Abstract
Introduction
Severity assessment and site-of-care decisions for patients with community-acquired pneumonia (CAP) are pivotal for patients' safety and adequate allocation of resources. Late admission to the intensive care unit (ICU) has been associated with increased mortality in CAP. We aimed to review and meta-analyze systematically the performance of clinical prediction rules to identify CAP patients requiring ICU admission or intensive treatment.
Methods
We systematically searched Medline, Embase, and the Cochrane Controlled Trials registry for clinical trials evaluating the performance of prognostic rules to predict the need for ICU admission, intensive treatment, or the occurrence of early mortality in patients with CAP.
Results
Sufficient data were available to perform a meta-analysis on eight scores: PSI, CURB-65, CRB-65, CURB, ATS 2001, ATS/IDSA 2007, SCAP score, and SMART-COP. The estimated AUC of PSI and CURB-65 scores to predict ICU admission was 0.69. Among scores proposed for prediction of ICU admission, ATS-2001 and ATS/IDSA 2007 scores had better operative characteristics, with a sensitivity of 70% (CI, 61 to 77) and 84% (48 to 97) and a specificity of 90% (CI, 82 to 95) and 78% (46 to 93), but their clinical utility is limited by the use of major criteria.
ATS/IDSA 2007 minor criteria have good specificity (91% CI, 84 to 95) and moderate sensitivity (57% CI, 46 to 68). SMART-COP and SCAP score have good sensitivity (79% CI, 69 to 97, and 94% CI, 88 to 97) and moderate specificity (64% CI, 30 to 66, and 46% CI, 27 to 66). Major differences in populations, prognostic factor measurement, and outcome definition limit comparison. Our analysis also highlights a high degree of heterogeneity among the studies.
Conclusions
New severity scores for predicting the need for ICU or intensive treatment in patients with CAP, such as ATS/IDSA 2007 minor criteria, SCAP score, and SMART-COP, have better discriminative performances compared with PSI and CURB-65. High negative predictive value is the most consistent finding among the different prediction rules. These rules should be considered an aid to clinical judgment to guide ICU admission in CAP patients.
Introduction
Community-acquired pneumonia (CAP) is a major health problem. In the United States, 500,000 adults are hospitalized annually for CAP [1], of whom 10% to 20% are admitted to the intensive care unit (ICU) [2]. Because site of care is a major determinant of costs, clinical prediction rules have been developed to identify patients with low mortality who can be safely treated as outpatients [3].
Since 1993, efforts have been made to identify severe community-acquired pneumonia (SCAP) requiring admission to the ICU because the ICU is an expensive and scarce resource. Concurrently, delay in ICU admission of CAP patients has been shown to be associated with increased mortality [4-6]. In 1993, the American Thoracic Society (ATS) proposed a definition of severe CAP requiring ICU admission [7]. Since then, these criteria have been updated twice [8,9], and various clinical prediction rules have been developed to predict SCAP [10-12]. In addition to the variety of the prediction rules, the assessment of their validity is further hampered by the absence of a unique definition of SCAP and the inclusion of ICU admission or intensive treatment in the definition, which exposes prediction rules for SCAP to incorporation bias [13].
The goal of our search was to review systematically the performance of existing clinical prediction rules to identify in the Emergency Department patients with CAP requiring ICU admission or intensive treatment.
Materials and methods
Search strategy and study selection
We systematically searched Medline, Embase, and the Cochrane Controlled Trials registry by using the following key words: community-acquired pneumonia AND (decision tree OR clinical prediction rule OR clinical prediction score OR clinical decision rule OR clinical decision score OR management studies OR outcome studies OR ICU admission OR ICU need OR invasive management OR severity assessment). The search was performed for articles in English, French, Italian, Spanish, and German languages and limited to articles with an abstract and completed on the first of March 2012. To ensure a comprehensive literature search, we examined reference lists from retrieved articles and reference literature (guidelines and systematic reviews) and questioned experts in CAP for possible missing studies.
Study inclusion and data extraction
Eligible studies were prospective or retrospective studies evaluating clinical prediction rules in adult immunocompetent patients with CAP to predict the need for ICU admission, intensive treatment, or early mortality (< 14 days). The evaluation had to be performed during the first 24 hours after hospital admission. Studies addressing specific patient subgroups based on etiology or age were excluded. A prediction rule was defined as the combination of two or more clinical or biologic markers. Four investigators (CM, NG, SC, and OG) evaluated studies for possible inclusion. All studies were evaluated independently by at least two investigators. Nonrelevant studies were excluded based on title and abstract. For potentially relevant studies, the full text was obtained, and two investigators (CM, NG) independently assessed study eligibility and extracted the data on study design, patient characteristics, and outcomes. Disagreements were resolved by consensus or by discussion with a third reviewer (AP)
Quality assessment
We used modified quality criteria based on the guidelines for assessing quality in prognostic studies [14]. Two investigators (CM, NG) assessed study quality independently. Each of six items was scored from 0 to 2. Studies with a total quality score between 11 and 12 were considered "good," between 9 to 10, "moderate," and 8 or less was considered "poor."
Data analysis
For each score, the diagnostic performances (sensitivity, specificity, likelihood ratios, and diagnostic odds ratios) to predict different definitions of SCAP (ICU admission, early death, or intensive treatment) at the usual cut-off were pooled by using the method of the inverse of the variance. Random effects were systematically introduced [15]. Heterogeneity was measured by the I-square index [16] and tested with the Cochran test. Potential heterogeneity factors were explored by subgroup analyses for the Pneumonia Severity Index (PSI) (only score with more than 10 studies). A sensitivity analysis was conducted to check the robustness of the pooled sensitivities and specificities by removing each study, one by one. The R package "meta: Meta-analysis with R, version 1.6-1" was used for these analyses. For the PSI and CURB-65 (Confusion, Urea, Respiratory Rate, Blood pressure, Age > 65 years) scores, a summary ROC curve was assessed by the approach proposed by Moses et al. [17]. As several sensitivities and specificities were reported in the studies at different cut-offs, we used a linear mixed model with a correlation structure to take the dependence of the measures into account. The 95% confidence intervals of the areas under the curves were obtained by bootstrap. This analysis was performed with S-plus 8.0 for Windows. The significance level was 0.05 for all analyses. Forest plots of the Sensibility and Specificity were used for the graphic display of the results.
Results
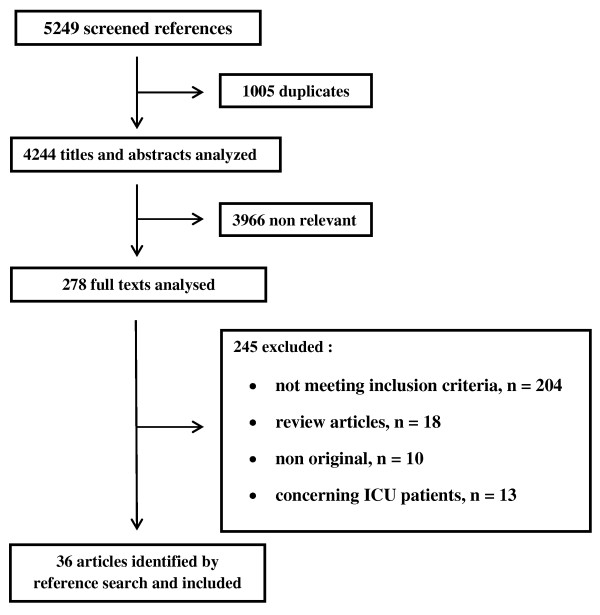
The search retrieved a total of 5,249 references, among which 1,005 duplicates were identified. Of the 4,244 remaining articles, 3,966 were excluded based on title and abstract (Figure 1). Full texts were obtained for the remaining 278 articles. Ten did not contain original data, 13 concerned only ICU patients, 204 did not meet inclusion criteria, 18 were review articles, and 33 satisfied inclusion criteria. Three articles [18-20] were identified by manual search of the references, leading to a total of 36 included articles [5,10-12,18-50]. Main characteristics of included studies are detailed in Table 1.
