Abstract
Clinical practice guidelines recommend an arteriovenous fistula as the preferred vascular access for hemodialysis, but quantitative associations between vascular access type and various clinical outcomes remain controversial. We performed a systematic review of cohort studies to evaluate the associations between type of vascular access (arteriovenous fistula, arteriovenous graft, and central venous catheter) and risk for death, infection, and major cardiovascular events. We searched MEDLINE, EMBASE, and article reference lists and extracted data describing study design, participants, vascular access type, clinical outcomes, and risk for bias. We identified 3965 citations, of which 67 (62 cohort studies comprising 586,337 participants) met our inclusion criteria. In a random effects meta-analysis, compared with persons with fistulas, those individuals using catheters had higher risks for all-cause mortality (risk ratio=1.53, 95% CI=1.41–1.67), fatal infections (2.12, 1.79–2.52), and cardiovascular events (1.38, 1.24–1.54). Similarly, compared with persons with grafts, those individuals using catheters had higher risks for mortality (1.38, 1.25–1.52), fatal infections (1.49, 1.15–1.93), and cardiovascular events (1.26, 1.11–1.43). Compared with persons with fistulas, those individuals with grafts had increased all-cause mortality (1.18, 1.09–1.27) and fatal infection (1.36, 1.17–1.58), but we did not detect a difference in the risk for cardiovascular events (1.07, 0.95–1.21). The risk for bias, especially selection bias, was high. In conclusion, persons using catheters for hemodialysis seem to have the highest risks for death, infections, and cardiovascular events compared with other vascular access types, and patients with usable fistulas have the lowest risk.
Although life-sustaining, hemodialysis is marked by persistently high mortality, morbidity, and healthcare use. Worldwide, over 1.5 million persons are treated with hemodialysis, and 10%–25% of them die each year.1 Effective hemodialysis requires repeated and reliable access to the bloodstream through a central venous catheter or a surgically created arteriovenous communication (an autologous fistula or a synthetic graft).2 However, vascular access thrombosis and infection occur frequently and are the leading cause of dialysis-related morbidity.1,2 Each year, persons on hemodialysis are hospitalized two times on average, with 1 in 10 hospitalizations caused by vascular access infection.1 A central venous catheter is required when the arteriovenous fistula or graft fails to sufficiently mature for dialysis or becomes occluded by thrombosis.
Clinical practice guidelines strongly recommend the arteriovenous fistula as the preferred access option for all persons receiving hemodialysis, because observational data show that mature fistulas are more durable and associated with lower morbidity and mortality compared with grafts and catheters.3–5 Low rates of fistula use have led to initiatives, such as Fistula First in the United States, aimed at achieving the clinical and organizational changes needed to increase fistula use.6 Increasing fistula creation is a national health objective in the United States.7 Furthermore, the proportion of patients treated with functioning fistulas is considered a proxy for the quality of hemodialysis care, and reimbursement has been linked to performance targets in some jurisdictions.8 Notwithstanding current practice policies, achieving a suitable fistula is challenging or impossible in some persons,9 and repeated procedures are often necessary.2 There has been concern that resource-intensive programs implemented to maximize fistula use relative to grafts may have inadvertently led to increased unsuccessful fistula attempts and catheter use, resulting in smaller incremental benefits than anticipated10 and increased potential harm, which may have been underestimated.11 To date, no randomized trials have evaluated the benefits and harms of hemodialysis access strategies or the clinical practices and policies established to achieve them.
