Abstract
OBJECTIVE:
To determine if obesity and dietary quality in low-income children differed by participation in the Supplemental Nutrition Assistance Program (SNAP), formerly the Food Stamp Program.
METHODS:
The study population included 5193 children aged 4 to 19 with household incomes ≤130% of the federal poverty level from the 1999–2008 NHANES. Diet was measured by using 24-hour recalls.
RESULTS:
Among low-income US children, 28% resided in households currently receiving SNAP benefits. After adjusting for sociodemographic differences, SNAP participation was not associated with a higher rate of childhood obesity (odds ratio = 1.11, 95% confidence interval [CI]: 0.71–1.74). Both SNAP participants and low-income nonparticipants were below national recommendations for whole grains, fruits, vegetables, fish, and potassium, while exceeding recommended limits for processed meat, sugar-sweetened beverages, saturated fat, and sodium. Zero percent of low-income children met at least 7 of 10 dietary recommendations. After multivariate adjustment, compared with nonparticipants, SNAP participants consumed 43% more sugar-sweetened beverages (95% CI: 8%–89%), 47% more high-fat dairy (95% CI: 7%, 101%), and 44% more processed meats (95% CI: 9%–91%), but 19% fewer nuts, seeds, and legumes (95% CI: –35% to 0%). In part due to these differences, intakes of calcium, iron, and folate were significantly higher among SNAP participants. Significant differences by SNAP participation were not evident in total energy, macronutrients, Healthy Eating Index 2005 scores, or Alternate Healthy Eating Index scores.
CONCLUSIONS:
The diets of low-income children are far from meeting national dietary recommendations. Policy changes should be considered to restructure SNAP to improve children’s health.
KEY WORDS: Supplemental Nutrition Assistance Program, Food Stamps, nutrition, diet quality, children
What’s Known on This Subject:
The Supplemental Nutrition Assistance Program (SNAP) is the largest federal nutrition assistance program. Studies among adults suggest that SNAP participation may be associated with suboptimal diets. Few studies have extensively examined these associations among children.
What This Study Adds:
SNAP participation was not associated with childhood obesity. SNAP children consumed diets poorer in some aspects than nonparticipants, but intake of some micronutrients was higher. The diets of both groups of low-income children were far from meeting dietary guidelines.
The Food Stamp Program, renamed the Supplemental Nutrition Assistance Program (SNAP) in 2008, is the largest of 15 federal nutrition assistance programs. The Food Stamp Program was implemented in 1964 to provide food assistance and distribute agricultural commodities to low-income individuals.1 Participation is at its highest since the program’s inception; in 2011, 45 million Americans received food stamps, at a cost of $72 billion.2,3 Program eligibility is generally determined by having a household income ≤130% of the federal poverty level (FPL), equivalent to a gross monthly income of $2389 for a 4-person household in 2011.4,5 SNAP benefits can be used to purchase most foods and beverages except for alcohol, supplements, and prepared foods.
Although initially established as a program to reduce food insecurity, current obesity trends have increased the emphasis on encouraging participants to choose healthful, nutrient-rich foods.6,7 Unlike other food assistance programs, SNAP does not use a defined food list or have menu standards; its effects on dietary quality are not well established.8 Because few foods are ineligible for purchase with SNAP benefits, some public health advocates have questioned whether SNAP benefits are excessively used to buy nutrient-poor foods that may promote obesity and poor health over time.9 A 2000 US Department of Agriculture (USDA) analysis of the 1994–1996 Continuing Survey of Food Intake by Individuals suggested that Food Stamp participants consumed more meat, added sugars, and total fat after receiving benefits; differences were not observed for fruits, vegetables, total grains, and dairy products.10 A 2008 USDA report using 1999–2004 NHANES data found that adult Food Stamp recipients consumed a greater proportion of calories from solid fats, added sugars, and alcoholic beverages compared with income-eligible nonparticipants.11
SNAP has been shown to reduce poverty among the poorest Americans by providing resources to purchase food.12 We would hope that dietary quality would be better among program participants because of these additional benefits. Unfortunately, previous studies suggest that SNAP participation may be associated with suboptimal dietary patterns among low-income adults. These associations have not been extensively examined in children, who represent 47% of SNAP beneficiaries.13–16 Early-life dietary patterns are especially important for low-income children who are at higher risk for obesity and obesity-related metabolic consequences.17–20 The high rates of obesity and food insecurity in low-income populations underscore the importance of employing SNAP as a program to promote healthier food choices. In a national sample of low-income children, we investigated overall dietary quality and whether differences were present by SNAP participation in (1) overweight and obesity status, (2) consumption of foods and nutrients, and (3) overall dietary quality.
Methods
Study Population
NHANES is an ongoing, multistage cross-sectional survey administered by the National Center for Health Statistics. This analysis combined data from the 1999–2008 surveys to maximize a sufficient representation of SNAP participants. The analytical sample was restricted to children aged 4 to 19 years with household incomes ≤130% FPL who had complete dietary data. For the interview component, proxy respondents (a parent/guardian) reported for children aged 4 to 5 years and assisted with survey completion for children aged 6 to 11 years. Children aged 12 to 19 years reported for themselves. The analytical sample comprised 5193 children.
SNAP Participation
Current SNAP participants were classified as program participation at the time of the NHANES interview. Nonparticipants were classified as not receiving Food Stamp benefits within the past 12 months. Former participants (individuals who were not receiving benefits at the time of the survey but had received benefits within the past 12 months) were excluded to provide a more appropriate comparison between current SNAP participants and income-eligible nonparticipants.
Overweight and Obesity Status
NHANES reports BMI as kg/m2 from measured height and weight.21 For children aged 4 to 17 years, BMI was transformed into z scores by using the 2000 Centers for Disease Control and Prevention Growth Charts and categorized into normal weight, overweight, or obese by using established age- and gender-specific cutpoints.22,23 For children aged 18 to 19 years, BMI was classified into standard weight categories.24
Dietary Intake
From 1999 through 2002, NHANES administered one 24-hour dietary recall in-person to study participants. From 2003 through 2008, a second recall was administered over the phone 3 to 10 days after the first examiation.25
Foods, Food Groups, and Nutrients
We selected foods, food groups and nutrients based on their importance to children’s growth and future adult health (Supplemental Table 6).26–28 We then estimated servings by calculating the grams of intake of each food and applying common serving sizes. Nutrient intakes were derived from the NHANES nutrient files; contributions from dietary supplements were excluded. Consumption levels were compared with national dietary recommendations for chronic disease prevention (Supplemental Table 7).27,29,30
Dietary Patterns
Overall dietary quality was assessed by using the Healthy Eating Index 2005 (HEI-2005) and the Alternate Healthy Eating Index (AHEI). The USDA MyPyramid Equivalents Databases were used to estimate MyPyramid equivalents for the HEI-2005.31 The AHEI was developed by the Harvard School of Public Health as a dietary pattern related to chronic disease risk in adults, although this has not been examined in children.32,33 For this analysis, we modified the original 9 AHEI components by excluding trans fat, which was unavailable in NHANES, and alcohol, which was considered inappropriate for children’s dietary quality. Multivitamin use was defined as any use in the past 30 days.34 The maximum AHEI score was rescaled to the original 87.5 points for comparability with other studies.
