Abstract
Purpose
To assess the ability of volar locked plating to achieve and maintain normal radiographic parameters for articular stepoff, volar tilt, radial inclination, ulnar variance, and radial height in distal radius fractures.
Methods
We performed a retrospective review of 185 distal radius fractures that underwent volar locked plating with a single plate design over a 5-year period. We reviewed radiographs and recorded measurements for volar tilt, radial inclination, ulnar variance, radial height, and articular stepoff. We used logistic regression to determine the association between return to radiographic standard norms and fracture type.
Results
At the first and final postoperative follow-up visits, we observed articular congruence less than 2 mm in 92% of fractures at both times. Normal volar tilt (11°) was restored in 46% at the first follow-up and 48% at the final one. Radial inclination (22°) was achieved in 44% at the first follow-up and 43% at the final one, and ulnar variance (01 ± 2 mm) was achieved in 53% at the first follow-up and 53% at the final one. In addition, radial height (14 ± 1mm) was restored in 14% at the first follow-up and 12% at the final one. More complex, intra-articular fractures (AO class B and C and Frykman types 3, 4, 7, and 8) were less likely to be restored to normal radiographic parameters. However, because of the small sample size for some fracture types, it was difficult to discover significant associations between fracture type and radiographic outcome.
Conclusions
Volar locked plating for distal radius fractures achieved articular stepoff less than 2 mm in most fractures but only restored and maintained normal radiographic measurements for volar tilt, radial inclination, and ulnar variance in 50% of fractures. The ability of volar locked plating to restore and maintain ulnar variance and volar tilt decreased with more complex intra-articular fracture types.
Keywords: Distal radius fractures, volar locked plating
Volar Plate Fixation has become the preferred method of internal fixation for distal radius fractures.1–6 Chen and Jupiter7 and Orbay and Fernandez8, 9 showed that compared with other methods of fixation, volar plating for distal radius fractures allows for better anatomic reduction, earlier return of hand and upper limb function, decreased amount of occupational therapy postoperatively, less pain, decreased risk of displacement, and increased cost savings. Because of the correlation between anatomic reduction and functional outcome, locked plating systems were developed for distal radius fractures to assist with fixation in more difficult cases, such as in unstable osteoporotic bone and highly comminuted fractures.4
On standard posteroanterior and lateral radiographs, 5 measurements can be used to evaluate the anatomy of the distal radius: volar tilt, radial inclination, ulnar variance, radial height, and articular surface congruity. Abnormalities in the anatomy of the wrist joint have been shown to lead to decreased grip strength and range of motion, instability of the distal radioulnar joint, pain, Kienböck disease, acute scapholunate instability, ulnocarpal impaction, and radioulnar impingement.7, 10–16 Regarding articular congruency, Knirk and Jupiter17 demonstrated that failure to achieve or maintain congruity of the articular surface (defined as stepoff of < 2 mm) until union was the most important factor in the development of radiographic evidence of posttraumatic arthritis after fracture.
In this study, we hypothesized that volar locked plating would help restore and maintain normal volar tilt, radial inclination, ulnar variance, and radial height, and provide articular congruency with less than 2 mm of stepoff. We also hypothesized that the ability to achieve normal radiographic measurements would be associated with fracture classification.
MATERIALS AND METHODS
Between 2005 and 2009, 3 board-certified, fellowship-trained orthopedic hand surgeons at our level 1 traumacentertreated 420 distal radius fractures in 408 patients with operative fixation. All fractures underwent fixation with a Hand Innovations DVR plate (DePuy, Warsaw, IN). Most plates used had 3 or 4 holes and were of standard size. In most cases, the distal row of the plate was filled entirely or 1 hole was left empty. Both smooth pegs and threaded screws were used with equal frequency. Entry criteria for the study were age greater than 18 years; availability of adequate series of radiographs, including at least 1 preoperative posteroanterior (PA) and lateral radiograph (an injury film, postreduction film, or both) and 2 postoperative PA and lateral radiographs (1 taken at the first postoperative follow-up visit and 1 at least 6 weeks after surgery); open reduction and internal fixation using a single type of volar locking plate with no other type of fixation used; no prior fixation; and a minimum follow-up of 6 weeks postoperatively. Of the 420 fractures identified, we excluded 235, which left 185 fractures available for study. We excluded 66 fractures because of a lack of adequate radiographs, 39 because a different type of plate was used, 59 because additional fixation or fixation with another device was employed (ie, Kirschner wires, external fixator), 64 because of follow-up less than 6 weeks, and 7 because patients underwent revision surgery for nonacute fractures (ie, fractures > 3 wk old, nonunions, or failure of previous fixation).
We collected and managed study data using Research Electronic Data Capture electronic data capture tools.18 Research Electronic Data Capture is a secure, Web-based application designed to support data capture for research studies and provides an intuitive interface for validated data entry, audit trails for tracking data manipulation and export procedures, automated export procedures for seamless data downloads to common statistical packages, and procedures for importing data from external sources.18, 19 After we obtained institutional review board approval, 2 fellowship-trained musculoskeletal radiologists and a senior orthopedic resident reviewed de-identified PA and lateral radiographs from the time of injury or after closed reduction, initial postoperative follow-up, and minimum 6-week postoperative follow-up. No reviewers were participants in the operative procedures. Each fracture with an injury film was classified according to the Frykman and AO classification systems by a board-certified, fellowship-trained hand surgeon.20–23 For the AO classification system, we categorized fractures as A, B, or C and then further divided them into 1, 2, or 3. We did not classify fractures without injury films (48 fractures out of 185).
