Abstract
Objective
To examine prevalences of substance use disorders (SUD) and comprehensive patterns of comorbidities among psychiatric patients ages 18–64 years (N=40,099) in an electronic health records (EHR) database.
Method
DSM-IV diagnoses among psychiatric patients in a large university system were systematically captured: SUD, anxiety (AD), mood (MD), personality (PD), adjustment, childhood-onset, cognitive/dementia, dissociative, eating, factitious, impulse-control, psychotic (schizophrenic), sexual/gender identity, sleep, and somatoform diagnoses. Comorbidities and treatment types among patients with a SUD were examined.
Results
Among all patients, 24.9% (n=9,984) had a SUD, with blacks (35.2%) and Hispanics (32.9%) showing the highest prevalence. Among patients with a SUD, MD was prevalent across all age groups (50.2–56.6%). Patients aged 18–24 years had elevated odds of comorbid PD, adjustment, childhood-onset, impulse-control, psychotic, and eating diagnoses. Females had more PD, AD, MD, eating, and somatoform diagnoses, while males had more childhood-onset, impulse-control, and psychotic diagnoses. Blacks had greater odds than whites of psychotic and cognitive/dementia diagnoses, while whites exhibited elevated odds of PA, AD, MD, childhood-onset, eating, somatoform, and sleep diagnoses. Women, blacks, and Native American/multiple-race adults had elevated odds of using inpatient treatment; men, blacks, and Hispanics had increased odds of using psychiatric emergency care. Comorbid MD, PD, adjustment, somatoform, psychotic, or cognitive/dementia diagnoses increased inpatient treatment.
Conclusion
Patients with a SUD, especially minority members, use more inpatient or psychiatric emergency care than those without. Findings provide evidence for research on understudied diagnoses and underserved populations in the real-world clinical settings.
Keywords: anxiety disorders, comorbidity, comparative effectiveness research, electronic health records, mood disorders, personality disorders, substance-related disorders
Introduction
According to US national survey data, 46.4% of adults aged ≥18 years have a lifetime psychiatric disorder (alcohol or drug, 15%; anxiety [AD], 28.8%; mood [MD], 20.8%; conduct [CD], 9.5%; attention deficit hyperactivity [ADHD], 8.1%; oppositional-defiant [ODD], 8.5%; intermittent-explosive disorders, 5.2%), and about 60% of adults with a disorder have another one in their lifetime (Kessler et al., 2005). An estimated 12.2% of men and 5.8% of women aged ≥18 years have a substance use disorder (SUD: alcohol/drug abuse or dependence) in the past year (SAMHSA, 2011a). Psychiatric conditions before adulthood increase the risk for developing a SUD (Najt et al., 2011; O’Neil et al., 2011). Early substance use increases odds of subsequent psychiatric disorders (Brook et al., 2000; Glantz et al., 2009). Additionally, SUD and other disorders may interact with one another through multiple mechanisms (self-medication, substance-related neurotoxic effects, common risk factors), resulting in severe comorbidities (Kushner et al., 2000; Swendsen et al., 2010). The level of severity generally increases with the number of comorbid disorders (Glantz et al., 2009; Wu et al., 2011a). Survey data suggest a higher magnitude of association of SUD with other disorders among women than men, but racial differences in comorbidity are infrequently reported (Compton et al., 2005; Smith et al., 2006).
Survey data focus on certain disorders considered to be common in the general population and include inadequate information about treatment settings to inform treatment burden. Hence, research on comorbidity among clinical patients is needed to fill this gap. However, clinical studies frequently include small sample sizes of patients from a single setting (inpatient, outpatient) or specialty only (substance abuse, mental health). Due to a small sample size, results are limited by descriptive findings. Variations in the sample characteristics and settings also lead to mixed rates of disorders. For example, among 226 drug-dependent individuals, 59.5% had a PD (Kokkevi et al., 1998). Among 100 addiction patients, 49% had an AD or MD (Lubman et al., 2007). In a multisite analysis of treatment-seeking or street drug users (N=37–189 across five sites), lifetime MD (18.0–40.9% across sites), antisocial/borderline PD (13.7–39.6%), AD (12.9–16.8%), and psychotic disorders (5.0–12.1%) were comparatively prevalent (Torrens et al., 2011). In a sample of 70 psychiatric inpatients with a SUD, Grilo et al., (1997) reported high rates of PD (men, 82%; women, 76%), MD (men, 52%; women, 70%), AD (men, 33%; women, 19%), and psychotic disorder (30%, men; 24%, women).
Comorbid SUD complicates treatment decision-making, predicts poor outcomes, and increases healthcare costs, thus requiring comprehensive diagnostic data from a large sample to inform subgroup differences in comorbidity and treatment (McGovern and McLellan, 2008; Najt et al., 2011). While survey data demonstrate associations of comorbid SUDs and other disorders, they are limited in informing treatment, as severe subsets (psychiatric patients, inpatients) often are excluded from the sampling, and assessments are limited to certain disorders. Clinical research provides another source of valuable data for elucidating comorbidity, but sample sizes tend to be small, constraining subgroup analyses. Results of clinical studies sometimes are affected by study inclusion and exclusion criteria, and individuals with severe conditions are frequently excluded (McGovern and McLellan, 2008; O’Neil et al., 2011). Therefore, there is limited information about diagnoses and comorbidity not studied by surveys or small-scale clinical research.
The US Health Information Technology for Economic and Clinical Health (HITECH) Act pushes for national adoption of the electronic health records (EHR) system to improve the efficiency and quality of healthcare delivery. The EHR provides clinicians with comprehensive clinical information about each patient to increase treatment efficiency and safety through improving integration of care (Silow-Carroll et al., 2012). Consequently, use of the EHR data from patients in the real-life medical settings to discern the quality of healthcare delivery has become a priority for research (Institute of Medicine [IOM], 2009). An effective use of the EHR holds potential for transforming health care and implementing patient-centered care (e.g., clinical decision support, coordinated team care), including healthcare for SUDs (Bates and Bitton, 2010; Tai et al., 2012). To achieve such goals, one initial step is to develop a knowledge base on patients who use treatments in the real-life settings through research on their personal medical records to inform research and designs for patient-centered care (IOM, 2009).
Use of the EHR has increased. In 2011, 42% of surveyed U.S. physicians used an EHR system that meets federal standards (Jamoom et al., 2012). Patients’ personal medical record data are the basic staple of health learning, but the EHRs have been a greatly underutilized information resource for research (IOM, 2010). Compared with surveys of self-reports of clinical staff, claims data, or prescription data, EHRs include more important details about each patient’ diagnoses and treatment use. Recognized the necessity to integrate clinical information systems to provide real-time assistance to clinicians, a psychiatric EHR system (“MindLinc”) designed by a psychiatrist to taken into account the need of comprehensive assessments, medical evaluations, and evidence-based guidelines for treating persons with psychiatric conditions has been developed and used since 1998 (Gersing and Krishnan, 2002). The MindLinc EHR is among the first EHR systems to receive the federal government’s meaningful use stamp of approval. By capturing all patients’ medical records systematically, large EHRs serve as an anonymous, HIPAA-compliant data repository for conducting research to gauge psychiatric conditions, including diagnoses and treatments not available from surveys or small-scale clinical research (Wu et al., 2011b). Such research is timely relevant to the adoption of the EHR system in routine practice and use of the EHRs to improve care as it informs key clinical profiles and disparities for various patient groups in the real-world settings and allows comparisons of findings with survey-based estimates.
Aims of the study
We capitalize on a large EHR database to determine patterns of comorbid SUDs and other disorders among psychiatric patients aged 18–64 years who accessed psychiatric treatment in a large medical center hospital and its clinics (outpatient, inpatient, emergency department). To meet the goal set by the Institute of Medicine for reducing health disparities by key demographics (IOM, 2009), we examine SUDs among psychiatric patients and establish comprehensive patterns of comorbidities among patients with a SUD by age, sex, and racial/ethnic backgrounds. We estimate associations of age, sex, and race/ethnicity with each diagnosis and determine demographic and diagnostic profiles associated with use of costly inpatient or emergency treatments versus outpatient care.
