Abstract
Frequent hemodialysis requires using the vascular access more often than with conventional hemodialysis, but whether this increases the risk for access-related complications is unknown. In two separate trials, we randomly assigned 245 patients to receive in-center daily hemodialysis (6 days per week) or conventional hemodialysis (3 days per week) and 87 patients to receive home nocturnal hemodialysis (6 nights per week) or conventional hemodialysis, for 12 months. The primary vascular access outcome was time to first access event (repair, loss, or access-related hospitalization). Secondary outcomes were time to all repairs and time to all losses. In the Daily Trial, 77 (31%) of 245 patients had a primary outcome event: 33 repairs and 15 losses in the daily group and 17 repairs, 11 losses, and 1 hospitalization in the conventional group. Overall, the risk for a first access event was 76% higher with daily hemodialysis than with conventional hemodialysis (hazard ratio [HR], 1.76; 95% confidence interval [CI], 1.11–2.79; P=0.017); among the 198 patients with an arteriovenous (AV) access at randomization, the risk was 90% higher with daily hemodialysis (HR, 1.90; 95% CI, 1.11–3.25; P=0.02). Daily hemodialysis patients had significantly more total AV access repairs than conventional hemodialysis patients (P=0.011), with 55% of all repairs involving thrombectomy or surgical revision. Losses of AV access did not differ between groups (P=0.58). We observed similar trends in the Nocturnal Trial, although the results were not statistically significant. In conclusion, frequent hemodialysis increases the risk of vascular access complications. The nature of the AV access repairs suggests that this risk likely results from increased hemodialysis frequency rather than heightened surveillance.
Establishing and maintaining a suitable vascular access for hemodialysis has long been considered the Achilles heel of hemodialysis. Any intervention that potentially increases risk to the vascular access must be carefully evaluated.
Frequent hemodialysis provides multiple physiologic and quality-of-life benefits to patients with ESRD. The Frequent Hemodialysis Network (FNH) Daily Trial showed that, compared with conventional thrice-weekly hemodialysis, in-center hemodialysis performed 6 days per week improved self-reported health-related quality of life, left ventricular mass, and several other surrogate outcomes.1 Similar improvement trends have been seen with nocturnal hemodialysis performed 6 nights per week.2,3 Yet despite these demonstrated benefits, frequent hemodialysis may have potential risks. Compared with conventional hemodialysis, frequent hemodialysis requires using the vascular access up to twice as often. In addition to direct trauma caused by more frequent venipuncture of arteriovenous accesses, more frequent access use could theoretically result in increased endothelial trauma due to shear forces created by returning blood, more inflammation, and greater exposure to bacterial pathogens. These factors, in turn, could cause more access stenosis, thrombosis, and infection. In the FHN Daily Trial and Nocturnal Trial, we tested the hypothesis that both types of frequent hemodialysis would increase the risk of vascular access complications.
