Abstract
This study examined the nature and determinants of longitudinal trajectories of disaster-related posttraumatic stress disorder (PTSD) symptoms in older persons affected by a large-magnitude disaster. Two hundred six adults age 60 or older (mean=69, range=60–92) who resided in the Galveston Bay area when Hurricane Ike struck in September 2008 completed telephone interviews an average of 3-, 6-, and 15-months after this disaster. Latent growth mixture modeling was employed to identify predominant trajectories of disaster-related PTSD symptoms over time; and pre-, peri-, and post-disaster determinants of these trajectories were then examined. A 3-class solution optimally characterized PTSD symptom trajectories, with the majority (78.7%) of the sample having low/no PTSD symptoms over all assessments (i.e., resistant); 16.0% having chronically elevated symptoms (i.e., chronic); and 5.3% having a delayed onset course of symptoms (i.e., delayed-onset). Lower education, greater severity of Hurricane Ike exposure (i.e., Ike-related physical illness or injury and high level of community destruction), and greater number of traumatic and stressful life events after Hurricane Ike, particularly financial problems, were associated with a chronic PTSD trajectory. Greater number of traumatic and stressful life events, particularly financial problems after Hurricane Ike, was also associated with a delayed-onset trajectory. These findings suggest that there are heterogeneous trajectories of disaster-related PTSD symptoms in older adults and that these trajectories have common and unique determinants. They also underscore the importance of prevention efforts designed to mitigate the effects of post-disaster stressors, most notably financial distress, in older persons affected by disasters.
Keywords: disaster, posttraumatic stress disorder, longitudinal data, older adults, latent modeling, risk factors
INTRODUCTION
Exposure to a disaster increases risk for posttraumatic stress disorder (PTSD; Acierno et al, 2007; Acierno et al, 2006; Amstadter et al, 2009; Galea et al, 2007; Galea et al, 2005; Galea et al, 2008; Kessler et al, 2008; Norris et al, 2002a; Norris et al, 2002b; Pietrzak et al, 2012b). After a disaster, PTSD symptoms may evolve in complex ways and be characterized by heterogeneous symptom trajectories. Common trajectories of PTSD symptoms that have been identified in trauma-affected samples include minimal to no symptoms over time (i.e., resistant); initial mild-to-moderate symptoms followed by a reduction to minimal/no symptoms over time (i.e., resilient); chronically elevated symptoms over time (i.e., chronic) and initial minimal/no symptoms followed by an increase in symptoms over time (i.e., delayed onset; Bonanno et al, 2008; Bonanno et al, 2012; Bonnano, 2005; deRoon-Cassini et al, 2010; Norris et al, 2009).
Determinants of disaster-related PTSD symptom severity and probable diagnosis may be divided into three categories based on their temporal relation to a disaster (Freedy et al, 1994). Pre-disaster factors are those that precede a disaster, such as female sex, ethnic minority status, lower education and income, and medical and psychiatric history (Norris et al., 2002a; Norris et al., 2002b). Prior exposure to disasters may also help “inoculate” against disaster-related psychological distress, as familiarity or experience in recovering from a disaster may help enhance coping skills (Knight et al, 2000; Norris & Murrell, 1988). Peri-disaster factors are those that occur around the time of the disaster, such as greater severity of trauma exposure, personal losses, community destruction; and peri-disaster dissociative and autonomic symptoms (Bovin & Marx, 2011; Ozer et al, 2003; Shalev et al, 1998). Post-disaster factors are those that occur after a disaster and may affect recovery, such as social support and secondary traumas and life stressors (Acierno et al., 2006; Brewin et al, 2000; Cerda et al, 2012, in press; Kessler et al, 2012; Miguel-Tobal et al, 2006; Person et al, 2006; Tracy et al, 2011). While these studies suggest that a broad range of pre-, peri-, and post-disaster factors may be related to severity and probable diagnoses of disaster-related PTSD, little is known about how they are related to heterogeneous longitudinal trajectories of disaster-related PTSD symptoms.
To date, no study of which we are aware has examined the nature of predominant trajectories of disaster-related PTSD symptoms in older persons. Characterization of such trajectories in this population is important for several reasons. First, older persons may have physical limitations, diminished sensory and cognitive capacities, and/or financial difficulties that may affect their preparation for, adaptability to, and recovery from a disaster (Aldrich & Benson, 2008; Dyer et al, 2008; Fernandez et al, 2002). Second, there are unique risk factors for psychopathology in disaster-affected older adults (Acierno et al., 2006; Phifer & Norris, 1989), including the presence of a chronic psychiatric and/or medical condition, as well as the cumulative burden of trauma and stress, which may increase risk for disaster-related psychopathology (Acierno et al., 2006; Fernandez et al., 2002; Sakauye et al, 2009). Third, older persons are often exposed to a greater level of danger during disasters, are less likely to receive warnings, and often endure greater financial losses (Acierno et al., 2006; Aldrich et al., 2008; Sakauye et al., 2009; Thompson et al, 1993). Fourth, older adults are also more likely to experience subsyndromal than syndromal levels of PTSD symptoms (Glaesmer et al, 2012; Pietrzak et al, 2012a; van Zelst et al, 2003; Yang et al, 2003); and may be uniquely affected by certain risk factors for disaster-related psychopathology (e.g., disaster-related financial losses; Acierno et al., 2007; Kohn et al, 2005; Yang et al., 2003). Taken together, this work suggests that, after a disaster, older adults may exhibit heterogeneous patterns of psychopathology, which may have unique risk factors. For example, older adults with greater personal losses and community destruction may be more likely to have a chronic symptom trajectory, while those who experience an increasing burden of financial distress in the aftermath of a disaster may be more likely to experience a delayed-onset symptom trajectory. Characterization of the nature and determinants of these trajectories in older adults is useful, as it can help identify potentially modifiable factors associated with problematic PTSD symptom trajectories that are specific to this population.
Hurricane Ike was the third costliest hurricane to ever make landfall in the United States, accounting for $29.6 billion in damages. It also caused 195 deaths, and prompted the largest search-and-rescue operation in U.S. history and largest evacuation of Texans in state history (Berg, 2009). In the current study, we sought to examine the nature and determinants of longitudinal trajectories of Hurricane Ike-related PTSD symptoms at 3-, 6-, and 15-months after this disaster in older persons directly affected by this large-magnitude disaster.