Materials and methods
Data source
Since 1998, the Duke University Medical Center (DUMC) Department of Psychiatry has used the MindLinc EHR system in all its clinics and inpatient facilities to capture systematically each patient’s medical records (Gersing and Krishnan, 2003). MindLinc is the largest known psychiatry registry in the United States, presently containing nearly 220,000 individual patients from about 40 organizations across the country. This system supplies health care providers with a readily available means of monitoring patients’ courses of treatment (Gersing et al., 2007; Wu et al., 2011b). To address the issue of completeness of data, the EHR system includes a quality check that requires the attending clinicians (psychiatrists, psychiatry residents) to complete required fields for a clinical visit (diagnosis, clinician, services, medications, side effects, billing codes, allergies). A longitudinal data repository is built, comprising all qualified visit data for each patient. To comply with HIPAA requirements, all the 18 identifiers specified by the HIPAA guidelines are removed from the data repository. DUMC serves patients from all possible sources (physician referrals, emergency departments, self-referrals). The analytic sample included 40,099 unique patients aged 18–64 years who accessed psychiatric treatment in the DUMC between January 1, 2000, and December 31, 2010. Due to age-related decreases in SUDs and increases in cognitive/dementia diagnosis, results for patients aged 65+ years will be presented in a separate paper.
Psychiatric diagnoses
Psychiatric diagnoses listed in the medical record were noted at each visit and coded according to the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, (DSM-IV) (American Psychiatric Association, 2000). The DSM-IV is accessible within the EHR application to permit clinicians to evaluate patients’ chief complaints, symptoms, mental and medical status examination findings, social/family history, and medical history data again the DSM-IV criteria. The EHR captures detailed information on DSM-IV codes (when the diagnosis started, when the diagnosis ended, if diagnosis a primary disorder, if diagnosis a rule out, if symptom active or historical), and the level of baseline severity and improvement. For SUDs, the EHR includes a “Habit/Substance Use” domain that has multiple functionalities to allow the treating clinician to assess the patient’s history of substance use, patterns of current use, American Society of Addiction Medicine dimensions, and SUD diagnoses.
Consistent with studies on comorbidity (Kessler et al., 2005), we examined lifetime patterns for each patient logged in the EHR (primary and secondary diagnoses; current and remitted diagnoses). The same diagnosis of a patient was counted only once in the analysis. All 17 major DSM-IV diagnoses were examined: SUD (alcohol, tobacco, drugs), anxiety (AD), adjustment, mood (MD), childhood-onset (e.g., mental retardation, learning, attention-deficit and disruptive behavior, pervasive developmental), cognitive/dementia, dissociative, eating, factitious, impulse-control (e.g., gambling, intermittent-explosive), psychotic (schizophrenic), sexual (including gender identity), sleep, somatoform, personality (PD; mainly borderline, antisocial) disorders, mental disorders due to a general medical condition (GMC), and other conditions of clinical attention (e.g., relational problems). All diagnoses were based on treatment visits and assigned by the evaluating clinicians (psychiatrists, psychiatric residents, licensed PhD-level psychologists). Because it is critical to investigate the extent to which the EHR captures demographic and diagnostic patterns that are consistent with findings from other data sources, the focus on lifetime patterns not only allows comparisons of results with other studies, but also identifies diagnoses of concern for informing priority areas.
Demographics and treatment setting
Demographics included age at first psychiatric visit logged in the database, sex, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, Asian/Pacific-Islander, other [multiple-race, Native American], unknown/missing), and marital status (single, married, separated/divorced/widowed, unknown/missing). Treatment type (setting) was categorized into mutually exclusive groups: any psychiatric inpatient, psychiatric emergency care (regardless of outpatient), and outpatient only. All treatments were related to psychiatric conditions. Among users of psychiatric emergency care, 32% also received inpatient treatment; the latter were included in the inpatient group.
Data analyses
χ2 tests were conducted to determine differences in demographics and treatment setting by SUD status. Patterns of SUD by age at first psychiatric visit, sex, and race/ethnicity were determined to inform health disparities, as were patterns of comorbid diagnoses among patients with a SUD. Logistic regression analyses were performed among patients with a SUD to determine associations of age, sex, and race/ethnicity with each diagnosis while controlling for potential confounding effects of treatment setting, calendar year, and comorbid diagnoses. Multinomial logistic regression analyses were conducted to identify demographic correlates of inpatient and of psychiatric emergency treatment (vs. outpatient only) while controlling for calendar year and number of comorbid diagnoses. Finally, associations of each comorbid diagnosis with inpatient and psychiatric emergency treatment (vs. outpatient only), respectively, were determined using multinomial logistic regression procedures to control for age, sex, race/ethnicity, and calendar year. To reduce chances of false positives, significant P-values were set conservatively at <0.01 for descriptive analyses. All analyses were conducted by SAS V9.2 (SAS, 2010).
Results
Demographics and treatment setting by SUD (Table 1)
Table 1.
Demographics and treatment settings of psychiatric patients aged 18–64 years in a large electronic health records database, by substance use disorder (SUD) status: 2000–2010 (N=40,099)
| N (%) | Total | With a SUD diagnosis | Without a SUD diagnosis | χ2 (df) P-value |
|---|---|---|---|---|
|
| ||||
| Sample size | N=40,099 | N=9,984 | N=30,115 | |
| Age at first visit, years | ||||
| 18–24 | 5692 (14.2) | 1724 (17.3) | 3968 (13.2) | 521.6 (3) |
| 25–34 | 8317 (20.7) | 2397 (24.0) | 5920 (19.7) | <0.001 |
| 35–44 | 10097 (25.2) | 2841 (28.5) | 7256 (24.1) | |
| 45–64 | 15993 (39.9) | 3022 (30.3) | 12971 (43.1) | |
|
| ||||
| Sex | ||||
| Male | 16793 (41.9) | 6226 (62.4) | 10567 (35.1) | 2291.0 (1) |
| Female | 23306 (58.1) | 3758 (37.6) | 19548 (64.9) | <0.001 |
|
| ||||
| Race/ethnicity | ||||
| White, non-Hispanic | 24909 (62.1) | 5447 (54.6) | 19462 (64.6) | 869.1 (5) |
| Black, non-Hispanic | 10408 (26.0) | 3664 (36.7) | 6744 (22.4) | <0.001 |
| Hispanic | 213 (0.5) | 70 (0.7) | 143 (0.5) | |
| Asian/Pacific-Islander | 440 (1.1) | 49 (0.5) | 391 (1.3) | |
| Native American/multiple-race | 937 (2.3) | 201 (2.0) | 736 (2.4) | |
| Unknown | 3192 (8.0) | 553 (5.5) | 2639 (8.8) | |
|
| ||||
| Marital status | ||||
| Single | 10883 (27.1) | 3851 (38.6) | 7032 (23.4) | 1366.8 (3) |
| Married | 11791 (29.4) | 1843 (18.5) | 9948 (33.0) | <0.001 |
| Separated, divorced, widowed | 4629 (11.5) | 1482 (14.8) | 3147 (10.4) | |
| Unknown | 12796 (31.9) | 2808 (28.1) | 9988 (33.2) | |
|
| ||||
| Treatment setting | ||||
| Any inpatient | 8181 (20.4) | 2487 (24.9) | 5694 (18.9) | 4839.9 (2) |
| Psychiatric emergency | 8290 (20.7) | 4263 (42.7) | 4027 (13.4) | <0.001 |
| Outpatient only | 23628 (58.9) | 3234 (32.4) | 20394 (67.7) | |
Among patients aged 18–64 years, 24.9% (n=9,984) received a SUD diagnosis (abuse or dependence on alcohol or other psychoactive drug, nicotine dependence, substance-induced disorders). Compared with patients without a SUD, patients with a SUD included more adults aged 18–44 years (69.8% vs. 57.0%), men (62.4% vs. 35.1%), blacks (36.7% vs. 22.4%), single (38.6% vs. 23.4%) or separated/divorced/widowed (14.8% vs. 10.4%) adults, inpatients (24.9% vs. 18.9%), and psychiatric emergency patients (42.7% vs. 13.4%).
