Abstract
Pulmonary lymphangioleiomyomatosis (LAM) is a rare disease found almost exclusively in women that is characterized by neoplastic growth of atypical smooth muscle-like cells in the lung, destruction of lung parenchyma, and obstruction of lymphatics. These processes lead to the formation of lung cysts, rupture of which results in spontaneous pneumothorax. Progression of LAM often results in loss of pulmonary function and death. LAM affects predominantly women of childbearing age and is exacerbated by pregnancy. The only proven treatment for LAM is lung transplantation, and even then LAM cells will often return to the transplanted lung. However, methodical and targeted approaches toward understanding LAM pathophysiology have led to the discovery of new potential therapeutic avenues. For example, the mutational inactivation of tumor suppressor complex genes tuberous sclerosis complex 1 or tuberous sclerosis complex 2 has been shown to be present in lung LAM cells. These mutations occur sporadically or in association with inherited hamartoma syndrome tuberous sclerosis (TSC). Since TSC genes function as negative regulators of the mammalian target of rapamycin, a major controller of cell growth, metabolism, and survival, rapamycin analogs have recently been used to treat LAM patients with promising results. Similarly, studies focusing on the importance of estrogen in LAM progression have suggested that anti-estrogen therapy might prove to be an alternative means of treating LAM. This minireview summarizes recent progress in understanding LAM pathophysiology, including the latest preclinical and clinical studies, and insights regarding the role of hormones in LAM.
Keywords: Simvastatin, Uterine Leiomyomas, mTORC1 Signaling, Myometrial Cell, Lymphangioleiomyomatosis
Introduction
Lymphangioleiomyomatosis (LAM), a rare genetic disorder affecting primarily women of childbearing age, is an enigmatic and devastating disease with no effective treatment. The major aspect of LAM is neoplastic LAM cell proliferation in the lung, which leads to the destruction of pulmonary connective tissue and the formation of multiple cysts, rupture of which results in spontaneous pneumothorax. Interestingly, LAM occurs almost exclusively in adult women, suggesting that hormones may play an important role in the regulation of disease pathogenesis [48, 60]. LAM is associated with high incidence of angiomyoleiomas (AMLs) that occur most frequently in kidney; extrarenal sites are liver and retroperitoneum [77]. Pulmonary LAM can occur sporadically or in association with the inherited hamartoma syndrome tuberous sclerosis (TSC) [46, 73]. In fact, LAM is regarded as the primary form of pulmonary involvement in women with TSC. One of the major advances in understanding LAM pathology was discovering that LAM cell growth is caused at least in part by mutational inactivation of the tumor suppressor genes tuberous sclerosis complex 1 (TSC1) or tuberous sclerosis complex 2 (TSC2) [6, 8, 23, 65, 72]. The subsequent discovery that TSC1/TSC2 functions as a negative regulator of the mammalian target of rapamycin (mTOR) in LAM [28, 41] has led to the promising use of rapamycin analogs in the clinic for treatment of LAM and TSC [3, 10, 22, 38, 59]. Animal studies demonstrate a mechanistic link between TSC2 loss and cystic lung destruction in LAM [29]. The estrogen requirement for TSC2-null cell survival and metastasis [84] suggests that steroid signaling may also play a role in LAM pathogenesis, and their importance is currently the focus of intense study.
Lung Pathology in LAM
In pulmonary LAM, similar to severe emphysema, the lungs contain distinctive diffuse bilateral cystic changes throughout lung parenchyma [77]. Most cysts are 0.5–2 cm in size but can be as large as 10 cm. One of the key histologic hallmarks of LAM is the presence of multinodular smooth muscle-like LAM cells. These cells are often found at the edges of cysts or along pulmonary lymphatics, but can also be located in perivascular regions. In some instances, the pulmonary cysts are lined by LAM cells. Alternatively, LAM cell bundles at the edge of a cyst form polyp-like protrusions into the cyst lumen. In advanced disease, LAM cells infiltrate bronchioli of distal airways, vessel walls, the thoracic duct, and lymph nodes of the thorax or retroperitoneum. Fibrotic tissue is usually not abundant in LAM lesions and lung.
The origin of the LAM cell in the lung is not established [9, 52]. Unlike orderly parallel or concentric patterns normally present in smooth muscle cells of airways and vasculature, LAM cells grow in haphazard manner. Although LAM cells resemble smooth muscle cells, they are morphologically heterogeneous with shapes ranging from small, round, and spindle-like, to oval and epithelioid. LAM cell masses infiltrating into lymph nodes often grow in papillary clusters of oval and round cells. Immunohistochemically, LAM cells are similar to normal smooth muscle cells and express smooth muscle α-actin, vimentin, and desmin. LAM cells are also immunopositive for the Human Melanoma Black-45 (HMB-45) antibody that recognizes a melanocyte-related protein gp100. Melanoma-associated protein CD63 and melanocytic antigen PNL2 are also detected in LAM lesions [85]. Importantly, only 20–70 % of subjects with LAM have LAM cells that are reactive for HMB-45. Furthermore, in some cases, HMB-45-positive cells show dual reactivity for urotensin II, urotensin-related peptide, and their receptor [51]. Finally, there is an inverse correlation between reactivity for melanocytic markers and proliferating rate of LAM cells [12]. Significance of LAM cell populations with different cell lineage markers and proliferating rates remains to be established. Notably, as discussed later, estrogen and progesterone receptors have been detected primarily in the nuclei of LAM cells [61].