MATERIALS AND METHODS
Sample
A total of 658 adults age 18 or older who had been living in Galveston County or Chambers County, Texas for at least one month before September 13, 2008 when Hurricane Ike struck participated in this study. A disproportionate stratified cluster sampling was employed to acquire samples of individuals residing in areas of Galveston County or Chambers County that experienced more damage from Hurricane Ike and that were more likely to be exposed to hurricane-related traumas. The cooperation rate for the full sample was 83%. A total of three assessments were conducted. The median date of the first assessment was December 21, 2008 (3 months, 9 days after Hurricane Ike made landfall in Texas); second assessment was April 05, 2009 (6 months, 24 days after Hurricane Ike made landfall); and third assessment was December 28, 2009 (15 months, 15 days after Hurricane Ike made landfall). Interviews were conducted by experienced interviewers at the University of Michigan Institute for Social Research using a computer-assisted interview system. Interviewer training was tailored to the protocol and survey content, with special emphasis on the context for this study. In their training, interviewers were taught to listen for and observe cues from the respondent that might indicate difficulty comprehending the survey. Interviewers were also trained in how to handle unusual circumstances the might emerge during the interviews, such as respondents’ having hearing, cognitive, or serious medical difficulties; difficulty comprehending survey material; and reluctance to engage in the interview. If an interviewer noticed that a respondent had any of these difficulties, he or she would temporarily discontinue the interview and promptly discuss this with the study supervisor for appropriate follow up. If the interviewer and supervisor concluded that a potential respondent had a limitation that rendered them unable complete the interview, the interview was suspended and coded a non-interview; of respondents aged 60 or older, 5 were coded as non-interviews. Interviews lasted an average of 70 minutes. Additional details regarding sampling and recruitment procedures are available elsewhere (Norris et al, 2010). Two hundred six respondents (31.3% of full sample) were 60 or older at the time of the interview and are the focus of this study. Data were weighted to correct for oversampling and non-response.
Assessments
Hurricane Ike-related PTSD symptoms were assessed using the PTSD Checklist-Specific Stressor Version (Weathers et al, 1993), a 17-item self-report instrument that assesses DSM-IV symptoms of PTSD related to a specific traumatic event. Total scores on the PCL-S range from 17 to 85. Questions regarding Hurricane-Ike PTSD symptoms were assessed by phrasing each of the 17 PCL items in the following manner: “How much were you bothered by repeated, disturbing memories, thoughts, or images of Hurricane Ike? Would you say not at all, a little bit, moderately, quite a bit, or extremely?” In a prior study that employed a receiver operating characteristic (ROC) curve analysis of PCL-S scores in the current sample, a score ≥ 37 was found to be optimal in identifying older persons with a probable DSM-IV-based diagnosis of Hurricane Ike-related PTSD (Pietrzak et al, 2012c). Thus, scores that meet or exceed this threshold are indicative of clinically significant Ike-related PTSD symptoms.
Hurricane Ike exposures were assessed using questions that asked about respondents’ experiences during and after Hurricane Ike. These experiences were grouped into 9 categories: (1) threat to safety of self or family/friends; (2) injury or health problem to self or household member; (3) family member or close friend injured or killed; (4) saw dead bodies during or after Hurricane Ike; (5) damage to three or more types of property (e.g., residence, furnishings, cars/vehicles); (6) financial loss (i.e., lost income as a result of Hurricane Ike); (7) displacement from home > 10 days; (8) lacking two or more necessities for > 1 week (e.g., shelter, electricity, food/water, transportation); and (9) high level of area disruption or damage (sum of ratings of damage and disruption to area schools, churches, streets/highways in the top third for the full sample); Cronbach’s α for summary hurricane exposure measures=.80. A count of these nine exposures was computed as a summary measure of Hurricane Ike exposure.
Traumatic life events were assessed by asking respondents about their exposure to 10 Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV; American Psychiatric Association, 2000) Criterion A-qualifying traumas (e.g., prior disaster exposure, serious accident, sudden unexpected death of someone close (Breslau et al, 1998). Frequency of these events was assessed at each of the assessments: at the first assessment, respondents were asked whether they had experienced these events prior to Hurricane Ike; at the two follow-up assessments, they were asked how many traumatic events they had experienced since the prior interview. Numbers of traumatic life events over the two follow-up assessments were summed to yield a summary measure of total traumatic life events between the initial and last assessment.
Stressful life events. Twelve stressful life events that had occurred in respondents’ lifetimes prior to the disaster were assessed (e.g., serious illness or injury, divorce or break-up, serious financial problems; Boardman et al, 2001). Frequencies of these events were assessed at each of the assessments: at the first assessment, respondents were asked whether they had experienced these events prior to Hurricane Ike; at the two follow-up assessments, they were asked how many stressful life events they had experienced since the prior interview. Numbers of stressful life events over the two follow-up assessments were summed to yield a summary measure of total stressful life events between the initial and last assessment.
History of psychopathology prior to Hurricane Ike was also assessed using the PCL-S, Patient Health Questionnare-9 (PHQ-9; Spitzer et al, 1999)), and Generalized Anxiety Disorder-7 (GAD-7; Spitzer et al, 2006)). The PCL-S queried respondents about PTSD symptoms related to their ‘worst’ traumatic event. The PCL-S was modified to include additional questions about symptom duration and related dysfunction; a probable diagnosis of worst event-related PTSD required endorsement of DSM-IV criteria for PTSD (Pietrzak et al., 2012c). Lifetime history of major depression and generalized anxiety disorder (GAD) prior to Hurricane Ike were assessed using modified versions of the PHQ-9 and GAD-7, which assessed lifetime severity of these disorders. A PHQ-9 score ≥ 10 and GAD-7 score ≥ 8 with concomitant distress and/or functional impairment was indicative of a positive screen for major depression and GAD, respectively.
Peri-event autonomic activation was assessed using the four-item “STRS” scale (Bracha et al, 2004), which assessed self-reported severity of shortness of breath; trembling, shaking, or buckling knees; racing or pounding heart, and/or sweaty palms or other sweating at the time of Hurricane Ike and in the first few hours afterward (Cronbach’s α =.85).
Peri-event dissociative symptoms were measured using a modified version of the Peritraumatic Dissociative Experiences Questionnaire (PDEQ; Marmar et al, 1997), which assessed the extent to which a respondent experienced eight different dissociative symptoms (e.g., feeling disconnected from one’s body, blanking out) during or immediately after Hurricane Ike (Cronbach’s α=.92).
