Abstract
Objective
To examine the proposed disruptive mood dysregulation disorder (DMDD) diagnosis in a child psychiatric outpatient population. Evaluation of DMDD included 4 domains: clinical phenomenology, delimitation from other diagnoses, longitudinal stability, and association with parental psychiatric disorders.
Method
Data were obtained from 706 children aged 6–12 years who participated in the Longitudinal Assessment of Manic Symptoms (LAMS) study (sample was accrued from November 2005 to November 2008). DSM-IV criteria were used, and assessments, which included diagnostic, symptomatic, and functional measures, were performed at intake and at 12 and 24 months of follow-up. For the current post hoc analyses, a retrospective diagnosis of DMDD was constructed using items from the K-SADS-PL-W, a version of the Schedule for Affective Disorders and Schizophrenia for School-Age Children, which resulted in criteria closely matching the proposed DSM-5 criteria for DMDD.
Results
At intake, 26% of participants met the operational DMDD criteria. DMDD+ vs DMDD– participants had higher rates of oppositional defiant disorder (relative risk [RR] = 3.9, P < .0001) and conduct disorder (RR = 4.5, P < .0001). On multivariate analysis, DMDD+ participants had higher rates of and more severe symptoms of oppositional defiant disorder (rate and symptom severity P values < .0001) and conduct disorder (rate, P < .0001; symptom severity, P = .01), but did not differ in the rates of mood, anxiety, or attention-deficit/hyperactivity disorders or in severity of inattentive, hyperactive, manic, depressive, or anxiety symptoms. Most of the participants with oppositional defiant disorder (58%) or conduct disorder (61%) met DMDD criteria, but those who were DMDD+ vs DMDD– did not differ in diagnostic comorbidity, symptom severity, or functional impairment. Over 2-year follow-up, 40% of the LAMS sample met DMDD criteria at least once, but 52% of these participants met criteria at only 1 assessment. DMDD was not associated with new onset of mood or anxiety disorders or with parental psychiatric history.
Conclusions
In this clinical sample, DMDD could not be delimited from oppositional defiant disorder and conduct disorder, had limited diagnostic stability, and was not associated with current, future-onset, or parental history of mood or anxiety disorders. These findings raise concerns about the diagnostic utility of DMDD in clinical populations.
Irritable mood and temper outbursts are common in youth referred for psychiatric treatment.1,2 They are also the core features of the proposed diagnosis disruptive mood dysregulation disorder (DMDD) in DSM-5.3 DMDD is characterized primarily by frequent, severe, recurrent temper outbursts and chronically irritable and/or angry mood, both of which must be present for at least a year. The DSM-5 Work Groups raised concerns that many youth with severe, nonepisodic irritable mood are inappropriately diagnosed with bipolar disorder.4 The DMDD diagnosis was constructed to capture the phenomenology of youth with severe, chronic irritability, with the goal of reducing the chance that youth with this phenotype would receive a bipolar diagnosis.
The DSM-5 Work Groups note that there is currently relatively limited research to support the DMDD diagnosis.4 Most available studies focus on an overlapping but not identical construct called severe mood dysregulation (SMD). SMD includes the core criteria of DMDD, but also requires symptoms of chronic hyperarousal such as insomnia, agitation, distractibility, racing thoughts, flight of ideas, pressured speech, and intrusiveness.5 Published research on SMD has primarily been from a carefully phenotyped cohort of 146 youth referred to the National Institute of Mental Health (NIMH) Intramural Program.6 The youth with SMD were predominantly male (66%) and had high lifetime rates of attention-deficit/hyperactivity disorder (ADHD; 85%), oppositional defiant disorder (86%), and anxiety disorders (58%). About 16% met lifetime criteria for major depressive disorder (MDD). The youth with SMD were shown to be different from youth with a specified phenotype of bipolar I disorder (requiring distinct episodes of manic symptoms, including either elated mood or grandiosity) on a number of domains, including lower familial rates of bipolar disorder, lower onset rates of manic and hypomanic episodes over prospective follow-up, and differences on several neuropsychological domains and measures of brain structure and functioning.6
Other studies relevant to the SMD/DMDD phenotype have been post hoc analyses of large datasets in which a retrospective diagnosis of SMD was derived from the existing phenotypic variables. In the Great Smoky Mountains Study, 1.8% of the sample met SMD criteria with severe functional impairment, which made it much more common than bipolar disorder (0.1% of the sample).7 The severely impaired SMD youth from this community sample were predominantly male (66%), but differed from those in the NIMH studies, as only about 32% met criteria for ADHD; 42%, for oppositional defiant disorder; and 21%, for any anxiety disorder. In addition, there was very little longitudinal stability of the SMD diagnosis (83% met SMD criteria at only 1 wave). A retrospective SMD diagnosis was applied to 4 large aggregated community samples and 2 large clinical samples, which were assessed using the NIMH Diagnostic Interview Schedule-IV.6 Preliminary analyses indicated that in the community samples, 15% of youth with oppositional defiant disorder met SMD criteria, as did about 25% of the youth with oppositional defiant disorder in the clinical samples.
Additional data specific to the DMDD diagnosis are needed; however, given the time constraints involved with the release of the upcoming DSM-5, carefully performed prospective studies are not possible. One way to evaluate DMDD is to take data from existing cohorts and retrospectively construct a DMDD diagnosis, similar to what was done for SMD. The Longitudinal Assessment of Manic Symptoms (LAMS) study is one source that can provide suitable data, as participants were sampled from all children presenting for new evaluation at 9 different university-affiliated clinics and were carefully assessed using semistructured interviews.
In order to evaluate the validity of the DMDD diagnosis, it is useful to keep in mind the 5 phases of systematic study proposed by Robins and Guze8 that are necessary to validate a particular diagnostic classification in psychiatry. Using the LAMS cohort, we can provide relevant data on 4 of these phases: (1) clinical description, (2) delimitation from other disorders, (3) follow-up study, and (4) family study. In this article, we examine the clinical phenomenology of LAMS participants who met a DMDD diagnostic phenotype at intake and evaluate whether the DMDD phenotype can be delimited from other diagnoses, is stable over a 2-year follow-up period, and predicts new onset of DSM-IV diagnoses. Lastly, we assess the association of the DMDD phenotype with parental history of different psychiatric disorders.
