Abstract
Hip fracture is a significant health problem for older adults and generally requires surgery followed by intensive rehabilitation. Informal caregivers (CGs) can provide vital assistance to older adults recovering from hip fracture. Caregiving is a dyadic process that affects both CGs and care recipients (CRs). In a feasibility study, we assessed the effects of using a theory-based online hip fracture resource program for CGs on both CGs and CRs. In this article, we discuss our recruitment process and the lessons learned. Participants were recruited from six acute hospitals, and CGs used the online resource program for 8 weeks. A total of 256 hip fracture patients were screened, and 164 CRs were ineligible. CG screening was initiated when CRs were determined to be eligible. Among 41 eligible dyads, 36 dyads were recruited. Several challenges to the recruitment of these dyads for online studies were identified, including a low number of eligible dyads in certain hospitals and difficulty recruiting both the CR and the CG during the short hospital stay. Field nurses often had to make multiple trips to the hospital to meet with both the CR and the CG. Thus, when a subject unit is a dyad recruited from acute settings, the resources required for the recruitment may be more than doubled. These challenges could be successfully alleviated with careful planning, competent field staff members, collaboration with hospital staff members, and efficient field operations.
Keywords: Recruitment, Online Studies, Dyads, Caregivers, Hip Fracture
The older adult population in the United States has grown rapidly, reaching approximately 38 million adults (13% of the population) aged 65 or older in 2007 (Galson, 2009; National Family Caregivers Association, 2010). Recent advancements in healthcare have prolonged the life expectancy of individuals, creating a larger number of older adults living with chronic conditions. Traditionally, family members and significant others have assumed the role of the caregiver (CG) for older adults. Compared to formal CGs (i.e., healthcare providers), these CGs, referred to as informal CGs, provide uncompensated care for their care recipients (CRs) (Gould, 2004; National Family Caregivers Association, 2010). With the rapid growth of the older adult population, the demand for these “informal CGs” (herein will be referred to as “CGs”) has significantly increased.
Depending on the CRs’ health and functional status, CGs are involved in various care-related activities, such as the provision of physical care and emotional support, looking after CRs’ finances, and other logistical matters (Gould, 2004; Li, Melnyk, & McCann, 2004; Rabow, Hauser, & Adams, 2004; Wolff & Kasper, 2004). These caregiving situations can significantly influence the lives of CGs and their family members. In most caregiving studies, CRs are viewed as potential stressors for CGs, and research outcomes tend to focus on the impact of this stress on CGs (Lyons, Zarit, Sayer, & Whitlatch, 2002; Pruchono, 1997). Caregiving, however, is a dyadic process involving both the CG and the CR. In fact, caregiving experiences may result in stress for the CR as well as the CG or may result in positive outcomes, such as strengthening the relationships within the dyad (Balducci, et al., 2008; Clemmer, Ward-Griffin, & Forbes, 2008) or building resilience and a sense of empowerment and self-efficacy (Shawler, 2006).
When older adults experience acute illnesses requiring extensive rehabilitation therapies and/or lifestyle modifications, the role of the CG is particularly important. As older adults transition through different healthcare settings and healthcare providers, CGs remain engaged through the entire recovery process and offer constant support (Lin & Lu, 2007; Macleod, Chesson, Blackledge, Hutchison, & Ruta, 2005). The importance of the CG’s role in the CR’s management of illnesses and adherence to guidelines has also been demonstrated in studies (Bogardus, et al., 2004; Clark & Dunbar, 2003). These findings demonstrate the importance of optimal CG support, which can be better understood by investigating its impact on the CG-CR dyad (Whitlatch, 2008).
Our investigative team conducted a feasibility study for a future trial that would test the effects of an online hip fracture CG resource program on both CR and CG health outcomes. In this study, we recruited older adult hip fracture CR-CG dyads in selected acute hospitals. During the trial, we encountered specific challenges in recruiting these dyads, including the small number of eligible dyads in certain hospitals, the CRs’ short length of stay, and the dyads’ high level of stress, as well as multiple tasks that the dyads needed to be engaged in after the CRs’ surgery. Those challenges were overcome by multiple strategies and provided us with valuable information in preparing for the future study. In this article, we discuss our recruitment process and the lessons learned.
Recruitment of Older Adult CR-CG Dyads in Acute Settings: Prior Findings
Recruitment of CR-CG Dyads
A few studies have investigated the impact of the CG’s role on the CR’s health outcomes. Bogardus et al. (2004) found that CGs’ agreement with treatment recommendations (e.g., medications, care planning) could promote patients’ adherence to those recommendations. Other studies have shown the effects of family-based approaches to improve the patients’ self-management and adherence to the recommended treatment (Clark & Dunbar, 2003). Thus the effects of CG support interventions could be better understood by investigating their impact on the CG-CR dyad (Whitlatch, 2008). There is, however, a lack of studies that assess outcomes of dyads, and prior findings suggest some difficulty in recruitment.
Generally, the number of available CR-CG dyads is much smaller than that of individual CRs or CGs because some CRs do not have available CGs and, even when they do, the CG and CR both must meet the eligibility criteria and be willing to participate. In a study that investigated the quality of life for stroke survivors and their CGs, 171 people who survived a stroke were approached; however, only 30 dyads (17.5%) were eligible and only 22 dyads participated (Adams, 2003). In another study that used a web-based support program for individuals with advanced cancer and their informal CGs, researchers found an unusually high decline rate (Buss, et al., 2008). During enrollment, a total of 896 patients with advanced cancer and their CGs were approached, and 452 (50.4%) dyads declined to participate. Of those approached, 96 patients (21.2%) later were ineligible. Interestingly, only 10.5% of dyads (n = 49) declined the study due to computer-related factors (e.g., uncomfortable with using or learning to use the web-based program) (Buss, et al., 2008). Other top reasons for decline included a lack of interest (29.6%, n = 134) and personal factors (22.8%, n = 103), such as time commitment, which is consistent with other studies (Ransom, Azzarello, & McMillan, 2006).
