Abstract
Of the chlamydia species that can cause infections in humans, C. trachomatis is responsible for lower urinary tract diseases in men and women. C. trachomatis infections are prevalent worldwide, but current research is focused on females, with the burden of disease and infertility sequelae considered to be a predominantly female problem. However, a role for this pathogen in the development of male urethritis, epididymitis, and orchitis is widely accepted. Also, it can cause complications such as chronic prostatitis and infertility. This review summarizes C. trachomatis infection in the male genitourinary tract, including urethritis, epididymitis, orchitis, and its complications, and addresses the microbiology, epidemiology, screening, clinical manifestations, diagnosis, and treatment.
Keywords: Chlamydia, Chronic prostatitis, Epididymitis, Infertility orchitis, Urethritis
MICROBIOLOGY
Chlamydiae are small gram-negative obligate intracellular microorganisms that preferentially infect squamocolumnar epithelial cells. Chlamydia species which can cause infections in humans are C. pneumoniae, C. psittaci and C. trachomatis. Of the three species, C. trachomatis is responsible for sexually transmitted diseases (STDs) in men and women. Identified in 1907, C. trachomatis was the first chlamydial agent discovered in humans [1]. The life cycle of C. trachomatis consists of an extracellular form (the elementary body) and the intracellular form (the reticulate body). The elementary body attaches to and penetrates columnar epithelial cells, where it transforms into the reticulate body, the active reproductive form of the organism. The reticulate body forms large inclusions within cells and then begins to reorganize into small elementary bodies. C. trachomatis can be differentiated into 18 serovars (serologically variant strains) based on monoclonal antibody-based typing assays. Serovars A, B, Ba, and C are associated with trachoma (a serious eye disease that can lead to blindness), serovars D-K are associated with genital tract infections, and L1-L3 are associated with lymphogranuloma venereum.
The pathophysiologic mechanisms of chlamydiae are poorly understood. The initial response to infected epithelial cells is a neutrophilic infiltration followed by lymphocytes, macrophages, plasma cells, and eosinophilic invasion. The release of cytokines and interferons by the infected epithelial cell initializes this inflammatory cascade. Infection with chlamydial organisms invokes a humoral cell response, resulting in secretory immunoglobulin A (IgA) and circulatory IgM and IgG antibodies and a cellular immune response.
EPIDEMIOLOGY
Chlamydia is the most common bacterial sexually transmitted infection in the world, causing an estimated 89 million new cases of infection each year [2]. Ethnic group or socioeconomic deprivation, introducing a screening program that is less available and accessible, and less acceptable to people from vulnerable and disadvantaged groups, could create or widen existing inequalities in chlamydia prevalence. According to the Centers for Disease Control and Prevention (CDC) 2009, the last 5 years have seen an increasing rate of infection (43.5%) and it is more common in women than in men (3:1) in United States (US) [3]. In United Kingdom in 2004, 104,155 cases of chlamydia were diagnosed in genitourinary medicine clinics [4]. The number of diagnosed infections has been increasing steadily since 1995, partly owing to increased numbers of people being tested: nearly 700,000 genital infections and sexually transmitted infections were diagnosed in genitourinary clinics in 2003 compared with 442,000 in 1995. The National Chlamydia Screening Programme reported that the prevalence in 16 to 24-year-olds was 6.2% in women and 5.3% in men in 2007 [4]. The prevalence in young men was the same as in young women. The examination of risk factors for chlamydia in the prevalence and case-control studies did not find any factors, other than young age. The number of new partners in the past 12 months was the strongest predictor of infection [4].
Population based studies in Europe and the US suggest that the prevalence of chlamydia in men and women aged 15 to 24 years is 2-6% [5-8]. The peak age group for infection is 16 to 19 years in women and 20 to 24 years in men [9].
SCREENING
Asymptomatic chlamydial infection is common among both men and women, and detection often relies on screening. Routine laboratory screening for common STDs is indicated for sexually active adolescents. The CDC and the US Preventive Services Task Force each recommend annual chlamydial screening for all sexually active women ≤25 years of age and also for older women with risk factors (e.g., those who have a new sex partner or multiple sex partners). The benefits of screening could be demonstrated in areas where the prevalence of infection and rates of pelvic inflammatory diseases are decreasing since the screening programs began [10-12]. Evidence is insufficient to recommend routine screening for C. trachomatis in sexually active young men based on feasibility, efficacy, and cost-effectiveness. However, screening of sexually active young men should be considered in clinical settings associated with high prevalence of chlamydia (e.g., adolescent clinics, correctional facilities, and STD clinics). For the persons in correctional facilities, universal screening of adolescent females for chlamydia should be conducted at intake in juvenile detention or jail facilities. Universal screening of adult females should be conducted at intake among adult females up to 35 years of age (or on the basis of local institutional prevalence data) [3].