Considering the extensive public policy recommendations and actions to promote fistula use, we aimed to quantify the associations between vascular access type and mortality, infection, and cardiovascular events and assess the quality of available epidemiologic data. We did a systematic review of cohort studies to evaluate the association between hemodialysis access type and mortality, infection, hospitalization, and cardiovascular events in persons with end stage kidney disease treated with hemodialysis according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses.12
Results
Characteristics of Included Studies
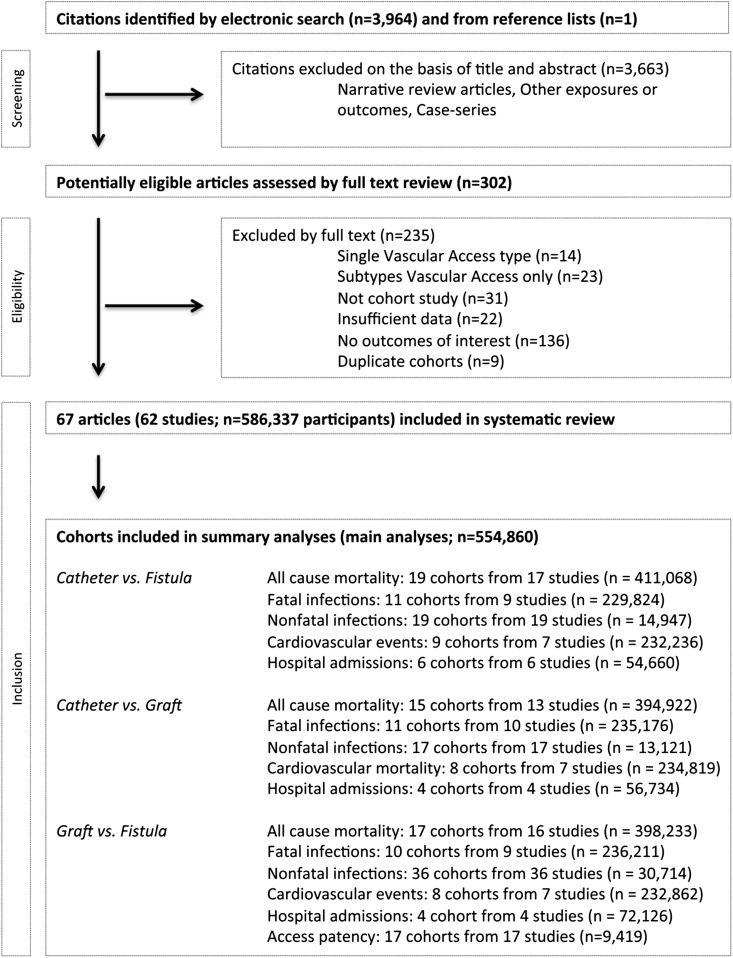
Electronic searching identified 3964 citations, and one study was identified from reference lists (Figure 1). We excluded 3898 citations on title and abstract or detailed review. We could include 67 articles published between 1985 and 2011 (62 studies) reporting data on 363 vascular access type comparisons in 586,337 participants. Study characteristics including full reference list, sample size, population characteristics, and follow-up are reported in Supplemental Tables 1 and 2. Nineteen articles were published from the same data sources: the Hemodialysis (HEMO) study, the US Renal Data System, the Canadian Organ Replacement Registry, the Dialysis Outcomes Practice Pattern Study, and the Fresenius Medical Care database. Four publications included potentially duplicative cohorts, which we included separately in sensitivity analyses. Three study authors provided clarification or additional unpublished data (Supplemental Table 3). We could include 209 unique access type comparisons in summary analyses (n=545,441) and 62 comparisons in sensitivity analyses (n=446,621).
Figure 1.
Flow diagram of the identification process for eligible studies. Hospitalizations were from any cause.