Deregulation of Cellular Signaling and its Potential Therapeutic Targeting
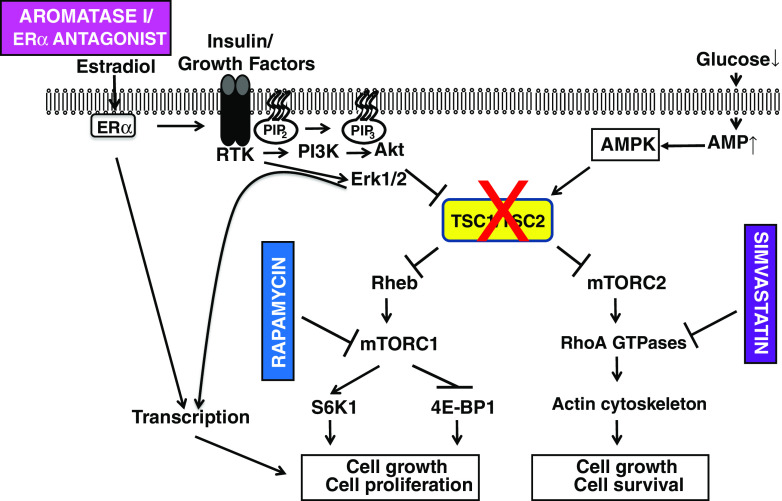
The proliferative activity of LAM cells has been attributed to the loss of function of tumor suppressor complex TSC in smooth muscle α-actin-positive LAM cells [28, 33] (Fig. 1). TSC consists of two ubiquitously and conservatively expressed proteins called hamartin (TSC1) and tuberin (TSC2) [41]. TSC1, a 130-kDa protein, binds ezrin–radexin–meozin proteins, and show activity towards Rho GTPase [54]. TSC2, a 200-kDa protein, functions as a GTPase-activating protein (GAP) toward the small GTPase Rheb [42]. GAP activity of TSC2 is regulated by two types of phosphorylation, inhibitory or activatory.
Fig. 1.
Signaling pathways that contribute to LAM cell growth and proliferation. TSC1 and TSC2 form a complex that inhibits both Rheb and mTORC2 activity. Both estrogen and growth factors trigger receptor tyrosine kinase activation, leading to activation of Erk1/2 and Akt. In addition to promoting ERα-mediated transcription, these two kinases also promote phosphorylation of TSC2, leading to loss of TSC1/TSC2-mediated inhibition of Rheb and mTORC2. Rheb GTPase then activates mTORC1, which promotes cell growth and proliferation via S6K1 and 4E-BP1 signaling. mTORC2 promotes RhoA GTPase activity, leading to rearrangements in the actin cytoskeleton followed by increased cell growth and survival. In contrast, low glucose levels lead to elevated AMP-activated kinase activity, phosphorylation of TSC2 at a different site, and increased inhibitory activity of the TSC1/TSC2 complex. In LAM cells, either TSC1 or TSC2 (usually TSC2) is inactivated, resulting in constitutive mTORC1/mTORC2 signaling and subsequent proliferation. Estradiol can also promote LAM cell proliferation through both genomic and nongenomic pathways. Notably, simvastatin, rapamycin, and inhibitors of estrogen signaling (aromatase inhibitors and ERα antagonists) can inhibit LAM proliferation at the indicated steps in the signaling pathways
Under normal growth conditions, activation of phosphatidylinositol 3-kinase-Akt or Erk1/2 by growth factors, cytokines, and hormones results in inhibitory TSC2 phosphorylation and inactivation of TSC2 GAP activity. The phosphorylation of TSC2 disrupts interaction between TSC1 and TSC2, which then attenuates its membrane localization and its inhibition of Rheb GTPase activity [7]. This, in turn, leads to Rheb-induced activation of the mTOR complex 1 (mTORC1) growth-promoting signaling [7]. TSC1 or TSC2 can be also phosphorylated by PKC and IKKβ leading to inhibition of TSC activity and activation of mTORC1 signaling [55, 57, 75].
In contrast, cellular stress conditions activate the GAP activity of TSC2, leading to suppression of Rheb and mTORC1 signaling. For example, under nutrient deprived conditions (low glucose and ATP levels), AMP-activated protein kinase (AMPK) and glycogen synthesis kinase 3 cooperatively phosphorylate TSC2 at a different site, leading to activation TSC2 GAP activity [43, 44]. GAP activation then results in Rheb GTPase inactivation and mTORC1 inhibition. Under this condition, AMPK also directly phosphorylates Raptor in mTORC1, and can interact with and phosphorylate kinase Ulk1 to initiate autophagy [13, 50].
In pulmonary LAM, loss of TSC1/TSC2 results in the constitutive activation of mTORC1 signaling, leading to unrestricted growth of LAM cells in the lung [28, 33]. Sensitivity of mTORC1 to rapamycin demonstrated in preclinical studies [28, 33, 34, 58] paved the way to promising use of rapamycin analogs in the clinic [59]. Rapamycin, however, induces only allosteric inhibition of mTOR without affecting mTOR catalytic activity, thus providing only partial inhibition of mTORC1. As such, although the rapamycin analog sirolimus markedly improved quality of life and stabilized pulmonary function in LAM patients, decline in pulmonary function resumed almost immediately upon cessation of treatment [3] [59]. In TSC patients, sirolimus induced most AML size reduction only during the first year of treatment without a marked effect during the second year [10]. This clinical evidence underscores the limitation of rapamycin and the need for novel therapeutic target(s) for treatment of LAM [24, 53].
Loss of TSC1/TSC2 in LAM and TSC not only induces uncontrolled cell growth but also affects cell viability. Primary cultures of human cells derived from LAM lungs and TSC2-null cells demonstrated insensitivity to high doses of type I interferon β (IFNβ) [26] that is known to suppress tumor progression. LAM and TSC-associated AMLs show decreased levels of type II IFNγ [15]. Requirement for IFNγ for inhibition of TSC2-null lesions was demonstrated by marked decrease of renal carcinogenesis in TSC2+/− mice crossed with IFNγ transgenic mice expressing high serum levels of IFNγ [39]. Combination of rapamycin with IFNγ has greater inhibitory effects on TSC2-null cell survival as compared to a single agent [17, 27]. Upregulation of cellular signaling including STAT1 and STAT3 is also known to be involved in tumor progression. Primary cultures of human cells derived from LAM lungs and TSC2-null cells demonstrated insensitivity to high doses of IFNβ [26], and increased STAT1 and STAT3 maintaining cell survival [17, 19, 27]. Reduction of STAT3 levels or activity sensitizes TSC2-null and human LAM-derived cells to growth inhibitory and pro-apoptotic affects of IFNγ [27]. Thus, IFN signaling may represent one of potential directions for an adjuvant therapy in LAM and TSC once drugs become available for clinical use.
Survival of TSC2-null cells depends on autophagy and its pharmacological inhibition prevents survival of TSC2-null cells and blocks TSC2-null tumors [62]. Thus, dual inhibition of mTORC1 signaling with rapamycin analogs and cell survival with drugs targeting autophagy may represent another potential therapeutic strategy for LAM and TSC.