Study Covariates
Covariates of interest included the child’s age, gender, race/ethnicity, household reference person’s (HR) place of birth, HR education level, HR marital status, household size, health insurance status, poverty income ratio, household food security, and participation in other food assistance programs. The HR was ≥18 years and owned or rented the residence of the study participant. Missing indicators were used to account for missing HR place of birth, HR education level, HR marital status, or other food assistance program participation. Household food security was assessed by using the USDA 18-item US Food Security Survey Module.35
Statistical Analysis
To make nationally representative estimates, we used complex Mobile Examination Center and dietary survey weights that account for different sampling probabilities and participation rates for NHANES across the 10-year period.
Means and distributions of foods and nutrients were estimated for all low-income children, and by age, gender and food security groups using the National Cancer Institute statistical method for usual dietary intake, which accounts for the within-person variation of dietary intake while preserving the complex NHANES weighting scheme.36 The National Cancer Institute method involves 2 SAS macros using “integerized” dietary survey weights.37,38 Standard errors were estimated by using the balanced repeated replication method.
Sociodemographic characteristics between SNAP participants and nonparticipants were compared by using χ2 tests. Associations between SNAP participation and children’s weight status were examined by fitting multinomial logistic regression models for childhood weight status, using normal weight as the reference. The first model adjusted for age and gender. The multivariate model included all study covariates. Models were estimated separately by subgroups of age, gender, and food security status.
To estimate the relative difference in dietary intake by SNAP participation, linear regression models were fit for log-transformed outcomes (due to the skewness of dietary outcomes). Dietary outcome values of 0 were recoded to half of the minimum amount consumed. Models were adjusted for all study covariates and total energy. Relative differences for the HEI-2005 and AHEI were estimated using the same models for foods and nutrients.
All statistical tests were 2-sided. Significance was considered at P < .05. Statistical analyses were performed by using SAS 9.3 (SAS Institute Inc, Cary, NC).
Results
Of the 5193 low-income children in the study population, 27.9% participated in SNAP at the time of the survey. Children participating in SNAP were significantly more likely to be from a single-parent household, enrolled in public health insurance (eg, SCHIP, Medicaid), participate in other nutrition assistance programs, live below the FPL, and report lower household food security than nonparticipants (Table 1).
TABLE 1.
Sociodemographic Characteristics of Children ≤130% FPL
| SNAP Nonparticipants (n = 3831) | SNAP Participants (n = 1362) | |||
|---|---|---|---|---|
| n | % | n | % | |
| Age, mean ± SE. | 12.0 ± 0.2 | 10.4 ± 0.2 | ||
| % girl | 1949 | 49.1 | 715 | 53.3 |
| Race | ||||
| Non-Hispanic white | 723 | 48.8 | 223 | 37.9 |
| African American | 1161 | 17.7 | 652 | 31.2 |
| Hispanic/Latino | 1801 | 26.0 | 430 | 24.9 |
| Other or multiple ethnicities | 146 | 7.5 | 57 | 6.0 |
| % HR born in the United States | 2152 | 73.3 | 1022 | 78.8 |
| HR education level | ||||
| <12 y | 1680 | 33.1 | 764 | 49.6 |
| High school graduate | 917 | 28.6 | 332 | 30.5 |
| Some college | 776 | 26.2 | 211 | 16.4 |
| College graduate or higher | 243 | 12.2 | 21 | 3.5 |
| HR marital status | ||||
| Single | 700 | 18.5 | 416 | 26.8 |
| Married or living with partner | 1975 | 60.6 | 448 | 38.7 |
| Widowed/ divorced/ separated | 794 | 20.9 | 391 | 34.4 |
| Household size, mean ± SE | 4.6 ± 0.1 | 4.8 ± 0.1 | ||
| Health insurance status | ||||
| Not insured | 1066 | 23.9 | 106 | 9.4 |
| Insured with public insurance | 1510 | 36.7 | 1145 | 81.1 |
| Insured with private insurance | 1199 | 39.4 | 106 | 9.5 |
| Poverty income ratio | ||||
| 0% to 25% FPL | 988 | 25.1 | 268 | 18.2 |
| 25% to 50% FPL | 428 | 8.7 | 328 | 21.6 |
| 50% to 75% FPL | 632 | 15.0 | 396 | 29.1 |
| 75% to 100% FPL | 762 | 19.3 | 214 | 15.8 |
| 100% to 130% FPL | 1021 | 31.8 | 156 | 15.3 |
| Household food security | ||||
| Full food security | 2439 | 68.7 | 572 | 40.0 |
| Marginal food security | 422 | 8.5 | 199 | 13.5 |
| Low food security | 652 | 15.1 | 376 | 29.1 |
| Very low food security | 313 | 7.7 | 215 | 17.5 |
| Current school breakfast participation | ||||
| Consumed school breakfast 0-2 times in past week | 1298 | 31.9 | 395 | 26.7 |
| Consumed school breakfast 3-5 times in past week | 1176 | 27.1 | 673 | 48.3 |
| Current school lunch Participation | ||||
| Consumed school lunch 0-2 times in past week | 574 | 13.4 | 157 | 12.4 |
| Consumed school lunch 3-5 times in past week | 2253 | 55.8 | 975 | 67.5 |
| Current household WIC participation | 84 | 2.2 | 53 | 4.7 |
All differences in sociodemographic characteristics between SNAP participants and nonparticipants were statistically significant (P < .05), except for gender and HR birthplace. WIC, Special Supplemental Nutrition Program for Women, Infants and Children.
Among SNAP participants, 18.7% were overweight, and 17.5% were obese (Table 2). After multivariate adjustment, there was no association with SNAP participation and childhood overweight (odds ratio [OR] = 0.95, 95% confidence interval: CI 0.69–1.30) or obesity (OR = 1.11, 95% CI: 0.71–1.74), compared with low-income nonparticipants. Within age, gender, and food security subgroups, SNAP participants and nonparticipants had similar high rates of childhood overweight and obesity; no significant associations were observed after multivariate adjustment (Supplemental Table 8).