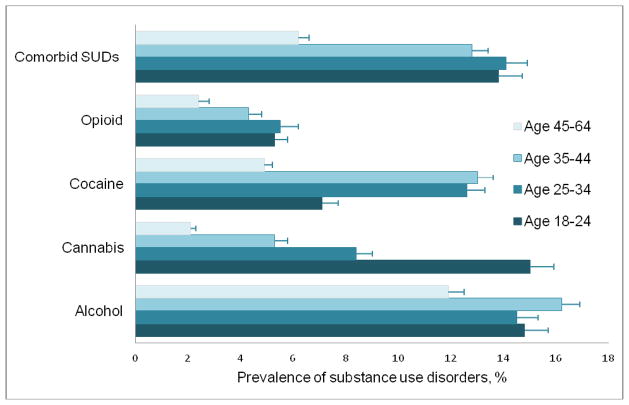
SUDs among patients (Figure 1)
Fig. 1.
Prevalence of substance use disorders (SUDs) by age group among psychiatric patients aged 18–64 years (N=40,099)
Note: Error bars indicate the upper limit of 95% confidence intervals.
Among patients aged 18–64 years (N=40,099), 14.5% had one SUD only, and another 10.6% had 2+ SUDs (alcohol, 10.4%; cocaine, 8.8%; cannabis, 6.0%; opioids, 3.9%; polysubstance, 2.3%; nicotine, 2.0%, amphetamine, 0.4%; hallucinogen, 0.3%; other, 2.0%). Of those with a SUD, 42.6% had 2+ SUDs. SUD prevalences by age, sex, and race/ethnicity are available online only (eTables 1–3).
Age
Adults aged 18–44 years had higher rates than those aged 45–64 of any SUD (28.1–30.3% vs. 18.9%) and 2+ SUDs (12.8–14.1% vs. 6.2%). Cannabis diagnoses (15.0%) were most common among adults aged 18–24 years, while cocaine diagnoses (12.6–13.0%) were most prevalent among adults aged 25–44.
Sex
Men had higher rates than women of all SUDs: any SUD (37.1% vs. 16.1%), 2+ SUDs (16.5% vs. 6.3%), alcohol (22.4% vs. 7.9%), cocaine (12.9% vs. 5.9%), cannabis (9.6% vs. 3.5%), opioid (5.5% vs. 2.8%), polysubstance (3.6% vs. 1.4%), and nicotine (3.0% vs. 1.2%) diagnoses.
Race/ethnicity
Blacks had the highest rate of any SUD (35.2%) and 2+ SUDs (17.3%). Hispanics (32.9%) had a higher rate of any SUD than whites (21.9%), Native American/multiple-race adults (21.5%), and Asians/Pacific-Islanders (11.1%). Rates of alcohol and cocaine diagnoses were elevated among blacks (18.0%, 20.1%, respectively) and Hispanics (23.5%, 13.1%, respectively).
Comorbidities among patients with a SUD
MD (54.2%) and AD (24.5%) were the most prevalent diagnoses among patients with a SUD (n=9,984), followed by PD (13.0%), psychotic (11.1%), adjustment (7.3%), cognitive/dementia (5.4%), childhood-onset (4.8%), somatoform (2.0), and eating (1.8%) diagnoses. Comorbidity prevalences by age, sex, and race/ethnicity are available online only (eTables 4–6).
Age
Adults aged 18–44 years had more PD (13.6–15.3%) and psychotic diagnoses (11.3–12.4%) than adults aged 45–64 (10.0%, 9.7%, respectively). Young adults aged 18–24 years had more adjustment (9.2%), eating (2.8%), and impulse control (2.2%) diagnoses, whereas those aged 35–44 had more MD diagnoses than those aged 18–24 (56.6% vs. 50.2%). Adults aged 45–65 years had more cognitive/dementia diagnoses (11.7%) than adults aged 18–44 (1.2–3.6%); adults aged 35–64 years (2.3%) had more somatoform diagnoses than those aged 18–24 (1.0%).
Sex
Men had more psychotic (12.3% vs. 9.3%), childhood-onset (5.3% vs. 4.1%), and impulse-control (1.4% vs. 0.6%) diagnoses than women, while women had more adjustment (8.1% vs. 6.8%), AD (33.3% vs. 19.1%), MD (66.3% vs. 46.9%), PD (18.0% vs. 9.1%), eating (3.9% vs. 0.4%), somatoform (3,1% vs. 1.3%), and 2+ comorbid diagnoses (50.3% vs. 33.6%) than men.
Race/ethnicity
Whites had more 2+ comorbid diagnoses (43.7%) than other groups (11.4% among Hispanics to 38.7% among Asians/Pacific-Islanders). Blacks had more psychotic diagnoses (19.2%) than other groups (5.7–8.2%). Whites (58.4%), blacks (50.1%), Native American/multiple-race adults (47.8%), and Asians/Pacific-Islanders (42.9%) had more MD diagnoses than Hispanics (25.7%). Whites had more PD (14.6%) than other groups (2.9% among Hispanics to 11.6% among blacks). Whites also had more childhood-onset (6.1% vs. 2.8%), eating (2.6% vs. 0.5%), sleep (1.2% vs. 0.5%), and somatoform diagnoses (2.5% vs. 1.4%) than blacks.
Adjusted analyses of demographic profiles of comorbid diagnoses (Table 2)
Table 2.