Another potential therapeutic target is downstream of the multiprotein complex, mTORC2 [41]. The first established function of TORC2 was the rapamycin-insensitive cell cycle-dependent regulation of actin cytoskeleton through activation of Rho GTPase [67, 68]. Identification of mTORC2 in mammals confirmed its rapamycin-insensitive regulation of actin cytoskeleton through Rho GTPases RhoA and Rac1 [45, 64]. The Rho family of small GTPases consists of three major members including RhoA, Rac1, and Cdc42 [18]. In its GTP-bound state, activated RhoA promotes stress fiber and focal adhesion formation. TSC1 and TSC2 regulate RhoA and Rac1 GTPase activities in reciprocal fashion [32]. Overexpression of TSC1 promotes stress fiber formation through suppression of Rac1 [32] and activation of RhoA GTPase [54]. Loss of TSC2 similarly induces a rapamycin-insensitive increase in stress fiber formation due to TSC1-dependent activation of RhoA GTPase [31, 32]. Thus, in TSC2-null cells, mTORC2 modulates proliferation and survival through RhoA GTPase and Bcl2 proteins [30].
Importantly, geranylgeranylation of Rho GTPase, which ensures membrane localization and its activation [63], can be inhibited by statins, small molecule inhibitors of 3-hydroxy-3-methylglutaryl coenzyme A reductase [11]. Statins are a group of drugs derived either from fungi (lovastatin, simvastatin, pravastatin, and mevastatin) or made synthetically (atorvastatin and fluvastatin) with pleiotropic effects [11]. Preclinical studies of statins suggest potential differential effects on TSC2-null cells in vitro and in vivo [53]. Thus, atorvastatin inhibits growth of TSC2 −/− p53 −/− MEFs and TSC2-null ELT3 cells from Eker rat [20] but has no effect on subcutaneous tumors formed by TSC2 −/− p53 −/− MEFs in vivo [56]. In contrast, simvastatin by inhibiting Rho GTPase activity, promotes apoptosis of TSC2-null cells in vitro and in tumors in vivo [30]. Thus, combined therapy with simvastatin and rapamycin might be a potent means of blocking TSC2-null tumor progression. In fact, recent work using a mouse model of LAM provides exciting preclinical evidence supporting the use rapamycin and simvastatin together as a potential treatment of LAM [29]. This model recapitulates major features of human LAM including the constitutive activation of mTORC1, VEGF-D expression [25, 80], lymphangiogenesis [69], progressive destruction of lung parenchyma, and decreased survival. Most importantly, this model establishes a mechanistic link between loss of TSC2 and lung destruction in LAM. Interestingly, treatment of these mice with rapamycin inhibited TSC2-null lesion growth in the lung by a cytostatic mechanism, while simvastatin growth inhibitory effects on TSC2-null lesions were predominantly pro-apoptotic [29]. Simvastatin markedly inhibited expression of extracellular matrix degrading enzymes metalloproteinases and prevented alveolar destruction in mouse LAM model [29]. The combination of rapamycin and simvastatin prevented both growth of TSC2-null lesions and lung destruction by inhibiting matrix metalloproteinase expression [29]. Thus, targeting both mTORC2 and mTORC1 by a combination of pro-apoptotic simvastatin and cytostatic rapamycin shows promise for combinational therapeutic intervention in LAM. However, a retrospective study of LAM patients on statins cautions about the use of statins [14]. Thus, further preclinical and clinical studies are needed to determine potential intermolecular differences of statins, their pharmacokinecs and pharmacodynamics, and safety.
Steroid Effects on LAM Progression
Several lines of clinical evidence suggest that LAM development and progression depend on estrogen signaling. First is the notable sexual dimorphism of LAM, whereby nearly all reported cases are in women. In fact, only a handful male LAM patients have been identified and their phenotype appears to be much less severe [21, 40, 66]. In addition, LAM progression seems to increase during pregnancy [5], when estrogen levels are high, and possibly slows after menopause, when estrogen levels drop [47]. Similarly, LAM seems to worsen in women taking exogenous estrogens, such as oral contraception or hormone replacement [70, 78].
In addition to the aforementioned clinical evidence, in vitro studies further support a role for estrogen in LAM progression. First, isolated LAM cells from the lungs of LAM patients express high levels of the estrogen receptor alpha (ERα) [61], which is known to be a potent mediator of estrogen-induced proliferation in the uterus and in breast cancer. Second, estradiol treatment of these isolated human LAM cells in vitro promotes significant proliferation. Interestingly, this proliferation seems to involve both nuclear and extranuclear actions of ERα, as estradiol stimulates both transcription of proliferative genes as well as activation of Erk1/2 (most likely through transactivation of the EGF receptor [36]). In fact, MEK inhibition prevents estradiol-induced proliferation, meaning that extranuclear (nongenomic) estradiol actions are actually required for estradiol-mediated proliferation of LAM cells [16, 81]. Similarly, estradiol promotes proliferation and blocks apoptosis in cultured ELT3 leiomyoma cells [83]. These cells are derived from a uterine leiomyoma isolated from a TSC2-deficient rat called the Eker rat [79]. In fact, estrogen promotes metastasis of ELT3 cells that have been subcutaneously injected into mice [83]. As with LAM cells cultured in in vitro, MEK inhibition seems to prevent the pro-metastatic effects of estradiol on ELT3 cells, again suggesting that MEK/Erk signaling, perhaps stimulated by estradiol, is required for LAM progression. Together, these data indicate that estrogen is an important promoter of LAM progression, and that anti-estrogen therapy, either through estrogen receptor blockade or aromatase inhibition, might prove to be an effective approach in treating women with LAM. In fact, a new trial called TRAIL (Trial of Aromatase Inhibition in Lymphangioleiomyomatosis) is examining the potential use of aromatase inhibitors in the treatment of LAM.
While estradiol levels are, on average, higher in women than in men, males still produce significant amounts of estrogens. In contrast, women uniquely produce another steroid that might regulate LAM—progesterone. Like ERα, progesterone receptors are expressed in human LAM cells and in ELT3 cells derived from Eker rats [61]. Unlike estradiol, it is not clear that progesterone significantly alters proliferation of LAM and leiomyoma cells in vitro. In fact, clinically, progesterone is considered to be antiproliferative in uterine leiomyoma cells, which has led to the hypothesis that progesterone might actually be useful in preventing progression of disease in LAM patients. Thus, in some occasions over the past several years, progesterone has been used as a treatment for LAM. However, a careful retrospective analysis of LAM patients treated with various progestins suggested that, in fact, progesterone had no positive, and possibly a slightly negative, effect on LAM progression [74]. Thus, exogenous progestin is currently not recommended for patients with LAM.