METHOD
Detailed description of the LAMS study methodology has been published previously.9,10 The LAMS study screened children presenting for initial psychiatric assessment at 9 outpatient clinics affiliated with 4 academic medical centers: Case Western Reserve University, Cincinnati Children's Medical Center, the Ohio State University, and the University of Pittsburgh Medical Center. The institutional review boards at each site approved all study procedures prior to commencing the study. Parents provided written consent to complete the screening procedure described below. Parents then provided written consent, and children assented to participate in the intake assessment and longitudinal study. The sample was accrued from November 14, 2005, to November 28, 2008.
Participant Ascertainment
Parents/guardians of eligible children who were new patients to LAMS outpatient clinics completed the Parent General Behavior Inventory 10-Item Mania Scale (PGBI-10M) to screen for elevated symptoms of mania (ESM).11 Total scores range from 0 to 30. Each patient whose parent or guardian rated the child at or above a score of 12 (ESM+) was invited to participate in the study. Subsequently, a smaller demographically matched comparison group of patients who scored 11 or lower (ESM–) was also enrolled.
To be eligible, patients must (1) not have received mental health treatment in the LAMS-affiliated outpatient clinics within the past year, (2) be 6–12 years of age, (3) speak English, (4) have an accompanying parent/guardian who speaks English, and (5) not have a sibling or other child in the same household who already participated in the LAMS screening.9
The PGBI-10M screen was completed by the parents/guardians of 2,622 children; 1,124 (43%) of the children screened ESM+. Of these, 621 (55%) decided to continue in the next study phases. There were no sociodemographic differences between children/families agreeing to enroll in the longitudinal study and those who did not. ESM–children were sampled with replacement, resulting in inclusion of 86 children without ESM.9
Intake Assessment
Diagnoses
Children and their parents/guardians completed the Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL)12 with additional depression and manic symptom items derived from the Washington University in St. Louis Kiddie Schedule for Affective Disorders and Schizophrenia (WASH-U K-SADS),13 as well as items to screen for pervasive developmental disorders. The resulting instrument, the K-SADS-PL-W, is a semistructured interview that assesses current and lifetime psychiatric diagnoses.
Unmodified DSM-IV diagnostic criteria were used, except the criteria for bipolar disorder not otherwise specified (NOS) from the Course and Outcome of Bipolar Youth study14 were applied: (1) elated mood plus 2 associated symptoms of mania (eg, grandiosity, decreased need for sleep) or irritable mood plus 3 associated symptoms, (2) change in functioning (increase or decrease), (3) the abnormal mood and associated symptoms must be present for a total of at least 4 hours within a 24-hour period, and (4) the participant must have had at least 4 days of meeting the above-noted criteria in his or her lifetime. Bipolar spectrum diagnoses included all participants who met criteria for cyclothymia, bipolar disorder NOS, or bipolar I or II disorder. All diagnoses were reviewed and confirmed by a licensed child psychiatrist or psychologist.
Symptomatic assessment
Mood symptoms were assessed in 2 ways: occurring specifically within the context of a mood episode (ie, “filtered” ratings) and irrespective of association with a distinct change in mood (“unfiltered” ratings). Filtered ratings were quantified using the K-SADS Depression Rating Scale–10 item15 and the K-SADS Mania Rating Scale16 constructed from the K-SADS-PL-W mood items. Unfiltered ratings were obtained regarding the past 2 weeks using the Young Mania Rating Scale17 and the Children's Depression Rating Scale-Revised (CDRS-R).18,19 As irritability is the primary symptom of the DMDD phenotype, we removed this item from the total scores so that we could look at nonoverlapping mood symptomatology.
Questionnaires assessed dimensions of nonmood symptoms. Parent-reported scores on the ADHD, oppositional defiant disorder, and conduct disorder subscales of the Child and Adolescent Symptom Inventory-4R (CAASI-4R)20 were examined. The parent-completed Screen for Child Anxiety Related Emotional Disorders (SCARED-P)21 quantified symptoms of anxiety over the past 6 months.
Functional assessment
Study interviewers completed the Children's Global Assessment Scale22 to quantify current impairment and most severe level of impairment over the participants’ lifetime.
Demographics and school and treatment history
These were obtained by direct interview of the primary caregiver.
Family history
The Family History Screen23 collected information on psychiatric disorders in the participants’ biological parents.
Longitudinal Follow-Up Assessments
The instruments from the intake assessment were repeated every 12 months. However, the time frame for lifetime measures (ie, past psychiatric diagnoses) was for the prior 12 months.
Retrospective DMDD Diagnosis
The operational definition of DMDD used the current ratings of the following items from the K-SADS-PL-W, resulting in criteria closely matching the proposed DSM-5 criteria.3
Severe recurrent temper outbursts. This criterion consisted of the “loses temper” item: “severe temper outbursts 2–5 times per week” at threshold.
Chronic irritability. This criterion consisted of both the “easily annoyed or angered” (“easily annoyed or angered daily or almost daily”) and “angry or resentful” (“angry or resentful daily or almost daily”) items at threshold.
Duration. Participants who completed the K-SADS-PL-W oppositional defiant disorder supplement were assessed for whether the symptoms were present for at least 6 months, independent of whether they met full criteria for oppositional defiant disorder. This duration differs from DMDD criterion D, which states that symptoms must be present for an interval of 12 or more months and that there cannot be 3 or more consecutive months during the interval when the person was without the symptoms of criteria A–C.
Impairment in more than 1 setting. The oppositional defiant disorder supplement determined whether impairment occurred in at least 2 settings.
Episodes of elated mood plus manic-specific symptoms lasting more than 1 day cannot be present. DMDD criterion H excludes participants with episodic manic symptoms lasting more than 1 day at a time, thus excluding youth with bipolar I or II disorders and potentially some with bipolar disorder NOS and cyclothymia. However, because whether the DMDD phenotype can be delimited from bipolar disorder (other than by using an exclusion criterion) is a question to be evaluated, participants with bipolar spectrum diagnoses were included in the DMDD group.