Results
Baseline Characteristics
In the Daily Trial, 198 patients (81%) were using an arteriovenous fistula or graft at randomization, and 47 patients (19%) were using tunneled catheters (Table 1). In the Nocturnal Trial, the proportion of patients using arteriovenous fistulae or grafts was 53%. Of these, 72% of patients cannulated their access using the buttonhole technique.
Table 1.
Baseline characteristics
| Variable | Daily Trial | Nocturnal Trial | ||||
|---|---|---|---|---|---|---|
| Conventional (n=120) | Daily (n=125) | All (n=245) | Conventional (n=42) | Nocturnal (n=45) | All (n=87) | |
| Age (yr) | 52.0±14.1 | 48.9±13.6 | 50.4±13.9 | 54.0±12.9 | 51.7±14.4 | 52.8±13.6 |
| Male sex | 73 (60.8) | 78 (62.4) | 151 (61.6) | 28 (66.7) | 29 (64.4) | 57 (65.5) |
| Race/ethnicity | ||||||
| Black | 53 (44.2) | 49 (39.2) | 102 (41.6) | 11 (26.2) | 12 (26.7) | 23(26.4) |
| White | 46 (38.3) | 43 (34.4) | 89 (36.3) | 21 (50.0) | 27 (60.0) | 48 (55.2) |
| Native American, aboriginal Canadian, Alaska Native, First Nation | 4 (3.3) | 4 (3.2) | 8 (3.3) | 2 (4.8) | 1 (2.2) | 3 (3.4) |
| Asian | 5 (4.2) | 11 (8.8) | 16 (6.5) | 7 (16.7) | 5 (11.1) | 12 (13.8) |
| Native Hawaiian/other Pacific Islander | 3 (2.5) | 1 (0.8) | 4 (1.6) | 0 (0) | 0 (0) | 0 (0) |
| Other/mixed/unknown | 9 (7.5) | 17 (13.6) | 26 (10.5) | 1 (2.4) | 0 (0) | 1 (1.2) |
| Hispanic/Latino | 31 (26) | 38 (30) | 69 (28.2) | 0 (0) | 0 (0) | 0 (0) |
| ESRD vintage | ||||||
| <2 yr | 35 (29.2) | 37 (29.6) | 72 (29.4) | 30 (71.4) | 28 (62.2) | 58 (66.7) |
| 2–5 yr | 42 (35.0) | 34 (27.2) | 76 (31.0) | 5 (11.9) | 8 (17.8) | 13 (14.9) |
| >5 yr | 43 (35.8) | 54 (43.2) | 97 (39.6) | 7 (16.7) | 9 (20.0) | 16 (18.4) |
| Comorbid conditions | ||||||
| Diabetes | 50 (41.7) | 50 (40.0) | 100 (40.8) | 18 (42.9) | 19 (42.2) | 37 (42.5) |
| Congestive heart failure | 24 (20) | 25 (20) | 49 (20.0) | 7 (16.7) | 5 (11.1) | 12 (13.8) |
| Laboratory values | ||||||
| Albumin (g/dl) | 3.94±0.46 | 3.94±0.37 | 3.94±0.42 | 3.92±0.51 | 3.90±0.48 | 3.91±0.49 |
| Hemoglobin (g/dl) | 12.0±1.2 | 11.9±1.3 | 11.9±1.3 | 11.9±1.1 | 11.6±1.1 | 11.8±1.1 |
| Vascular access used at randomization | ||||||
| Arteriovenous fistula | 71 (59) | 82 (66) | 153 (63) | 17 (40) | 22 (49) | 39 (45) |
| Arteriovenous graft | 23 (19) | 22 (18) | 45 (18) | 4 (10) | 3 (7) | 7 (8) |
| Tunneled catheter | 26 (22) | 21 (17) | 47 (19) | 21 (50) | 20 (44) | 41 (47) |
| Buttonhole technique used (n) | — | — | — | 14 | 19 | 33 |
Unless otherwise indicated, values are expressed as number of patients (percentage). Values expressed with a plus/minus sign are the mean ± SD.
Competing Events
Thirty of 245 patients in the Daily Trial and 6 of 87 patients in the Nocturnal Trial died or underwent transplantation before they reached the primary vascular access outcome. One patient in the Nocturnal Trial was lost to follow-up. Complete vascular access event data were available for all remaining patients.
Deaths Related to Vascular Access
