Abstract
Background
Higher muscle mass is associated with better outcomes and longevity in patients with chronic disease states. Imaging studies such as dual-energy X-ray absorptiometry (DEXA) are among the gold standard methods for assessing body fat and lean body mass (LBM), approximately half of which is comprised of skeletal muscle mass. Elaborate imaging devices, however, are not commonly available in routine clinical practice and therefore easily accessible and cost-effective, but reliable muscle mass biomarkers are needed. One such marker is serum creatinine, derived from muscle-based creatine, which is inexpensive and ubiquitously available, and it can serve as a biomarker of skeletal muscle mass in human subjects.
Methods and results
In 118 hemodialysis patients, we found that the 3-month averaged serum creatinine concentration correlated well with DEXA-measured LBM. The recent literature regarding serum creatinine as a surrogate of muscle mass is summarized, as is the literature concerning the use of other measures of muscle mass, such as plasma gelsolin and actin, and urinary creatinine excretion. We have also reviewed the role of dietary meat intake in serum creatinine variability along with several biomarkers of dietary meat intake (creatine, carnitine, carnosine, ophidine, anserine, 3-methyl-l-histidine and 1-methylhistidine).
Conclusion
In summary, none of these biomarkers was studied in CKD patients. We advance the hypothesis that in both health and disease, under steady state, serum creatinine can serve as a reliable muscle mass biomarker if appropriate adjustment for full or residual kidney function and dietary meat intake is undertaken.
Keywords: Serum creatinine, Hemodialysis, Protein–energy wasting (PEW), Lean body mass (LBM), Nutritional status, Skeletal muscle mass
Introduction
The accurate assessment of nutritional status and body composition is of paramount importance in providing nutritional care to patients with chronic kidney disease (CKD) and end-stage renal disease (ESRD), as malnutrition and the protein–energy wasting syndrome are among the strongest risk factors for morbidity and mortality. Body composition is typically divided into fat mass and fat-free mass also known as lean body mass (LMB). Compared to body fat mass, which stores energy in the form of adipose tissue, LBM includes muscle and visceral proteins and consists predominantly of water, protein, glycogen and minerals. In people with water retaining states, such as CKD, it is also important to assess body water volume separately from the other components of LMB. The LBM compartment therefore is heterogeneous and its measure is affected by fluctuations in water and electrolyte distribution, which are of a more dynamic nature in patients receiving renal replacement therapy [1]. Approximately half of LBM is comprised of skeletal muscle mass [2]. Recent studies suggest that higher muscle mass is associated with greater longevity in people with CKD and other chronic disease states [3, 4]. We present and summarize the recent literature regarding serum creatinine as a surrogate marker of muscle mass, show new information supporting this contention (including the results of a pilot study that examines the correlation between serum creatinine and muscle in dialysis patients) and review the literature of other markers of muscle mass and the role of dietary meat intake in creatinine variability as well as other biomarkers of meat intake.
Creatinine as a muscle mass surrogate
The accurate assessment of nutritional status and body composition is instrumental in providing optimal care to patients with chronic disease states including those with CKD. Imaging studies such as dual-energy X-ray absorptiometry (DEXA) are among the gold standard methods for assessing body composition [1, 5, 6]. However, this method requires an instrument that is not commonly available in clinical practice, and therefore other easily accessible, cost-effective and reliable markers of body composition are needed. Ideally, the measurements in a simple blood test combined with height, weight, and gender would be a convenient approach to estimate LBM including skeletal muscle mass and fat mass.
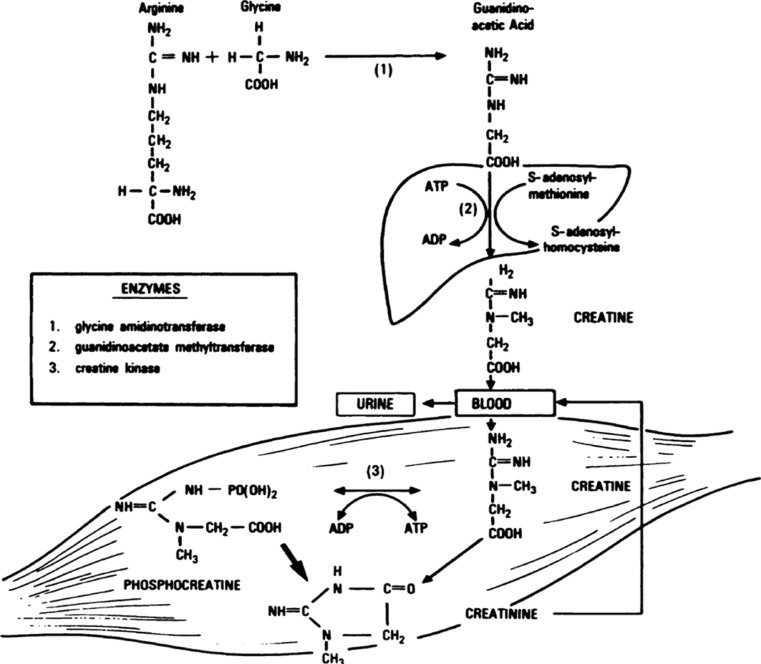
In the past few years, emerging data have revived the old notion that serum creatinine level is a reliable and cost-effective surrogate marker of muscle mass in stable chronic dialysis patients in whom kidney function is minimal to nonexistent and who maintain stable dose of dialysis therapy [4, 7–12]. Creatinine (from the Greek κρέας, flesh) is a breakdown product of creatine phosphate in muscle (see Fig. 1). Under the steady-state and stable kidney function, creatinine is usually produced at a relatively constant rate by the body depending on the absolute amount of muscle mass [13]. Creatinine is filtered out of the blood by the glomeruli (and is excreted to smaller extent in the proximal tubules of the kidney). Since there is little to no tubular reabsorption of creatinine, its renal clearance is often used to estimate glomerular filtration rate. Under stable kidney function, the serum or plasma concentration of serum creatinine can also reflect skeletal muscle mass, if its non-muscle-mass-dependent variations (such as due to renal filtration or meat intake) can be accurately accounted for. In people with stable kidney function and urine output, a 24-h urinary creatinine is usually a constant number based on skeletal muscle mass save variations due to meat intake [13].
Fig. 1.
