Abstract
Purpose
C-reactive protein (CRP) is a general marker for inflammation and it has been associated with prostate cancer. We hypothesized that a correlation may exist between CRP and prostate cancer in patients undergoing transrectal biopsy of the prostate because of rising prostate-specific antigen (PSA) levels.
Materials and Methods
From January 2009 to March 2012, we retrospectively reviewed 710 patients who visited our urology department and were diagnosed as having a PSA value over 4.0 ng/mL. Patients with acute infections, rheumatoid arthritis, gout, asthma, chronic lung disease, myocardial infarction, or apoplexy and those who had taken nonsteroidal anti-inflammatory drugs were exempted from the research because these variables could have impacted CRP. After we applied the exclusion criteria, we selected 63 patients with prostate cancer and 140 patients with benign prostatic hyperplasia (BPH).
Results
A total of 203 patients were observed: 140 patients had BPH, and 63 patients had prostate cancer. Prostate cancer patients were divided into two groups by tumor-node-metastasis classification. The patients below T2 were group A, and those above T3 were group B. The natural logarithm of C-reactive protein (lnCRP) differed between the BPH group and the prostate cancer group. The lnCRP also differed between the BPH group and prostate cancer groups A and B (p<0.05).
Conclusions
The serum CRP level of the prostate cancer group was higher than that of the BPH group. Inflammation may be correlated with prostate cancer according to the serum CRP level.
Keywords: C-reactive protein, Prostate-specific antigen, Prostatic neoplasms
INTRODUCTION
Recent studies have suggested that chronic inflammation is positively associated with cancer [1,2]. For example, stomach, liver, and colon cancer are common in patients with inflammatory colitis [3]. There is considerable correlation between the prognosis of various cancers and specific inflammatory markers and cytokines as well as systemic, nonspecific inflammatory markers such as C-reactive protein (CRP). CRP is a general marker of inflammation, and it is known to be correlated with cancer risks [1]. Also, CRP is reported to have usability as a biomarker in urologic cancer [4]. For example, elevation of CRP levels, which indicates the presence of a cancer-associated systemic inflammatory response, is linked to lower survival in patients with urologic cancers, including renal cell carcinoma and cancers of upper urinary tract, bladder, and prostate.
Inflammation is supposed to be one of the carcinogens of prostate cancer. Inflammation has been shown in prostate biopsy tissues, prostatectomy specimens, and chips from transurethral resection of the prostate. The existence of CRP can be checked through immunochemical examination of the cytoplasm and nucleus of prostate cancer tissue [2].
Macrophage inhibitory cytokine-1 (MIC-1), also known as prostate-derived factor, is a molecule of the transforming growth factor-β super family and has been associated with the progression of various types of diseases, including prostate cancer. Inflammation-associated cytokines may play a critical role in the functional regulation of the MIC-1 gene in the early stages of prostate cancer development [5]. Prostate cancer cell-induced cytokine production by peripheral blood mononuclear cells (PBMCs) and interleukin (IL)-6 is involved in the development of prostate cancers. PBMCs are capable of carrying out an "immune-modulatory dialogue" with colon cancer cells expressed by an increased production of proinflammatory cytokines by the PBMCs [6]. The expression of IL-7 and IL-15 genes in prostate tissue and corresponding serum titers are significantly increased in patients with early stage prostate cancer as compared with patients with benign prostatic hyperplasia (BPH) [7].
Analysis of the results of recent articles suggests that inflammation influences the occurrence of prostate cancer. We hypothesized that a correlation may exist between inflammation and prostate cancer according to the serum CRP level in patients undergoing transrectal biopsy of the prostate because of a rising prostate-specific antigen (PSA) level.
MATERIALS AND METHODS
From January 2009 to March 2012, we retrospectively reviewed 710 patients who visited our urology department and were diagnosed as having PSA over 4.0 ng/mL and prostate volume over 20 mL. CRP was measured in 251 patients before prostate biopsy. Of those patients, 73 had prostate cancer and 178 had BPH.
Patients who had acute infections, rheumatoid arthritis, gout, asthma, chronic lung disease, myocardial infarction, or apoplexy or who had taken nonsteroidal anti-inflammatory drugs were exempted from the research because these variables can impact CRP. After we applied the exclusion criteria, we chose 63 patients with prostate cancer and 140 patients with BPH for the case-control analysis.