TABLE 2.
Participation in SNAP and Associations With Weight Status for Children ≤130% FPL
| SNAP Nonparticipants | SNAP Participants | Age- and Gender-Adjusted | Multivariate-Adjusteda | |||
|---|---|---|---|---|---|---|
| n (%) | n (%) | OR | 95% CI | OR | 95% CI | |
| Normal wt | 2318 (63.4) | 818 (63.8) | Ref | Ref | ||
| Overweight | 813 (21.6) | 270 (18.7) | 0.94 | 0.70–1.28 | 0.95 | 0.69–1.30 |
| Obese | 649 (14.9) | 254 (17.5) | 1.31 | 0.91–1.89 | 1.11 | 0.71–1.74 |
Model adjusted for age, gender, race/ethnicity, HR place of birth, HR education level, HR marital status, household size, health insurance, poverty income ratio, household food security, and participation in other food assistance programs.
Both groups of children were far from meeting national dietary recommendations for fruits, vegetables, whole grains, fish and shellfish, and nuts, seeds, and legumes (Table 3). Mean consumption of fruits, vegetables, and whole grains, was ≤1 serving/day. Mean fish and shellfish consumption was ≤0.5 servings/week. Mean consumption of nuts, seeds and legumes ranged from 1.5 to 2.4 servings/week. In comparison, both groups of children exceeded recommended limits for refined grains, processed meat, high-fat dairy products (eg, milk, cheese, yogurt, ice cream), and sugar-sweetened beverages (SSBs). Mean consumption of refined grains was between 5.6 and 5.7 servings/day. Mean consumption of processed meat ranged from 2.6 to 2.8 servings per week. Mean consumption of high-fat dairy products was between 1.3 and 1.4 servings per day. For SSBs, mean consumption ranged from 2.3 to 2.5 servings per day.
TABLE 3.
Consumption of Selected Foods, Food Groups, and Nutrients Among Children ≤130% FPL by SNAP Participation Status
| SNAP Participation | Mean | Median | (10th, 90th) | % Meeting Guideline | Relative Differencea | ||
|---|---|---|---|---|---|---|---|
| Coef | 95% CI | ||||||
| Foods and food groups | |||||||
| Whole grains, servings/d | Nonparticipants | 0.6 | 0.4 | (0.1, 1.5) | 1 | Ref | |
| Participants | 0.5 | 0.3 | (0, 1.2) | 1 | 0.89 | 0.59–1.33 | |
| Refined grains, servings/d | Nonparticipants | 5.7 | 5.5 | (3.7, 7.7) | 97 | Ref | |
| Participants | 5.6 | 5.4 | (3.6, 7.7) | 96 | 1.05 | 0.95–1.16 | |
| Fruits, servings/d | Nonparticipants | 1 | 0.8 | (0.2, 2.1) | 10 | Ref | |
| Participants | 0.8 | 0.6 | (0.1, 1.9) | 7 | 0.98 | 0.64–1.49 | |
| 100% fruit juice, servings/d | Nonparticipants | 1.2 | 0.9 | (0.2, 2.7) | — | Ref | |
| Participants | 1.1 | 0.8 | (0.2, 2.5) | — | 1.04 | 0.68–1.59 | |
| Vegetables, servings/d | Nonparticipants | 0.7 | 0.6 | (0.2, 1.3) | 0 | Ref | |
| Participants | 0.7 | 0.6 | (0.2, 1.3) | 0 | 1.40 | 0.78–2.52 | |
| Potatoes, servings/wk | Nonparticipants | 3.6 | 3.4 | (1.7, 5.7) | — | Ref | |
| Participants | 3.4 | 3.2 | (1.5, 5.5) | — | 0.98 | 0.69–1.38 | |
| Fish/shellfish, servings/wk | Nonparticipants | 0.5 | 0.5 | (0.2, 0.8) | 0 | Ref | |
| Participants | 0.4 | 0.3 | (0.2, 0.6) | 0 | 1.00 | 0.81–1.22 | |
| Nuts, seeds, legumes, servings/wk | Nonparticipants | 2.1 | 1.2 | (0.2, 5.0) | 13 | Ref | |
| Participants | 1.4 | 0.8 | (0.1, 3.4) | 7 | 0.81* | 0.65–1.00 | |
| Processed meat, servings/wk | Nonparticipants | 2.4 | 2.3 | (0.9, 4.9) | 44 | Ref | |
| Participants | 2.8 | 2.5 | (0.9, 5.1) | 40 | 1.44* | 1.09–1.91 | |
| High-fat dairy products, servings/d | Nonparticipants | 1.3 | 1.1 | (0.3, 2.4) | — | Ref | |
| Participants | 1.4 | 1.2 | (0.4, 2.5) | — | 1.47* | 1.07–2.01 | |
| Flavored milk, servings/d | Nonparticipants | 0.4 | 0.2 | (0, 1.0) | — | Ref | |
| Participants | 0.4 | 0.3 | (0, 1.1) | — | 1.08 | 0.82–1.41 | |
| Sweets and bakery desserts, servings/d | Nonparticipants | 1.4 | 1.3 | (0.6, 2.3) | 3 | Ref | |
| Participants | 1.4 | 1.3 | (0.6, 2.4) | 3 | 1.03 | 0.78–1.35 | |
| Salty snacks, servings/d | Nonparticipants | 0.5 | 0.4 | (0.1, 0.9) | — | Ref | |
| Participants | 0.5 | 0.5 | (0.2, 1.0) | — | 1.30 | 0.94–1.82 | |
| Sugar-sweetened beverages, servings/d | Nonparticipants | 2.5 | 2.1 | (0.7, 4.6) | 8 | Ref | |
| Participants | 2.3 | 2.0 | (0.7, 4.3) | 7 | 1.43* | 1.08–1.89 | |
| Water, servings/d | Nonparticipants | 1 | 0.1 | (0, 3.2) | — | Ref | |
| Participants | 1.5 | 0.3 | (0, 4.4) | — | 3.94* | 2.27–6.84 | |
| Nutrients | |||||||
| Total energy, kcal/d | Nonparticipants | 1571 | 1350 | (541, 2866) | — | Ref | |