When the CRs are older adults, the availability of dyads is further decreased due to the CRs’ underlying medical conditions, such as comorbidities or the inability to perform certain activities (Lewis, et al., 2003; Witham & McMurdo, 2007). Prior findings also showed challenges with the recruitment of CGs of older adults (Amador, Travis, McAuley, Bernard, & McCutcheon, 2006; Gallagher-Thompson, Solano, Coon, & Arean, 2003; Murphy, et al., 2007; Steinhauser, et al., 2006). Many CGs take on caregiving responsibilities in addition to their significant obligations to their own family and full time job. Furthermore, many CGs of older adults have their own health problems (Steinhauser, et al., 2006). Thus, participation in trials can be viewed as an additional burden for those CGs.
Caregiving Research in Acute Settings
The majority of caregiving studies in older adults have focused on CGs of older adults with chronic illnesses, and the CGs were often recruited in community settings (Cassie & Sanders, 2008; Kim & Schulz, 2008; Washington, Meadows, Elliott, & Koopman, 2011). Many older adults, however, also experience acute illnesses or injuries, and their CGs often face the caregiving role without much preparation and have a great deal of support needs (Nahm, Resnick, Orwig, Magaziner, & Degrezia, 2010; Shyu, Chen, Wu, & Cheng, 2010).
Only few studies were conducted employing older adults and/or their CGs recruited from acute care settings. Most of those studies included patients with cardiac problems who tended to be middle age or young older adults, and the majority of their CGs were spouses (Broadbent, Ellis, Thomas, Gamble, & Petrie, 2009; Kukafka, Lussier, Eng, Patel, & Cimino, 2002; McCauley, 1995). For instance, in a randomized controlled trial (N = 223; mean age, 56.4 years), investigators tested the effect of an online health intervention program on participants who were admitted for acute coronary syndromes (Reid, et al., 2011). The intervention group received a personally tailored physical-activity plan upon discharge and had access to a secure website for activity planning and tracking. The findings showed superior outcomes for the intervention group at follow ups.
In another study (N = 57 spouses, mean age, 50), researchers assessed the effects of an in-hospital illness perception intervention session for myocardial infarction (MI) patients and their spouses. Findings showed that spouses in the intervention group had a better understanding of the illness, lower concern, and fewer questions about their partner's heart condition. The extent of care needed by the individuals admitted to the hospital due to acute heart problems is usually quite different from the care needed by older adult hip fracture patients. The CGs of hip fracture patients have to manage not only physical and emotional care, but also have to help their CRs transition through different care settings while receiving extensive rehabilitation. In addition, half of the CGs of hip fracture patients are children (48% in this study) of the patients, who have to juggle their own work and family lives. For these CGs online resource programs may be beneficial as they can be accessed without time and geographic limitation. Further studies are needed to identify optimal methods in delivering those interventions to the patients and their caregivers from the acute setting.
An Overview of the Study Design and Recruitment
Study design
The online hip fracture CG resource program included self-learning modules, moderated discussion boards, an Ask-the-Experts section, and a virtual library. The program was developed in conformance with the stress, appraisal, and coping theory (Lazarus, 1999; Lazarus & Folkman, 1984) and self-efficacy theory (Bandura, 1997a, 1998, 1997b). For the feasibility study, 36 CR-CG dyads were recruited from the six acute hospital settings. Upon admission to the study, both the patient and his/her CG completed the baseline survey. The CG then received an in-service about the online resource center and used it for 8 weeks. A follow-up survey was conducted on both the patient and CG at the end of 8 weeks.
Recruitment
The eligibility criteria for CRs included (1) being 50 years or older; (2) having had surgery for treatment of a hip fracture within 1 week of being screened; and (3) being able to perform activities of daily living independently before experiencing the hip fracture. A CR was excluded if he or she (1) was non-English speaking; (2) did not have a CG who met the CG inclusion criteria; (3) was institutionalized at the time of the fracture; or (4) had any serious psychiatric or additional medical conditions (e.g., cancer under active treatment, dementia, or chronic alcohol or narcotic abuse). A CG was eligible if he/she was (1) 21 years or older; (2) identified as a CG who provided the CR with the majority of assistance in personal care and household tasks during post-surgery recovery; (3) a resident of Maryland; (4) able to access the Internet (e.g., at home or libraries); (5) able to use the Internet on his/her own; and (6) able to achieve a score of at least 27 on the Mini-Mental State Examination (MMSE). A CG was excluded if he/she: (1) was non-English speaking; (2) required significant medical treatment (e.g., chemotherapy, radiation therapy, or hemo/peritoneal dialysis); (3) depended on the selected assistive devices for ambulation (e.g., a scooter, or wheelchair); or (4) had a CR who did not meet the inclusion criteria or who refused to participate.
Upon approval from all necessary Institutional Review Boards, initial recruitment began in three selected inner-city hospitals in Maryland in July 2008. Due to a lack of available participant dyads in those three, three additional hospitals were added from December 2008 to January 2009. Recruitment was completed in August 2009.
The first step in our dyad recruitment process was the identification of potentially eligible hip fracture patients. This was accomplished by trained field nurses, who visited hospitals and reviewed admission logs (specific HIPAA rules were followed for this process). Once a potential patient was identified, the field nurse went to the unit where the patient was admitted, communicated with the patient’s clinical staff, and visited the patient to explain the study. If the patient agreed to participate and gave permission to contact his/her CG, the research nurse contacted the CG and assessed his or her eligibility. If both the CR and CG met the eligibility criteria and agreed to participate, the nurse obtained consent from both the CR and CG.
