Abstract
The neurobiological basis of psychogenic movement disorders remains poorly understood and the management of these conditions difficult. Functional neuroimaging studies have provided some insight into the pathophysiology of disorders implicating particularly the prefrontal cortex, but there are no studies on psychogenic dystonia, and comparisons with findings in organic counterparts are rare. To understand the pathophysiology of these disorders better, we compared the similarities and differences in functional neuroimaging of patients with psychogenic dystonia and genetically determined dystonia, and tested hypotheses on the role of the prefrontal cortex in functional neurological disorders. Patients with psychogenic (n = 6) or organic (n = 5, DYT1 gene mutation positive) dystonia of the right leg, and matched healthy control subjects (n = 6) underwent positron emission tomography of regional cerebral blood flow. Participants were studied during rest, during fixed posturing of the right leg and during paced ankle movements. Continuous surface electromyography and footplate manometry monitored task performance. Averaging regional cerebral blood flow across all tasks, the organic dystonia group showed abnormal increases in the primary motor cortex and thalamus compared with controls, with decreases in the cerebellum. In contrast, the psychogenic dystonia group showed the opposite pattern, with abnormally increased blood flow in the cerebellum and basal ganglia, with decreases in the primary motor cortex. Comparing organic dystonia with psychogenic dystonia revealed significantly greater regional blood flow in the primary motor cortex, whereas psychogenic dystonia was associated with significantly greater blood flow in the cerebellum and basal ganglia (all P < 0.05, family-wise whole-brain corrected). Group × task interactions were also examined. During movement, compared with rest, there was abnormal activation in the right dorsolateral prefrontal cortex that was common to both organic and psychogenic dystonia groups (compared with control subjects, P < 0.05, family-wise small-volume correction). These data show a cortical–subcortical differentiation between organic and psychogenic dystonia in terms of regional blood flow, both at rest and during active motor tasks. The pathological prefrontal cortical activation was confirmed in, but was not specific to, psychogenic dystonia. This suggests that psychogenic and organic dystonia have different cortical and subcortical pathophysiology, while a derangement in mechanisms of motor attention may be a feature of both conditions.
Keywords: psychogenic movement disorder, fixed dystonia, DYT1 gene, functional imaging, motor, cerebellum, basal ganglia, dorsolateral prefrontal cortex, attention
Introduction
Medically unexplained neurological symptoms account for up to 30% of neurology out-patient referrals (Carson et al., 2000; Stone et al., 2009), and movement disorders are a common presentation (Hinson and Haren, 2006). The historical nomenclature is complex, emphasizing poor understanding of their pathophysiology. Some terms are descriptive (functional disorders, medically unexplained symptoms), whilst others refer to putative aetiology (psychogenic, hysteria, non-organic) or mechanism (dissociative or conversion disorder) (Rowe, 2010). Here, we use the term ‘psychogenic’ because of its widespread clinical use, particularly in relation to movement disorders (Nowak and Fink, 2009).
Despite the use of established diagnostic criteria (Fahn and Williams, 1988; Williams et al., 1995; Gupta and Lang, 2009), the diagnosis of psychogenic movement disorders remains a significant challenge (Lang and Voon, 2011) and a ‘crisis for neurology’ (Hallett, 2006). A better understanding of their neurobiology may help improve diagnosis, treatment and prognosis, which remain poor.
Functional neuroimaging has been used to examine sensory and motor psychogenic neurological disorders (Tiihonen et al., 1995; Marshall et al., 1997; Spence et al., 2000; Vuilleumier et al., 2001; Mailis-Gagnon et al., 2003; Werring et al., 2004; Burgmer et al., 2006; Ghaffar et al., 2006; de Lange et al., 2007, 2010; Kanaan et al., 2007, 2010; Stone et al., 2007; Cojan et al., 2009; Voon et al., 2010a, b). The focus has been predominantly on negative motor symptoms, such as paralysis. To our knowledge, no neuroimaging studies have specifically examined psychogenic dystonia. Moreover, the published neuroimaging studies have not compared psychogenic neurological disorders with their organic counterparts, instead comparing the changes in neural activation with performance of an unaffected limb or healthy volunteers (Nowak and Fink, 2009).
We studied the pathophysiology of psychogenic dystonia using functional neuroimaging in patients with psychogenic dystonia, compared with both healthy controls, and patients with genetically confirmed organic dystonia. To investigate movement-related activations in a homogeneous sample, we chose to examine patients presenting with fixed dystonia of the right lower limb. While dystonia of the lower limb can arise from organic neurological disease (McKeon et al., 2008), a fixed immobile posture first arising in adulthood without clinical or laboratory evidence for organic disease is a characteristic presentation of psychogenic dystonia (Lang, 1995; Schrag et al., 2004; Hinson and Haren, 2006; Gupta and Lang, 2009; Ibrahim et al., 2009; Hallett, 2010). All patients fulfilled probable to clinically established criteria for psychogenic dystonia (Fahn and Williams, 1988). We used H215O PET to measure normalized regional cerebral blood flow during three tasks in which participants rested, held a fixed posture or undertook paced ankle movements of their right leg (which was affected in all patients). Continuous monitoring of the surface EMG and footplate manometry were used to monitor task performance.
Previous studies using PET neuroimaging on organic dystonia have revealed disease-related metabolic patterns seen in both active and inactive states (Eidelberg et al., 1998; Hutchinson et al., 2000; Siebner et al., 2003), leading us to examine group differences in regional cerebral blood flow averaged across all tasks (task-independent effects). We predicted that this would reveal both similarities and differences between organic and psychogenic dystonia, consistent with previous electrophysiological findings (Espay et al., 2006; Avanzino et al., 2008; Quartarone et al., 2009). We also predicted that there would be abnormal prefrontal cortical activation in psychogenic dystonia during movement-related tasks (task-dependent effects, revealed as group × task interactions), given previous work that has implicated the prefrontal cortex as a common neurobiological substrate in psychogenic movement disorders (Nowak and Fink, 2009; Bell et al., 2010).
Materials and methods
Participants
We studied three groups of participants: (i) patients with psychogenic dystonia (n = 6); (ii) patients with organic dystonia due to a confirmed DYT1 gene mutation (n = 5); and (iii) healthy control subjects (n = 6), matched for age and gender. In all patients, dystonia affected the right lower limb. All patients with psychogenic dystonia fulfilled current criteria for clinically definite psychogenic dystonia (Gupta and Lang, 2009). Patients were recruited by experienced movement disorders specialists from the movement disorders outpatient clinic, National Hospital for Neurology and Neurosurgery, University College London Hospitals NHS Foundation Trust, London, UK (Schrag et al., 2004; Ibrahim et al., 2009).
The following exclusion criteria were applied: age <18 years, pregnancy, additional neurological signs or abnormalities on clinical investigations, serious medical comorbidity and current major affective or psychotic disorders (American Psychiatric Association, 1994). All patients with psychogenic dystonia had unremarkable standard investigations for secondary dystonia (Calne and Lang, 1988), including MRI brain and spine, except for one finding of left frontal small focal dysplasia and one of mild lumbar disc protrusion. Two patients had additionally undergone CSF examination with normal results. Both groups of patients were tested for the DYT1 gene mutation. No patient had concomitant complex regional pain syndrome. Follow-up information was available for all patients with psychogenic dystonia >10 years post imaging, with no change in diagnosis or resolution of dystonia.