Schematic presentation of creatinine metabolism and the pathway of breakdown of creatine phosphate in the muscle (adapted from Heymsfield et al. [13])
In the early 1980s, Schutte et al. [7] examined 24 healthy men and found that total plasma creatinine correlated strongly with urinary creatinine excretion and with weight, total body water and anthropometrically estimated LBM. Donadio et al. [5] examined 27 adult hemodialysis patients and found LBM estimated by bioelectrical impedance analysis (BIA) and DEXA correlated well with serum creatinine. In addition, Keshaviah et al. [8] supported these results showing a strong relationship between serum creatinine level and skeletal muscle mass in peritoneal dialysis patients. Recently, Noori et al. [12] examined the correlation of DEXA-measured LBM and predicted LBM based on serum concentrations of creatinine and anthropometric measurements, such as mid-arm muscle circumference (MAMC) and handgrip strength (HGS), in 118 randomly selected hemodialysis patients who underwent extensive clinical and nutritional evaluation including DEXA and 725 hemodialysis patients in whom LBM was estimated using the portable near-infrared (NIR) technique. In this latter study, serum creatinine, MAMC and HGS displayed the highest correlations with LBM. The authors developed three regression equations based on serum creatinine, MAMC and HGS to estimate LBM [12]. In women, there was less bias with serum creatinine and MAMC compared to other methods [12]. Nevertheless, serum creatinine-based equation to estimate LBM was reliable and practical in this study.
Pilot study of serum creatinine as a muscle mass surrogate in dialysis patients
We studied hemodialysis patients who participated in the Nutritional and Inflammatory Evaluation in Dialysis (NIED) Study [14]. The original patient cohort was derived over 5 years (2001–2006) from a pool of approximately 3000 hemodialysis outpatients in eight chronic dialysis facilities in the South Bay area of Los Angeles [15–22]. Included were 893 hemodialysis outpatients who had been undergoing hemodialysis treatment for at least 8 weeks, who were 18 years or older and who gave informed consent. Participants with acute infections or an anticipated life expectancy of less than 6 months (e.g., due to a metastatic malignancy or advanced HIV/AIDS disease) were excluded. The body composition of 757 of these patients was measured using the portable NIR technique in the dialysis clinics, and 725 of the patients also had triceps skinfold thickness (TSF), mid-arm muscle circumference and serum creatinine measurements. One out of every five of these patients, selected randomly underwent additional testing in the General Clinical Research Center (GCRC) on the Harbor-UCLA campus that included DEXA and other body composition measures. Hence, 118 patients participated this pilot body composition substudy, which took place on the day after their routine hemodialysis treatment.
The reference test for assessment of body composition was DEXA performed with a Hologic Series Delphi-A Fan [23] Beam X-ray Bone Densitometer with software version 12.4 (Hologic, Bedford, MA, USA). Measurements were performed as previously described [1, 5, 6] with participants wearing a hospital gown, with no metal snaps, and all artifacts removed. Participants laid supine on the table and were centered in the scan field with arms at their sides, palms down and thighs separated. Legs were rotated inward 25° until their toes touched each other and then taped together to maintain this position. Scans were analyzed using the whole body fan beam method to determine lean mass, fat mass, bone mineral content and % total body fluid. Monthly predialysis serum creatinine concentrations were measured on a mid-week day.
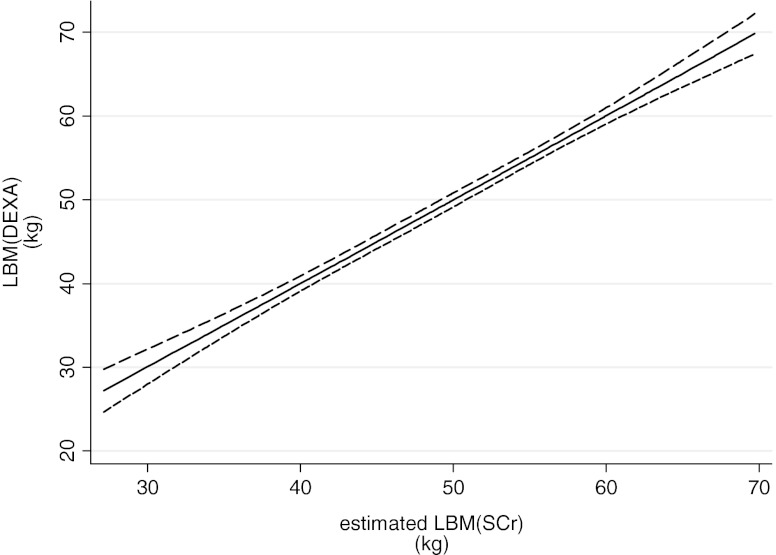
Table 1 shows the general characteristics of the study population in both the larger NIR cohort (n = 725) and the smaller DEXA sub-cohort (n = 118). Patients in the main cohort were slightly older than the DEXA sub-cohort and included fewer men and African-Americans compared to the DEXA sub-cohort. Table 2 illustrates differences based on plot-based analyses and provides the correlation test results between DEXA-measured LBM and the LBM derived from three previously described regression equations using serum creatinine, HGS and mid-arm muscle circumference (MAMC) [12]. Compared to DEXA, all three equations appear to accurately estimate the LBM. All three methods tended to underestimate LBM among participants with higher LBM. Figure 2 shows the association between LBM and serum creatinine based on the prediction models [12]. Figure 3 depicts cubic splines that illustrate the association between the DEXA-measured LBM and the LBM estimated by each of the three regression equations based on serum creatinine, MAMC and HGS. The association with serum creatinine was strong, linear and with narrow confidence intervals.
Table 1.
Demographic and clinical characteristics of 725 HD patients in the main NIR cohort and 118 HD patients in the DEXA sub-cohort upon body composition measurement
| Main NIR cohort (n = 725) | DEXA sub-cohort (n = 118) | |
|---|---|---|
| AGE | 54 ± 15 | 49 ± 12 |
| Men (%) | 53 | 57 |
| Diabetes (%) | 53 | 52 |
| African-American (%) | 31 | 40 |
| Weight (kg) | 72.4 ± 18.9 | 74.5 ± 18.4 |
| Height (inch) | 65.2 ± 4.3 | 65.3 ± 4.1 |
| Body mass index (kg/m2) | 26.5 ± 6.1 | 27.0 ± 6.0 |
| DEXA LBM (kg) | n/a | 49.8 ± 9.9 |
| NIR LBM (kg) | 51.9 ± 10.9 | n/a |
| Dialysis vintage (months) | 30.8 ± 33.6 | 41.1 ± 32.9 |
| Dialysis dose (Kt/V) | 1.6 ± 0.3 | 1.7 ± 0.3 |
| nPNA (gr/kg/day) | 1.06 ± 0.24 | 1.1 ± 0.2 |
| Blood hemoglobin (gr/dl) | 12.0 ± 0.9 | 12.2 ± 0.7 |
| Serum albumin (gr/dl) | 3.8 ± 0.4 | 4.0 ± 0.3 |
| Creatinine (mg/dl) | 10.2 ± 3.3 | 10.8 ± 3.0 |
| Urea nitrogen (mg/dl) | 63.3 ± 15.1 | 63.0 ± 16.2 |
Values are presented as mean ± standard deviation or percentage
nPNA Normalized protein nitrogen appearance
Table 2.