CLINICAL MANIFESTATIONS AND COMPLICATIONS OF CHLAMYDIAL INFECTION IN MALE GENITOURINARY TRACT
C. trachomatis is a bacterium whose sexually transmitted strains D-K cause genital tract infections in women (cervicitis and urethritis) and men (urethritis, epididymitis, orchitis and prostatitis). However, chlamydia is known as a 'silent' pathogen because about three-quarters of infected women and about half of infected men have no symptoms [13]. Symptoms of chlamydia, if present, include discharge of mucopurulent or purulent material, dysuria, urethral pruritus, urinary frequency or urgency, and lower abdominal or pelvic pain and show up about 1 to 3 weeks after being infected. One of the most common symptoms for in cases of chlamydia in men is a painful urination. In the worst cases chlamydia infection can, without treatment, lead on to other problems such as epididymitis or orchitis if the infection has made it to the testicles. This is particularly worrisome because it can occasionally cause a man to become sterile.
Other C. trachomatis strains, L1, L2 and L3 cause lymphogranuloma venereum. This tropical sexually transmitted infection is currently responsible for outbreaks of ulcerative proctitis mainly affecting homosexual men (many with human immunodeficiency virus infection) in various European countries and the US [14-16].
Potential problem without treatment of the chlamydia infection is chronic complications. Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) is divided into two categories, inflammatory (which corresponds to the former chronic nonbacterial prostatitis), and non-inflammatory (which corresponds to the former prostatodynia) [17]. The problem is that although in semen and expressed prostatic secretions there is evidence of inflammation, no pathogens are usually found in samples analyzed when routine culture methods are used. The clinical symptoms of patients with CPPS IIIA and IIIB are similar, perineal pain, often radiating to the genital area, urinary symptoms, ejaculatory disturbance, and are of chronic nature. The cause of CP/CPPS has not yet been established and there is a lot of controversy regarding its etiology [18]. However, there is some substantial empirical support for a potential role of genitourinary tract infections in CP/CPPS as the etiology of this disease. For many years attempts have been made to prove the role of certain microorganisms in the pathogenesis of CP/CPPS. Attention has focused on C. trachomatis, the most frequent cause of non-gonococcal urethritis in sexually active men. Even the evidence is conflicting, C. trachomatis has been suggested as an etiologic agent in chronic prostatitis (examining urine, prostatic fluid, semen or prostate tissue). Mardh et al. [19] found that one third of men with chronic prostatitis had antibodies to C. trachomatis compared with 3% of controls. Shortliffe et al. [20] found that 20% of patients with nonbacterial prostatitis had antichlamydial antibody titers in the prostatic fluid. Bruce et al. [21] found that 56% of patients with 'subacute or chronic prostatitis' were infected with C. trachomatis. In a follow-up study, they found that 6 of 55 men with abacterial prostatitis, including 31 believed to have chlamydial prostatitis, met strict criteria for positive diagnosis for chlamydial prostatitis based on identification of the organisms by culturing or immunofluorescence [22]. Chlamydia has also been isolated in prostate tissue specimens [23-25]. However, further evaluation of the chlamydial etiology of prostatitis is required to make any definitive statement on the association between isolation of this organism and prostatitis.
Sequelae of C. trachomatis infection in men also may include male factor infertility but why this occurs remains uncertain. There have been a number of studies on the relationship between C. trachomatis infection and sperm quality, with conflicting results. Recent studies have generally found that men with a current infection of C. trachomatis have poorer quality ejaculates compared than men who do not [26-28]. It has been observed that persistent infection can result in the scarring of ejaculatory ducts or loss of stereocilia [29]. In addition to any changes in semen quality, there is growing evidence to suggest that exposure to C. trachomatis can affect sperm function [30,31]. In vitro experiments have shown that C. trachomatis triggers tyrosine phosphorylation of sperm proteins [32], induces premature sperm death [33] and stimulates an apoptosis-like response in sperm [34,35], leading to increased levels of sperm DNA fragmentation [35,36].
