Abstract
Up to now, it is still unknown whether microcirculation of deeper peripheral tissue (knee) can be modulated by acupuncture or acupressure on a meridian acupoint. The goal of this pilot study was to investigate possible effects of acupressure at the Xiyangguan acupoint (GB33) on the regional oxygen saturation of the deeper knee tissues by near-infrared spectroscopy (NIRS). Twelve healthy volunteers with a mean age of 23.8 ± 1.6 years were investigated. Acupressure stimulation was performed for 5 minutes at the Xiyangguan acupoint. The results of the controlled study showed a significant increase of the values of regional oxygen saturation on the stimulated side of the knee (P = 0.033), whereas the opposite side on the same knee showed insignificant changes. These results may serve as a valuable basis for monitoring a possible therapeutic effect (e.g., after Khalifa therapy) in patients with knee problems.
1. Introduction
As one of the complementary and alternative treatments (CAMs), acupuncture or acupressure has been utilized to improve health in Asia and Western countries. Although the mechanism of acupuncture remains still unknown in detail, acupuncture stimulation was confirmed to increase the blood flow velocity of the peripheral arterioles [1]. Up to now, studies have shown that the blood circulation of the body surface can be modulated by acupuncture or acupressure [2, 3]. But it is still unknown whether the microcirculation of the deeper peripheral tissue can be modulated by acupuncture or acupressure.
Near-infrared spectroscopy (NIRS) is a spectroscopic method that uses the near-infrared region of the electromagnetic spectrum (from about 800 nm to 2500 nm). Medical applications of NIRS center on the noninvasive measurement of the amount and oxygen content of hemoglobin [4]. The advantage of NIRS is that it can typically penetrate much deeper into a sample than mid-infrared radiation [5].
Acupressure treatment normally uses fingertips, rather than needles, to stimulate acupoints on the skin and has been shown to be a successful treatment for a variety of medical disorders.
The goal of the present pilot study was to investigate possible effects of acupressure at the Xiyangguan acupoint (GB33) on the regional oxygen saturation of the knee tissues at a depth of 2–4 cm, by using NIRS.
2. Materials and Methods
2.1. Healthy Volunteers
Twelve healthy volunteers (5 females, 7 males) with a mean age ± SD of 23.8 ± 1.6 years were investigated at the Medical University of Graz. None of the subjects had any neurological or cardiovascular disorders, and none of them was taking any medication. They were informed about the nature of the investigation and were paid for their participation. The study was approved by the local ethics committee, and all participants provided written informed consent.
2.2. Acupressure
Acupressure stimulation was performed at the Xiyangguan (GB33) acupoint. This point is located on the lateral side of the knee, 3 cun (cun is a relative body measure; 1 cun corresponds to the breadth of the distal phalanx of the thumb) directly proximal to Yanglingquan (GB34), at the depression superior to the lateral epicondyle of the femur, between the femur and the tendon of biceps femoris. Stimulation of Xiyangguan is indicated in cases of swelling and pain in the knee caused by inflammatory processes [6]. To assess the reliability and validity of acupressure, pressure was applied by the same Chinese medical doctor experienced in Traditional Chinese Medicine (TCM). The thumb pressure was steady and estimated to be about 3 × 105 Pa (mean force measured ~ 30 N/cm2), as described in [7].
2.3. Evaluation Parameters
For the measurement of the regional oxygen saturation (rSO2), a two-channel INVOS 5100 Oximeter (Somanetics Corp., Troy, USA) was used. The principle of this system is based on NIRS technology, which is a noninvasive method for measuring regional oxygenation through the intact skin, which has been applied successfully in research and numerous clinical indications for many years [8]. Near-infrared light (730 and 805 nm) is emitted through the skin and after passing different kinds of tissue (muscle and bone) the returned light is detected at two distances from the light source (3 and 4 cm). Based upon this principle, the spectral absorption of blood in deeper structures (2–4 cm) can be determined and defined as rSO2. Before starting the measurement, the skin was cleaned with the enclosed skin-prep pad. Then two sensors were applied below the right and left lateral sides of the patella of the right leg (see Figure 1). To minimize external light influence, the knee was covered with a black cloth during the recording and stimulation procedure. After a resting time of five minutes, the rSO2 data were recorded.