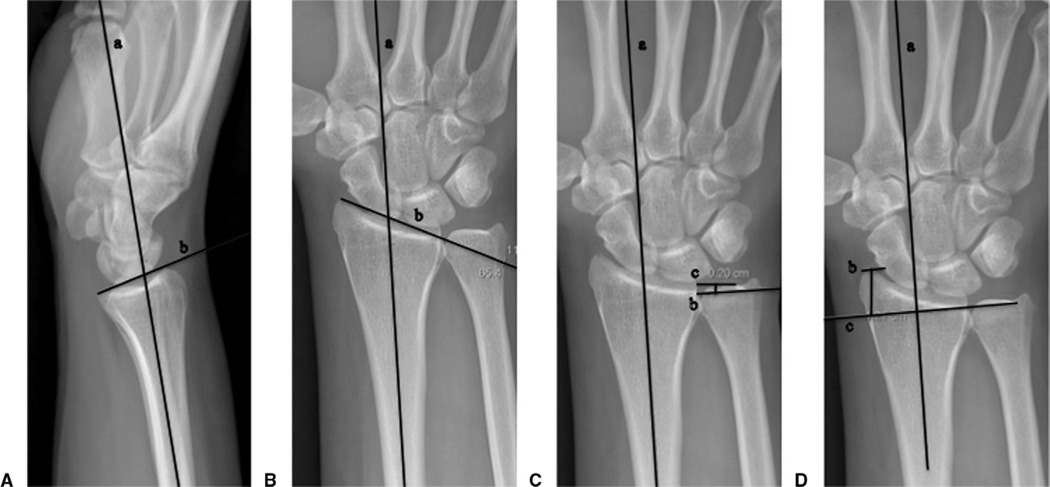
We measured volar tilt, radial inclination, ulnar variance, and radial height on each film (injury or postreduction, first postoperative, and second postoperative) and recorded them in either degrees or millimeters. Articular congruency was categorized as 0 to 2 mm, or 2 mm or greater. Days to the first postoperative follow-up ranged from 1 to 34 (median, 11 d) and days from surgery to the second postoperative follow-up ranged from 42 to 170 (median, 83 d). We excluded radiographs that were of inadequate quality to make accurate measurements. Methods for making measurements were based on those described by Mann et al.14 We measured volar tilt on a lateral radiograph by determining the angle formed between the long axis of the radius and a line drawn along the articular surface16 (Fig. 1A). Normal volar tilt was considered to be 11° ± 5°.24 We measured radial inclination on a PA radiograph by determining the angle formed between the long axis of the radius and a line drawn from the distal tip of the radial styloid to the ulnar corner of the lunate fossa25 (Fig. 1B). Normal radial inclination was considered to be 22° ± 3°.10, 26 We measured ulnar variance on a PA radiograph using the method of perpendiculars. We identified the long axis of the radius and drew a line perpendicular to this, extending through the ulnar-most corner of the lunate fossa. We recorded the distance between this line and the distal-most point of the ulnar dome as the ulnar variance, where a positive number denoted ulnar positive and a negative number denoted ulnar negative15 (Fig. 1C). Normal ulnar variance was considered to be 0.7 ± 1.5 mm.27 We determined radial height by finding the long axis of the radius and then extending a line perpendicular to it at the tip of the radial styloid on a PA radiograph. We recorded the distance between this line and the distal-most point of the ulnar dome10 (Fig. 1D). Normal radial height was considered to be 14 ± 1 mm.28 We defined the accepted functional range for each measurement, excluding radial height, based on functional outcomes from the literature (≤ 20° dorsal angulation, ≥10° radial inclination, ≤5 mm ulnar variance, and < 2 mm stepoff).14, 16, 17, 29
FIGURE 1.
Method of measuring A volar tilt, B radial inclination, C ulnar variance, and D radial height.
We evaluated articular congruency by looking at the articular surface of the distal radius on either a PA or lateral film. We measured any noted stepoff and recorded it as either less than 2 mm or 2 mm or greater. We chose 2 mm as a cutoff based on the work of Knirk and Jupiter,17 who demonstrated that patients with 2 mm or more of stepoff after reduction of distal radius fractures had a significant chance of developing radiographic evidence of posttraumatic arthritis.
We conducted a pilot study with 10 fractures and 4 radiographs per fracture (injury, after closed reduction, at initial postoperative follow-up, and at second postoperative follow-up) to assess interobserver agreement for 5 measurements: volar tilt, radial inclination, ulnar variance, radial height, and articular stepoff. Four observers (2 fellowship-trained musculoskeletal radiologists, a senior orthopedic resident, and a senior medical student) each looked at all 40 films independently and made all 5 measurements for each film. The average Spearman rank correlation coefficient between readers was greater than 0.75 for all measurements except articular stepoff. Therefore, we divided the total number of fractures among 3 observers for the purpose of measuring volar tilt, radial inclination, ulnar variance, and radial height. However, because the interobserver correlation was low, each observer measured articular stepoff for every film, and a consensus measurement among the 3 observers was recorded.