Adjusted logistic regression1 of comorbid diagnoses among psychiatric patients aged 18–64 years with a substance use disorder (N=9,984)
| Comorbid diagnosis | Age 18–24 vs. 45+ | Age 25–34 vs. 45+ | Age 35–44 vs. 45+ | Female vs. male | White vs. black | Hispanic vs. black | Asian/Pacific-Islander vs. black | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||
| Adjusted estimates | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI |
| Personality | 1.59 | 1.31–1.95 | 1.74 | 1.46–2.07 | 1.46 | 1.24–1.73 | 1.79 | 1.59–2.03 | 1.53 | 1.34–1.76 | 0.30 | 0.07–1.22 | 1.08 | 0.42–2.80 |
| Adjustment | 1.46 | 1.15–1.84 | 1.03 | 0.82–1.28 | 0.97 | 0.79–1.20 | 1.15 | 0.99–1.35 | 0.95 | 0.80–1.13 | 1.22 | 0.43–3.43 | 1.36 | 0.56–3.28 |
| Anxiety | 1.04 | 0.89–1.22 | 1.38 | 1.21–1.58 | 1.20 | 1.06–1.36 | 2.06 | 1.87–2.27 | 1.99 | 1.78–2.23 | 0.90 | 0.38–2.11 | 1.10 | 0.52–2.31 |
| Mood | 0.90 | 0.79–1.02 | 1.07 | 0.95–1.20 | 1.16 | 1.04–1.30 | 2.12 | 1.95–2.31 | 1.47 | 1.34–1.61 | 0.59 | 0.34–1.03 | 0.92 | 0.51–1.66 |
| Childhood-onset | 4.44 | 3.26–6.05 | 2.04 | 1.48–2.81 | 1.33 | 0.95–1.85 | 0.78 | 0.63–0.96 | 1.82 | 1.43–2.31 | ---- | ---- | ||
| Impulse-control | 2.94 | 1.62–5.32 | 1.78 | 0.98–3.21 | 1.18 | 0.64–2.16 | 0.41 | 0.25–0.65 | 0.90 | 0.60–1.37 | ---- | ---- | ||
| Eating | 2.04 | 1.25–3.33 | 1.40 | 0.87–2.27 | 1.41 | 0.89–2.23 | 9.22 | 6.02–14.1 | 4.54 | 2.76–7.47 | ---- | ---- | ||
| Psychotic | 1.40 | 1.12–1.74 | 1.12 | 0.92–1.36 | 0.99 | 0.83–1.20 | 0.63 | 0.55–0.73 | 0.34 | 0.30–0.40 | ---- | ---- | ||
| Dissociative | 0.18 | 0.04–0.82 | 0.13 | 0.03–0.57 | 0.57 | 0.23–1.37 | 12.4 | 3.68–41.5 | 2.05 | 0.85–4.94 | ---- | ---- | ||
| Cognitive/dementia | 0.11 | 0.07–0.19 | 0.31 | 0.23–0.42 | 0.34 | 0.27–0.44 | 0.73 | 0.60–0.90 | 0.79 | 0.64–0.96 | ---- | ---- | ||
| Sexual/gender identity | 0.52 | 0.13–2.00 | 0.72 | 0.24–2.17 | 0.72 | 0.26–1.99 | 0.22 | 0.06–0.73 | 2.23 | 0.81–6.16 | ---- | ---- | ||
| Somatoform | 0.58 | 0.33–1.03 | 1.03 | 0.69–1.55 | 1.17 | 0.81–1.69 | 2.01 | 1.49–2.72 | 1.68 | 1.20–2.37 | ---- | ---- | ||
| Sleep | 1.00 | 0.49–2.06 | 0.88 | 0.46–1.70 | 1.29 | 0.74–2.25 | 0.98 | 0.62–1.54 | 1.86 | 1.08–3.21 | ---- | ---- | ||
| Mental disorder-GMC2 | 0.46 | 0.15–1.42 | 0.37 | 0.13–1.01 | 0.69 | 0.33–1.47 | 1.11 | 0.59–2.11 | 1.18 | 0.59–2.38 | ---- | ---- | ||
| Other conditions3 | 1.10 | 0.90–1.34 | 0.89 | 0.74–1.06 | 0.93 | 0.79–1.09 | 1.20 | 1.05–1.36 | 0.87 | 0.76–1.00 | 0.77 | 0.32–1.81 | 1.42 | 0.62–3.25 |
AOR: adjusted odds ratio; CI: confidence interval.
Each model adjusted for treatment setting and calendar year; results for Native American and multiple-race individuals are not reported because of lack of significance or small sample sizes.
GMC: Mental disorders due to a general medical condition not otherwise specified.
Other conditions that may be a focus of clinical attention (mainly relational problems).
Bold face: P < 0.05.
----: Estimates are not included due to unstable estimates.
Logistic regression analyses were performed among patients with a SUD to estimate associations of age at first visit, sex, and race/ethnicity with each comorbid diagnosis while controlling for patients’ marital status, treatment setting, and calendar year.
Compared with patients aged 45–64 years, those aged 18–24 showed elevated odds of PD, adjustment, childhood-onset, impulse-control, eating, and psychotic diagnoses; patients ages 25–34 had increased odds of PD, AD, and childhood-onset diagnoses; patients ages 35–44 had elevated odds of PD, AD, and MD. Odds of dissociative and cognitive/dementia diagnoses were elevated among patients aged 45–64 years. Women showed greater odds than men of PD, AD, MD, eating, dissociative, and somatoform diagnoses, while men had elevated odds of childhood-onset, impulse-control, psychotic, cognitive/dementia, and sexual diagnoses. Blacks had greater odds than whites of psychotic and cognitive/dementia diagnoses, while whites showed elevated odds of PD, AD, MD, childhood-onset, eating, somatoform, and sleep diagnoses.
Adjusted analyses of demographic profiles of treatment settings (Table 3)
Table 3.
Adjusted multinomial logistic regression of treatment type among psychiatric patients aged 18–64 years with a substance use disorder (N=9,844)
| Adjusted analysis1 | Inpatient vs. outpatient | Psychiatric emergency vs. outpatient | ||
|---|---|---|---|---|
|
| ||||
| AOR | 95% CI | AOR | 95% CI | |
| Age 18–24 vs. 45+ | 0.62 | 0.52–0.74 | 1.19 | 1.02–1.39 |
| Age 25–34 vs. 45+ | 0.74 | 0.64–0.87 | 1.67 | 1.45–1.92 |
| Age 35–44 vs. 45+ | 0.82 | 0.71–0.95 | 1.40 | 1.22–1.60 |
| Female vs. male | 1.13 | 1.01–1.27 | 0.88 | 0.79–0.97 |
| White vs. black | 0.63 | 0.56–0.72 | 0.42 | 0.38–0.47 |
| Hispanic vs. black | 2.63 | 0.64–10.76 | 5.50 | 1.97–15.39 |
| Asian/Pacific-Islander vs. black | 1.04 | 0.50–2.18 | 0.48 | 0.24–0.97 |
| Other vs. black | 1.68 | 1.14–2.49 | 0.82 | 0.56–1.21 |
AOR: adjusted odds ratio; CI: confidence interval; Other: Native American or multiple-race.
The model adjusted for marital status, calendar year, and number of comorbid diagnoses.
Bold face: P < 0.05.
Multinomial logistic regression analyses of patients with a SUD were performed to identify correlates of inpatient and psychiatric emergency treatment (vs. outpatient only) while adjusting for patients’ marital status, number of comorbid diagnoses, and calendar year.
Compared with patients aged 45–64 years, all younger groups had lower odds of using inpatient treatment but greater odds of using emergency services. Females had elevated odds of using inpatient treatment, whereas males had increased odds of using emergency treatment. Compared with blacks, whites had lower odds of using inpatient and emergency care, Native American/multiple-race adults had greater odds of using inpatient treatment, Hispanics had greater odds using psychiatric emergency care, and Asians/Pacific-Islanders showed reduced odds of using emergency services.
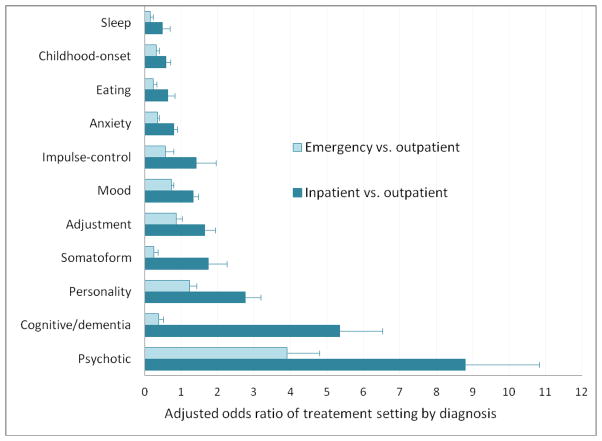
Adjusted analyses of diagnostic profiles of treatment settings (Figure 2)
Fig. 2.
Adjusted odds ratio of comorbid diagnostic profiles of psychiatric emergency and inpatient treatment use compared with outpatient psychiatric treatment among psychiatric patients aged 18–64 years with a substance use disorder (N=9,844)
Note: Error bars indicate the upper limit of 95% confidence intervals Each model of treatment use in relation to a diagnosis adjusted for age, sex, race, marital status, and calendar year.
Multinomial logistic regression analyses of patients with a SUD were conducted to identify comorbid diagnoses associated with use of inpatient or emergency treatment (vs. outpatient only) while adjusting for age of first psychiatric visit, sex, race/ethnicity, marital status, and calendar year. Psychotic and PD diagnoses increased odds of inpatient and emergency treatments. Cognitive/dementia, somatoform, adjustment, and MD diagnoses increased odds of inpatient treatment, while AD, eating, childhood-onset, and sleep diagnoses had lower odds of inpatient treatment (online only eTables 7).