Symptoms are not occurring exclusively during a psychotic or mood disorder or are better accounted for by another disorder. LAMS interviewers rate symptoms in the oppositional defiant disorder section only if they do not occur exclusively during a psychotic or mood disorder or are clearly accounted for by another disorder.
The proposed DSM-5 criteria for DMDD specify that individuals meeting criteria for DMDD and oppositional defiant disorder should be given a diagnosis of DMDD. As a goal of these analyses is to evaluate whether DMDD can be delimited from existing DSM-IV diagnoses, this criterion was not applied.
One participant did not have complete information on duration and impairment and was excluded from analyses.
Statistical Analyses
Statistical analyses were performed using IBM SPSS version 20.0 (Armonk, New York). Univariate analyses used standard parametric (t, χ2) or nonparametric (Mann-Whitney U) tests. Multivariate logistic regression models were built with group (eg, DMDD+) as the outcome variable. Variables that had a potential association with the outcome variable at a level of P < .10 on the univariate tests were entered using a forward conditional method with P < .05 as criteria for entry and P > .10 for removal.24
For some analyses, participants with oppositional defiant disorder and participants with conduct disorder were pooled (indicated in the article by the phrase oppositional defiant disorder/conduct disorder).
RESULTS
Intake Assessment
Severe, recurrent temper outbursts were present in 52% of the LAMS sample, and chronic irritability was present in 35%. The DMDD phenotype was present in 26% (n = 184) of LAMS participants and was significantly more common in the ESM+ vs ESM– participants (28% vs 14%; relative risk [RR] = 1.99; 95% confidence interval [CI], 1.16–3.41; P = .006), so ESM status was included as a potential covariate in the multivariate models. An additional 5% (n = 34) of the sample had both severe, recurrent temper outbursts and chronic irritability, but did not meet full criteria for DMDD because they did not have impairment in 2 settings (n = 27), did not meet duration criteria (n = 3), or met neither the impairment nor duration criteria (n = 4).
Table 1 compares the 184 DMDD+ participants with the 522 DMDD– participants on factors measured at intake. DMDD+ participants did not significantly differ from DMDD– participants in the rates of bipolar spectrum diagnoses, any depressive disorders, MDD, or anxiety disorders. DMDD+ participants had higher rates of disruptive behavior disorders, dysthymia, elimination disorders, and ADHD as compared to the DMDD– group. In the multivariate model, only oppositional defiant disorder and conduct disorder remained significantly associated with DMDD (oppositional defiant disorder: Wald χ2 = 124, odds ratio [OR] = 68.7 [95% CI, 32.6–144.7], P < .0001; conduct disorder: Wald χ2 = 92, OR = 77.8 [95% CI, 32.0–189.1], P < .0001).
Table 1.
Factors at Intake by Disruptive Mood Dysregulation Disorder Status
| DMDD+ (n=184) | DMDD– (n = 522) | Test Statistic/Relative Risk (95% CI) | P Value | |
|---|---|---|---|---|
| Demographics | ||||
| Sex, male, % | 66 | 68 | 0.96 (0.86–1.09) | NS |
| Race, white, % | 59 | 66 | 0.89 (0.77–1.01) | .06 |
| Age, mean ± SD, y | 9.3 ± 1.8 | 9.5 ± 2.0 | t = 1.2 | NS |
| Lives with both biological parents, % | 28 | 34 | 0.84 (0.65–1.09) | NS |
| Primary caretaker education, % | ||||
| No or some high school | 13 | 10 | Z = 1.8 | .08 |
| GED or high school diploma | 25 | 26 | ||
| Some post–high school, no degree | 30 | 26 | ||
| Associate's degree or other post–high school certification | 21 | 17 | ||
| Bachelor's degree or higher | 12 | 21 | ||
| Diagnoses, % | ||||
| Any mood disorder | 44 | 39 | 1.13 (0.93–1.37) | NS |
| Any bipolar spectrum diagnosis | 24 | 23 | 1.06 (0.78–1.43) | NS |
| Bipolar I/II disorder | 9 | 11 | 0.78 (0.46–1.33) | NS |
| Cyclothymia/bipolar disorder NOS | 15 | 12 | 1.32 (0.87–2.00) | NS |
| Any depressive disorder | 20 | 17 | 1.21 (0.85–1.70) | NS |
| MDD | 7 | 7 | 0.92 (0.48–1.73) | NS |
| Dysthymic disorder | 4 | 2 | 2.84 (1.09–7.53) | .03 |
| Depressive disorder NOS | 9 | 8 | 1.15 (0.67–1.97) | NS |
| Oppositional defiant disorder or conduct disorder | 96 | 24 | 4.03 (3.44–4.70) | < .0001 |
| Oppositional defiant disorder | 78 | 20 | 3.94 (3.26–4.77) | < .0001 |
| Conduct disorder | 18 | 4 | 4.46 (2.66–7.53) | < .0001 |
| ADHD | 79 | 61 | 1.29 (1.17–1.43) | < .0001 |
| Any anxiety disorder | 20 | 20 | 0.96 (0.69–1.35) | NS |
| Psychotic disorder | 2 | 2 | 1.03 (0.34–3.25) | NS |
| Pervasive developmental disorder | 3 | 7 | 0.44 (0.19–1.02) | .04 |
| Elimination disorders | 25 | 18 | 1.39 (1.02–1.89) | .04 |
| Dimensional measures of psychopathology, mean ± SD | ||||
| YMRS total scorea | 15.5 ± 7.7 | 13.1 ± 8.0 | t = 3.5 | .0004 |
| CDRS-R total scorea | 33.3 ± 9.5 | 30.6 ± 10.2 | t = 3.2 | .002 |
| K-SADS Depression Rating Scale total score | 7.9 ± 5.7 | 6.6 ± 6.0 | t = 2.6 | .009 |
| K-SADS Mania Rating Scale total scorea | 10.8 ± 8.4 | 7.7 ± 8.0 | t = 4.4 | < .0001 |
| CAASI-4R subscale score | ||||
| ADHD—inattentive | 19.5 ± 6.1 | 17.4 ± 6.7 | t = 3.7 | .0001 |
| ADHD—hyperactive/impulsive | 17.9 ± 6.7 | 15.5 ± 6.9 | t = 4.1 | < .0001 |
| ADHD—combined | 37.4 ± 11.3 | 32.9 ± 12.1 | t = 4.4 | < .0001 |
| Oppositional defiant disorder | 19.2 ± 4.5 | 14.1 ± 6.0 | t = 12.0 | < .0001 |
| Conduct disorder | 8.2 ± 5.5 | 4.5 ± 4.5 | t = 8.2 | < .0001 |
| SCARED-P score | 18.2 ± 12.7 | 18.2 ± 14.1 | t = 0.0 | NS |
| Functioning | ||||
| CGAS score (current), mean ± SD | 50.7 ± 9.1 | 56.0 ± 10.3 | t = 6.6 | < .0001 |
| CGAS score (most severe past), mean ± SD | 47.7 ± 10.4 | 50.1 ± 9.6 | t = 2.3 | .024 |
| Ever repeated a grade, % | 16 | 17 | 0.96 (0.66–1.41) | NS |
| Ever received special education class or behavioral intervention in school, % | 28 | 30 | 0.93 (0.71–1.21) | NS |
| Lifetime treatment history, % | ||||
| Psychotropic medication | 59 | 62 | 0.95 (0.83–1.09) | NS |
| Psychiatric hospitalization | 10 | 9 | 1.18 (0.71–1.96) | NS |
Irritability item not included in the total score.