Figure 1.

Measurement site with applied sensors during acupressure stimulation.
2.4. Procedure
The persons were investigated in a supine position. Acupressure started after a 5-minute resting phase. The measurement profile is shown in Figure 2. Three measurement points were evaluated (a, immediately before starting the stimulation; b, 2 min after starting the stimulation; and c, immediately after the end of the 5-minute stimulation period.
Figure 2.
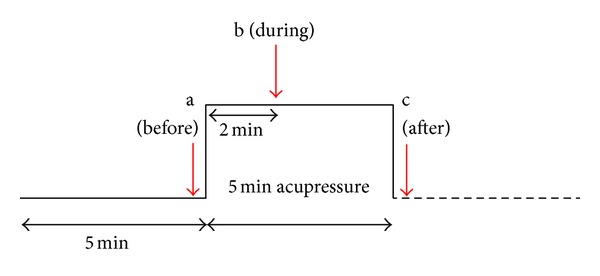
Measurement profile of the volunteer study. The measurement points are indicated (a–c).
The study was performed as a controlled study. The parameter rSO2 was measured at two different locations at the stimulated knee. Location 1 (acupressure side) was in a distance of 2 cm from the acupuncture point Xiyangguan (comp. Figure 1). Location 2 (serving as control) was on the same knee, on the opposite side of the patella. We did not measure the results of other acupuncture points within this study.
2.5. Statistical Analysis
The rSO2 values of both the acupressure and the opposite side were tested with one way repeated measures ANOVA (SigmaPlot 12.0, Systat Software Inc., Chicago, USA). The Holm-Sidak method was used for post-hoc analysis. The level of significance was defined as P < 0.05.
3. Results
All subjects completed the study, and the measurements could be performed without any technical problems. Stimulation was perceived as painless and not discomforting. Figure 3(a) shows the increase of the rSO2 values during and after acupressure being applied to the acupoint Xiyangguan in all 12 healthy volunteers.
Figure 3.
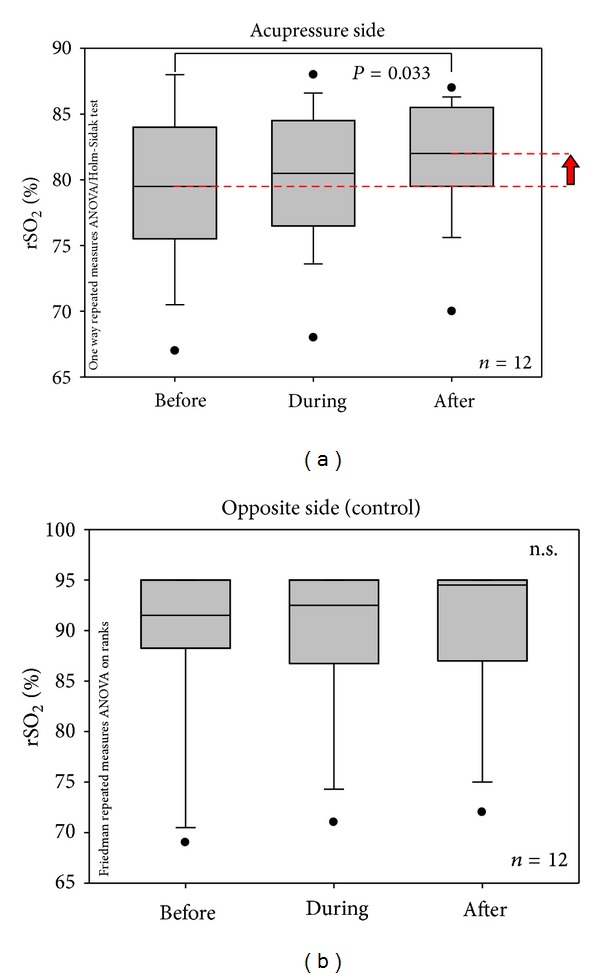
(a) Box plot presentation of changes of regional oxygen saturation values in 12 healthy volunteers before, during, and after acupressure (comp. Figure 2) on the stimulated side (acupressure side). Note the significant increase immediately after the 5-minute acupressure phase; the median of the rSO2 was increased by 2.5% compared to baseline values. The ends of the boxes define the 25th and 75th percentiles with a line at the median, and error bars defining the 10th and 90th percentiles. (b) Box plot presentation of changes of regional oxygen saturation values in 12 healthy volunteers before, during, and after acupressure (comp. Figure 2) on the opposite (control) side. For further explanations, see Figure 3(a).