Figure 1.
Study flow chart.
Table 1.
Main characteristics of included studies
| Study first author | Year of publication | Studied scores | End point | Prevalence end point | Uni- versus multicentric | Prospective/Retrospective | Ambulatory/Hospitalized | Number | NTBR | Major criteria excluded |
|---|---|---|---|---|---|---|---|---|---|---|
| Ananda-Rajah | 2008 | PSI/CURB-65 | ICU admission | 10.50% | Uni | R | H | 408 | Included | n |
| Angus | 2002 | PSI/ATS 2001/ATS 1993/URB | ICU admission | 12.70% | Multi | P | H | 1,339 | Included | n |
| Brown | 2009 | IDSA-ATS 2007/SMART-COP/CURB-65/SCAP | IT in ICU/IT/ICU admission | 12.35% | Uni | R | A+H | 2,413 | Excluded | n |
| Buising | 2006 | PSI/ATS 2001/CURB/CURB-65 | ICU admission/death or ICU | 6.60% | Uni | P | A+H | 392 | Included | n |
| Buising | 2007 | PSI/CURB/CURB-65/CORB | Vent/vaso ICU | 6.30% | Uni | P | A+H | 330 | Included | n |
| Calbo | 2004 | PSI | ICU admission | 3.30% | Uni | P | H | 362 | Included | n |
| Capelastegui | 2006 | CURB-65 | ICU admission | 4.09% | Uni | R | H | 1,100 | Included | n |
| Chalmers | 2008 | CRB-65/CURB-65 | Vent/vaso | 10.20% | Multi | P | A+H | 1,007 | Excluded | n |
| Chalmers | 2011 | IDSA-ATS 2007/SMART-COP/CURB-65/SCAP/CURB/CRB-65/PSI, ATS 2001 minor | Vent/vaso ICU admission |
6.4% 7.6% |
Uni | P | H | 1,062 | Excluded | y |
| Charles | 2008 | SMART-COP/CURB-65/PSI | Vent/vaso | 10.30% | Multi | P | A+H | 882 | Included | n |
| Davis | 2010 | SMART-COP/SMARTACOP | Vent/vaso | 21.00% | Uni | P | H | 184 | Excluded | n |
| Escobar | 2008 | Abbreviated PSI | ICU admission | 12.30% | Uni | R | H | 6,147 | Included | n |
| Espana | 2006 | ATS 2001/PSI/CURB-65/SCAP | Death, vent, or septic shock | 7.10% | Uni | P | A+H | 1,057 | Included | n |
| Death, vent or septic shock | 5.90% | Uni | P | A+H | 719 | Included | n | |||
| Death, vent or septic shock | 11.9% | Multi | R | H | 1,121 | Included | n | |||
| Espana | 2010 | SCAP/PSI/CURB-65 | ICU admission | NA | Multi | R | H | 712 | Included | n |
| Ewig | 2000 | PSI | ICU admission | 9% | Uni | P | H | 232 | Included | n |
| Ewig | 2004 | ATS 2001/PSI/CURB/CRB/URB/ | ICU admission | 16.70% | Uni | p | H | 696 | Excluded | n |
| Ewig | 1998 | ATS 1993/ATS 2001 | ICU admission | 16% | Uni | p | H | 332 | Excluded | n |
| Feagan | 2000 | PSI | ICU admission | 13.60% | Multi | r | H | 858 | Included | n |
| Frei | 2004 | SBP/pH/O2 saturation/pulse | ICU admission | 17% | Uni | r | H | 782 | Included | n |
| Fukuyama | 2011 | IDSA-ATS 2007/SMART-COP/CURB-65/SCAP/PSI/A-DROP | ICU admission Death, vent, or septic shock |
7.6% 11.9% |
Uni | p | H | 505 | Excluded | n |
| Garcia-Vidal | 2008 | PSI | Early death | 2.3% | Uni | p | H | 2,457 | Included | |
| Garau | 2008 | PSI | ICU admission | 5% | Multi | r | H | 3,233 | Included | n |
| Kamath | 2003 | CURB | ICU admission | 10% | Uni | p | H | 100 | Excluded | n |
| Lamy | 2004 | PSI | ICU admission | 14% | Uni | r | H | 152 | Included | n |
| Liapikou | 2009 | IDSA-ATS 2007/ATS 2001/PSI | ICU admission | 11% | Uni | p | H | 2,102 | Excluded | n(y) |
| Man | 2007 | PSI/CURB-65/CRB-65/ATS 2001 | ICU admission | 4% | Uni | p | H | 1,016 | Included | n |
| Marrie | 2007 | PSI/CURB-65 | ICU admission | 10% | Multi | p | H | 3,675 | Included | n |
| Neill | 1996 | CURB | Mortality and ICU | 11% | Uni | p | H | 251 | Excluded | n |
| Phua | 2009 | PSI/CURB-65/IDSA-ATS 2007 | ICU admission | 15% | Uni | p | H | 1,017 | Excluded | y |
| Putinati | 2003 | PSI | ICU admission | 10% | Uni | p | H | 229 | Included | n |
| Renaud | 2007 | PSI | ICU admission | 3.70% | Multi | p | H | 566 | Included | n |
| PSI | ICU admission | 10.50% | Multi | p | H | 761 | Included | n | ||
| Renaud | 2009 | REA-ICU | Early ICU admission < 3 | 4.40% | Multi | p | A+H | 4,593 | Excluded | y |
| Restrepo | 2008 | PSI/ATS 2001 | ICU admission | 19.90% | Multi | r | H | 730 | Excluded | n |
| Riley | 2004 | ATS 2001/PSI | ICU admission | 23.69% | Uni | r | H | 498 | Excluded | n |
| Roson | 2001 | PSI | ICU admission | 8% | Uni | p | H | 533 | Included | n |
| Shah | 2010 | CURB-65/PSI | ICU admission | 23.30% | Uni | p | A+H | 150 | Included | n |
| Van der Eerden | 2004 | PSI | ICU admission | 8.00% | Uni | p | H | 260 | Included | n |
A, ambulatory; H, hospitalized; ICU, intensive care unit; IT, intensive treatment; P, prospective; R, retrospective; n, number; y, yes; NTBR, not to be resuscitated; Vent, ventilation; Vaso, vasopressor.
Scores
We identified 11 main severity scores based on 20 variables. Components of the main severity scores are illustrated in Figure 2. Sufficient data were available to perform a meta-analysis on eight scores: PSI, CURB-65, CRB-65 (Confusion, Respiratory Rate, Blood pressure, Age > 65), CURB (Confusion, Urea, Respiratory rate, Blood pressure), ATS 2001 criteria, ATS/Infectious Disease Society of America (IDSA) 2007 criteria, SCAP score (Severe Community-Acquired Pneumonia), and SMART-COP (Systolic Blood pressure, Multilobar infiltrate, Albumin, Respiratory Rate, Tachycardia, Confusion, low Oxygen, low PH) (Table 2) Score definitions are included in the Additional file 1. Forrest plots for specificity and sensitivity of the eight scores for the prediction of ICU admission are provided in Additional file 2.