Difference plot (based on modified Bland-Altman tests) comparing DEXA-measured LBM and each of the three estimates of the LBM using serum creatinine, MAMC and HGS in 118 HD patients
| LBM (kg) estimated by variables | Limits of agreement | Mean difference (95 % CI) | Correlation* (r) | Correlation P-value |
|---|---|---|---|---|
| All (n = 118) | ||||
| SCr | −6.7 to 6.7 | 0.0 (−0.6,0.6) | 0.34 | <0.001 |
| MAMC | −7.0 to 7.0 | 0.0 (−0.7, 0.7) | 0.35 | <0.001 |
| HGS | −7.0 to 7.0 | 0.0 (−0.6, 0.6) | 0.35 | <0.001 |
*Pearson correlation between difference and DEXA values.
DEXA Dual energy X-ray absorptiometry, MAMC mid-arm muscle circumference, HGS handgrip strength, SCr serum creatinine
Fig. 2.
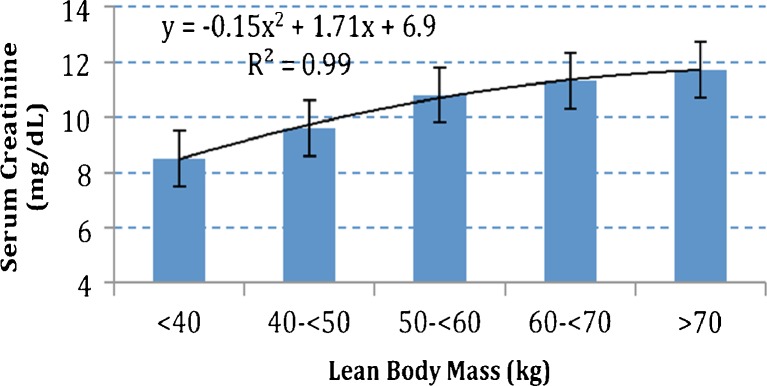
Association between LBM and serum creatinine in 118 hemodialysis patients
Fig. 3.
Spline model with 95 % confidence interval reflecting correlation between the LBM-measured by DEXA and estimated LBM values by a regression equation using serum creatinine (SCr) in 118 long-term hemodialysis patients (adapted from Noori et al. [12])
Serum creatinine as a muscle surrogate in the literature
Table 3 shows some recent studies where serum creatinine was used as a surrogate marker of LBM and/or skeletal muscle mass. Despite their variable results, most studies show that serum creatinine correlate well measures of muscle mass. Additionally, there has been a sizeable literature demonstrating that low LBM in the dialysis population is associated with increased mortality.
Table 3.
Selected studies where serum creatinine (SCr) concentration has been used as a muscle mass surrogate
| Authors, year | Population | Study goals | Findings/conclusions | Better biomarker for muscle mass |
|---|---|---|---|---|
| Keshaviah et al. [8], 1994 | 17 (healthy), 27 (HD) and 71 (PD) patients | To compare different techniques to assess LBM | There was no statistical difference between the total body water and creatinine kinetics techniques, but the bio-impedance values were systematically higher than those obtained by the kinetic technique. | |
| Heimburger et al. [60], 2000 | 115 CKD patients | 1. To assess the prevalence of malnutrition and to study the relationship between various nutritional parameters in CKD patients. | 1. HGS showed a strong correlation with DEXA measured LBM and low HGS was the factor with the strongest independent association with malnutrition. | HGS > albumin, transthyretin, urine creatinine |
| Kaizu et al. [61], 2002 | 46 anuric HD patients | To examine the validity of the creatinine kinetic method for determining creatinine production by comparing it with the direct dialysate creatinine quantification method as a means to assess protein nutritional status of hemodialysis patients. | 1. The creatinine kinetic model is a method to calculate the creatinine production rate using pre and postdialysis creatinine and was found to correlate with muscle mass estimated by Cr in dialysate and CT thigh muscle though there was some overestimation particularly in females perhaps due to no sex specific formulas or accurate volume of distribution calculation. | SCr = Cr in dialysate = CT thigh muscle > MAMC, 3 methyl-histadine |
| Oterdoom et al. [27], 2008 | 604 renal transplant patients | To investigate determinants of 24-h creatinine excretion in urine and prospectively to investigate whether 24-h creatinine excretion in urine, as measure of muscle mass is associated with mortality and graft loss in renal transplant recipients. | Urinary creatinine excretion as measure of muscle mass is associated with mortality and graft loss after renal transplantation. | UrCr |
| Donadio et al. [5], 2008 | 27 HD patients | To assess correlation of BIA with DEXA-measured LBP. | There was no difference between LBM estimated by BIA and DEXA and both correlated well with SCr. | SCr = BIA = DEXA |
| Noori et al. [11], 2010 | 742 HD patients | 1. To examine and compare the sex-specific mortality predictability of LBM and FM, assessed by the NIR interactance. | 1. In men, the lowest quartile of FM was associated with an increased risk of death where higher FM, and not LBM was associated with greater survival. | FM > LBM |
| 2. In women, higher FM and LBM was associated with greater survival. | ||||
| 3. The excess FM relative to LBM was linearly associated with greater survival in all subjects. | ||||
| 4. FM is superior to LBM in conferring survival advantages of large body size to HD patients. | ||||
| Noori et al. [4], 2010 | 792 HD patients | 1. To examine the correlations of anthropometric and biochemical measures with DEXA-measured LBM in HD patients to determine which serves as a better surrogate for LBM. | 1. MAMC (r = 0.54, P < 0.001) and SCr (r = 0.36, P < 0.01) had the strongest correlations with DEXA-measured LBM. | MAMC > SCr |
| 2. To study the outcome predictability of LBM estimated by MAMC and SCr and compare them with TSF. | 2. Patients with highest MAMC reported better mental health score. | |||
| 3. To examine the association of MAMC with QoL. | 3. Decreased risk of death was observed in hemodialysis patients with higher MAMC, higher SCr and higher TSF. | |||
| 4. High MAMC are associated with greater survival in patients with low TSF and in patients with high TSF thickness, thus suggesting that muscle mass may possibly be more important than peripheral body fat mass in predicting survival in HD patients. | ||||
| Kalantar-Zadeh et al. [10], 2010 | 121,762 HD patients | 1. To validate 3-month averaged pre-HD SCr as a marker for muscle mass in subgroup of 117 patients. | 1. Higher BMI (up to 45) and a higher SCr are each independently and incrementally associated with greater survival even after adjustment for nutritional status and inflammation. | SCr > BMI |
| 2. To study adjusted dry weight and SCr concentration and their changes over time as predictors of mortality in HD patients. | 2. A gain in dry weight accompanied by a concurrent increase in muscle mass (SCr) is associated with the greatest survival, whereas weight loss accompanied by loss in muscle mass bears the highest mortality. A weight loss with gain of muscle mass confers higher survival than weight gain with loss of muscle mass. | |||
| Noori et al. [12], 2011 | 118/612 (Development/validation cohort) HD patients | 1. To examine correlation between DEXA-measured LBM with SCr (3-month averaged), albumin, prealbumin, anthropometric measurements, nPNA and subjective assessment. | 1. LBM calculated by SCr, MAMC, and handgrip strength had the highest correlations with LBM calculated by DEXA and when validated by NIR interactance. | SCr > MAMC |
| 2. To develop equations to estimate LBM and compare to DEXA-measured LBM. | 2. Serum albumin and prealbumin levels did not correlate well with DEXA-measured LBM. | |||
| 3. To test validity of equations in validation cohort compared to NIR technique. | 3. LBM calculated by HGS, MAMC, SCr underestimated LBM particularly at LBM > 50 kg. | |||