There were three vascular access–related deaths in the two trials. In the Daily Trial, one patient from each group died of arteriovenous access hemorrhage. In the Nocturnal Trial, one patient receiving home nocturnal hemodialysis died of air embolism through the tunneled catheter. After this death, all patients receiving hemodialysis at home with tunneled catheters used needle-free access device extension sets that prevent blood loss or air entry in the event of accidental separation of the catheter port from the dialysis bloodline.
Primary Outcome
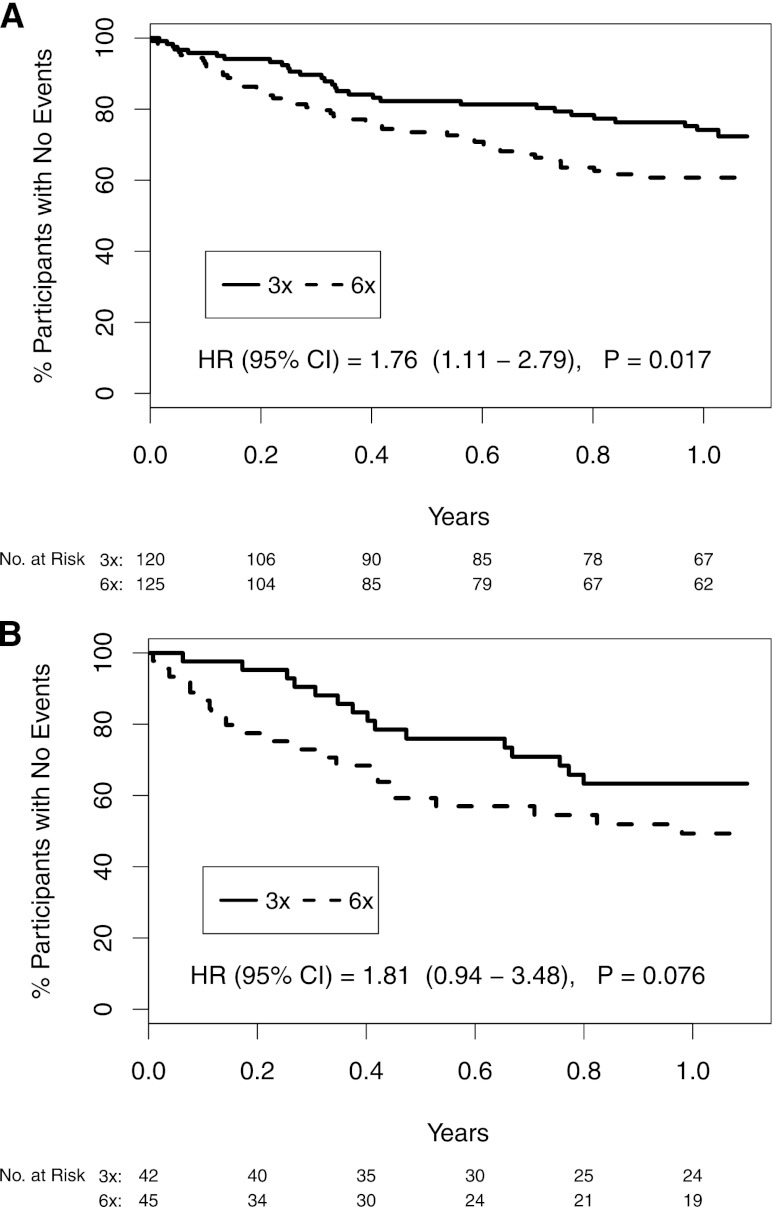
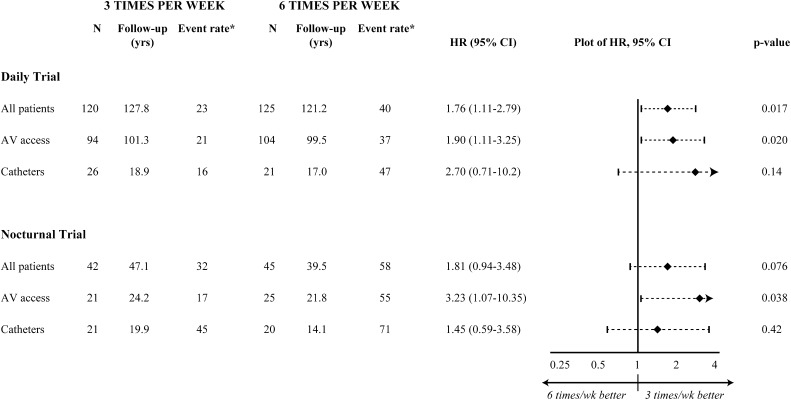
In the Daily Trial, 29 of 120 patients in the conventional group and 48 of 125 patients in the daily group reached the primary outcome (event rate, 23 versus 40 events per 100 patient-years, respectively). The types of events were as follows: in the daily group, 33 repairs and 15 losses; in the conventional group, 17 repairs, 11 losses, and 1 hospitalization. Compared with conventional hemodialysis, the hazard ratio (HR) of having a vascular access event due to daily hemodialysis was 1.76 (95% confidence interval [CI], 1.11–2.79; P=0.017) (Figure 1A). In the subgroup of patients with an arteriovenous fistula or graft at randomization, the HR was 1.90 (95% CI, 1.11–3.25; P=0.020). In patients with catheters, the HR was 2.70 (95% CI, 0.71–10.2; P=0.14) (Figure 2).
Figure 1.
Kaplan-Meier curves of time to first access repair, access loss, or access hospitalization. (A) Daily Trial. (B) Nocturnal Trial.
Figure 2.
Forest plot of time to first access repair, access loss, or access hospitalization by trial and access subgroup. *Event rates expressed as number of events per 100 patient-years. AV access, arteriovenous fistulae and arteriovenous grafts.
In the Nocturnal Trial, 15 of 42 patients in the conventional group and 23 of 45 patients in the nocturnal group reached the primary outcome (event rate, 32 versus 58 events per 100 patient-years, respectively). The types of events were as follows: in the nocturnal group, 10 repairs, 12 losses, and 1 hospitalization; in the conventional group, 5 repairs and 10 losses. Compared with conventional hemodialysis, the HR of having a vascular access event due to nocturnal hemodialysis was 1.81 (95% CI, 0. 94–3.48; P=0.076) (Figure 1B). In the subgroup of patients with an arteriovenous fistula or graft at randomization, the HR was 3.23 (95% CI, 1.07–10.35; P=0.038). In patients with catheters, the HR was 1.45 (95% CI, 0.59–3.58; P=0.42) (Figure 2).
Secondary Outcomes
In the Daily Trial, 106 conventional and 114 daily patients used an arteriovenous access at some point during follow-up, and 34 conventional and 37 daily patients used at least one tunneled catheter. Significantly more total arteriovenous access repairs occurred in the daily group (HR, 1.68; 95% CI, 1.13–2.51; P=0.011). The hazard ratio for repairs was higher for the graft than the fistula subgroup in the Daily Trial (graft subgroup: HR, 2.20, 95% CI, 1.26–3.87, P=0.0059; fistula subgroup: HR, 1.28, 95% CI, 0.71–2.32, P=0.41). Total arteriovenous access losses did not significantly differ between randomly assigned groups (HR, 1.21; 95% CI, 0.61–2.39; P=0.58) (Table 2).
Table 2.