Post-disaster collective efficacy, which is defined as mutual trust among neighbors and willingness of neighbors to intervene on behalf of the common good (Sampson et al, 1997), was assessed using a scale that assesses perceptions of social cohesion (sample item: “This is a close-knit or unified neighborhood”) and informal social control (sample item: “If some children were spray-painting graffiti on a local building, how likely is it that your neighbors would do something about it?”) since Hurricane Ike. The mean of items served as the measure of interest (Cronbach’s α=.86); higher scores indicate higher levels of collective efficacy.
Data Analysis
To characterize longitudinal trajectories of Hurricane Ike-related PTSD symptoms, we conducted latent growth mixture modeling (LGMM) using robust full-information maximum likelihood estimation in Mplus (Muthén, 2004). LGMM allows one to evaluate whether the population under study is composed of a mixture of subpopulations that display distinct trajectories of change over time instead of computing a single mean for the population, as in traditional regression or growth-curve approaches (Curran & Hussong, 2003; Muthén, 2004; Nylund et al, 2007). A univariate single-class growth model was first identified without covariates. We then compared 2- to 6-class unconditional LGMMs and assessed their relative fit using conventional indices, including the Bayesian Information Criterion (BIC), sample size-adjusted BIC (SSA-BIC), Akaike Information Criterion (AIC), entropy, the Lo-Mendell-Rubin likelihood ratio test (LRT; Lo et al, 2001), and the bootstrapped likelihood ratio test (BLRT; McLachlan & Peel, 2000; Nylund et al., 2007). We identified the best-fitting model based on smaller BIC, SSA-BIC, and AIC values, higher entropy values, and on results of the LRT and the BLRT, which quantify the likelihood that the data can be better described by a model with one less trajectory. In addition to inspecting these formal criteria, our efforts to identify the best fitting model of longitudinal trajectories considered class sizes, average latent class probabilities, parsimony, and interpretability of the solutions; we also aimed to select a final model that contained at least 5% of the total sample in the smallest class (Muthén, 2004; Nylund et al., 2007). Each respondent was assigned to the class having the greatest posterior probability. Finally, to characterize determinants of longitudinal trajectories of Hurricane Ike-related PTSD symptoms, we conducted a stepwise multinomial logistic regression analysis. Trajectory group was entered as the dependent variable in this analysis and the least symptomatic trajectory class was specified as the reference group. Pre-, peri-, and post-disaster variables associated with trajectory group membership at the p<0.05 level in bivariate analysis of variance or χ2 analyses were entered as independent variables. If any of the independent variables were correlated at the r>0.50 level (e.g., number of traumas and stressors before and after Ike), a composite score was computed and entered into this analysis. If a composite variable emerged as being significantly related to trajectory group, a post-hoc analysis was conducted to evaluate which variable(s) that comprise this variable were independently related to this outcome; α was set to 0.001 for these analyses to reduce the likelihood of making a Type I error.
RESULTS
Trajectories of Ike-related PTSD symptoms
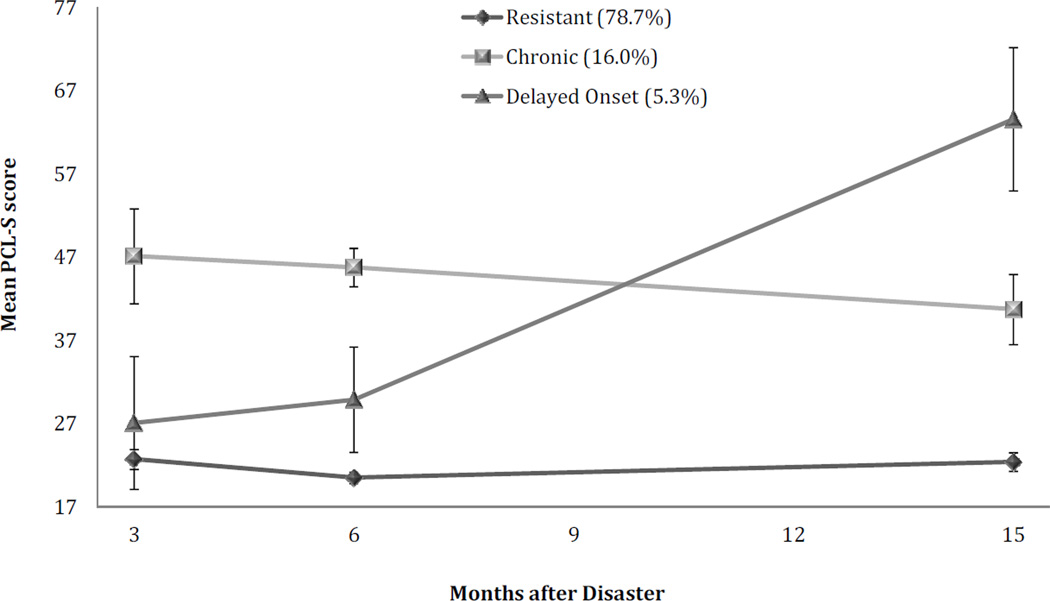
Table 1 shows fit statistics of 1 to 6 class solutions of disaster-related PTSD symptoms over the three assessments. Although BIC, SSA-BIC, and AIC fit statistics suggested relative improvements in fit of models with an increasing number of classes, Entropy values were highest for the 2- and 3-class models, and the BLRT suggested that the 3-class model fit significantly better than the 2-class model. Based on these fit statistics, average latent class probabilities (all >95%), theory, and interpretability/parsimony of the various models (Muthén, 2004; Nylund et al., 2007), we chose the 3-class model as optimal. In this model, 162 (78.7%) respondents had no/low disaster-related PTSD symptoms over time (labeled “Resistant”); 33 (16.0%) had chronically elevated PTSD symptoms over all assessments (labeled “Chronic”); and 11 (5.3%) had a delayed-onset course of PTSD symptoms characterized by low/no symptoms at the first assessment and increasing symptoms over time (labeled “Delayed Onset”). Figure 1 shows mean PCL-S scores over time for each of these groups.
Table 1.