Abbreviations: ADHD = attention-deficit/hyperactivity disorder, CAASI-4R = Child and Adolescent Symptom Inventory-4R, CDRS-R = Children's Depression Rating Scale-Revised, CGAS = Children's Global Assessment Scale, CI = confidence interval, DMDD– = did not meet criteria for disruptive mood dysregulation disorder, DMDD+ = met criteria for disruptive mood dysregulation disorder, GED = General Equivalency Diploma, K-SADS = Schedule for Affective Disorders and Schizophrenia for School-Age Children, MDD = major depressive disorder, NOS = not otherwise specified, NS = nonsignificant, SCARED-P = Screen for Child Anxiety Related Emotional Disorders, YMRS = Young Mania Rating Scale.
On dimensional measures of psychopathology, DMDD+ youth had significantly higher total scores on the Young Mania Rating Scale, CDRS-R, and K-SADS Mania Rating Scale (all with the irritability item removed), the K-SADS Depression Rating Scale, and the CAASI-4R ADHD subscales and oppositional defiant disorder and conduct disorder scales. On multivariate analysis, only the CAASI-4R oppositional defiant disorder and conduct disorder total scores were significantly associated with DMDD (CAASI-4R oppositional defiant disorder: Wald χ2 = 45, OR = 1.16 [95% CI, 1.11–1.21], P < .0001; CAASI-4R conduct disorder: Wald χ2 = 6.1, OR = 1.05 [95% CI, 1.01–1.10], P = .01), along with nonwhite race becoming significantly associated with DMDD in the model (Wald χ2 = 5.2, OR = 1.58 [95% CI, 1.07–2.35], P = .02).
Youth with DMDD were more impaired than those without DMDD. However, they were not more likely to have repeated a grade, received special educational intervention, taken psychotropic medication, or have a history of inpatient psychiatric hospitalization.
Longitudinal Course
Participants who did not complete any follow-up assessments were less likely to live with both biological parents than those who did complete a follow-up assessment (20% vs 35%); otherwise, there were no significant demographic differences between groups. There were no differences among participants without follow-up versus those with follow-up in the rates of baseline depressive disorders, bipolar spectrum diagnoses, ADHD, anxiety disorders, psychotic disorders, or oppositional defiant disorder/conduct disorder or in baseline DMDD and ESM status.
The 12-month assessment was available for 525 participants (74% of the sample), with 21% meeting DMDD criteria. Of those meeting criteria for DMDD at intake, 53% continued to meet criteria at 12 months. Of the 111 participants who were DMDD+ at the 12-month assessment, 71 (64%) were DMDD+ at intake. For comparison, 85% of participants who met full criteria for ADHD at intake also did so at the 12-month follow-up.
Both 12-month and 24-month follow-up assessments were available in 433 participants (61% of the sample). Of those 433 participants, 172 (40%) met DMDD criteria for at least 1 assessment, including 27% of the ESM– subjects. Of those 172 participants who were DMDD+ at intake or follow-up, 90 (52%) met criteria at only 1 assessment, while 50 (29%) met criteria at 2 assessments and 32 (19%) met criteria for all 3 assessments. In comparison, of the participants who met criteria for ADHD at intake or follow-up, 18% met criteria at only 1 assessment; 21%, at 2 assessments; and 61%, at all 3 assessments.
In participants with both follow-up visits, DMDD at intake was not associated with new onset of bipolar spectrum diagnoses (including bipolar I and II disorders), depressive disorders (including MDD), anxiety disorders, psychotic disorders, or conduct disorder over follow-up (Table 2). A diagnosis of DMDD at either intake or follow-up was significantly associated with a diagnosis at intake or follow-up of oppositional defiant disorder/conduct disorder (71% of those with oppositional defiant disorder/conduct disorder had DMDD vs 3% without oppositional defiant disorder/conduct disorder; χ2 = 277, P < .0001) and ADHD (44% vs 23%; χ2 = 20.0, P < .0001), but not MDD (42% vs 38%, χ2 = 0.4, P = .52), any depressive disorder (44% vs 37%, χ2 = 2.0, P = .16), bipolar I and II disorders (41% vs 38%; χ2 = 0.4, P = .52), bipolar spectrum diagnoses (44% vs 36%; χ2 = 3.1, P = .08), any anxiety disorder (41% vs 38%; χ2 = 0.4, P = .52), or psychotic disorder (52% vs 38%; χ2 = 1.9, P = .17).
Table 2.