Description of all repairs and losses, considering all accesses used during follow-up
| Daily Trial | Nocturnal Trial | |||||
|---|---|---|---|---|---|---|
| Variable | Conventional | Daily | HR (95% CI) | Conventional | Nocturnal | HR (95% CI) |
| AVF/AVGa | ||||||
| Patients (n) | 106 (79/28)b | 114 (90/28)b | 28 (23/6)b | 32 (29/3)b | ||
| Total follow-up (yr) | 87.9 (67.1/20.8) | 95.8 (76.9/18.9) | 24.2 (18.8/5.4) | 24.3 (22.0/2.3) | ||
| Repairs | ||||||
| Angioplasty | 21 (11/10) | 28 (14/14) | 5 (3/2) | 14 (13/1) | ||
| Stent placement | 2 (2/0) | 2 (1/1) | 0 (0/0) | 0 (0/0) | ||
| Thrombectomy | 10 (3/7) | 22 (5/17) | 1 (0/1) | 2 (1/1) | ||
| Surgical revision | 5 (3/2) | 14 (7/7) | 1 (1/0) | 0 (0/0) | ||
| Overall rate (per 100 patient-yr) | 43 | 69 | 1.68 (1.13–2.51) P=0.011 | 29 | 66 | 2.29 (0.94–5.59) P=0.069 |
| Losses | ||||||
| Stenosis/thrombosis | 8 (5/3) | 13 (5/8) | 2 (1/1) | 2 (2/0) | ||
| SItenosis/thrombosis | ||||||
| Infection | 2 (0/2) | 2 (0/2) | 1 (0/1) | 0 (0/0) | ||
| Otherc | 1 (1/0) | 3 (2/1) | 0 (0/0) | 0 (0/0) | ||
| Unknown | 4 (2/2) | 2 (1/1) | 1 (0/1) | 2 (2/0) | ||
| Overall rate (per 100 patient-yr) | 17 | 21 | 1.21 (0.61–2.39) P=0.58 | — | — | — |
| Catheters | ||||||
| Patients (n) | 34 | 37 | 24 | 23 | ||
| Total follow-up (yr) | 20.8 | 18.9 | 19.0 | 18.1 | ||
| Repairs (n) | ||||||
| Fibrin sheath stripping | 1 | 4 | 0 | 1 | ||
| Repair broken component | 0 | 0 | 1 | 0 | ||
| Losses (n) | ||||||
| Poor flows/thrombosis | 7 | 2 | 8 | 8 | ||
| Infection | 2 | 7 | 4 | 5 | ||
AVF, arteriovenous fistula; AVG, arteriovenous graft.
Results for arteriovenous accesses are presented as total number of patients (AVF number/AVG number). Overall hazard ratios are for AVF and AVG combined. For separate rates for AVF and AVG, see text.
Numbers for AVF and AVG are greater than total number because some patients had more than one type of arteriovenous access during follow-up.
Other reasons were as follows: one ligation for aneurysm, one severe swelling/hematoma, two profuse bleeding from laceration.
In the Nocturnal Trial, 28 conventional and 32 nocturnal patients used an arteriovenous access at some point during follow-up, and 24 conventional and 23 nocturnal patients used at least one tunneled catheter. More total arteriovenous access repairs occurred in the nocturnal group, but this result did not reach statistical significance (HR, 2.29; 95% CI, 0.94–5.59; P=0.069). Unlike in the Daily Trial, this trend was driven by arteriovenous fistulae repairs (fistula subgroup: HR, 2.87; 95% CI, 0.94–8.73; P=0.063). Only five graft repairs occurred in the Nocturnal Trial, precluding analysis of this subgroup. The number of total arteriovenous access losses was low and similar in nocturnal and conventional groups (Table 2).
Compared with the rope-ladder technique, the use of the buttonhole technique was associated with longer periods between successive arteriovenous access events (HR, 0.44; 95% CI, 0.20–0.97; P=0.041).
Discussion
To date, opinions regarding the potential effects of frequent hemodialysis on vascular access have been controversial. Some authors have postulated that frequent hemodialysis may actually be beneficial to the vascular access because of fewer intradialytic hypotensive episodes, better hemostasis at puncture sites, and lower required blood flow rates.4 This view has been supported primarily by small, uncontrolled studies describing very low vascular access event rates with daily and nocturnal hemodialysis.5–8 Two nonrandomized studies suggested that, compared with conventional dialysis, daily dialysis is associated with a five-fold decrease in access complications.9,10 However, two literature reviews suggested the opposite.11,12 These reviews highlighted two North American nonrandomized studies that reported a trend to doubling of access interventions in patients receiving daily hemodialysis with arteriovenous fistulae.13–15 Because observational studies can be affected by selection bias and confounding, it is difficult to draw conclusions from these prior studies.