Figure 2.
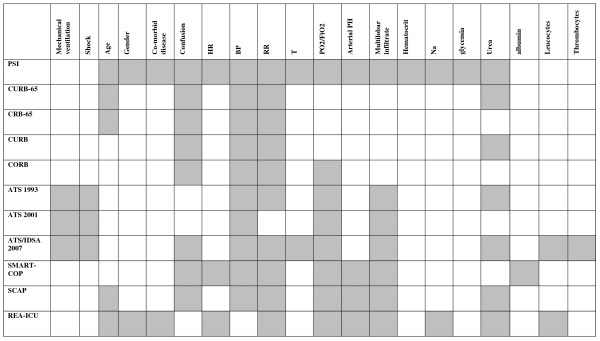
Components of the main severity scores. Criteria used in the score appear as shaded areas. BP, blood pressure; HR, heart rate; RR, respiratory rate; T, temperature.
Table 2.
Operative characteristics of the principal scores to predict ICU admission at their usual cut-off (95% CI)
| Sensitivity | Specificity | NLR | PLR | DOR | |
|---|---|---|---|---|---|
| PSI ≥ 4 | 75.0 (71-78) | 48.0 (44-52) | 0.53 (0.46-0.6) | 1.5 (1.4-1.6) | 2.9 (2.4-3) |
| CURB-65 ≥ 3 | 56.2 (41-70) | 74.2 (68-79) | 0.64 (0.51-0.79) | 2.1 (1.6-2.7) | 3.6 (2.2-5.8) |
| CRB-65 ≥ 3 | 34.2 (18-55) | 90.6 (89-92) | 0.72 (0.54-0.97) | 3.6 (1.9-6.9) | 5.0 (2.0-12.7) |
| CURB ≥ 2 | 76.8 (48-92) | 68.6 (53-81) | 0.35 (0.18-0.70) | 2.3 (1.9-2.7) | 5.5 (3.7-8.2) |
| ATS 2001 | 69.5 (61-77) | 90.1 (82-95) | 0.37 (0.30-0.46) | 7.3 (4.4-12.2) | 24.6 (13.1-46.4) |
| ATS 2007 | 83.8 (48-97) | 77.7 (46-93) | 0.22 (0.08-0.66) | 3.8 (1.7-8.6) | 17.6 (13.1-24.1) |
| ATS 2007a | 57.0 (46-68) | 90.5 (84-95) | 0.48 (0.38-0.6) | 5.9 (3.8-9.3) | 13.1 (7.7-22.3) |
| SCAP | 93.8 (88-97) | 45.6 (27-66) | 0.13 (0.06-0.26) | 1.8 (1.2-2.6) | 14.9 (6.7-33.1) |
| SMART-COP | 79.0 (69-87) | 64.2 (30-66) | 0.15 (0.03-0.91) | 2.6 (1.3-5.3) | 14.9 (8.6-25.7) |
DOR, diagnostic odds ratio; NLR, negative likelihood ratio; PLR, positive likelihood ratio. aMinor criteria.
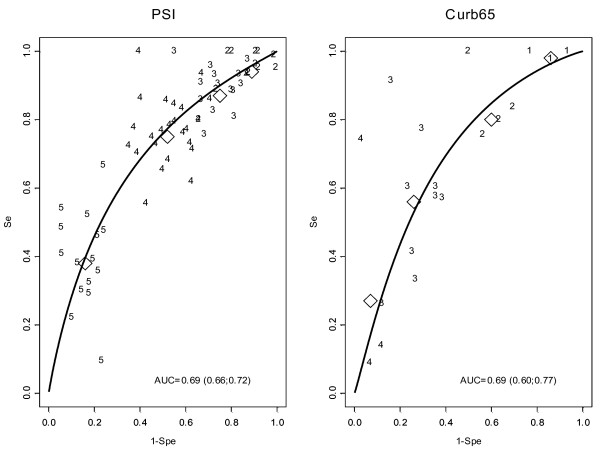
PSI
Twenty-four studies [5,18,19,21,22,24-26,32,34,36,39-52], including 20,622 patients and 2,073 ICU admissions (10.1%), evaluated the performance of PSI to predict ICU need. A PSI score category of IV or more had a pooled sensitivity of 75% and a specificity of 48%. A cut-off of V increased specificity to 84% and decreased sensitivity to 38%. The global performance of PSI to predict ICU admission was modest, with an AUC of 0.69 (Figure 3). Significant heterogeneity was present. Performance of PSI to predict an alternative definition of SCAP, including mortality, was superior, with a pooled sensitivity of 92.4% (CI, 89 to 95) and specificity of 56.2% (CI, 43 to 69) in four cohorts including 3,195 patients [11,49].
Figure 3.
SROC curve and area under the curve (AUC) of Pneumonia Severity Index (PSI) and CURB-65 to predict ICU admission. Individual studies are represented by a number indicating the cut-off used. Their place on the diagram represents the sensitivity and specificity of the individual study. Diamonds represent meta-analytic test statistics for each cut-off.
CURB-65
CURB-65 was studied in nine cohorts [21,24,25,27,40,42,47,49,50] including a total of 5,773 patients and 479 ICU admissions (8.3%). At the usual cut-off value of 3 or more, pooled sensitivity was 56%, and specificity, 74%. The global performance of CURB-65 to predict ICU admission was similar to PSI with an AUC of 0.69 (Figure 3). Significant heterogeneity was present. The performance of CURB-65 to predict the need for ventilation or vasopressors was studied in three publications [10,28,50] including 2,951 patients, 264 requiring intensive treatment. Results were similar, with a pooled sensitivity of 57.2% (CI, 37 to 75) and specificity of 77.2% (CI, 73 to 81).
CRB-65
CRB-65 is a simplified version of the CURB-65 including only clinical predictors. Two studies [40,50] including 2,078 patients and 122 ICU patients (5.8%) calculated the performance of CRB-65 to predict ICU admission. For a threshold of 3 or more, pooled sensitivity was 34%, and specificity, 91%.
CURB (original BTS rule)
Performance of CURB to predict ICU admission was studied in four cohorts [24,25,32,38] totaling 1,418 patients and 161 ICU admissions (12.1%). Pooled sensitivity of a CURB score of 2 or more to predict ICU admission was 76.8%, and specificity, 68.6%. Significant heterogeneity was observed.
ATS 2001
The original ATS criteria for severe CAP published in 1993 [7] included 10 criteria. Some of these criteria were assessed at admission, and others, at any time during clinical course, limiting their use as a prediction rule. A new set of criteria was proposed by Ewig in 1998 [33] and adopted by the ATS in 2001. This prediction rule consists of two major (mechanical ventilation or shock) and three minor criteria (blood pressure < 90 mm Hg at admission, PaO2/FiO2 < 250 mm Hg, and multilobar involvement on chest radiograph). The prediction rule is considered positive in the presence of one major or two minor criteria.