Recruitment Results
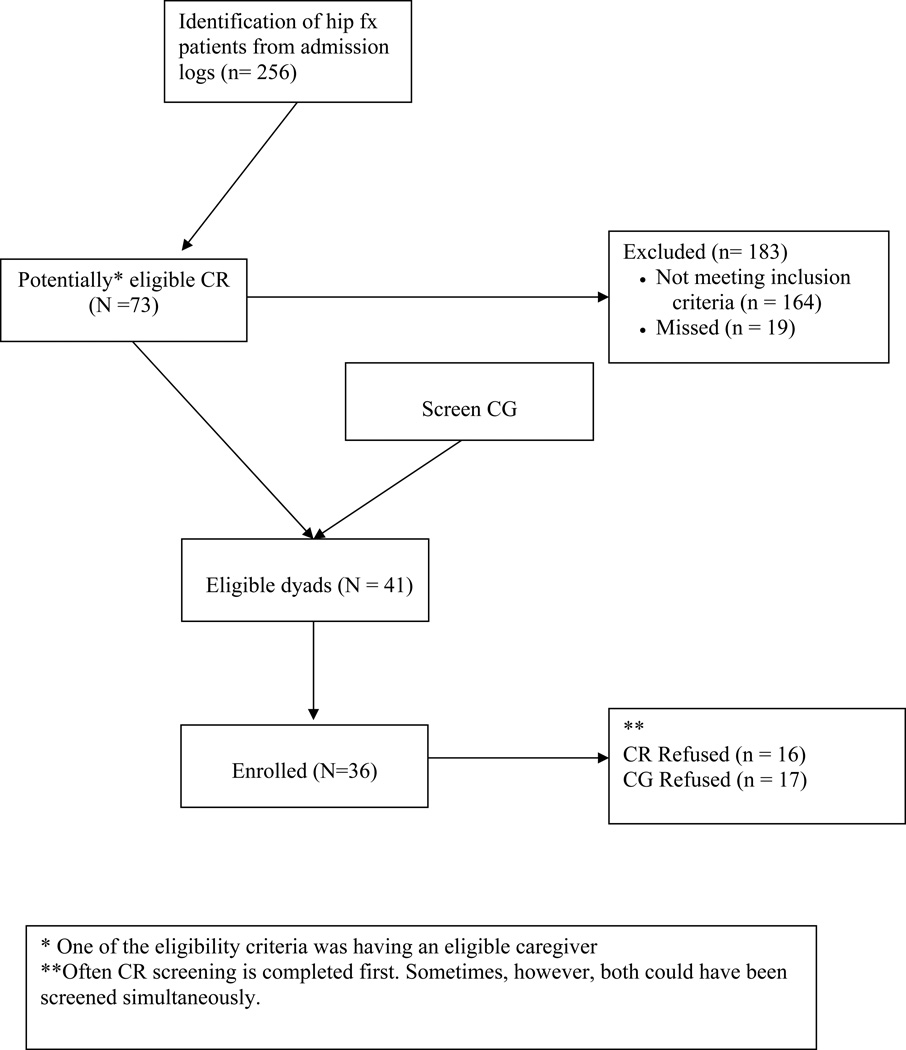
During the study period, a total of 256 hip fracture patients were identified. Among those, 164 patients were ineligible and 19 patients were discharged before eligibility status could be confirmed. Once the patient was deemed to be ineligible, the recruitment process stopped. A total of 41 dyads were eligible and 36 dyads were enrolled. (See Figure 1 for an enrollment flow diagram.)
Figure 1.
Dyad enrollment flow.
As shown in Table 1, the most frequent reasons for patients to be ineligible were serious comorbidities (n = 49), not having an eligible CG (n = 35), and not living in the community setting prior to the hip fracture (n = 28). Comparable CG ineligibility statistics are not available since CG screening was initiated only if the CR was determined to be eligible.
Table 1.
Ineligibility Reasons for Patients
| No. of Patients |
Criteria |
|---|---|
| 15 | Less than 50 years old |
| 19 | Did not receive a hip repair surgery or received a hip surgery without having a hip fracture |
| 16 | Unable to perform ADLs independently before experiencing the hip fracture |
| 8 | Unable to pass the Evaluation to Sign the Consent Form |
| 1 | Non-English speaking |
| 35 | CG does not meet the CG inclusion criteria |
| 28 | Was institutionalized at the time of the fracture |
| 49 | Had any of the following serious comorbidities -- a myocardial infarction or stroke concurrent with the hip fracture, schizophrenia, end stage renal disease, AIDS, cancer with metastasis or cancer under active treatment, dementia, or chronic alcohol or narcotic abuse |
Note: A patient could have met multiple ineligibility criteria.
Reasons for CR and/or CG refusal to participate in the study during the screening process, which occurred for 37 potentially eligible dyads, are presented in Table 2. The most frequent reasons for refusal for CRs were “not interested” (n = 10) and “concerned about CG burden” (n = 6), whereas the most frequent reason for CG refusal was “being too busy” (n = 12). Other reasons for CG refusal included concerns about additional burden and situations that required the CR’s readmission to the acute care hospital.
Table 2.
CR/CG Refusal
| Title | No. of participants |
Criteria |
|---|---|---|
| CR | 2 | Too busy |
| 10 | Not interested | |
| 6 | Concerned about CG burden | |
| 0 | Is participating in another study | |
| 9 | Other | |
| CG | 1 | No response |
| 12 | Too busy | |
| 3 | Not interested | |
| 9 | Other (e.g., CRs’ readmission to the hospital and too much stress due to the CR’s hospitalization) |
The majority of the CGs were female (n = 18, 67%), White (n = 24, 89%), and married (n = 22, 82%) and had at least some college education (n = 20, 74%). The mean age was 55.5 ± 12.7 years. A child of the CR assumed the CG role most frequently (n = 13, 48%), followed by the CR’s spouse (n = 10, 37%). One third (n = 9, 33%) were providing care to another person in addition to the CR. More than half (n = 14, 51.9%) were currently employed either part-time or full-time. The majority of the CGs owned a computer (n = 22, 81.5%). The average years of web experience was 11.7 ± 4.8 (range, 4 to 20), and the mean time spent using the web was 12.3 ± 11.07 hours per week (range, .5 to 50 hours). The majority of CRs were White (n = 24, 89%) and female (n = 27, 63%). The mean age was 73.96 ± 11.0 years. The majority (n = 21, 77.8%) of CRs had two or more comorbidities.