| Participants | 1714 | 1487 | (610, 3098) | — | 0.99 | 0.93–1.04 | |
| EPA+DHA, g/d | Nonparticipants | 0.04 | 0.04 | (0.02, 0.07) | 0 | Ref | |
| Participants | 0.03 | 0.03 | (0.01, 0.05) | 0 | 1.24 | 0.94–1.63 | |
| ALA, g/d | Nonparticipants | 1.3 | 1.3 | (0.8, 1.9) | 48 | Ref | |
| Participants | 1.2 | 1.2 | (0.7, 1.8) | 49 | 1.01 | 0.94–1.07 | |
| MUFA, % energy | Nonparticipants | 12.1 | 12.1 | (9.9, 14.3) | — | Ref | |
| Participants | 12.2 | 12.2 | (10.1, 14.4) | — | 1.00. | 0.95–1.05 | |
| PUFA, % energy | Nonparticipants | 6.1 | 6 | (4.8, 7.4) | — | Ref | |
| Participants | 6.1 | 6 | (4.8, 7.4) | — | 1.01 | 0.96–1.06 | |
| Saturated fat, % energy | Nonparticipants | 11.4 | 11.4 | (9.5, 13.3) | 0 | Ref | |
| Participants | 11.9 | 11.9 | (10.0, 13.9) | 0 | 1.02 | 0.97–1.08 | |
| Dietary cholesterol, mg/d | Nonparticipants | 233 | 222 | (140, 340) | 81 | Ref | |
| Participants | 219 | 208 | (130, 320) | 86 | 1.01 | 0.94–1.09 | |
| Total fat, % energy | Nonparticipants | 32.3 | 32.3 | (27.4, 37.2) | 73 | Ref | |
| Participants | 32.9 | 32.9 | (28.0, 37.8) | 69 | 1.01 | 0.97–1.06 | |
| Carbohydrates, % energy | Nonparticipants | 55.6 | 55.6 | (49.7, 61.5) | 97 | Ref | |
| Participants | 55.5 | 55.5 | (49.6, 61.4) | 97 | 1.00 | 0.98–1.03 | |
| Protein, % energy | Nonparticipants | 13.1 | 13 | (10.7, 15.7) | 95 | Ref | |
| Participants | 12.7 | 12.6 | (10.3, 15.3) | 93 | 1.00 | 0.96–1.03 | |
| Folate, mg/d | Nonparticipants | 382 | 364 | (233, 552) | 80 | Ref | |
| Participants | 381 | 364 | (232, 551) | 82 | 1.08* | 1.00–1.17 | |
| Dietary fiber, g/d | Nonparticipants | 13.4 | 12.9 | (8.5, 18.9) | 0 | Ref | |
| Participants | 12.7 | 12.2 | (8.0, 18.0) | 0 | 1.04 | 0.97–1.11 | |
| Sodium, mg/d | Nonparticipants | 3268 | 3150 | (2094, 4582) | 15 | Ref | |
| Participants | 3131 | 3021 | (1996, 4402) | 18 | 1.00 | 0.95–1.05 | |
| Potassium, mg/d | Nonparticipants | 2346 | 2268 | (1492, 3294) | 2 | Ref | |
| Participants | 2187 | 2115 | (1375, 3089) | 1 | 0.99 | 0.95–1.04 | |
| Calcium, mg/d | Nonparticipants | 946 | 905 | (552, 1388) | 42 | Ref | |
| Participants | 955 | 916 | (559, 1399) | 45 | 1.08* | 1.02–1.14 | |
| Iron, mg/d | Nonparticipants | 15 | 14.4 | (9.6, 21.1) | 86 | Ref | |
| Participants | 14.8 | 14.2 | (9.5, 20.9) | 99 | 1.07* | 1.01–1.13 | |
ALA, alpha-linolenic acid; Coef, coefficient; DHA, docosahexaenoic acid; EPA, eicosapentaenoic acid; MUFA, monounsaturated fatty acid; PUFA, monounsaturated fatty acid; Ref, reference; —, no available guideline for this food or nutrient.
Models adjusted for age, gender, race/ethnicity, HR place of birth, HR education level, HR marital status, household size, health insurance, poverty income ratio, household food security, participation in other food assistance programs, and total energy.
P < .05.
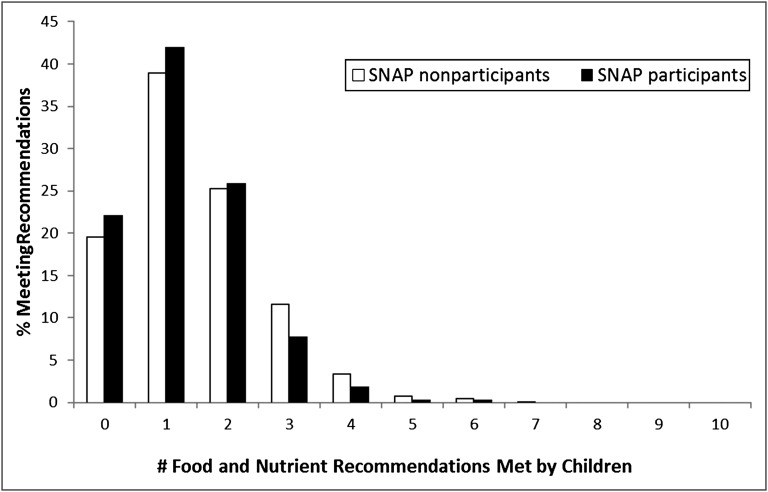
Figure 1 shows the percentage of low-income children meeting 10 selected food and nutrient recommendations with their daily dietary intake: whole grains, fruits, vegetables, fish/shellfish, nuts/seeds/legumes, processed meats, SSBs, saturated fat, sodium, and potassium. Approximately 22% of SNAP participants and 20% of nonparticipants met none of the dietary recommendations. Zero percent of low-income children, regardless of SNAP participation, met at least 7 national dietary recommendations.
FIGURE 1.
Percentage of low-income children meeting 10 food and nutrient guidelines for whole grains, fruits, vegetables, fish/shellfish, nuts/seeds/legumes, processed meats, SSBs, saturated fat, sodium, and potassium.
Several relative differences became greater after adjustment for age, gender, and other covariates. SNAP participants consumed 19% fewer servings of nuts, seeds, and legumes than nonparticipants (relative difference [RD] = 0.81, 95% CI: 0.65–1.00). SNAP participants also consumed 44% more servings of processed meats (RD = 1.44, 95% CI: 1.09–1.91), 47% more servings of high-fat dairy products (RD = 1.47, 95% CI: 1.07–2.01), 43% more servings of SSBs (RD = 1.43, 95% CI: 1.08–1.89), and nearly 4 times as much water (RD = 3.94, 95% CI: 2.27–6.84) than nonparticipants after multivariate adjustment. No significant differences in whole grains, fruits, vegetables, or fish and shellfish were observed between groups.