Length of treatment
Finally, we explored length of treatment. Patients with a SUD on average had a longer length of psychiatric treatment logged in the EHRs than patients without a SUD (mean [standard error]: 459 days [8.4] vs. 355 days [4.0], P<0.001). Among patients with a SUD, users of inpatient treatment (738 days [21.4]) had a longer length of psychiatric treatment than users of emergency care (374 days [12.0]) or outpatient treatment only (356 days [11.6], P<0.001).
Discussion
Recent health care reform in the United States pushes for national adoption of the EHR system, and the use of EHRs for research to inform the quality of care has been recognized. This study presents new and the most comprehensive patterns of psychiatric comorbidities and treatment settings in the large, non-research sample of adults in the real-world medical settings from an EHR system. The EHR database of a large university-based hospital and all its psychiatric clinics has systematically captured medical records of patients from rural, urban, and suburban areas. These findings have timely implications for clinical care and research. First, SUDs were common among blacks and Hispanics, and nicotine dependence was under-diagnosed. Second, comorbidities were prevalent among patients with a SUD who also used more costly psychiatric inpatient (women, blacks, Native American/multiple-race adults) or emergency (men, blacks, Hispanics) care than patients without a SUD. Third, among patients with a SUD, women and whites had more comorbidities than men and blacks. These distinct sex and racial/ethnic differences in treatment setting and diagnostic profiles in real-world settings support longitudinal research to elucidate disparities in diagnosis and treatment outcomes.
SUDs are prevalent across all age groups
National surveys show a marked decline in past-year alcohol or drug disorders from 20% in the 18–25 age group to 7% in the 26+ group (SAMHSA, 2011a). However, this age pattern may not reflect treatment-seeking individuals. Due to stigma, denial, or cost, individuals with SUDs often have a lengthy delay in treatment-seeking after their onset (SAMHSA, 2011b; Wu et al., 2007). Treatments for SUDs typically occur in adulthood; individuals with chronic SUD or comorbidities are most likely to use treatment (SAMHSA, 2011b; Wu et al., 1999). High SUD prevalence among patients aged 18–44 or 45–64 in this study is consistent with data from treatment-seeking adults (SAMHSA, 2010), indicating that, in psychiatric settings, all non-elderly adults should be screened for SUDs and treated as needed.
SUDs affect more blacks than whites
High SUD prevalences among Hispanics and blacks have implications for research. National surveys reveal an increase in cannabis disorders among Hispanics and blacks (Compton et al., 2004; Wu et al., 2012) and elevated odds of SUDs among young Hispanics (Wu et al., 2011c). Although cannabis lacks an acceptable level of safety for medical use and accounts for the majority of illicit drug-related diagnoses in addiction treatment (Drug Enforcement Administration, 2011; SAMHSA, 2010), the number of states supporting medicinal marijuana has increased (ProCon.org), suggesting its increased availability. Cannabis use by psychiatric patients can be particularly dangerous, as it is associated with numerous psychiatric problems (Nussbaum et al., 2011). Meta-analyses show associations between cannabis use and psychotic disorders (Foti et al., 2010; Large et al., 2011). Men and blacks in this study have the highest rates of psychotic and cannabis diagnoses. While causality cannot be inferred from the data, there is a need to monitor cannabis use and cannabis-related problems and to use EHRs to evaluate the impact of SUD treatment on courses of psychiatric disorders and vice versa (Kendall and Kessler, 2002).
Nicotine dependence is under-diagnosed
Compared with the national survey of adults, which estimates that 13% of American adults have nicotine dependence within a year (Grant et al., 2004), the low prevalence of nicotine dependence (2%) in this study suggests under-detection or diagnosis, an area that requires research to specify barriers to effective assessment and intervention. Other reports also stress similar concerns. Specifically, clinicians’ lack of training in nicotine dependence treatment, inadequate resources, competing priorities, perceptions about nicotine dependence as less harmful than other SUDs, and limited reimbursement all may contribute to under-diagnosis (Association of American Medical Colleges, 2007; Hitsman et al., 2009; Prochaska, 2010). Additionally, individual-level barriers may be substantial among psychiatric patients, including psychosocial or cognitive impairments interfering with motivation to quit, lack of resources supporting abstinence, perceptions about smoking as non-problematic, and use of smoking as a self-medication or behavioral filler to promote social interactions (Aubin, 2009; Hitsman et al., 2009; Morisano et al., 2009; Moss et al., 2010). Concerted efforts by patients, clinicians, and administrators are needed to promote treatment (Moss et al., 2010; Prochaska, 2010). The use of the EHR in routine practice and the Patient Protection and Affordable Care Act can make screening and intervention for tobacco smoking an essential part of care by specifying smoking and dependence screeners as common data elements in the EHR (Ghitza et al., 2011).
The majority of patients with a SUD receive inpatient/emergency care
Early psychiatric disorders as well as environmental or familial risk factors can increase risk of SUDs or intensify psychiatric conditions (Kessler, 2004; O’Neil et al., 2011). Persons with comorbidities are likely to comprise a severe set using more treatment due to impairment. Consistent with findings from patients aged 2–17 (Wu et al., 2011b), more patients with a SUD received inpatient or emergency services than patients without a SUD (68% vs. 32%); however, adults used more inpatient/emergency services than children (68% vs. 43%), suggesting an aged-related increase in diagnosis and treatment use. EHR data also reveal that psychotic and PD diagnoses increase inpatient and emergency treatment and that MD, somatic, and adjustment diagnoses account for inpatient treatment. However, these diagnoses, except for MD, are not routinely collected in major surveys, suggesting that EHR data provide valuable clinical information about understudied diagnoses and can be used to evaluate their clinical courses in relation to SUD. Further, MD, AD, PD, and psychotic diagnoses are comparatively common among patients with a SUD (Barnett et al., 2007; Cohen, 2008). Survey data estimate that 41% of American adults with a history of drug use disorder have a history of MD (Conway et al., 2006). This study adds clinical evidence that MD is the most prevalent comorbid diagnosis and pervasive in all age groups (50–57%), which can be related to their bidirectional associations (one increases risk for the other) (Glantz et al., 2009) or a particularly severe nature of comorbid MD and SUD. Given its high prevalence and association with inpatient treatment, all patients with a SUD should be assessed for MD, and integrated mental and addiction treatments should be considered routine care for individuals with a SUD.
Women and minority members disproportionally use inpatient treatment
Survey data show more robust associations between SUD and psychiatric disorders (AD, MD) among women than men and indicate greater psychopathology in women (Compton et al., 2005; Conway et al., 2006; Wu et al., 2010). Adjusted analyses of patients with a SUD showed elevated odds of PD, AD, MD, eating, dissociative, and somatoform diagnoses among women, and elevated odds of childhood-onset (ADHD, mental retardation), impulse-control, and psychotic diagnoses among men. These findings highlight sex differences in diagnosis (Hanel et al., 2009) and show clinical evidence of greater inpatient treatment but lower emergency service use among women than men. They underscore the need to incorporate sex-specific manifestations into treatment plans and to use EHRs to conduct sex-specific research on clinical courses and treatment responses (IOM, 2010).
Lastly, racial/ethnic differences in comorbidities and treatment location have implications for research and treatment. While blacks had greater psychotic and cognitive/dementia diagnoses than whites, whites generally had more comorbidities (PD, AD, MD, childhood-onset, eating, somatoform, sleep) (Snowden et al., 2009; Muroff et al., 2008). However, blacks were more likely than whites to receive inpatient or emergency treatment. Hispanics also showed elevated odds of emergency treatment. Such racial/ethnic differences in diagnoses and treatments are noted in prior studies, and support the usefulness of EHRs to elucidate factors contributing to disparities in diagnosis and treatment use (IOM, 2009; Lindsey et al., 2010; Strakowski et al., 1995). Specifically, while inpatient/emergency treatment use by blacks can be related to psychotic or cognitive/dementia diagnoses, disparities in comorbidity and treatment may be influenced by multiple factors or biases, such as racial/ethnic differences in access to primary care and cultural-related treatment-seeking behaviors and attitudes toward mental illness (Garland et al., 2005; Lindsey et al., 2010; Snowden et al., 2009). For example, greater comorbidities among whites but lower rates of inpatient/emergency treatment may relate partly to whites’ greater use of healthcare, resulting in more diagnostic assessments and treatments in outpatient settings; greater use of inpatient or emergency care among minority members may be explained partly by lower access to or use of primary care, contributing to under-diagnosis or delay in treatment (Garland et al., 2005; Snowden et al., 2009). These possible sources of bias in treatment-seeking, care use, and diagnoses warrant research to elucidate racial/ethnic variations in health status.