DIAGNOSIS
Culture, nucleic acid hybridization tests, and nucleic acid amplification tests (NAATs) are available for the detection of C. trachomatis. Culture and hybridization tests require urethral swab specimens, whereas NAATs can be performed on urine specimens. The sensitivity and specificity of the NAATs are clearly the highest of any of the test platforms for the diagnosis of chlamydial infections. Nonculture tests such as enzyme immunoassays (EIA) and DNA probe assays are inferior to NAATs with respect to performance. According to the Expert Consultation Meeting Summary Report 2009, NAATs are recommended for detection of reproductive tract infections caused by C. trachomatis in men and women with and without symptoms [37]. Optimal specimen types for NAATs are first catch urine from men and vaginal swabs from women. There is little need for urethral swab specimens and in some studies these samples are less sensitive than urine; urethral swab specimens and male urine were equivalent in specificity. For female screening, vaginal swab specimens are the preferred specimen type. Female urine, while acceptable, may have reduced performance when compared to genital swab samples. NAATs are also recommended for the detection of rectal and oropharyngeal infections caused by C. trachomatis.
Point-of-care testing methods can provide results within hours after the tests are carried out, which could allow infected patients to be treated immediately, as well as allowing the immediate identification of recent sexual partners who should also be tested. The Chlamydia Rapid Test is a point-of-care test that has reported improved accuracy. However, according to the recent systematic review of the clinical effectiveness and cost-effectiveness of rapid point-of-care tests for the detection of genital chlamydia infection, NAATs was found to be less costly and more effective [38]. There are currently no point-of-care assays on the market that are suitable for routine use, although some may be of use in high risk populations where immediate treatment is the overriding concern due to poor follow up. The group felt that development of improved point-of-care tests desirable.
TREATMENT
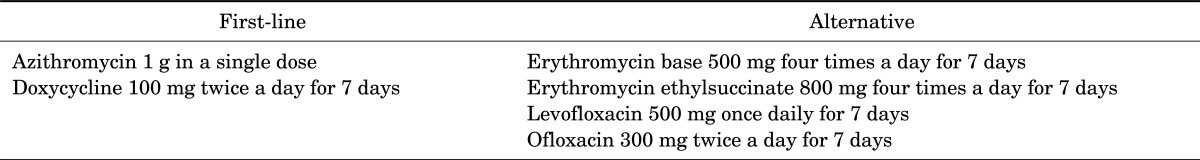
The approach to the management of uncomplicated genital chlamydial infection in adults includes 1) treatment of patients (to reduce complications and prevent transmission to sex partners), 2) treatment of sex partners (to prevent reinfection of the index patient and infection of other partners), 3) risk-reduction counseling, and 4) repeat chlamydial testing in women a few months after treatment (to identify recurrent/persistent infections) [39]. Uncomplicated lower genital tract chlamydia infections can be cured by a single dose or short course of antibiotics. Clinical trials continue to demonstrate equivalent efficacy and tolerability of azithromycin and doxycycline regimens, and both remain recommended as first-line therapy in nonpregnant individuals. Azithromycin 1 g and doxycycline 100 mg bd for 7 days have been shown to be >95% effective in the treatment of uncomplicated lower genital tract C. trachomatis infection (Table 1). For those with upper genital tract disease i.e., pelvic inflammatory disease, a prolonged course of treatment for up to 14 days is recommended [40].
TABLE 1.
Treatment of uncomplicated lower genital tract Chlamydia trachomatis infection
More data and clinical experience are available to support the efficacy, safety, and tolerability of azithromycin in pregnant women. Evidence is building that expedited partner therapy, with provision of treatment or a prescription, may be just as effective as or more effective than standard partner referral in ensuring partner treatment and preventing chlamydia recurrence in women. Although there are more studies needed and barriers to be addressed before its widespread use, expedited partner therapy will be recommended as an option for partner management.
Test of cure is not routinely recommended if standard treatment has been given, there is confirmation that the patient has adhered to therapy, and there is no risk of reinfection. However, if these criteria cannot be met or if the patient is pregnant a test of cure is advised. This should be taken using the same technique as was used for the initial testing. Ideally, a minimum of 3 to 5 weeks post-treatment is required as NAATs will demonstrate residual DNA/RNA even after successful treatment of the organism.