| Streja et al. [26], 2011 | 10,090 renal transplant patients | 1. To examine the relationship of pretransplant BMI and SCr and post-transplant patient and graft survival. | 1. Patients with lower 3-month averaged pretransplant creatinine had higher risk of death after adjustment for inflammation and transplant data as well as higher risk of graft failure. | Cr > BMI |
| Molnar et al. [25], 2011 | 14,632 waitlisted renal transplant patients | To examine associations of BMI, pretransplant SCr as a surrogate marker of muscle mass and changes in weight with mortality in a large national cohort of transplant-waitlisted dialysis patients. | Transplant waitlisted hemodialysis patients with lower muscle mass and/or unintentional weight or muscle loss have higher mortality in this observational study. | SCr |
| Moreau-Gaudry et al. [62], 2011 | 1,205 MHD patients from Europe | To analyze the association between SCr and mortality. | BMI should not be used by itself but in conjunction with SCr as a surrogate of LBM to improve its morbid-mortality predictive power. | SCr > BMI |
| Walther et al. [63], 2012 | 81 Dialysis patients | To analyze the association between predialysis SCr and change in SCr between midweek dialysis sessions and nutritional markers and mortality. | Predialysis creatinine and interdialytic change in creatinine are both strongly associated with proxies of nutritional status and mortality in hemodialysis patients and are highly correlated. | SCr |
nPNA Normalized protein nitrogen appearance
In the general population, Oterdoom et al. [24] showed that low creatinine excretion, as an indirect measure of low muscle mass, is associated with increased incidence of cardiovascular events and all-cause mortality, independent of insulin resistance. Recently, Kalantar-Zadeh et al. [9] examined the relationship of mortality with changes in dry weight and in serum creatinine in a cohort of 121,762 hemodialysis patients followed for up to 5 years. They used a new method for calculating a composite ranking score, and confirmed that BMI (measured by 3-month averaged BMI) and serum creatinine levels (3-month averaged dialysis dose-adjusted serum creatinine concentrations) simultaneously predicted decreased mortality even after extensive multivariate adjustment (including for measures of nutritional status and inflammation) [9]. In a sub-cohort of patients in whom change could be examined, weight decline and serum creatinine decline in the setting of stable dialysis dose (indicating muscle mass loss) were both associated with increased mortality, whereas a rise in creatinine was associated with reduced mortality [9]. Concordant changes in these two body composition surrogates also predicted mortality, but analyses of discordant combinations indicated that creatinine (and thus presumably muscle mass) had a stronger impact on most patients in this cohort [9].
The above-referenced composite ranking score was also used in waitlisted dialysis patients to assess associations of serum creatinine with mortality [25]. Higher serum creatinine, as a surrogate of larger muscle mass, was independently and incrementally associated with greater survival in waitlisted dialysis patients even after extensive multivariate adjustment for available surrogates of nutritional status and inflammation. Additionally, patients with high muscle mass and low body weight reported the best survival. The concordant combination of the changes in these two body composition surrogates, if pointing in the same direction, maintained the same graded death predictability [25]. In addition, in 10,090 kidney transplant recipients with comprehensive pretransplant data as hemodialysis patients, who were followed for up to 6 years post-transplantation, higher pretransplant serum creatinine, a surrogate of muscle mass, was associated with lower mortality and graft loss, in that there was a 2.2-fold increased risk of combined death or graft loss with the pretransplant serum creatinine < 4 mg/dl, whereas a pretransplant serum creatinine≥14 mg/dl exhibited 22 % greater graft and patient survival, when compared to the reference pretransplant serum creatinine of 8 to <10 mg/dl [26]. Oterdoom et al. [27] found similar results in 604 renal transplant recipients. They found that lower creatinine excretion as a measure of muscle mass was associated with mortality and graft loss after renal transplantation, independent of insulin resistance and its related factors [27].
Inaccuracies in kidney function estimation using serum creatinine
Given the undeniable fact that serum creatinine co-varies closely with the skeletal muscle mass, its utility in estimating the glomerular filtration rate (eGFR) using such equations as the modification of diet in renal disease (MDRD) or Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) may not be an appropriate primary outcome measure when subjects exhibit weight variations during a given study [28]. In a recent study by Pergola et al. [29], the eGFR by the MDRD equation, using serum creatinine and, was the primary outcome variable. It was argued that weight loss associated reduction in skeletal muscle might have artificially increased eGFR in this study [30], although the investigators clarified that the weight loss in the intervention group did not co-vary with serum creatinine [30]. In another study, weight loss in diabetic persons reduced serum creatinine from 2.0 to 1.5 mg/dl (P < 0.05) [31], and eGFR increased by 13 ml/min. In yet another study on obesity, an 8 % weight loss increased eGFR by 8.9 ml/min by reducing serum creatinine [32]. Similarly fasting for Ramadhan increased eGFR likely due to loss of muscle [33]. Hence, muscle loss might be misrepresented as an improvement in renal function. A true creatinine clearance would be needed to substantiate true changes in GFR in such studies that examine renal function as the main outcome measure.
Other biomarkers of muscle mass
Plasma gelsolin
Plasma gelsolin is a secreted high-molecular-weight actin-binding protein that normally circulates at 190–300 mg/l and is mainly produced and secreted by myocytes [34–38]. There are two different types of gelsolin, cytoplasmic isoform and plasma isoform [38]. Plasma gelsolin binds to actin and may play a role in innate immunity neutralizing exogenous bacterial lipid mediators such as lipopolysaccharide and lipoteichoic acid [39, 40]. Similarly to stem cell transplant patients [41], critically ill surgical patients [42], major trauma [43] and septic patients [44], low plasma gelsolin is associated with increased mortality in hemodialysis patients [36]. Assuming the plasma gelsolin level is a marker of muscle mass in hemodialysis patients, the results of these observations support previous findings that protein–energy wasting has a major role in the mortality of ESRD patients [18, 45].