The values of rSO2 of the opposite side are presented in Figure 3(b). No statistically significant differences were found on this side, although the median was increased during and after acupressure.
4. Discussion
Acupressure is a noninvasive strategy used to manage multiple symptoms in a variety of patient populations [9], including relieving pain [10], managing nausea and vomiting [11], and many other applications.
The acupuncture point Xiyangguan (GB33) is located on the gall bladder meridian. This meridian runs along the lateral aspect of the thigh and knee, going further downward along the anterior border of the fibula. As mentioned in the methods section, GB33 is located lateral to the knee joint. It is a conventional acupoint in the treatment of knee osteoarthritis [12]. In the present study, the oxygen saturation of a healthy knee could be affected by acupressure at GB33 in a depth of 2–4 cm. Our results are in accordance with the meridian theory, which states that firstly, the area along the meridian will be affected by stimulating acupoints on the meridian, and secondly, the function of local tissues can be affected by stimulating nearby acupoints [13].
In recent years, we have investigated the relationship between acupuncture and cerebral microcirculation using NIRS. In three healthy male volunteers, acupuncture at specific acupuncture points led to an increase in oxygenated hemoglobin and in the tissue oxygenation index. However, needling and laser puncture at placebo points did not produce the same effect on cerebral oxygenation [14]. In 16 adult volunteers, a significant decrease was found in oxyhemoglobin after needle insertion and stimulation, accompanied by an increase in deoxyhemoglobin [15]. The results suggest that NIRS technology may be useful in visualizing and quantifying the cerebral vascular effects of acupuncture and acupuncture-like stimulation on microcirculation [16].
The primary application of NIRS to the human body uses the fact that the transmission and absorption of NIR light in human body tissues contains information about hemoglobin concentration changes. NIRS can be used to quantify blood flow, blood volume, oxygen consumption, reoxygenation rates, and muscle recovery time [17]. In comparison with laser Doppler flowmetry (LDF), NIRS can typically penetrate much deeper into a sample. NIRS can penetrate the tissue in a depth of 2–4 cm, whereas LDF can only penetrate the tissue in a depth of about 1–3 mm. NIRS is more sensitive than LDF with regard to detecting changes in tissue inflow [18]. Besides, NIRS systems are usually portable, even wireless instrumentation is available, which enables investigations in freely moving subjects [19]. It has also been suggested as a method for arthroscopic evaluation of low grade degenerated cartilage lesions [20].
To the best of our knowledge, this is the first study which evaluates the effects of acupressure on the regional blood oxygenation of the knee tissues using NIRS.
Studies have investigated the mechanism of acupuncture or acupressure with respect to peripheral microcirculation. The blood flow velocity was found to be increased after continuous digital acupressure. It has also been suggested that cyclic Guanosine Monophosphate (cGMP) mediates the signaling functions of nitric oxide (NO) to improve local microcirculation [21]. A neurovascular transmission model for the acupuncture-induced NO effect has been proposed by Hsiao and Tsai [22]. In this model, the acupuncture stimulus is able to influence connective tissue via mechanical force transfer to the extracellular matrix (ECM). Through the ECM, the mechanotransduction stimulus can be translated or travel from the acupuncture points including local tissue and cells. Cells in the local tissue that have received mechanotransduction induce different types of NO production to induce changes in blood flow and local circulation [22]. By assessing the responses of arteriolar blood flow to acupuncture stimulation in rabbits, it was found that the arteriolar diameter significantly increased to 131% ± 14% in the acupuncture group when compared with the pretreatment value. Blood flow velocity and blood flow rate showed similar trends. The treatment effect remained manifest for 40–50 min after the end of stimulation and irradiation [23].
