Abstract
Ticagrelor, a novel reversible antiplatelet agent, has a Food and Drug Administration (FDA) black box warning to avoid maintenance doses of aspirin (ASA) >100 mg/daily. This restriction is based on the hypothesis that ASA doses >100 mg somehow decreased ticagrelor’s benefit in the Platelet Inhibition and Patient Outcomes (PLATO) U.S. cohort. However, these data are highly postrandomized, come from a very small subgroup in PLATO (57% of patients in the U.S. site), and make no biological sense. Moreover, the ticagrelor-ASA interaction was not significant by any multivariate Cox regression analyses. The Complete Response Review for ticagrelor indicates that for U.S. PLATO patients, an ASA dose >300 mg was not a significant interaction for vascular outcomes. In the ticagrelor-ASA >300 mg cohort, all-cause and vascular mortality were not significantly increased (hazard ratio [HR] 1.27 [95% CI 0.84–1.93], P = 0.262 and 1.39 [0.87–2.2], P = 0.170), respectively. Furthermore, for major adverse cardiovascular events (MACEs), 30-day all-cause mortality, and 30-day vascular mortality, the strongest interaction is the diabetes-ASA interaction. That is, patients who had diabetes had significantly fewer MACEs through study end (0.49 [0.34–0.63], P < 0.0001), significantly less 30-day all-cause mortality (0.33 [0.20–0.56], P < 0.0001), and significantly less 30-day vascular mortality (0.35 [0.22–0.55], P < 0.0001), respectively, when given high-dose (300–325 mg) ASA, regardless of treatment (clopidogrel or ticagrelor) assignment. The black box warning for the use of maintenance ASA doses >100 mg with ticagrelor is inappropriate for patients with diabetes and not evidence based.
Ticagrelor was compared with clopidogrel in the PLATO trial, which randomized 18,624 patients with acute coronary syndrome (ACS) to either ticagrelor (180 mg loading dose plus 90 mg twice daily maintenance dose) plus ASA versus clopidogrel (300–600 mg loading dose plus 75 mg once daily maintenance dose) plus ASA (1). Ticagrelor lead to a significant reduction in the primary end point (a composite of death from vascular causes, myocardial infarction, or stroke) compared with clopidogrel (9.8 vs. 11.7%; 95% CI 0.77–0.92, P < 0.001, respectively). Importantly, the benefit of ticagrelor was driven equally by the reduction of vascular death (P < 0.001) and myocardial infarction (P < 0.005), with 89 events favoring ticagrelor each, but not stroke (P = 0.22), with 19 fewer events in the clopidogrel arm (1).
A post hoc secondary analysis from the PLATO trial was undertaken to suggest that the increased use of ASA 300–325 mg (53.6%) in the U.S. compared with the rest of the world (1.7%) was the only factor to explain (out of 37 variables explored) the regional interaction that ticagrelor was less effective and potentially more harmful than clopidogrel (2). However, this interaction was not significant, is highly postrandomized, comes from a very small subgroup of PLATO, and makes no biological sense (3).
Ticagrelor-ASA hypothesis
The claimed ticagrelor-ASA interaction states that ticagrelor plus low-dose ASA is beneficial, whereas increasing doses of ASA in combination with ticagrelor produces adverse effects. Ticagrelor, having nearly complete P2Y12 platelet receptor blockade, does not exhibit the added antiaggregatory benefit derived from ASA, in contrast to what is seen with clopidogrel. Moreover, it is postulated that the incomplete and variable P2Y12 blockade seen with clopidogrel derives more benefit from ASA with less display of adverse effects. This hypothesis distinguishes between ASA-mediated effects in platelets versus targeting endothelial cells in the vessel wall; that is, in platelets, ASA’s inhibition of cyclooxygenase (COX)-1 causes a decrease in thromboxane A2 formation, inhibiting platelet aggregation. However, at higher doses, ASA also blocks the COX-2– mediated production of the vasodilator prostacyclin, causing an increase in vascular resistance.
The PLATO sponsor conducted a study in anesthetized dogs in an attempt to show vascular effects secondary to inhibition of prostacyclin production. The study showed no difference between ticagrelor and ASA compared with clopidogrel and ASA combination or ASA alone when absolute blood flow was examined. The FDA records indicate that “there is no clear explanation why ASA’s proposed inhibition of endothelial prostacyclin is able to outweigh ticagrelor’s, but not clopidogrel’s beneficial effects of thromboxane-A2 inhibition, platelet inhibition, and interactions with phosphodiesterase isoforms” (3). It is entirely unclear why ASA adds to the lower platelet inhibition produced by clopidogrel but not to the greater platelet inhibition produced by ticagrelor and why ASA’s ability at higher dosages to block COX-2–mediated production of the vasodilator prostacyclin produces vasoconstriction would only manifest in ticagrelor patients. In short, there is no clear explanation of why the reduced prostacyclin vasoconstriction should be relevant selectively and exclusively only to ticagrelor. The other major weakness of this hypothesis is that the platelet aggregation assay results aren’t consistent with the clinical bleeding rates in PLATO, for which higher ASA dosage is associated with more bleeding and likely a more additive effect upon bleeding with ticagrelor than with clopidogrel (3).