There were no differences in total energy or macronutrient intake between SNAP participants and nonparticipants. Although mean sodium intake was high (ranging from 3131 to 3268 mg/day) and mean potassium intake was low (ranging from 2187 to 2346 mg/day), there were no differences in sodium and potassium intake by SNAP participation. Mean calcium intake ranged from 946 to 955 mg/day. Most low-income children met the Estimated Average Requirement for folate and iron. After multivariate adjustment, SNAP participants had 8% higher folate intake (RD = 1.08, 95% CI 1.00–1.17), 8% higher calcium intake (RD = 1.08, 95% CI 1.02–1.14), and 7% higher iron intake (RD = 1.07, 95% CI 1.01–1.13) than nonparticipants.
In subgroup analyses by gender, age group, and food security status, similar levels of foods, food groups, and nutrients were consumed (Supplemental Tables 9, 10, and 11). However, girl SNAP participants had higher vegetable consumption (RD = 1.98, 95% CI: 1.08–3.62) compared with girl nonparticipants. Children in food-insecure households receiving SNAP reported higher consumption of refined grains (RD = 1.17, 95% CI: 1.02–1.34) than food-insecure nonparticipants. Boys participating in SNAP also had higher intake of saturated fat (RD = 1.06, 95% CI: 1.01–1.12), compared with boy nonparticipants.
For the HEI-2005, SNAP participants and nonparticipants scored 45.6 and 47.2, respectively, out of a maximum 100 points (Table 4). Among both groups, the lowest scores were dark green vegetables, orange vegetables and legumes, and whole grains. The highest scores were meat and beans, milk, saturated fat, and total grains. After adjusting for covariates, SNAP participants had a 97% higher whole grains score than nonparticipants (RD = 1.97, 95% CI: 1.13–3.44) and a 17% higher milk score (RD = 1.17, 95% CI: 1.04–1.31) compared with nonparticipants. There was no difference in the total HEI-2005 score after multivariate adjustment (RD = 1.00, 95% CI: 0.96–1.04).
TABLE 4.
Participation in SNAP and Children’s Dietary Quality as Measured by the HEI-2005
| Component | Standards for Maximum Score | Maximum Score | SNAP Participation | Mean ± SD | % of Maximum Score | Relative Differencea | |
|---|---|---|---|---|---|---|---|
| Coef | 95% CI | ||||||
| Total fruit | ≥ 0.8 cup per 1000 kcal | 5 | Nonparticipants | 2.2 ± 0.1 | 44 | Ref | |
| Participants | 2.1 ± 0.1 | 42 | 1.50 | 0.94–2.39 | |||
| Whole fruit | ≥ 0.4 cup per 1000 kcal | 5 | Nonparticipants | 1.7 ± 0.1 | 34 | Ref | |
| Participants | 1.4 ± 0.1 | 28 | 1.01 | 0.53–1.92 | |||
| Total vegetables | ≥ 1.1 cup per 1000 kcal | 5 | Nonparticipants | 2.2 ± 0.0 | 44 | Ref | |
| Participants | 1.9 ± 0.1 | 38 | 0.93 | 0.76–1.13 | |||
| Dark green and orange vegetables and legumes | ≥ 0.4 cup per 1000 kcal | 5 | Nonparticipants | 0.7 ± 0.0 | 14 | Ref | |
| Participants | 0.6 ± 0.1 | 12 | 1.05 | 0.59–1.88 | |||
| Total grains | ≥ 3.0 oz per 1000 kcal | 5 | Nonparticipants | 4.6 ± 0.0 | 92 | Ref | |
| Participants | 4.5 ± 0.1 | 90 | 0.98 | 0.95–1.02 | |||
| Whole grains | ≥ 1.5 oz per 1000 kcal | 5 | Nonparticipants | 0.7 ± 0.0 | 14 | Ref | |
| Participants | 0.7 ± 0.1 | 14 | 1.97* | 1.13–3.44 | |||
| Milk | ≥ 1.3 cup per 1000 kcal | 10 | Nonparticipants | 6.1 ± 0.1 | 61 | Ref | |
| Participants | 6.3 ± 0.2 | 63 | 1.17* | 1.04–1.31 | |||
| Meat and beans | ≥ 2.5 oz per 1000 kcal | 10 | Nonparticipants | 6.8 ± 0.1 | 68 | Ref | |
| Participants | 6.6 ± 0.1 | 66 | 1.01 | 0.89–1.14 | |||
| Oils | ≥ 12 g per 1000 kcal | 10 | Nonparticipants | 4.9 ± 0.1 | 49 | Ref | |
| Participants | 4.9 ± 0.2 | 49 | 1.01 | 0.86–1.19 | |||
| Saturated fat | ≤ 7% energy | 10 | Nonparticipants | 6.5 ± 0.1 | 65 | Ref | |
| Participants | 5.9 ± 0.2 | 59 | 1.07 | 0.74–1.55 | |||
| Sodium | ≤ 0.7 g per 1000 kcal | 10 | Nonparticipants | 4.7 ± 0.1 | 47 | Ref | |
| Participants | 4.5 ± 0.1 | 45 | 0.90 | 0.24–3.34 | |||
| Calories from SOFAAS | ≤ 20% energy | 20 | Nonparticipants | 9.3 ± 0.2 | 47 | Ref | |
| Participants | 9.1 ± 0.3 | 46 | 1.27 | 0.92–1.77 | |||
| Total score | 100 | Nonparticipants | 47.2 ± 0.5 | 47 | Ref | ||
| Participants | 45.6 ± 0.6 | 46 | 1.00 | 0.96–1.04 | |||
Food or nutrient guideline is the recommended maximum. Coef, coefficient; Ref, reference; SOFAAS, solid fats, alcohol, and added sugars.
Models adjusted for age, gender, race/ethnicity, HR place of birth, HR education level, HR marital status, household size, health insurance, poverty income ratio, household food security, and participation in other food assistance programs.
P < .05.
The total AHEI scores for SNAP participants and nonparticipant were 21.0 and 23.2, respectively, out of a maximum of 87.5 points (Table 5). Both groups had low scores for vegetables, fruits, and nuts and soy protein. Compared with nonparticipants, SNAP participants had an 18% lower score for nuts and soy protein (RD = 0.82, 95% CI: 0.67–1.00), after adjusting for covariates. There was no significant multivariate-adjusted difference in the overall AHEI score between SNAP participants and nonparticipants (RD = 0.96, 95% CI: 0.91–1.01).
TABLE 5.