Fit statistics of latent growth mixture models of disaster-related PTSD symptoms
| Log likelihood |
BIC | SSA-BIC | AIC | Entropy | LRT | BLRT | |
|---|---|---|---|---|---|---|---|
| 1-class | −2067.02 | 4176.67 | 4151.32 | 4150.04 | - | - | - |
| 2-class | −2007.53 | 4073.68 | 4038.82 | 4037.07 | .965 | .0009 | <.00001 |
| 3-class | −1975.70 | 4025.98 | 3981.62 | 3979.39 | .933 | .20 | <.0001 |
| 4-class | −1955.90 | 4002.38 | 3948.51 | 3945.80 | .931 | .22 | <.00001 |
| 5-class | −1935.94 | 3978.44 | 3915.07 | 3911.88 | .928 | .18 | <.00001 |
| 6-class | −1918.53 | 3959.59 | 3886.72 | 3883.05 | .932 | .19 | <.0001 |
Note. BIC=Bayesian Information Criterion; SSA-BIC=Sample-size adjusted Bayesian Information Criterion; AIC=Akaike Information Criterion; LRT=Lo-Mendell-Rubin Adjusted Likelihood Ratio Test; BLRT=Parametric Bootstrapped Likelihood Ratio Test. Smaller BIC, SSA-BIC, and AIC values, and higher entropy values indicate better fitting models; significant values for the LRT and the BLRT quantify the likelihood that the data can be better described by a model with one less trajectory.
Figure 1.
Trajectories of disaster-related PTSD symptoms as a function of time since Hurricane Ike in older persons
Note. PCL-S=PTSD Checklist-Specific Stressor Version (score range=17–85); Scores ≥ 37 are indicative of clinically elevated PTSD symptoms (Pietrzak et al., 2012c); Error bars represent 95% confidence intervals
Descriptive statistics
Table 2 shows descriptive statistics for all study variables in the full sample, as well as by trajectory group. On average, respondents had approximately two significant Hurricane Ike exposures, the most common of which were experiencing life threat to self or other (38.3%), being displaced from home ≥ 10 days (34.1%), and incurring a financial loss because of Ike (27.6%).
Table 2.
Demographic, exposure, and clinical characteristics by PTSD symptom trajectory group
| Full sample (n=206) |
Resistant (n=162) |
Chronic Dysfunction (n=33) |
Delayed Dysfunction (n=11) |
Omnibus test of difference |
Pairwise Contrasts |
||
|---|---|---|---|---|---|---|---|
| n (weighted %) or weighted mean (SE) |
n (weighted %) or weighted mean (SE) |
n (weighted %) or weighted mean (SE) |
n (weighted %) or weighted mean (SE) |
F or χ2 | p | ||
| Age | 69.2 (0.5) | 69.3 (0.6) | 68.3 (1.7) | 68.1 (1.9) | 0.50 | 0.61 | - |
| Female sex | 127 (46.4%) | 95 (49.7%) | 26 (52.0%) | 6 (6.2%) | 11.34 | 0.003 | 1,2>3 |
| White, non-Hispanic race/ethnicity | 136 (76.7%) | 117(86.2%) | 16 (61.9%) | 3 (6.2%) | 54.69 | <0.001 | 1,2>3 |
| Some college or higher education | 103 (41.5%) | 88 (49.7%) | 14 (20.0%) | 1 (0%) | 19.21 | <0.001 | 1>2,3 |
| Married/living with partner | 98 (62.7%) | 85 (69.3%) | 10 (56.0%) | 3 (6.7%) | 23.45 | <0.001 | 1,2>3 |
| Household income >$40K | 78 (35.6%) | 68 (40.3%) | 10 (30.0%) | 0 (0%) | 10.50 | 0.005 | 1,2>3 |
| Employed in past week | 49 (22.5%) | 41 (25.0%) | 7 (20.0%) | 1 (0%) | 6.50 | 0.039 | 1>3 |
| Experienced disaster prior to Ike | 99 (59.3%) | 75 (56.2%) | 20 (60.0%) | 4 (87.5%) | 5.88 | 0.053 | 3>1 |
| Hurricane Ike exposure | 1.9 (2.1) | 1.1 (0.1) | 4.4 (0.3) | 5.3 (0.3) | 111.29 | <0.001 | 2,3>1 |
| Serious illness or injury before Ike | 105 (46.4%) | 81 (49.3%) | 19 (54.2%) | 5 (6.2%) | 11.48 | 0.003 | 1,2>3 |
| History of psychopathology | 43 (34.7%) | 26 (18.4%) | 15 (68.8%) | 2 (93.3%) | 5.88 | 0.053 | 2,3>1 |
| Autonomic activation | 1.7 (0.2) | 0.9 (0.2) | 4.8 (0.5) | 3.6 (0.6) | 28.99 | <0.001 | 2,3>1 |
| Dissociative symptoms | 10.6 (0.4) | 9.2 (0.4) | 17.0 (0.9) | 13.2 (1.1) | 33.20 | <0.001 | 2>3>1 |
| Number of traumas before Ike | 2.6 (0.1) | 2.4 (0.1) | 3.0 (0.4) | 3.5 (0.4) | 3.58 | 0.030 | 3>1,2 |
| Number of stressors before Ike | 3.9 (0.2) | 3.7 (0.2) | 5.3 (0.6) | 2.9 (0.6) | 4.60 | 0.011 | 2>1,3 |
| Number traumas after Ike | 0.8 (0.1) | 0.5 (0.1) | 0.7 (0.2) | 3.3 (0.2) | 94.01 | <0.001 | 3>1,2 |
| Number of stressors after Ike | 2.2 (0.2) | 1.0 (0.1) | 3.1 (0.4) | 11.2 (0.4) | 244.35 | <0.001 | 3>2>1 |
| Collective efficacy | 3.9 (0.1) | 4.1 (0.1) | 3.6 (0.2) | 2.9 (0.2) | 16.29 | <0.001 | 1>2>3 |
Note. 1=Resistant group; 2=Chronic Dysfunction group; and 3=Delayed Dysfunction group.
Compared to the Delayed Dysfunction group, the Resistant and Chronic Dysfunction groups were more likely to be female, White, non-Hispanic, married/living with partner, and to have a household income >$40K; the Resistant group was more likely than the Chronic and Delayed Dysfunction groups to have college or higher education, and more likely than the Delayed Dysfunction group to be employed in the week prior to the initial interview. Compared to the Resistant group, the Chronic and Delayed Dysfunction groups reported greater severity of Hurricane Ike exposure and peri-traumatic autonomic activation, and were more likely to have a history of psychopathology. The Delayed Dysfunction group reported experiencing more traumas before and after Ike compared to the Resistant and Chronic Dysfunction groups; they were also more likely than the Resistant group to have experienced a disaster prior to Ike; and reported a greater number of stressors after Ike than the Chronic Dysfunction group, which reported more stressors before Ike than the Resistant and Delayed Dyfunction groups, and more stressors after Ike than the Resistant group. The Resistant and Delayed Dysfunction groups were more likely to have experienced a serious illness or injury before Ike; the Chronic Dysfunction group reported greater severity of peri-traumatic dissociative symptoms than the Delayed Dysfunction group, who reported greater severity of these symptoms relative to the Resistant group. Finally, the Resistant group reported a higher level of community efficacy than the Chronic Dysfunction group, who reported a higher level of efficacy than the Delayed Dysfunction group.