The 63 patients are diagnosed with prostate cancer underwent computed tomography, magnetic resonance imaging, and bone scan. Twenty-six patients underwent radical retropubic prostatectomy and one patient underwent a pelvic lymph node dissection. Also, prostate cancer was found in two patients after transurethral resection of the prostate. The clinical stage of prostate cancer was described by the tumor-node-metastasis (TNM) stage, and the prostate cancer patients were classified into two groups according to the TNM classification. Patients below T2 were assigned to group A, and patients above T3 were assigned to group B.
We used t-tests to examine the correlation between CRP and BPH and prostate cancer. We conducted analysis of variance inspection to compare the CRP level of the BPH group, prostate cancer group A, and prostate cancer group B. A p-values below 0.05 indicated statistical significance. The turbid immune assay was used to measure high-sensitivity CRP (hs-CRP). We designated the results in mg/L, and the limit of determination was 0.02 mg/L. The CRP level was determined by the natural logarithm of C-reactive protein (lnCRP) level. Statistical analysis was performed with the statistical program PASW ver. 18.0 (IBM Co., Armonk, NY, USA).
RESULTS
Two hundred three patients were analyzed. Their average age was 64.5±9.28 years (mean±standard deviation [SD]; range, 44 to 91 years). The average age of the 140 BPH patients was 62.2±9.04 years (range, 48 to 91 years). The average age of the 63 prostate cancer patients was 67.2±8.98 years (range, 44 to 79 years). Prostate cancer stages were distributed as follows: 2 patients T1, 41 patients T2, 9 patients T3, and 11 patients T4. Group A (below T2) included 43 patients. Group B (above T3) included 20 patients. The baseline data of the participants are shown in Table 1.
TABLE 1.
Baseline characteristics of the participants

Values are presented as mean±SD (range).
PCa, prostate cancer; BPH, benign prostatic hypertrophy; lnCRP, natural logarithm of C-reactive protein; PSA, prostate-specific antigen; SD, standard deviation.
a:Prostate cancer patients tumor-node-metastasis (TNM) classification below T2. b:Prostate cancer patients with TNM classification above T3.
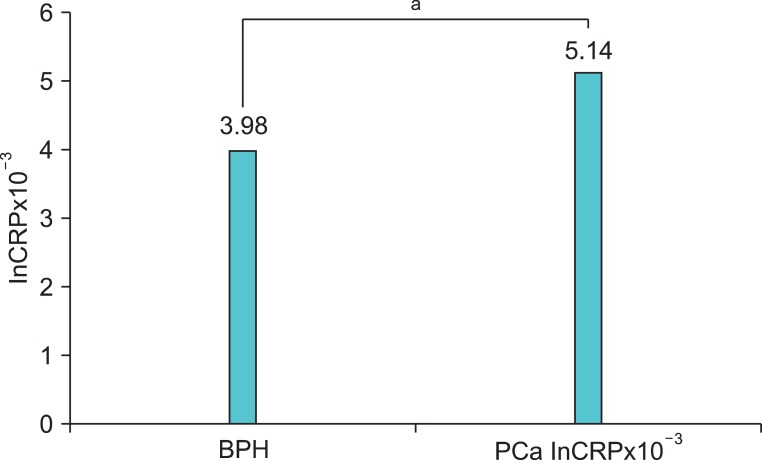
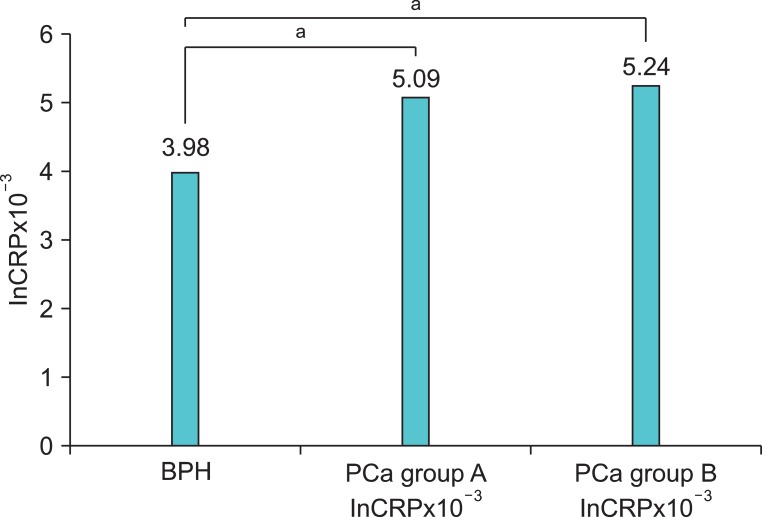
The mean lnCRP level of the BPH group was 3.98±0.43 mg/L. The mean lnCRP level of the prostate cancer group was 5.14±1.43 mg/L. There was a statistically significant difference between the two groups (p<0.05) (Fig. 1). Considering the prostate cancer stages, the mean lnCRP level of prostate cancer group A was 5.09±1.38 mg/L, and that of group B was 5.24±1.58 mg/L. The mean lnCRP level of the BPH group differed from the lnCRP level of group A (p<0.05). There was also a significant difference in lnCRP level between the BPH group and prostate cancer group B (p<0.05) (Fig. 2). There was no correlation between PSA and CRP level (p=0.12).