The study was approved by the joint ethics committee of the National Hospital for Neurology and Neurosurgery and the Institute of Neurology, and the Administration of Radioactive Substances Advisory Committee, UK. Participants gave written informed consent in accordance with the Declaration of Helsinki.
Task and monitoring
There were three types of task (‘rest’, ‘post’ or ‘move’). Participants lay supine in the scanner, with eyes open, and their right foot held in a customized open cast strapped to their lower limb. Thus, the right foot was held in an inverted and plantar-flexed position, ensuring that the position of the limb was controlled in all three types of tasks.
During tasks, starting 30 s before scanning, participants listened to pacing cues generated by a metronome. During rest tasks, participants explicitly lay relaxed. During the post task, participants maintained the distal part of the right lower limb in a fixed tonically contracted posture with the foot both inverted and plantar-flexed, which, for the control participants, simulated the dystonic posture of patients. During the move task, participants flexed and extended their right foot against a footplate dynamometer within the cast every 8 s, in time with the metronome (0.125 Hz) over 125 s. The range of ankle movement was the maximum possible extension–flexion movement of the ankle for each subject. We also confirmed that all patients were able to perform this task with visible movement in all patients. Participants were asked to relax the left lower limb throughout. Each type of task was repeated four times per participant, in a counterbalanced order.
Surface EMG recordings were obtained from right gastrocnemius and tibialis anterior muscles, and left (contralateral) gastrocnemius. EMG and footplate activity were monitored using a computer monitor, allowing for monitoring of EMG changes during post and move tasks against a subject-specific electrophysiological baseline. The EMG data were analysed using Signal software (version 4.07, Cambridge Electronic Design Ltd.) to calculate the root mean square amplitude over each scanning epoch per task.
Statistical analyses
SPSS software (version 16.0.2; SPSS Inc.) was used for statistical analyses of the clinical characteristics of the participants and the EMG data related to task monitoring. Repeated-measures ANOVA was performed on the EMG data, with ‘Group' as a between-subjects factor (three levels: controls, psychogenic dystonia and organic dystonia) and ‘Task' (three levels: rest, post and move) and ‘Muscle' (two levels: right gastrocnemius and tibialis anterior muscles) as within-subjects factors. Mauchly’s test was performed to examine for a violation of the assumption of sphericity, and, if present, the degrees of freedom were corrected using the Greenhouse–Geisser method. The significance level was set at P < 0.05. Conditional on a significant F-value, post hoc t-tests were performed to explore the strength of the main effects.
Positron emission tomography data acquisition and analyses
Regional cerebral blood flow was measured from the distribution of radioactivity following an intravenous injection of 15O-labelled water (H215O) using a CTI Siemens ECAT HR+ PET scanner. Twelve scans were acquired per participant, with an interscan interval of ∼8 min. Over 20 s, 6–10 mCi were delivered. Image acquisition began 5 s before the rising phase of the count curve, ∼30 s after injection and continued for 90 s. Correction for tissue attenuation used a transmission scan from 68Ga/68Ge sources. Corrected data were reconstructed by 3D filtered back-projection with 63 2.4-mm thick transverse planes (128 × 128 2.1-mm pixels in plane). A full description of the H215O activation technique is given (Siebner et al., 2003; Friston, 2007).
Data were preprocessed and analysed with statistical parametric mapping using SPM8 software (Wellcome Trust Centre for Neuroimaging, ION, London, UK; http://www.fil.ion.ucl.ac.uk/spm/software/spm8/) implemented in MATLAB 7 (version R2010b, The MathWorks, Inc.) using standardized procedures (Friston et al., 1994; Friston, 2007), including realignment for head movements using the first scan of each participant as a reference, and spatial warping to a standardized anatomic space (Talairach and Tournoux, 1988), by matching each realigned image to the PET template of the Montreal Neurological Institute (MNI) (Friston et al., 1995). Normalized images were smoothed with an isotropic Gaussian kernel of 16-mm full-width at half-maximum to both accommodate anatomic heterogeneity between subjects and permit the application of Gaussian fields to the derived statistical images (Friston et al., 1990).
The group, task, subject-specific and covariate effects (global blood flow) were estimated according to the general linear model at each voxel using a flexible factorial design (Friston et al., 1994). We specified three factors (group, task and subject) and between-subject grand mean scaling. Global effects were accounted for by scan-specific proportional scaling of global activity to a nominal mean global activity of 50 ml/dl/min. Supplementary Fig. 1 shows the design matrix.
SPM(t) maps were generated to assess the effects of Task and Group, and the interaction of these factors. To test hypotheses about regionally specific group and/or task effects, the estimates were compared using t-contrasts. Analysis of conjunctions was performed based on the global null (Friston et al., 1999), indicating that contrasts were consistently high and jointly significant (Friston et al., 2005). A threshold of P < 0.05 with whole-brain correction for multiple independent comparisons was applied when examining for the main effect of Task across all groups. When examining the main effect of Group across all tasks, the SPM maps produced were inclusively masked by the contrast of move versus rest of the control group to identify changes within a core motor network (there were no significant differences between the ‘all subjects’ motor map and the ‘controls only’ motor map). Given the neuroimaging literature on other psychogenic movement disorders that points to a role of the prefrontal cortex, Brodmann areas 10 and 46 bilaterally were selected a priori as anatomical regions of interest using the WFU PickAtlas SPM toolbox (version 3.0.3; Functional MRI Laboratory, Wake Forest University School of Medicine, NC, USA; http://fmri.wfubmc.edu/software/PickAtlas) (Maldjian et al., 2003), when examining for Group × Task interactions, using a small-volume correction at a corrected threshold P < 0.05. All activations are reported using MNI coordinates.
Results
Table 1 summarizes the demographic and clinical characteristics of the patients with psychogenic and organic dystonia. All participants completed all tasks. EMG data were successfully obtained from all participants, except two in the psychogenic dystonia group, owing to technical problems.
Table 1.