The Origin of the LAM Cell
One of the most significant mysteries in LAM concerns how LAM cells appear in the lung. Do LAM cells originate in the lung or do they enter the lungs from other sites? Significant evidence suggests the latter; a metastatic nature of LAM [82]. The strongest of this evidence comes from LAM patients who have required lung transplantation due to progressive loss of lung function. Interestingly, many of these women develop recurrent LAM tumors in their lungs, and the new lesions are genetically identical to those that were present in the original lungs [1, 49]. These data suggest that the new lung LAM cells must have migrated to the lungs from other tumors within the body. Further proof comes from genetic analysis of lung LAM lesions. Careful analysis of TSC mutations in lung LAM cells demonstrated that they were identical to those found in angiomyolipoma cells, but not normal kidney cells or lymphocytes, thus suggesting a metastatic nature of these TSC-null tumor cells [8, 65, 71].
If lung LAM is indeed metastatic, then the next important question centers around the origin of these LAM cells. To begin to address this question, one must start by re-addressing the sexual dimorphism of LAM. As mentioned, the sensitivity to estradiol with regard to proliferation of metastasis suggests that the higher estrogens levels in women may partially explain the almost exclusive occurrence in women. However, men still produce significant amounts of estradiol and LAM is still discovered in anovulatory women, indicating that estradiol is not the only answer. Another possible explanation for the sexual dimorphism of LAM is related to the unique presence of a uterus in women that could serve as an origin of LAM cells. Lung LAM lesions and uterine leiomyomas share many important features, including the presence of similar appearing myometrial cell types, the expression of estrogen and progesterone receptors, and the exquisite growth sensitivity to estrogens. Interestingly, a recent study that looked carefully for the microscopic presence of LAM cells in the uterus of patients with lung LAM revealed that every patient had leiomyomas present, and all but one contained actual LAM lesions in the uterus [37].
Furthermore, LAM share similar features to another rare disease called benign metastasizing leiomyomas, a less aggressive lung disease where it is well established that uterine leiomyomas metastasize to the lungs (both lung and uterine lesions share the same genetic signatures [4, 76]), sometimes even years after uterine leiomyomas were removed surgically [2, 35]. Together, these data suggest that LAM might originate from TSC2-null myometrial cells and that estradiol may then promote proliferation and metastasis of these myometrial cells, thus explaining the overwhelming predominance of LAM in women. Notably, as in LAM, benign metastasizing leiomyoma has been reported in a handful of men, suggesting that, in very rare situations, lung leiomyomas-like lesions can form in the lungs through other mechanisms that do not involve the uterus. Further studies are needed to better characterize the metastatic nature of LAM; however, understanding how LAM reaches the lungs will almost certainly lead to new therapeutic avenues for LAM patients.
Challenges and Future Directions
As reviewed above, recent research has uncovered novel and exciting information regarding the pathogenesis and progression of LAM; however, many challenges still remain. These include definitive identification of the cell type(s) responsible for initiating LAM, and a more complete understanding regarding how steroid and mTOR signaling work together to promote LAM proliferation. More complete characterization of these important issues will undoubtedly lead to more directed and effective therapeutic interventions, and will bring hope of a cure for this rare but sometimes devastating disease.
Acknowledgments
Dr. Vera Krymskaya receives support from the NIH/NHLBI and The LAM Foundation. Dr. Stephen Hammes is supported by the LAM Foundation and the DOD. We apologize to those investigators whose important work we did not discuss for the sake of conciseness.
References
- 1.Astrinidis A, Khare L, Carsillo T, Smolarek T, Au KS, Northrup H, Henske EP. Mutational analysis of the tuberous sclerosis gene TSC2 in patients with pulmonary lymphangioleiomyomatosis. J Med Genet. 2000;37(1):55–57. doi: 10.1136/jmg.37.1.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Awonuga AO, Shavell VI, Imudia AN, Rotas M, Diamond MP, Puscheck EE. Pathogenesis of benign metastasizing leiomyoma: a review. Obstet Gynecol Surv. 2010;65(3):189–195. doi: 10.1097/OGX.0b013e3181d60f93. [DOI] [PubMed] [Google Scholar]
- 3.Bissler JJ, McCormack FX, Young LR, Elwing JM, Chuck G, Leonard JM, Schmithorst VJ, et al. Sirolimus for angiomyolipoma in tuberous sclerosis complex or lymphangioleiomyomatosis. N Engl J Med. 2008;358(2):140–151. doi: 10.1056/NEJMoa063564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bowen JM, Cates JM, Kash S, Itani D, Gonzalez A, Huang D, Oliveira A, Bridge JA. Genomic imbalances in benign metastasizing leiomyoma: characterization by conventional karyotypic, fluorescence in situ hybridization, and whole genome SNP array analysis. Cancer Genet. 2012;205(5):249–254. doi: 10.1016/j.cancergen.2012.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brunelli A, Catalini G, Fianchini A. Pregnancy exacerbating unsuspected mediastinal lymphangioleiomyomatosis and chylothorax. Int J Gynaecol Obstet. 1996;52(3):289–290. doi: 10.1016/0020-7292(95)02619-3. [DOI] [PubMed] [Google Scholar]