Our preliminary study has some limitations. We did not measure environmental temperature which could possibly also affect the results, but this is not very probable. It is also possible that the articular cavity can influence the measurement results, and this could also be a reason for the variation among the subjects before the procedure. Moreover, the informative value of our results may be compromised by the fact that already baseline values differ strongly between the acupressure side and the opposite (control) side, being much higher on the opposite side.
Acupressure is a noninvasive therapy, which is readily accepted by people with needle phobia. It can be used similar to acupuncture, for example, in the treatment of knee osteoarthritis or other diseases related to the knee [24].
5. Conclusion
The following conclusion can be drawn from the present pilot study. The values of regional oxygen saturation (rSO2) on the stimulated side of the knee were significantly increased immediately after acupressure stimulation, whereas the opposite (control) side on the same knee showed insignificant changes. Further investigations with a four-channel NIRS system for measurements on both knees are in progress.
Conflict of Interests
No conflict of interest declared.
Authors' Contribution
G. Litscher and M. Ofner contributed equally to this study.
Acknowledgments
The present study is a pilot study for the project “Interdisciplinary Evaluation of Acute Effects of the Khalifa Therapy in Patients with Ruptured Anterior Cruciate Ligament in the Knee” (project part: Biomedical Engineering and Analyses Focused on NIRS—Thermography and Doppler Flowmetry). The pilot study was also supported by the Stronach Medical Group, Eurasia-Pacific Uninet, the Department of Science of the City of Graz, and Sino-Austrian research projects. It is part of the research area Sustainable Health Research at the Medical University of Graz.
References
- 1.Litscher G. Bioengineering assessment of acupuncture—part 2: monitoring of microcirculation. Critical Reviews in Biomedical Engineering. 2006;34(4):273–294. doi: 10.1615/critrevbiomedeng.v34.i4.10. [DOI] [PubMed] [Google Scholar]
- 2.Hsiu H, Hsu WC, Chen BH, Hsu CL. Differences in the microcirculatory effects of local skin surface contact pressure stimulation between acupoints and nonacupoints: possible relevance to acupressure. Physiological Measurement. 2010;31(6):829–841. doi: 10.1088/0967-3334/31/6/007. [DOI] [PubMed] [Google Scholar]
- 3.Hsiu H, Hsu WC, Chang SL, Hsu CL, Huang SM, Lin YYW. Microcirculatory effect of different skin contacting pressures around the blood pressure. Physiological Measurement. 2008;29(12):1421–1434. doi: 10.1088/0967-3334/29/12/006. [DOI] [PubMed] [Google Scholar]
- 4.Borrat Frigola X, Mercadal Mercadal J, Zavala E. Near-infrared spectroscopy in the postanesthesia recovery care unit: noninvasive monitoring of peripheral perfusion. Revista Española de Anestesiología y Reanimación. 2010;57(6):364–373. doi: 10.1016/s0034-9356(10)70249-8. [DOI] [PubMed] [Google Scholar]
- 5.Fallgatter AJ, Ehlis AC, Wagener A, Michel T, Herrmann MJ. Near-infrared spectroscopy in psychiatry. Nervenarzt. 2004;75(9):911–916. doi: 10.1007/s00115-002-1457-2. [DOI] [PubMed] [Google Scholar]
- 6.Yan J. Skills with Illustrations of Chinese Acupuncture and Moxibustion. Changsha, China: Hunan Science & Technology Press; 2006. [Google Scholar]
- 7.Litscher G. Effects of acupressure, manual acupuncture and Laserneedle acupuncture on EEG bispectral index and spectral edge frequency in healthy volunteers. European Journal of Anaesthesiology. 2004;21(1):13–19. doi: 10.1017/s0265021504001036. [DOI] [PubMed] [Google Scholar]
- 8.Litscher G, Schwarz G, editors. Transcranial Cerebral Oximetry. Lengerich, Germany: Pabst Science Publishers; 1997. [Google Scholar]
