Abstract
Managing the complex tendo Achilles defect involves reconstructing the Achilles tendon as well as providing soft tissue cover to the heel area. The advent of microsurgery has revolutionised the reconstruction of this difficult defect providing a number of options to the reconstructive surgeon. We present a case of complex tendo Achilles defect reconstructed by the latissimus dorsi free flap.
KEY WORDS: Complex defect, reconstruction, tendo-Achille
INTRODUCTION
Managing tendo-Achilles injuries is a tall order not just due to the tenuous blood supply to the tissues around the ankle joint but also because the reconstructed tendon has to withstand the stresses of normal walking and running. When such injuries are also combined with soft tissue cover loss in the area, the task becomes even more uphill. Numerous methods of tendo-Achilles repair with soft tissue cover are available to the surgeon, all having their respective advantages and disadvantages. The advent of microsurgery has opened up many new and promising options for the reconstructive surgeon to deal with such injuries successfully. We present a case complex tendo-Achilles defect which was reconstructed by using the free latissimus dorsi muscle flap along with its tendon.
CASE REPORT
A 50-year-old gentleman presented to the plastic surgery OPD of our hospital with complains of wound over posterior aspect of right heel for 1 month. He had a history of sudden onset pain and a feeling of ‘give’ while working in the fields 3 months back. His local physician referred him to an orthopaedic colleague who operated upon him twice in a span of 2 months with unfavourable results. Persistence of wound in the Achilles tendon area prompted the patient to seek plastic surgical opinion and hence he visited our OPD. The patient was a farmer by occupation and the sole bread winner of his family. Upon examination there was a 7 × 5 cms wound at the tendo Achilles area. The medial malleolar area was skin grafted and had a small raw area of about 2 × 2 cms near the anterior edge of the graft [Figure 1]. The skin of the medial malleolar area appeared to have been raised as a flap to cover the defect over the tendo Achilles which had necrosed distally later on. The plantar flexion at the ankle joint was extremely weak and the patient was unable to bear his weight on his toes. The patient was counselled regarding the extent and severity of his problems and the options for reconstructing complex tendo Achilles defects. It was decided to offer the patient a free flap reconstruction of the complex defect.
Figure 1.

Photograph showing defect over the posterior aspect of right Achilles tendon area and skin graft over the medial malleolar area
FLAP ANATOMY AND OPERATIVE DETAILS
The patient was taken for surgery under general anaesthesia with endotracheal intubation. The patient was kept in a semi right lateral position so that the affected limb was down and the surface with the raw area faced the surgeon operating on the limb. The defect at the tendo Achilles area was surgically excised to expose the site of previous repair. The turned down portion of the tendo Achilles used to repair the defect in the previous surgery was found to be in a state of progressive necrosis with scarring in the adjoining areas [Figure 2]. The skin graft over the medical malleolar area was also excised and the defect completely freed of all dead tissue and necrotic debris. A defect of almost 5 cms was found in the Achilles tendon after debridement. The left latissimus dorsi muscle was harvested through a vertical incision running along the left flank, along with its vascular pedicle which was traced right up to the axillary vessels. The muscle was harvested along with its tendon [Figure 3]. The incision was closed in layers after haemostasis under suction drain. The tendon of the latissimus dorsi muscle was used to reconstruct the defect in the tendo Achilles and the muscle was used to cover the reconstructed tendon as well as the adjacent raw areas [Figure 4]. The subscapular vessels were anastomosed to the posterior tibial artery and its vena in an end to side fashion and the flap was inset into the defect [Figure 5]. The whole area was covered with a split skin graft and light compressive dressing along with limb splintage and elevation was done. The postoperative period was uneventful. The drain was removed at 48 hours and the patient discharged on Day 7 with ankle splint and instruction for home care of the skin graft. The patient was followsed up after 6 weeks after which graded weight bearing was started. Follow-up at 6 months revealed a good strength of plantar flexion and ability of the patient to bear his weight on his toes whereupon unassisted full weight bearing was started [Figures 6 and 7].