Risk of Bias
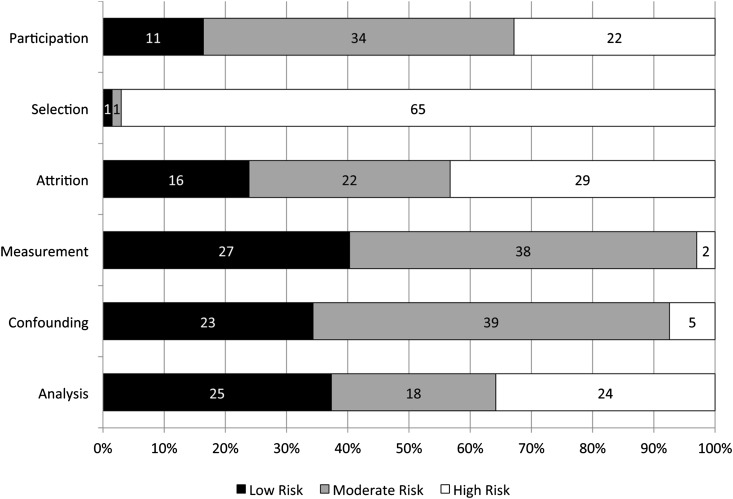
We found that reporting of methods was incomplete in many studies, and no study was at low risk for bias in all domains that we assessed (Figure 2). All except two small studies13,14 (3%) compared outcomes according to the hemodialysis access achieved as opposed to the hemodialysis access attempted or intended, and thus, they were considered at high risk of selection bias. One study (n=32) compared a strategy based on arteriovenous access attempts with a strategy based on catheter insertion without surgical attempts in persons older than 75 years who were eligible to receive an arteriovenous access.13 The other study (n=30) compared local infections after femoral graft or fistula placement in persons with limited surgical options.14 All remaining studies compared persons for whom a fistula or a graft was successful with persons who used catheters for any reason.
Figure 2.
Risk of bias in the included articles. Two items were considered for each quality domain to define the risk of bias of the included articles (n=67) as described in Supplemental Table 4; numbers indicate the numbers of articles.
Patient Outcomes
Catheter Versus Fistula
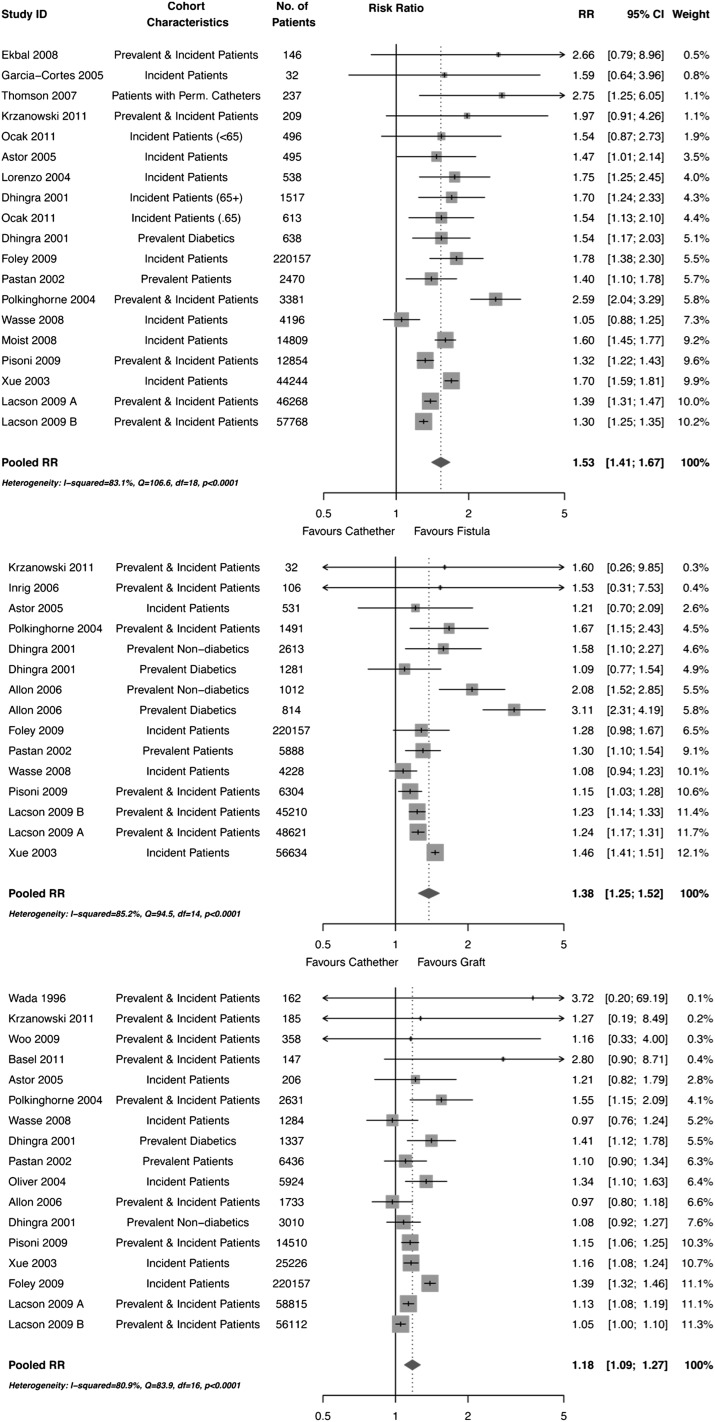
Persons using catheters had increased risk of all-cause mortality (risk ratio [RR]=1.53, 95% confidence interval [95% CI]=1.41–1.67), fatal (RR=2.12, 95% CI=1.79–2.52) and nonfatal (RR=4.66, 95% CI=2.63–8.26) infection, major cardiovascular event (RR=1.38, 95% CI=1.24–1.54), and hospitalization (RR=1.68, 95% CI=1.33–2.12) compared with persons using fistulas (Figure 3 and Supplemental Figure 1). We explored the heterogeneity in the analysis of all-cause mortality (I2>83%) with prespecified subgroup analyses (Supplemental Figure 2). Associations were similar between studies evaluating access at baseline (initial access) and studies using updated access types in analyses (time-varying). We noted weaker and nonsignificant associations with mortality in studies published after 2004 and larger studies. RRs were materially the same in studies, regardless of the level of adjustment in analyses.
Figure 3.