Participation in SNAP and Children’s Dietary Quality as Measured by a Modified AHEI
| Component | Standards for Maximum Score | Maximum Score | SNAP Participation | Mean ± SE | % of Maximum Score | RDa | |
|---|---|---|---|---|---|---|---|
| Coef | 95% CI | ||||||
| Vegetables (excluding potatoes) | 5 servings/d | 10 | Nonparticipants | 1.3 ± 0.1 | 13 | ||
| Participants | 1.3 ± 0.1 | 13 | 1.40 | 0.78–2.52 | |||
| Fruits | 4 servings/d | 10 | Nonparticipants | 1.8 ± 0.1 | 18 | ||
| Participants | 1.5 ± 0.1 | 15 | 0.96 | 0.64–1.46 | |||
| Nuts and soy protein | 1 serving/d | 10 | Nonparticipants | 1.2 ± 0.1 | 12 | ||
| Participants | 0.7 ± 0.1 | 7 | 0.82* | 0.67–1.00 | |||
| Ratio of white to red meat | 4:01 | 10 | Nonparticipants | 2.5 ± 0.1 | 25 | ||
| Participants | 2.2 ± 0.1 | 22 | 1.11 | 0.81–1.52 | |||
| Cereal fiber | 15 g/d | 10 | Nonparticipants | 2.4 ± 0.1 | 24 | ||
| Participants | 2.3 ± 0.1 | 23 | 1.20 | 0.88–1.63 | |||
| Ratio of polyunsaturated to saturated fat | 1:01 | 10 | Nonparticipants | 5.7 ± 0.1 | 57 | ||
| Participants | 5.4 ± 0.1 | 54 | 0.99 | 0.95–1.05 | |||
| Multivitamin use | Any use in past 30 d | 7.5 | Nonparticipants | 3.4 ± 0.1 | 45 | ||
| Participants | 3.0 ± 0.1 | 40 | 0.93* | 0.87–0.99 | |||
| Total score (rescaled to original) | 87.5 | Nonparticipants | 23.2 ± 0.4 | 27 | |||
| Participants | 21.0 ± 0.5 | 24 | 0.96 | 0.91–1.01 | |||
Models adjusted for age, gender, race/ethnicity, HR place of birth, HR education level, HR marital status, household size, health insurance, poverty income ratio, household food security, total energy intake, and participation in other food assistance programs.
P < .05.
Discussion
The prevalence of childhood obesity has increased in recent decades.39 In this national sample of low-income children, more than one-third of low-income children were overweight or obese; however, SNAP participation was not associated with higher rates of overweight or obesity after multivariate adjustment. These findings corroborate the results of a USDA review of SNAP participation and obesity in children,40 although evidence increasingly suggests an association between SNAP participation and obesity in adult women.40,41
All low-income children in the study consumed fewer servings of fruits, vegetables, whole grains, fish and shellfish, nuts, seeds and legumes, dietary fiber, and potassium, and more servings of refined grains, processed meat, high-fat dairy, SSBs, saturated fat, and sodium when compared with national recommendations. As shown in previous studies, the dietary intake of low-income children falls far short of national recommendations, with ∼1 in 5 low-income children not meeting any of the dietary recommendations.42–44 Although there was no difference by SNAP participation, all low-income children had low scores for both dietary quality measures. Mean HEI scores were between the 40th and 50th percentiles of the general population, and mean AHEI scores were within the lowest quintile of dietary quality from the original AHEI report; low AHEI scores have predicted greater risks of chronic disease among adults.31–33,45 These findings underscore the need to develop policies and educational programs to encourage healthier food choices among low-income children and families.
Although the diets of low-income SNAP participants and nonparticipants were similar in terms of total energy and macronutrients, there were some differences after multivariate adjustment. The nutritional intake of SNAP participants appeared better in some ways: more water, folate, calcium, and iron. In other ways, their food intake was worse: fewer nuts, seeds, and legumes and more processed meats, high-fat dairy products, and SSBs than nonparticipants. Ironically, the higher intakes of foods not generally regarded as healthy (eg, refined grains, processed meats, high-fat dairy) may have contributed to the higher intakes of folate, iron, and calcium in SNAP participants. The lack of major differences between groups could have resulted from a modest nutritional benefit with the program among SNAP recipients combined with a diet that would have been worse without the program. However, SNAP participation did not raise the nutritional quality of children’s diets to anywhere close to national recommendations.
The high intake of SSBs by low-income children deserves attention for its implications for the Farm Bill reauthorization. It was estimated that as much as $4 billion of SNAP benefits in 2011 were used to purchase soft drinks by program participants.46 In an effort to improve the diets of SNAP participants, New York City recently requested a waiver to restrict SSB purchases with SNAP benefits. Although the USDA denied its request, public health advocates have supported similar policies to improve dietary quality for SNAP participants and have urged policymakers to align SNAP with the Dietary Guidelines for Americans.9,47,48
This study also found that SNAP participants had high intakes of beverages (eg, SSBs, high-fat dairy, water), compared with nonparticipants. Coupled with lower household food security, increasing water consumption, and possibly beverages in general, might have been used not only to address thirst but as a coping strategy for experiences of food insecurity by SNAP participants.49
This study has limitations. One is the cross-sectional nature of the data, which makes it difficult to determine temporality. Variables like household food security may predict SNAP participation or mediate its association with obesity and dietary quality. The results did not change when household food security was excluded from multivariate models; thus, it was retained as a covariate because bivariate analyses showed significant differences in household food security by SNAP participation. Measurement error is always a problem with dietary intake; however, 24-hour recalls to assess children’s diets have been validated for energy intake using doubly labeled water in other studies.50,51 Information on external influences would also enhance knowledge of how the larger environment affects the use of SNAP benefits and dietary intake.52
This study could not control for “self-selection bias” or other unmeasured differences between SNAP participants and nonparticipants. Although some variables related to self-selection were accounted for (eg, household food security, participation in other food assistance programs), there may be other unmeasured characteristics, such as access to healthier foods. We cannot determine the extent that these differences may be explained by SNAP participation. Another limitation is the low SNAP participation rate in NHANES. This may be due to lower NHANES response rates among SNAP households, misreporting of SNAP participation, which may be related to gender, marital status, or income, or other household eligibility criteria not captured by NHANES.4,53,54
Conclusions
The name change to the Supplemental Nutrition Assistance Program in 2008 and the SNAP Nutrition Education and Obesity Prevention Grant Program for nutrition education in 2010 indicate a growing emphasis on promoting improved food choices in SNAP.6,55 This study highlights the poor dietary quality of low-income children compared with national recommendations for foods and nutrients. Importantly, it suggests possible differences in dietary intake between SNAP participants and low-income nonparticipants with respect to specific foods (eg, more SSBs, high-fat dairy products, processed meats, and fewer nuts, seeds, and legumes), which may have, in part, contributed to higher intakes of micronutrients (eg, calcium, iron, folate), despite no differences in overall dietary quality scores.