Determinants of Ike-related PTSD symptom trajectories
Results of a stepwise multinomial logistic regression analysis revealed that greater severity of Hurricane Ike exposure (odds ratio [OR]=6.45, 95% confidence interval [CI]=2.87–14.53) and greater number of traumas and stressors between the 3- and 15-month assessments (OR=6.82, 95%CI=1.86–24.96) were associated positively with the chronic PTSD trajectory, while some college or higher education was associated negatively with this outcome (OR=0.15, 95%CI=0.03–0.67). The only variable associated with the delayed-onset PTSD trajectory was the number of traumas and stressors after Hurricane Ike (OR=57.16, 95%CI=10.20–320.36). None of the other variables were significant, all Wald χ2’s<3.26, all p’s>0.07. The interaction of Hurricane Ike exposure severity×number of traumas and stressors after Hurricane Ike was not significantly associated with chronic or delayed-onset PTSD trajectories, Wald χ2=0.33, p=0.56. Post-hoc analyses revealed that experiencing a physical illness or injury (OR=31.42; 95%CI=7.52–131.34) and a high level of community damage (OR=7.24; 95%CI=1.98–26.46) because of Hurricane Ike; and experiencing significant financial problems after Ike (OR=44.70, 95%CI=9.83–203.29) were independently related to the chronic PTSD trajectory. Experiencing significant financial problems after Ike was also independently related to the delayed-onset PTSD trajectory (OR=47.44, 1.50– 501.31).
DISCUSSION
Using a sample of 206 older adults who were recently affected by a large magnitude disaster, we found that the majority (78.7%) had low/no PTSD symptoms over all assessments; 16.0% had chronic, clinically significant symptoms; and 5.3% had a delayed-onset course of clinically significant symptoms. This solution is consistent with prior longitudinal studies of general adult samples of trauma survivors, which have similarly observed that a majority have minimal or no symptoms after a traumatic event, while a relatively smaller proportion have chronic or other patterns of adaptation (Bonanno et al, 2006; Bonanno et al., 2008; Bonanno et al., 2012; Bonnano, 2005; deRoon-Cassini et al., 2010; Norris et al., 2009).
We found that greater severity of Hurricane Ike exposure, and greater number of traumas and stressors since this disaster were associated positively with a chronic PTSD symptom trajectory, while some college or higher education was associated negatively with this trajectory. A greater number of traumas and stressors since Hurricane Ike was also associated with a delayed-onset PTSD trajectory. These findings extend prior work on factors associated with symptom severity of probable diagnoses of disaster-related PTSD and related psychopathology to provide a characterization of determinants of heterogeneous longitudinal trajectories of disaster-related PTSD symptoms in older adults.
Results of the current study corroborate a growing body of prior disaster mental health research, which found that post-disaster life stressors and traumas (Brewin et al., 2000; Cerda et al., 2012, in press; Kessler et al., 2012; Norris & Uhl, 1993; Norris et al., 2002a; Norris et al., 2002b; Tracy et al., 2011), including financial losses (Acierno et al., 2006; Galea et al., 2008; Rajkumar et al, 2011, in press; Su et al, 2010), are linked to severity, probable diagnoses, and chronicity of PTSD and related disorders. The finding that greater education was negatively related to a chronic symptom trajectory also accords with previous studies demonstrating the protective effect of this variable on risk for disaster-related PTSD and related mental disorders (Armenian et al, 2000; Norris et al., 2002a; Norris et al., 2002b; North et al, 2012; Yuan et al, 2012, in press). Results of the current study are also in line with prior work conducted in older disaster survivors, which found that community destruction and financial consequences of disasters were uniquely linked to post-disaster psychological difficulties (Acierno et al., 2007; Phifer et al., 1989; Yang et al., 2003).
Importantly, they extend this work to suggest that experiencing a physical injury or illness is additionally associated with a chronic trajectory of disaster-related PTSD symptoms in older persons. Taken together, these results highlight the need for continued monitoring and timely intervention for disaster-affected older persons, particularly those with lower levels of education, disaster-related physical injury or illness, high level of community disruption, and financial distress. For example, disaster prevention and intervention efforts focused on building community resilience, which encompass multi-level strategies to reduce risk and resource inequities; foster organizational linkages; and bolster social support across individuals, families, and communities at large, may help reduce the burden of psychological distress after disasters (Agani et al., 2010; Hobfoll et al., 2007; Landau, 2007; Norris et al., 2009). Among older adults, who often have fixed incomes and may not have the financial resources to manage post-disaster expenses, community-based intervention strategies that address financial difficulties may be especially helpful in mitigating disaster-related psychological distress.
This study has some methodological limitations that must be noted. First, PTSD symptoms were assessed using a screening instrument, so it is unclear if results would differ if diagnostic instruments or clinician interviews were to be utilized. Employment of such methods may reveal a lower proportion of persons who have a chronic or delayed-onset PTSD symptom trajectory, as they are more conservative and specific in diagnosing PTSD compared to screening instruments such as the PCL-S. Second, because the age distribution of the sample was skewed toward the 60–69 age range, generalizability of these results is limited to “young-old” persons. Third, given that the current study focused on the psychological effects of Hurricane Ike, comprehensive information regarding respondents’ medical histories, and ambulatory/disability and cognitive status, which may be linked to post-disaster psychopathology (Aldrich et al., 2008; Fernandez et al., 2002; Sakauye et al., 2009), was not obtained. Fourth, while peri-traumatic reactions such as autonomic arousal and dissociation (Brewin et al., 2000; Ozer et al., 2003), and community efficacy (Norris et al., 2008) are known risk factors for PTSD, and were associated with symptomatic PTSD trajectories in bivariate analyses in the current study, they were not significant when considered in the context of other covariates in a multivariate analysis. Retrospective recall bias and/or reduced statistical power in this analysis, which capitalized on identifying covariates with the largest magnitude association with symptomatic PTSD trajectories, may, at least in part, account for this finding. Additional research in larger samples of disaster-affected older persons will be useful in further evaluating the nature of post-disaster psychological symptom trajectories, and pre-, peri-, and post-disaster determinants of these trajectories in this population.
