Abstract
Background:
Facet cysts are implicated in neural compression in the lumbar spine. Surgery is the definitive treatment for symptomatic facet cysts since the failure rate for conservative treatment is quite high; however, the role of physical/manual medicine practitioners in the management of symptomatic facet cysts has not been well explored. This case report will add to the body of evidence of spontaneous resolution of symptoms associated with facet cysts in the chiropractic literature.
Case:
A 58 year old female presented with acute low back and right leg pain which she attributed to a series of exercise classes that involved frequent foot stomping. Physical examination did not elicit any objective evidence of radiculopathy but MRI and CT scans revealed a facet cyst impinging on the right L5 nerve root. Injections and surgery were recommended; however, the patient’s radicular symptoms completely resolved after three months without surgical intervention.
Summary:
There is currently a paucity of data in the literature regarding the chiropractor’s role in the management of symptomatic facet cysts. The case presented here has added to this literature and possible areas for future research have been explored.
Keywords: facet, cyst, lumbar spine
Abstract
Contexte :
Les kystes synoviaux lombaires sont impliqués dans la compression nerveuse au niveau du rachis lombaire. La chirurgie est le traitement définitif pour les kystes synoviaux lombaires symptomatiques puisque le taux d’échec du traitement conservateur est assez élevé, mais le rôle des médecins et des chiropraticiens dans la gestion de ces kystes n’a pas été suffisamment exploré. Cette étude de cas va enrichir l’ensemble de la preuve de la résolution spontanée des symptômes associés à des kystes synoviaux lombaires dans la documentation de la chiropratique.
Cas :
Une femme de 58 ans souffrant d’une douleur aiguë au niveau lombaire et à la jambe droite attribue cette douleur à une série de cours de conditionnement physique qui comportaient des trépignements fréquents. L’examen physique n’a révélé aucune preuve objective de radiculopathie, mais l’IRM et la tomodensitométrie ont révélé un kyste synovial lombaire qui pressait la racine nerveuse L5 droite. On a recommandé des injections et la chirurgie, mais les symptômes radiculaires du patient ont complètement disparu après trois mois, sans intervention chirurgicale.
Résumé :
Actuellement, il y a un manque de données dans la documentation concernant le rôle du chiropraticien dans la gestion des kystes synoviaux lombaires symptomatiques. Le cas présenté ici a enrichi ce corpus et a permis d’explorer des domaines possibles de recherches futures.
Keywords: facette, kyste, rachis lombaire
Introduction
Sciatica, defined as pain that radiates into the buttock, hip, and down one or both legs to the foot, affects only 10% of patients with low back pain1 but is a significant cause of pain and suffering in patients and a diagnostic challenge for clinicians. Lesions that are associated with sciatica that are being reported in increasing numbers are facet cysts, although this increased frequency is likely attributed to advances in imaging rather than a reflection of prevalence.2
Surgical excision has been recognized as the definitive treatment for symptomatic facet cysts.2,3,4 Conservative forms of treatment have not been as widely documented and the reported success rates have been substantially lower than that of surgery.3,4,5 Furthermore, management of symptomatic facet cysts in the chiropractic literature has been reported in only three cases.6,7 In order to better explore the chiropractor’s role in the management of facet cysts and to illuminate potential areas of research, more data must be documented regarding these lesions. This current paper will add to the body of evidence by presenting a case of spontaneously resolving symptoms associated with a facet cyst.
Case History
A 58 year old female presented to a private chiropractic clinic with a complaint of right sided lower back pain that began 5 days previously. The patient attributed the onset of her symptoms to a series of Qigong classes in which she was instructed to frequently stomp her feet. She had been taking these classes for one month prior to the onset of her symptoms. The pain was constant and described as dull in character. It was rated as 2 out of 10 on a Numeric Rating Scale with 0 being “no pain” and 10 being “pain as bad as it could be”. However, certain positions or movements (included sitting, standing, walking, twisting of the lumbar spine and transitioning between recumbent, sitting and standing positions) caused sharp radiating pain down the posterolateral aspect of her right leg to the plantar aspect of her right foot that was rated as 10/10 and would usually last for 15–20 minutes. None of these aggravating factors were consistent in causing the leg pain. Relief was obtained by lying down on her back; however the pain consistently caused her to wake up twice at night – once at approximately 2am and again at approximately 7am. She could not recall her sleeping position or any specific events that occur during these times. She denied any night sweats and did not report any recent weight loss, fever or trauma. Her medical history and systems review did not reveal any other past or present injuries or conditions and her family medical history was unremarkable.