Statistical methods
The sample is summarized by demographic variables in which the minimum, maximum, and 25th, 50th and 75th percentiles are given for continuous variables (age, days from injury to surgery, days from surgery to first follow-up, days from surgery to second follow-up, volar tilt, radial inclination, ulnar variance, and radial height) and proportions are given for categorical variables (sex, hand dominance, injured hand, surgeon, location, and stepoff). The proportion of patients who fell in the normal ranges is given for each time point and fracture type. In addition, the mean and standard deviation of each measure are given by time and fracture type. To determine whether fracture type may be related to having a measurement in the normal range, a logistic model that also adjusted for the average presurgery measure, age, and sex is presented. This was done for the AO classification with 3 groups and for the Frykman classification with 4 groups. The 4 Frykman groups were (1,2), (3,4), (5,6), and (7,8).
RESULTS
Table 1 lists patient demographics. As expected, the vast majority of preoperative films were not within the range of radiographic norms (Table 2). At any measure for both first and second follow-up visit, no more than 50% of fractures achieved the normal metric for volar tilt, radial inclination, ulnar variance, and radial height (Tables 3, 4). The means of all radiographic measurements were improved from injury to first postoperative follow-up and stayed relatively similar at the second postoperative follow-up. In 5 cases, there was penetration of distal screws or pegs through the subchondral surface, which appeared to result from subsidence of the fracture fragments.
TABLE 1.
Patient Characteristics
| Variable | |
|---|---|
| Age (y) | 49 (min = 18, 25th = 34, 75th = 61, max = 89) |
| Sex | |
| Male | 52% (96) |
| Female | 48% (89) |
| Hand dominance | |
| Left | 10% (19) |
| Right | 60% (110) |
| Both | 0.5% (1) |
| Unknown | 30% (55) |
| Injured hand | |
| Left | 60% (109) |
| Right | 41% (76) |
| Injury to surgery (d) | 5 (min = 0, 25th = 2, 75th = 10, max = 34) |
| Surgery to first follow-up (d) | 11 (min = 1, 25th = 9, 75th = 13, max = 34) |
| Surgery to second follow-up (d) | 83 (min = 42, 25th = 67, 75th = 102, max = 170) |
min, minimum; max, maximum; 25th and 75th, percentiles.
TABLE 2.
Measurement for Injury Films
| n | Volar Tilt* | Radial Inclination | Ulnar Variance† | Radial Height | Stepoff | |
|---|---|---|---|---|---|---|
| Overall (% [n]) | 137 | 4% (6) | 26% (35) | 24% (33) | 2% (3) | 58% (80) |
| Mean (SD) | −17° (21.8°) | 13° (10.1°) | 4 mm (4.9 mm) | 3 mm (7.5 mm) | ||
| Minimum to maximum | −71° to 58° | −27° to 29° | −23 to 21 mm | −20 to 18 mm | ||
| AO class (% [n]) | ||||||
| 1 | 31 | 0% | 29% (9) | 39% (12) | 0% | 97% (30) |
| 2 | 6 | 17% (1) | 17% (1) | 0% | 0% | 83% (5) |
| 3 | 3 | 33% (1) | 33% (1) | 33% (1) | 0% | 33% (1) |
| 4 | 3 | 0% | 33% (1) | 33% (1) | 0% | 33% (1) |
| 5 | 3 | 0% | 33% (1) | 33% (1) | 0% | 33% (1) |
| 6 | 10 | 0% | 40% (4) | 40% (4) | 10% (1) | 60% (6) |
| 7 | 42 | 5% (2) | 31% (13) | 24% (10) | 0% | 60% (25) |
| 8 | 39 | 5% (2) | 13% (5) | 10% (4) | 5% (2) | 28% (11) |
| Frykman (% [n]) | ||||||
| 1 | 9 | 11% (1) | 22% (2) | 44% (4) | 0% | 89% (8) |
| 2 | 14 | 0% | 29% (4) | 29% (4) | 0% | 93% (13) |
| 3 | 18 | 6% (1) | 39% (7) | 56% (10) | 6% (1) | 56% (10) |
| 4 | 14 | 14% (2) | 50% (7) | 21% (3) | 0% | 36% (5) |
| 5 | 4 | 0% | 25% (1) | 25% (1) | 0% | 100% (4) |
| 6 | 10 | 0% | 20% (2) | 10% (1) | 0% | 100% (10) |
| 7 | 23 | 4% (1) | 26% (6) | 17% (4) | 0% | 44% (10) |
| 8 | 45 | 2% (1) | 13% (6) | 13% (6) | 4% (2) | 44% (20) |
Data represent the percentage of fractures that fall into the normal range for each parameter and for each fracture classification, the mean measurement achieved, and the range of measurements for each parameter.
Minus values indicate dorsal tilt.
Minus values indicate negative ulnar variance.
TABLE 3.