Lessons Learned: Challenges and Strategies
The recruitment of dyads is a stepwise process since it tends to begin with one party of the dyad, which then leads to the recruitment of the other party. Several challenges arose related to recruiting older adult hip fracture patients, and some were related to the recruitment of CGs. Others were related to the nature of online studies. When recruiting dyads, all of these factors interplay synergistically.
Identification of Eligible Dyads
Challenges
The first step for the recruitment of CR-CG dyads was the identification of potential hip fracture patients in hospitals. In our study, eligible patients were identified by the field nurses who visited hospitals and reviewed the admission logs. We selected this approach as opposed to other methods, such as having clinical staff make referrals or initiate the recruitment process (Buss, et al., 2008; Nichols, et al., 2004; Steinhauser, et al., 2006), because relying on primary care providers’ referrals might have resulted in missed opportunities. However, we found that locating family CGs often required additional assistance from the clinical staff since CGs were often not present when the research nurse visited the patient on the unit and the clinical staff tended to know their visiting schedules along with other useful information (e.g., if the CGs were from out of state).
Strategies
Informing necessary clinical staff about the study and establishing rapport between the study field staff and the clinical staff are critical in recruiting dyads. For instance, most hospitals use specific approaches in managing hip fracture cases, such as case management, and the persons who oversee these processes work closely with the CGs.
In our study, we identified a point person in each hospital who served as an advocate for the study. This person helped us understand how the hospital manages hip fracture care and helped us identify clinical staff involved in the care. To inform the staff about the study, we offered carefully planned inservices to all necessary staff. For instance, we found that although hip fracture patients were often admitted to surgery or orthopedic units, depending on the available beds, patients could be admitted to other units. Thus, staff on those units needed to be aware of our studies. In addition, care managers and/or social workers as well as physical and occupational therapists needed to be included in the inservices because they also worked with both hip fracture patients and their CGs. To include all of the necessary units in the inservices, we asked for guidance from the nursing administrators (e.g., directors or managers) and either invited the staff to our inservices or went to their staff meetings to present our studies. When the units were busy, our field staff members offered one-on-one inservices during the staff nurses’ breaks. We found that the research staff could establish a better rapport using this approach, but it took a great deal of resources.
Composite Eligibility Criteria for the Dyad
Challenges
During the early recruitment phase, we found that the number of eligible dyads in the selected three inner-city hospitals was smaller than expected. Those hospitals were selected based on their average yearly number of admissions due to hip fractures, their availability during the recruitment period, and the logistical aspects of the study’s field operation (e.g., the field nurse’s travel distance and time). We projected the number of eligible dyads from each hospital based on its admission statistics and the recruitment rates from previous hip studies conducted by the Baltimore Hip Study Group investigators (Magaziner, et al., 2006; Resnick, et al., 2007). However, many hip fracture patients from these hospitals were ineligible because they did not have eligible CGs (e.g., homeless, no CG) and/or did not meet other eligibility criteria (e.g., comorbidities). Thus, to expedite recruitment, three additional hospitals outside of the inner city area were added.
Strategies
Our investigative team confirmed the importance of monitoring and developing strategies for the recruitment process. This was especially helpful for recruiting dyads because the processes tended to be more complex. Maintaining close communication with the field staff and involving them in field operation meetings helped identify issues and strategies. For example, early identification of recruitment challenges in our inner-city hospitals led us to establish additional recruitment settings early in the trial. Although this addition required more resources (e.g., additional time from field nurses, efforts handling additional Institutional Review Board applications, and staff inservices), we were able to achieve the target sample size within the projected recruitment period.
Brief Hospital Length of Stay
Challenges
Hip fracture patients stay in the acute setting for only approximately 3 days, unless there are other health problems (Browner, 2003; Koval, Chen, Aharonoff, Egol, & Zuckerman, 2004; Morrison, Chassin, & Siu, 1988). During this short period, patients undergo a fast transition from the emergency room to the operation room and then onto the regular unit, where they begin therapy sessions. Simultaneously, CGs are busy taking care of their CRs. Enrollment of older adult hip fracture patients and their CGs in this acute phase is challenging and resource intensive. Usually our research nurse did not have an opportunity to introduce the study to the patient until the second visit. When a potential patient was identified, he/she was often in the operation room, exhausted from recovering from surgery, or being seen by a therapist. These factors greatly increased the amount of time the research nurses spent on recruitment, including travel time and downtime waiting for patients. In some cases, when the nurse visited the patient a second time, he/she had already been discharged.
Strategies
Support from the hospital staff was especially helpful in dealing with the patient’s short hospital stay and the dyads’ busy schedules (Buss, et al., 2008; Steinhauser, et al., 2006; Witham & McMurdo, 2007). For example, study point persons (e.g., care managers, social workers) in hospitals were instrumental because they had more interactions with CGs and could explain our study to them. They also tended to know the patients’ discharge date, which was important information for the field nurse when she needed to plan follow-up visits.
Caregivers’ Stress Level and Busy Schedule
Challenges
Caregivers of hip fracture patients face unique issues, starting with the initial shock of the event and suddenly having to rearrange their routine obligations to take care of their loved ones, which includes not only physical care but also other logistical responsibilities (e.g., managing hospital bills and arranging care after discharge). These CGs were stressed and physically and mentally exhausted. Thus, some CGs perceived participation in an online study to be an additional stressor and burden (Steinhauser, et al., 2006).