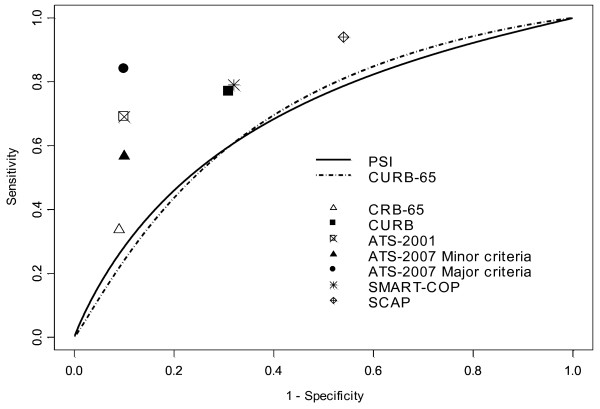
We identified eight studies [5,22,24,32,33,39,40,45,49] including a total number of 7,116 patients with 908 ICU admissions (12.8%). The pooled sensitivity was 69.5%, and specificity, 90.1%. Pooled AUC could not be calculated because of insufficient data. Performance of the 2001 ATS criteria in comparison with PSI and CURB-65 is illustrated in Figure 4. A supplementary study [11] validated this rule to predict a composite definition of SCAP (in-hospital death, mechanical ventilation, or shock) in three cohorts including 2,897 patients and 252 SCAP (8.7%). Pooled sensitivity of the ATS 2001 criteria was 52.7%, and specificity, 95.1%. One study validated the use of the ATS 2001 minor criteria on a cohort excluding patients with therapeutic limitations or major criteria [50]. Sensitivity and specificity of two or more minor criteria to predict ICU admission were 47% and 91%.
Figure 4.
Pooled discriminative performance of the principal scores for severe CAP compared with Pneumonia Severity Index (PSI) and CURB-65 ROC curve.
ATS-IDSA 2007
A new prediction rule was proposed by the ATS and the Infectious Disease Society of America (IDSA) in 2007. This rule, known as the ATS-IDSA rule, consists of two major (mechanical ventilation or shock) and nine minor criteria (Figure 2). The rule is considered positive in the presence of one major or three minor criteria. We found five publications evaluating this rule [23,39,42,49,50]. Two studies, including 2,400 patients and 266 ICU patients (11%), validated the original rule to predict ICU admission [39,49]. Pooled sensitivity was 84%, and specificity, 78%.
Four studies [23,39,42,50] evaluated the performance of the minor criteria in a total of 6,412 patients including 650 ICU patients (10.1%). Pooled sensitivity was 57%, and specificity, 90%. Significant heterogeneity was present. Performance of the 2007 ATS-IDSA rule in comparison with PSI and CURB-65 is illustrated in Figure 4.
SMART-COP
Charles et al. [10] developed a prediction rule based on eight weighted criteria (see Additional File 1). This rule was validated in five external cohorts of pneumonia patients and further adapted and validated in two cohorts [29,50]. Pooled sensitivity of SMART-COP to predict the need for vasopressors or mechanical ventilation was 79%, and specificity, 68%.
Two studies evaluated this rule to predict ICU admission [49,50], with a pooled sensitivity of 79% and specificity of 64% on 1,567 patients including 112 ICU admissions (7.1%).
SCAP score
Espana et al. [11] derived and validated a prediction rule based on eight weighted criteria (see Additional File 1). Pooled performance of this rule on three cohorts totaling 3,402 patients (SCAP, 9%) to predict a composite definition of SCAP (in-hospital death, mechanical ventilation, or shock) was 92% (0.83 to 0.97) for sensitivity and 64% (0.5 to 0.76) for specificity.
Pooled performance of the SCAP score to predict ICU admission in two recent cohorts [49,50] was similar in terms of sensitivity (94%) but lower regarding specificity (46%)
Other scores
Renaud et al. [12] proposed a prediction rule (REA-ICU index) based on 11 predictors (see Additional File 1). This rule was derived to predict early ICU admission (day 1 to day 3), excluding patients with an obvious ICU indication at admission and patients with therapeutic limitations (not to be resuscitated, NTBR order) and validated on four North American and European prospective multicenter cohorts including 6,560 patients. AUC was 0.81 (CI, 0.78 to 0.83) on the overall population.
An abbreviated version of the PSI was tested on an administrative database [30], and some authors proposed to modify the CURB rule to include an oxygenation parameter [25] (CORB). These scores have not been validated in other cohorts.
Quality assessment and sources of heterogeneity
We completed quality assessment according to the criteria developed by Hayden et al. [14].
Nine studies were considered good (scores ≥ 11); 23, moderate (9 to 10); and four poor (≤ 8) quality (see Additional file 3). Important differences were observed in terms of design, populations, and ICU admission rates. Twenty-nine studies included only hospitalized patients, and seven included both hospitalized and ambulatory patients. Patients with therapeutic limitations (NTBR order) were excluded in 15 of 36 studies, and patients with an obvious indication for ICU, in three [12,42,47]. ICU admission rate varied from 3.3% [26] to 23.9% [45], and receipt of intensive treatment in the ICU was highly variable (16% to 100% [25,33]). When multiple measures of the same variable were available, as for vital signs, the measure introduced into the prediction rule was the first available one in four studies, the most abnormal one in five, and not specified in the majority of studies.
We performed an analysis to identify sources of heterogeneity for the only score (PSI) evaluated in at least 10 studies. Analyses did not reveal any significant factor of heterogeneity for sensitivity. Three factors influenced specificity: inclusion of NTBR patients decreased specificity; studies of good quality or high prevalence (≥ 15%) showed higher specificity. Nevertheless, the NTBR factor is highly correlated with the quality of the study (the NTBR patients were more frequently excluded in high-quality studies) and the prevalence (NTBR patients were more frequently excluded in studies with a high prevalence). NTBR exclusion is suspected to be the main factor explaining the heterogeneity observed in the specificity. The association between specificity and prevalence or quality may be caused by the correlation with NTBR exclusion.
Sensitivity analysis showed that the conclusions of the meta-analyses were robust and not caused by a single study. Sensitivity and specificity did not vary by more than 10%, except for CURB score: the study by Ewig [32] has a lower sensitivity and higher specificity than do other studies, but only four studies were included in this analysis.
Discussion
In this systematic review of clinical prediction rules to predict severe CAP, PSI and CURB-65 have similar performances to identify patients requiring ICU admission. A PSI score of 4 or more is more sensitive (75% versus 56%) but less specific (47% versus 74%) than a CURB-65 score of 3 or more. These two scores, derived and validated to predict 30-day mortality, perform poorly to predict ICU admission, with an estimated AUC of 0.69. This performance is inferior to their original application: AUC for prediction of 30-day mortality was 0.80 in a recent systematic review [53].
Some explanations are available for this difference. These prediction rules, and especially the PSI, are heavily weighted by comorbidities and age and tend to consider as severe, patients in whom CAP is a terminal event. In many cohorts, the mortality rate is higher than the ICU admission rate, suggesting that an important proportion of patients with CAP die without being considered for ICU admission [21,39]. Age, a major component of these scores, is often negatively associated with ICU admission or intensive treatment [12,25,41] Exclusion of patients with therapeutic limitations may improve the specificity of these scores for ICU admission. In our heterogeneity analysis, PSI specificity increased from 45% to 56% when studies including NTBR patients were excluded (P = 0.008).
A new generation of scores, specifically developed to predict ICU admission, focuses on the severity of the pneumonia itself rather than on age and comorbid conditions. Overall, the performance of these scores seems superior to that of the PSI or CURB-65, particularly regarding specificity (90.1% and 90.5% for the ATS 2001 score and ATS/IDSA 2007 minor criteria versus 48.0% and 74.2% for PSI and CURB-65).