Clinical characteristics of the patients with psychogenic or organic dystonia
| Patient ID | Age (years) | Sex | Precipitant/cause | Disease duration (years) | Fixed or mobile | Overall extent/severity of dystonia at time of investigation | 10-year follow-up |
|---|---|---|---|---|---|---|---|
| Psy-1 | 42 | M | Neck injury | 6 | Fixed | Right lower limb only | No change, but responds to botulinum toxin injections |
| Psy-2 | 46 | F | Arthroscopy | 7 | Fixed | Right lower limb only | No change, but responds to botulinum toxin injections |
| Psy-3 | 39 | F | Peripheral injury and psychological stressor | 7 | Fixed | Right upper and lower limb | No change overall. Initially good improvement with botulinum toxin injections and cognitive behavioural therapy but recurrence a few years later |
| Psy-4 | 25 | F | Tingling and weakness of legs | 2 | Fixed | Right lower limb only | Fluctuations, worsened with development of other functional symptoms |
| Psy-5 | 48 | F | During psychotherapy | 4 | Fixed | Generalized (both ankles and right upper limb); wheelchair bound; additional functional symptoms | No change |
| Psy-6 | 34 | M | Peripheral injury | 8 | Fixed | Both lower limbs; wheelchair bound; additional functional symptoms | Partial improvement with bilateral tibial nerve neurolysis with phenol injections; able to walk with stick |
| Org-1 | 22 | F | DYT1 | 14 | Mobile | Generalized; can walk unaided with medication | Some progression but continues to respond to medication |
| Org-2 | 31 | M | DYT1 | 9 | Relatively fixed right leg, but can return to normal position | Generalized; can walk unaided but with difficulty | No follow-up |
| Org-3 | 34 | M | DYT1 | 28 | Mobile | Generalized; able to walk unaided with medication | Some progression but responds to medication; no recent follow-up |
| Org-4 | 53 | F | DYT1 | 36 | Mobile | Generalized; walks with stick, due to task-specific dystonia right arm switched to using left hand | Response to medication, but progressive disease course. Underwent pallidal stimulation with improvement |
| Org-5 | 36 | F | DYT1 | 10 | Mobile | Mildly affected (right hand tremor and writer’s cramp, and mild foot dystonia) | No follow-up |
Main effect of task: expected changes in the motor network during movement or posture compared with rest
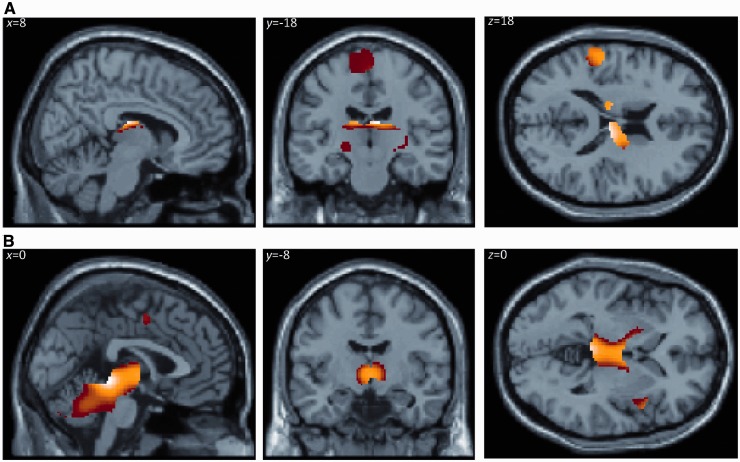
The performance of movement of the right foot (move versus rest, all groups) was associated with expected increases in regional cerebral blood flow in the core motor network, engaging left sensorimotor cortex (medial leg area), bilateral parietal cortices, bilateral thalamus, bilateral putamen and bilateral cerebellum (Fig. 1 and Supplementary Table 1). Maintaining a fixed posture with the right foot against the footplate (post versus rest, all groups) was associated with similar brain activation and there were no significant differences in regional cerebral blood flow revealed by the contrast move versus post across all groups, signifying that the post task provoked similar activation as the move task when compared with rest (pooling data from all groups).
Figure 1.
SPM(t) map of regional cerebral blood flow differences for the contrast of move versus rest (P < 0.05, corrected) averaged across all three groups. The sagittal (x = −6), coronal (y = −18) and axial (z = −2) images are projected onto a representative brain T1-weighted image in standard anatomical space (MNI template).
Main effect of group: cortical–subcortical differentiation in regional cerebral blood flow characterizes the distinction between organic and psychogenic dystonia
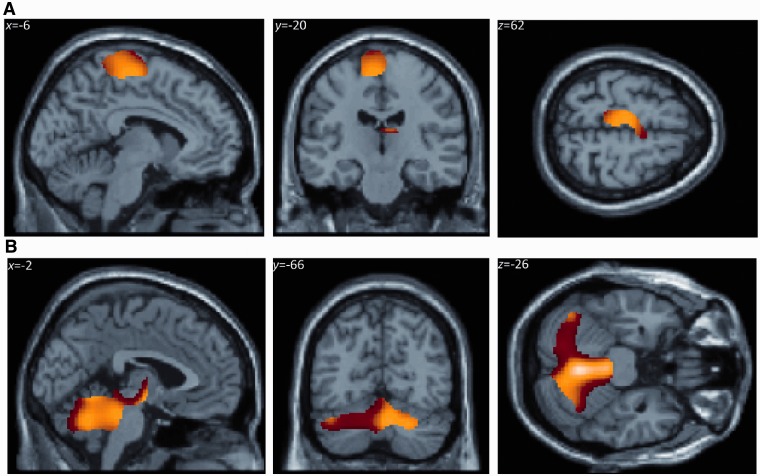
The global effects of group, averaged across all tasks, revealed significant differences between psychogenic and organic dystonia. Comparing organic dystonia with healthy controls revealed significant increases in regional cerebral blood flow in left primary motor cortex (medial leg area), left premotor cortex, bilateral parietal cortices, bilateral thalamus, right globus pallidus internus and bilateral cerebellum, and decreases in regional cerebral blood flow in bilateral thalamus and bilateral cerebellum (Fig. 2A and B; Tables 2 and 3). Compared with healthy control subjects, psychogenic dystonia was associated with significant increases in regional cerebral blood flow in left globus pallidus internus, right caudate, bilateral cerebellum and bilateral thalamus, and abnormally decreased regional cerebral blood flow in left primary motor cortex (medial leg area), left supplementary motor area, left thalamus and left cerebellum (Fig. 3A and B; Tables 4 and 5). Comparing organic dystonia with psychogenic dystonia revealed significant increases in regional cerebral blood flow in left primary motor cortex (medial leg area), left premotor area, right parietal cortex, right thalamus, right caudate and left cerebellum, whereas psychogenic dystonia was associated with significantly greater regional cerebral blood flow in cerebellum, putamen, thalamus and left subthalamic nucleus when compared with organic dystonia (Fig. 4A and B; Supplementary Table 2A and B).
Figure 2.
SPM(t) maps showing differences in regional cerebral blood flow between organic dystonia group and control subjects, averaged across all three tasks. The maps show regions with either increased (A) or decreased (B) regional cerebral blood flow (P < 0.05, corrected), within the core motor network defined by regions that in control subjects showed activation in the contrast move versus rest (P < 0.05, corrected).
Table 2.
Cluster peaks of increased normalized regional cerebral blood flow for the contrast organic dystonia versus control subjects averaged across all tasks, within a core motor network, thresholded P < 0.05, family-wise error corrected for multiple comparisons
| Location | Laterality | Coordinates of peak activity |
T-value of peak regional cerebral blood flow difference | ||
|---|---|---|---|---|---|
| x | y | z | |||
| Premotor cortex | Left | −52 | 0 | 8 | 8.73 |
| Premotor cortex | Left | −16 | −16 | 74 | 6.35 |
| Primary motor cortex (leg area) | Left/Right | 2 | −32 | 70 | 13.64 |
| Temporoparietal junction | Left | −56 | −24 | 18 | 17.57 |
| Temporoparietal junction | Right | 66 | −36 | 20 | 12.18 |
| Insula | Left | −40 | 0 | 4 | 5.59 |
| Thalamus | Right | 8 | −18 | 18 | 25.23 |
| Thalamus | Right | 16 | −8 | 20 | 22.20 |
| Thalamus | Left | −14 | −16 | 18 | 19.29 |
| Lateral thalamus | Right | 30 | −26 | 4 | 8.39 |
| Globus pallidus internus/thalamus | Right | 24 | −16 | −6 | 5.75 |
| Cerebellar hemisphere | Left | −28 | −50 | −28 | 15.80 |
| Cerebellar hemisphere | Right | 32 | −44 | −36 | 9.01 |
| Cerebellar hemisphere | Right | 18 | −32 | −24 | 6.65 |
Coordinates refer to standard anatomic space using the MNI template.
Table 3.