Primary outcome: risk of all-cause mortality for the use of central venous catheters versus fistulas or grafts and the use of arteriovenous grafts versus fistulas in people on hemodialysis; studies are ordered by weight. We pooled the estimates reported by Polkinghorne et al.31 for the comparison of catheters versus fistulas (three estimates) and catheters versus grafts (three estimates) according to the time spent on hemodialysis when patients were registered; we also pooled the estimates reported by Foley et al.32 for the comparison of catheters versus fistulas and catheters versus grafts (each with three estimates) according to whether the patient has a catheter only, a catheter with a maturing fistula, or a graft.
Catheter Versus Graft
Persons using catheters had increased risk of all-cause mortality (RR=1.38, 95% CI=1.25–1.52), fatal (RR=1.49, 95% CI=1.15–1.93) and nonfatal (RR=2.78, 95% CI=1.80–4.29) infection, cardiovascular event (RR=1.26, 95% CI=1.11–1.43), and hospitalization (RR=1.51, 95% CI=1.30–1.75) compared with those individuals using grafts. When we explored the heterogeneity in the analysis of all-cause mortality (I2>85%), we noted weaker associations in studies that had a smaller proportion of men.
Graft Versus Fistula
Persons using grafts had increased risk of all-cause mortality (RR=1.18, 95% CI=1.09–1.27), fatal (RR=1.36, 95% CI=1.17–1.58) and nonfatal (RR=2.76, 95% CI=2.13–3.58) infection, and hospitalization (RR=1.26, 95% CI=1.13–1.40) compared with those individuals using fistulas. The effect of exposure to graft compared with fistula on cardiovascular events was uncertain (RR=1.07, 95% CI=0.95–1.21). Heterogeneity in the analysis for all-cause mortality (I2>80%) remained unexplained by subgroup analyses.
Cumulative Meta-Analyses, Publication Bias, and Sensitivity Analyses
Cumulative meta-analysis of all comparisons showed that the observed pooled risks of mortality have been statistically significant since 2001–2002. Subsequent studies have conferred little gain in precision and have not materially changed the estimated risks of death (Supplemental Figure 3). We observed no funnel plot asymmetry or statistical evidence of small study effects or publication bias in any of the analyses. Separate inclusion of estimates from publications based on potentially duplicative cohorts in meta-analyses of all combined or adjusted studies did not change the observed associations. Pooled estimates were materially unchanged when estimates based on different adjustment methods from the same study were entered in primary meta-analyses or subgroup analyses, when we excluded cohorts comparing catheters versus fistulas and grafts combined (Supplemental Appendix), or when we used studies including persons requiring complex surgical procedures or specific populations (children or HIV-positive persons).