When considering scores derived over time, secular trends must be considered. Use of noninvasive ventilation (NIV) for severe CAP has increased over the last decade. This might have changed the proportion of patients receiving invasive mechanical ventilation. However, NIV was explicitly included in the definition of mechanical ventilation in most studies using that end point [10,25,29]. As the efficacy of NIV in alleviating respiratory failure for CAP patients is still debated, NIV is unlikely to have induced a major bias in the performance of the prediction rules over time. Furthermore, the principal scores (SCAP rule, SMART-COP, ATS 2007, and REA-ICU) have been proposed recently, at a time during which NIV for respiratory failure was routinely used.
Inclusion of major criteria in the ATS rules (mechanical ventilation and shock) improves their diagnostic performance but is not useful clinically, because these patients have an obvious indication for ICU admission. However, use of the minor criteria only does not seem to reduce the specificity of the ATS/IDSA 2007 score, as suggested by our results, with a pooled specificity of 90.5%. In a recent prospective cohort excluding patients with major criteria or therapeutic limitations, ATS-IDSA minor criteria had an AUC of 0.85 to predict ICU admission [50].
SMART-COP, REA-ICU, and SCAP scores seem to have operative characteristics similar to the ATS minor criteria but are less extensively validated. Also, confidence intervals are wide, and the use of different definitions of severe CAP limits comparison. Not surprisingly, these prediction rules share an important proportion of their predictive variables, as illustrated in Figure 2. Use of these three rules is more difficult than that of the ATS minor criteria, because of the weighting of the different predictive factors and the use of age-adjusted cut-offs.
Although the new generation of scores seems to have enhanced operative characteristics to predict ICU admission, their clinical utility is still debated. With a 10% prevalence of severe CAP and 57% sensitivity, even a specificity of 91% (as reached by the ATS-IDSA 2007 minor criteria) will lead to a positive predictive value of only 41%, leading to an important overuse of ICU resources. High negative predictive value is the most consistent finding among the different studies, suggesting that these scores could be more relevant to exclude the presence of a severe CAP than to aid in performing triage in patients for ICU admission. However, this high negative predictive value is mainly due to the low prevalence of severe patients. With a pooled sensitivity of 57%, the ATS-IDSA 2007 minor criteria would fail to identify almost one half of the patients with severe CAP, an unacceptably high proportion.
CAP is a complex and evolving inflammatory disease and critical clinical deterioration can result from various processes: respiratory failure, circulatory failure, destabilization of a preexisting comorbidity, appropriateness of initial antibiotic therapy, or hospital-acquired illnesses. It is not surprising that no single clinical rule has sufficient operating characteristics to be useful in this wide spectrum of evolution profiles.
The new generation of clinical prediction rules focuses on the early detection of respiratory and circulatory failure. Inclusion of various biomarkers such as procalcitonin [54], endothelin-1 [55], co-peptin [56], pro-atrial natriuretic peptide [57,58], or adrenomedullin [59] is hoped to improve this detection. Nevertheless, these biomarkers will probably fail to predict clinical deterioration due to hospital-acquired complications or decompensated comorbidities. It is even dubious whether they will detect circulatory or respiratory failure in patients admitted in the very early course of their disease.
In our view, rather than a definitive response to severity assessment, clinical prediction rules in patients with CAP should be considered an aid to clinical judgment particularly useful for less-experienced clinicians. Some of the included variables are consistently associated with a grim evolution, and their identification in an individual patient should alert for this possibility and trigger its timely reassessment and a thorough evaluation for intensive care or high-dependency-unit admission.
Strengths
Our review incorporates the most recent published studies and updates the systematic review by Chalmers et al. [60]. We also used somewhat different inclusion criteria and data analysis. We did not include subgroups of patients based on age or pathogen, leading to the noninclusion of three studies [61-63]. Among the 40 studies included in the two systematic reviews, 24 were included in both, 12 in our work only, and four in the study by Chalmers et al. only. We decided against aggregating different definitions of SCAP, in an attempt to limit heterogeneity, and computed the performances of the prediction rules for the different definitions of SCAP. We included large recent studies [49,50] and could estimate the pooled performance of the more-recent prediction rules, SMART-COP and SCAP score. This allows direct comparison between recent prediction rules. Although included studies differed partially between our systematic review and that by Chalmers et al., our final results are very similar, mutually strengthening their validity.
Limitations
An important limitation of systematic reviews is their dependence on the quality of the included studies. Although the majority of included studies were considered of good or moderate quality, several pitfalls remain in the prediction of severe CAP. First, as already discussed, two biases are highly prevalent in these studies: inclusion in the studied population of patients not at risk for ICU admission (patients with therapeutic limitations); and use as a predictor of a surrogate of the outcome (use of mechanical ventilation and vasopressors, which are universally delivered only in an intensive or intermediate care unit).
Second, no universally accepted definition exists of severe CAP. The most frequently used proxy, ICU admission, is heavily influenced by ICU beds availability, local ICU admission policy, or subjectivity of the ICU specialist's evaluation. Use of a subjective decision such as ICU admission as a gold standard might lead to circular reasoning, because a perfect rule would be the one fitting usual practice. However, alternative definitions of SCAP, such as receipt of intensive treatment, do not seem to modify importantly operative characteristics of the prediction rules [23].
Third, definition of a "false positive" ICU admission is unclear: some patients might benefit from ICU admission even if they are not receiving vasopressors or mechanical ventilation (for example, through better fluid resuscitation).
Fourth, some of the studied rules have been fully incorporated in expert society recommendations. This might lead to contamination of ICU admission practices, further leading to an overestimation of their accuracy.
Finally, major heterogeneity was present among included studies, limiting the validity of the meta-analysis.
Conclusions
PSI and CURB-65 do not have sufficient operating characteristics to be useful for making ICU triage decisions in severe CAP. Newer rules, specifically conceived to aid in identifying severe CAP, perform better but still have insufficient test characteristics to be a major help in everyday decisions. Recent clinical prediction rules should be considered an aid to clinical judgment to guide ICU admission in CAP patients. Clinical trials evaluating this issue should exclude patients who are not candidates for ICU admission and predicting factors that make ICU admission mandatory. Inclusion of new biomarkers, dynamic reassessment of the severity scores, and impact studies evaluating their use would deserve evaluation in future clinical research.
Key messages
• Identification of severe community-acquired pneumonia (SCAP) should allow admission of patients at the appropriate level of care.
• Traditional severity scores, the PSI and CURB 65, perform poorly to identify patients requiring ICU admission.
• New dedicated scores have better operative characteristics and could be useful adjuncts to clinical judgment.
Abbreviations
ATS: American Thoracic Society; AUC: area under the curve; CAP: community-acquired pneumonia; CURB: confusion, urea, respiratory rate, blood pressure; ICU: intensive care unit; IDSA: Infectious Disease Society of America; NIV: noninvasive ventilation; NTBR: not-to-be resuscitated; PSI: pneumonia severity index; ROC: receiver operating characteristic; SCAP: severe community-acquired pneumonia; SMART-COP: systolic blood pressure, multilobar infiltrate, albumin, respiratory rate, tachycardia, confusion, low oxygen, low pH.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
APe, CM, and NG designed the study. CM, NG, OG, and SC collected the data. APo and CC performed the statistical analysis. CM and NG wrote the draft. All authors critically revised the manuscript and approved the final version for publication.
Supplementary Material
Definition of the different scores. This file contains the detailed components and cut-offs values of the different prediction rules (PSI, CURB-65, ATS-2001, IDSA/ATS 2007, SCAP score, SMART-COP, and REA-ICU).
Forrest plots of sensitivity/specificity of the different scores to predict ICU admission. This file contains the Forrest plots of the eight meta-analyzed scores (PSI, CURB-65, CURB, CRB-65, SMART-COP, SCAP score, ATS-2001, and IDSA/ATS 2007) for the outcome ICU admission.