Cluster peaks of increased normalized regional cerebral blood flow for the contrast control subjects versus organic dystonia averaged across all tasks, within a core motor network, thresholded P < 0.05, family-wise error corrected for multiple comparisons
| Location | Laterality | Coordinates of peak activity |
T-value of peak regional cerebral blood flow difference | ||
|---|---|---|---|---|---|
| x | y | z | |||
| Frontal operculum | Right | 62 | 8 | 8 | 17.01 |
| Dorsal anterior cingulate cortex | Left | −6 | −2 | 48 | 17.01 |
| Thalamus | Left/Right | 0 | −8 | 0 | 15.53 |
| Dorsal midbrain | Right | 2 | −34 | −4 | 21.34 |
| Cerebellar hemisphere | Right | 8 | −56 | −28 | 12.66 |
| Cerebellar hemisphere | Left | −40 | −62 | −50 | 5.47 |
Coordinates refer to standard anatomic space using the MNI template.
Figure 3.
SPM(t) maps showing differences in regional cerebral blood flow between psychogenic dystonia group and control subjects, averaged across all three tasks. The maps show regions with either increased (A) or decreased (B) regional cerebral blood flow (P < 0.05, corrected), within the core motor network defined by regions that in control subjects showed activation in the contrast move versus rest (P < 0.05, corrected). Cf. Figure 2 in terms of the cortical and subcortical differences.
Table 4.
Cluster peaks of increased normalized regional cerebral blood flow for the contrast psychogenic dystonia versus control subjects averaged across all tasks, within a core motor network, thresholded P < 0.05, family-wise error corrected for multiple comparisons
| Location | Laterality | Coordinates of peak activity |
T-value of peak regional cerebral blood flow difference | ||
|---|---|---|---|---|---|
| x | y | z | |||
| Temporoparietal junction | Right | 60 | −34 | 20 | 12.14 |
| Globus pallidus/thalamus | Left | −14 | −10 | −8 | 19.24 |
| Dorsal thalamus | Left | −12 | −22 | 18 | 18.74 |
| Dorsal thalamus | Right | 16 | −8 | 20 | 15.80 |
| Tegmentum | Left/Right | 6 | −34 | −32 | 14.52 |
| Caudate | Right | 16 | −8 | 20 | 15.80 |
| Cerebellar hemisphere | Left | −26 | −58 | −28 | 14.92 |
| Cerebellar vermis | Right | 2 | −56 | −8 | 14.75 |
Coordinates refer to standard anatomical space using the MNI template.
Table 5.
Cluster peaks of increased normalized regional cerebral blood flow for the contrast control subjects versus psychogenic dystonia averaged across all tasks, within a core motor network, thresholded P < 0.05, family-wise error corrected for multiple comparisons
| Location | Laterality | Coordinates of peak activity | T-value of peak regional cerebral blood flow difference | ||
|---|---|---|---|---|---|
| x | y | z | |||
| Inferior frontal cortex | Right | 56 | 6 | 8 | 11.77 |
| Supplementary motor area | Left | −2 | −4 | 64 | 12.61 |
| Primary motor cortex | Left | −16 | −28 | 76 | 7.25 |
| Temporoparietal junction | Left | −68 | −32 | 24 | 10.91 |
| Dorsal anterior cingulate | Left | −2 | −6 | 48 | 9.94 |
| Inferior parietal lobule | Left | −50 | −26 | 18 | 8.37 |
| Thalamus/red nucleus/colliculi | Left | −6 | −32 | −2 | 17.89 |
| Cerebellar hemisphere | Left | −14 | −70 | −50 | 20.33 |
| Cerebellar hemisphere | Left | −46 | −50 | −50 | 18.77 |
Coordinates refer to standard anatomical space using the MNI template.
Figure 4.
SPM(t) maps showing differences in regional cerebral blood flow between organic dystonia and psychogenic dystonia groups, averaged across all three tasks. The statistical parametric maps show regions with relatively increased regional cerebral blood flow (P < 0.05, corrected) in either organic dystonia (A) or psychogenic dystonia (B), within the core motor network defined by regions that in control subjects showed activation in the contrast move versus rest (P < 0.05, corrected). Notably, organic dystonia shows predominantly enhanced cortical regional cerebral blood flow, whereas psychogenic dystonia shows predominantly enhanced subcortical regional cerebral blood flow when these groups are compared with each other.
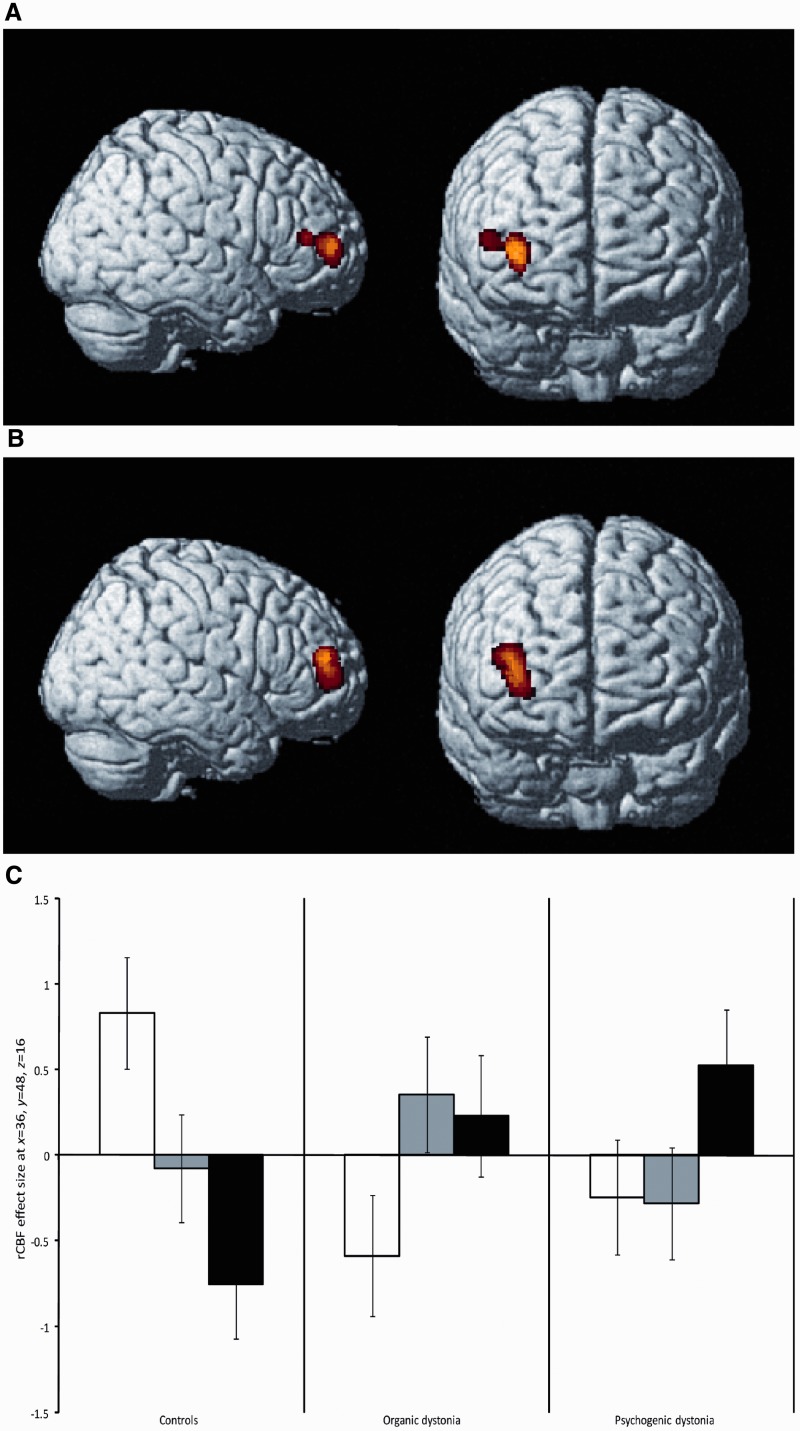
Group × task interaction: common activations of dorsolateral/polar prefrontal cortex during movement compared with rest in dystonia
Whilst there were no significant differences in regional cerebral blood flow between groups when comparing the move versus rest and move versus post contrasts in the whole-brain analysis, comparing the move versus rest contrasts in patients with organic dystonia versus healthy controls revealed significant increases in regional cerebral blood flow in the right dorsolateral/polar prefrontal cortex in the a priori region of interest analysis (T-score at peak increase in activity: 3.93; MNI coordinates in millimetres: x = 36; y = 48; z = 14) (Fig. 5A and C), and similar contrasts were seen in patients with psychogenic dystonia versus controls (T-score at peak increase in activity: 4.07; MNI coordinates in millimetres: x = 36; y = 48; z = 16) (Fig. 5B and C). An analysis of conjunction confirmed increases in regional cerebral blood flow in the right dorsolateral/polar prefrontal cortex in both organic and psychogenic dystonia.