Measurement for First Postoperative Follow-up Films
| n | Volar Tilt* | Radial Inclination | Ulnar Variance† | Radial Height | Stepoff | |
|---|---|---|---|---|---|---|
| Overall (% [n]) | 185 | 46% (85) | 44% (91) | 53% (98) | 14% (26) | 92% (170) |
| Mean (SD) | 7° (6.9°) | 21° (4.1°) | 0.4 mm (2.3 mm) | 10.8 mm (3.0 mm) | ||
| Minimum to maximum | −21° to 24° | 9° to 29° | −4.6 to 12.4 mm | 1.8–18.1 mm | ||
| AO class | ||||||
| 1 | 31 | 58% (18) | 45% (14) | 64.5% (20) | 13% (4) | 100% (31) |
| 2 | 6 | 33% (2) | 67% (4) | 66.7% (4) | 33% (2) | 100% (6) |
| 3 | 3 | 100% (3) | 100% (3) | 66.7% (2) | 0% | 100% (3) |
| 4 | 3 | 33% (1) | 33% (1) | 100% (3) | 0% | 100% (3) |
| 5 | 3 | 33% (1) | 33% (1) | 66.7% (2) | 0% | 67% (2) |
| 6 | 10 | 60% (6) | 40% (4) | 40.0% (4) | 10% (1) | 90% (9) |
| 7 | 42 | 48% (20) | 57% (24) | 50.0% (21) | 21% (9) | 95% (40) |
| 8 | 39 | 39% (15) | 39% (15) | 51.3% (20) | 8% (3) | 85% (33) |
| P value | .684 | .950 | .068 | .310 | .640 | |
| Frykman | ||||||
| 1 | 9 | 56% (5) | 44% (4) | 66.7% (6) | 11% (1) | 100% (9) |
| 2 | 14 | 57% (8) | 57% (8) | 85.7% (12) | 0% | 100% (14) |
| 3 | 18 | 44% (8) | 50% (9) | 38.9% (7) | 11% (2) | 89% (16) |
| 4 | 14 | 64% (9) | 50% (7) | 57.1% (8) | 14% (2) | 86% (12) |
| 5 | 4 | 50% (2) | 50% (2) | 50.0% (2) | 0% | 100% (4) |
| 6 | 10 | 40% (4) | 40% (4) | 30.0% (3) | 50% (5) | 100% (10) |
| 7 | 23 | 30% (7) | 39% (9) | 43.5% (10) | 17% (4) | 96% (22) |
| 8 | 45 | 51% (23) | 51% (23) | 62.2% (28) | 11% (5) | 89% (40) |
| Four-group P value | .773 | .963 | .021‡ | .126 | .709 |
Data represent the percentage of fractures that fall into the normal range for each parameter and for each fracture classification, the mean measurement achieved, and the range of measurements for each parameter. P values are from a logistic model that also includes age, sex, presurgery measure average, AO classification with 3 groups, and Frykman classification with 4 groups.
Minus values indicate dorsal tilt.
Minus values indicate negative ulnar variance.
Statistically significant value.
TABLE 4.
Measurement for Second Postoperative Follow-Up Films
| n | Volar Tilt* | Radial Inclination | Ulnar Variance† | Radial Height | Stepoff | |
|---|---|---|---|---|---|---|
| Overall (% [n]) | 185 | 48% (88) | 43% (79) | 52% (97) | 12% (22) | 92% (171) |
| Mean (SD) | 7° (6.1°) | 22° (4.5°) | 0.9 mm (2.2 mm) | 10.5 mm (3.0 mm) | ||
| Minimum to maximum | −13° to 25° | 2° to 30° | −5.6 to 8.2 mm | 2.4–18.7 mm | ||
| AO class | ||||||
| 1 | 31 | 65% (20) | 52% (16) | 71% (22) | 16% (5) | 100% (31) |
| 2 | 6 | 67% (4) | 50% (3) | 50% (3) | 50% (3) | 100% (6) |
| 3 | 3 | 100% (3) | 67% (2) | 33% (1) | 33% (1) | 100% (3) |
| 4 | 3 | 67% (2) | 0% | 100% (3) | 33% (1) | 100% (3) |
| 5 | 3 | 67% (2) | 67% (2) | 67% (2) | 0% | 67% (2) |
| 6 | 10 | 60% (6) | 30% (3) | 40% (4) | 0% | 90% (9) |
| 7 | 42 | 38% (16) | 50% (21) | 60% (25) | 14% (6) | 95% (40) |
| 8 | 39 | 39% (15) | 28% (11) | 36% (14) | 8% (3) | 80% (31) |
| P value | .019† | .483 | .174 | .071 | .547 | |
| Frykman | ||||||
| 1 | 9 | 89% (8) | 89% (8) | 67% (6) | 0% | 100% (9) |
| 2 | 14 | 57% (8) | 50% (7) | 79% (11) | 14% (2) | 100% (14) |
| 3 | 18 | 33% (6) | 44% (8) | 44% (8) | 6% (1) | 89% (16) |
| 4 | 14 | 71% (10) | 43% (6) | 64% (9) | 14% (2) | 86% (12) |
| 5 | 4 | 25% (1) | 25% (1) | 0% | 50% (2) | 100% (4) |
| 6 | 10 | 50% (5) | 40% (4) | 80% (8) | 30% (3) | 100% (10) |
| 7 | 23 | 39% (9) | 9% (2) | 44% (10) | 13% (3) | 91% (21) |
| 8 | 45 | 47% (21) | 49% (22) | 49% (22) | 13% (6) | 87% (39) |
| Four-group P value | .292 | .109 | .296 | .121 | .756 |
Data represent the percentage of fractures that fall into the normal range for each parameter and for each fracture classification, the mean measurement achieved, and the range of measurements for each parameter. P values are from a logistic model that also includes age, sex, presurgery measure average, AO classification with 3 groups, and Frykman classification with 4 groups.
Minus values indicate dorsal tilt.
Minus values indicate negative ulnar variance.
Statistically significant value.
