zeo Inc., Sunovion, and receives research support from GlaxoSmithKline.
MaryKate Martelon and K. Yvonne Woodworth report no conflicts of interest.
CONTRIBUTORS
Dr. Biederman had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Dr. Biederman substantially contributed to the conception and design, drafting, critical revision of the intellectual content, supervision, administrative/technical/material support, and funding for this manuscript. Ms. Martelon substantially contributed to the data analysis and interpretation, drafting, and statistical analysis for this manuscript. Dr. Faraone substantially contributed to the conception and design, data analysis and interpretation, critical revision of the intellection content, statistical analysis, and funding for this manuscript. Ms. Woodworth substantially contributed to the drafting, critical revision of the intellectual content, and administrative/technical/material support for this manuscript. Dr. Spencer substantially contributed to the conception and design, drafting, critical revision of the intellectual content, administrative/technical/material support, and supervision for this manuscript. Dr. Wozniak substantially contributed to the conception and design, drafting, critical revision of the intellectual content, administrative/technical/material support, and supervision for this manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Achenbach TM. Manual for the Child Behavior Checklist/4-18 and the 1991 Profile. University of Vermont, Department of Psychiatry; Burlington, VT: 1991. [Google Scholar]
- Akiskal H, Maser J, Zeller P, Endicott J, Coryell W, Keller M, Warshaw M, Clayton P, Goodwin F. Switching from ‘unipolar’ to bipolar II. Arch Gen Psychiatry. 1995;52:114–123. doi: 10.1001/archpsyc.1995.03950140032004. [DOI] [PubMed] [Google Scholar]
- Althoff RR, Rettew DC, Faraone SV, Boomsma DI, Hudziak JJ. Latent class analysis shows strong heritability of the CBCL-juvenile bipolar phenotype. Biol Psychiatry. 2006;60:903–911. doi: 10.1016/j.biopsych.2006.02.025. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone S, Hatch M, Mennin D, Taylor A, George P. Conduct disorder with and without mania in a referred sample of ADHD children. J Affect Disord. 1997;44:177–188. doi: 10.1016/s0165-0327(97)00043-8. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone SV, Keenan K, Benjamin J, Krifcher B, Moore C, Sprich-Buckminster S, Ugaglia K, Jellinek MS, Steingard R, Spencer T, Norman D, Kolodny R, Kraus I, Perrin J, Keller MB, Tsuang MT. Further evidence for family-genetic risk factors in attention deficit hyperactivity disorder. Patterns of comorbidity in probands and relatives in psychiatrically and pediatrically referred samples. Arch Gen Psychiatry. 1992;49:728–738. doi: 10.1001/archpsyc.1992.01820090056010. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone SV, Mick E, Williamson S, Wilens TE, Spencer TJ, Weber W, Jetton J, Kraus I, Pert J, Zallen B. Clinical correlates of ADHD in females: findings from a large group of girls ascertained from pediatric and psychiatric referral sources. J Am Acad Child Adolesc Psychiatry. 1999;38:966–975. doi: 10.1097/00004583-199908000-00012. [DOI] [PubMed] [Google Scholar]
- Biederman J, Monuteaux M, Mick E, Spencer T, Wilens T, Klein K, Price JE, Faraone SV. Psychopathology in females with attention-deficit/hyperactivity disorder: A controlled, five-year prospective study. Biol Psychiatry. 2006a;60:1098–1105. doi: 10.1016/j.biopsych.2006.02.031. [DOI] [PubMed] [Google Scholar]