Limitations and strengths
Results should be interpreted within the following context. First, patients were from one large, academic medical center; 90% of patients were residents of North Carolina, with the remaining patients from neighboring states (South Carolina, Virginia, Tennessee, Florida, Georgia, West Virginia). Because all individuals who accessed DUMC for psychiatric care (outpatient, emergency department, inpatient) have been systemically captured in the longitudinal EHRs, findings represent patients’ diagnostic and treatment profiles at an academic hospital setting that serves a population of rural, urban, and suburban residents in the North Carolina (southeastern) areas. North Carolina has a higher proportion of blacks (22.0% vs. 13.1%) than the distribution in the total U.S. population (US Census, 2012). This is reflected in the EHRs, which is a strength by permitting detailed comparisons to determine clinical differences between whites and blacks, a priority area of disparity research (IOM, 2009). Although patients include all available individuals who sought care at DUMC, the generalizability of the findings to psychiatric patients in the other regions or settings (mental health, addiction) is limited. Variations in clinicians’ expertise and clinical resources may influence patients’ profiles. For example, hospitals (DUMC) may serve more patients with severe or urgent psychiatric conditions that require emergency or inpatient hospitalizations than mental health or addiction facilities where emergency or inpatient services are unavailable. Greater availability of treatment resources also indicate that patients in a hospital might receive more diagnostic assessments than patients in a non-hospital setting where treatment resources are comparatively limited. Results from these EHRs are not generalizable to patient in mental health/addiction settings that provide outpatient care only and survey respondents who have not used psychiatric treatment.
In addition, diagnoses logged systematically in the EHRs as part of usual clinical practice may not comparable to research-based, self-reported disorders from pre-determined survey questions or responses to diagnostic instruments administered by lay interviewers. Actual treatment-related diagnoses are based on non-standardized clinical evaluations typical of usual care settings, and they reflect clinical diagnoses and treatment use of patients with diverse demographic backgrounds in the real-life setting. They are not perfect, as diagnoses may be influenced by patients’ demographics and treatment use, clinicians’ specialties and training, insurance coverage (billable diagnoses), and variations in clinical detection and practices (Garland et al., 2005; Snowden et al., 2009; Wu et al., 2011b). Nonetheless, use of a comprehensive EHR in the routine care, providing clinicians with a ready access to longitudinal treatment history data and embedded assessment tools within the EHR, may help diagnostic assessments. Specifically, patients’ diagnoses and treatments are based on treating clinicians’ evaluations using fuller information from patients’ presentations and histories, mental status and medical examinations, laboratory data, treatment options, and information from clinical interactions among clinicians, patients, and family members logged in the EHRs (Wu et al., 2011b). Despite that the EHRs include much more information on diagnoses, treatments, evaluations (medical, mental, laboratory examinations) than surveys, results from EHRs may underestimate the true extent of psychiatric disorders. Constraints in provider time and resources make it infeasible to implement universal screening for all possible psychiatric conditions. Like studies that analyze existing treatment or insurance claim data, information on treatment use outside of the clinic is unavailable for analysis. Nonetheless, findings from the EHRs are likely to provide a more inclusive picture of diverse patterns of psychiatric diagnoses among patients seen in the community than estimates from cross-sectional surveys of convenience samples or insurance claim data.
This study has strengths not available from traditional clinical or survey studies. EHRs are less affected by self-report bias associated with survey questions and study-specific disorders of interest and selection of participants. EHRs capture all available psychiatric diagnoses and patients seen in the real-life treatment settings. They provide the opportunity to document clinically important diagnoses omitted in surveys, allow comparisons of wide-ranging patterns of comorbidities between whites and blacks, and add new findings for Hispanics and Asians/Pacific-Islanders. Research-based diagnoses typically are not confirmed by medical examinations, and diagnostic validity depends on the quality of self-report assessments and interviews. Nonetheless, both types of research are needed to complement one another in providing fuller pictures of diagnoses. Further, compared with use of insurance claim data for research, EHRs include complete and potentially more accurate treatment encounter data (Silfen, 2006; Weiner et al., 2007). The growing use of the EHR offers opportunities for research and clinical learning. However, it is critical that an initial investigation is conducted to evaluate the quality of EHR data.
In conclusion, this is one of the largest studies of non-research psychiatric patients recruited naturally in the real-life community treatment settings. It presents inclusive patterns of comorbidities and treatment needs from adults seen in psychiatric inpatient, outpatient, or emergency care settings. Psychiatric patients with a SUD used more emergency and inpatient care and had a longer length of treatment than patients without a SUD. These newer findings add clinically important evidence for understudied diagnoses and document unusually broad ranges of comorbid diagnoses for women and nonwhites. These results support the IOM’s calls for use of the EHRs for research to understand the quality of healthcare and to use the findings from the EHRs as learning tools to inform healthcare (IOM, 2010).
Supplementary Material
eTable 1. Prevalence of substance use disorders (SUDs) by age group among psychiatric patients aged 18–64 years
eTable 2. Prevalence of substance use disorders (SUDs) by sex among psychiatric patients aged 18–64 years
eTable 3. Prevalence of substance use disorders (SUDs) by race/ethnicity among psychiatric patients aged 18–64 years
eTable 4. Prevalence of comorbid psychiatric diagnoses by age group among psychiatric patients aged 18–64 years with a substance use disorder (SUD)
eTable 5. Prevalence of comorbid psychiatric diagnoses by sex among psychiatric patients aged 18–64 years with a substance use disorder (SUD)
eTable 6. Prevalence of comorbid psychiatric diagnoses by race among psychiatric patients aged 18–64 years with a substance use disorder (SUD)
eTable 7. Adjusted multinomial regression of psychiatric treatment type among psychiatric patients aged 18–64 years with a SUD (N=9,844)
Acknowledgments
Role of Funding Source: This work was made possible by the Department of Psychiatry of Duke University Medical Center and research grants from the U.S. National Institute on Drug Abuse of the National Institutes of Health (R21DA027503, R33DA027503, R01DA019623, and R01DA019901; PI, LT Wu). The National Institutes of Health had no role in design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health or the Department of Psychiatry of Duke University Medical Center.
This study was approved by the Duke University Institutional Review Board. The authors thank A. Deo Garlock and staff of the MindLinc for their contribution to the data repository.