Circulating actin and myosin
A recent study by Lee et al. [36] imply that circulating actin is a potential surrogate of damaged muscle in dialysis patients and correlated with poor outcomes. As to whether circulating myosin is a positive or negative correlate of muscle mass or whether any meaningful association exists remains to be seen in future studies.
Urinary creatinine
In individuals whose kidney function is in steady state and still have urine output, the 24-h urinary creatinine concentration is usually a reliable surrogate of skeletal muscle mass, although it may also co-vary with the amount of dietary meat intake [13, 46]. Recently, lower urinary creatinine excretion rate has been shown to correlate with higher cardiovascular events and poorer survival in a cohort of people with coronary artery disease [3]. Ix et al. [46] have shown that urinary creatinine can be estimated with commonly available variables with little bias and moderate precision. It is important to note that many dialysis patients have minimal to no urine output, so that the urine creatinine cannot be measured in this group of patient.
Biomarkers of dietary meat intake
Given a main origin of serum creatinine being skeletal muscle-based creatine, it has long been argued that ingestion of striated muscle in form of meat, chicken and fish can increase serum creatinine level [47]. Hence, one cannot ignore the role of striated muscle ingestion, which is also rich in protein, in the forgoing discussion. This is especially the case in view of our own previous publications that show that higher protein intake and better nutritional status is associated with higher serum creatinine levels and greater survival [48]. As one instance of this, we have already reported that greater appetite is positively associated with survival in these hemodialysis patients [49]. Greater appetite is most likely associated with greater ingestion of striated muscle, which can increase serum creatinine. Hence, when serum creatinine is used as a surrogate of muscle mass, it is important that dietary meat intake can be accounted for. A recently published paper by Dragsted [50] has summarized the most important biomarkers of meat intake in healthy populations [50]. We summarize the some of these markers in healthy patients and in ESRD patients.
Creatine
Creatine, the precursor of creatinine, is a nitrogenous organic acid that occurs naturally in vertebrates and contributes to energy supply to muscle cells (see Fig. 1). Creatine is produced in the vertebrate body from amino acids l-arginine, glycine and l-methionine primarily in the kidney and liver. It is transported in the blood for use by muscle cells. Approximately 95 % of the human body’s total creatine is located in skeletal muscle (Fig. 1). In humans, approximately half of stored creatine originates from ingested meat. In healthy people, daily consumption of meat increases serum creatine level [51]. Serum creatine would therefore seem to be a promising marker for meat and fish intake, although correction for muscle mass measured by other techniques would be required for quantitative estimates [50]. However, we are unaware of any study examining creatine as a marker of meat intake in CKD or ESRD patients.
Carnitine
Serum carnitine level is lower in vegetarians [52] and in patients on parenteral diet [53] than in omnivores, suggesting that serum carnitine is a potential marker of meat intake. However, it is not clear that carnitine is a marker of meat intake in hemodialysis patients, in whom the supplementation of carnitine may or may not have an impact on the cardiovascular system [54].
Carnosine
The dipeptide beta-alanyl-histidine (carnosine) is present in muscle and nerve tissues in most vertebrates, although levels are low in most kinds of fish. Since dietary intake of nerve tissues is limited, carnosine might be a potential marker of muscle intake from animals, fish and shellfish [50, 55]. Similarly to other abovementioned markers, it is not known whether carnosine is a good marker of meat intake in ESRD patients.
Ophidine and anserine
Anserine (beta-alanyl-1-methyl-l-histidine), a dipeptide similar to carnitine and ophidine, is present in skeletal muscle from many types of vertebrate animals [55]. Human muscle does not contain anserine, which could therefore be a good candidate to measure meat intake in ESRD patients [56]. We are not aware of any study about the use of these markers of meat intake in in the setting of renal dysfunction.
3-Methyl-l-histidine and 1-methylhistidine
Another potential marker of dietary meat intake is 1-methylhistidine which has a long elimination half-life in healthy persons (17 h) and could therefore serve as a good marker of meat intake from the past several days prior to its level measurement [57, 58].Moreover, 3-methyl-l-histidine is a degradation product of actin and myosin, the major components of meat. As 3-methyl-l-histidine can originate from endogenous muscle sources, it would be an unreliable marker of meat intake [59].There are currently no data regarding the role of these molecules as markers of meat intake in CKD or ESRD patients.
Conclusions
Serum creatinine is a reliable, cheap, and easily accessible marker of muscle mass in stable chronic dialysis patients. Using serum creatinine as a surrogate marker of skeletal muscle mass, it has been proven that muscle mass is an important predictor of survival in dialysis patients. While several new biomarkers have been proposed as surrogate markers of muscle mass, currently, there is not enough evidence to support the clinical use of these molecules for this purpose. By simultaneously measuring serum creatinine, another kidney filtration marker (such as Cystatin C) and a dietary meat intake marker, we should be able to develop equations that can reliably estimate total muscle mass in both healthy people and patients with chronic disease states. Our research groups is currently engaged in developing such approaches, given the importance of both quality and quantity of skeletal muscle mass and emerging pharmaceutical interventions to module and improve muscle status in health and disease.
Acknowledgement
We thank DaVita Clinical Research for providing the clinical data, analysis and review for this research project. The authors of this manuscript certify that they comply with the ethical guidelines for authorship and publishing in the Journal of Cachexia, Sarcopenia and Muscle [64].
Funding Sources
This study was supported by KKZ’s research grants from the National Institutes of Health, National Institute of Diabetes, Digestive and Kidney Disease grant R01-DK078106, R21-DK078012 and K24-DK091419; a research grant from DaVita; a General Clinical Research Center grant # M01-RR00425 from the National Centers for Research Resources, National Institutes of Health; and a philanthropic grant from Mr. Harold C. Simmons. MZM received grants from the National Developmental Agency (KTIA-OTKA-EU 7KP-HUMAN-MB08-A-81231) from the Research and Technological Innovation Fund, and is recipient of the Hungarian Eötvös Scholarship (MÖB/77-2/2012).
Conflict of Interests
None
Footnotes
Patel and Molnar contributed equally to this article.