Notwithstanding these limitations, this study is among the first of which we are aware to characterize the nature and determinants of longitudinal trajectories of disaster-related PTSD symptoms in older adults. Methodological strengths of this study include a rigorous sampling strategy; collection of data within two to five months of a major disaster; and assessment of a comprehensive range of pre-, peri-, and post-disaster risk factors for PTSD (Norris et al., 2010). Taken together, results of this study suggest that older adults exhibit heterogeneous trajectories of PTSD symptoms after a disaster, with a considerable proportion—21.3%—experiencing clinically elevated symptoms, even 15 months later. Lower levels of education, disaster-related physical injury or illness, high level of community disruption, and significant post-disaster financial problems were independently linked to a chronic symptom trajectory, and financial problems were linked to delayed dysfunction. Taken together, results of this study highlight the need for continued monitoring and amelioration of stressful life events, most notably financial distress, in disaster-affected older persons, as they were most strongly related to both the chronicity and delayed onset of clinically elevated PTSD symptoms. Further research is needed to evaluate the effectiveness of prevention and treatment efforts that target the specific needs of this population in mitigating risk for PTSD and related disorders in the aftermath of a disaster.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Acierno R, Ruggiero KJ, Galea S, Resnick HS, Koenen K, Roitzsch J, de Arellano M, Boyle J, Kilpatrick DG. Psychological sequelae resulting from the 2004 Florida hurricanes: implications for postdisaster intervention. American Journal of Public Health. 2007;97(Suppl 1):S103–S108. doi: 10.2105/AJPH.2006.087007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acierno R, Ruggiero KJ, Kilpatrick DG, Resnick HS, Galea S. Risk and protective factors for psychopathology among older versus younger adults after the 2004 Florida hurricanes. American Journal of Geriatric Psychiatry. 2006;14:1051–1059. doi: 10.1097/01.JGP.0000221327.97904.b0. [DOI] [PubMed] [Google Scholar]
- Agani F, Landau J, Agani N. Community-building before, during, and after times of trauma: the application of the LINC model of community resilience in Kosovo. American Journal of Orthopsychiatry. 2010;80:143–149. doi: 10.1111/j.1939-0025.2010.01017.x. [DOI] [PubMed] [Google Scholar]
- Aldrich N, Benson WF. Disaster preparedness and the chronic disease needs of vulnerable older adults. Preventing Chronic Disease. 2008;5:A27. [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders, fourth edition, text revision. Washington, DC: American Psychiatric Press; 2000. [Google Scholar]
- Amstadter AB, Acierno R, Richardson LK, Kilpatrick DG, Gros DF, Gaboury MT, Tran TL, Trung LT, Tam NT, Tuan T, Buoi LT, Ha TT, Thach TD, Galea S. Post-typhoon prevalence of posttraumatic stress disorder, major depressive disorder, panic disorder, and generalized anxiety disorder in a Vietnamese sample. Journal of Traumatic Stress. 2009;22:180–188. doi: 10.1002/jts.20404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armenian HK, Morikawa M, Melkonian AK, Hovanesian AP, Haroutunian N, Saigh PA, Akiskal K, Akiskal HS. Loss as a determinant of PTSD in a cohort of adult survivors of the 1988 earthquake in Armenia: implications for policy. Acta Psychiatrica Scandinavica. 2000;102:58–64. doi: 10.1034/j.1600-0447.2000.102001058.x. [DOI] [PubMed] [Google Scholar]
- Berg R. Hurricane Ike Tropical Cyclone Report. National Hurricane Center. 2009:01–23. [Google Scholar]
- Boardman JD, Finch BK, Ellison CG, Williams DR, Jackson JS. Neighborhood disadvantage, stress, and drug use among adults. Journal of Health and Social Behavior. 2001;42:151–165. [PubMed] [Google Scholar]
- Bonanno GA, Galea S, Bucciarelli A, Vlahov D. Psychological resilience after disaster: New York City in the aftermath of the September 11th terrorist attack. Psychol Sci. 2006;17:181–186. doi: 10.1111/j.1467-9280.2006.01682.x. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Ho SMY, Chan JCK, Kwong RSY, Cheung CKY, Wong CPY, Wong VCW. Psychological resilience and dysfunction among hospitalized survivors of the SARS epidemic in Hong Kong: A latent class approach. Health Psychology. 2008;27:659–667. doi: 10.1037/0278-6133.27.5.659. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Mancini AD, Horton JL, Powell TM, Leardmann CA, Boyko EJ, Wells TS, Hooper TI, Gackstetter GD, Smith TC. Trajectories of trauma symptoms and resilience in deployed U.S. military service members: prospective cohort study. Br J Psychiatry. 2012;200:317–323. doi: 10.1192/bjp.bp.111.096552. [DOI] [PubMed] [Google Scholar]
- Bonnano GA. Resilience in the face of potential trauma. Current Directions in Psychological Science. 2005;14:135–138. [Google Scholar]
- Bovin MJ, Marx BP. The importance of the peritraumatic experience in defining traumatic stress. Psychological Bulletin. 2011;137:47–67. doi: 10.1037/a0021353. [DOI] [PubMed] [Google Scholar]
- Bracha HS, Williams AE, Haynes SN, Kubany ES, Ralston TC, Yamashita JM. The STRS (shortness of breath, tremulousness, racing heart, and sweating): A brief checklist for acute distress with panic-like autonomic indicators, development and factor structure. Annals of General Psychiatry. 2004;3:8. doi: 10.1186/1475-2832-3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N, Kessler R, Chilcoat H, Schultz L, Davis G, Andreski P. Trauma and posttraumatic stress disorder in the community: The 1996 Detroit area survey of trauma. Archives of General Psychiatry. 1998;55:626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Brewin C, Andrews B, Valentine J. Meta-analysis of risk factors for post-traumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology. 2000;68:748–766. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- Cerda M, Bordelois PM, Galea S, Norris F, Tracy M, Koenen KC. The course of posttraumatic stress symptoms and functional impairment following a disaster: what is the lasting influence of acute versus ongoing traumatic events and stressors? Social Psychiatry and Psychiatric Epidemiology. 2012 doi: 10.1007/s00127-012-0560-3. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran PJ, Hussong AM. The use of latent trajectory models in psychopathology research. Journal of Abnormal Psychology. 2003;112:526–544. doi: 10.1037/0021-843X.112.4.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- deRoon-Cassini TA, Mancini A, Rusch MD, Bonanno GA. Psychopathology and resilience following traumatic injury: A latent growth mixture model analysis. Rehabilitation Psychology. 2010;55:1–11. doi: 10.1037/a0018601. [DOI] [PubMed] [Google Scholar]