Footnotes
Contributors: L-T Wu developed research aims and questions and wrote the drafts of the paper. K Gersing designed the electronic health record database system. B Burchett managed the database and conducted statistical analyses. All authors contributed to critical revisions and interpretations of the findings to result in the final manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 2000. text revision. [Google Scholar]
- Association of American Medical Colleges. Full Report. 2007. 2007 Association of American Medical Colleges, Physician Behavior and Practice Patterns Related to Smoking Cessation. [Google Scholar]
- Aubin HJ. Management of emergent psychiatric symptoms during smoking cessation. Curr Med Res Opin. 2009;25:519–25. doi: 10.1185/03007990802707600. [DOI] [PubMed] [Google Scholar]
- Barnett JH, Werners U, Secher SM, Hill KE, Brazil R, Masson K, Pernet DE, Kirkbride JB, Murray GK, Bullmore ET, Jones PB. Substance use in a population-based clinic sample of people with first-episode psychosis. Br J Psychiatry. 2007;190:515–20. doi: 10.1192/bjp.bp.106.024448. [DOI] [PubMed] [Google Scholar]
- Bates DW, Bitton A. The future of health information technology in the patient-centered medical home. Health Aff (Millwood) 2010;29:614–21. doi: 10.1377/hlthaff.2010.0007. [DOI] [PubMed] [Google Scholar]
- Brook JS, Richter L, Rubenston E. Consequences of adolescent drug use on psychiatric disorders in early adulthood. Annals of Medicine. 2000;32:401–407. doi: 10.3109/07853890008995947. [DOI] [PubMed] [Google Scholar]
- Cohen P. Child development and personality disorder. Psychiatric Clinics of North America. 2008;31:477–493. doi: 10.1016/j.psc.2008.03.005. [DOI] [PubMed] [Google Scholar]
- Compton WM, Conway KP, Stinson FS, Colliver JD, Grant BF. Prevalence, correlates, and comorbidity of DSM-IV antisocial personality syndromes and alcohol and specific drug use disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry. 2005;66:677–85. doi: 10.4088/jcp.v66n0602. [DOI] [PubMed] [Google Scholar]
- Compton WM, Grant BF, Colliver JD, Glantz MD, Stinson FS. Prevalence of marijuana use disorders in the United States: 1991–1992 and 2001–2002. JAMA. 2004;291:2114–2121. doi: 10.1001/jama.291.17.2114. [DOI] [PubMed] [Google Scholar]
- Conway KP, Compton W, Stinson FS, Grant BF. Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2006;67:247–57. doi: 10.4088/jcp.v67n0211. [DOI] [PubMed] [Google Scholar]
- Drug Enforcement Administration (DEA), Department of Justice. Denial of Petition To Initiate Proceedings To Reschedule Marijuana. Federal Register. 2011 Jul Friday 8;76(131) [Google Scholar]
- Foti DJ, Kotov R, Guey LT, Bromet EJ. Cannabis use and the course of schizophrenia: 10-year follow-up after first hospitalization. Am J Psychiatry. 2010;167:987–993. doi: 10.1176/appi.ajp.2010.09020189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland AF, Lau AS, Yeh M, McCabe KM, Hough RL, Landsverk JA. Racial and ethnic differences in utilization of mental health services among high-risk youths. Am J Psychiatry. 2005;162:1336–1343. doi: 10.1176/appi.ajp.162.7.1336. [DOI] [PubMed] [Google Scholar]
- Gersing K, Burchett B, March J, Ostbye T, Krishnan KR. Predicting antipsychotic use in children. Psychopharmacology Bulletin. 2007;40:116–124. [PubMed] [Google Scholar]
- Gersing K, Krishnan R. Clinical computing: Clinical Management Research Information System (CRIS) Psychiatric Services. 2003;54:1199–1200. doi: 10.1176/appi.ps.54.9.1199. [DOI] [PubMed] [Google Scholar]
- Gersing KR, Krishnan KR. Practical evidence-based medicine. Psychopharmacology Bulletin. 2002;36:20–26. [PubMed] [Google Scholar]
- Ghitza UE, Sparenborg S, Tai B. Improving drug abuse treatment delivery through adoption of harmonized electronic health record systems. Subst Abuse Rehabil. 2011;2:125–131. doi: 10.2147/SAR.S23030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glantz MD, Anthony JC, Berglund PA, Degenhardt L, Dierker L, Kalaydjian A, Merikangas KR, Ruscio AM, Swendsen J, Kessler RC. Mental disorders as risk factors for later substance dependence: estimates of optimal prevention and treatment benefits. Psychol Med. 2009;39:1365–77. doi: 10.1017/S0033291708004510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Chou SP, Stinson FS, Dawson DA. Nicotine dependence and psychiatric disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2004;61:1107–15. doi: 10.1001/archpsyc.61.11.1107. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Martino S, Walker ML, Becker DF, Edell WS, McGlashan TH. Psychiatric comorbidity differences in male and female adult psychiatric inpatients with substance use disorders. Compr Psychiatry. 1997;38:155–9. doi: 10.1016/s0010-440x(97)90068-7. [DOI] [PubMed] [Google Scholar]
- Hanel G, Henningsen P, Herzog W, Sauer N, Schaefert R, Szecsenyi J, Löwe B. Depression, anxiety, and somatoform disorders: vague or distinct categories in primary care? Results from a large cross-sectional study. J Psychosom Res. 2009;67:189–97. doi: 10.1016/j.jpsychores.2009.04.013. [DOI] [PubMed] [Google Scholar]
- Hitsman B, Moss TG, Montoya ID, George TP. Treatment of tobacco dependence in mental health and addictive disorders. Can J Psychiatry. 2009;54:368–78. doi: 10.1177/070674370905400604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. Initial national priorities for comparative effectiveness research. Washington, DC: Institute of Medicine; 2009. [Google Scholar]
- Institute of Medicine. Clinical data as the basic staple of health learning: Creating and protecting a public good: workshop summary. Washington, DC: The National Academies Press; 2010. [PubMed] [Google Scholar]
- Jamoom E, Beatty P, Bercovitz A, Woodwell D, Palso K, Rectsteiner E. NCHS data brief no. 98. Hyattsville, MD: US Department of Health and Human Services, CDC, National Center for Health Statistics; 2012. Physician adoption of electronic health record systems: United States, 2011. [PubMed] [Google Scholar]
- Kendall PC, Kessler RC. The impact of childhood psychopathology interventions on subsequent substance abuse: policy implications, comments, and recommendations. Journal of Consulting and Clinical Psychology. 2002;70:1303–1306. [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. Erratum in: Arch Gen Psychiatry. 2005;62:768. Merikangas, Kathleen R [added] [DOI] [PubMed] [Google Scholar]
- Kokkevi A, Stefanis N, Anastasopoulou E, Kostogianni C. Personality disorders in drug abusers: prevalence and their association with AXIS I disorders as predictors of treatment retention. Addict Behav. 1998;23:841–53. [PubMed] [Google Scholar]
- Kushner MG, Abrams K, Borchardt C. The relationship between anxiety disorders and alcohol use disorders: a review of major perspectives and findings. Clin Psychol Rev. 2000;20:149–71. doi: 10.1016/s0272-7358(99)00027-6. [DOI] [PubMed] [Google Scholar]
- Large M, Sharma S, Compton MT, Slade T, Nielssen O. Cannabis use and earlier onset of psychosis: a systematic meta-analysis. Arch Gen Psychiatry. 2011;68:555–561. doi: 10.1001/archgenpsychiatry.2011.5. [DOI] [PubMed] [Google Scholar]
- Lindsey MA, Joe S, Muroff J, Ford BE. Social and clinical factors associated with psychiatric emergency service use and civil commitment among African-American youth. Gen Hosp Psychiatry. 2010;32:300–9. doi: 10.1016/j.genhosppsych.2010.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubman DI, Allen NB, Rogers N, Cementon E, Bonomo Y. The impact of co-occurring mood and anxiety disorders among substance-abusing youth. J Affect Disord. 2007;103:105–12. doi: 10.1016/j.jad.2007.01.011. [DOI] [PubMed] [Google Scholar]
- McGovern MP, McLellan AT. The status of addiction treatment research with co-occurring substance use and psychiatric disorders. J Subst Abuse Treat. 2008;34:1–2. doi: 10.1016/j.jsat.2007.03.007. [DOI] [PubMed] [Google Scholar]
- Morisano D, Bacher I, Audrain-McGovern J, George TP. Mechanisms underlying the comorbidity of tobacco use in mental health and addictive disorders. Can J Psychiatry. 2009;54:356–67. doi: 10.1177/070674370905400603. [DOI] [PubMed] [Google Scholar]