New Onset of Disorder at 12- or 24-Month Follow-Up by Disruptive Mood Dysregulation Disorder Status at Intake, %
| Disorder With New Onset at 12 or 24 Mo | DMDD+ at Intake | DMDD– at Intake | Relative Risk (95% CI) | P Value |
|---|---|---|---|---|
| Bipolar spectrum disorder | 8.5 | 10.1 | 0.84 (0.41–1.70) | NS |
| Bipolar I/II disorder | 5.5 | 8.0 | 0.69 (0.31–1.53) | NS |
| Depressive disorder | 11.3 | 9.1 | 1.26 (0.68–2.31) | NS |
| Major depressive disorder | 4.7 | 4.1 | 1.13 (0.45–2.81) | NS |
| Anxiety disorder | 13.3 | 9.5 | 1.40 (0.79–2.48) | NS |
| Conduct disorder | 3.4 | 2.2 | 1.55 (0.49–4.94) | NS |
| Psychotic disorder | 2.9 | 2.2 | 1.33 (0.42–4.26) | NS |
Abbreviations: CI = confidence interval, DMDD- = did not meet criteria for disruptive mood dysregulation disorder, DMDD+ = met criteria for disruptive mood dysregulation disorder, NS = nonsignificant.
Distinction From Oppositional Defiant Disorder and Conduct Disorder
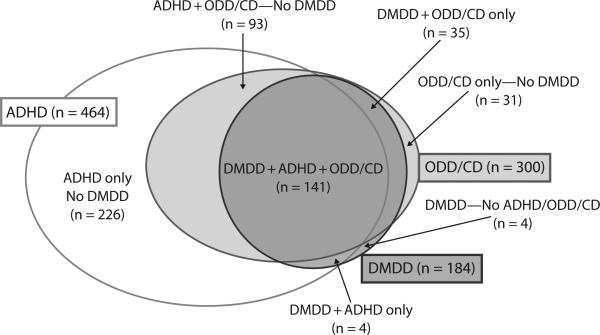
At the intake assessment, 58% of youth with oppositional defiant disorder and 61% of youth with conduct disorder were DMDD+. Nearly all (96%) of DMDD+ youth met criteria for oppositional defiant disorder or conduct disorder (RR vs DMDD– = 4.03 [95% CI, 3.44–4.70]), and 77% met criteria for both ADHD and oppositional defiant disorder/conduct disorder (RR vs DMDD– = 4.30 [95% CI, 3.52–5.26]; Figure 1). In contrast, 41% of participants with MDD (RR vs no MDD = 0.96 [95% CI, 0.68–1.36]) and 40% of those with bipolar spectrum diagnoses (RR vs no bipolar spectrum diagnoses = 0.91 [95% CI, 0.74–1.13]) had comorbid oppositional defiant disorder or conduct disorder; 27% of MDD (RR vs no MDD = 0.79 [95% CI, 0.49–1.27]) and 34% of participants with bipolar spectrum diagnoses (RR vs no bipolar spectrum diagnoses = 1.03 [95% CI, 0.74–1.13]) had both ADHD and oppositional defiant disorder/conduct disorder. There was no difference in the rate of DMDD in participants with oppositional defiant disorder/conduct disorder who were ESM+ (59%) versus those that were ESM– (55%; RR = 1.07 [95% CI, 0.71–1.61]). Participants with oppositional defiant disorder/conduct disorder who were DMDD+ did not have significantly different rates of bipolar spectrum diagnoses, depressive disorders, anxiety disorders, or ADHD compared to those who were DMDD– (Table 3). DMDD+ vs DMDD– oppositional defiant disorder/conduct disorder participants did not differ in Young Mania Rating Scale, CDRS-R, K-SADS Depression Rating Scale and K-SADS Mania Rating Scale total scores, CAASI-4R ADHD subscales, SCARED-P total scores, and Children's Global Assessment Scale.
Figure 1.
Overlap of Disruptive Mood Dysregulation Disorder (DMDD), Attention-Deficit/Hyperactivity Disorder (ADHD), and Oppositional Defiant Disorder (ODD)/Conduct Disorder (CD)
Table 3.
Factors at Intake by Disruptive Mood Dysregulation Disorder Status in Participants With Oppositional Defiant Disorder or Conduct Disorder
| DMDD+ (n=176) | DMDD– (n = 124) | Test Statistic/Relative Risk (95% CI) | P Value | |
|---|---|---|---|---|
| Demographics | ||||
| Sex, male, % | 67 | 74 | 0.90 (0.78–1.05) | NS |
| Race, white, % | 58 | 65 | 0.90 (0.75–1.08) | NS |
| Age, mean ± SD, y | 9.3 ± 1.8 | 9.5 ± 2.0 | t = 1.2 | NS |
| Lives with both biological parents, % | 28 | 27 | 1.05 (0.72–1.52) | NS |
| Primary caretaker education, % | ||||
| No or some high school | 13 | 20 | Z = 1.9 | .06 |
| GED or high school diploma | 25 | 29 | ||
| Some post–high school, no degree | 29 | 24 | ||
| Associate's degree or other post–high school certification | 22 | 15 | ||
| Bachelor's degree or higher | 12 | 12 | ||
| Diagnoses, % | ||||
| Any mood disorder | 42 | 44 | 0.94 (0.72–1.22) | NS |
| Any bipolar spectrum diagnosis | 22 | 20 | 1.10 (0.70–1.72) | NS |
| Any depressive disorder | 19 | 24 | 0.80 (0.52–1.23) | NS |
| ADHD | 80 | 75 | 1.07 (0.94–1.21) | NS |
| Any anxiety disorder | 20 | 22 | 0.91 (0.58–1.43) | NS |
| Psychotic disorder | 2 | 3 | 0.53 (0.12–2.32) | NS |
| Pervasive developmental disorder | 3 | 1 | 4.23 (0.52–34.7) | NS |
| Dimensional measures of psychopathology, mean ± SD | ||||
| YMRS total scorea | 15.5 ± 7.8 | 15.0 ± 7.6 | t = 0.6 | NS |
| CDRS-R total scorea | 33.1 ± 9.5 | 32.3 ± 10.3 | t = 0.7 | NS |
| K-SADS Depression Rating Scale total score | 7.8 ± 5.7 | 7.1 ± 5.9 | t = 1.0 | NS |
| K-SADS Mania Rating Scale total scorea | 10.6 ± 8.3 | 8.8 ± 7.8 | t = 1.9 | .06 |
| CAASI-4R subscale score | ||||
| ADHD—inattentive | 19.6 ± 6.0 | 18.4 ± 6.3 | t = 1.7 | NS |
| ADHD—hyperactive/impulsive | 18.1 ± 6.6 | 17.3 ± 6.5 | t = 1.0 | NS |
| ADHD—combined | 37.7 ± 11.1 | 35.7 ± 11.5 | t = 1.5 | NS |
| SCARED-P score | 17.8 ± 12.4 | 17.3 ± 12.4 | t = 0.3 | NS |
| Functioning, mean ± SD | ||||
| CGAS score (current) | 50.8 ± 9.2 | 51.5 ± 10.3 | t = 0.6 | NS |
| CGAS score (most severe past) | 48.1 ± 10.3 | 46.1 ± 10.3 | t = 1.3 | NS |
Irritability item not included in the total score.