Figure 5.
SPM(t) maps showing abnormally increased regional cerebral blood flow in dorsolateral/polar prefrontal cortex in both organic (A) and psychogenic dystonia (B) versus control subjects during movement of the right foot compared with rest (contrast move versus rest, illustrated P < 0.001 uncorrected). The differential activation in this region was significant (P < 0.05 corrected) when family-wise corrected within the a priori region of interest defined by Brodmann areas 10 and 46 (see ‘Materials and methods’ section). An analysis of conjunction confirmed increases in regional cerebral blood flow in the right dorsolateral/polar prefrontal cortex in both dystonia groups versus control subjects (T-score at peak increase in activity: 2.93; MNI coordinates in millimetres: x = 40; y = 50; z = 20). The bar chart (C) illustrates the regional profiles of task-specific regional cerebral blood flow (and 90% confidence intervals; at MNI coordinate x = 36; y = 48; z = 16). The regional cerebral blood flow values are mean-corrected within each group (white bars = rest; grey bars = post; black bars = move).
EMG analysis
There were significant main effects of Group [F(2,11) = 4.43; P < 0.05] and Task [F(2,22) = 18.2; P < 0.001]. As expected, there was a significant interaction between task and muscle [F(2,22) = 4.11; P < 0.05]. Post hoc two-sample two-tailed t-tests revealed that there was a trend towards the overall mean root mean square amplitude across all tasks being higher in organic dystonia than in controls (P = 0.06), and higher in organic dystonia than in psychogenic dystonia (P = 0.002, with Bonferroni correction), but not different between controls and psychogenic dystonia (P = 0.21). However, the arbitrary units of surface EMG require caution in interpreting between-subject effects. Post hoc two-tailed paired t-tests of task effects within group showed that there was a graded increase in mean root mean square amplitude between rest and post, and between post and move, respectively, across all groups in the case of gastrocnemius muscle, and post and move were similarly greater than rest for the tibialis anterior muscle (P < 0.05, with Bonferroni correction).
Discussion
In support of our principal hypothesis we have demonstrated that there are anatomically distinct patterns of abnormal regional cerebral blood flow in psychogenic and organic dystonia. To identify task-independent effects in each disease group compared with controls, we averaged across all three tasks and found that patients with organic dystonia showed increased regional cerebral blood flow, indicative of greater local neurometabolic rate, in primary motor, premotor and parietal cortices, together with reduced flow in the cerebellum. In contrast, patients with psychogenic dystonia were characterized by an opposite pattern of activation, showing increased regional cerebral blood flow in the cerebellum and basal ganglia, with reduced flow in the primary motor cortex. Not only did the two groups of patients differ from healthy controls, they also differed significantly from each other in these regions. We then sought task-dependent effects in the prefrontal cortex, identifying significant increases in movement-related activation in the right dorsolateral/polar prefrontal cortex in both organic and psychogenic dystonia (but not in healthy controls).
Previous functional neuroimaging studies on organic dystonia have yielded variable results, in part because of the heterogeneity of dystonias and study methods. Fluorodeoxyglucose-PET imaging studies have identified disease-specific patterns of abnormal metabolic brain network activity characterized by relative increases in areas including the supplementary motor area in patients with sporadic dystonia, and manifesting and non-manifesting DYT1 gene carriers (Eidelberg et al., 1998). A recent H215O PET study also showed task-related abnormal sensorimotor activation in primary dystonia (Carbon et al., 2010), consistent with our findings. In contrast, neuroimaging studies of other functional neurological disorders have predominantly implicated the prefrontal cortex (Nowak and Fink, 2009; Bell et al., 2010). However, whether this is a true marker of the psychogenic aetiology, or whether its role is secondary to being in a dysfunctional neurological state that is common to both psychogenic and organic neurological disorders remained unclear. Our study provides support for the latter interpretation with similar abnormal changes in the prefrontal areas being seen in both disease groups.
The identification of cortical–subcortical neuroimaging features that differentiate organic from psychogenic dystonia complements studies on plasticity in dystonia. Patients with organic dystonia have been reported to have abnormally increased cortical plasticity using a paired associative stimulation paradigm, whereas those with psychogenic dystonia do not (Quartarone et al., 2009). This difference implies that the latter group does not have an abnormal tendency to strengthen cortical sensory-motor associations. The hallmark of psychogenic dystonia may therefore be related to abnormalities in subcortical processing, not accessible through transcranial magnetic stimulation. In support of this, previous neuroimaging studies also point to subcortical correlates of psychogenic neurological disorders (Vuilleumier et al., 2001; Black et al., 2004; Voon et al., 2010a, b). The basal ganglia, cerebellum and thalamus mediate fronto-subcortical loops that relate to motor intention or attention, with further modulation possible by reciprocal connections with the amygdala and orbitofrontal cortex (Cummings, 1993), leading to a convergent theory invoking disruption of movement, motivation and attention at multiple levels of a distributed network (Black et al., 2004). Brown and Marsden (1998) proposed that the basal ganglia facilitate a form of focused motor attention subserving the automatic binding of cortical motor areas in a coherent sequence of motor activity and thought. Psychogenic dystonia may reflect dysfunction of these fronto-subcortical circuits, rather than a disorder of motor cortical plasticity and metabolism.