Ticagrelor-ASA interaction is not significant in PLATO short-term results but other interactions, including diabetes, are
The FDA Complete Response Review states that the most striking PLATO result was the reported long-term mortality benefit of ticagrelor. PLATO provides much less substantial evidence of short-term benefits and beneficial effects on thrombotic events. This combination of results is inconsistent with those of all earlier platelet inhibitor ACS trials, which have shown strong short-term benefits and smaller or no later benefits particularly regarding mortality. The ticagrelor-ASA interaction is not significant for the short-term results and not significant for mortality results regardless whether short- or long-term. The short-term results and mortality results demonstrate that three other interactions are more important and creditable than the ticagrelor-ASA interaction. These interactions are the following:
1) Patients with diabetes appear to benefit from higher ASA dosage regardless of treatment arm.
2) Ticagrelor interacts favorably with statins—or inappropriate restriction of statin dosages was detrimental to clopidogrel patients in PLATO.
3) Ticagrelor patients undergoing early percutaneous coronary intervention fare worse than clopidogrel patients.
The FDA transcript summarizes that when applying Cox regressions analyses the interaction term for ticagrelor and region is insignificant in all regressions. For short-term results there is no major U.S. versus rest of the world discrepancy that requires explanation. The interaction term for ticagrelor and ASA dosage is insignificant in all regressions. The short-term results do not support worse outcomes with higher ASA dosage in ticagrelor patients alone.
Ticagrelor-ASA interaction is significant for sponsor’s primary end point but a spurious correlation cannot be ruled out
The Complete Response Review states that the proposed ticagrelor-ASA interaction hypothesis suffers from many problems: the definition is not obvious, the determination is uncertain in many patients, the interaction is not consistent for various definitions and for different end points and time points, and the interpretation is flawed. For instance, it is unclear how the ASA dose has been defined since the mean, median, and the maximum doses were not matched. Another important issue is the time frame for which the ASA dose was used in the summary statistics, since it differs for the entire trial period: should the last 10 days, the last dose, or the loading ASA doses be considered? In fact, another statistical problem is the handling of the missed data. Since there are about a dozen variations to consider and analyze the effects of before choosing one, it should not be surprising that one, or more, associations may be “significant.” Importantly, the definition of ASA dosage is completely post hoc and derived after the study was unblinded and analyzed. Besides the definition not being obvious, there are problems with the PLATO determinations of ASA dosage. The FDA report indicates that some drugs (carbasalate [a calcium salt of acetylsalicylate used in Europe], anoprin [miscoded to chlorphenamine], and “inj loparin” [enoxaparin]) had been miscoded to ASA (3).
Finally, there is a converse problem with handling “missing” values. In PLATO, sites recorded concomitant drugs, including ASA, if the patient received the drug. There was no specific place to record that a drug was not given. Moreover, while examining the case report forms of patients without ASA records, there was not infrequently a statement recorded justifying why ASA was not given. These patients also had higher baseline rates of histories of gastrointestinal bleeding and peptic ulcer disease (3).
Conclusions
The aforementioned data clearly indicate that it is inappropriate to follow a black box warning for ASA dosages >100 mg with ticagrelor in patients with diabetes. A more plausible argument is that high-dose ASA improves clopidogrel benefit and may partially explain the disadvantage with ticagrelor versus clopidogrel in the U.S. Patients assigned to high-dose ASA (300–325 mg) in the randomized Clopidogrel Optimal Loading Dose Usage to Reduce Recurrent Events/Optimal Antiplatelet Strategy for Interventions (CURRENT-OASIS 7) trial had a significant reduction in recurrent ischemia (0.3 vs. 0.5%, P = 0.02) and all-cause mortality (2.2 vs. 2.5%, P = 0.1 [just missing statistical significance]) compared with low-dose (75–100 mg) ASA (4). Although high-dose ASA increased minor bleeds (5.0 vs. 4.4%, P = 0.04), it did not significantly increase major bleeding events. Thus, randomized evidence shows that high-dose ASA in the U.S. cohort would most likely have reduced mortality in the clopidogrel cohort rather than increased mortality in the ticagrelor cohort. The aforementioned data clearly indicate the inappropriateness of the statement that “ticagrelor’s benefit is diminished by high-dose ASA.” Clearly, evidence from CURRENT-OASIS 7 and the FDA Complete Response Review shows that the ticagrelor-ASA black box warning is not justifiable.