Abbreviations: ADHD = attention-deficit/hyperactivity disorder, CAASI-4R = Child and Adolescent Symptom Inventory-4R, CDRS-R = Children's Depression Rating Scale-Revised, CGAS = Children's Global Assessment Scale, CI = confidence interval, DMDD– = did not meet criteria for disruptive mood dysregulation disorder, DMDD+ = met criteria for disruptive mood dysregulation disorder, GED = General Equivalency Diploma, NS = nonsignificant, SCARED-P = Screen for Child Anxiety Related Emotional Disorders, YMRS = Young Mania Rating Scale.
In the participants diagnosed with oppositional defiant disorder or conduct disorder (n = 180) at intake who also had both follow-up assessments, those with DMDD did not differ significantly from those without DMDD in the rates of new onset of bipolar spectrum diagnoses (9% vs 18%; RR = 0.5 [95% CI, 0.21–1.22]), depressive disorders (12% vs 12%; RR = 0.96 [95% CI, 0.39–2.39]), psychotic disorders (3% vs 4%; RR = 0.75 [95% CI, 0.16–3.61]), or anxiety disorders (13% vs 16%; RR = 0.86 [95% CI, 0.39–1.89]).
Parental Psychiatric History
DMDD+ participants at intake did not significantly differ from DMDD– participants in the rates of a screening diagnosis in at least 1 biological parent of depression (DMDD+ 67% vs DMDD– 63%, RR = 1.06 [95% CI, 0.94–1.20]), bipolar disorder (23% vs 20%, RR = 1.19 [95% CI, 0.86–1.66]), anxiety disorder (49% vs 55%, RR = 0.88 [95% CI, 0.74–1.05]), psychotic disorder (14% vs 11%, RR = 1.31 [95% CI, 0.84–2.05]), substance use disorder (48% vs 45%, RR = 1.06 [95% CI, 0.88–1.26]), ADHD (30% vs 26%, RR = 1.12 [95% CI, 0.86–1.47]), or conduct disorder (43% vs 39%, RR = 1.10 [95% CI, 0.90–1.34]).
DISCUSSION
The results of these analyses indicate that severe recurrent temper outbursts and chronic irritability are common symptoms in youth presenting for outpatient psychiatric assessment. Moreover, the proposed DMDD diagnosis is common in university child psychiatric outpatient settings. However, DMDD did not identify a phenotype that was clearly differentiated from disruptive behavioral disorders or had a distinct course and outcome, substantial longitudinal stability, or an association with a parental history of mood or anxiety disorders. In comparison to other diagnoses in the LAMS cohort, the degree of overlap between disruptive behavior disorders (oppositional defiant disorder/conduct disorder) and DMDD was far greater than the overlap between oppositional defiant disorder/conduct disorder and mood disorders, and the longitudinal stability of the DMDD diagnosis was far less than the stability of ADHD.
The study results should be considered with regard to the following limitations. The LAMS participants were disproportionately recruited to have elevated PGBI-10M scores, and DMDD was associated with increased PGBI-10M scores. The PGBI-10M has 2 items that assess irritability, although it is in the context of unusually happy mood: (1) periods of feeling unusually happy as well as struggling to control inner feelings of rage and (2) periods of feeling unusually happy when almost everything got on their nerves. Therefore, the sample may not be representative of the cohort of all participants who were screened, which could affect the rates of DMDD and the phenomenology of the DMDD+ participants assessed. However, it is notable that ESM status at baseline was not a significant factor in the multivariate analyses. DMDD criteria were extracted from K-SADS questions so that only a retrospective diagnosis could be applied. The instrument used for ascertaining family history (the Family History Screen) uses a few screening questions to determine diagnoses in family members; these results should be interpreted with caution. The majority of participants presented to outpatient services at academic psychiatry departments, so results may not generalize to other clinical settings or to community samples.
In LAMS, DMDD could not be clearly differentiated from oppositional defiant disorder and conduct disorder. On multivariate assessment, DMDD status at intake was associated only with oppositional defiant disorder and conduct disorder diagnoses, and these associations were not affected by ESM status. At intake, the majority of youth with oppositional defiant disorder (59%) or conduct disorder (61%) also met criteria for DMDD. These percentages are substantially higher than those found in some clinical cohorts, where approximately 25% of the oppositional defiant disorder participants met DMDD criteria.6 However, a clinical sample from a recent treatment study25 had similar levels of overlap of SMD with oppositional defiant disorder and conduct disorder, as 44% of participants with oppositional defiant disorder and 67% of those with conduct disorder met SMD criteria. The oppositional defiant disorder/conduct disorder youth with DMDD did not differ from those without DMDD in age, sex, rates of comorbid disorders or of onset of new disorders over follow-up, dimensional psychopathology, or functional impairment. The degree of diagnostic overlap between DMDD and oppositional defiant disorder/conduct disorder (RR = 4.0) was many orders of magnitude greater than for other mood disorders in the sample such as MDD or bipolar spectrum diagnoses, both of which were not significantly associated with oppositional defiant disorder/conduct disorder (RR, 0.9–1.0).
DMDD was not specifically associated with disorders other than oppositional defiant disorder and conduct disorder, although DMDD was present in 40%–50% of youth diagnosed with anxiety, depressive, and bipolar spectrum disorders during the first 2 years of the study. On multivariate analysis, DMDD was associated with dimensional psychopathology only in the domains of disruptive behavior disorders. DMDD at intake did not specifically predict future onset of mood or anxiety disorders over follow-up. Finally, DMDD was not associated with a parental history of ADHD or mood, anxiety, conduct, or substance use disorders. These findings stand in contrast to results from epidemiologic studies,7,26–28 which found that chronic irritability (including SMD) in childhood was associated with future onset of depressive and anxiety disorders.