References
- 1.Kamimura MA, Avesani CM, Cendoroglo M, Canziani ME, Draibe SA, Cuppari L. Comparison of skinfold thicknesses and bioelectrical impedance analysis with dual-energy X-ray absorptiometry for the assessment of body fat in patients on long-term haemodialysis therapy. Nephrol Dial Transplant. 2003;18:101–5. doi: 10.1093/ndt/18.1.101. [DOI] [PubMed] [Google Scholar]
- 2.Lee RC, Wang Z, Heo M, Ross R, Janssen I, Heymsfield SB. Total-body skeletal muscle mass: development and cross-validation of anthropometric prediction models. Am J Clin Nutr. 2000;72:796–803. doi: 10.1093/ajcn/72.3.796. [DOI] [PubMed] [Google Scholar]
- 3.Ix JH, de Boer IH, Wassel CL, Criqui MH, Shlipak MG, Whooley MA. Urinary creatinine excretion rate and mortality in persons with coronary artery disease: the heart and soul study. Circulation. 2010;121:1295–303. doi: 10.1161/CIRCULATIONAHA.109.924266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Noori N, Kopple JD, Kovesdy CP, Feroze U, Sim JJ, Murali SB, et al. Mid-arm muscle circumference and quality of life and survival in maintenance hemodialysis patients. Clin J Am Soc Nephrol. 2010;5:2258–68. doi: 10.2215/CJN.02080310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Donadio C, Halim AB, Caprio F, Grassi G, Khedr B, Mazzantini M. Single- and multi-frequency bioelectrical impedance analyses to analyse body composition in maintenance haemodialysis patients: comparison with dual-energy X-ray absorptiometry. Physiol Meas. 2008;29:S517–24. doi: 10.1088/0967-3334/29/6/S43. [DOI] [PubMed] [Google Scholar]
- 6.Negri AL, Barone R, Veron D, Fraga A, Arrizurieta E, Zucchini A, et al. Lean mass estimation by creatinine kinetics and dual-energy X-ray absorptiometry in peritoneal dialysis. Nephron Clin Pract. 2003;95:c9–14. doi: 10.1159/000073013. [DOI] [PubMed] [Google Scholar]
- 7.Schutte JE, Longhurst JC, Gaffney FA, Bastian BC, Blomqvist CG. Total plasma creatinine: an accurate measure of total striated muscle mass. J Appl Physiol. 1981;51:762–6. doi: 10.1152/jappl.1981.51.3.762. [DOI] [PubMed] [Google Scholar]
- 8.Keshaviah PR, Nolph KD, Moore HL, Prowant B, Emerson PF, Meyer M, et al. Lean body mass estimation by creatinine kinetics. J Am Soc Nephrol. 1994;4:1475–85. doi: 10.1681/ASN.V471475. [DOI] [PubMed] [Google Scholar]
- 9.Kalantar-Zadeh K, Streja E, Molnar MZ, Lukowsky LR, Krishnan M, Kovesdy CP, et al. Mortality prediction by surrogates of body composition: an examination of the obesity paradox in hemodialysis patients using composite ranking score analysis. Am J Epidemiol. 2012;175:793–803. doi: 10.1093/aje/kwr384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kalantar-Zadeh K, Streja E, Kovesdy CP, Oreopoulos A, Noori N, Jing J, et al. The obesity paradox and mortality associated with surrogates of body size and muscle mass in patients receiving hemodialysis. Mayo Clinic Proc. 2010;85:991–1001. doi: 10.4065/mcp.2010.0336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Noori N, Kovesdy CP, Dukkipati R, Kim Y, Duong U, Bross R, et al. Survival predictability of lean and fat mass in men and women undergoing maintenance hemodialysis. Am J Clin Nutr. 2010;92:1060–70. doi: 10.3945/ajcn.2010.29188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Noori N, Kovesdy CP, Bross R, Lee M, Oreopoulos A, Benner D, et al. Novel equations to estimate lean body mass in maintenance hemodialysis patients. Am J Kidney Dis. 2011;57:130–9. doi: 10.1053/j.ajkd.2010.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heymsfield SB, Arteaga C, McManus C, Smith J, Moffitt S. Measurement of muscle mass in humans: validity of the 24-hour urinary creatinine method. Am J Clin Nutr. 1983;37:478–94. doi: 10.1093/ajcn/37.3.478. [DOI] [PubMed] [Google Scholar]
- 14.Colman S, Bross R, Benner D, Chow J, Braglia A, Arzaghi J, et al. The nutritional and inflammatory evaluation in dialysis patients (NIED) study: overview of the NIED study and the role of dietitians. J Ren Nutr. 2005;15:231–43. doi: 10.1053/j.jrn.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 15.Rambod M, Kovesdy CP, Bross R, Kopple JD, Kalantar-Zadeh K. Association of serum prealbumin and its changes over time with clinical outcomes and survival in patients receiving hemodialysis. Am J Clin Nutr. 2008;88:1485–94. doi: 10.3945/ajcn.2008.25906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kalantar-Zadeh K, Kopple JD, Kamranpour N, Fogelman AM, Navab M. HDL-inflammatory index correlates with poor outcome in hemodialysis patients. Kidney Int. 2007;72:1149–56. doi: 10.1038/sj.ki.5002491. [DOI] [PubMed] [Google Scholar]
- 17.Bross R, Zitterkoph J, Pithia J, Benner D, Rambod M, Kovesdy CP, et al. Association of serum total iron-binding capacity and its changes over time with nutritional and clinical outcomes in hemodialysis patients. Am J Nephrol. 2009;29:571–81. doi: 10.1159/000191470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rambod M, Bross R, Zitterkoph J, Benner D, Pithia J, Colman S, et al. Association of Malnutrition-Inflammation Score with quality of life and mortality in hemodialysis patients: a 5-year prospective cohort study. Am J Kidney Dis. 2009;53:298–309. doi: 10.1053/j.ajkd.2008.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shantouf R, Kovesdy CP, Kim Y, Ahmadi N, Luna A, Luna C, et al. Association of serum alkaline phosphatase with coronary artery calcification in maintenance hemodialysis patients. Clin J Am Soc Nephrol. 2009;4:1106–14. doi: 10.2215/CJN.06091108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rambod M, Kovesdy CP, Kalantar-Zadeh K. Malnutrition-Inflammation Score for risk stratification of patients with CKD: is it the promised gold standard? Nat Clin Pract Nephrol. 2008;4:354–5. doi: 10.1038/ncpneph0834. [DOI] [PubMed] [Google Scholar]
- 21.Rambod M, Kovesdy CP, Kalantar-Zadeh K. Combined high serum ferritin and low iron saturation in hemodialysis patients: the role of inflammation. Clin J Am Soc Nephrol. 2008;3:1691–701. doi: 10.2215/CJN.01070308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Raj, DS, Shah, VO, Rambod, M, Kovesdy, CP, Kalantar-Zadeh, K. Association of soluble endotoxin receptor CD14 and mortality among patients undergoing hemodialysis. Am J Kidney Dis. 2009 [e-published Sep 2009]. [DOI] [PMC free article] [PubMed]
- 23.About DCI—Introduction. In: DCI Dialysis Clinic Inc homepage (http://www.diciinc.org); 2001–2002. Nashville, TN: Dialysis Clinic.