Although it would have been optimal if the research nurse could have explained the study and obtained consent from both the patient and his/her CG simultaneously, the CGs often were not present when the research nurse visited the patient. Thus, when the patient expressed interest in the study and met the inclusion criteria, the research nurse asked for permission to contact the CG and inquired about the best contact method (e.g., revisit the hospital, telephone calls to the CG). It often took multiple attempts to contact a CG, and several CGs required the nurse to come to their homes or offices.
Strategies
Field research nurses must be appropriately trained to understand the situation and make proper judgments when they approach participants (Leonard, et al., 2003; Livingston, Guest, Bateman, Woodcock, & Taylor, 1994). For instance, when the patient and CG look tired and/or are busy, the field research nurse may just introduce herself, show her understanding of the situation, and ask for a better time to return. Although this may increase the cost, it can yield a better recruitment. We found that even field research nurses who had more than 20 years of experience in recruiting older adult hip fracture patients needed additional training in the logistical aspects of recruiting dyads.
Our investigative team used a structured method of training field research nurses, including protocol instructions, scenario-based case studies, simulation of interview processes, and an orientation for each hospital. A training manual was developed, which included the research protocol, instruments, the instructions to administer the interview, and the scales that the research nurses could use for their interviews. The research nurses reviewed the manual prior to coming to orientation. The one-and-a half day orientation included the following content: (1) review of the protocol and instruments; (2) case scenarios that might occur during the data collection process; (3) simulation of the interview processes; (4) the questions and answers session; and (4) logistics (e.g., documentation of mileages, times, etc.). We found that experienced research nurses often had their own way of organizing field work and came with helpful suggestions. The research nurses simulated the interview process using “actors” (we used research associates), and their interviews were monitored by the primary investigator and the project manager. When the field work was initiated, the primary investigator and/or the project manager demonstrated the interview first and then observed the research nurses’ interview skills.
When following up with busy and stressed CGs, collaboration with the clinical staff proved to be helpful. For instance, care managers’ meetings with the CGs regarding the CRs’ care plans provided an excellent opportunity for the field research nurse to introduce the study. During the initial field operation meeting, we recognized that the efforts required for contacting the CGs were considerably greater than initially planned. To understand the complexity of the recruitment process, we had the field staff document the number of phone calls and visits required to recruit dyads and any accompanying information in a log. In our study, it took an average of 4.7 ± 2.9 phone calls and 3.4 ± 1.4 visits to recruit a single dyad.
Recruitment Tracking System/Enrollment Report
Tracking recruitment activities is critical, and a well-structured tracking form is very helpful. When the study unit is a dyad, the research team must be particularly careful in designing the form. The researchers must think through the recruitment process and the expected recruitment report data prior to the development of the form. Specific instructions and definitions of terms must accompany the form. For instance, in our study, screening occurred in multiple phases for each CR and CG, and the number of screened patients included all patients regardless of their completion status. Initially, our enrollment report form captured the eligibility of the dyads; however, we recognized the need for separate eligibility reports for each CR and CG. We added the CR eligibility report but could not add the CG report because we stopped the screening process when the patient was deemed to be ineligible.
Specific procedures were required for contacting CGs. For instance, the field nurse made three attempts by telephone to contact the CGs. If the CGs did not return the calls, the nurse confirmed the CG’s intention to participate in the study with the CR and determined the need for further follow up. The project manager made detailed notes whenever the field staff members had to make decisions about recruitment issues.
Online Study-Related Lessons Learned
In addition to the challenges in recruiting dyads, our study was an online study. Computer-related factors have been identified as barriers for participation in online studies (Dillman & Smyth, 2007; McNeill, Viswanath, Bennett, Puleo, & Emmons, 2007; Rainie, 2005). Considering the rapid growth of technology, however, this is becoming less of an issue. For instance, in a study that used a web-based support program for people with advanced cancer and their informal CGs, only 10.5% of dyads (n = 49) declined to participate in the study due to computer-related factors (Buss, et al., 2008), compared to 29.6% (n = 134) who declined the study due a lack of interest (29.6%, n = 134) and 22.8% (n = 103) who declined due to personal factors.
In this study, the major reason for refusal was “being too busy” (n = 12, 48%); only 3 (12%) refused because they were not interested in the study. A few CGs who did participate in the study indicated that the information from the program was very helpful; however, it was not easy to find the time needed for the study. Compared with our prior online studies (Nahm, et al., 2010; Nahm, Resnick, & & Mills, 2003), which used online recruitment strategies, participation in this study appeared to be perceived as more burdensome (Nahm, Resnick, & Gaines, 2004).
There seems to be a difference in perception of online interventions between online users recruited online versus those recruited face to face. This may be due to individuals recruited online being more comfortable with using computers as part of their daily routine. With the exploding popularity of online communication and Internet use, more CGs may participate in online studies in the near future.
Recruitment of Older Adult Hip Fracture CR-CG Dyads during the Acute Phase
Findings from this study shed important light on current research involving CGs of older adult patients who experience acute illnesses. Most prior caregiver studies have focused on CGs who take care of older adults with chronic illnesses or deteriorating conditions (Clemmer, et al., 2008; King, Hartke, & Denby, 2007; Mackenzie, et al., 2007; O'Connell, Baker, & Prosser, 2003; Steinhauser, et al., 2006), and the CGs were often recruited through provider referrals at home, or in the community (Clemmer, et al., 2008; King, et al., 2007; Mackenzie, et al., 2007; O'Connell, et al., 2003; Steinhauser, et al., 2006). Very little was known about the characteristics and support needs of CGs who take care of older adults in the acute phase. In particular, regaining baseline functions is often the major treatment goal in some acute illnesses, Caregivers who face those situations must be educated about the importance of and approaches to restorative care. Currently in health care, the length of stay in acute hospital settings is getting shorter, and the role of CGs in older adults’ health is becoming more important. It would be optimal for these CGs to be prepared to provide competent care. Considering the prevalent use of the Internet, online support programs offer an excellent opportunity to provide just-in-time support to these CGs. More studies need to be conducted to identify optimal types, avenues, and timing of the programs, as well as effective strategies to recruit participants to those studies.