The FHN trials are the largest randomized controlled trials to examine whether frequent hemodialysis performed six times per week poses any risks or benefits to the vascular access. Vascular access was prespecified as the major safety outcome.1,3,16 We found that daily hemodialysis significantly increased the risk of vascular access complications, as measured by time to first access repair, loss, or access-related hospitalization (HR, 1.76; 95% CI, 1.11–2.79; P=0.017). In the subgroup of 198 patients using an arteriovenous fistula or graft at randomization, a similarly increased risk was observed with daily hemodialysis (HR, 1.90; 95% CI, 1.11–3.25; P=0.020). Although the rates of permanent access loss did not significantly differ between groups, the rate of total arteriovenous repairs was significantly higher in the daily group (HR, 1.68; 95% CI, 1.13–2.51; P=0.011). In the Daily Trial, this result appeared to be driven by more graft repairs, especially surgical revisions and thrombectomies. Catheter events were too few to allow us to draw meaningful conclusions regarding the effects of daily dialysis on this type of access. Similar trends were observed for the Nocturnal Trial, although most results did not reach statistical significance, probably because of low statistical power. It is noteworthy that the point estimate of the HR for the primary outcome was similar between the Daily and Nocturnal trials. These trends appeared to be driven by more fistula angioplasties in the nocturnal group.
One previous randomized trial of nocturnal hemodialysis was conducted in Alberta, Canada, with 53 patients followed for 6 months.2 Rates of bacteremia, insertion or replacement of tunneled dialysis catheters, angiography, and surgical interventions were similar between patients receiving nocturnal and conventional dialysis (P=0.85). Given differences in definitions, statistical analysis, and follow-up times, it is difficult to make direct comparisons between the two trials. However, it is worth mentioning that nocturnal patients in the Alberta trial did undergo more surgical interventions and angioplasties than did conventional patients (10 versus 4).2 This trial, similar to ours, was limited by low statistical power.
What are the potential mechanisms for the observed increased risk of access complications with daily hemodialysis? We considered the possibility that patients receiving daily hemodialysis who are seen in the dialysis unit up to twice as often may have had more intensive surveillance of their access, resulting in increased referrals for repairs, such as angioplasty. However, the nature of repairs required suggests that this was not the case. More than half the repairs in the daily group were thrombectomies or surgical revisions: 36 in total in the daily group compared with just 15 in the conventional group. These procedures probably resulted in salvage of many accesses that would have otherwise been lost permanently. Had FHN centers not had rapid availability of these procedures, the rate of arteriovenous access losses may have been higher. We also considered that physicians may have raised blood flow targets for daily patients to achieve the target eKt/V with minimal time per session. However, average blood flows did not differ between daily and conventional patients throughout the trial (data not shown). That similar trends were observed in the Nocturnal Trial supports that heightened surveillance and increased blood flow targets are not likely explanations for our findings. Patients receiving nocturnal dialysis at home do not have increased surveillance by the health care team, and blood flow targets are lower than with conventional dialysis.
Rather, we hypothesize that more frequent use of the arteriovenous access itself causes vascular access dysfunction. Although increased frequency of venipuncture may result in direct access damage, the mechanisms causing stenosis may be indirect. Stenotic fistula and graft lesions are associated with profibrotic cytokine production, local inflammation, and neointimal proliferation.17,18 Repeated trauma at venipuncture sites and turbulent blood flow may promote this process. Most access problems in our study were related to stenosis or thrombosis, supporting this theory. However, contrary to our hypothesis, increased exposure to bacterial pathogens does not seem to play a role because the risk of access infection was not increased with frequent hemodialysis.
Are there factors that may attenuate the risk of access complications with frequent hemodialysis? It is possible that lower blood flows used with nocturnal hemodialysis (approximately 200 ml/min instead of >400 ml/min) may protect against stenosis and thrombosis. Although the two trials were not formally compared, there appeared to be fewer thromboses, thrombectomies, and surgical revisions in the Nocturnal Trial than in the Daily Trial, supporting this hypothesis. Some have hypothesized that self-cannulation or cannulation by a single caregiver (as occurred in the Nocturnal Trial) may be more protective than cannulation by multiple nurses or dialysis technicians (as occurred in the Daily Trial). That the HR for arteriovenous access repairs was higher in the Nocturnal than in the Daily Trial suggests that this is not the case. We did observe fewer access events with buttonhole than with rope-ladder technique, mainly driven by fewer thrombotic complications requiring repair. This has been seen elsewhere.19 It may be that fewer venipuncture sites and establishment of an endothelial tunnel for needle entry may reduce trauma and release of inflammatory mediators. This finding must be weighed against recent studies suggesting that the buttonhole technique may increase infection risk20,21
Some may read this report and conclude that frequent hemodialysis is best performed with a tunneled catheter. We emphasize that our results do not in any way support this conclusion. Only about 20 patients per group used tunneled catheters at randomization in each trial, limiting our ability to draw meaningful conclusions about the effects of frequent hemodialysis on catheters. Although further large randomized trials of frequent hemodialysis may not be feasible, rigorous prospective studies with matched control groups may shed light on this issue.
The increased risk of access complications with frequent hemodialysis may have significant clinical impact. If repair procedures are not readily available, patients may lose their permanent arteriovenous access and end up with a tunneled catheter. In addition, frequent repairs could eventually frustrate both the patient and the care team, resulting in abandonment of the arteriovenous access in favor of a tunneled catheter. Finally, costs to maintain a functional arteriovenous access would be greater with frequent than with conventional hemodialysis, and these costs must be considered in evaluating cost-effectiveness of the therapy.