CONCLUSIONS
A role for C. trachomatis in the development of male urologic diseases such as urethritis, epididymitis, and orchitis is widely accepted. Also, C. trachomatis can cause chronic prostatitis and infertility. Ascending chlamydial infections have been thought to be an infective cause of prostatitis. Unfortunately, the definitive association between C. trachomatis and prostatitis is limited by various factors. Sequelae of C. trachomatis infection may include male factor infertility but why this remains uncertain. Optimal specimen types for NAATs are first catch urine from men and vaginal swabs from women. Clinical trials continue to demonstrate equivalent efficacy and tolerability of azithromycin and doxycycline regimens, and both remain recommended as first-line therapy. Futher evaluation of chlamydial etiology of prostatitis and infertility is reguired to make definitive statement on the association between isolation of this organism and the diseases.
Footnotes
The authors have nothing to disclose.
References
- 1.Halberstadter L, von Prowazek S. Uber Zelleinschlusse parasitarer Natur beim Trachom. Arb Gesundh (Berlin) 1907;26:44–47. [Google Scholar]
- 2.World Health Organization. Global prevalence and incidence of selected curable sexually transmitted infections. Overview and estimates. Geneva: World Health Organization; 2001. [Google Scholar]
- 3.Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2009. Atlanta: Centers for Disease Control and Prevention; 2010. [Google Scholar]
- 4.Low N, McCarthy A, Macleod J, Salisbury C, Campbell R, Roberts TE, et al. Epidemiological, social, diagnostic and economic evaluation of population screening for genital chlamydial infection. Health Technol Assess. 2007;11:iii–iv. ix–xii, 1–165. doi: 10.3310/hta11080. [DOI] [PubMed] [Google Scholar]
- 5.Miller WC, Ford CA, Morris M, Handcock MS, Schmitz JL, Hobbs MM, et al. Prevalence of chlamydial and gonococcal infections among young adults in the United States. JAMA. 2004;291:2229–2236. doi: 10.1001/jama.291.18.2229. [DOI] [PubMed] [Google Scholar]
- 6.van Bergen J, Gotz HM, Richardus JH, Hoebe CJ, Broer J, Coenen AJ, et al. Prevalence of urogenital Chlamydia trachomatis increases significantly with level of urbanisation and suggests targeted screening approaches: results from the first national population based study in the Netherlands. Sex Transm Infect. 2005;81:17–23. doi: 10.1136/sti.2004.010173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fenton KA, Korovessis C, Johnson AM, McCadden A, McManus S, Wellings K, et al. Sexual behaviour in Britain: reported sexually transmitted infections and prevalent genital Chlamydia trachomatis infection. Lancet. 2001;358:1851–1854. doi: 10.1016/S0140-6736(01)06886-6. [DOI] [PubMed] [Google Scholar]
- 8.Andersen B, Olesen F, Moller JK, Ostergaard L. Population-based strategies for outreach screening of urogenital Chlamydia trachomatis infections: a randomized, controlled trial. J Infect Dis. 2002;185:252–258. doi: 10.1086/338268. [DOI] [PubMed] [Google Scholar]
- 9.The UK Collaborative Group for HIV and STI Surveillance. Mapping the issues. HIV and other sexually transmitted infections in the United Kingdom. London: Health Protection Agency Centre for Infections; 2005. [Google Scholar]
- 10.Scholes D, Stergachis A, Heidrich FE, Andrilla H, Holmes KK, Stamm WE. Prevention of pelvic inflammatory disease by screening for cervical chlamydial infection. N Engl J Med. 1996;334:1362–1366. doi: 10.1056/NEJM199605233342103. [DOI] [PubMed] [Google Scholar]