FIG. 1.
Value of natural logarithm of C-reactive protein (lnCRP) was significantly higher in the prostate cancer (PCa) group than in the benign prostatic hypertrophy (BPH) group (a:p<0.05).
FIG. 2.
Value of logarithm of C-reactive protein (lnCRP) in PCa group A (5.09±1.38) and group B (5.24±1.58) was significantly higher than in the benign prostatic hypertrophy (BPH) group (3.98±0.43) (p<0.05). PCa group A, prostate cancer patients with tumor-node-metastasis (TNM) classification below T2; PCa group B, prostate cancer patients with TNM classification above T3 (a:p<0.05).
DISCUSSION
Even though a causal role of chronic inflammation, recurrent inflammation, or infection is not yet established in prostate cancer, inflammation is considered to contribute to the carcinogenesis process [8]. The role of inflammation includes effects on cytokines and growth factors that participate in tumor growth, the induction of cyclooxygenase-2 in macrophages and the epithelium, and, last, generation of reactive oxygen species causing mutation and nitro-oxidant materials related to tumor growth.
Infiltration of chronic inflammation is very common in the peripheral zone of the prostate where most prostate cancer occurs. The lesions showing inflammation and atrophy, although differing in histology and medical terminology, show epithelial cell proliferation as a group. In these lesions, the heterogeneous expression of the GSTP1 gene is likely to be damaged by oxygen [9].
In a study in genetically modified mice that develop prostate cancer, the incidence of prostate cancer was significantly lower in mice supplemented with celecoxib, a COX-2 inhibitor, than in mice not given celecoxib. The results of this study suggest that celecoxib may have a role in chemoprevention of prostate cancer [10]. This study proves that inflammation is one of the risk factors of cancer. Also, it shows that controlling inflammation can reduce the occurrence of cancer.
A positive correlation between serum CRP and tumor stage is observed in prostate cancer patients. A correlation is also observed between the rise CRP and faster progression of the tumor. This result proves that inflammation participates in tumor progression [2,11]. In addition, this study confirmed the existence of CRP in the cytoplasm and nucleus of prostate cancer patients by immunochemical test. Cytoplasmic CRP has a positive correlation with cancer metastasis when prostate cancer is diagnosed. Nuclear CRP has a correlation with the observation of spreading when prostate cancer recurs [2]. CRP is clearly an independent predicting factor of cancer-specific survival in prostate cancer patients [11].
CRP is clearly confirmed as a factor predicting overall survival of castration-resistant prostate cancer patients treated with docetaxel [12]. Rising plasma CRP suggests a poor prognosis [13]. High CRP is shown in prostate cancer patients who develop bone metastasis [14].
A limitation of this study is the small study population of only 203 patients. Future prospective study should include a larger population of patients for more accurate results. To classify pathological inflammation levels, we need to research the correlation between CRP and prostate biopsy specimens.
CONCLUSIONS
The serum hs-CRP level of the prostate cancer group was higher than that of the BPH group. Inflammation may be correlated with prostate cancer on the basis of the serum hs-CRP level. There was no correlation between PSA and the hs-CRP level.
Footnotes
The authors have nothing to disclose.