- Moss TG, Weinberger AH, Vessicchio JC, Mancuso V, Cushing SJ, Pett M, Kitchen K, Selby P, George TP. A tobacco reconceptualization in psychiatry: toward the development of tobacco-free psychiatric facilities. Am J Addict. 2010;19:293–311. doi: 10.1111/j.1521-0391.2010.00051.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muroff J, Edelsohn GA, Joe S, Ford BC. The role of race in diagnostic and disposition decision making in a pediatric psychiatric emergency service. General Hospital Psychiatry. 2008;30:269–276. doi: 10.1016/j.genhosppsych.2008.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Najt P, Fusar-Poly P, Brambilla P. Co-occurring mental and substance abuse disorders: a review on the potential predictors and clinical outcomes. Psychiatr Res. 2011;186:159–164. doi: 10.1016/j.psychres.2010.07.042. [DOI] [PubMed] [Google Scholar]
- Nussbaum A, Thurstone C, Binswanger I. Medical marijuana use and suicide attempt in a patient with major depressive disorder. Am J Psychiatry. 2011;168:778–81. doi: 10.1176/appi.ajp.2011.10121769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Neil KA, Conner BT, Kendall PC. Internalizing disorders and substance use disorders in youth: comorbidity, risk, temporal order, and implications for intervention. Clin Psychol Review. 2011;31:104–112. doi: 10.1016/j.cpr.2010.08.002. [DOI] [PubMed] [Google Scholar]
- Prochaska JJ. Failure to treat tobacco use in mental health and addiction treatment settings: a form of harm reduction? Drug Alcohol Depend. 2010;110:177–82. doi: 10.1016/j.drugalcdep.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ProCon.org. Should marijuana be a medical option? Available at: http://medicalmarijuana.procon.org/
- Silfen E. Documentation and coding of ED patient encounters: an evaluation of the accuracy of an electronic medical record. Am J Emerg Med. 2006;24:664–78. doi: 10.1016/j.ajem.2006.02.005. [DOI] [PubMed] [Google Scholar]
- Silow-Carroll S, Edwards JN, Rodin D. Using electronic health records to improve quality and efficiency: the experiences of leading hospitals. The Commonwealth Fund; Jul, 2012. [PubMed] [Google Scholar]
- Smith SM, Stinson FS, Dawson DA, Goldstein R, Huang B, Grant BF. Race/ethnic differences in the prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med. 2006;36:987–98. doi: 10.1017/S0033291706007690. [DOI] [PubMed] [Google Scholar]
- Snowden LR, Catalano R, Shumway M. Disproportionate use of psychiatric emergency services by african americans. Psychiatr Serv. 2009;60:1664–71. doi: 10.1176/ps.2009.60.12.1664. [DOI] [PubMed] [Google Scholar]
- Strakowski SM, Lonczak HS, Sax KW, West SA, Crist A, Mehta R, Thienhaus OJ. The effects of race on diagnosis and disposition from a psychiatric emergency service. J Clin Psychiatry. 1995;56:101–7. [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. NSDUH Series H-41, HHS Publication No. (SMA) 11-4658. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2011a. Results from the 2010 National Survey on Drug Use and Health: Summary of National Findings. [Google Scholar]
- Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. The TEDS Report: length of time from first use to adult treatment admission. Rockville, MD: 2011b. [Google Scholar]
- Substance Abuse and Mental Health Services Administration, Office of Applied Studies. National Admissions to Substance Abuse Treatment Services, DASIS Series: S-45, DHHS Publication No. (SMA) 09–4360. Rockville, MD: 2009. Treatment Episode Data Set (TEDS). Highlights-2007. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. What you need to know about health reform? Substance Abuse and Mental Health Services Administration News. 2010 Sep-Oct;18(5) [Google Scholar]
- Swendsen J, Conway KP, Degenhardt L, Glantz M, Jin R, Merikangas KR, Sampson N, Kessler RC. Mental disorders as risk factors for substance use, abuse and dependence: results from the 10-year follow-up of the National Comorbidity Survey. Addiction. 2010;105:1117–28. doi: 10.1111/j.1360-0443.2010.02902.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tai B, Wu LT, Clark HW. Electronic health records: essential tools in integrating substance abuse treatment with primary care. Subst Abuse Rehabil. 2012;3:1–8. doi: 10.2147/SAR.S22575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torrens M, Gilchrist G Domingo-Salvany A; psyCoBarcelona Group. Psychiatric comorbidity in illicit drug users: substance-induced versus independent disorders. Drug Alcohol Depend. 2011;113:147–56. doi: 10.1016/j.drugalcdep.2010.07.013. [DOI] [PubMed] [Google Scholar]
- US census. [Accessed September 17, 2012];State & County QuickFacts: North Carolina. http://quickfacts.census.gov/qfd/states/37000.html.
- Weiner MG, Lyman JA, Murphy S, Weiner M. Electronic health records: high-quality electronic data for higher-quality clinical research. Inform Prim Care. 2007;15:121–7. doi: 10.14236/jhi.v15i2.650. [DOI] [PubMed] [Google Scholar]
- Wu LT, Ling W, Burchett B, Blazer DG, Yang C, Pan JJ, Reeve BB, Woody GE. Use of item response theory and latent class analysis to link poly-substance use disorders with addiction severity, HIV risk, and quality of life among opioid-dependent patients in the Clinical Trials Network. Drug Alcohol Depend. 2011a;118:186–93. doi: 10.1016/j.drugalcdep.2011.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Kouzis AC, Leaf PJ. Influence of comorbid alcohol and psychiatric disorders on utilization of mental health services in the National Comorbidity Survey. Am J Psychiatry. 1999;156:1230–6. doi: 10.1176/ajp.156.8.1230. [DOI] [PubMed] [Google Scholar]
- Wu LT, Pilowsky DJ, Schlenger WE, Hasin D. Alcohol use disorders and the use of treatment services among college-age young adults. Psychiatr Serv. 2007;58:192–200. doi: 10.1176/appi.ps.58.2.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Woody GE, Yang C, Blazer DG. Subtypes of nonmedical opioid users: results from the national epidemiologic survey on alcohol and related conditions. Drug Alcohol Depend. 2010;112:69–80. doi: 10.1016/j.drugalcdep.2010.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Gersing K, Burchett B, Woody GE, Blazer DG. Substance use disorders and comorbid Axis I and II psychiatric disorders among young psychiatric patients: Findings from a large electronic health records database. J Psychiatr Res. 2011b;45:1453–62. doi: 10.1016/j.jpsychires.2011.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Woody GE, Yang C, Pan JJ, Blazer DG. Racial/Ethnic variations in substance-related disorders among adolescents in the United States. Arch Gen Psychiatry. 2011c;68:1176–85. doi: 10.1001/archgenpsychiatry.2011.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Woody GE, Yang C, Pan JJ, Reeve BB, Blazer DG. A dimensional approach to understanding severity estimates and risk correlates of marijuana abuse and dependence in adults. Int J Methods Psychiatr Res. 2012;21:117–33. doi: 10.1002/mpr.1354. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Prevalence of substance use disorders (SUDs) by age group among psychiatric patients aged 18–64 years
eTable 2. Prevalence of substance use disorders (SUDs) by sex among psychiatric patients aged 18–64 years
eTable 3. Prevalence of substance use disorders (SUDs) by race/ethnicity among psychiatric patients aged 18–64 years
eTable 4. Prevalence of comorbid psychiatric diagnoses by age group among psychiatric patients aged 18–64 years with a substance use disorder (SUD)
eTable 5. Prevalence of comorbid psychiatric diagnoses by sex among psychiatric patients aged 18–64 years with a substance use disorder (SUD)
eTable 6. Prevalence of comorbid psychiatric diagnoses by race among psychiatric patients aged 18–64 years with a substance use disorder (SUD)
eTable 7. Adjusted multinomial regression of psychiatric treatment type among psychiatric patients aged 18–64 years with a SUD (N=9,844)