The prefrontal cortex is a common neurobiological substrate in the competing hypotheses of generation of functional neurological symptoms (Nowak and Fink, 2009; Bell et al., 2010), with diverse hypotheses of impaired generation of motor intention (Spence et al., 2000; Roelofs et al., 2002; Burgmer et al., 2006), motor conceptualization (Roelofs et al., 2006), disruption of motor execution (Vuilleumier et al., 2001; de Lange et al., 2008; Cojan et al., 2009), impaired self-monitoring (de Lange et al., 2007; Cojan et al., 2009), self-agency (Voon et al., 2010b), limbic processing (Marshall et al., 1997; Vuilleumier et al., 2001; Voon et al., 2010a) or ‘top-down’ regulation from higher-order frontal regions leading to impaired motor execution (Tiihonen et al., 1995; Kanaan et al., 2007; de Lange et al., 2010; Voon et al., 2011). Previous studies of functional neurological disorders or psychogenic movement disorders have reported increased prefrontal cortical activity or activation on the right (Tiihonen et al., 1995; Marshall et al., 1997; Kanaan et al., 2007; Cojan et al., 2009; de Lange et al., 2010) or left (Werring et al., 2004; Stone et al., 2007), although there are also reports of reductions on the left (Spence et al., 2000). This motivated our regions of interest analysis, and the present finding of abnormal prefrontal cortex activation during movement (when compared with rest) in patients with psychogenic dystonia is therefore not surprising.
What is the significance of this right prefrontal cortical activation? Firstly, it is important to note that our data show, for the first time, that the prefrontal abnormalities in a psychogenic movement disorder are matched by equivalent abnormalities in organic dystonia. This argues against the hypothesis that it is a marker of psychogenic disorders per se. Activation of the dorsolateral prefrontal cortex has been previously shown to occur in organic dystonia during performance of random joystick movements (Ceballos-Baumann et al., 1995), even without deficits in cognitive executive function or working memory (Jahanshahi et al., 2003). There are two interpretations of this; first, that prefrontal overactivity is epiphenomenal, merely reflecting the patients’ increased efforts to consciously control abnormal postures, or, second, that overactivity represents a form of ‘top-down’ compensatory control to suppress abnormal movements (Brooks, 1995). Our data do not discriminate between these possibilities. Distinguishing the network abnormalities that provoke dystonia from compensatory changes remains a challenge.
Secondly, the prefrontal cortical regions form part of an extended motor network (for a review, see Rowe and Siebner, 2012), with activation occurring during many motor tasks including attention, selection, planning, monitoring and inhibition of action, conscious motor intentions, goal-directed and novel movements. Unlike the strongly lateralized activations of primary motor cortex, right prefrontal cortical activations are observed even when the selected, attended or inhibited action is made by the right hand. Changes in these higher-order motor processes, and their prefrontal cortical substrates, have been linked to the aetiology of psychogenic paralysis (Nowak and Fink, 2009). An emerging concept is that organic dystonia also represents an abnormality in the interaction between attention, arousal and movement. For example, enhanced cortical plasticity within the motor system (Edwards et al., 2006) could produce a vulnerability to develop associations between involuntary movements and tasks. This may account for the tendency in organic dystonia for insidious spread over the years to involve other movements (Edwards and Rothwell, 2011). Our results suggest that there may be a similar derangement of the mechanisms of motor attention in psychogenic dystonia, as has been implicated in other psychogenic movement disorders (Voon et al., 2010a).
There are limitations to the present study. First, we are limited by the sample size. Nevertheless, our study compares favourably with the existing literature on psychogenic neurological disorders, in which the majority of studies have sample sizes ranging from one to eight, with the largest sample size being 16 (Voon et al., 2010a). The larger studies have tended to include clinically heterogeneous groups. In contrast, we aimed to match patients closely with the affected region and establish comparable task conditions in all groups. We cannot exclude the possibility of subtle phenotypic differences within each group, but this cannot account for our results, which reveal that the two patient groups show changes in opposite directions with respect to the controls. Our study also included both healthy controls and organic dystonia groups to allow for comparison not only with voluntary movement, but also with organic dystonia.
Second, a potential concern is that an organic neurological disease underlying the dystonia may have been missed and consequently the patients in the psychogenic group might have been misclassified. However, all patients had thorough neurological assessments and there was no change in diagnosis over a 10-year post-imaging period, making this unlikely.
Third, the task adopted was related to the patients’ functional deficit. It could therefore be argued that the imaging abnormalities noted in the patient groups might have been confounded by differences in motor performance, effort or sensory feedback. To address this, we attempted to create comparable tasks for all groups with EMG monitoring and included the post condition. The results show that while there is a significant graded increase in EMG signal between rest and post, and between post and move, there is little difference in imaging results between move versus post and post versus rest contrasts. This suggests that any increase in motor activity from a baseline provokes similar changes in neuroimaging.
Fourth, we, like others (Siebner et al., 2003; Carbon et al., 2010), adopted PET as our imaging method. Owing to its low spatial resolution, we cannot examine the finer details of subcortical change, although it would be of interest to differentiate changes within subregions of the basal ganglia. However, with functional MRI using the blood oxygen level–dependent contrast, the differences in blood oxygen level–dependent values between individuals limits the analyses to the examination of Task × Group interactions. Such a technique would have missed the main group effects that we found.
In conclusion, we demonstrate, for the first time, that there is a distinctive pathophysiological signature shown by functional neuroimaging that separates organic from psychogenic dystonia. We also show that the prefrontal cortex is implicated in organic and psychogenic dystonia. We suggest that an integrated approach to psychogenic movement disorders is required to understand the modulation of motor control by attention and emotion (Voon et al., 2010a; Edwards and Rothwell, 2011). Within such an overarching framework, comparisons should be made with organic disorders as well as healthy subjects. Functional neuroimaging in particular offers new insights into the pathophysiology of psychogenic movement disorders, which we propose is critical to improving the diagnosis, therapy and prognosis of this major group of disabling neurological disorders.
Funding
This work was supported by the Wellcome Trust (to R.S.J.F. and J.B.R., 054016 and 088324 and the Wellcome Trust Centre for Neuroimaging, Institute of Neurology, London, UK) and the Raymond Way Neuropsychiatry unit, London (to A.E.S.). A.R.M. was supported by the East of England Multi-Professional Deanery and Foundation School and thanks Addenbrooke’s Postgraduate Medical Centre of Cambridge University Hospitals NHS Foundation Trust, and Parkinson’s UK for their support. K.P.B. acknowledges support from Ipsen and from the Halley Stewart Trust through Dystonia Society (UK), the Wellcome Trust MRC strategic neurodegenerative disease initiative award (089698), the Dystonia Coalition and Parkinson’s UK (G-1009). J.B.R. was additionally supported by the National Institute for Health Research Cambridge Biomedical Research Centre and the James S. McDonnell Foundation.
Supplementary material
Supplementary material is available at Brain online.