References
- 1.Lee S, Choe JW, Kim HK, Sung J. High-sensitivity C-reactive protein and cancer. J Epidemiol. 2011;21:161–168. doi: 10.2188/jea.JE20100128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Elsberger B, Lankston L, McMillan DC, Underwood MA, Edwards J. Presence of tumoural C-reactive protein correlates with progressive prostate cancer. Prostate Cancer Prostatic Dis. 2011;14:122–128. doi: 10.1038/pcan.2011.5. [DOI] [PubMed] [Google Scholar]
- 3.Platz EA, De Marzo AM. Epidemiology of inflammation and prostate cancer. J Urol. 2004;171(2 Pt 2):S36–S40. doi: 10.1097/01.ju.0000108131.43160.77. [DOI] [PubMed] [Google Scholar]
- 4.Saito K, Kihara K. C-reactive protein as a biomarker for urological cancers. Nat Rev Urol. 2011;8:659–666. doi: 10.1038/nrurol.2011.145. [DOI] [PubMed] [Google Scholar]
- 5.Dubey S, Vanveldhuizen P, Holzbeierlein J, Tawfik O, Thrasher JB, Karan D. Inflammation-associated regulation of the macrophage inhibitory cytokine (MIC-1) gene in prostate cancer. Oncol Lett. 2012;3:1166–1170. doi: 10.3892/ol.2012.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Salman H, Ori Y, Bergman M, Djaldetti M, Bessler H. Human prostate cancer cells induce inflammatory cytokine secretion by peripheral blood mononuclear cells. Biomed Pharmacother. 2012;66:330–333. doi: 10.1016/j.biopha.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 7.Mengus C, Le Magnen C, Trella E, Yousef K, Bubendorf L, Provenzano M, et al. Elevated levels of circulating IL-7 and IL-15 in patients with early stage prostate cancer. J Transl Med. 2011;9:162. doi: 10.1186/1479-5876-9-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lucia MS, Torkko KC. Inflammation as a target for prostate cancer chemoprevention: pathological and laboratory rationale. J Urol. 2004;171(2 Pt 2):S30–S34. doi: 10.1097/01.ju.0000108142.53241.47. [DOI] [PubMed] [Google Scholar]
- 9.Lehrer S, Diamond EJ, Mamkine B, Droller MJ, Stone NN, Stock RG. C-reactive protein is significantly associated with prostate-specific antigen and metastatic disease in prostate cancer. BJU Int. 2005;95:961–962. doi: 10.1111/j.1464-410X.2005.05447.x. [DOI] [PubMed] [Google Scholar]
- 10.Gupta S, Adhami VM, Subbarayan M, MacLennan GT, Lewin JS, Hafeli UO, et al. Suppression of prostate carcinogenesis by dietary supplementation of celecoxib in transgenic adenocarcinoma of the mouse prostate model. Cancer Res. 2004;64:3334–3343. doi: 10.1158/0008-5472.can-03-2422. [DOI] [PubMed] [Google Scholar]
- 11.McCall P, Catlow J, McArdle PA, McMillan DC, Edwards J. Tumoral C-reactive protein and nuclear factor kappa-B expression are associated with clinical outcome in patients with prostate cancer. Cancer Biomark. 2011-2012;10:91–99. doi: 10.3233/CBM-2012-0236. [DOI] [PubMed] [Google Scholar]
- 12.Ito M, Saito K, Yasuda Y, Sukegawa G, Kubo Y, Numao N, et al. Prognostic impact of C-reactive protein for determining overall survival of patients with castration-resistant prostate cancer treated with docetaxel. Urology. 2011;78:1131–1135. doi: 10.1016/j.urology.2011.07.1416. [DOI] [PubMed] [Google Scholar]
- 13.Beer TM, Lalani AS, Lee S, Mori M, Eilers KM, Curd JG, et al. C-reactive protein as a prognostic marker for men with androgen-independent prostate cancer: results from the ASCENT trial. Cancer. 2008;112:2377–2383. doi: 10.1002/cncr.23461. [DOI] [PubMed] [Google Scholar]
- 14.Latif Z, McMillan DC, Wallace AM, Sattar N, Mir K, Jones G, et al. The relationship of circulating insulin-like growth factor 1, its binding protein-3, prostate-specific antigen and C-reactive protein with disease stage in prostate cancer. BJU Int. 2002;89:396–399. doi: 10.1046/j.1464-4096.2001.01641.x. [DOI] [PubMed] [Google Scholar]