SNAP has the potential to influence the diets of 45 million participants, 47% of whom are children, by providing additional resources to purchase food.13 The low intake of nutritious food among children participating in SNAP represents a significant missed opportunity for the program to promote health during an important life stage. Policy changes should be considered to restructure SNAP as a program that goes beyond alleviating food insecurity by increasing the availability, marketing, and desirability of healthier foods that better support the use of SNAP benefits for nutritious foods to improve children’s health.56
Supplementary Material
Glossary
- AHEI
Alternate Healthy Eating Index
- CI
confidence interval
- FPL
federal poverty level
- HEI
Healthy Eating Index
- HR
household reference person
- OR
odds ratio
- RD
relative difference
- SNAP
Supplemental Nutrition Assistance Program
- SSBs
sugar-sweetened beverages
- USDA
US Department of Agriculture
Footnotes
FINANCIAL DISCLOSURE: Dr Mozaffarian received payment from Bunge for the development of educational presentations, and ad hoc travel reimbursement and/or honoraria for one-time scientific presentation on diet and cardiometabolic disease; the other authors have indicated they have no financial relationships relevant to this article to disclose. Ms Foerster has participated in this research using personal time. Her salary is paid, in part, from USDA SNAP-Ed funds through the State of California.
FUNDING: This article was commissioned by the Robert Wood Johnson Foundation through its Healthy Eating Research program. Additional support was provided by the Aetna Foundation. Dr Leung was supported by a National Institutes of Health (NIH) training grant 5 T32 CA009001-35. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the Robert Wood Johnson Foundation, the Aetna Foundation, or the NIH. Funded by the National Institutes of Health (NIH).
References
- 1.From Food Stamps to the Supplemental Nutrition Assistance Program. Legislative timeline. Available at: www.fns.usda.gov/snap/rules/Legislation/timeline.pdf. Accessed July 23, 2012
- 2.Monthly data SNAP. Available at: www.fns.usda.gov/pd/34SNAPmonthly.htm. 2012. Accessed March 9, 2012
- 3.Current participation SNAP. Available at: www.fns.usda.gov/pd/30SNAPcurrHH.htm. Accessed March 9, 2012
- 4.Eligibility. Supplemental Nutrition Assistance Program. www.fns.usda.gov/snap/applicant_recipients/eligibility.htm. 2011. Accessed October 13, 2011
- 5.FY 2011 Income Eligibility Standards. Available at: www.fns.usda.gov/snap/government/FY11_Income_Standards.htm. 2011. Accessed October 12, 2011
- 6.Name change SNAP. Available at: www.fns.usda.gov/snap/outreach/pdfs/toolkit/2011/Community/Basics/SNAP_name.pdf. Accessed August 25, 2011
- 7.Ogden CL, Carroll MD, Kit BK, Flegal K. Prevalence of obesity in the United States, 2009–2010. Hyattsville, MD: National Center for Health Statistics; 2012 [Google Scholar]
- 8.Nutrition Assistance Programs. Available at: www.fns.usda.gov/fns. 2011. Accessed October 13, 2011
- 9.Brownell KD, Ludwig DS. The Supplemental Nutrition Assistance Program, soda, and USDA policy: who benefits? JAMA. 2011;306(12):1370–1371 [DOI] [PubMed] [Google Scholar]
- 10.Wilde PE, McNamara PE, Ranney CK. The effect on dietary quality of participation in the Food Stamp and WIC programs. Washington, DC: Economic Research Service, US Department of Agriculture; 2000 [Google Scholar]
- 11.Cole N, Fox MK. Diet quality of Americans by Food Stamp participation status: data from the National Health and Nutrition Examination Surveys, 1999–2004. Alexandria, VA: Food and Nutrition Service, US Department of Agriculture; 2008 [Google Scholar]
- 12.Tiehen L, Ver Ploeg M. SNAP Benefits Alleviate the Incidence and Intensity of Poverty. Washington, DC: Economic Research Service, US Department of Agriculture; 2012 [Google Scholar]
- 13.Eslami E, Filion K, Strayer M. Characteristics of Supplemental Nutrition Assistance Program Households: Fiscal Year 2010. Alexandria, VA: Office of Research and Analysis, Food and Nutrition Service, U.S. Department of Agriculture; 2011 [Google Scholar]
- 14.Cason KL, Cox RH, Burney JL, Poole KP, Wenrich TR. Do food stamps without education improve the nutrient intake of recipients? Topics Clin Nutr. 2002;17(4):74–82 [Google Scholar]
- 15.Hampl JS, Sass S. Focus groups indicate that vegetable and fruit consumption by food stamp-eligible Hispanics is affected by children and unfamiliarity with non-traditional foods. J Am Diet Assoc. 2001;101(6):685–687 [DOI] [PubMed] [Google Scholar]
- 16.Wiig K, Smith C. The art of grocery shopping on a food stamp budget: factors influencing the food choices of low-income women as they try to make ends meet. Public Health Nutr. 2009;12(10):1726–1734 [DOI] [PubMed] [Google Scholar]
- 17.Biro FM, Wien M. Childhood obesity and adult morbidities. Am J Clin Nutr. 2010;91(5):1499S–1505S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patrick H, Nicklas TA. A review of family and social determinants of children’s eating patterns and diet quality. J Am Coll Nutr. 2005;24(2):83–92 [DOI] [PubMed] [Google Scholar]
- 19.Tercyak KP, Tyc VL. Opportunities and challenges in the prevention and control of cancer and other chronic diseases: children’s diet and nutrition and weight and physical activity. J Pediatr Psychol. 2006;31(8):750–763 [DOI] [PubMed] [Google Scholar]
- 20.Sharma AJ, Grummer-Strawn LM, Dalenius K, et al. Obesity prevalence among low-income, preschool-aged children—United States, 1998–2008. Report No. 28. Atlanta, GA: Centers for Disease Control and Prevention; 2009
- 21.Anthropometry Procedures Manual. Atlanta, GA: Centers for Disease Control and Prevention; 2004 [Google Scholar]
- 22.Vidmar S, Carlin J, Hesketh K, Cole TJ. Standardizing anthropometric measures in children and adolescents with new functions for egen. Stata J. 2004;4(1):50–55 [Google Scholar]
- 23.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320(7244):1240–1243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.About BMI for Adults. Healthy weight. 2009. Available at: www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html. Accessed August 25, 2011
- 25.MEC In-person dietary interviews procedure manual. Atlanta, GA: Centers for Disease Control and Prevention; 2002