Study quality assessment. Global and detailed quality assessment for each included study is provided in this file.
Contributor Information
Christophe Marti, Email: christophe.marti@hcuge.ch.
Nicolas Garin, Email: nicolas.garin@hcuge.ch.
Olivier Grosgurin, Email: olivier.grosgurin@hcuge.ch.
Antoine Poncet, Email: antoine.poncet@hcuge.ch.
Christophe Combescure, Email: christophe.combescure@hcuge.ch.
Sebastian Carballo, Email: sebastian.carballo@hcuge.ch.
Arnaud Perrier, Email: arnaud.perrier@unige.ch.
References
- Marston BJ, Plouffe JF, File TM Jr, Hackman BA, Salstrom SJ, Lipman HB, Kolczak MS, Breiman RF. Incidence of community-acquired pneumonia requiring hospitalization: results of a population-based active surveillance study in Ohio: The Community-Based Pneumonia Incidence Study Group. Arch Intern Med. 1997;157:1709–1718. doi: 10.1001/archinte.1997.00440360129015. [DOI] [PubMed] [Google Scholar]
- Ewig S, Torres A. Severe community-acquired pneumonia. Clin Chest Med. 1999;20:575–587. doi: 10.1016/S0272-5231(05)70237-9. [DOI] [PubMed] [Google Scholar]
- Fine MJ, Auble TE, Yealy DM, Hanusa BH, Weissfeld LA, Singer DE, Coley CM, Marrie TJ, Kapoor WN. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997;336:243–250. doi: 10.1056/NEJM199701233360402. [DOI] [PubMed] [Google Scholar]
- Chalfin DB, Trzeciak S, Likourezos A, Baumann BM, Dellinger RP. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007;35:1477–1483. doi: 10.1097/01.CCM.0000266585.74905.5A. [DOI] [PubMed] [Google Scholar]
- Restrepo MI, Mortensen EM, Velez JA, Frei C, Anzueto A. A comparative study of community-acquired pneumonia patients admitted to the ward and the ICU. Chest. 2008;133:610–617. doi: 10.1378/chest.07-1456. [DOI] [PubMed] [Google Scholar]
- Renaud B, Santin A, Coma E, Camus N, Van Pelt D, Hayon J, Gurgui M, Roupie E, Herve J, Fine MJ, Brun-Buisson C, Labarere J. Association between timing of intensive care unit admission and outcomes for emergency department patients with community-acquired pneumonia. Crit Care Med. 2009;37:2867–2874. doi: 10.1097/CCM.0b013e3181b02dbb. [DOI] [PubMed] [Google Scholar]
- Niederman MS, Bass JB Jr, Campbell GD, Fein AM, Grossman RF, Mandell LA, Marrie TJ, Sarosi GA, Torres A, Yu VL. Guidelines for the initial management of adults with community-acquired pneumonia: diagnosis, assessment of severity, and initial antimicrobial therapy: American Thoracic Society, Medical Section of the American Lung Association. Am Rev Respir Dis. 1993;148:1418–1426. doi: 10.1164/ajrccm/148.5.1418. [DOI] [PubMed] [Google Scholar]
- Niederman MS, Mandell LA, Anzueto A, Bass JB, Broughton WA, Campbell GD, Dean N, File T, Fine MJ, Gross PA, Martinez F, Marrie TJ, Plouffe JF, Ramirez J, Sarosi GA, Torres A, Wilson R, Yu VL. Guidelines for the management of adults with community-acquired pneumonia: diagnosis, assessment of severity, antimicrobial therapy, and prevention. Am J Respir Crit Care Med. 2001;163:1730–1754. doi: 10.1164/ajrccm.163.7.at1010. [DOI] [PubMed] [Google Scholar]
- Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, Dowell SF, File TM Jr, Musher DM, Niederman MS, Torres A, Whitney CG. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(Suppl 2):S27–S72. doi: 10.1086/511159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles PG, Wolfe R, Whitby M, Fine MJ, Fuller AJ, Stirling R, Wright AA, Ramirez JA, Christiansen KJ, Waterer GW, Pierce RJ, Armstrong JG, Korman TM, Holmes P, Obrosky DS, Peyrani P, Johnson B, Hooy M, Grayson ML. SMART-COP: a tool for predicting the need for intensive respiratory or vasopressor support in community-acquired pneumonia. Clin Infect Dis. 2008;47:375–384. doi: 10.1086/589754. [DOI] [PubMed] [Google Scholar]
- Espana PP, Capelastegui A, Gorordo I, Esteban C, Oribe M, Ortega M, Bilbao A, Quintana JM. Development and validation of a clinical prediction rule for severe community-acquired pneumonia. Am J Respir Crit Care Med. 2006;174:1249–1256. doi: 10.1164/rccm.200602-177OC. [DOI] [PubMed] [Google Scholar]
- Renaud B, Labarere J, Coma E, Santin A, Hayon J, Gurgui M, Camus N, Roupie E, Hemery F, Herve J, Salloum M, Fine MJ, Brun-Buisson C. Risk stratification of early admission to the intensive care unit of patients with no major criteria of severe community-acquired pneumonia: development of an international prediction rule. Crit Care (London) 2009;13:R54. doi: 10.1186/cc7781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worster A, Carpenter C. Incorporation bias in studies of diagnostic tests: how to avoid being biased about bias. Canadian J Emerg Med. 2008;10:174–175. doi: 10.1017/s1481803500009891. [DOI] [PubMed] [Google Scholar]
- Hayden JA, Cote P, Bombardier C. Evaluation of the quality of prognosis studies in systematic reviews. Ann Intern Med. 2006;144:427–437. doi: 10.7326/0003-4819-144-6-200603210-00010. [DOI] [PubMed] [Google Scholar]
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moses LE, Shapiro D, Littenberg B. Combining independent studies of a diagnostic test into a summary ROC curve: data-analytic approaches and some additional considerations. Stat Med. 1993;12:1293–1316. doi: 10.1002/sim.4780121403. [DOI] [PubMed] [Google Scholar]
- Lamy O, Van Melle G, Cornuz J, Burnand B. Clinical management of immunocompetent hospitalized patients with community-acquired pneumonia. Eur J Intern Med. 2004;15:28–34. doi: 10.1016/j.ejim.2003.11.003. [DOI] [PubMed] [Google Scholar]
- Ewig S, Seifert K, Kleinfeld T, Goke N, Schafer H. Management of patients with community-acquired pneumonia in a primary care hospital: a critical evaluation. Respir Med. 2000;94:556–563. doi: 10.1053/rmed.1999.0775. [DOI] [PubMed] [Google Scholar]
- Neill AM, Martin IR, Weir R, Anderson R, Chereshsky A, Epton MJ, Jackson R, Schousboe M, Frampton C, Hutton S, Chambers ST, Town GI. Community acquired pneumonia: aetiology and usefulness of severity criteria on admission. Thorax. 1996;51:1010–1016. doi: 10.1136/thx.51.10.1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ananda-Rajah MR, Charles PGP, Melvani S, Burrell LL, Johnson PDR, Grayson ML. Comparing the pneumonia severity index with CURB-65 in patients admitted with community acquired pneumonia. Scand J Infect Dis. 2008;40:293–300. doi: 10.1080/00365540701663381. [DOI] [PubMed] [Google Scholar]