Our study has several strengths. We obtained detailed vascular access data prospectively in the setting of the largest randomized trials of frequent hemodialysis to date. All events were adjudicated by a committee blinded to group allocation. Finally, the consistency of the hazard ratios across both trials strengthens the robustness of these results. The limitations of our study also need to be considered. We did not collect detailed information on why patients were sent for various repair procedures, and we could not capture whether heightened surveillance led to more access procedures in the frequent dialysis groups. Competing risks of death and transplantation were high in these trials but were relatively equal between groups. Duration of follow-up was relatively short and may not have been long enough to detect differences in access losses. Despite being the largest trials in this field to date, statistical power was limited, especially in the Nocturnal Trial, to detect differences in the types of repairs and in individual subgroups. Finally, as with all randomized trials, the generalizability of our results is limited.
In conclusion, frequent hemodialysis increased the risk of vascular access complications, largely because of the need for more repair procedures in patients with arteriovenous accesses. The nature of the repairs suggests that this risk was probably a consequence of increased hemodialysis frequency rather than heightened surveillance. Further studies may help to elucidate the effects of frequent hemodialysis on tunneled catheter performance and complications, as well as the relative safety of buttonhole versus other cannulation techniques.
Concise Methods
Trial Design
The FHN trials have been described in detail elsewhere.16 In the Daily Trial, 245 patients from 11 sites in the United States and Canada were randomly assigned to receive daily hemodialysis (1.5–2.75 hours per session, 6 days per week) or conventional hemodialysis (2.5–4.5 hours per session, 3 days per week). Both groups received their hemodialysis treatments in outpatient settings. In the Daily Trial, all accesses were cannulated by nurses or dialysis technicians. In the Nocturnal Trial, 87 patients from nine centers in the United States and Canada were randomly assigned to receive nocturnal hemodialysis (at least 6 hours, 6 nights per week) or conventional hemodialysis. For this trial, all patients and/or their caregivers were trained to perform hemodialysis at home, including cannulation of the access. Patients were followed for 12 months. The prespecified major safety outcome was vascular access complications.16
Vascular Access Data
Detailed vascular access data were captured on specific event reporting forms.
Access repair was defined as any procedure performed on the access that resulted in continued use of the same access. We recorded angioplasty, stenting, thrombectomy, and surgical revision for arteriovenous accesses and stripping of fibrin sheaths and repair of broken components for catheters. Because thrombolysis of catheters using tissue plasminogen activator was not captured accurately across all centers, we did not include thrombolysis in the final definition of repair.
Access loss was defined as abandonment (i.e., access no longer being used) or removal of the access for any reason. This included replacing tunneled catheters over a wire. If a patient was using an arteriovenous fistula or graft but then had a new tunneled catheter inserted, this was counted as an arteriovenous fistula or graft loss. Elective removals of catheters upon successful use of a new arteriovenous fistula or graft were recorded but were not counted as events. A vascular access outcomes committee blinded to group allocation reviewed all access events to determine whether the event met the definition of repair or loss.
Coordinators captured all deaths and hospitalizations on separate event forms. An independent outcomes committee blinded to group allocation reviewed these forms, discharge summaries, and supplementary chart information to determine whether each death or hospitalization was access related or non–access related.
Outcomes
The primary vascular access outcome was defined as the composite of time to first access repair, loss, or access-related hospitalization. If an access loss occurred within 10 days of a repair procedure, the loss was counted instead of the repair. Prespecified secondary outcomes were time to any repair and time to any loss. Specific reasons for repair and loss were defined as descriptive outcomes only.
Statistical Analyses
Primary Analysis
Data from each trial were analyzed separately. We plotted Kaplan-Meier survival curves of the risk of reaching the primary outcome for each group and used the log-rank test to compare differences between the curves.22 We used Cox proportional hazards models to estimate the relative change in hazard rate of the primary outcome due to daily or nocturnal hemodialysis.23 For the Daily Trial, we adjusted for effects of clinical center. We censored patients at the time of death, transplant, or loss to follow-up in all analyses. Patients who had elective removal of a catheter when an arteriovenous fistula or graft was used were followed until the end of follow-up or until they had an event.
Additional Analyses
For each trial, we repeated the primary analysis after grouping patients by access type (arteriovenous fistulae or grafts and catheters). Elective switches from a catheter to a fistula or graft were treated as censoring events.
We evaluated the two secondary outcomes of time to all losses and time to all repairs using Andersen-Gill models.24 For the analyses of access losses, each successive access contributed sequentially to the periods of risk; access hospitalizations and repairs were ignored. For the repairs-only analyses, losses and hospitalizations were ignored. Multiple repairs that occurred within 10 days were treated as a single repair event. Because of few catheter events, we restricted our statistical comparisons of the secondary outcomes to arteriovenous fistulae and grafts.