Figure 2.
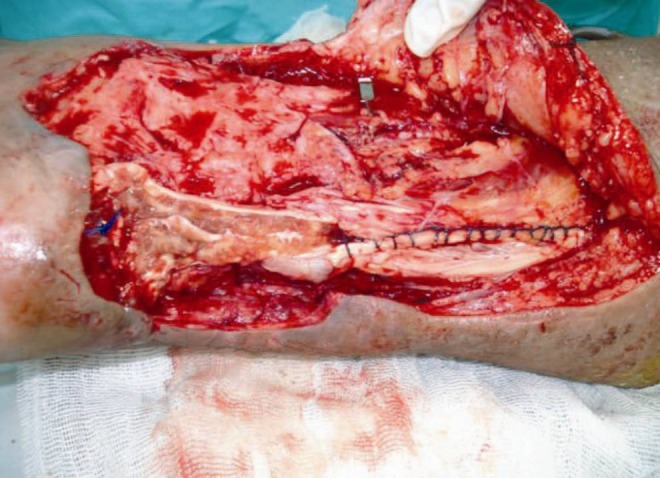
Necrosed turn down flap used to reconstruct the Achilles tendon in during the previous surgeries
Figure 3.
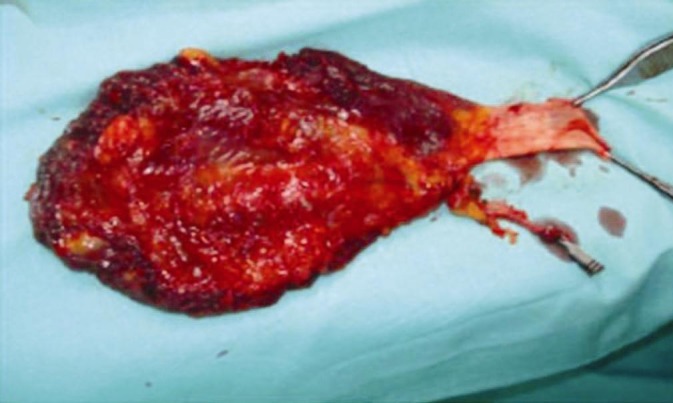
Harvested latissimus dorsi muscle with its tendon
Figure 4.
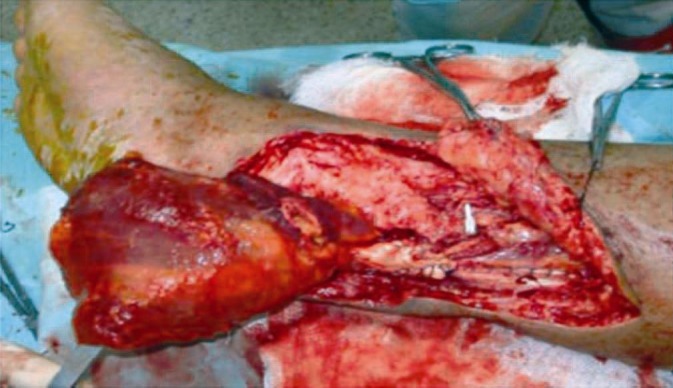
Tendon of latissimus dorsi muscle has been used to reconstruct the segmental defect in the Achilles tendon
Figure 5.

Latissimus dorsi muscle flap completely inset into the defect
Figure 6.

Healed flap at 6 months. Patient able to stand on tip toes
Figure 7.