Conclusion
This study’s findings on the recruitment of dyads consisting of hip fracture patients and their CGs for online CG support programs provide important information for future studies and help fill the gaps in current CG research. During the study, we identified specific challenges related to the complexity of identifying and recruiting eligible dyads, as well as constraints in online studies. In particular, researchers must be aware that when a study unit is an older adult CR-CG dyad and the dyads are recruited from acute settings, the resources required for recruitment could be more than doubled. These issues and budgetary constraints could be successfully alleviated with interdisciplinary collaboration, careful planning, and efficient field operations with specific protocols, as well as competent field staff members.
With the rapid growth and popularity of information communication technology, the use of online interventions can be beneficial for the CGs of older adults who experience hip fractures as they have a great deal of support needs. Although these CGs recognize the importance of resource programs, participation in online support studies could be perceived as additional burden when the dyads undergo stressful events in acute settings, such as surgery and transfers. Further studies are needed to investigate specific strategies to overcome theses barriers and to develop more usable programs to meet the dyads’ needs.
Acknowledgments
This study was supported by Grant R21AG029578 from the National Institute on Aging.
Contributor Information
Eun-Shim Nahm, University of Maryland School of Nursing, 655 W. Lombard St, Suite 455 C, Baltimore, MD 21201, Tel: (W) 410-706-4913 / FAX: 410-706-3289, enahm@son.umaryland.edu.
Denise Orwig, University of Maryland School of Medicine.
Barbara Resnick, University of Maryland School of Medicine.
Jay Magaziner, University of Maryland School of Medicine
Michele Bellantoni, Johns Hopkins University School of Medicine.
Robert Sterling, University of Maryland School of Medicine.
References
- Adams C. Quality of life for caregivers and stroke survivors in the immediate discharge period. Applied Nursing Research. 2003;16:126–130. doi: 10.1016/s0897-1897(03)00005-3. [DOI] [PubMed] [Google Scholar]
- Amador TK, Travis SS, McAuley WJ, Bernard M, McCutcheon M. Recruitment and retention of ethnically diverse long-term family caregivers for research. Journal of Gerontological Social Work. 2006;47(3–4):139–152. doi: 10.1300/J083v47n03_09. [DOI] [PubMed] [Google Scholar]
- Balducci C, Mnich E, McKee KJ, Lamura G, Beckmann A, Krevers B, et al. Negative impact and positive value in caregiving: validation of the COPE index in a six-country sample of carers. Gerontologist. 2008;48:276–286. doi: 10.1093/geront/48.3.276. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: The Exercise of Control. New York: Freeman; 1997a. [Google Scholar]
- Bandura A. Health promotion from the perspective of social cognitive theory. Psychological and Health. 1998;13:623–649. [Google Scholar]
- Bandura A, editor. Self-efficacy in Changing Societies. New York: Cambridge University Press; 1997b. [Google Scholar]
- Bogardus ST, Bradley EH, Williams CS, Maciejewski PK, Gallo WT, Inouye SK. Achieving goals in geriatric assessment: role of caregiver agreement and adherence to recommendations. Journal of the American Geriatrics Society. 2004;52(1):99–105. doi: 10.1111/j.1532-5415.2004.52017.x. [DOI] [PubMed] [Google Scholar]
- Broadbent E, Ellis CJ, Thomas J, Gamble G, Petrie KJ. Can an illness perception intervention reduce illness anxiety in spouses of myocardial infarction patients? A randomized controlled trial. Journal of Psychosomatic Research. 2009;67:11–15. doi: 10.1016/j.jpsychores.2008.11.006. [DOI] [PubMed] [Google Scholar]
- Browner BD, Jupiter JB, Levine AM, Trafton PG. Skeletal Trauma: Basic Science, Management, and Reconstruction. 3rd ed. Canada: Saunders; 2003. [Google Scholar]
- Buss MK, DuBenske LL, Dinauer S, Gustafson DH, McTavish F, Cleary JF. Patient/Caregiver influences for declining participation in supportive oncology trials. The Journal of Supportive Oncology. 2008;6(4):168–174. [PubMed] [Google Scholar]
- Cassie KM, Sanders S. Familial caregivers of older adults. Journal of Gerontological Social Work. 2008;50(Suppl 1):293–320. doi: 10.1080/01634370802137975. [DOI] [PubMed] [Google Scholar]
- Clark PC, Dunbar SB. Family Partnership Intervention: A Guide for a Family Approach to Care of Patients With Heart Failure. AACN Clinical Issues. 2003;14:467–476. doi: 10.1097/00044067-200311000-00008. [DOI] [PubMed] [Google Scholar]
- Clemmer SJ, Ward-Griffin C, Forbes D. Family members providing home-based palliative care to older adults: the enactment of multiple roles. Canadian Journal on Aging. 2008;27:267–283. doi: 10.3138/cja.27.3.267. [DOI] [PubMed] [Google Scholar]
- Dillman DA, Smyth JD. Design effects in the transition to web-based surveys. American Journal of Preventive Medicine. 2007;32(5 suppl):S90–S96. doi: 10.1016/j.amepre.2007.03.008. [DOI] [PubMed] [Google Scholar]
- Gallagher-Thompson D, Solano N, Coon D, Arean P. Recruitment and retention of latino dementia family caregivers in intervention research: issues to face, lessons to learn. Gerontologist. 2003;43:45–51. doi: 10.1093/geront/43.1.45. [DOI] [PubMed] [Google Scholar]
- Galson SK. [Retrieved September 10, 2011];Surgeon General's Perspectives: Self-Management Programs: One Way To Promote Healthy Aging. 2009 from http://www.surgeongeneral.gov/library/publichealthreports/sgp124-4.pdf.