Patients with diabetes in PLATO had a significant reduction in MACE, 30-day all-cause mortality, and 30-day vascular mortality on high-dose ASA, regardless of treatment arm (HR 0.49 [95% CI 0.34–0.63], P < 0.0001; 0.33 [0.20–0.56], P < 0.0001; and 0.35 [0.22–0.55], P < 0.0001, respectively) (Table 1) (3). Patients with diabetes represent a sizeable cohort in ACS trials and comprised ∼25% of the entire PLATO population (1). It is a well-known phenomenon that patients with diabetes are more likely to be ASA resistant. Moreover, several trials have clearly indicated that diabetic patients who are ASA resistant on 75–100 mg of ASA can become responders to higher doses of ASA (5–7). Thus, a reduction in MACE, 30-day all-cause mortality, and 30-day vascular mortality with the use of high-dose ASA in patients with diabetes from the PLATO trial is consistent with a growing body of evidence. The PLATO diabetes-ASA interaction makes it highly inappropriate to recommend a black box warning for ASA doses >100 mg with ticagrelor.
TABLE 1.
Death rates based on potential ticagrelor interactions in the PLATO trial
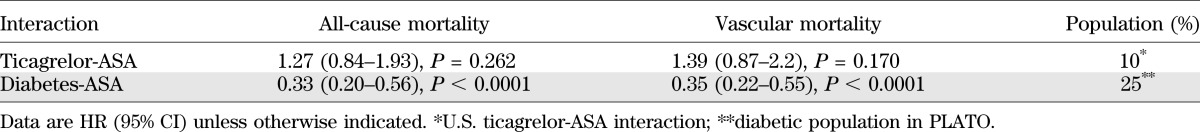
A limitation of a potential diabetes-ASA interaction is that evidence is based on postrandomization analyses. However, in the PLATO trial the interaction was highly significant, unlike the ticagrelor-ASA interaction. Furthermore, the diabetic population represented a much larger (25%) cohort of the PLATO population, whereas the U.S. ticagrelor-ASA interaction represents a much smaller percentage of PLATO (10%).
Should nondiabetic subjects receive low-dose ASA with ticagrelor? Or should patients with diabetes receive high-dose ASA with ticagrelor? Answers to these questions are not clear. Another trial, with random assignment of ASA dosages, is urgently needed to determine the appropriate ASA dose for the patient treated with ticagrelor. In summary, the black box warning for ASA dosages >100 mg with ticagrelor is inappropriate and unjustifiable, especially for patients with diabetes.
ACKNOWLEDGMENTS
V.L.S. is listed as an inventor for the issued U.S. patent “Treating vascular events with statins by inhibiting PAR-1 and PAR-4” (7,842,716) assigned to HeartDrug Research and has two pending applications: “Treating cardiac arrhythmias, heart failure, peripheral vascular disease, and stroke with cyclopentyl-triazolo-pyrimidine or derivative thereof” (U.S.N. 61/253,829), assigned to HeartDrug, and “Method for treatment of platelet activity with E5555” (U.S.N. 61/080,791), assigned to Eisai and HeartDrug. V.L.S. received funding for research studies with clopidogrel and E5555, and consultant fees from the manufacturers of both clopidogrel and ticagrelor. No other potential conflicts of interest relevant to this article were reported.
J.J.D. developed the concept and wrote the manuscript. V.L.S. developed the concept and edited the manuscript.
The authors thank C.M. Gibson (ATLAS ACS 2) and P. Tricoci (TRACER) for the trial data clarification.
Footnotes
See accompanying commentary, p. 709.
REFERENCES
- 1.Wallentin L, Becker RC, Budaj A, et al. PLATO Investigators Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 2009;361:1045–1057 [DOI] [PubMed] [Google Scholar]
- 2.Mahaffey KW, Wojdyla DM, Carroll K, et al. Ticagrelor compared with clopidogrel by geographic region in the Platelet Inhibition and Patient Outcomes (PLATO) Trial. Circulation 2011;124:544–554 [DOI] [PubMed]
- 3.U.S. Food and Drug Administration. Drug approval package: Brilinta (tricagrelor) tablets. Available from http://www.accessdata.fda.gov/drugsatfda_docs/nda/2011/022433Orig1s000TOC.cfm Accessed 10 May 2012
- 4.Mehta SR, Tanguay JF, Eikelboom JW, et al. Double-dose versus standard-dose clopidogrel and high-dose versus low-dose ASA in individual undergoing percutaneous coronary intervention for acute coronary syndromes (CURRENT-OASIS 7): a randomized factorial trial. Lancet 2010;376:1203–1205 [DOI] [PubMed] [Google Scholar]
- 5.Addad F, Chakroun T, Elalamy I, et al. Antiplatelet effect of once- or twice-daily ASA dosage in stable coronary artery disease patients with diabetes. Int J Hematol 2010;92:296–301 [DOI] [PubMed] [Google Scholar]
- 6.Mirkhel A, Peyster E, Sundeen J, et al. Frequency of aspirin resistance in a community hospital. Am J Cardiol 2006;98:577–579 [DOI] [PubMed] [Google Scholar]
- 7.Capodanno D, Patel A, Dharmashankar K, et al. Pharmacodynamic effects of different aspirin dosing regimens in type 2 diabetes mellitus patients with coronary artery disease. Circ Cardiovasc Interv 2011;4:180–187 [DOI] [PubMed] [Google Scholar]