Whereas the percentage of fractures reaching the normal measures increased for all fracture types from the time of injury to the first postoperative visit, the percentage of fractures falling within the normal range for some measurements decreased for several fracture types (Tables 2–4), which indicated a potential loss of reduction. When the change in measurement for each parameter was less than the standard deviation, this was most likely the result of small differences in observer measurements or changes in the rotation of the radiograph. However, when the change in measurement for each parameter from the initial to the final postoperative follow-up was greater than the standard deviation, we reanalyzed the films to evaluate for loss of reduction. A total of 25 fractures fell into this category. Of these, 19 had minimal or no loss of reduction, findings attributable to mild changes in the rotation of the radiograph. Five fractures had loss of reduction: 4 were C3 fractures and 1 was a C2 fracture. In 2 of these 4 fractures, the screws in the distal end of the plate were too short, which led to loss of fixation. One fracture had a previous fracture malunion proximal to the fracture site, which resulted in overall poor alignment of the fracture fragments. Of all radiographic parameters, radial height was least likely to be restored to normal, whereas radial inclination was the measurement least likely to be maintained within the normal range from initial follow-up to the final postoperative follow-up, especially in more complex fracture types.
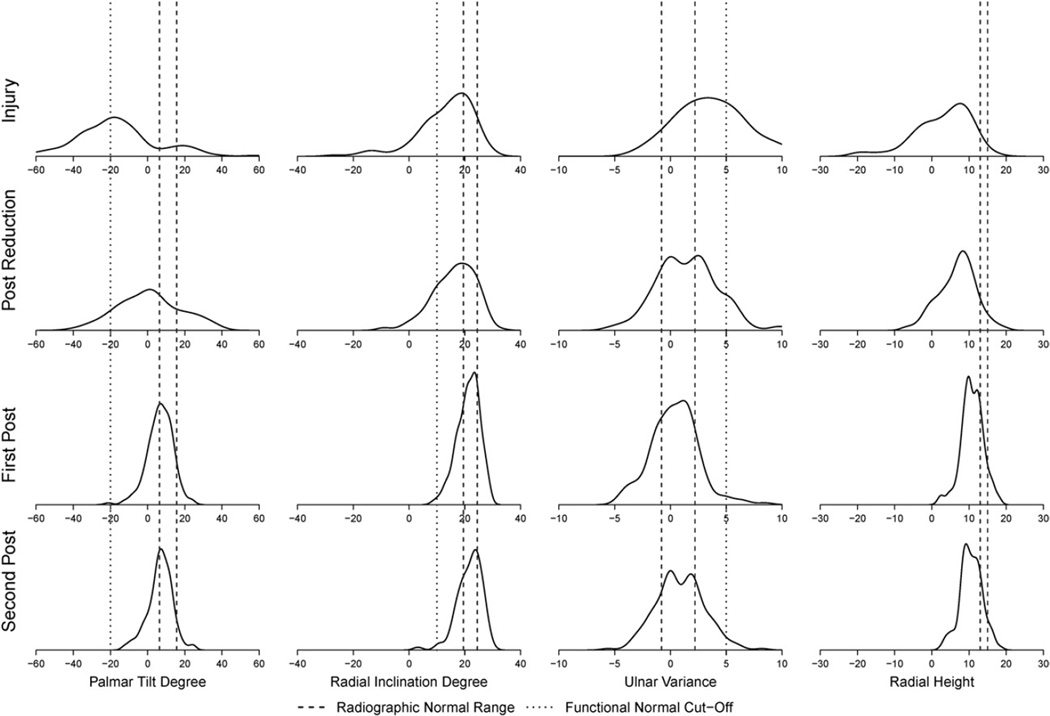
At the initial postsurgery follow-up, correction of ulnar variance was associated with Frykman classification (P = .021). Patients with Frykman types 3, 6, and 7 (intra-articular fractures involving the radiocarpal joint, distal radioulnar joint, or both) were less likely than other patients to achieve a normal ulnar variance (Table 3). At the final follow-up, only correction of volar tilt was associated with AO classification (P = .019). Patients with AO classifications of C1 to C3 (complex, intra-articular fractures) were less likely than others to achieve a normal measure of volar tilt (Table 4). Figure 2 shows the distributions of each measurement and how they compared with the radiographic norm and also with the acceptable functional range from the time of injury to the second postoperative follow-up. Whereas the group as a whole approached the radiographic norm for each measurement, many fractures did not achieve a measurement within the normal range.
FIGURE 2.
Distribution of palmar tilt, radial inclination, ulnar variance, and radial height over time 4 points: injury, postreduction, first postoperative follow-up, and second postoperative follow-up. Radiographic normal range (volar tilt, 11°; radial inclination, 22°; ulnar variance, 0.7 mm; and radial height, 14 mm) and functional normal range (≤ 20° dorsal angulation, ≥ 10° radial inclination, ≤ 5 mm ulnar variance) are depicted.