Patient able to stand on toes at 6 months
The latissimus dorsi muscle is a Type V muscle and is the gold standard of donor composite tissue transfer because of its dependability and applicability. It is useful in the reconstruction of extensive defects, contaminated wounds and osteomyelitic or osteoradionecrotic bones. The vascular pedicle (thoracodorsal vessel) is long and reliable and has a good diameter. It can be extended by including the subscapular vessels up to its axillary origin where it is 6 mm in diameter and gives an additional 2.2 cms of length. The origin of the muscle extends from the seventh thoracic spine to the iliac crest and it inserts with a broad quadrilateral tendon of about 3 inches in length on the medial lip of the bicipital groove. The muscle can be split in to two parts along the transverse and descending branches of the thoracodorsal vessels and can also be thinned peroperatively to decrease its bulk and give a good aesthetic appearance. The muscle flap can also include additional tissue like the lower three slips of the serratus anterior muscle and the scapular and para-scapular flaps on the same pedicle.[1]
DISCUSSION
The management of posterior heel defects with segmental loss of the Achilles tendon and overlying skin and soft tissues is complex. The aims of the reconstructive exercise in such cases are: 1) To provide a tendon reconstruction that can withstand the mechanical and shear forces required for normal functions of walking, running and standing on tip toe; 2) to provide vascularised soft tissue cover to address the contour defect, protect the tendon reconstruction and allow smooth gliding of the tendon; and 3) to provide durable skin cover to allow wearing of shoes.[2] The availability of local muscle, skin or fascia to cover tissue defects in the lower leg is limited. Earlier, treatment involved multi-staged procedures, long hospital stays and often, a too high rate of complications. The advent of microsurgery since the early 1970s has changed this scenario. Despite this procedures have been developed that use local tissues along with fascia or tendon grafts to manage these defects. Such options include 1) medial plantar flap with tensor fascia lata tendon graft;[3] 2) pedicled medial plantar flap with vascularised plantar aponeurosis[4] and 3) Sural island myofasciocutaneous flap with lateral belly of the gastrocnemius muscle.[5] With the advancement of microsurgical techniques, free tissue transfer has provided an elegant method of soft tissue cover for posterior ankle defects. Free tissue transfer supplies vascularised tissue to enhance wound healing and to protect against infection. Early report of composite flaps for reconstructing the tendon as well as providing cover have included a free groin flap with an external oblique aponeurosis sheet and a free groin flap with iliac bone and abdominal fascia.[6,7] Other composite flaps have been described such as the lateral thigh flap with vascularised fascia lata,[8] free scapular/para scapular flap with fascial extension[9] and the free ALT with a fascia lata extension.[10]
An underutilized donor site for Achilles tendon region reconstructions is the latissimus dorsi. The latissimus dorsi was first used to reconstruct the Achilles tendon and to provide soft tissue coverage in 1999.[11] The latissimus dorsi muscle is a good choice for composite reconstruction in the Achilles tendon area because of its reliable vascular pedicle, its dependability, ease of harvest and minimal donor site morbidity. The donor area can be closed completely if only the muscle is harvested and it does not lead to a significant post-operative functional deficit in the movements of the ipsilateral arm. Transfer of the muscle alone followed by a split thickness skin graft, improves the appearance of both the recipient and the donor sites.