Finally, for patients using arteriovenous accesses in the Nocturnal Trial, we assessed the effect of using buttonhole technique on all losses, repairs, or access hospitalizations. We used the Andersen-Gill model, treating buttonhole technique as a time-dependent covariate. Buttonhole status was imputed for 6.4% of patient records on the basis of usage patterns observed among the patients’ nonmissing data (see Supplemental Material).
All analyses were performed with SAS 9.2 (Cary, NC).
The authors are indebted to the patients who participated in the study and to the U.S. Renal Data System for providing additional hospitalization data. These trials were registered at Clinical Trials.gov #NCT00264758 and #NCT00271999.
Disclosures
R.S.S. and R.M.L. have unrestricted research grants from Fresenius Medical Care Canada and Baxter Inc. M.R. is a consultant for Amgen and DaVita. R.S.L. sits on the Machine Medical Advisory Board for Fresenius Medical Care North America (Sorbent Machine).
Acknowledgments
This study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases, the Centers for Medicare & Medicaid Services, and the National Institutes of Health (NIH) Research Foundation. The investigators and sponsors are grateful for the support of contributors to the NIH Foundation: Amgen, Baxter, and Dialysis Clinics, and support from Fresenius Medical Care. R.S. was funded by a Canadian Institutes of Health Randomized Trials Mentorship Award.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
See related editorial, “Can Frequent Hemodialysis Be Too Frequent?,” on pages 334–336.
This article contains supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2012060595/-/DCSupplemental.
References
- 1.Chertow GM, Levin NW, Beck GJ, Depner TA, Eggers PW, Gassman JJ, Gorodetskaya I, Greene T, James S, Larive B, Lindsay RM, Mehta RL, Miller B, Ornt DB, Rajagopalan S, Rastogi A, Rocco MV, Schiller B, Sergeyeva O, Schulman G, Ting GO, Unruh ML, Star RA, Kliger AS, FHN Trial Group : In-center hemodialysis six times per week versus three times per week. N Engl J Med 363: 2287–2300, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Culleton BF, Walsh M, Klarenbach SW, Mortis G, Scott-Douglas N, Quinn RR, Tonelli M, Donnelly S, Friedrich MG, Kumar A, Mahallati H, Hemmelgarn BR, Manns BJ: Effect of frequent nocturnal hemodialysis vs conventional hemodialysis on left ventricular mass and quality of life: a randomized controlled trial. JAMA 298: 1291–1299, 2007 [DOI] [PubMed] [Google Scholar]
- 3.Rocco MV, Lockridge RS, Jr, Beck GJ, Eggers PW, Gassman JJ, Greene T, Larive B, Chan CT, Chertow GM, Copland M, Hoy CD, Lindsay RM, Levin NW, Ornt DB, Pierratos A, Pipkin MF, Rajagopalan S, Stokes JB, Unruh ML, Star RA, Kliger AS, Kliger A, Eggers P, Briggs J, Hostetter T, Narva A, Star R, Augustine B, Mohr P, Beck G, Fu Z, Gassman J, Greene T, Daugirdas J, Hunsicker L, Larive B, Li M, Mackrell J, Wiggins K, Sherer S, Weiss B, Rajagopalan S, Sanz J, Dellagrottaglie S, Kariisa M, Tran T, West J, Unruh M, Keene R, Schlarb J, Chan C, McGrath-Chong M, Frome R, Higgins H, Ke S, Mandaci O, Owens C, Snell C, Eknoyan G, Appel L, Cheung A, Derse A, Kramer C, Geller N, Grimm R, Henderson L, Prichard S, Roecker E, Rocco M, Miller B, Riley J, Schuessler R, Lockridge R, Pipkin M, Peterson C, Hoy C, Fensterer A, Steigerwald D, Stokes J, Somers D, Hilkin A, Lilli K, Wallace W, Franzwa B, Waterman E, Chan C, McGrath-Chong M, Copland M, Levin A, Sioson L, Cabezon E, Kwan S, Roger D, Lindsay R, Suri R, Champagne J, Bullas R, Garg A, Mazzorato A, Spanner E, Rocco M, Burkart J, Moossavi S, Mauck V, Kaufman T, Pierratos A, Chan W, Regozo K, Kwok S, Frequent Hemodialysis Network (FHN) Trial Group : The effects of frequent nocturnal home hemodialysis: the Frequent Hemodialysis Network Nocturnal Trial. Kidney Int 80: 1080–1091, 2011. 21775973 [Google Scholar]
- 4.Twardowski ZJ: Blood access in daily hemodialysis. Hemodial Int 8: 70–76, 2004 [DOI] [PubMed] [Google Scholar]
- 5.Pinciaroli A: Results of daily hemodialysis in Catanzaro: A 12-year experience with 22 patients treated for more than 1 year. Home Hemodialysis International 2: 12–17, 1998 [DOI] [PubMed] [Google Scholar]
