Abstract
Kawasaki disease (KD) is a systemic vasculitis of unknown etiology and a leading cause of acquired heart disease. It is assumed that there is an activation of the immune system by an infectious trigger in a genetically susceptible host. Neuroblastoma is the most common extracranial solid tumor in young children. It mainly originates from primordial neural crest cells that generate the adrenal medulla and sympathetic ganglia. A diagnosis of concurrent KD and neuroblastoma in a living child has been made in only one previous report. We report the second case and review the literature.
1. Introduction
Kawasaki disease (KD) is an acute vasculitis of childhood that predominantly affects the coronary arteries. The etiology of KD remains unknown; however, an infectious agent is strongly suspected based on clinical and epidemiologic features [1]. It typically affects children younger than 5 years of age. The peak age of incidence of KD is from 6 months to 2 years of age and it is rare in infants ≤3 months old [2]. The highest annual incidence rates of KD are reported from Japan with 206.2 and 239.6 per 100,000 children aged 0 to 4 years in 2009 and 2010, respectively [3].
Neuroblastoma is the most common extracranial solid tumor in children, accounting for 8% to 10% of all childhood cancers. The prevalence is about 1 case per 7,000 live births, and there are about 800 new cases of neuroblastoma per year in the United States [4, 5]. It is the most common cancer diagnosed during infancy and occurs most frequently in children less than 5 years of age, with a median age of 17 months at presentation [6]. We here report an extremely rare case of an infant diagnosed with concurrent Kawasaki disease and neuroblastoma.
2. Case Report
An 18-month-old girl was admitted to our infectious diseases department with a fever for 6 days and puffy red eyes. On physical examination, she was acutely ill, febrile, and irritable. Bulbar conjunctivitis, facial erythema at midline, red fissured lips, and a strawberry tongue were other significant findings (Figure 1(a)). There were also several small bilateral cervical lymphadenopathies, the greatest of which was 1.5 × 1.0 cm. On hospital day 2, mild swelling and desquamation developed on her hands and feet (Figure 1, inset). Transthoracic echocardiography demonstrated a 3 mm dilatation in her right coronary artery, and a diagnosis of Kawasaki disease was made.
Figure 1.
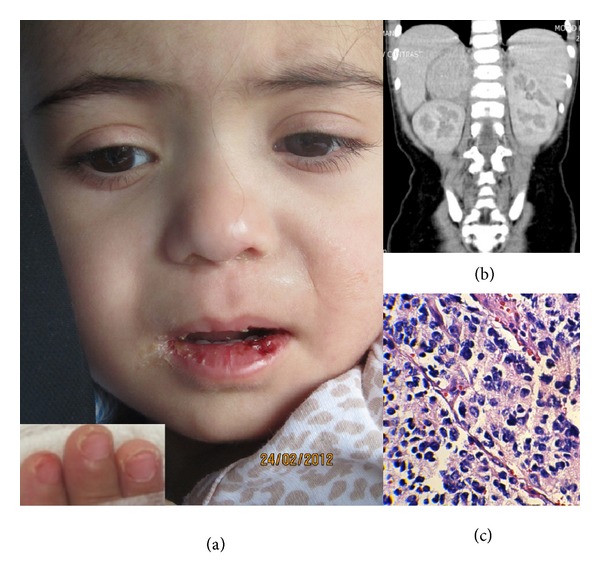
Clinical, radiographic, and pathologic features of a patient with concurrent Kawasaki disease and neuroblastoma. Red fissured lips (a) and desquamation of finger tips (inset). Computed tomography scan showing a mass originating from the right adrenal gland (b). Histopathology showing a tumor composed of predominantly atypical small round cells arranged in sheets, with pleomorphic nuclei, pink cytoplasm, and high mitotic indices (c).
She received 2 gr/kg intravenous immunoglobulin (IVIG) for two days as well as aspirin 80 mg/kg/day. Due to the persistence of fever, a computed tomography scan of the brain, chest, abdomen, and pelvis was performed, which was remarkable for a 3 cm × 3 cm abdominal mass originating from the right adrenal gland and with foci of calcification (Figure 1(b)). A 24-hour urine collection showed elevated vanillylmandelic acid levels at 8.5 mg/24 h (normal range: 2–5 mg/24 h). Exploratory laparatomy and total adrenalectomy without any gross residual tumor were performed. The pathology was reported as a stroma-poor undifferentiated neuroblastoma with unfavorable prognosis (Figure 1(c)). MYCN amplification by fluorescence in situ hybridization revealed 8 copy numbers of this oncogene. A bone scan as well as a bone marrow aspiration and biopsy were unremarkable. Three days after laparotomy, she developed periungual desquamation over the distal parts of her extremities. Chemotherapy with the N6 protocol (Cyclophosphamide/Adriamycin/Vincristine alternating with Cisplatin and VP-16) was initiated. The patient had an unremarkable course and repeat imaging three months later showing no evidence of residual tumor. The patient is free of tumor after 18 months at the time of the report of this case.
3. Discussion
Yanagisawa et al. reported a 6-month-old male infant who died of KD and had a small encapsulated mass in the left paravertebral region found on necropsy. The histopathological diagnosis was neuroblastoma [7]. In another study on autopsy results of 61 cases of KD who died between 2 months and 8 years after complete recovery of KD, one patient had a neuroblastoma on autopsy [8]. The case reported here is the second living child reported in the literature with concurrent KD and neuroblastoma. The only other available report is a 4-month-old boy with KD who developed acute urinary retention on the third day of admission and was later found to have a stroma-poor undifferentiated neuroblastoma [9]. Neuroblastoma is one of the malignancies in infants that may be diagnosed as an incidental finding by imaging studies [10, 11], like in our case. Adrenal incidentalomas are slightly more frequent in the right adrenal gland and in females [11]. Our patient was also a girl with a tumor originating from the right adrenal gland.