- Gould DA. Family caregivers and the health care system. In: Levine C, Murrary T, editors. The Cultures of Caregiving. Baltimore, MD: The Johns Hopkins University Press; 2004. p. 1012. [Google Scholar]
- Kim Y, Schulz R. Family caregivers' strains: comparative analysis of cancer caregiving with dementia, diabetes, and frail elderly caregiving. J Aging Health. 2008;20:483–503. doi: 10.1177/0898264308317533. [DOI] [PubMed] [Google Scholar]
- King RB, Hartke RJ, Denby F. Problem-solving early intervention: a pilot study of stroke caregivers. Rehabilitation Nursing. 2007;32:68–76. doi: 10.1002/j.2048-7940.2007.tb00154.x. [DOI] [PubMed] [Google Scholar]
- Koval KJ, Chen AL, Aharonoff GB, Egol KA, Zuckerman JD. Clinical pathway for hip fractures in the elderly: The hospital for joint disease experience. Clinical Orthopedics and Related Research. 2004;1(425):72–81. doi: 10.1097/01.blo.0000132266.59787.d2. [DOI] [PubMed] [Google Scholar]
- Koval KJ, Chen AL, Aharonoff GB, Egol KA, Zuckerman JD. Clinical pathway for hip fractures in the elderly: The hospital for joint diseases experience. Clinical Orthopedics and Related Research. 2004;1(425):72–81. doi: 10.1097/01.blo.0000132266.59787.d2. [DOI] [PubMed] [Google Scholar]
- Kukafka R, Lussier YA, Eng P, Patel VL, Cimino JJ. Web-based tailoring and its effect on self-efficacy: results from the MI-HEART randomized controlled trial. Proceedings / AMIA Annual Symposium. 2002 [PMC free article] [PubMed] [Google Scholar]
- Lazarus R. Stress and Emotion: A new Synthesis. New York: Springer; 1999. [Google Scholar]
- Lazarus R, Folkman S. Stress, Appraisal, and Coping. New York: Springer; 1984. [Google Scholar]
- Leonard NR, Lester P, Rotheram-Borus MJ, Mattes K, Gwadz M, Ferns B. Successful recruitment and retention of participants in longitudinal behavioral research. AIDS Education & Prevention. 2003;15:269–281. doi: 10.1521/aeap.15.4.269.23827. [DOI] [PubMed] [Google Scholar]
- Lewis JH, Kilgore ML, Goldman DP, Trimble EL, Kaplan R, Montello MJ, et al. Participation of patients 65 years of age or older in cancer clinical trials. Journal of Clinical Oncology. 2003;21:1383–1389. doi: 10.1200/JCO.2003.08.010. [DOI] [PubMed] [Google Scholar]
- Li H, Melnyk BM, McCann R. Review of intervention studies of families with hospitalized elderly relatives. Journal of Nursing Scholarship. 2004;36:54–59. doi: 10.1111/j.1547-5069.2004.04011.x. [DOI] [PubMed] [Google Scholar]
- Lin PC, Lu CM. Psychosocial factors affecting hip fracture elder's burden of care in Taiwan. Orthopaedic Nursing. 2007;26:155–161. doi: 10.1097/01.NOR.0000276964.23270.92. [DOI] [PubMed] [Google Scholar]
- Livingston PM, Guest CS, Bateman A, Woodcock N, Taylor HR. Cost-effectiveness of recruitment methods in a population-based epidemiological study: the Melbourne Visual Impairment Project. Australian Journal of Public Health. 1994;18:314–318. doi: 10.1111/j.1753-6405.1994.tb00251.x. [DOI] [PubMed] [Google Scholar]
- Lyons KS, Zarit SH, Sayer AG, Whitlatch CJ. Caregiving as a dyadic process: perspectives from caregiver and receiver. Journals of Gerontology Series B-Psychological Sciences & Social Sciences. 2002;57:195–204. doi: 10.1093/geronb/57.3.p195. [DOI] [PubMed] [Google Scholar]
- Mackenzie A, Perry L, Lockhart E, Cottee M, Cloud G, Mann H. Family carers of stroke survivors: needs, knowledge, satisfaction and competence in caring. Disability & Rehabilitation. 2007;29(2):111–121. doi: 10.1080/09638280600731599. [DOI] [PubMed] [Google Scholar]
- Macleod M, Chesson RA, Blackledge P, Hutchison JD, Ruta N. To what extent are carers involved in the care and rehabilitation of patients with hip fracture? Disability & Rehabilitation. 2005;27:1117–1122. doi: 10.1080/09638280500056303. [DOI] [PubMed] [Google Scholar]
- Magaziner J, Wehren L, Hawkes WG, Orwig D, Hebel JR, Fredman L, et al. Women with hip fracture have a greater rate of decline in bone mineral density than expected: another significant consequence of a common geriatric problem. Osteoporosis International. 2006;17:971–977. doi: 10.1007/s00198-006-0092-3. [DOI] [PubMed] [Google Scholar]
- McCauley KM. Assessing social support in patients with cardiac disease. Journal of Cardiovascular Nursing. 1995;10:73–80. doi: 10.1097/00005082-199510000-00007. [DOI] [PubMed] [Google Scholar]
- McNeill LH, Viswanath K, Bennett GG, Puleo E, Emmons KM. Feasibility of using a web-based nutrition intervention among residents of multiethnic working-class neighborhoods. Preventing Chronic Disease. 2007;4(3):A55. [PMC free article] [PubMed] [Google Scholar]
- Morrison RS, Chassin MR, Siu AL. The medical consultant's role in caring for patients with hip fracture. Annals of Internal Medicine. 1988;128(12):1010–1020. doi: 10.7326/0003-4819-128-12_part_1-199806150-00010. [DOI] [PubMed] [Google Scholar]