- 9.Lee EJ, Frazier SK. The efficacy of acupressure for symptom management: a systematic review. Journal of Pain and Symptom Management. 2011;42(4):589–603. doi: 10.1016/j.jpainsymman.2011.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cho SH, Hwang EW. Acupressure for primary dysmenorrhoea: a systematic review. Complementary Therapies in Medicine. 2010;18(1):49–56. doi: 10.1016/j.ctim.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 11.Abraham J. Acupressure and acupuncture in preventing and managing postoperative nausea and vomiting in adults. Journal of Perioperative Practice. 2008;18(12):543–551. doi: 10.1177/175045890801801204. [DOI] [PubMed] [Google Scholar]
- 12.Meng CR, Fan L, Fu WB, Li Y. Clinical research on abdominal acupuncture plus conventional acupuncture for knee osteoarthritis. Journal of Traditional Chinese Medicine. 2009;29(4):249–252. doi: 10.1016/s0254-6272(09)60075-3. [DOI] [PubMed] [Google Scholar]
- 13.Litscher G. Integrative laser medicine and high-tech acupuncture at the Medical University of Graz, Austria, Europe. Evidence-Based Complementary and Alternative Medicine. 2012;2012:21 pages. doi: 10.1155/2012/103109.103109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Litscher G. Bioengineering assessment of acupuncture—part 5: cerebral near-infrared spectroscopy. Critical Reviews in Biomedical Engineering. 2006;34(6):439–457. doi: 10.1615/critrevbiomedeng.v34.i6.10. [DOI] [PubMed] [Google Scholar]
- 15.Litscher G, Wang L, Huber E. Changes in near-infrared spectroscopic parameters during manual stimulation with acupuncture needles. Biomedizinische Technik. 2002;47(4):76–79. doi: 10.1515/bmte.2002.47.4.76. [DOI] [PubMed] [Google Scholar]
- 16.Litscher G, Wang L. Cerebral near-infrared spectroscopy and acupuncture—preliminary results. Biomedizinische Technik. 2000;45(7-8):215–218. doi: 10.1515/bmte.2000.45.7-8.215. [DOI] [PubMed] [Google Scholar]
- 17.Boushel R, Piantadosi CA. Near-infrared spectroscopy for monitoring muscle oxygenation. Acta Physiologica Scandinavica. 2000;168(4):615–622. doi: 10.1046/j.1365-201x.2000.00713.x. [DOI] [PubMed] [Google Scholar]
- 18.Kaneko J, Sugawara Y, Matsui Y, Sakata H, Kokudo N. Comparison of near-infrared spectroscopy and laser doppler flowmetry for detecting decreased hepatic inflow in the porcine liver. Journal of Investigative Surgery. 2009;22(4):268–274. doi: 10.1080/08941930903040130. [DOI] [PubMed] [Google Scholar]
- 19.Shadgan B, Reid WD, Gharakhanlou R, Stothers L, MacNab AJ. Wireless near-infrared spectroscopy of skeletal muscle oxygenation and hemodynamics during exercise and ischemia. Spectroscopy. 2009;23(5-6):233–241. [Google Scholar]
- 20.Spahn G, Plettenberg H, Kahl E, Klinger HM, Mückley T, Hofmann GO. Near-infrared (NIR) spectroscopy. A new method for arthroscopic evaluation of low grade degenerated cartilage lesions. Results of a pilot study. BMC Musculoskeletal Disorders. 2007;8, article 47 doi: 10.1186/1471-2474-8-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jou NT, Ma SX. Responses of nitric oxide—cGMP release in acupuncture point to electroacupuncture in human skin in vivo using dermal microdialysis. Microcirculation. 2009;16(5):434–443. doi: 10.1080/10739680902915012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hsiao SH, Tsai LJ. A neurovascular transmission model for acupuncture-induced nitric oxide. JAMS Journal of Acupuncture and Meridian Studies. 2008;1(1):42–50. doi: 10.1016/S2005-2901(09)60006-6. [DOI] [PubMed] [Google Scholar]
- 23.Komori M, Takada K, Tomizawa Y, et al. Microcirculatory responses to acupuncture stimulation and phototherapy. Anesthesia and Analgesia. 2009;108(2):635–640. doi: 10.1213/ane.0b013e31819317bc. [DOI] [PubMed] [Google Scholar]
- 24.Jamtvedt G, Dahm KT, Holm I, Flottorp S. Measuring physiotherapy performance in patients with osteoarthritis of the knee: a prospective study. BMC Health Services Research. 2008;8, article 145 doi: 10.1186/1472-6963-8-145. [DOI] [PMC free article] [PubMed] [Google Scholar]