- 6.Kiellstrand CM, Blagg CR, Twardowski ZJ, Bower J: Blood access and daily hemodialysis: Clinical experience and review of the literature. ASAIO J 49: 645–649, 2003 [DOI] [PubMed] [Google Scholar]
- 7.Kooistra MP, Vos J, Koomans HA, Vos PF: Daily home haemodialysis in The Netherlands: Effects on metabolic control, haemodynamics, and quality of life. Nephrol Dial Transplant 13: 2853–2860, 1998 [DOI] [PubMed] [Google Scholar]
- 8.Agar JWM, Somerville CA, Dwyer KM, Simmonds RE, Boddington JM, Waldron CM: Nocturnal hemodialysis in Australia. Hemodial Int 7: 278–289, 2003 [DOI] [PubMed] [Google Scholar]
- 9.Quintaliani G, Buoncristiani U, Fagugli R, Kuluiranu H, Ciao G, Rondini L, Lowenthal DT, Reboldi G: Survival of vascular access during daily and three times a week hemodialysis. Clin Nephrol 53: 372–377, 2000 [PubMed] [Google Scholar]
- 10.Woods JD, Port FK, Orzol S, Buoncristiani U, Young E, Wolfe RA, Held PJ: Clinical and biochemical correlates of starting “daily” hemodialysis. Kidney Int 55: 2467–2476, 1999 [DOI] [PubMed] [Google Scholar]
- 11.Suri RS, Nesrallah GE, Mainra R, Garg AX, Lindsay RM, Greene T, Daugirdas JT: Daily hemodialysis: A systematic review. Clin J Am Soc Nephrol 1: 33–42, 2006 [DOI] [PubMed] [Google Scholar]
- 12.Shurraw S, Zimmerman D: Vascular access complications in daily dialysis: A systematic review of the literature. Minerva Urol Nefrol 57: 151–163, 2005 [PubMed] [Google Scholar]
- 13.Ting G: Blood access outcomes associated with short daily hemodialysis. Home Hemodialysis International 4: 42–46, 2000 [DOI] [PubMed] [Google Scholar]
- 14.Ting GO, Kjellstrand C, Freitas T, Carrie BJ, Zarghamee S: Long-term study of high-comorbidity ESRD patients converted from conventional to short daily hemodialysis. Am J Kidney Dis 42: 1020–1035, 2003 [DOI] [PubMed] [Google Scholar]
- 15.Lindsay RM, Leitch R, Heidenheim AP, Kortas C, London Daily/Nocturnal Hemodialysis Study : The London Daily/Nocturnal Hemodialysis Study—study design, morbidity, and mortality results. Am J Kidney Dis 42[Suppl]: 5–12, 2003 [DOI] [PubMed] [Google Scholar]
- 16.Suri RS, Garg AX, Chertow GM, Levin NW, Rocco MV, Greene T, Beck GJ, Gassman JJ, Eggers PW, Star RA, Ornt DB, Kliger AS, Frequent Hemodialysis Network Trial Group : Frequent Hemodialysis Network (FHN) randomized trials: Study design. Kidney Int 71: 349–359, 2007 [DOI] [PubMed] [Google Scholar]
- 17.Lee T, Roy-Chaudhury P: Advances and new frontiers in the pathophysiology of venous neointimal hyperplasia and dialysis access stenosis. Adv Chronic Kidney Dis 16: 329–338, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stracke S, Konner K, Köstlin I, Friedl R, Jehle PM, Hombach V, Keller F, Waltenberger J: Increased expression of TGF-beta1 and IGF-I in inflammatory stenotic lesions of hemodialysis fistulas. Kidney Int 61: 1011–1019, 2002 [DOI] [PubMed] [Google Scholar]
- 19.van Loon MM, Goovaerts T, Kessels AG, van der Sande FM, Tordoir JH: Buttonhole needling of haemodialysis arteriovenous fistulae results in less complications and interventions compared to the rope-ladder technique. Nephrol Dial Transplant 25: 225–230, 2010 [DOI] [PubMed] [Google Scholar]
- 20.MacRae JM, Ahmed SB, Atkar R, Hemmelgarn BR: A randomized trial comparing buttonhole with rope ladder needling in conventional hemodialysis patients. Clin J Am Soc Nephrol 7: 1632–1638, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chow J, Rayment G, San Miguel S, Gilbert M: A randomised controlled trial of buttonhole cannulation for the prevention of fistula access complications. J Ren Care 37: 85–93, 2011 [DOI] [PubMed] [Google Scholar]
- 22.Kaplan EL, Meier P: Non-parametric estimation from incomplete observations. J Am Stat Assoc 53: 457–481, 1958 [Google Scholar]
- 23.Cox DR: Regression models and life tables. J R Stat Soc, B 34: 187–220, 1972 [Google Scholar]
- 24.Andersen PK, Gill RD: Cox's regression model for counting processes: A large sample study. Ann Stat 10: 1100–1120, 1982 [Google Scholar]