- Murphy MR, Escamilla MI, Blackwell PH, Lucke KT, Miner-Williams D, Shaw V, et al. Assessment of caregivers' willingness to participate in an intervention research study. Research in Nursing & Health. 2007;30:347–355. doi: 10.1002/nur.20186. [DOI] [PubMed] [Google Scholar]
- Nahm E-S, Bausell B, Resnick B, Covington B, Magaziner J, Brennan PF. Effects of a Social Cognitive Theory Based Hip Fracture Prevention Website for Older Adults. CIN: Computers, Informatics, Nursing. 2010;28:371–379. doi: 10.1097/NCN.0b013e3181f69d73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahm E-S, Resnick B, Mills ME. A model of Computer-Mediated social Support Among Older Adults. AMIA Annual Symposium Proceedings. 2003:948. [PMC free article] [PubMed] [Google Scholar]
- Nahm E-S, Resnick B, Gaines J. Testing of the Reliability and Validity of the Computer-Mediated Social Support Measures Among Older Adults: a Preliminary Study. CIN: Computers, Informatics, Nursing. 2004;22:211–219. doi: 10.1097/00024665-200407000-00009. [DOI] [PubMed] [Google Scholar]
- Nahm ES, Resnick B, Orwig D, Magaziner J, Degrezia M. Exploration of informal caregiving following hip fracture. Geriatric Nursing. 2010;31:254–262. doi: 10.1016/j.gerinurse.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Family Caregivers Association. [Retrieved 2011, September 10];Who are America's Family Caregivers? 2010 from http://www.thefamilycaregiver.org/who_are_family_caregivers/
- Nichols L, Martindale-Adams J, Burns R, Coon D, Ory M, Mahoney D, et al. Social marketing as a framework for recruitment: illustrations from the REACH study. Journal of Aging & Health. 2004;16(5 Suppl):157S–176S. doi: 10.1177/0898264304269727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connell B, Baker L, Prosser A. The educational needs of caregivers of stroke survivors in acute and community settings. Journal of Neuroscience Nursing. 2003;35(1):21–28. doi: 10.1097/01376517-200302000-00006. [DOI] [PubMed] [Google Scholar]
- Pruchono RA, Burant CJ, Peters ND. Understanding the well-being of care receivers. The Gerontologist. 1997;37:102–109. doi: 10.1093/geront/37.1.102. [DOI] [PubMed] [Google Scholar]
- Rabow MW, Hauser JM, Adams J. Supporting family caregivers at the end of life: "they don't know what they don't know".[see comment] Jama. 2004;291(4):483–491. doi: 10.1001/jama.291.4.483. [DOI] [PubMed] [Google Scholar]
- Rainie L. [Retrieved May 10, 2010];What people do online. 2005 from http://www.pewinternet.org/Presentations/2005/What-people-do-online.aspx.
- Ransom S, Azzarello LM, McMillan SC. Methodological issues in the recruitment of cancer pain patients and their caregivers. Research in Nursing & Health. 2006;29:190–198. doi: 10.1002/nur.20129. [DOI] [PubMed] [Google Scholar]
- Reid RD, Morrin LI, Beaton LJ, Papadakis S, Kocourek J, McDonnell L, et al. Randomized trial of an internet-based computer-tailored expert system for physical activity in patients with heart disease. European Journal of Cardiovascular Prevention & Rehabilitation. 2011 doi: 10.1177/1741826711422988. [DOI] [PubMed] [Google Scholar]
- Resnick B, Orwig D, Yu-Yahiro J, Hawkes W, Shardell M, Hebel JR, et al. Testing the effectiveness of the exercise plus program in older women post-hip fracture. Annals of Behavioral Medicine. 2007;34:67–76. doi: 10.1007/BF02879922. [DOI] [PubMed] [Google Scholar]
- Shawler C. The empowerment of older mothers and daughters: rehabilitation strategies following a hip fracture. Geriatric Nursing. 2006;27:371–377. doi: 10.1016/j.gerinurse.2006.10.014. [DOI] [PubMed] [Google Scholar]
- Shyu YI, Chen MC, Wu CC, Cheng HS. Family caregivers' needs predict functional recovery of older care recipients after hip fracture. Journal of Advanced Nursing. 2010;66:2450–2359. doi: 10.1111/j.1365-2648.2010.05418.x. [DOI] [PubMed] [Google Scholar]
- Steinhauser KE, Clipp EC, Hays JC, Olsen M, Arnold R, Christakis NA, et al. Identifying, recruiting, and retaining seriously-ill patients and their caregivers in longitudinal research. Palliative Medicine. 2006;20:745–754. doi: 10.1177/0269216306073112. [DOI] [PubMed] [Google Scholar]
- Washington KT, Meadows SE, Elliott SG, Koopman RJ. Information needs of Informal Caregivers of Older Adults with Chronic Health Conditions. Patient Education & Counseling. 2011;83:37–44. doi: 10.1016/j.pec.2010.04.017. [DOI] [PubMed] [Google Scholar]
- Whitlatch C. Informal caregivers: communication and decision making. American Journal of Nursing. 2008;108(9 Suppl):73–77. doi: 10.1097/01.NAJ.0000336426.65440.87. [DOI] [PubMed] [Google Scholar]
- Witham MD, McMurdo ME. How to get older people included in clinical studies. Drugs & Aging. 2007;24:187–196. doi: 10.2165/00002512-200724030-00002. [DOI] [PubMed] [Google Scholar]
- Wolff JL, Kasper JD. Informal caregiver characteristics and subsequent hospitalization outcomes among recipients of care. Aging-Clinical & Experimental Research. 2004;16:307–313. doi: 10.1007/BF03324556. [DOI] [PubMed] [Google Scholar]