The patient’s history revealed that she was otherwise healthy and did not smoke or drink any alcohol and was not on any medications. Her diet was vegetarian although she does eat fish. She had three adult children and all three pregnancies and births were uneventful. She was a dentist but was only working part time. Prior to the chiropractic session, she did not seek any other forms of treatment. She denied seeing any other chiropractors but opted to see one due to her daughter’s insistence.
Physical examination revealed a woman 5’1” tall weighing 110 lbs with anterior head carriage but otherwise no spinal antalgia. No muscle atrophy or trophic changes were observed in her lower limbs. Observation of gait revealed that she walked with a slight limp favouring the right side. She was able to walk on her heels and toes but had mild unsteadiness on her heels. Active ranges of motion of the lumbar spine were full in extension and lateral flexion to either side. Forward flexion was reduced by 25% and reproduced her radicular symptoms. Neurological examination revealed normal and symmetrical sensation, 5/5 muscle strength and 2+ reflexes at all levels in the lower extremities. Straight leg raise was 90° on the left and 70° on the right due to hamstring muscle tightness. However, there were no signs of nerve root tension or exacerbation of her right leg symptoms. The Figure 4 manoeuvre produced local back pain bilaterally. Thomas’ test (knee to chest manoeuvre) produced a pulling sensation in the lumbar spine. Posterior shear test8, Gaenslen’s test8 and Yeoman’s tests8 were non-provocative. Palpation of the right hamstring musculature revealed hypertonicity compared to the contralateral side. The lumbar paraspinal and gluteal muscles were normal in tone and bilaterally symmetrical.
Chiropractic care consisted of needle acupuncture, stretches for her hamstrings and gluteal muscles and a neurogliding technique for her sciatic nerve as described by Butler9. Within a few days of the initial treatment, the patient experienced intolerable pain and went to the emergency department where she was prescribed pain medications. Due to the patient’s symptoms of severe pain, her family physician requisitioned a CT scan and an MRI. The MRI revealed right L4–5 lateral recess narrowing secondary to facet changes, disc bulge and a small cystic lesion (Figure 1). A CT scan corroborated these findings and confirmed the presence of a 7mm synovial cyst impinging on the right L5 nerve root (Figure 2).
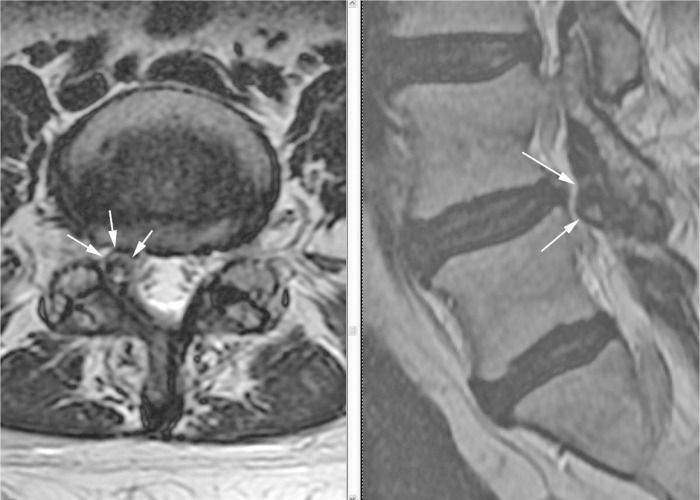
Figure 1.
Axial and parasagittal FRFSE (fast relaxation fast spin echo) T2 sequences show a cystic structure with hypointense rim and hyperintense content projecting ventrally from the right L4–5 facet joint and into the right lateral recess (white arrows). There is a mild disc bulge at this level (not visualized in this image).
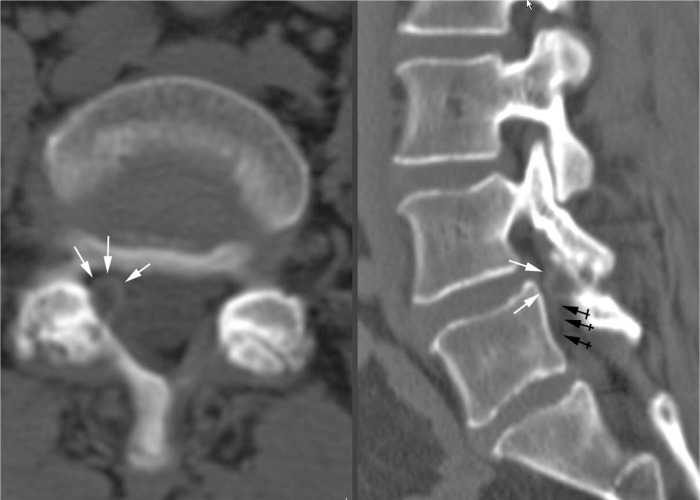
Figure 2.