- Biederman J, Monuteaux MC, Mick E, Spencer T, Wilens TE, Silva JM, Snyder LE, Faraone SV. Young adult outcome of attention deficit hyperactivity disorder: a controlled 10-year follow-up study. Psychol Med. 2006b;36:167–179. doi: 10.1017/S0033291705006410. [DOI] [PubMed] [Google Scholar]
- Biederman J, Petty CR, Day H, Goldin RL, Spencer T, Faraone SV, Surman CB, Wozniak J. Severity of the aggression/anxiety-depression/attention child behavior checklist profile discriminates between different levels of deficits in emotional regulation in youth with attention-deficit hyperactivity disorder. J Dev Behav Pediatr. 2012a;33:236–243. doi: 10.1097/DBP.0b013e3182475267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biederman J, Petty CR, Monuteaux MC, Evans M, Parcell T, Faraone SV, Wozniak J. The child behavior checklist-pediatric bipolar disorder profile predicts a subsequent diagnosis of bipolar disorder and associated impairments in ADHD youth growing up: a longitudinal analysis. J Clin Psychiatry. 2009;70:732–740. doi: 10.4088/JCP.08m04821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biederman J, Spencer T, Lomedico A, Day H, Petty CR, Faraone SV. Deficient emotional self-regulation and pediatric attention deficit hyperactivity disorder: a family risk analysis. Psychol Med. 2012b;42:639–646. doi: 10.1017/S0033291711001644. [DOI] [PubMed] [Google Scholar]
- Biederman J, Wozniak J, Kiely K, Ablon S, Faraone S, Mick E, Mundy E, Kraus I. CBCL clinical scales discriminate prepubertal children with structured-interview derived diagnosis of mania from those with ADHD. J Am Acad Child Adolesc Psychiatry. 1995;34:464–471. [PubMed] [Google Scholar]
- Carlson GA, Kelly KL. Manic symptoms in psychiatrically hospitalized children- what do they mean? J Affect Disord. 1998;51:123–135. doi: 10.1016/s0165-0327(98)00211-0. [DOI] [PubMed] [Google Scholar]
- Dienes KA, Chang KD, Blasey CM, Adleman NE, Steiner H. Characterization of children of bipolar parents by parent report CBCL. J Psychiatr Res. 2002;36:337–345. doi: 10.1016/s0022-3956(02)00019-5. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Althoff RR, Hudziak JJ, Monuteaux MC, Biederman J. The CBCL predicts DSM bipolar disorder in children: A receiver operating characteristic curve analysis. Bipolar Disord. 2005;7:518–524. doi: 10.1111/j.1399-5618.2005.00271.x. [DOI] [PubMed] [Google Scholar]
- Geller B, Warner K, Williams M, Zimerman B. Prepubertal and young adolescent bipolarity versus ADHD: assessment and validity using the WASH-U-KSADS, CBCL and TRF. J Affect Disord. 1998;51:93–100. doi: 10.1016/s0165-0327(98)00176-1. [DOI] [PubMed] [Google Scholar]
- Goldstein TR, Birmaher B, Axelson D, Goldstein BI, Gill MK, Esposito-Smythers C, Ryan ND, Strober MA, Hunt J, Keller M. Psychosocial functioning among bipolar youth. J Affect Disord. 2009;114:174–183. doi: 10.1016/j.jad.2008.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazell P, Lewin T, Carr V. Confirmation that Child Behavior Checklist clinical scales discriminate juvenile mania from attention deficit hyperactivity disorder. J Paediatr Child Health. 1999;35:199–203. doi: 10.1046/j.1440-1754.1999.t01-1-00347.x. [DOI] [PubMed] [Google Scholar]
- Hudziak J, Althoff RR, Rettew DC, Derks EM, Faraone SV. The prevalence and genetic architecture of CBCL-juvenile bipolar disorder. Biol Psychiatry. 2005;58:562–568. doi: 10.1016/j.biopsych.2005.03.024. [DOI] [PubMed] [Google Scholar]