DISCUSSION
Many studies have illustrated the importance of achieving anatomic reduction of distal radius fractures in terms of functional outcome and preservation of the normal biomechanics of the wrist. In 1951, Gartland and Werley30 demonstrated that acceptable reduction of distal radius fractures was based on restoration of volar tilt to 11° and radial inclination to 23° after closed reduction.7, 31 Porter and Stockley29 demonstrated that poorly reduced fractures (> 20° of dorsal angulation and/or < 10° of radial inclination) had worse outcomes with lower grip strength at 6 months and 2 years. Others have shown that in addition to decreased grip strength, dorsal angulation greater than 12° was associated with midcarpal instability, pain, decreased range of motion, and difficulty performing activities of daily living. 7, 10, 12, 14, 16, 29, 31–34
Restoration of normal radioulnar relationship has been shown to predict functional outcome after distal radius fractures as well. Mann et al16 and Altissimi et al14 demonstrated that residual ulnar-positive deformity greater than 5 mm was associated with unsatisfactory outcomes in more than 40% of patients with distal radius fractures. Changes in ulnar variance have also been associated with the development of acute scapholunate instability, ulnocarpal impaction, and radioulnar impingement.14, 15 Loss of radial height has been demonstrated to cause poor functional outcomes after fractures of the distal radius.10, 14, 35, 36
In addition to volar tilt, radial inclination, ulnar variance, and radial height, articular congruence is an important factor in the long-term outcome of fractures of the distal radius. In a retrospective review, Knirk and Jupiter17 noted that all patients who had articular stepoff of greater than 2 mm at the time of union developed radiographic evidence of posttraumatic arthritis. Only 11% of patients who had normal articular congruence at the time of union developed radiographic evidence of posttraumatic arthritis regardless of the amount of articular displacement at the time of injury. Nevertheless, the development of radiographic evidence of posttraumatic arthritis has not been shown to affect functional outcome.37
In recent years, the trend toward operative fixation of distal radius fractures reflects the negative impact that disruption of anatomical relationships and biomechanical properties of the wrist joint can have on outcomes.7 Residual dorsal angulation leads to increased torque and changes in load bearing across the radiocarpal and ulnocarpal joints.10, 14, 38 Changes in the normal volar tilt of the distal radius leads to a shift in contact points for load transfer and a significant increase in the axial load supported by the ulna and ulnocarpal joint of greater than 200%.7, 14, 36, 39 An increase or decrease in ulnar variance of as little as 1 mm can alter the biomechanics of the wrist as well. Residual ulnar-minus deformity can lead to scapholunate dissociation and excess ulnar-positive deformity can cause ulnocarpal impaction. Loss of radial height is associated with shifts in thecenterof rotation during pronation and supination, as well as an increased strain on the triangular fibrocartilage complex of up to 13%.7, 39–41
Newer techniques in plate fixation—namely, volar locked plating—have become the preferred method in treatment of these types of fractures because of their ability to help achieve and maintain stable fracture fixation despite osteoporotic or unstable or highly comminuted fractures. 4, 7, 42, 43 Martineau et al4 found open reduction internal fixation to be most successful at obtaining anatomic reduction in terms of palmar tilt, radial inclination, radial length, and articular gap/stepoff. Chen and Jupiter,7 Osada et al,43 and Cole et al44 showed that, compared with dorsal plates and nonlocking volar plates, volar locking plates provide increased biomechanical strength.
Up to 20° of dorsal angulation and a minimum of 10° of radial inclination have been shown to have acceptable functional results.29 Ulnar variance and radial height are less forgiving, with functional outcomes affected by only a few millimeters of change. In terms of articular congruence, almost no deformity is the generally accepted goal; 2 mm of stepoff is significant for the development of radiographic signs of posttraumatic arthritis.17
In our study, we demonstrated that volar locked plating improved all radiographic parameters from the time of injury to postoperative follow-up. While restoration of anatomic norms was achieved in less than 50% of fractures, average correction of radiographic measurements fell within acceptable functional ranges in 88% of patients based on values from the literature of < 20° of dorsal angulation,29 > 10° of radial inclination,29 and < 5 mm of ulnar variance.14, 16 Ulnar variance was the parameter most likely to be restored to normal, whereas radial height was least likely to be corrected and radial inclination was least likely to be maintained. The vast majority (> 90%) of fractures were reduced with less than 2 mm of articular stepoff. Although the more complex, intra-articular fractures were less likely to achieve normal radiographic parameters, because of the small sample size available for some fracture types, it was difficult to make a significant association between fracture type and radiographic outcome.
This study has some limitations. Because this is a retrospective review, the data are subject to confounding variables. Observers making radiographic measurements of volar tilt, radial inclination, ulnar variance, radial height, and articular stepoff were not blinded to results when evaluating each radiograph. In addition, our study did not include evaluation of functional outcomes. We did not compare volar locked plating with any other type of fixation, and our outcomes may have been influenced by the particular type of plate used or by the fact that we excluded more severe fracture types necessitating additional fixation (Kirschner wires, external fixators, etc). Our study was also limited because we only reviewed plain radiographs when making our measurements. Compared with computed tomography for evaluation of gap and stepoff in fractures of the distal radius, plain radiographs have been shown to underestimate the amount of articular incongruency.44 Thus, it is possible that we might have found more fractures with greater than 2 mm of articular stepoff if computed tomography scans had been used to evaluate the articular surface.
Acknowledgments
The authors thank Julie Daniels, Dr. Brandon Ramo, and Dr. Yu Shyr for assistance with this study.
The authors received support from UL1 TR000445 from NCATS (Nationalcenterfor Advancing Translational Sciences)/NIH (National Institutes of Health) for utilization of REDCap (Research Electronic Data Capture).
Footnotes
No benefits in any form have been received or will be received related directly or indirectly to the subject of this article.