Axial and reformatted right parasagittal CT views in bone windows show a juxtaarticular cyst with a thin rim of attenuated density (white arrows), occluding the right L5 lateral recess and compressing the right L5 nerve root (black arrows) anterior to a hypertrophied and narrowed right L4/5 facet joint with subchondral cystic changes.
A course of cortisone injections were recommended followed by surgical removal if the injections proved to be ineffective. The patient’s back pain was significantly exacerbated after the first injection however, so she refused any further medical interventions. She did not return to the initial chiropractor but sought acupuncture from a Traditional Chinese Medicine (TCM) provider for 6 sessions. In addition, she purchased an inversion table in order to self-administer gravity assisted traction. She did not find any of these treatment modalities helpful. The only relieving factor for her was Tai Chi. Three months after initial presentation, the patient reported that the radicular symptoms had completely resolved. At 2 years follow-up, she continued to be symptom free.
Discussion
The etiology of facet cysts remains unclear. Synovial cysts were originally described by Baker as resulting from degenerative processes in a joint.10 The most common explanation for cysts is that they frequently occur as a result of lumbar spine stress (excessive loading) in addition to a degenerative lesion of the soft lumbar tissue.11 It has been demonstrated that a statistically significant association exists between facet cysts and the frequency and severity of facet joint osteoarthritis and with spondylolis-thesis.3,12 Increased mobility of the involved joint appears to be an important precursor to the formation of the cysts. This notion is supported by the statistic that the majority of synovial cysts are found at the L4–L5 level which is considered the most mobile lumbar level.3,4
A literature search was conducted on MEDLINE using the search terms “synovial cyst” (MeSH and keyword) or “facet cyst” (keyword) combined with the following terms: “lumbosacral region” (MeSH); “spine” (MeSH and keyword); “lumbar” (keyword); “epidemiology” (MeSH and keyword); “therapeutics” (MeSH); “therapy” (keyword); “prognosis” (MeSH and keyword). The publication dates were from inception to 2011 with no limiters. Reference lists from articles were searched for additional pertinent studies.
Three articles were found in the literature pertaining to the epidemiology of facet cysts. One article retrospectively reviewed 303 consecutive MRI’s of patients referred primarily for back pain or radiculopathy at a single facility and found the prevalence of anterior lumbar facet cysts projecting into the vertebral canal to be 2.3%.12 A case series study reported that of 1800 CTs and MRIs of the lumbar spine, facet cysts were present in 0.6% of them.13 Another study identified 10 cysts in 2,000 reviews of CT lumbar spines.14 The majority of facet cysts occur in the lumbar spine, although rare cases of cervical and thoracic lesions have been reported.4
Patients with facet cysts are typically in their mid 60’s.3,4,11 Aside from the commonality of onset at an older age, facet cysts do not seem to exhibit any clinical symptoms that are specific to them. Low back pain is usually the initial symptom followed by unilateral or bilateral radicular pain. Neurogenic claudication is the next most common symptom. Sensory and motor deficits in a radicular distribution are found in less than half of patients3,4,11 whereas reflex changes are found in approximately 60% of patients15. Cauda equina syndrome may also occur; however, this is rare.3,4,11 If a cystic lesion is suspected, an MRI is considered the diagnostic imaging procedure of choice.3 On MRI, there is a well-defined rim that appears hypointense on all the MR sequences with contents that may be fluid, blood, air, calcification or fat.16
The most widely reported form of treatment for symptomatic facet cysts is surgery with the majority of the cases undergoing decompression (removing the thick, viscous contents of the cyst) or excision. Spinal fusion is sometimes performed but the value of this is still unclear.2 Khan reviewed 9 case series with a total of 460 patients and Epstein reviewed 14 case series with a total of 410 cases of facet cysts that were treated with laminectomy and resection.3,4 Follow-up times for the cases varied considerably, ranging from 3 months to 10 years and averaging at 6 months. Outcome measures were defined as: excellent (no residual symptoms/signs); good (mild residual symptoms/signs); fair (minimal to no improvement); and poor (worse). “Good” to “Excellent” outcomes were reported in 65 to 100 % of the cases. Complications of cyst recurrence, cerebrospinal fluid fistula, discitis, epidural hematoma, seroma, deep vein thrombosis and death were reported in a small percentage of the cases.3,4
Bydon reviewed 82 studies encompassing 966 patients who underwent surgery to determine postoperative symptomatic relief, recurrent back and leg pain and cyst recurrence after resection and decompression.2 The percentages of patients experiencing complete resolution of their back or leg pain after surgery were 92.5% and 91.1%, respectively with recurrence rates of 21.9% and 12.7%, respectively at a mean follow-up of 25.4 months. Same-level synovial cyst recurrence occurred in 1.8% of patients after decompression alone but 0% in patients who had decompression and fusion. Approximately 6% of patients required reoperation for correction of spinal instability and mechanical back pain.