- 24.Oterdoom LH, Gansevoort RT, Schouten JP, de Jong PE, Gans RO, Bakker SJ. Urinary creatinine excretion, an indirect measure of muscle mass, is an independent predictor of cardiovascular disease and mortality in the general population. Atherosclerosis. 2009;207:534–40. doi: 10.1016/j.atherosclerosis.2009.05.010. [DOI] [PubMed] [Google Scholar]
- 25.Molnar MZ, Streja E, Kovesdy CP, Bunnapradist S, Sampaio MS, Jing J, Krishnan M, Nissenson AR, Danovitch GM, Kalantar-Zadeh K. Associations of body mass index and weight loss with mortality in transplant-waitlisted maintenance hemodialysis patients. Am J Transplant: official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2011;11:725–36. [DOI] [PMC free article] [PubMed]
- 26.Streja E, Molnar MZ, Kovesdy CP, Bunnapradist S, Jing J, Nissenson AR, et al. Associations of pretransplant weight and muscle mass with mortality in renal transplant recipients. Clin J Am Soc Nephrol. 2011;6:1463–73. doi: 10.2215/CJN.09131010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Oterdoom LH, van Ree RM, de Vries AP, Gansevoort RT, Schouten JP, van Son WJ. Homan van der Heide, JJ, Navis, G, de Jong, PE, Gans, RO, Bakker, SJ. Urinary creatinine excretion reflecting muscle mass is a predictor of mortality and graft loss in renal transplant recipients. Transplantation. 2008;86:391–8. doi: 10.1097/TP.0b013e3181788aea. [DOI] [PubMed] [Google Scholar]
- 28.Kalantar-Zadeh, K, Amin, AN. Toward more accurate detection and risk stratification of chronic kidney disease. JAMA. 2012;307(18):1976–7. [DOI] [PubMed]
- 29.Pergola PE, Raskin P, Toto RD, Meyer CJ, Huff JW, Grossman EB, et al. Bardoxolone methyl and kidney function in CKD with type 2 diabetes. N Engl J Med. 2011;365:327–36. doi: 10.1056/NEJMoa1105351. [DOI] [PubMed] [Google Scholar]
- 30.Rogacev KS, Bittenbring JT, Fliser D. Bardoxolone methyl, chronic kidney disease, and type 2 diabetes. N Engl J Med. 2011;365:1745–6. doi: 10.1056/NEJMc1110239. [DOI] [PubMed] [Google Scholar]
- 31.Saiki A, Nagayama D, Ohhira M, Endoh K, Ohtsuka M, Koide N, et al. Effect of weight loss using formula diet on renal function in obese patients with diabetic nephropathy. Int J Obes (London). 2005;29:1115–20. doi: 10.1038/sj.ijo.0803009. [DOI] [PubMed] [Google Scholar]
- 32.Straznicky NE, Grima MT, Lambert EA, Eikelis N, Dawood T, Lambert GW, et al. Exercise augments weight loss induced improvement in renal function in obese metabolic syndrome individuals. J Hypertens. 2011;29:553–64. doi: 10.1097/HJH.0b013e3283418875. [DOI] [PubMed] [Google Scholar]
- 33.Bernieh B, Al Hakim MR, Boobes Y, Abu Zidan FM. Fasting Ramadan in chronic kidney disease patients: clinical and biochemical effects. Saudi J Kidney Dis Transplant: an official publication of the Saudi Center for Organ Transplantation. Saudi Arabia. 2010;21:898–902. [PubMed] [Google Scholar]
- 34.Kwiatkowski DJ, Mehl R, Izumo S, Nadal-Ginard B, Yin HL. Muscle is the major source of plasma gelsolin. J Biol Chem. 1988;263:8239–43. [PubMed] [Google Scholar]
- 35.Kwiatkowski DJ, Stossel TP, Orkin SH, Mole JE, Colten HR, Yin HL. Plasma and cytoplasmic gelsolins are encoded by a single gene and contain a duplicated actin-binding domain. Nature. 1986;323:455–8. doi: 10.1038/323455a0. [DOI] [PubMed] [Google Scholar]
- 36.Lee PS, Sampath K, Karumanchi SA, Tamez H, Bhan I, Isakova T, et al. Plasma gelsolin and circulating actin correlate with hemodialysis mortality. J Am Soc Nephrol. 2009;20:1140–8. doi: 10.1681/ASN.2008091008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kwiatkowski DJ, Mehl R, Yin HL. Genomic organization and biosynthesis of secreted and cytoplasmic forms of gelsolin. J Cell Biol. 1988;106:375–84. doi: 10.1083/jcb.106.2.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee PS, Bhan I, Thadhani R. The potential role of plasma gelsolin in dialysis-related protein–energy wasting. Blood Purif. 2010;29:99–101. doi: 10.1159/000245632. [DOI] [PubMed] [Google Scholar]
- 39.Bucki R, Byfield FJ, Kulakowska A, McCormick ME, Drozdowski W, Namiot Z, et al. Extracellular gelsolin binds lipoteichoic acid and modulates cellular response to proinflammatory bacterial wall components. J Immunol. 2008;181:4936–44. doi: 10.4049/jimmunol.181.7.4936. [DOI] [PubMed] [Google Scholar]
- 40.Bucki R, Georges PC, Espinassous Q, Funaki M, Pastore JJ, Chaby R, et al. Inactivation of endotoxin by human plasma gelsolin. Biochemistry. 2005;44:9590–7. doi: 10.1021/bi0503504. [DOI] [PubMed] [Google Scholar]
- 41.DiNubile MJ, Stossel TP, Ljunghusen OC, Ferrara JL, Antin JH. Prognostic implications of declining plasma gelsolin levels after allogeneic stem cell transplantation. Blood. 2002;100:4367–71. doi: 10.1182/blood-2002-06-1672. [DOI] [PubMed] [Google Scholar]
- 42.Lee PS, Drager LR, Stossel TP, Moore FD, Rogers SO. Relationship of plasma gelsolin levels to outcomes in critically ill surgical patients. Ann Surg. 2006;243:399–403. doi: 10.1097/01.sla.0000201798.77133.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mounzer KC, Moncure M, Smith YR, Dinubile MJ. Relationship of admission plasma gelsolin levels to clinical outcomes in patients after major trauma. Am J Respir Crit Care Med. 1999;160:1673–81. doi: 10.1164/ajrccm.160.5.9807137. [DOI] [PubMed] [Google Scholar]