- Dyer CB, Regev M, Burnett J, Festa N, Cloyd B. SWiFT: a rapid triage tool for vulnerable older adults in disaster situations. Disaster Medicine and Public Health Preparedness. 2008;2(Suppl 1):S45–S50. doi: 10.1097/DMP.0b013e3181647b81. [DOI] [PubMed] [Google Scholar]
- Fernandez LS, Byard D, Lin CC, Benson S, Barbera JA. Frail elderly as disaster victims: emergency management strategies. Prehospital & Disaster Medicine. 2002;17:67–74. doi: 10.1017/s1049023x00000200. [DOI] [PubMed] [Google Scholar]
- Freedy JR, Saladin ME, Kilpatrick DG, Resnick HS, Saunders BE. Understanding acute psychological distress following natural disaster. Journal of Traumatic Stress. 1994;7:257–273. doi: 10.1007/BF02102947. [DOI] [PubMed] [Google Scholar]
- Galea S, Brewin CR, Gruber M, Jones RT, King DW, King LA, McNally RJ, Ursano RJ, Petukhova M, Kessler RC. Exposure to hurricane-related stressors and mental illness after Hurricane Katrina. Archives of General Psychiatry. 2007;64:1427–1434. doi: 10.1001/archpsyc.64.12.1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S, Nandi A, Vlahov D. The epidemiology of post-traumatic stress disorder after disasters. Epidemiologic Reviews. 2005;27:78–91. doi: 10.1093/epirev/mxi003. [DOI] [PubMed] [Google Scholar]
- Galea S, Tracy M, Norris F, Coffey SF. Financial and social circumstances and the incidence and course of PTSD in Mississippi during the first two years after Hurricane Katrina. Journal of Traumatic Stress. 2008;21:357–368. doi: 10.1002/jts.20355. [DOI] [PubMed] [Google Scholar]
- Glaesmer H, Kaiser M, Braehler E, Freyberger HJ, Kuwert P. Posttraumatic stress disorder and its comorbidity with depression and somatisation in the elderly - a German community-based study. Aging and Mental Health. 2012;16:403–412. doi: 10.1080/13607863.2011.615740. [DOI] [PubMed] [Google Scholar]
- Hobfoll SE, Watson P, Bell CC, Bryant RA, Brymer MJ, Friedman MJ, Friedman M, Gersons BP, de Jong JT, Layne CM, Maguen S, Neria Y, Norwood AE, Pynoos RS, Reissman D, Ruzek JI, Shalev AY, Solomon Z, Steinberg AM, Ursano RJ. Five essential elements of immediate and mid-term mass trauma intervention: empirical evidence. Psychiatry. 2007;70:283–315. doi: 10.1521/psyc.2007.70.4.283. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Galea S, Gruber MJ, Sampson NA, Ursano RJ, Wessely S. Trends in mental illness and suicidality after Hurricane Katrina. Molecular Psychiatry. 2008;13:374–384. doi: 10.1038/sj.mp.4002119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, McLaughlin KA, Koenen KC, Petukhova M, Hill ED. The importance of secondary trauma exposure for post-disaster mental disorder. Epidemiology and Psychiatric Sciences. 2012;21:35–45. doi: 10.1017/s2045796011000758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight BG, Gatz M, Heller K, Bengtson VL. Age and emotional response to the Northridge earthquake: a longitudinal analysis. Psychology and Aging. 2000;15:627–634. doi: 10.1037//0882-7974.15.4.627. [DOI] [PubMed] [Google Scholar]
- Kohn R, Levav I, I.D. G, Machuca ME, Tamashiro R. Prevalence, risk factors and aging vulnerability for psychopathology following a natural disaster in a developing country. International Journal of Geriatric Psychiatry. 2005;20:835–841. doi: 10.1002/gps.1369. [DOI] [PubMed] [Google Scholar]
- Landau J. Enhancing resilience: families and communities as agents for change. Family Process. 2007;46:351–365. doi: 10.1111/j.1545-5300.2007.00216.x. [DOI] [PubMed] [Google Scholar]
- Lo Y, Mendell N, Rubin D. Testing the number of components in a normal mixture. Biometrika. 2001;88:767–778. [Google Scholar]
- Marmar CR, Weiss DS, Metzler TJ. The Peritraumatic Dissociative Experiences Questionnaire. In: Wilson JP, Keane TM, editors. Assessing psychological trauma and PTSD. New York: Guilford Press; 1997. pp. 412–428. [Google Scholar]
- McLachlan G, Peel D. Finite mixture models. New York, NY: Wiley; 2000. [Google Scholar]
- Miguel-Tobal JJ, Cano-Vindel A, Gonzalez-Ordi H, Iruarrizaga I, Rudenstine S, Vlahov D, Galea S. PTSD and depression after the Madrid March 11 train bombings. Journal of Traumatic Stress. 2006;19:69–80. doi: 10.1002/jts.20091. [DOI] [PubMed] [Google Scholar]
- Muthén B. Latent variable analysis: growth mixture modeling and related techniques for longitudinal data. In: Kaplan D, editor. Handbook of quantitative methodology for the social sciences. Newbury Park, CA: Sage Publications; 2004. pp. 345–368. [Google Scholar]
- Norris F, Uhl G. Chronic stress as a mediator of acute stress: the case of hurricane Hugo. Journal of Applied Social Psychology. 1993;23:1263–1284. [Google Scholar]
- Norris FH, Friedman MJ, Watson PJ. 60,000 disaster victims speak: Part II. Summary and implications of the disaster mental health research. Psychiatry. 2002a;65:240–260. doi: 10.1521/psyc.65.3.240.20169. [DOI] [PubMed] [Google Scholar]
- Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, Kaniasty K. 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981–2001. Psychiatry. 2002b;65:207–239. doi: 10.1521/psyc.65.3.207.20173. [DOI] [PubMed] [Google Scholar]
- Norris FH, Murrell SA. Prior experience as a moderator of disaster impact on anxiety symptoms in older adults. American Journal of Community Psychology. 1988;16:665–683. doi: 10.1007/BF00930020. [DOI] [PubMed] [Google Scholar]