[12,13] Atrophy of the denervated muscle over a couple of months leaves it thin, pliable and non-bulky. The muscle provides a good length of vascularised tendon for Achilles tendon reconstruction (up to 3 inches or 7.5 cms) and a large area of well vascularised tissue for coverage of the soft tissue defect. The donor vessels, the thoracodorsal or subscapular, have a good external diameter and little anatomic variation making it one of the most frequently harvested and used muscle in reconstructive microsurgery. The muscle can be harvested completely or in part and can also be used to carry with it a large area of the overlying skin. The denervated muscle usually atrophies and becomes fibrous and rarely needs debulking thus facilitating shoe wearing for the patient. An excellent functional result can be expected by 3-6 months with little residual disability. Full loading of the tendon like jogging, running and indulging in sports or other strenuous activities (farming in this example) can only be reliably assumed after a period of one to three years.[2]
RECOMMENDATIONS
In complex cases of segmental loss of the Achilles tendon with overlying skin and soft tissue defect good functional results with minimal donor site morbidity or functional loss can be expected from a latissimus dorsi muscle free flap, harvested along with its tendon for composite reconstruction of the defect.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Donald S. The latissimus dorsi muscle and musculo-cutaneous flap. In: Donald S, editor. Atlas of microsurgical composite tissue transplantation. 1st ed. Philadelphia: W. B Saunders Company; 1996. pp. 205–19. [Google Scholar]
- 2.Chalmers R, Tare M, Niranjan N. Vascularised achilles tendon graft reconstruction - by the tendon for the tendon. J Plast Reconstr Aesthet Surg. 2010;63:273–6. doi: 10.1016/j.bjps.2009.07.014. [DOI] [PubMed] [Google Scholar]
- 3.Taniguchi Y, Tamaki T. Reconstruction of the Achilles tendon and overlying skin defect with a medial plantar flap and fascia lata graft. J Reconstr Microsurg. 2000;16:423–5. doi: 10.1055/s-2006-947148. [DOI] [PubMed] [Google Scholar]
- 4.Dumont CE, Kessler J. A composite medial plantar flap for the repair of an Achilles tendon defect: A case report. Ann Plast Surg. 2001;47:666–8. doi: 10.1097/00000637-200112000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Rajendra Prasad JS, Cunha-Gomes D, Chaudhari C, Bhathena HM, Desain S, Kavarana NM. The venoneuroadipofascial pedicled distally based sural island myofasciocutaneous and muscle flaps: Anatomical basis of a new concept. Br J Plast Surg. 2002;5:203–9. doi: 10.1054/bjps.2001.3818. [DOI] [PubMed] [Google Scholar]
- 6.Taylor GI, Townsend P. Composite free flap and tendon transfer: An anatomical study and a clinical technique. Br J Plast Surg. 1979;32:170–83. doi: 10.1016/0007-1226(79)90030-4. [DOI] [PubMed] [Google Scholar]
- 7.Wei FC, Chen HC, Chuang CC, Noordhoff MS. Reconstruction of Achilles tendon and calcaneus defects with skin-aponeurosis-bone composite free tissue from the groin region. Plast Reconstr Surg. 1988;81:579–89. doi: 10.1097/00006534-198804000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Inoue T, Tanaka I, Imai K, Hatoko M. Reconstruction of Achilles tendon using vascularised fascia lata with free lateral thigh flap. Br J Plast Surg. 1990;43:728–31. doi: 10.1016/0007-1226(90)90199-a. [DOI] [PubMed] [Google Scholar]
- 9.Sauerbier M, Erdmann D, Schepler H, Bickert B, Germann G. The scapular/parascapular flap in reconstruction of distal lower extremity soft tissue defects over the Achilles tendon. Eur J Plast Surg. 1998;21:333–7. [Google Scholar]
- 10.Lee JW, Yu JC, Shieh SJ, Liu C, Pai JJ. Reconstruction of Achilles tendon and overlying soft tissue using the antero-lateral thigh free flap. Br J Plast Surg. 2000;3:574–7. doi: 10.1054/bjps.2000.3407. [DOI] [PubMed] [Google Scholar]
- 11.Lee HB, Lee DH, Oh SH, Tark KC, Kim SW, Chung YK, et al. Simultaneous reconstruction of the Achilles tendon and soft tissue defect using only a latissimus dorsi muscle free flap. Plast Reconstr Surg. 1999;104:111–9. [PubMed] [Google Scholar]
- 12.Gordon L, Buncke HJ, Alpert BS. Free latissimus dorsi muscle flap with split thickness skin graft cover: A report of 16 cases. Plast Reconstr Surg. 1982;70:173–8. doi: 10.1097/00006534-198208000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Bailey BN. Latissimus dorsi flap - a practical approach. Ann Acad Med Singapore. 1979;8:445–53. [PubMed] [Google Scholar]