Multiple factors may contribute to the disparate findings. Participant ascertainment may play a key role, as there are potential differences in the phenomenology of depressed and DMDD youth who are seeking treatment and enriched for the presence of manic symptomatology versus those in the community. In addition, epidemiologic samples would be expected to have much lower rates of DMDD and mood disorders in general, and bipolar disorder in particular, than the LAMS sample. Low numbers of participants with bipolar disorder can lead to difficulty in obtaining accurate estimates of the association of DMDD with bipolarity. Operationalization of the retrospective diagnoses could affect results, as some studies7,28 included irritability items drawn from the depression section of the assessment, which could increase the association of DMDD and later depression. Age of the participants and the duration of follow-up could also influence the findings. The LAMS cohort was 9½ years old on average at intake and was followed for only 2 years to date, so they were well before the maximum age of risk for onset of depression or bipolar disorder at the end of follow-up. In contrast, the epidemiologic studies often followed participants into young adulthood.7,26 These differences in methodology reinforce the need for multiple studies (preferably with repeated assessment and extended longitudinal follow-up) using different sampling and assessment strategies, to determine whether a clearer consensus on DMDD can emerge.
DMDD was not associated with bipolar disorder overall, or with a family history of manic symptoms. This lack of association lends support to the conceptualization that chronic irritability and temper outbursts are not specific manifestations of pediatric bipolar disorder. However, given that 44% of youth with bipolar I or II disorder would have met criteria for DMDD except for the bipolar diagnostic exclusion, clinicians will need to carefully assess for the presence of manic symptomatology in youth who have the DMDD phenotype, or children who actually have bipolar disorder could be mislabeled as having DMDD.
In the LAMS cohort, DMDD was a common but somewhat transient phenotype that could not be clearly differentiated from disruptive behavior disorders (oppositional defiant disorder and conduct disorder) and was otherwise not specifically associated with other diagnoses or symptom domains. These findings indicate that additional research will be required to clarify whether the DMDD phenotype is a valid, separate diagnostic entity.
Clinical Points.
■ The proposed disruptive mood dysregulation disorder (DMDD) diagnosis is not clearly differentiated from oppositional defiant disorder and conduct disorder in children presenting for psychiatric treatment.
■ Youth presenting for treatment with disruptive behavioral, anxiety, and mood disorders will frequently meet the proposed diagnostic criteria for DMDD.
■ Many youth with bipolar disorder will meet the primary symptom criteria for DMDD; therefore, careful assessment for manic symptomatology is required for children who present with features of DMDD.
Acknowledgment
The authors thank the National Institute of Mental Health for their support.
Funding/support: This study was supported by the National Institute of Mental Health (R01-MH073967, R01-MH073801, R01-MH073953, R01-MH073816).
Disclaimer: The authors acknowledge that the findings and conclusions presented in this paper are those of the authors alone and do not necessarily reflect the opinions of NIMH.
Footnotes
Potential conflicts of interest: Dr Findling receives or has received research support from, acted as a consultant for, received royalties from, and/or served on a speakers bureau for Abbott, Addrenex, Alexza, American Psychiatric Press, AstraZeneca, Biovail, Bristol-Myers Squibb, Dainippon Sumitomo, Forest, GlaxoSmithKline, Guilford Press, Johns Hopkins University Press, Johnson & Johnson, KemPharm, Eli Lilly, Lundbeck, Merck, National Institutes of Health, Neuropharm, Novartis, Noven, Organon, Otsuka, Pfizer, Physicians Postgraduate Press, Rhodes, Roche, Sage, Sanofi-Aventis, Schering-Plough, Seaside Therapeutics, Sepracor, Shionogi, Shire, Solvay, Stanley Medical Research Institute, Sunovion, Supernus, Transcept, Validus, WebMD, and Wyeth. Dr Fristad receives royalties from Guilford Press, American Psychiatric Publishing, and CFPSI Press. Dr Kowatch receives or has received research support from, acted as a consultant for, and/or served on a speakers bureau for Forest, AstraZeneca, Current Psychiatry, and the REACH Foundation. Dr Youngstrom has received travel support from Bristol-Myers Squibb and consulted with Lundbeck. Dr Arnold receives or has received research support from, acted as a consultant for, and/or served on a speakers bureau for Abbott, AstraZeneca, Biomarin, Celgene, Curemark, Eli Lilly, McNeil, Novartis, Noven, Neuropharm, Organon, Shire, Sigma Tau, and Targacept. Dr Frazier has received federal funding or research support from, acted as a consultant to, received travel support from, and/or received a speaker's honorarium from Forest, Ecoeos, IntegraGen, Shire, Bristol-Myers Squibb, National Institutes of Health, and the Brain and Behavior Research Foundation. Dr Birmaher receives or has received research support from and acted as a consultant for Schering Plough. He receives royalties from Random House and Lippincott Williams & Wilkins and support from NIMH. Drs Axelson, Horwitz, Ryan, and Hauser-Harrington; Mss Demeter, Gill, Depew, Gron, and Rowles; and Mr Kennedy report no potential conflict of interest.
REFERENCES
- 1.Bambauer KZ, Connor DF. Characteristics of aggression in clinically referred children. CNS Spectr. 2005;10(9):709–718. doi: 10.1017/s1092852900019702. [DOI] [PubMed] [Google Scholar]
- 2.Carlson GA, Potegal M, Margulies D, et al. Rages: what are they and who has them? J Child Adolesc Psychopharmacol. 2009;19(3):281–288. doi: 10.1089/cap.2008.0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.D 00 Disruptive mood dysregulation disorder. American Psychiatric Association DSM-5 Development; [August 9, 2012]. http://www.dsm5.org/ProposedRevision/Pages/proposedrevision.aspx?rid=397. Updated April 2012. [Google Scholar]
- 4. [August 9, 2012];Issues pertinent to a developmental approach to bipolar disorder in DSM-5. http://www.dsm5.org/Proposed%20Revision%20Attachments/APA%20Developmental%20Approaches%20to%20Bipolar%20Disorder.pdf. Updated 2010.