- 6.Cai X, Pacheco-Rodriguez G, Fan Q-Y, Haughey M, Samsel L, El-Chemaly S, Wu HP, et al. Phenotypic characterization of disseminated cells with TSC2 loss of heterozygosity in patients with lymphangioleiomyomatosis. Am J Resp Crit Care Med. 2010;182(11):1410–1418. doi: 10.1164/rccm.201003-0489OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cai S-L, Tee AR, Short JD, Bergeron JM, Kim J, Shen J, Guo R, Johnson CL, Kiguchi K, Walker CL. Activity of TSC2 is inhibited by AKT-mediated phosphorylation and membrane partitioning. J Cell Biol. 2006;173(2):279–289. doi: 10.1083/jcb.200507119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carsillo T, Astrinidis A, Henske EP. Mutations in the tuberous sclerosis complex gene TSC2 are a cause of sporadic pulmonary lymphangioleiomyomatosis. Proc Natl Acad Sci U S A. 2000;97(11):6085–6090. doi: 10.1073/pnas.97.11.6085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Darling TN, Pacheco-Rodriguez G, Gorio A, Lesma E, Walker C, Moss J. Lymphangioleiomyomatosis and TSC2−/− cells. Lymph Res Biol. 2010;8(1):59–69. doi: 10.1089/lrb.2009.0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Davies DM, de Vries PJ, Johnson SR, McCartney DL, Cox JA, Serra AL, Watson PC, et al. Sirolimus therapy for angiomyolipoma in tuberous sclerosis and sporadic lymphangioleiomyomatosis: a phase 2 trial. Clin Cancer Res. 2011;17(12):4071–4081. doi: 10.1158/1078-0432.CCR-11-0445. [DOI] [PubMed] [Google Scholar]
- 11.Demierre M-F, Peter DR, Higgins SB, Gruber EH, Lippman SM. Statins and cancer prevention. Nat Rev Cancer. 2005;5(12):930–942. doi: 10.1038/nrc1751. [DOI] [PubMed] [Google Scholar]
- 12.Dilling DF, Gilbert ER, Picken MM, Eby J, Love RB, Le Poole IC. A current viewpoint of lymphangioleiomyomatosis supporting immunotherapeutic treatment options. Am J Respir Cell Mol Biol. 2012;46:1–5. doi: 10.1165/rcmb.2011-0215TR. [DOI] [PubMed] [Google Scholar]
- 13.Egan DF, Shackelford DB, Mihaylova MM, Gelino S, Kohnz RA, Mair W, Vasquez DS, et al. Phosphorylation of ULK1 (hATG1) by AMP-activated protein kinase connects energy sensing to mitophagy. Science. 2011;331(6016):456–461. doi: 10.1126/science.1196371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.El-Chemaly S, Taveira-DaSilva A, Stylianou MP, Moss J. Statins in lymphangioleiomyomatosis: a word of caution. Eur Respir J. 2009;34(2):513–514. doi: 10.1183/09031936.00012709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.El-Hashemite N, Kwiatkowski DJ. Interferon-γ-Jak-Stat signaling in pulmonary lymphangioleiomyomatosis and renal angiomyolipoma: a potential therapeutic target. Am J Respir Cell Mol Biol. 2005;33(3):227–230. doi: 10.1165/rcmb.2005-0152RC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.El-Hashemite N, Walker V, Kwiatkowski DJ. Estrogen enhances whereas tamoxifen retards development of Tsc mouse liver hemangioma: a tumor related to renal angiomyolipoma and pulmonary lymphangioleiomyomatosis. Cancer Res. 2005;65(6):2474–2481. doi: 10.1158/0008-5472.CAN-04-3840. [DOI] [PubMed] [Google Scholar]
- 17.El-Hashemite N, Zhang H, Walker V, Hoffmeister KM, Kwiatkowski DJ. Perturbed IFN-γ-Jak-signal transducers and activators of transcription signaling in tuberous sclerosis mouse models: synergistic effects of rapamycin-IFN-γ treatment. Cancer Res. 2004;64(10):3436–3443. doi: 10.1158/0008-5472.CAN-03-3609. [DOI] [PubMed] [Google Scholar]
- 18.Etienne-Manneville S, Hall A. Rho GTPases in cell biology. Nature. 2002;420(6916):629–635. doi: 10.1038/nature01148. [DOI] [PubMed] [Google Scholar]
- 19.Fielhaber JA, Han Y-S, Tan J, Xing S, Biggs CM, Joung K-B, Kristof AS. Inactivation of mammalian target of rapamycin increases STAT1 nuclear content and transcriptional activity in {alpha}4- and protein phosphatase 2A-dependent fashion. J Biol Chem. 2009;284(36):24341–24353. doi: 10.1074/jbc.M109.033530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Finlay GA, Malhowski AJ, Liu Y, Fanburg BL, Kwiatkowski DJ, Toksoz D. Selective inhibition of growth of tuberous sclerosis complex 2 Null cells by atorvastatin is associated with impaired Rheb and Rho GTPase function and reduced mTOR/S6 kinase activity. Cancer Res. 2007;67(20):9878–9886. doi: 10.1158/0008-5472.CAN-07-1394. [DOI] [PubMed] [Google Scholar]
- 21.Fiore MG, Sanguedolce F, Lolli I, Piscitelli D, Ricco R. Abdominal lymphangioleiomyomatosis in a man with Klinefelter syndrome: the first reported case. Ann Diagn Pathol. 2005;9(2):96–100. doi: 10.1016/j.anndiagpath.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 22.Franz DN, Leonard J, Tudor C, Chuck G, Care M, Sethuraman G, Dinopoulos A, Thomas G, Crone KR. Rapamycin causes regression of astrocytomas in tuberous sclerosis complex. Ann Neurol. 2006;59(3):490–498. doi: 10.1002/ana.20784. [DOI] [PubMed] [Google Scholar]