- 11.Kamwendo F, Forslin L, Bodin L, Danielsson D. Decreasing incidences of gonorrhea- and chlamydia-associated acute pelvic inflammatory disease. A 25-year study from an urban area of central Sweden. Sex Transm Dis. 1996;23:384–391. doi: 10.1097/00007435-199609000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Mertz KJ, Levine WC, Mosure DJ, Berman SM, Dorian KJ. Trends in the prevalence of chlamydial infections. The impact of community-wide testing. Sex Transm Dis. 1997;24:169–175. doi: 10.1097/00007435-199703000-00009. [DOI] [PubMed] [Google Scholar]
- 13.van de Laar MJ, Morre SA. Chlamydia: a major challenge for public health. Euro Surveill. 2007;12:E1–E2. doi: 10.2807/esm.12.10.00735-en. [DOI] [PubMed] [Google Scholar]
- 14.Nieuwenhuis RF, Ossewaarde JM, Gotz HM, Dees J, Thio HB, Thomeer MG, et al. Resurgence of lymphogranuloma venereum in Western Europe: an outbreak of Chlamydia trachomatis serovar l2 proctitis in The Netherlands among men who have sex with men. Clin Infect Dis. 2004;39:996–1003. doi: 10.1086/423966. [DOI] [PubMed] [Google Scholar]
- 15.Nieuwenhuis RF, Ossewaarde JM, van der Meijden WI, Neumann HA. Unusual presentation of early lymphogranuloma venereum in an HIV-1 infected patient: effective treatment with 1 g azithromycin. Sex Transm Infect. 2003;79:453–455. doi: 10.1136/sti.79.6.453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blank S, Schillinger JA, Harbatkin D. Lymphogranuloma venereum in the industrialised world. Lancet. 2005;365:1607–1608. doi: 10.1016/S0140-6736(05)66490-2. [DOI] [PubMed] [Google Scholar]
- 17.Collins MM, Stafford RS, O'Leary MP, Barry MJ. How common is prostatitis? A national survey of physician visits. J Urol. 1998;159:1224–1228. [PubMed] [Google Scholar]
- 18.Motrich RD, Maccioni M, Molina R, Tissera A, Olmedo J, Riera CM, et al. Presence of INFgamma-secreting lymphocytes specific to prostate antigens in a group of chronic prostatitis patients. Clin Immunol. 2005;116:149–157. doi: 10.1016/j.clim.2005.03.011. [DOI] [PubMed] [Google Scholar]
- 19.Mardh P, Colleen S, Holmquist B. Chlamydia in chronic prostatitis. Br Med J. 1972;4:361. doi: 10.1136/bmj.4.5836.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shortliffe LM, Sellers RG, Schachter J. The characterization of nonbacterial prostatitis: search for an etiology. J Urol. 1992;148:1461–1466. doi: 10.1016/s0022-5347(17)36940-9. [DOI] [PubMed] [Google Scholar]
- 21.Bruce AW, Chadwick P, Willett WS, O'Shaughnessy M. The role of chlamydiae in genitourinary disease. J Urol. 1981;126:625–629. doi: 10.1016/s0022-5347(17)54660-1. [DOI] [PubMed] [Google Scholar]
- 22.Bruce AW, Reid G. Prostatitis associated with Chlamydia trachomatis in 6 patients. J Urol. 1989;142:1006–1007. doi: 10.1016/s0022-5347(17)38970-x. [DOI] [PubMed] [Google Scholar]
- 23.Poletti F, Medici MC, Alinovi A, Menozzi MG, Sacchini P, Stagni G, et al. Isolation of Chlamydia trachomatis from the prostatic cells in patients affected by nonacute abacterial prostatitis. J Urol. 1985;134:691–693. doi: 10.1016/s0022-5347(17)47387-3. [DOI] [PubMed] [Google Scholar]
- 24.Abdelatif OM, Chandler FW, McGuire BS., Jr Chlamydia trachomatis in chronic abacterial prostatitis: demonstration by colorimetric in situ hybridization. Hum Pathol. 1991;22:41–44. doi: 10.1016/0046-8177(91)90059-x. [DOI] [PubMed] [Google Scholar]
- 25.Shurbaji MS, Gupta PK, Myers J. Immunohistochemical demonstration of Chlamydial antigens in association with prostatitis. Mod Pathol. 1988;1:348–351. [PubMed] [Google Scholar]
- 26.Hosseinzadeh S, Eley A, Pacey AA. Semen quality of men with asymptomatic chlamydial infection. J Androl. 2004;25:104–109. doi: 10.1002/j.1939-4640.2004.tb02764.x. [DOI] [PubMed] [Google Scholar]