- 44.Lee PS, Patel SR, Christiani DC, Bajwa E, Stossel TP, Waxman AB. Plasma gelsolin depletion and circulating actin in sepsis: a pilot study. PloS One. 2008;3:e3712. doi: 10.1371/journal.pone.0003712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Molnar MZ, Czira ME, Rudas A, Ujszaszi A, Lindner A, Fornadi K, et al. Association of the malnutrition–inflammation score with clinical outcomes in kidney transplant recipients. Am J Kidney Dis. 2011;58:101–8. doi: 10.1053/j.ajkd.2010.11.027. [DOI] [PubMed] [Google Scholar]
- 46.Ix JH, Wassel CL, Stevens LA, Beck GJ, Froissart M, Navis G, et al. Equations to estimate creatinine excretion rate: the CKD epidemiology collaboration. Clin J Am Soc Nephrol. 2011;6:184–91. doi: 10.2215/CJN.05030610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Preiss DJ, Godber IM, Lamb EJ, Dalton RN, Gunn IR. The influence of a cooked-meat meal on estimated glomerular filtration rate. Ann Clin Biochem. 2007;44:35–42. doi: 10.1258/000456307779595995. [DOI] [PubMed] [Google Scholar]
- 48.Shinaberger CS, Kilpatrick RD, Regidor DL, McAllister CJ, Greenland S, Kopple JD, et al. Longitudinal associations between dietary protein intake and survival in hemodialysis patients. Am J Kidney Dis. 2006;48:37–49. doi: 10.1053/j.ajkd.2006.03.049. [DOI] [PubMed] [Google Scholar]
- 49.Kalantar-Zadeh K, Block G, McAllister CJ, Humphreys MH, Kopple JD. Appetite and inflammation, nutrition, anemia, and clinical outcome in hemodialysis patients. Am J Clin Nutr. 2004;80:299–307. doi: 10.1093/ajcn/80.2.299. [DOI] [PubMed] [Google Scholar]
- 50.Dragsted LO. Biomarkers of meat intake and the application of nutrigenomics. Meat Sci. 2010;84:301–7. doi: 10.1016/j.meatsci.2009.08.028. [DOI] [PubMed] [Google Scholar]
- 51.Delanghe J, De Slypere JP, De Buyzere M, Robbrecht J, Wieme R, Vermeulen A. Normal reference values for creatine, creatinine, and carnitine are lower in vegetarians. Clin Chem. 1989;35:1802–3. [PubMed] [Google Scholar]
- 52.Krajcovicova-Kudlackova M, Simoncic R, Bederova A, Babinska K, Beder I. Correlation of carnitine levels to methionine and lysine intake. Physiol Res. 2000;49:399–402. [PubMed] [Google Scholar]
- 53.Dahlstrom KA, Ament ME, Moukarzel A, Vinton NE, Cederblad G. Low blood and plasma carnitine levels in children receiving long-term parenteral nutrition. J Pediat Gastroenterol Nutr. 1990;11:375–9. doi: 10.1097/00005176-199010000-00016. [DOI] [PubMed] [Google Scholar]
- 54.Molyneux R, Seymour AM, Bhandari S. Value of carnitine therapy in kidney dialysis patients and effects on cardiac function from human and animal studies. Curr Drug Targets. 2012;13:285–93. doi: 10.2174/138945012799201595. [DOI] [PubMed] [Google Scholar]
- 55.Undrum T, Lunde H, Gjessing LR. Determination of ophidine in human urine. J Chromatogr. 1982;227:53–9. doi: 10.1016/S0378-4347(00)80355-2. [DOI] [PubMed] [Google Scholar]
- 56.Christman AA. Determination of anserine, carnosine, and other histidine compounds in muscle extractives. Anal Biochem. 1971;39:181–7. doi: 10.1016/0003-2697(71)90474-X. [DOI] [PubMed] [Google Scholar]
- 57.Abe H, Okuma E, Sekine H, Maeda A, Yoshiue S. Human urinary excretion of L-histidine-related compounds after ingestion of several meats and fish muscle. Int J Biochem. 1993;25:1245–9. doi: 10.1016/0020-711X(93)90074-O. [DOI] [PubMed] [Google Scholar]
- 58.Sjolin J, Hjort G, Friman G, Hambraeus L. Urinary excretion of 1-methylhistidine: a qualitative indicator of exogenous 3-methylhistidine and intake of meats from various sources. Metab Clin Exp. 1987;36:1175–84. doi: 10.1016/0026-0495(87)90245-9. [DOI] [PubMed] [Google Scholar]
- 59.Rennie MJ, Phillips S, Smith K. Reliability of results and interpretation of measures of 3-methylhistidine in muscle interstitium as marker of muscle proteolysis. J Appl Physiol. 2008;105:1380–1. doi: 10.1152/japplphysiol.90782.2008. [DOI] [PubMed] [Google Scholar]
- 60.Heimburger O, Qureshi AR, Blaner WS, Berglund L, Stenvinkel P. Hand-grip muscle strength, lean body mass, and plasma proteins as markers of nutritional status in patients with chronic renal failure close to start of dialysis therapy. Am J Kidney Dis. 2000;36:1213–25. doi: 10.1053/ajkd.2000.19837. [DOI] [PubMed] [Google Scholar]
- 61.Kaizu Y, Ohkawa S, Kumagai H. Muscle mass index in haemodialysis patients: a comparison of indices obtained by routine clinical examinations. Nephrol Dial Transplant. 2002;17:442–8. doi: 10.1093/ndt/17.3.442. [DOI] [PubMed] [Google Scholar]
- 62.Moreau-Gaudry X, Guebre-Egziabher F, Jean G, Genet L, Lataillade D, Legrand E, et al. Serum creatinine improves body mass index survival prediction in hemodialysis patients: a 1-year prospective cohort analysis from the ARNOS study. J Ren Nutr. 2011;21:369–75. doi: 10.1053/j.jrn.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 63.Walther CP, Carter CW, Low CL, Williams P, Rifkin DE, Steiner RW, et al. Interdialytic creatinine change versus predialysis creatinine as indicators of nutritional status in maintenance hemodialysis. Nephrol Dial Transplant. 2012;27:771–6. doi: 10.1093/ndt/gfr389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.von Haehling S, Morley JE, Coats AJ, Anker SD. Ethical guidelines for authorship and publishing in the Journal of Cachexia, Sarcopenia and Muscle. J Cachexia Sarcopenia Muscle. 2010;1:7–8. doi: 10.1007/s13539-010-0003-5. [DOI] [PMC free article] [PubMed] [Google Scholar]