- Norris FH, Sherrieb K, Galea S. Prevalence and consequences of disaster-related illness and injury from Hurricane Ike. Rehabilitation Psychology. 2010;55:221–230. doi: 10.1037/a0020195. [DOI] [PubMed] [Google Scholar]
- Norris FH, Stevens SP, Pfefferbaum B, Wyche KF, Pfefferbaum RL. Community resilience as a metaphor, theory, set of capacities, and strategy for disaster readiness. American Journal of Community Psychology. 2008;41:127–150. doi: 10.1007/s10464-007-9156-6. [DOI] [PubMed] [Google Scholar]
- Norris FH, Tracy M, Galea S. Looking for resilience: understanding the longitudinal trajectories of responses to stress. Social Science & Medicine. 2009;68:2190–2198. doi: 10.1016/j.socscimed.2009.03.043. [DOI] [PubMed] [Google Scholar]
- North CS, Oliver J, Pandya A. Examining a comprehensive model of disaster-related posttraumatic stress disorder in systematically studied survivors of 10 disasters. American Journal of Public Health. 2012;102:e40–e48. doi: 10.2105/AJPH.2012.300689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, Muthén B. Deciding on the number of classes in latent class analysis and growth mixture modeling. A Monte Carlo simulation study. Structural Equation Modeling. 2007;14:535–569. [Google Scholar]
- O'Sullivan TL, Kuziemsky CE, Toal-Sullivan D, Corneil W. Unraveling the complexities of disaster management: A framework for critical social infrastructure to promote population health and resilience. Social Science & Medicine. doi: 10.1016/j.socscimed.2012.07.040. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychological Bulletin. 2003;129:52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- Person C, Tracy M, Galea S. Risk factors for depression after a disaster. Journal of Nervous and Mental Disease. 2006;194:659–666. doi: 10.1097/01.nmd.0000235758.24586.b7. [DOI] [PubMed] [Google Scholar]
- Phifer JF, Norris FH. Psychological symptoms in older adults following natural disaster: nature, timing, duration, and course. Journal of Gerontology. 1989;44:S207–S217. doi: 10.1093/geronj/44.6.s207. [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Psychiatric comorbidity of full and partial posttraumatic stress disorder among older adults in the United States: results from wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. American Journal of Geriatric Psychiatry. 2012a;20:380–390. doi: 10.1097/JGP.0b013e31820d92e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrzak RH, Southwick SM, Tracy M, Galea S, Norris FH. Posttraumatic stress disorder, depression, and perceived needs for psychological care in older persons affected by Hurricane Ike. Journal of Affective Disorders. 2012b;138:96–103. doi: 10.1016/j.jad.2011.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrzak RH, Van Ness PH, Fried TR, Galea S, Norris F. Diagnostic utility and factor structure of the PTSD Checklist in older adults. International Psychogeriatrics. 2012c;24:1684–1696. doi: 10.1017/S1041610212000853. [DOI] [PubMed] [Google Scholar]
- Rajkumar AP, Mohan TS, Tharyan P. Lessons from the 2004 Asian tsunami: Epidemiological and nosological debates in the diagnosis of post-traumatic stress disorder in non-Western post-disaster communities. International Journal of Social Psychiatry. 2011 doi: 10.1177/0020764011423468. in press. [DOI] [PubMed] [Google Scholar]
- Sakauye KM, Streim JE, Kennedy GJ, Kirwin PD, Llorente MD, Schultz SK, Srinivasan S. AAGP position statement: disaster preparedness for older Americans: critical issues for the preservation of mental health. American Journal of Geriatric Psychiatry. 2009;17:916–924. doi: 10.1097/JGP.0b013e3181b4bf20. [DOI] [PubMed] [Google Scholar]
- Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: A multilevel study of collective efficacy. Science. 1997;5328:918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- Shalev AY, Sahar T, Freedman S, Peri T, Glick N, Brandes D, Orr SP, Pitman RK. A prospective study of heart rate response following trauma and the subsequent development of posttraumatic stress disorder. Archives of General Psychiatry. 1998;55:553–559. doi: 10.1001/archpsyc.55.6.553. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD - The PHQ primary care study. Journal of the American Medical Association. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Archives of Internal Medicine. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Su CY, Tsai KY, Chou FH, Ho WW, Liu R, Lin WK. A three-year follow-up study of the psychosocial predictors of delayed and unresolved post-traumatic stress disorder in Taiwan Chi-Chi earthquake survivors. Psychiatry and Clinical Neurosciences. 2010;64:239–248. doi: 10.1111/j.1440-1819.2010.02087.x. [DOI] [PubMed] [Google Scholar]
- Thompson MP, Norris FH, Hanacek B. Age differences in the psychological consequences of Hurricane Hugo. Psychology and Aging. 1993;8:606–616. doi: 10.1037//0882-7974.8.4.606. [DOI] [PubMed] [Google Scholar]
- Tracy M, Norris FH, Galea S. Differences in the determinants of posttraumatic stress disorder and depression after a mass traumatic event. Depression and Anxiety. 2011;28:666–675. doi: 10.1002/da.20838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Zelst WH, de Beurs E, Beekman AT, Deeg DJ, van Dyck R. Prevalence and risk factors of posttraumatic stress disorder in older adults. Psychotherapy and Psychosomatics. 2003;72:333–342. doi: 10.1159/000073030. [DOI] [PubMed] [Google Scholar]
- Weathers F, Litz B, Herman D, Huska J, Keane T. The PTSD checklist (PCL): Reliability, validity, and diagnostic utility. San Antonio, TX: Meeting of the International Society of Traumatic Stress Studies; 1993. [Google Scholar]
- Yang YK, Yeh TL, Chen CC, Lee CK, Lee IH, Lee LC, Jeffries KJ. Psychiatric morbidity and posttraumatic symptoms among earthquake victims in primary care clinics. General Hospital Psychiatry. 2003;25:253–261. doi: 10.1016/s0163-8343(03)00022-7. [DOI] [PubMed] [Google Scholar]
- Yuan KC, Ruoyao Z, Zhenyu S, Xudong Z, Jianzhong Y, Edwards JG, Edwards GD. Prevalence and predictors of stress disorders following two earthquakes. International Journal of Social Psychiatry. 2012 doi: 10.1177/0020764012453233. in press. [DOI] [PubMed] [Google Scholar]