Acknowledgements
We wish to thank Dr Valerie Voon for comments on the draft of this article.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Avanzino L, Martino D, van de Warrenburg BPC, Schneider SA, Abbruzzese G, Defazio G, et al. Cortical excitability is abnormal in patients with the “fixed dystonia” syndrome. Mov Disord. 2008;23:646–52. doi: 10.1002/mds.21801. [DOI] [PubMed] [Google Scholar]
- Bell V, Oakley DA, Halligan PW, Deeley Q. Dissociation in hysteria and hypnosis: evidence from cognitive neuroscience. J Neurol Neurosurg Psychiatry. 2010;82:332–9. doi: 10.1136/jnnp.2009.199158. [DOI] [PubMed] [Google Scholar]
- Black DN, Seritan AL, Taber KH, Hurley RA. Conversion hysteria: lessons from functional imaging. J Neuropsychiatry Clin Neurosci. 2004;16:245–51. doi: 10.1176/jnp.16.3.245. [DOI] [PubMed] [Google Scholar]
- Brooks DJ. The role of the basal ganglia in motor control: contributions from PET. J Neurol Sci. 1995;128:1–13. doi: 10.1016/0022-510x(94)00206-4. [DOI] [PubMed] [Google Scholar]
- Brown P, Marsden C. What do the basal ganglia do? Lancet. 1998;351:1801–4. doi: 10.1016/s0140-6736(97)11225-9. [DOI] [PubMed] [Google Scholar]
- Burgmer M, Konrad C, Jansen A, Kugel H, Sommer J, Heindel W, et al. Abnormal brain activation during movement observation in patients with conversion paralysis. Neuroimage. 2006;29:1336–43. doi: 10.1016/j.neuroimage.2005.08.033. [DOI] [PubMed] [Google Scholar]
- Calne DB, Lang AE. Secondary dystonia. Adv Neurol. 1988;50:9–33. [PubMed] [Google Scholar]
- Carbon M, Argyelan M, Habeck C, Ghilardi MF, Fitzpatrick T, Dhawan V, et al. Increased sensorimotor network activity in DYT1 dystonia: a functional imaging study. Brain. 2010;133(Pt 3):690–700. doi: 10.1093/brain/awq017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carson AJ, Ringbauer B, Stone J, McKenzie L, Warlow C, Sharpe M. Do medically unexplained symptoms matter? A prospective cohort study of 300 new referrals to neurology outpatient clinics. J Neurol Neurosurg Psychiatry. 2000;68:207–10. doi: 10.1136/jnnp.68.2.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ceballos-Baumann AO, Passingham RE, Warner T, Playford ED, Marsden CD, Brooks DJ. Overactive prefrontal and underactive motor cortical areas in idiopathic dystonia. Ann Neurol. 1995;37:363–72. doi: 10.1002/ana.410370313. [DOI] [PubMed] [Google Scholar]
- Cojan Y, Waber L, Carruzzo A, Vuilleumier P. Motor inhibition in hysterical conversion paralysis. Neuroimage. 2009;47:1026–37. doi: 10.1016/j.neuroimage.2009.05.023. [DOI] [PubMed] [Google Scholar]
- Cummings JL. Frontal-subcortical circuits and human behavior. Arch Neurol. 1993;50:873–80. doi: 10.1001/archneur.1993.00540080076020. [DOI] [PubMed] [Google Scholar]
- de Lange FP, Roelofs K, Toni I. Increased self-monitoring during imagined movements in conversion paralysis. Neuropsychologia. 2007;45:2051–8. doi: 10.1016/j.neuropsychologia.2007.02.002. [DOI] [PubMed] [Google Scholar]
- de Lange FP, Roelofs K, Toni I. Motor imagery: a window into the mechanisms and alterations of the motor system. Cortex. 2008;44:494–506. doi: 10.1016/j.cortex.2007.09.002. [DOI] [PubMed] [Google Scholar]
- de Lange FP, Toni I, Roelofs K. Altered connectivity between prefrontal and sensorimotor cortex in conversion paralysis. Neuropsychologia. 2010;48:1782–8. doi: 10.1016/j.neuropsychologia.2010.02.029. [DOI] [PubMed] [Google Scholar]
- Edwards MJ, Huang Y, Mir P, Rothwell JC, Bhatia KP. Abnormalities in motor cortical plasticity differentiate manifesting and nonmanifesting DYT1 carriers. Mov Disord. 2006;21:2181–6. doi: 10.1002/mds.21160. [DOI] [PubMed] [Google Scholar]
- Edwards MJ, Rothwell JC. Losing focus: how paying attention can be bad for movement. Mov Disord. 2011;26:1969–70. doi: 10.1002/mds.23920. [DOI] [PubMed] [Google Scholar]
- Eidelberg D, Moeller JR, Antonini A, Kazumata K, Nakamura T, Dhawan V, et al. Functional brain networks in DYT1 dystonia. Ann Neurol. 1998;44:303–12. doi: 10.1002/ana.410440304. [DOI] [PubMed] [Google Scholar]
- Espay AJ, Morgante F, Purzner J, Gunraj CA, Lang AE, Chen R. Cortical and spinal abnormalities in psychogenic dystonia. Ann Neurol. 2006;59:825–34. doi: 10.1002/ana.20837. [DOI] [PubMed] [Google Scholar]
- Fahn S, Williams DT. Psychogenic dystonia. Adv Neurol. 1988;50:431–55. [PubMed] [Google Scholar]
- Friston KJ. Statistical parametric mapping: the analysis of functional brain images. Amsterdam; London: Elsevier/Academic Press; 2007. [Google Scholar]
- Friston KJ, Ashburner J, Frith CD, Poline J-P, Heather JD, Frackowiak RSJ. Spatial registration and normalization of images. Hum Brain Mapp. 1995;3:165–89. [Google Scholar]
- Friston KJ, Frith CD, Liddle PF, Dolan RJ, Lammertsma AA, Frackowiak RS. The relationship between global and local changes in PET scans. J Cereb Blood Flow Metab. 1990;10:458–66. doi: 10.1038/jcbfm.1990.88. [DOI] [PubMed] [Google Scholar]
- Friston KJ, Holmes AP, Price CJ, Büchel C, Worsley KJ. Multisubject fMRI studies and conjunction analyses. Neuroimage. 1999;10:385–96. doi: 10.1006/nimg.1999.0484. [DOI] [PubMed] [Google Scholar]
- Friston KJ, Holmes AP, Worsley KJ, Poline J-J, Frith CD, Frackowiak RSJ. Statistical parametric maps in functional imaging: a general linear approach. Hum Brain Mapp. 1994;2:189–210. [Google Scholar]
- Friston KJ, Penny WD, Glaser DE. Conjunction revisited. Neuroimage. 2005;25:661–7. doi: 10.1016/j.neuroimage.2005.01.013. [DOI] [PubMed] [Google Scholar]
- Ghaffar O, Staines WR, Feinstein A. Unexplained neurologic symptoms: an fMRI study of sensory conversion disorder. Neurology. 2006;67:2036–8. doi: 10.1212/01.wnl.0000247275.68402.fc. [DOI] [PubMed] [Google Scholar]
- Gupta A, Lang AE. Psychogenic movement disorders. Curr Opin Neurol. 2009;22:430–6. doi: 10.1097/WCO.0b013e32832dc169. [DOI] [PubMed] [Google Scholar]
- Hallett M. Psychogenic movement disorders: a crisis for neurology. Curr Neurol Neurosci Rep. 2006;6:269–71. doi: 10.1007/s11910-006-0015-x. [DOI] [PubMed] [Google Scholar]
- Hallett M. Physiology of psychogenic movement disorders. J Clin Neurosci. 2010;17:959–65. doi: 10.1016/j.jocn.2009.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinson VK, Haren WB. Psychogenic movement disorders. Lancet Neurol. 2006;5:695–700. doi: 10.1016/S1474-4422(06)70523-3. [DOI] [PubMed] [Google Scholar]
- Hutchinson M, Nakamura T, Moeller JR, Antonini A, Belakhlef A, Dhawan V, et al. The metabolic topography of essential blepharospasm: a focal dystonia with general implications. Neurology. 2000;55:673–7. doi: 10.1212/wnl.55.5.673. [DOI] [PubMed] [Google Scholar]