- Angus DC, Marrie TJ, Scott Obrosky D, Clermont G, Dremsizov TT, Coley C, Fine MJ, Singer DE, Kapoor WN. Severe community-acquired pneumonia: use of intensive care services and evaluation of American and British Thoracic Society diagnostic criteria. Am J Respir Crit Care Med. 2002;166:717–723. doi: 10.1164/rccm.2102084. [DOI] [PubMed] [Google Scholar]
- Brown SM, Jones BE, Jephson AR, Dean NC. Validation of the Infectious Disease Society of America/American Thoracic Society 2007 guidelines for severe community-acquired pneumonia. Crit Care Med. 2009;37:3010–3016. doi: 10.1097/CCM.0b013e3181b030d9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buising KL, Thursky KA, Black JF, MacGregor L, Street AC, Kennedy MP, Brown GV. A prospective comparison of severity scores for identifying patients with severe community acquired pneumonia: reconsidering what is meant by severe pneumonia. Thorax. 2006;61:419–424. doi: 10.1136/thx.2005.051326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buising KL, Thursky KA, Black JF, MacGregor L, Street AC, Kennedy MP, Brown GV. Identifying severe community-acquired pneumonia in the emergency department: a simple clinical prediction tool. Emerg Med Australas. 2007;19:418–426. doi: 10.1111/j.1742-6723.2007.01003.x. [DOI] [PubMed] [Google Scholar]
- Calbo E, Ochoa de Echaguen A, Rodriguez-Carballeira M, Ferrer C, Garau J. Hospital admission, duration of stay and mortality in community-acquired pneumonia in an acute care hospital: correlation between a pneumonia prognosis index and conventional clinical criteria for assessing severity. Enferm Infecc Microbiol Clin. 2004;22:64–69. doi: 10.1157/13056884. [DOI] [PubMed] [Google Scholar]
- Capelastegui A, Espana PP, Quintana JM, Areitio I, Gorordo I, Egurrola M, Bilbao A. Validation of a predictive rule for the management of community-acquired pneumonia. Eur Respir J. 2006;27:151–157. doi: 10.1183/09031936.06.00062505. [DOI] [PubMed] [Google Scholar]
- Chalmers JD, Singanayagam A, Hill AT. Systolic blood pressure is superior to other haemodynamic predictors of outcome in community acquired pneumonia. Thorax. 2008;63:698–702. doi: 10.1136/thx.2008.095562. [DOI] [PubMed] [Google Scholar]
- Davis JS, Cross GB, Charles PG, Currie BJ, Anstey NM, Cheng AC. Pneumonia risk stratification in tropical Australia: does the SMART-COP score apply? Med J Aust. 2010;192:133–136. doi: 10.5694/j.1326-5377.2010.tb03450.x. [DOI] [PubMed] [Google Scholar]
- Escobar GJ, Fireman BH, Palen TE, Gardner MN, Lee JY, Clark MP, Kipnis P. Risk adjusting community-acquired pneumonia hospital outcomes using automated databases. Am J Manag Care. 2008;14:158–166. [PubMed] [Google Scholar]
- Espana PP, Capelastegui A, Quintana JM, Bilbao A, Diez R, Pascual S, Esteban C, Zalacain R, Menendez R, Torres A. Validation and comparison of SCAP as a predictive score for identifying low-risk patients in community-acquired pneumonia. J Infect. 2010;60:106–113. doi: 10.1016/j.jinf.2009.11.013. [DOI] [PubMed] [Google Scholar]
- Ewig S, de Roux A, Bauer T, Garcia E, Mensa J, Niederman M, Torres A. Validation of predictive rules and indices of severity for community acquired pneumonia. Thorax. 2004;59:421–427. doi: 10.1136/thx.2003.008110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewig S, Ruiz M, Mensa J, Marcos MA, Martinez JA, Arancibia F, Niederman MS, Torres A. Severe community-acquired pneumonia: assessment of severity criteria. Am J Respir Crit Care Med. 1998;158:1102–1108. doi: 10.1164/ajrccm.158.4.9803114. [DOI] [PubMed] [Google Scholar]
- Feagan BG, Marrie TJ, Lau CY, Wheeler SL, Wong CJ, Vandervoort MK. Treatment and outcomes of community-acquired pneumonia at Canadian hospitals. CMAJ. 2000;162:1415–1420. [PMC free article] [PubMed] [Google Scholar]
- Frei CR, Burgess DS. Community-acquired pneumonia: objective criteria to predict severe disease. J Infect Dis Pharmacother. 2004;6:39–48. [Google Scholar]
- Garau J, Baquero F, Perez-Trallero E, Perez JL, Martin-Sanchez AM, Garcia-Rey C, Martin-Herrero JE, Dal-Re R. Factors impacting on length of stay and mortality of community-acquired pneumonia. Clin Microbiol Infect. 2008;14:322–329. doi: 10.1111/j.1469-0691.2007.01915.x. [DOI] [PubMed] [Google Scholar]
- Garcia-Vidal C, Fernandez-Sabe N, Carratala J, Diaz V, Verdaguer R, Dorca J, Manresa F, Gudiol F. Early mortality in patients with community-acquired pneumonia: causes and risk factors. Eur Respir J. 2008;32:733–739. doi: 10.1183/09031936.00128107. [DOI] [PubMed] [Google Scholar]
- Kamath A, Pasteur MC, Slade MG, Harrison BD. Recognising severe pneumonia with simple clinical and biochemical measurements. Clin Med. 2003;3:54–56. doi: 10.7861/clinmedicine.3-1-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liapikou A, Ferrer M, Polverino E, Balasso V, Esperatti M, Piner R, Mensa J, Luque N, Ewig S, Menendez R, Niederman MS, Torres A. Severe community-acquired pneumonia: validation of the Infectious Diseases Society of America/American Thoracic Society guidelines to predict an intensive care unit admission. Clin Infect Dis. 2009;48:377–385. doi: 10.1086/596307. [DOI] [PubMed] [Google Scholar]
- Man SY, Lee N, Ip M, Antonio GE, Chau SS, Mak P, Graham CA, Zhang M, Lui G, Chan PK, Ahuja AT, Hui DS, Sung JJ, Rainer TH. Prospective comparison of three predictive rules for assessing severity of community-acquired pneumonia in Hong Kong. Thorax. 2007;62:348–353. doi: 10.1136/thx.2006.069740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marrie TJ, Shariatzadeh MR. Community-acquired pneumonia requiring admission to an intensive care unit: a descriptive study. Medicine (Baltimore) 2007;86:103–111. doi: 10.1097/MD.0b013e3180421c16. [DOI] [PubMed] [Google Scholar]
- Phua J, See KC, Chan YH, Widjaja LS, Aung NW, Ngerng WJ, Lim TK. Validation and clinical implications of the IDSA/ATS minor criteria for severe community-acquired pneumonia. Thorax. 2009;64:598–603. doi: 10.1136/thx.2009.113795. [DOI] [PubMed] [Google Scholar]
- Putinati S, Ballerin L, Piattella M, Ritrovato L, Zabini F, Potena A. Clinical policy for management and risk stratification of community-acquired pneumonia in patients hospitalized on the basis of conventional admission criteria. Rec Progr Med. 2003;94:199–203. [PubMed] [Google Scholar]
- Renaud B, Coma E, Hayon J, Gurgui M, Longo C, Blancher M, Jouannic I, Betoulle S, Roupie E, Fine MJ. Investigation of the ability of the Pneumonia Severity Index to accurately predict clinically relevant outcomes: a European study. Clin Microbiol Infect. 2007;13:923–931. doi: 10.1111/j.1469-0691.2007.01772.x. [DOI] [PubMed] [Google Scholar]