There are a few reports of cases with malignancy diagnosed following a diagnosis of KD. The malignancies reported are acute lymphoblastic leukemia in 3 cases, Hodgkin's disease in one case, osteosarcoma in one case, Schwannoma in one case, giant cell tumor of the tendon sheath in one case, and malignant reticuloma in one case [12, 13]. Alterations in the immune system have been postulated to underlie KD [14–16]. Whether such alterations predispose to certain types of malignancy as well is unclear. Larger epidemiological studies are required to determine whether the observed associations are mere coincidence or reflect true associations.
Disclosure
While this paper was under review, another report (Lim et al. Indian J Pediatr 2012 Dec) was published with two cases of concurrent KD and neuroblastoma, one in a 2-year-old girl and the other in a 3-year-old boy. Both cases presented with KD, and, after their fever did not respond to immunoglobulin, were discovered to have a paravertebral neuroblastoma and right adrenal neuroblastoma, respectively.
References
- 1.Freeman AF, Shulman ST. Kawasaki disease: summary of the American Heart Association guidelines. American Family Physician. 2006;74(7):1141–1150. [PubMed] [Google Scholar]
- 2.Lee EJ, Park YW, Hong YM. Epidemiology of Kawasaki disease in infants 3 months of age and younger. Korean Journal of Pediatrics. 2012;55:202–205. doi: 10.3345/kjp.2012.55.6.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nakamura Y, Yashiro M, Uehara R, et al. Epidemiologic features of Kawasaki disease in Japan: results of the 2009-2010 nationwide survey. Journal of Epidemiology. 2012;22(3):216–221. doi: 10.2188/jea.JE20110126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gurney JG, Davis S, Severson RK. Trends in cancer incidence among children in the U.S. Cancer. 1996;78:532–541. doi: 10.1002/(SICI)1097-0142(19960801)78:3<532::AID-CNCR22>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 5.Gurney JG, Ross JA, Wall DA, Bleyer WA, Severson RK, Robison LL. Infant cancer in the U.S.: histology-specific incidence and trends, 1973 to 1992. Journal of Pediatric Hematology/Oncology. 1997;19(5):428–432. doi: 10.1097/00043426-199709000-00004. [DOI] [PubMed] [Google Scholar]
- 6.London WB, Castleberry RP, Matthay KK, et al. Evidence for an age cutoff greater than 365 days for neuroblastoma risk group stratification in the Children’s Oncology Group. Journal of Clinical Oncology. 2005;23(27):6459–6465. doi: 10.1200/JCO.2005.05.571. [DOI] [PubMed] [Google Scholar]
- 7.Yanagisawa M, Kobayashi N, Matsuya S. Myocardial infarction due to coronary thromboarteritis, following acute febrile mucocutaneous lymph node syndrome (MLNS) in an infant. Pediatrics. 1974;54(3):277–280. [PubMed] [Google Scholar]
- 8.Tanaka N, Naoe S, Masuda H, Ueno T. Pathological study of sequelae of Kawasaki disease (MCLS). With special reference to the heart and coronary arterial lesions. Acta Pathologica Japonica. 1986;36(10):1513–1527. doi: 10.1111/j.1440-1827.1986.tb02823.x. [DOI] [PubMed] [Google Scholar]
- 9.Ohta S, Narita T, Kato H, Taga T, Takeuchi Y. A patient with kawasaki disease who developed acute urinary retention due to pelvic neuroblastoma. European Journal of Pediatrics. 2002;161(11):p. 631. doi: 10.1007/s00431-002-1050-5. [DOI] [PubMed] [Google Scholar]
- 10.Arnaldi G, Boscaro M. Adrenal incidentaloma. Best Practice & Research: Clinical Endocrinology & Metabolism. 2012;26:405–419. doi: 10.1016/j.beem.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 11.Mantero F, Terzolo M, Arnaldi G, et al. A survey on adrenal incidentaloma in Italy. Study Group on Adrenal Tumors of the Italian Society of Endocrinology. Journal of Clinical Endocrinology and Metabolism. 2000;85(2):637–644. doi: 10.1210/jcem.85.2.6372. [DOI] [PubMed] [Google Scholar]
- 12.Murray JC, Bomgaars LR, Carcamo B, Mahoney DH. Lymphoid malignancies following Kawasaki disease. American Journal of Hematology. 1995;50(4):299–300. doi: 10.1002/ajh.2830500414. [DOI] [PubMed] [Google Scholar]
- 13.Nakamura Y, Yanagawa H, Harada K, Kato H, Kawasaki T. Mortality among persons with a history of Kawasaki disease in Japan: the fifth look. Archives of Pediatrics and Adolescent Medicine. 2002;156(2):162–165. doi: 10.1001/archpedi.156.2.162. [DOI] [PubMed] [Google Scholar]
- 14.Lin CY, Lin CC, Hwang B, Chiang BN. The changes of interleukin-2, tumour necrotic factor and gamma-interferon production among patients with Kawasaki disease. European Journal of Pediatrics. 1991;150(3):179–182. doi: 10.1007/BF01963561. [DOI] [PubMed] [Google Scholar]
- 15.Rowley AH, Shulman ST. Pathogenesis and management of Kawasaki disease. Expert Review of Anti-Infective Therapy. 2010;8(2):197–203. doi: 10.1586/eri.09.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Onouchi Y, Gunji T, Burns JC, et al. ITPKC functional polymorphism associated with Kawasaki disease susceptibility and formation of coronary artery aneurysms. Nature Genetics. 2008;40(1):35–42. doi: 10.1038/ng.2007.59. [DOI] [PMC free article] [PubMed] [Google Scholar]