- 23.Glasgow CG, Steagall WK, Taveira-Dasilva A, Pacheco-Rodriguez G, Cai X, El-Chemaly S, Moses M, Darling T, Moss J. Lymphangioleiomyomatosis (LAM): molecular insights lead to targeted therapies. Respir Med. 2010;104(Suppl 1):S45–S58. doi: 10.1016/j.rmed.2010.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Glasgow CG, Steagall WK, Taveira-DaSilva A, Pacheco-Rodriguez G, Xiong C, El-Chemaly S, Moses M, Thomas D, Moss J. Lymphangioleiomyomatosis (LAM): molecular insights lead to targeted therapies. Respir Med. 2010;104(Supplement 1):S45–S58. doi: 10.1016/j.rmed.2010.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Glasgow CG, Taveira-DaSilva A, Pacheco-Rodriguez G, Steagall WK, Tsukada K, Cai X, El-Chemaly S, Mos J. Involvement of lymphatics in lymphangioleiomyomatosis. Lymph Res Biol. 2009;7(4):221–228. doi: 10.1089/lrb.2009.0017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goncharova EA, Goncharov DA, Chisolm A, Spaits MS, Lim PN, Cesarone G, Khavin I, et al. Interferon β augments tuberous sclerosis complex 2 (TSC2)-dependent inhibition of TSC2-null ELT3 and human lymphangioleiomyomatosis-derived cell proliferation. Mol Pharmacol. 2008;73(3):778–788. doi: 10.1124/mol.107.040824. [DOI] [PubMed] [Google Scholar]
- 27.Goncharova EA, Goncharov DA, Damera G, Tliba O, Amrani Y, Panettieri RA, Krymskaya VP. Signal transducer and activator of transcription 3 is required for abnormal proliferation and survival of TSC2-deficient cells: relevance to pulmonary lymphangioleiomyomatosis. Mol Pharmacol. 2009;76(4):766–777. doi: 10.1124/mol.109.057042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goncharova EA, Goncharov DA, Eszterhas A, Hunter DS, Glassberg MK, Yeung RS, Walker CL, et al. Tuberin regulates p70 S6 kinase activation and ribosomal protein S6 phosphorylation: a role for the TSC2 tumor suppressor gene in pulmonary lymphangioleiomyomatosis. J Biol Chem. 2002;277:30958–30967. doi: 10.1074/jbc.M202678200. [DOI] [PubMed] [Google Scholar]
- 29.Goncharova EA, Goncharov DA, Fehrenbach M, Khavin I, Duka B, Hino O, Colby TV, et al. Prevention of alveolar destruction and airspace enlargement in a mouse model of pulmonary lymphangioleiomyomatosis (LAM) Sci Transl Med. 2012;4(154):154ra134. doi: 10.1126/scitranslmed.3003840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goncharova EA, Goncharov DA, Li H, Pimtong W, Stephen L, Khavin I, Krymskaya VP. mTORC2 is required for proliferation and survival of TSC2-null cells. Mol Cell Biol. 2011;31(12):2484–2498. doi: 10.1128/MCB.01061-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Goncharova EA, Goncharov DA, Lim PN, Noonan D, Krymskaya VP. Modulation of cell migration and invasiveness by tumor suppressor TSC2 in Lymphangioleiomyomatosis. Am J Respir Cell Mol Biol. 2006;34:473–480. doi: 10.1165/rcmb.2005-0374OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Goncharova E, Goncharov D, Noonan D, Krymskaya VP. TSC2 modulates actin cytoskeleton and focal adhesion through TSC1-binding domain and the Rac1 GTPase. J Cell Biol. 2004;167(6):1171–1182. doi: 10.1083/jcb.200405130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Goncharova EA, Goncharov DA, Spaits M, Noonan D, Talovskaya E, Eszterhas A, Krymskaya VP. Abnormal smooth muscle cell growth in LAM: role for tumor suppressor TSC2. Am J Respir Cell Mol Biol. 2006;34:561–572. doi: 10.1165/rcmb.2005-0300OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Goncharova EA, Krymskaya VP. Pulmonary lymphangioleiomyomatosis (LAM): progress and current challenges. J Cell Biochem. 2008;103:369–382. doi: 10.1002/jcb.21419. [DOI] [PubMed] [Google Scholar]
- 35.Goyle KK, Moore DF, Jr, Garrett C, Goyle V. Benign metastasizing leiomyomatosis: case report and review. Am J Clin Oncol. 2003;26(5):473–476. doi: 10.1097/01.coc.0000037737.78080.E3. [DOI] [PubMed] [Google Scholar]
- 36.Hammes SR, Levin ER. Minireview: recent advances in extranuclear steroid receptor actions. Endocrinology. 2011;152(12):4489–4495. doi: 10.1210/en.2011-1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hayashi T, Kumasaka T, Mitani K, Terao Y, Watanabe M, Oide T, Nakatani Y, et al. Prevalence of uterine and adnexal involvement in pulmonary lymphangioleiomyomatosis: a clinicopathologic study of 10 patients. Am J Surg Pathol. 2011;35(12):1776–1785. doi: 10.1097/PAS.0b013e318235edbd. [DOI] [PubMed] [Google Scholar]
- 38.Herry I, Neukirch C, Debray M-P, Mignon F, Crestani B. Dramatic effect of sirolimus on renal angiomyolipomas in a patient with tuberous sclerosis complex. Eur J Intern Med. 2007;18(1):76–77. doi: 10.1016/j.ejim.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 39.Hino O, Kobayashi T, Mitani H. Prevention of hereditary carcinogenesis. Proc Jpn Acad. 2002;78:30–32. [Google Scholar]
- 40.Hohman DW, Noghrehkar D, Ratnayake S. Lymphangioleiomyomatosis: a review. Eur J Intern Med. 2008;19(5):319–324. doi: 10.1016/j.ejim.2007.10.015. [DOI] [PubMed] [Google Scholar]
- 41.Inoki K, Guan K-L. Tuberous sclerosis complex, implication from a rare genetic disease to common cancer treatment. Hum Mol Genet. 2009;18(R1):R94–R100. doi: 10.1093/hmg/ddp032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Inoki K, Li Y, Tian X, Guan K-L. Rheb GTPase is a direct target of TSC2 GAP activity and regulates mTOR signaling. Genes Dev. 2003;17(15):1829–1834. doi: 10.1101/gad.1110003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Inoki K, Ouyang H, Zhu T, Lindvall C, Wang Y, Zhang X, Yang Q, Bennett C, Harada Y, Stankunas K. TSC2 integrates Wnt and energy signals via a coordinated phosphorylation by AMPK and GSK3 to regulate cell growth. Cell. 2006;126(5):955–968. doi: 10.1016/j.cell.2006.06.055. [DOI] [PubMed] [Google Scholar]