REFERENCES
- 1.Gliatis JD, Plessas SJ, Davis TR. Outcome of distal radial fractures in young adults. J Hand Surg Br. 2000;25(6):535–543. doi: 10.1054/jhsb.2000.0373. [DOI] [PubMed] [Google Scholar]
- 2.Konrath GA, Bahler S. Open reduction and internal fixation of unstable distal radius fractures: results using the trimed fixation system. J Orthop Trauma. 2002;16(8):578–585. doi: 10.1097/00005131-200209000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Lenoble E, Dumontier C, Goutallier D, Apoil A. Fracture of the distal radius: a prospective comparison between trans-styloid and Kapandji fixations. J Bone Joint Surg Br. 1995;77(4):562–567. [PubMed] [Google Scholar]
- 4.Martineau PA, Berry GK, Harvey EJ. Plating for distal radius fractures. Orthop Clin North Am. 2007;38(2):193–201. doi: 10.1016/j.ocl.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 5.Rikli DA, Regazzoni P. The double plating technique for distal radius fractures. Tech Hand Up Extrem Surg. 2000;4(2):107–114. doi: 10.1097/00130911-200006000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Rozental TD, Blazar PE. Functional outcome and complications after volar plating for dorsally displaced, unstable fractures of the distal radius. J Hand Surg Am. 2006;31(3):359–365. doi: 10.1016/j.jhsa.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 7.Chen NC, Jupiter JB. Management of distal radial fractures. J Bone Joint Surg Am. 2007;89(9):2051–2062. doi: 10.2106/JBJS.G.00020. [DOI] [PubMed] [Google Scholar]
- 8.Orbay JL, Fernandez DL. Volar fixation for dorsally displaced fractures of the distal radius: a preliminary report. J Hand Surg Am. 2002;27(2):205–215. doi: 10.1053/jhsu.2002.32081. [DOI] [PubMed] [Google Scholar]
- 9.Orbay JL, Fernandez DL. Volar fixed-angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg Am. 2004;29(1):96–102. doi: 10.1016/j.jhsa.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 10.Jupiter JB. Fractures of the distal end of the radius. J Bone Joint Surg Am. 1991;73(3):461–469. [PubMed] [Google Scholar]
- 11.Owen RA, Melton LJ, Johnson KA, Ilstrup DM, Riggs BL. Incidence of Colles’ fracture in a North American community. Am J Public Health. 1982;72(6):605–607. doi: 10.2105/ajph.72.6.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McQueen M, Caspers J. Colles fracture: does the anatomical result affect the final function? J Bone Joint Surg Br. 1988;70(4):649–651. doi: 10.1302/0301-620X.70B4.3403617. [DOI] [PubMed] [Google Scholar]
- 13.Lindau T, Hagberg L, Adlercreutz C, Jonsson K, Aspenberg P. Distal radioulnar instability is an independent worsening factor in distal radial fractures. Clin Orthop Relat Res. 2000;(376):229–235. doi: 10.1097/00003086-200007000-00031. [DOI] [PubMed] [Google Scholar]
- 14.Mann FA, Wilson AJ, Gilula LA. Radiographic evaluation of the wrist: what does the hand surgeon want to know? Radiology. 1992;184(1):15–24. doi: 10.1148/radiology.184.1.1609073. [DOI] [PubMed] [Google Scholar]
- 15.Steyers CM, Blair WF. Measuring ulnar variance: a comparison of techniques. J Hand Surg Am. 1989;14(4):607–612. doi: 10.1016/0363-5023(89)90175-5. [DOI] [PubMed] [Google Scholar]
- 16.Altissimi M, Antenucci R, Fiacca C, Mancini GB. Long-term results of conservative treatment of fractures of the distal radius. Clin Orthop Relat Res. 1986;(206):202–210. [PubMed] [Google Scholar]
- 17.Knirk JL, Jupiter JB. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am. 1986;68(5):647–659. [PubMed] [Google Scholar]
- 18.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. [Accessed September 21, 2011];REDCap (Research Electronic Data Capture) [product information] http://www.project-redcap.org/.