- 5.Leibenluft E, Charney DS, Towbin KE, et al. Defining clinical phenotypes of juvenile mania. Am J Psychiatry. 2003;160(3):430–437. doi: 10.1176/appi.ajp.160.3.430. [DOI] [PubMed] [Google Scholar]
- 6.Leibenluft E. Severe mood dysregulation, irritability, and the diagnostic boundaries of bipolar disorder in youths. Am J Psychiatry. 2011;168(2):129–142. doi: 10.1176/appi.ajp.2010.10050766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brotman MA, Schmajuk M, Rich BA, et al. Prevalence, clinical correlates, and longitudinal course of severe mood dysregulation in children. Biol Psychiatry. 2006;60(9):991–997. doi: 10.1016/j.biopsych.2006.08.042. [DOI] [PubMed] [Google Scholar]
- 8.Robins E, Guze SB. Establishment of diagnostic validity in psychiatric illness: its application to schizophrenia. Am J Psychiatry. 1970;126(7):983–987. doi: 10.1176/ajp.126.7.983. [DOI] [PubMed] [Google Scholar]
- 9.Horwitz SM, Demeter CA, Pagano ME, et al. Longitudinal Assessment of Manic Symptoms (LAMS) study: background, design, and initial screening results. J Clin Psychiatry. 2010;71(11):1511–1517. doi: 10.4088/JCP.09m05835yel. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Findling RL, Youngstrom EA, Fristad MA, et al. Characteristics of children with elevated symptoms of mania: the Longitudinal Assessment of Manic Symptoms (LAMS) study. J Clin Psychiatry. 2010;71(12):1664–1672. doi: 10.4088/JCP.09m05859yel. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Youngstrom EA, Frazier TW, Demeter C, et al. Developing a 10-item mania scale from the Parent General Behavior Inventory for children and adolescents. J Clin Psychiatry. 2008;69(5):831–839. doi: 10.4088/jcp.v69n0517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kaufman J, Birmaher B, Brent D, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36(7):980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 13.Geller B, Zimerman B, Williams M, et al. Reliability of the Washington University in St. Louis Kiddie Schedule for Affective Disorders and Schizophrenia (WASH-U-KSADS) mania and rapid cycling sections. J Am Acad Child Adolesc Psychiatry. 2001;40(4):450–455. doi: 10.1097/00004583-200104000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Axelson D, Birmaher B, Strober M, et al. Phenomenology of children and adolescents with bipolar spectrum disorders. Arch Gen Psychiatry. 2006;63(10):1139–1148. doi: 10.1001/archpsyc.63.10.1139. [DOI] [PubMed] [Google Scholar]
- 15.Chambers WJ, Puig-Antich J, Hirsch M, et al. The assessment of affective disorders in children and adolescents by semistructured interview: test-retest reliability of the Schedule for Affective Disorders and Schizophrenia for School-Age Children, Present Episode Version. Arch Gen Psychiatry. 1985;42(7):696–702. doi: 10.1001/archpsyc.1985.01790300064008. [DOI] [PubMed] [Google Scholar]
- 16.Axelson D, Birmaher BJ, Brent D, et al. A preliminary study of the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children Mania Rating Scale for children and adolescents. J Child Adolesc Psychopharmacol. 2003;13(4):463–470. doi: 10.1089/104454603322724850. [DOI] [PubMed] [Google Scholar]
- 17.Young RC, Biggs JT, Ziegler VE, et al. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry. 1978;133(5):429–435. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- 18.Overholser JC, Brinkman DC, Lehnert KL, et al. Children's Depression Rating Scale-Revised: development of a short form. J Clin Child Psychol. 1995;24(4):443–452. [Google Scholar]
- 19.Poznanski EO, Grossman JA, Buchsbaum Y, et al. Preliminary studies of the reliability and validity of the Children's Depression Rating Scale. J Am Acad Child Psychiatry. 1984;23(2):191–197. doi: 10.1097/00004583-198403000-00011. [DOI] [PubMed] [Google Scholar]
- 20.Gadow KD, Sprafkin J. Child and Adolescent Symptom Inventory-4R. Checkmate Plus; Stony Brook, NY: 2005. [Google Scholar]
- 21.Birmaher B, Khetarpal S, Brent D, et al. The Screen for Child Anxiety Related Emotional Disorders (SCARED): scale construction and psychometric characteristics. J Am Acad Child Adolesc Psychiatry. 1997;36(4):545–553. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- 22.Shaffer D, Gould MS, Brasic J, et al. A Children's Global Assessment Scale (CGAS). Arch Gen Psychiatry. 1983;40(11):1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- 23.Weissman MM, Wickramaratne P, Adams P, et al. Brief screening for family psychiatric history: the Family History Screen. Arch Gen Psychiatry. 2000;57(7):675–682. doi: 10.1001/archpsyc.57.7.675. [DOI] [PubMed] [Google Scholar]
- 24.Hosmer DW, Lemeshow S. In: Applied Logistic Regression. Shewhart WA, Wilks SS, editors. Wiley & Sons, Inc.; New York, NY: 2000. [Google Scholar]
- 25.Waxmonsky J, Pelham WE, Gnagy E, et al. The efficacy and tolerability of methylphenidate and behavior modification in children with attention-deficit/hyperactivity disorder and severe mood dysregulation. J Child Adolesc Psychopharmacol. 2008;18(6):573–588. doi: 10.1089/cap.2008.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stringaris A, Cohen P, Pine DS, et al. Adult outcomes of youth irritability: a 20-year prospective community-based study. Am J Psychiatry. 2009;166(9):1048–1054. doi: 10.1176/appi.ajp.2009.08121849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stringaris A, Goodman R. Longitudinal outcome of youth oppositionality: irritable, headstrong, and hurtful behaviors have distinctive predictions. J Am Acad Child Adolesc Psychiatry. 2009;48(4):404–412. doi: 10.1097/CHI.0b013e3181984f30. [DOI] [PubMed] [Google Scholar]
- 28.Leibenluft E, Cohen P, Gorrindo T, et al. Chronic versus episodic irritability in youth: a community-based, longitudinal study of clinical and diagnostic associations. J Child Adolesc Psychopharmacol. 2006;16(4):456–466. doi: 10.1089/cap.2006.16.456. [DOI] [PubMed] [Google Scholar]