- 44.Inoki K, Zhu T, Guan KL. TSC2 mediates cellular energy response to control cell growth and survival. Cell. 2003;115:577–590. doi: 10.1016/S0092-8674(03)00929-2. [DOI] [PubMed] [Google Scholar]
- 45.Jacinto E, Loewith R, Schmidt A, Lin S, Ruegg MA, Hall A, Hall MN. Mammalian TOR complex 2 controls the actin cytoskeleton and is rapamycin insensitive. Nat Cell Biol. 2004;6(11):1122–1128. doi: 10.1038/ncb1183. [DOI] [PubMed] [Google Scholar]
- 46.Johnson SR. Lymphangioleiomyomatosis. Eur Respir J. 2006;27(5):1056–1065. doi: 10.1183/09031936.06.00113303. [DOI] [PubMed] [Google Scholar]
- 47.Johnson SR, Tattersfield AE. Decline in lung function in lymphangioleiomyomatosis: relation to menopause and progesterone treatment. Am J Respir Crit Care Med. 1999;160(2):628–633. doi: 10.1164/ajrccm.160.2.9901027. [DOI] [PubMed] [Google Scholar]
- 48.Juvet SC, McCormack FX, Kwiatkowski DJ, Downey GP. Molecular pathogenesis of lymphangioleiomyomatosis: lessons learned from orphans. Am J Respir Cell Mol Biol. 2006;36:398–408. doi: 10.1165/rcmb.2006-0372TR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Karbowniczek M, Astrinidis A, Balsara BR, Testa JR, Lium JH, Colby TV, McCormack FX, Henske EP. Recurrent lymphangiomyomatosis after transplantation: genetic analyses reveal a metastatic mechanism. Am J Respir Crit Care Med. 2003;167(7):976–982. doi: 10.1164/rccm.200208-969OC. [DOI] [PubMed] [Google Scholar]
- 50.Kim J, Kundu M, Viollet B, Guan K-L. AMPK and mTOR regulate autophagy through direct phosphorylation of Ulk1. Nat Cell Biol. 2011;13(2):132–141. doi: 10.1038/ncb2152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kristof AS, You Z, Han Y-S, Giaid A. Protein expression of urotensin II, urotensin-related peptide and their receptor in the lungs of patients with lymphangioleiomyomatosis. Peptides. 2010;31(8):1511–1516. doi: 10.1016/j.peptides.2010.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Krymskaya VP. Smooth muscle-like cells in lymphangioleiomyomatosis. Proc Am Thorac Soc. 2008;5:119–126. doi: 10.1513/pats.200705-061VS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Krymskaya VP. Treatment option(s) for pulmonary lymphangioleiomyomatosis: progress and current challenges. Am J Respir Cell Mol Biol. 2012;46(5):563–565. doi: 10.1165/rcmb.2011-0381ED. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lamb RF, Roy C, Diefenbach TJ, Vinters HV, Johnson MW, Jay DG, Hall A. The TSC1 tumour suppressor hamartin regulates cell adhesion through ERM proteins and the GTPase Rho. Nat Cell Biology. 2000;2(5):281–287. doi: 10.1038/35010550. [DOI] [PubMed] [Google Scholar]
- 55.Lee D-F, Kuo H-P, Chen C-T, Hsu J-M, Chou C-K, Wei Y, Sun H-L, et al. IKKβ suppression of TSC1 links inflammation and tumor angiogenesis via the mTOR pathway. Cell. 2007;130(3):440–455. doi: 10.1016/j.cell.2007.05.058. [DOI] [PubMed] [Google Scholar]
- 56.Lee N, Woodrum C, Nobil A, Rauktys A, Messina M, Dabora S. Rapamycin weekly maintenance dosing and the potential efficacy of combination sorafenib plus rapamycin but not atorvastatin or doxycycline in tuberous sclerosis preclinical models. BMC Pharmacol. 2009;9(1):8. doi: 10.1186/1471-2210-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ma L, Chen Z, Erdjument-Bromage H, Tempst P, Pandolfi PP. Phosphorylation and functional inactivation of TSC2 by Erk: implications for tuberous sclerosis and cancer pathogenesis. Cell. 2005;121(2):179–193. doi: 10.1016/j.cell.2005.02.031. [DOI] [PubMed] [Google Scholar]
- 58.McCormack FX. Lymphangioleiomyomatosis. Chest. 2008;133(2):507–516. doi: 10.1378/chest.07-0898. [DOI] [PubMed] [Google Scholar]
- 59.McCormack FX, Inoue Y, Moss J, Singer LG, Strange C, Nakata K, Barker AF, et al. Efficacy and safety of sirolimus in lymphangioleiomyomatosis. N Engl J Med. 2011;364:1595–1606. doi: 10.1056/NEJMoa1100391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Meraj R, Wikenheiser-Brokamp KA, Young LR, McCormack FX. Lymphangioleiomyomatosis: new concepts in pathogenesis, diagnosis, and treatment. Semin Respir Crit Care Med. 2012;33(05):486–497. doi: 10.1055/s-0032-1325159. [DOI] [PubMed] [Google Scholar]
- 61.Ohori NP, Yousem SA, Sonmez-Alpan E, Colby TV. Estrogen and progesterone receptors in lymphangioleiomyomatosis, epithelioid hemangioendothelioma, and sclerosing hemangioma of the lung. Am J Clin Pathol. 1991;96(4):529–535. doi: 10.1093/ajcp/96.4.529. [DOI] [PubMed] [Google Scholar]
- 62.Parkhitko A, Myachina F, Morrison TA, Hindi KM, Auricchio N, Karbowniczek M, Wu JJ, et al. Tumorigenesis in tuberous sclerosis complex is autophagy and p62/sequestosome 1 (SQSTM1)-dependent. Proc Natl Acad Sci. 2011;108(30):12455–12460. doi: 10.1073/pnas.1104361108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sahai E, Marshal CJ. Rho-GTPases and cancer. Nat Rev Cancer. 2002;2:133–142. doi: 10.1038/nrc725. [DOI] [PubMed] [Google Scholar]
- 64.Sarbassov DD, Ali Siraj M, Do-Hyung K, Guertin DA, Latek RR, Erdjument-Bromage H, Tempst P, Sabatini DM. Rictor, a novel binding partner of mTOR, defines a rapamycin-insensitive and raptor-independent pathway that regulates the cytoskeleton. Curr Biol. 2004;14(14):1296–1302. doi: 10.1016/j.cub.2004.06.054. [DOI] [PubMed] [Google Scholar]
- 65.Sato T, Seyama K, Fujii H, Maruyama H, Setoguchi Y, Iwakami S, Fukuchi Y, Hino O. Mutation analysis of the TSC1 and TSC2 genes in Japanese patients with pulmonary lymphangioleiomyomatosis. J Hum Genet. 2002;47(1):20–28. doi: 10.1007/s10038-002-8651-8. [DOI] [PubMed] [Google Scholar]