- 26.Lloyd-Jones D, Adams RJ, Brown TM, et al. Heart disease and stroke statistics—2010 update: a report from the American Heart Association. Circulation. 2011;121(7):e46–e215 [DOI] [PubMed] [Google Scholar]
- 27.Gidding SS, Dennison BA, Birch LL, et al. American Heart Association. American Academy of Pediatrics . Dietary recommendations for children and adolescents: a guide for practitioners: consensus statement from the American Heart Association. Circulation. 2005;112(13):2061–2075 [DOI] [PubMed] [Google Scholar]
- 28.2010. The USDA Food and Nutrient Database for Dietary Studies, 4.1—documentation and user guide [published correction appears in Circulation. 2006;113(23)e857. Available at: www.ars.usda.gov/SP2UserFiles/Place/12355000/pdf/fndds/fndds4_doc.pdf#formats. Accessed October 8, 2011
- 29.Dietary Guidelines for Americans, 2010. Washington, DC: US Department of Agriculture and U.S. Department of Health and Human Services; 2010 [Google Scholar]
- 30.Otten JJ, Hellwig JP, Meyers DW. Dietary Reference Intakes: The Essential Guide to Nutrient Requirements. Washington, DC: Food and Nutrition Board, Institute of Medicine; 2006 [Google Scholar]
- 31.Guenther PM, Reedy J, Krebs-Smith SM, Reeve BB, Basiotis PP. Development and Evaluation of the Healthy Eating Index—2005. Washington, DC: Center for Nutrition Policy and Promotion, US Department of Agriculture; 2007 [Google Scholar]
- 32.Fung TT, McCullough ML, Newby PK, et al. Diet-quality scores and plasma concentrations of markers of inflammation and endothelial dysfunction. Am J Clin Nutr. 2005;82(1):163–173 [DOI] [PubMed] [Google Scholar]
- 33.McCullough ML, Feskanich D, Stampfer MJ, et al. Diet quality and major chronic disease risk in men and women: moving toward improved dietary guidance. Am J Clin Nutr. 2002;76(6):1261–1271 [DOI] [PubMed] [Google Scholar]
- 34.Radimer K, Bindewald B, Hughes J, Ervin B, Swanson C, Picciano MF. Dietary supplement use by US adults: data from the National Health and Nutrition Examination Survey, 1999–2000. Am J Epidemiol. 2004;160(4):339–349 [DOI] [PubMed] [Google Scholar]
- 35.Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to Measuring Household Food Security. Washington, DC: Food and Nutrition Service, US Department of Agriculture; 2000 [Google Scholar]
- 36.Usual Dietary Intakes. The NCI method. Available at: http://riskfactor.cancer.gov/diet/usualintakes/method.html. 2011. Accessed February 14, 2012
- 37.Moshfegh A, Goldman J, Ahuja J, Rhodes D, LaComb R. What We Eat in America, NHANES 2005–2006: Usual Nutrient Intakes From Food and Water Compared to 1997 Dietary Reference Intakes for Vitamin D, Calcium, Phosphorus, and Magnesium. Washington, DC: Agricultural Research Service, US Department of Agriculture; 2009 [Google Scholar]
- 38.Usual Dietary Intakes. SAS macros for analysis of a single dietary component. http://riskfactor.cancer.gov/diet/usualintakes/macros_single.html. 2010. Accessed February 14, 2012
- 39.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303(3):242–249 [DOI] [PubMed] [Google Scholar]
- 40.Ver Ploeg M, Ralston K. Food Stamps and Obesity: What Do We Know? EIB-34. Washington, DC: Economic Research Service, US Department of Agriculture; 2008 [Google Scholar]
- 41.DeBono NL, Ross NA, Berrang-Ford L. Does the Food Stamp Program cause obesity? A realist review and a call for place-based research. Health Place. 2012;18(4):747–756 [DOI] [PubMed] [Google Scholar]
- 42.Brady LM, Lindquist CH, Herd SL, Goran MI. Comparison of children’s dietary intake patterns with US dietary guidelines. Br J Nutr. 2000;84(3):361–367 [PubMed] [Google Scholar]
- 43.Nutrition and Weight Status—Healthy People. Healthy People 2010 topics & objectives. Available at: www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=29. 2011. Accessed October 15, 2011
- 44.Devaney B, Kim M, Carriquiry A, Camano-Garcia G. Assessing the nutrient intakes of vulnerable subgroups. Princeton, NJ: Mathematica Policy Research, Inc; 2005
- 45.Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med. 2011;364(25):2392–2404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shenkin JD, Jacobson MF. Using the Food Stamp Program and other methods to promote healthy diets for low-income consumers. Am J Public Health. 2010;100(9):1562–1564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Accelerating Progress in Obesity Prevention Solving the weight of the nation. Washington, DC: Institute of Medicine; 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Barnhill A. Impact and ethics of excluding sweetened beverages from the SNAP program. Am J Public Health. 2011;101(11):2037–2043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lappalainen R, Mennen L, van Weert L, Mykkänen H. Drinking water with a meal: a simple method of coping with feelings of hunger, satiety and desire to eat. Eur J Clin Nutr. 1993;47(11):815–819 [PubMed] [Google Scholar]
- 50.Burrows TL, Martin RJ, Collins CE. A systematic review of the validity of dietary assessment methods in children when compared with the method of doubly labeled water. J Am Diet Assoc. 2010;110(10):1501–1510 [DOI] [PubMed] [Google Scholar]
- 51.Johnson RK, Driscoll P, Goran MI. Comparison of multiple-pass 24-hour recall estimates of energy intake with total energy expenditure determined by the doubly labeled water method in young children. J Am Diet Assoc. 1996;96(11):1140–1144 [DOI] [PubMed] [Google Scholar]
- 52.Simon M. Food Stamps: Follow the Money. Are Corporations Profiting From Hungry Americans? Oakland, CA: Eat Drink Politics; 2012 [Google Scholar]
- 53.Kissmer C. Reaching Those in Need: Supplemental Nutrition Assistance Program Participation Rates in 2007—Summary. Washington, DC: Food and Nutrition Service, US Department of Agriculture; 2009.
- 54.Bollinger CR, David MH. Modeling discrete choice with response error: Food Stamp participation. J Am Stat Assoc. 1997;92(439):827–835 [Google Scholar]
- 55.Healthy Hunger-Free Kids Act of 2010. Children nutrition programs. Available at: www.fns.usda.gov/cnd/governance/legislation/CNR_2010.htm. 2011. Accessed October 15, 2011
- 56.SNAP to Health A Fresh Approach to Improving Nutrition in the Supplemental Nutrition Assistance Program. Washington, DC: Center for the Study of the Presidency and Congress; 2012 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.