- 27.Bezold G, Politch JA, Kiviat NB, Kuypers JM, Wolff H, Anderson DJ. Prevalence of sexually transmissible pathogens in semen from asymptomatic male infertility patients with and without leukocytospermia. Fertil Steril. 2007;87:1087–1097. doi: 10.1016/j.fertnstert.2006.08.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Al-Mously N, Cross NA, Eley A, Pacey AA. Real-time polymerase chain reaction shows that density centrifugation does not always remove Chlamydia trachomatis from human semen. Fertil Steril. 2009;92:1606–1615. doi: 10.1016/j.fertnstert.2008.08.128. [DOI] [PubMed] [Google Scholar]
- 29.Gonzalez-Jimenez MA, Villanueva-Diaz CA. Epididymal stereocilia in semen of infertile men: evidence of chronic epididymitis? Andrologia. 2006;38:26–30. doi: 10.1111/j.1439-0272.2006.00708.x. [DOI] [PubMed] [Google Scholar]
- 30.Pacey AA, Eley A. Chlamydia trachomatis and male fertility. Hum Fertil (Camb) 2004;7:271–276. doi: 10.1080/14647270400016373. [DOI] [PubMed] [Google Scholar]
- 31.Eley A, Pacey AA, Galdiero M, Galdiero M, Galdiero F. Can Chlamydia trachomatis directly damage your sperm? Lancet Infect Dis. 2005;5:53–57. doi: 10.1016/S1473-3099(04)01254-X. [DOI] [PubMed] [Google Scholar]
- 32.Hosseinzadeh S, Brewis IA, Pacey AA, Moore HD, Eley A. Coincubation of human spermatozoa with Chlamydia trachomatis in vitro causes increased tyrosine phosphorylation of sperm proteins. Infect Immun. 2000;68:4872–4876. doi: 10.1128/iai.68.9.4872-4876.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hosseinzadeh S, Brewis IA, Eley A, Pacey AA. Co-incubation of human spermatozoa with Chlamydia trachomatis serovar E causes premature sperm death. Hum Reprod. 2001;16:293–299. doi: 10.1093/humrep/16.2.293. [DOI] [PubMed] [Google Scholar]
- 34.Eley A, Hosseinzadeh S, Hakimi H, Geary I, Pacey AA. Apoptosis of ejaculated human sperm is induced by co-incubation with Chlamydia trachomatis lipopolysaccharide. Hum Reprod. 2005;20:2601–2607. doi: 10.1093/humrep/dei082. [DOI] [PubMed] [Google Scholar]
- 35.Satta A, Stivala A, Garozzo A, Morello A, Perdichizzi A, Vicari E, et al. Experimental Chlamydia trachomatis infection causes apoptosis in human sperm. Hum Reprod. 2006;21:134–137. doi: 10.1093/humrep/dei269. [DOI] [PubMed] [Google Scholar]
- 36.Gallegos G, Ramos B, Santiso R, Goyanes V, Gosalvez J, Fernandez JL. Sperm DNA fragmentation in infertile men with genitourinary infection by Chlamydia trachomatis and Mycoplasma. Fertil Steril. 2008;90:328–334. doi: 10.1016/j.fertnstert.2007.06.035. [DOI] [PubMed] [Google Scholar]
- 37.Association of Public Health Laboratories. Laboratory diagnostic testing for Chlamydia trachomatis and Neisseria gonorrhoeae [Internet] Silver Spring: Association of Public Health Laboratories; c2010-2012. [cited 2013 Jan 30]. Available from: http://www.aphl.org/aphlprograms/infectious/std/documents/ctgclabguidelinesmeetingreport.pdf. [Google Scholar]
- 38.Hislop J, Quayyum Z, Flett G, Boachie C, Fraser C, Mowatt G. Systematic review of the clinical effectiveness and cost-effectiveness of rapid point-of-care tests for the detection of genital chlamydia infection in women and men. Health Technol Assess. 2010;14:1–97. doi: 10.3310/hta14290. [DOI] [PubMed] [Google Scholar]
- 39.Geisler WM. Management of uncomplicated Chlamydia trachomatis infections in adolescents and adults: evidence reviewed for the 2006 Centers for Disease Control and Prevention sexually transmitted diseases treatment guidelines. Clin Infect Dis. 2007;44(Suppl 3):S77–S83. doi: 10.1086/511421. [DOI] [PubMed] [Google Scholar]
- 40.Akande V, Turner C, Horner P, Horne A, Pacey A; Impact of Chlamydia trachomatis in the reproductive setting: British Fertility Society Guidelines for practice. Hum Fertil (Camb) 2010;13:115–125. doi: 10.3109/14647273.2010.513893. [DOI] [PMC free article] [PubMed] [Google Scholar]