- 66.Schiavina M, Di Scioscio V, Contini P, Cavazza A, Fabiani A, Barberis M, Bini A, et al. Pulmonary lymphangioleiomyomatosis in a karyotypically normal man without tuberous sclerosis complex. Am J Respir Crit Care Med. 2007;176(1):96–98. doi: 10.1164/rccm.200610-1408CR. [DOI] [PubMed] [Google Scholar]
- 67.Schmelzle T, Hall MN. TOR, a central controller of cell growth. Cell. 2000;103:253–262. doi: 10.1016/S0092-8674(00)00117-3. [DOI] [PubMed] [Google Scholar]
- 68.Schmidt A, Bickle M, Beck T, Hall MN. The yeast phosphatidylinositol kinase homolog TOR2 activates RHO1 and RHO2 via the exchange factor ROM2. Cell. 1997;88:531–542. doi: 10.1016/S0092-8674(00)81893-0. [DOI] [PubMed] [Google Scholar]
- 69.Seyama K, Kumasaka T, Kurihara M, Mitani K, Sato T. Lymphangioleiomyomatosis: a disease involving the lymphatic system. Lymphat Res Biol. 2010;8(1):21–31. doi: 10.1089/lrb.2009.0018. [DOI] [PubMed] [Google Scholar]
- 70.Shen A, Iseman MD, Waldron JA, King TE. Exacerbation of pulmonary lymphangioleiomyomatosis by exogenous estrogens. Chest. 1987;91(5):782–785. doi: 10.1378/chest.91.5.782. [DOI] [PubMed] [Google Scholar]
- 71.Smolarek TA, Wessner LL, McCormack FX, Mylet JC, Menon AG, Henske EP. Evidence that lymphangiomyomatosis is caused by TSC2 mutations: chromosome 16p13 loss of heterozygosity in angiomyolipomas and lymph nodes from women with lymphangiomyomatosis. Am J Hum Genet. 1998;62(4):810–815. doi: 10.1086/301804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Smolarek TA, Wessner LL, McCormack FX, Mylet JC, Menon AG, Henske EP. Evidence that lymphangiomyomatosis is caused by TSC2 mutations: chromosome 16p13 loss of heterozygosity in angiolipomas and lymph nodes from women with lymphangiomyomatosis. Am J Hum Genet. 1998;62:810–815. doi: 10.1086/301804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Taveira-DaSilva AM, Pacheco-Rodriguez G, Moss J. The natural history of lymphangioleiomyomatosis: markers of severity, rate of progression and prognosis. Lymph Res Biol. 2010;8(1):9–19. doi: 10.1089/lrb.2009.0024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Taveira-DaSilva AM, Stylianou MP, Hedin CJ, Hathaway O, Moss J. Decline in lung function in patients with lymphangioleiomyomatosis treated with or without progesterone. Chest. 2004;126(6):1867–1874. doi: 10.1378/chest.126.6.1867. [DOI] [PubMed] [Google Scholar]
- 75.Tee AR, Manning BD, Roux PP, Cantley LC, Blenis J. Tuberous sclerosis complex gene products, tuberin and hamartin, control mTOR signaling by acting as a GTPase-activating protein complex toward Rheb. Curr Biol. 2003;13(15):1259–1268. doi: 10.1016/S0960-9822(03)00506-2. [DOI] [PubMed] [Google Scholar]
- 76.Tietze L, Gunther K, Horbe A, Pawlik C, Klosterhalfen B, Handt S, Merkelbach-Bruse S. Benign metastasizing leiomyoma: a cytogenetically balanced but clonal disease. Hum Pathol. 2000;31(1):126–128. doi: 10.1016/S0046-8177(00)80210-5. [DOI] [PubMed] [Google Scholar]
- 77.Travis WD, Colby TV, Koss MN, Rosado-de-Christenson ML, Müller NL, King TE., Jr . AFIP atlas of nontumor pathology: non-neoplastic disorders of the lower respiratory tract. Washington, DC: American Registry of Pathology; 2002. [Google Scholar]
- 78.Wahedna I, Cooper S, Williams J, Paterson IC, Britton JR, Tattersfield AE. Relation of pulmonary lymphangio-leiomyomatosis to use of the oral contraceptive pill and fertility in the UK: a national case control study. Thorax. 1994;49(9):910–914. doi: 10.1136/thx.49.9.910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Walker CL, Hunter D, Everitt JI. Uterine leiomyoma in the Eker rat: a unique model for important diseases of women. Genes Chromosome Cancer. 2003;38(4):349–356. doi: 10.1002/gcc.10281. [DOI] [PubMed] [Google Scholar]
- 80.Young LR, VanDyke R, Gulleman PM, Inoue Y, Brown KK, Schmidt LS, Linehan WM, et al. Serum vascular endothelial growth factor-D prospectively distinguishes lymphangioleiomyomatosis from other diseases. Chest. 2010;138(3):674–681. doi: 10.1378/chest.10-0573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Yu J, Astrinidis A, Howard S, Henske EP. Estradiol and tamoxifen stimulate LAM-associated angiomyolipoma cell growth and activate both genomic and nongenomic signaling pathways. Am J Physiol Lung Cell Mol Physiol. 2004;286(4):L694–L700. doi: 10.1152/ajplung.00204.2003. [DOI] [PubMed] [Google Scholar]
- 82.Yu J, Henske EP. mTOR activation, lymphangiogenesis, and estrogen-mediated cell survival: the “perfect storm” of pro-metastatic factors in LAM pathogenesis. Lymphat Res Biol. 2010;8(1):43–49. doi: 10.1089/lrb.2009.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Yu JJ, Robb VA, Morrison TA, Ariazi EA, Karbowniczek M, Astrinidis A, Wang C, et al. Estrogen promotes the survival and pulmonary metastasis of tuberin-null cells. Proc Natl Acad Sci U S A. 2009;106(8):2635–2640. doi: 10.1073/pnas.0810790106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Yu JJ, Robb VA, Morrison TA, Ariazi EA, Karbowniczek M, Astrinidis A, Wang C, et al. Estrogen promotes the survival and pulmonary metastasis of tuberin-null cells. Proc Natl Acad Sci. 2009;106(8):2635–2640. doi: 10.1073/pnas.0810790106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zhe X, Schuger L. Combined smooth muscle and melanocytic differentiation in lymphangioleiomyomatosis. J Histochem Cytochem. 2004;52(12):1537–1542. doi: 10.1369/jhc.4A6438.2004. [DOI] [PubMed] [Google Scholar]