- Ibrahim NM, Martino D, van de Warrenburg BP, Quinn NP, Bhatia KP, Brown RJ, et al. The prognosis of fixed dystonia: a follow-up study. Parkinsonism Relat Disord. 2009;15:592–7. doi: 10.1016/j.parkreldis.2009.02.010. [DOI] [PubMed] [Google Scholar]
- Jahanshahi M, Rowe J, Fuller R. Cognitive executive function in dystonia. Mov Disord. 2003;18:1470–81. doi: 10.1002/mds.10595. [DOI] [PubMed] [Google Scholar]
- Kanaan RA, Craig TK, Wessely SC, David AS. Imaging repressed memories in motor conversion disorder. Psychosom Med. 2007;69:202–5. doi: 10.1097/PSY.0b013e31802e4297. [DOI] [PubMed] [Google Scholar]
- Lang AE. Psychogenic dystonia: a review of 18 cases. Can J Neurol Sci. 1995;22:136–43. doi: 10.1017/s031716710004021x. [DOI] [PubMed] [Google Scholar]
- Lang AE, Voon V. Psychogenic movement disorders: past developments, current status, and future directions. Mov Disord. 2011;26:1175–86. doi: 10.1002/mds.23571. [DOI] [PubMed] [Google Scholar]
- Mailis-Gagnon A, Giannoylis I, Downar J, Kwan CL, Mikulis DJ, Crawley AP, et al. Altered central somatosensory processing in chronic pain patients with “hysterical” anesthesia. Neurology. 2003;60:1501–7. doi: 10.1212/wnl.60.9.1501. [DOI] [PubMed] [Google Scholar]
- Maldjian JA, Laurienti PJ, Kraft RA, Burdette JH. An automated method for neuroanatomic and cytoarchitectonic atlas-based interrogation of fMRI data sets. Neuroimage. 2003;19:1233–9. doi: 10.1016/s1053-8119(03)00169-1. [DOI] [PubMed] [Google Scholar]
- Marshall JC, Halligan PW, Fink GR, Wade DT, Frackowiak RS. The functional anatomy of a hysterical paralysis. Cognition. 1997;64:B1–8. doi: 10.1016/s0010-0277(97)00020-6. [DOI] [PubMed] [Google Scholar]
- McKeon A, Matsumoto JY, Bower JH, Ahlskog JE. The spectrum of disorders presenting as adult-onset focal lower extremity dystonia. Parkinsonism Relat Disord. 2008;14:613–9. doi: 10.1016/j.parkreldis.2008.01.012. [DOI] [PubMed] [Google Scholar]
- Nowak DA, Fink GR. Psychogenic movement disorders: aetiology, phenomenology, neuroanatomical correlates and therapeutic approaches. Neuroimage. 2009;47:1015–25. doi: 10.1016/j.neuroimage.2009.04.082. [DOI] [PubMed] [Google Scholar]
- Quartarone A, Rizzo V, Terranova C, Morgante F, Schneider S, Ibrahim N, et al. Abnormal sensorimotor plasticity in organic but not in psychogenic dystonia. Brain. 2009;132:2871–7. doi: 10.1093/brain/awp213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roelofs K, de Bruijn ERA, Van Galen GP. Hyperactive action monitoring during motor-initiation in conversion paralysis: an event-related potential study. Biol Psychol. 2006;71:316–25. doi: 10.1016/j.biopsycho.2005.07.002. [DOI] [PubMed] [Google Scholar]
- Roelofs K, van Galen GP, Keijsers GP, Hoogduin CA. Motor initiation and execution in patients with conversion paralysis. Acta Psychol (Amst) 2002;110:21–34. doi: 10.1016/s0001-6918(01)00068-3. [DOI] [PubMed] [Google Scholar]
- Rowe JB. Conversion disorder: understanding the pathogenic links between emotion and motor systems in the brain. Brain. 2010;133:1295–7. doi: 10.1093/brain/awq096. [DOI] [PubMed] [Google Scholar]
- Rowe JB, Siebner HR. The motor system and its disorders. Neuroimage. 2012;61:464–77. doi: 10.1016/j.neuroimage.2011.12.042. [DOI] [PubMed] [Google Scholar]
- Schrag A, Trimble M, Quinn N, Bhatia K. The syndrome of fixed dystonia: an evaluation of 103 patients. Brain. 2004;127:2360–72. doi: 10.1093/brain/awh262. [DOI] [PubMed] [Google Scholar]
- Siebner HR, Filipovic SR, Rowe JB, Cordivari C, Gerschlager W, Rothwell JC, et al. Patients with focal arm dystonia have increased sensitivity to slow-frequency repetitive TMS of the dorsal premotor cortex. Brain. 2003;126:2710–25. doi: 10.1093/brain/awg282. [DOI] [PubMed] [Google Scholar]
- Spence SA, Crimlisk HL, Cope H, Ron MA, Grasby PM. Discrete neurophysiological correlates in prefrontal cortex during hysterical and feigned disorder of movement. Lancet. 2000;355:1243–4. doi: 10.1016/S0140-6736(00)02096-1. [DOI] [PubMed] [Google Scholar]
- Stone J, Carson A, Duncan R, Coleman R, Roberts R, Warlow C, et al. Symptoms ‘unexplained by organic disease’ in 1144 new neurology out-patients: how often does the diagnosis change at follow-up? Brain. 2009;132:2878–88. doi: 10.1093/brain/awp220. [DOI] [PubMed] [Google Scholar]
- Stone J, Zeman A, Simonotto E, Meyer M, Azuma R, Flett S, et al. FMRI in patients with motor conversion symptoms and controls with simulated weakness. Psychosom Med. 2007;69:961–9. doi: 10.1097/PSY.0b013e31815b6c14. [DOI] [PubMed] [Google Scholar]
- Talairach J, Tournoux P. Co-planar stereotaxic atlas of the human brain: 3-dimensional proportional system: an approach to medical cerebral imaging. Stuttgart; New York: Thieme; Thieme Medical; 1988. [Google Scholar]
- Tiihonen J, Kuikka J, Viinamaki H, Lehtonen J, Partanen J. Altered cerebral blood flow during hysterical paresthesia. Biol Psychiatry. 1995;37:134–5. doi: 10.1016/0006-3223(94)00230-Z. [DOI] [PubMed] [Google Scholar]
- Voon V, Brezing C, Gallea C, Ameli R, Roelofs K, LaFrance WC, Jr, et al. Emotional stimuli and motor conversion disorder. Brain. 2010a;133:1526–36. doi: 10.1093/brain/awq054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voon V, Brezing C, Gallea C, Hallett M. Aberrant supplementary motor complex and limbic activity during motor preparation in motor conversion disorder. Mov Disord. 2011;26:2396–403. doi: 10.1002/mds.23890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voon V, Gallea C, Hattori N, Bruno M, Ekanayake V, Hallett M. The involuntary nature of conversion disorder. Neurology. 2010b;74:223–8. doi: 10.1212/WNL.0b013e3181ca00e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vuilleumier P, Chicherio C, Assal F, Schwartz S, Slosman D, Landis T. Functional neuroanatomical correlates of hysterical sensorimotor loss. Brain. 2001;124:1077–90. doi: 10.1093/brain/124.6.1077. [DOI] [PubMed] [Google Scholar]
- Werring DJ, Weston L, Bullmore ET, Plant GT, Ron MA. Functional magnetic resonance imaging of the cerebral response to visual stimulation in medically unexplained visual loss. Psychol Med. 2004;34:583–9. doi: 10.1017/S0033291703008985. [DOI] [PubMed] [Google Scholar]
- Williams DT, Ford B, Fahn S. Phenomenology and psychopathology related to psychogenic movement disorders. Adv Neurol. 1995;65:231–57. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.