- 20.Alffram PA, Bauer GC. Epidemiology of fractures of the forearm: a biomechanical investigation of bone strength. J Bone Joint Surg Am. 1962;(44):105–114. [PubMed] [Google Scholar]
- 21.Frykman G. Fracture of the distal radius including sequelae—shoulder-hand-finger syndrome, disturbance in the distal radio-ulnar joint and impairment of nerve function: a clinical and experimental study. Acta Orthop Scand. 1967;(108):103. doi: 10.3109/ort.1967.38.suppl-108.01. [DOI] [PubMed] [Google Scholar]
- 22.Kreder HJ, Hanel DP, McKee M, Jupiter J, McGillivary G, Swiontkowski MF. Consistency of AO fracture classification for the distal radius. J Bone Joint Surg Br. 1996;78(5):726–731. [PubMed] [Google Scholar]
- 23.Mueller M, Nazarian S, Koch P, Schatzker J. The comprehensive classification of long bones. New York (NY): Springer-Verlag; 1990. [Google Scholar]
- 24.Medoff RJ. Essential radiographic evaluation for distal radius fractures. Hand Clin. 2005;21(4):279–288. doi: 10.1016/j.hcl.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 25.Friberg S, Lundström B. Radiographic measurements of the radiocarpal joint in normal adults. Acta Radiol Diagn (Stockh) 1976;17(2):249–256. doi: 10.1177/028418517601700212. [DOI] [PubMed] [Google Scholar]
- 26.Mekhail AO, Ebraheim NA, McCreath WA, Jackson WT, Yeasting RA. Anatomic and x-ray film studies of the distal articular surface of the radius. J Hand Surg Am. 1996;21(4):567–573. doi: 10.1016/S0363-5023(96)80005-0. [DOI] [PubMed] [Google Scholar]
- 27.Jung JM, Baek GH, Kim JH, Lee YH, Chung MS. Changes in ulnar variance in relation to forearm rotation and grip. J Bone Joint Surg Br. 2001;83(7):1029–1033. doi: 10.1302/0301-620x.83b7.11062. [DOI] [PubMed] [Google Scholar]
- 28.Mann FA, Raissdana SS, Wilson AJ, Gilula LA. The influence of age and gender on radial height. J Hand Surg Am. 1993;18(4):711–713. doi: 10.1016/0363-5023(93)90324-v. [DOI] [PubMed] [Google Scholar]
- 29.Porter M, Stockley I. Fractures of the distal radius: intermediate and end results in relation to radiologic parameters. Clin Orthop Relat Res. 1987;(220):241–252. [PubMed] [Google Scholar]
- 30.Gartland JJ, Werley CW. Evaluation of healed Colles’ fractures. J Bone Joint Surg Am. 1951;33(4):895–907. [PubMed] [Google Scholar]
- 31.Rubinovich RM, Rennie WR. Colles’ fracture: end results in relation to radiologic parameters. Can J Surg. 1983;26(4):361–363. [PubMed] [Google Scholar]
- 32.Fernandez DL. Correction of post-traumatic wrist deformity in adults by osteotomy, bone-grafting, and internal fixation. J Bone Joint Surg Am. 1982;64(8):1164–1178. [PubMed] [Google Scholar]
- 33.Jupiter JB, Masem M. Reconstruction of post-traumatic deformity of the distal radius and ulna. Hand Clin. 1988;4(3):377–390. [PubMed] [Google Scholar]
- 34.Taleisnik J, Watson HK. Midcarpal instability caused by malunited fractures of the distal radius. J Hand Surg Am. 1984;9(3):350–357. doi: 10.1016/s0363-5023(84)80222-1. [DOI] [PubMed] [Google Scholar]
- 35.Solgaard S. Function after distal radius fracture. Acta Orthop Scand. 1988;59(1):39–42. doi: 10.3109/17453678809149341. [DOI] [PubMed] [Google Scholar]
- 36.Czitrom AA, Dobyns JH, Linscheid RL. Ulnar variance in carpal instability. J Hand Surg Am. 1987;12(2):205–208. doi: 10.1016/s0363-5023(87)80272-1. [DOI] [PubMed] [Google Scholar]
- 37.Forward DP, Davis TR, Sithole JS. Do young patients with malunited fractures of the distal radius inevitably develop symptomatic post-traumatic arthritis? J Bone Joint Surg Br. 2008;90(5):629–637. doi: 10.1302/0301-620X.90B5.19448. [DOI] [PubMed] [Google Scholar]
- 38.Short WH, Palmer AK, Werner FW, Murphy DJ. A biomechanical study of distal radial fractures. J Hand Surg Am. 1987;12(4):529–534. doi: 10.1016/s0363-5023(87)80202-2. [DOI] [PubMed] [Google Scholar]
- 39.Adams BD. Effects of radial deformity on distal radioulnar joint mechanics. J Hand Surg Am. 1993;18(3):492–498. doi: 10.1016/0363-5023(93)90098-N. [DOI] [PubMed] [Google Scholar]
- 40.Pogue DJ, Viegas SF, Patterson RM, Peterson PD, Jenkins DK, Sweo TD, et al. Effects of distal radius fracture malunion on wrist joint mechanics. J Hand Surg Am. 1990;15(5):721–727. doi: 10.1016/0363-5023(90)90143-f. [DOI] [PubMed] [Google Scholar]
- 41.Short WH, Werner FW, Fortino MD, Palmer AK. Distribution of pressures and forces on the wrist after simulated intercarpal fusion and Kienböck’s disease. J Hand Surg Am. 1992;17(3):443–449. doi: 10.1016/0363-5023(92)90345-p. [DOI] [PubMed] [Google Scholar]
- 42.Liporace FA, Gupta S, Jeong GK, Stracher M, Kummer F, Egol KA, et al. A biomechanical comparison of a dorsal 3.5-mm T-plate and a volar fixed-angle plate in a model of dorsally unstable distal radius fractures. J Orthop Trauma. 2005;19(3):187–191. doi: 10.1097/00005131-200503000-00006. [DOI] [PubMed] [Google Scholar]
- 43.Osada D, Viegas SF, Shah MA, Morris RP, Patterson RM. Comparison of different distal radius dorsal and volar fracture fixation plates: a biomechanical study. J Hand Surg Am. 2003;28(1):94–104. doi: 10.1053/jhsu.2003.50016. [DOI] [PubMed] [Google Scholar]
- 44.Cole RJ, Bindra RR, Evanoff BA, Gilula LA, Yamaguchi K, Gelberman RH. Radiographic evaluation of osseous displacement following intra-articular fractures of the distal radius: reliability of plain radiography versus computed tomography. J Hand Surg Am. 1997;22(5):792–800. doi: 10.1016/s0363-5023(97)80071-8. [DOI] [PubMed] [Google Scholar]