A relatively small number of cases have been published about conservative approaches to symptomatic facet cysts in comparison to operative approaches. Khan reported on 3 case series with a total of 59 patients3 and Epstein reviewed 2 case series including 34 cases4 treated with steroid injections into the facet joints. Success rates ranged from approximately 33% to 43% after an average of 6 months of follow-up. Shah conducted a literature review of conservative treatments for facet cysts and found only 149 cases in total (this included 10 of the authors’ own cases).5 Conservative measures that were reported included facet injections, epidural injections, bed rest, oral analgesics, physical therapy, bracing and chiropractic care. A success rate of 53% was reported for the combined 149 cases. The endpoint used to determine failure of treatment was the need for subsequent surgery.5
Although surgery is currently considered the most successful treatment for symptomatic facet cysts, evidence is based solely on case reports. Moreover published cases of symptomatic facet cysts in the physical/manual medicine literature are rare.6,7 In order to provide guidance for clinical decisions such as effective treatment approaches (ranging from exercises to watchful waiting) and recommended wait times before surgical referral, population based studies and randomized clinical trials need to be conducted.
In the present case, the patient’s age of onset, non-specific clinical presentation, co-morbid imaging findings and location of the cyst at L4–L5 are consistent with previously published data. Although she had symptoms of pain radiating down her right leg, there were no objective findings in the physical examination to corroborate any radiculopathy. Previously published cases6,7,17,18,19 also lacked hard neurological findings. This could be indicative of a subgroup of patients with facet cysts that have a positive prognosis for symptom resolution. In addition, imaging studies revealed a facet cyst concomitant with facet degeneration and a disc bulge. Interestingly, lumbar disc lesions share a similar clinical presentation to facet cysts and the pathophysiology of both involve excessive mechanical loading of aberrant structures of the lumbar spine.15 It is therefore possible that rather than being discrete entities, disc herniations and facet cysts develop from a common underlying process. If this is the case, elucidating the process will help us to prevent or better manage these debilitating conditions.
After three months, the patient’s symptoms spontaneously resolved. This timeframe approximates what was reported in previous cases of resolving symptoms of facet cysts6,7,17,18 and may be suggestive of an appropriate period of watchful waiting. Despite multiple treatment modalities being used, the patient only reported relief with gentle exercises. Similar observations were reported by Taylor in which various modalities were used but the patient only responded to lumbar stabilization exercises.6 Cox’s multimodal treatment also included lumbar stabilization exercises but the effective/ineffective components of the treatment regimen were not delineated.7 Exercise therefore may be a key component of treating symptomatic facet cysts although there is insufficient information to specify what type of exercise.
This study has some limitations. Firstly, the patient sought multiple forms of treatment so it was difficult to determine which or if any of the modalities contributed to the resolution of her symptoms. Secondly, follow-up imaging was not performed to determine if the patient’s facet cyst had disappeared or if her symptoms merely resolved without any structural change. This would have further illuminated the link between imaging findings and symptoms.
Summary
Facet cysts are implicated in causing symptoms of back pain and radiculopathy in patients in their mid sixties. The current literature indicates that surgery is the most successful form of treatment for symptomatic facet cysts; however, there is a paucity of data in the physical/manual medicine literature regarding these lesions. The case presented here has added to be body of evidence for symptomatic facet cysts. Possible areas for future research have been explored.