- McGough JJ, Loo SK, McCracken JT, Dang J, Clark S, Nelson SF, Smalley SL. CBCL pediatric bipolar disorder profile and ADHD: comorbidity and quantitative trait loci analysis. J Am Acad Child Adolesc Psychiatry. 2008;47:1151–1157. doi: 10.1097/CHI.0b013e3181825a68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, Georgiades K, Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication--Adolescent Supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mick E, Biederman J, Pandina G, Faraone SV. A preliminary meta-analysis of the child behavior checklist in pediatric bipolar disorder. Biol Psychiatry. 2003;53:1021–1027. doi: 10.1016/s0006-3223(03)00234-8. [DOI] [PubMed] [Google Scholar]
- Mick E, Kim JW, Biederman J, Wozniak J, Wilens T, Spencer T, Smoller JW, Faraone SV. Family based association study of pediatric bipolar disorder and the dopamine transporter gene (SLC6A3) Am J Med Genet B Neuropsychiatr Genet. 2008;147B:1182–1185. doi: 10.1002/ajmg.b.30745. [DOI] [PubMed] [Google Scholar]
- Orvaschel H. Schedule for Affective Disorder and Schizophrenia for School-Age Children Epidemiologic Version. Nova Southeastern University, Center for Psychological Studies; Ft. Lauderdale: 1994. [Google Scholar]
- Spencer TJ, Faraone SV, Surman CB, Petty C, Clarke A, Batchelder H, Wozniak J, Biederman J. Toward defining deficient emotional self-regulation in children with attention-deficit/hyperactivity disorder using the Child Behavior Checklist: a controlled study. Postgrad Med. 2011;123:50–59. doi: 10.3810/pgm.2011.09.2459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Meter AR, Moreira AL, Youngstrom EA. Meta-analysis of epidemiologic studies of pediatric bipolar disorder. J Clin Psychiatry. 2011;72:1250–1256. doi: 10.4088/JCP.10m06290. [DOI] [PubMed] [Google Scholar]
- Volk HE, Todd RD. Does the child behavior checklist juvenile bipolar disorder phenotype identify bipolar disorder? Biol Psychiatry. 2007;62:115–120. doi: 10.1016/j.biopsych.2006.05.036. [DOI] [PubMed] [Google Scholar]
- Wals M, Hillegers MH, Reichart CG, Ormel J, Nolen WA, Verhulst FC. Prevalence of psychopathology in children of a bipolar parent. J Am Acad Child Adolesc Psychiatry. 2001;40:1094–1102. doi: 10.1097/00004583-200109000-00019. [DOI] [PubMed] [Google Scholar]
- Wozniak J, Biederman J, Kwon A, Mick E, Faraone S, Orlovsky K, Schnare L, Cargol C, van Grondelle A. How cardinal are cardinal symptoms in pediatric bipolar disorder? An examination of clinical correlates. Biol Psychiatry. 2005;58:583–588. doi: 10.1016/j.biopsych.2005.08.014. [DOI] [PubMed] [Google Scholar]
- Wozniak J, Faraone SV, Mick E, Monuteaux M, Coville A, Biederman J. A controlled family study of children with DSM-IV bipolar-I disorder and psychiatric co-morbidity. Psychol Med. 2010;40:1079–1088. doi: 10.1017/S0033291709991437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wozniak J, Monuteaux M, Richards J, Lail K, Faraone SV, Biederman J. Convergence between structured diagnostic interviews and clinical assessment on the diagnosis of pediatric-onset bipolar disorder. Biol Psychiatry. 2003;53:938–944. doi: 10.1016/s0006-3223(03)00344-5. [DOI] [PubMed] [Google Scholar]
- Wozniak J, Spencer T, Biederman J, Kwon A, Monuteaux M, Rettew J, Lail K. The clinical characteristics of unipolar versus bipolar major depression in ADHD youth. J Affect Disord. 2004;82:S59–S69. doi: 10.1016/j.jad.2004.05.013. [DOI] [PubMed] [Google Scholar]
- Youngstrom E, Youngstrom JK, Starr M. Bipolar diagnoses in community mental health: Achenbach Child Behavior Checklist profiles and patterns of comorbidity. Biol Psychiatry. 2005;58:569–575. doi: 10.1016/j.biopsych.2005.04.004. [DOI] [PubMed] [Google Scholar]