- Riley PD, Aronsky D, Dean NC. Validation of the 2001 American Thoracic Society criteria for severe community-acquired pneumonia. Crit Care Med. 2004;32:2398–2402. doi: 10.1097/01.CCM.0000147443.38234.D2. [DOI] [PubMed] [Google Scholar]
- Roson B, Carratala J, Dorca J, Casanova A, Manresa F, Gudiol F. Etiology, reasons for hospitalization, risk classes, and outcomes of community-acquired pneumonia in patients hospitalized on the basis of conventional admission criteria. Clin Infect Dis. 2001;33:158–165. doi: 10.1086/321808. [DOI] [PubMed] [Google Scholar]
- Shah BA, Ahmed W, Dhobi GN, Shah NN, Khursheed SQ, Haq I. Validity of pneumonia severity index and CURB-65 severity scoring systems in community acquired pneumonia in an Indian setting. Indian J Chest Dis. 2010;52:9–17. [PubMed] [Google Scholar]
- van der Eerden MM, de Graaff CS, Bronsveld W, Jansen HM, Boersma WG. Prospective evaluation of pneumonia severity index in hospitalised patients with community-acquired pneumonia. Respir Med. 2004;98:872–878. doi: 10.1016/j.rmed.2004.02.022. [DOI] [PubMed] [Google Scholar]
- Fukuyama H, Ishida T, Tachibana H, Nakagawa H, Iwasaku M, Saigusa M, Yoshioka H, Arita M, Hashimoto T. Validation of scoring systems for predicting severe community-acquired pneumonia. Intern Med. 2011;50:1917–1922. doi: 10.2169/internalmedicine.50.5279. [DOI] [PubMed] [Google Scholar]
- Chalmers JD, Taylor JK, Mandal P, Choudhury G, Singanayagam A, Akram AR, Hill AT. Validation of the Infectious Diseases Society of America/American Thoratic Society Minor Criteria for Intensive Care Unit Admission in Community-Acquired Pneumonia Patients Without Major Criteria or Contraindications to Intensive Care Unit Care. Clin Infect Dis. 2011;53:503–511. doi: 10.1093/cid/cir463. [DOI] [PubMed] [Google Scholar]
- Putinati S, Ballerin L, Zabini F, Piattella M, Ritrovato L, Simoni M, Potena A. Predictive rules for prognosis in community-acquired pneumonia. Minerva Pneumol. 2005;44:85–91. [Google Scholar]
- Renaud B, Coma E, Labarere J, Hayon J, Roy PM, Boureaux H, Moritz F, Cibien JF, Guerin T, Carre E, Lafontaine A, Bertrand MP, Santin A, Brun-Buisson C, Fine MJ, Roupie E. Routine use of the Pneumonia Severity Index for guiding the site-of-treatment decision of patients with pneumonia in the emergency department: a multicenter, prospective, observational, controlled cohort study. Clin Infect Dis. 2007;44:41–49. doi: 10.1086/509331. [DOI] [PubMed] [Google Scholar]
- Chalmers JD, Singanayagam A, Akram AR, Mandal P, Short PM, Choudhury G, Wood V, Hill AT. Severity assessment tools for predicting mortality in hospitalised patients with community-acquired pneumonia: systematic review and meta-analysis. Thorax. 2010;65:878–883. doi: 10.1136/thx.2009.133280. [DOI] [PubMed] [Google Scholar]
- Schuetz P, Suter-Widmer I, Chaudri A, Christ-Crain M, Zimmerli W, Mueller B. Prognostic value of procalcitonin in community-acquired pneumonia. Eur Respir J. 2011;37:384–392. doi: 10.1183/09031936.00035610. [DOI] [PubMed] [Google Scholar]
- Schuetz P, Christ-Crain M, Zimmerli W, Mueller B. Repeated measurements of endothelin-1 precursor peptides predict the outcome in community-acquired pneumonia. Intensive Care Med. 2011;37:970–980. doi: 10.1007/s00134-011-2208-2. [DOI] [PubMed] [Google Scholar]
- Kruger S, Ewig S, Kunde J, Hanschmann A, Marre R, Suttorp N, Welte T. C-terminal provasopressin (copeptin) in patients with community-acquired pneumonia: influence of antibiotic pre-treatment: results from the German competence network CAPNETZ. J Antimicrob Chemother. 2009;64:159–162. doi: 10.1093/jac/dkp148. [DOI] [PubMed] [Google Scholar]
- Christ-Crain M, Breidthardt T, Stolz D, Zobrist K, Bingisser R, Miedinger D, Leuppi J, Tamm M, Mueller B, Mueller C. Use of B-type natriuretic peptide in the risk stratification of community-acquired pneumonia. J Intern Med. 2008;264:166–176. doi: 10.1111/j.1365-2796.2008.01934.x. [DOI] [PubMed] [Google Scholar]
- Kruger S, Ewig S, Kunde J, Hartmann O, Suttorp N, Welte T. Pro-atrial natriuretic peptide and pro-vasopressin for predicting short-term and long-term survival in community-acquired pneumonia: results from the German Competence Network CAPNETZ. Thorax. 2010;65:208–214. doi: 10.1136/thx.2009.121178. [DOI] [PubMed] [Google Scholar]
- Christ-Crain M, Morgenthaler NG, Stolz D, Muller C, Bingisser R, Harbarth S, Tamm M, Struck J, Bergmann A, Muller B. Pro-adrenomedullin to predict severity and outcome in community-acquired pneumonia [ISRCTN04176397] Crit Care. 2006;10:R96. doi: 10.1186/cc4955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chalmers JD, Mandal P, Singanayagam A, Akram AR, Choudhury G, Short PM, Hill AT. Severity assessment tools to guide ICU admission in community-acquired pneumonia: systematic review and meta-analysis. Intensive Care Med. 2011;37:1409–1420. doi: 10.1007/s00134-011-2261-x. [DOI] [PubMed] [Google Scholar]
- Spindler C, Ortqvist A. Prognostic score systems and community-acquired bacteraemic pneumococcal pneumonia. Eur Respir J. 2006;28:816–823. doi: 10.1183/09031936.06.00144605. [DOI] [PubMed] [Google Scholar]
- Kontou P, Kuti JL, Nicolau DP. Validation of the Infectious Diseases Society of America/American Thoracic Society criteria to predict severe community-acquired pneumonia caused by Streptococcus pneumoniae. Am J Emerg Med. 2009;27:968–974. doi: 10.1016/j.ajem.2008.07.037. [DOI] [PubMed] [Google Scholar]
- Feldman C, Alanee S, Yu VL, Richards GA, Ortqvist A, Rello J, Chiou CC, Chedid MB, Wagener MM, Klugman KP. Severity of illness scoring systems in patients with bacteraemic pneumococcal pneumonia: implications for the intensive care unit care. Clin Microbiol Infect. 2009;15:850–857. doi: 10.1111/j.1469-0691.2009.02901.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Definition of the different scores. This file contains the detailed components and cut-offs values of the different prediction rules (PSI, CURB-65, ATS-2001, IDSA/ATS 2007, SCAP score, SMART-COP, and REA-ICU).
Forrest plots of sensitivity/specificity of the different scores to predict ICU admission. This file contains the Forrest plots of the eight meta-analyzed scores (PSI, CURB-65, CURB, CRB-65, SMART-COP, SCAP score, ATS-2001, and IDSA/ATS 2007) for the outcome ICU admission.
Study quality assessment. Global and detailed quality assessment for each included study is provided in this file.