References
- 1.Jarvik JG, Deyo RA. Diagnostic evaluation of low back pain with emphasis on imaging. Annals Int Med. 2002;137:586–97. doi: 10.7326/0003-4819-137-7-200210010-00010. [DOI] [PubMed] [Google Scholar]
- 2.Bydon A, Xu R, Parker S, et al. Recurrent back and leg pain and cyst reformation after surgical resection of spinal synovial cysts: systematic review of reported postoperative outcomes. Spine J. 2010;10:820–826. doi: 10.1016/j.spinee.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 3.Khan AM, Girardi F. Spinal lumbar synovial cysts. Diagnosis and management challenge. Eur Spine J. 2006;15:1176–1182. doi: 10.1007/s00586-005-0009-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Epstein NE. Lumbar synovial cysts: A review of diagnosis, surgical management, and outcome assessment. J Spinal Disord Tech. 2004;17:321–325. doi: 10.1097/01.bsd.0000096267.75190.eb. [DOI] [PubMed] [Google Scholar]
- 5.Shah RV, Lutz GE. Lumbar intraspinal synovial cysts: conservative management and review of the world’s literature. Spine J. 2003;3:479–488. doi: 10.1016/s1529-9430(03)00148-7. [DOI] [PubMed] [Google Scholar]
- 6.Taylor DN. Spinal synovial cysts and intersegmental instability: A chiropractic case. J Manipulative Physiol Ther. 2007;30:152–157. doi: 10.1016/j.jmpt.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 7.Cox JM, Cox JM., II Chiropractic treatment of lumbar spine synovial cysts: A report of two cases. J Manipulative Physiol Ther. 2005;28:143–147. doi: 10.1016/j.jmpt.2005.01.011. [DOI] [PubMed] [Google Scholar]
- 8.Magee DJ. Orthopedic physical assessment. 4th Edition. Philadelphia: Saunders; 2002. [Google Scholar]
- 9.Butler DS. Melbourne. Churchill Livingstone; 1991. Mobilisation of the nervous system. [Google Scholar]
- 10.Indar R, Tsiridis E, Morgan M, et al. Intraspinal lumbar synovial cysts: Diagnosis and surgical management. Surg J R Coll Surg Edinb Irel. 2004;2:141–44. doi: 10.1016/s1479-666x(04)80074-x. [DOI] [PubMed] [Google Scholar]
- 11.Christophis P, Asamoto S, Kuchelmeister K, Schachenmayr W. “Juxtafacet cysts”, a misleading name for cystic formations of mobile spine. Eur Spine J. 2007;16:1499–1505. doi: 10.1007/s00586-006-0287-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Doyle AJ, Merrilees M. Synovial cysts of the lumbar facet joints in a symptomatic population. Spine. 2004;29:874–878. doi: 10.1097/00007632-200404150-00010. [DOI] [PubMed] [Google Scholar]
- 13.Eyster EF, Scott WR. Lumbar synovial cysts: Report of eleven cases. Neurosurgery. 1989;24:112–115. doi: 10.1227/00006123-198901000-00021. [DOI] [PubMed] [Google Scholar]
- 14.Lemish W, Apsimon T, Chakera T. Lumbar intraspinal synovial cysts. Recognition and CT diagnosis. Spine. 1989;14:1378–1383. doi: 10.1097/00007632-198912000-00016. [DOI] [PubMed] [Google Scholar]
- 15.Adams MA, Roughley PJ. What is intervertebral disc degeneration, and what causes it? Spine. 2006;31:2151–2161. doi: 10.1097/01.brs.0000231761.73859.2c. [DOI] [PubMed] [Google Scholar]
- 16.Palmieri F, Cassar-Pullicino VN, Lalam RK, et al. Migrating lumbar facet joint cysts. Skeletal Radiol. 2006;35:220–26. doi: 10.1007/s00256-005-0072-2. [DOI] [PubMed] [Google Scholar]
- 17.Maezawa Y, Baba H, Uchida K, et al. Spontaneous remission of a solitary intraspinal synovial cyst of the lumbar spine. Eur Spine J. 2000;9:85–87. doi: 10.1007/s005860050016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mercader J, Gomez J, Cardenal C. Intraspinal synovial cyst: Diagnosis by CT-follow-up and spontaneous remission. Neuroradiology. 1985;27:346–348. doi: 10.1007/BF00339570. [DOI] [PubMed] [Google Scholar]
- 19.Swartz PG, Murtagh FR. Spontaneous resolution of an intraspinal synovial cyst. Am J Neuroradiol. 2003;24:1261–1263. [PMC free article] [PubMed] [Google Scholar]