Arteriovenous Access Patency
Fifteen studies reported data on arteriovenous access patency (Supplemental Table 5). However, information reported was variable and insufficient to produce pooled summary statistics. Four studies reported adjusted data, and the remainder provided only crude comparisons. Survival plots or 1- to 5-year access survival probabilities were reported by all but three studies; 11 studies reported significantly greater patency rates for fistulas then grafts, and 2 studies reported nonsignificant differences (Supplemental Appendix).
Discussion
In our meta-analysis, including 62 cohort studies comprising over 500,000 participants, we found that persons using central venous catheters for hemodialysis experience a much higher risk of death, infection, cardiovascular events, and hospitalization compared with persons who achieve an arteriovenous fistula or a graft as hemodialysis access. Graft use is associated with increased risk of death, infection, and hospitalization but has weaker and uncertain associations with cardiovascular events. In absolute terms, catheter use is associated with 80–134 additional deaths per 1000 person-years compared with fistula use and 60–125 additional deaths per 1000 person-years compared with graft use. Graft use is associated with 18–54 additional deaths for every 1000 persons each year compared with fistula use (Table 1). The direction of the risk for mortality (lower in fistula and graft users than catheter users and lower in fistula users than graft users) is highly consistent across existing observational studies.
Table 1.
Summary of absolute risks of death from all causes, major cardiovascular events, and fatal infections associated with dialysis vascular access types
| Reference Annual Event Riska | Vascular Access Comparison | Meta-Analytical RR (95% CI) | Heterogeneity (I2; P Value) | Number of Additional Events per 1000 Patients Exposed per Year (95% CI) |
|---|---|---|---|---|
| All-cause mortality | ||||
| 0.20 for fistula users | Catheter versus fistula | 1.53 (1.40–1.67) | 83.9%; <0.01 | 106 (80–134) excess with catheter |
| 0.24 for graft users | Catheter versus graft | 1.38 (1.25–1.52) | 86.2%; <0.01 | 91 (60–125) excess with catheter |
| 0.20 for fistula users | Graft versus fistula | 1.18 (1.09–1.27) | 82.1%; <0.01 | 36 (18–54) excess with graft |
| Major cardiovascular events | ||||
| 0.10 for fistula users | Catheter versus fistula | 1.38 (1.24–1.54) | 0%; 0.47 | 38 (24–54) excess with catheter |
| 0.11 for graft users | Catheter versus graft | 1.26 (1.11–1.43) | 0%; 0.57 | 28 (12–46) excess with catheter |
| 0.10 for fistula users | Graft versus fistula | 1.07 (0.95–1.21) | 0%; 0.52 | 7 (−5–21)b excess with graft |
| Fatal infections | ||||
| 0.03 for fistula users | Catheter versus fistula | 2.12 (1.79–2.52) | 0%; 0.82 | 28 (20–38) excess with catheter |
| 0.04 for graft users | Catheter versus graft | 1.49 (1.15–1.93) | 0%; 0.23 | 17 (5–32) excess with catheter |
| 0.03 for fistula users | Graft versus fistula | 1.36 (1.17–1.58) | 0%; 0.78 | 9 (4–15) excess with graft |
Outcome measure includes all-cause mortality, fatal or nonfatal cardiovascular events, and fatal infection events as defined in each study, with RRs obtained from the meta-analysis. Reference risks are from the United States Renal Data System.1
The 95% CI includes negative numbers, indicating that the superiority of graft versus fistula for cardiovascular events is uncertain (the 95% CI ranges between 5 fewer events and 21 in excess with grafts).
Colonization of foreign material within the vascular space by skin micro-organisms causing infection and bacteremia may directly lead to hospitalization, access failure, and death, and it may explain, in part, the mechanism by which catheter and graft use may be associated with poorer survival.15 In addition, chronically colonized surface biofilm in synthetic access-related material may increase the risk of cardiovascular disease in persons on hemodialysis by inflammation.16 In support of this hypothesis, we found that use of grafts and catheters was associated with stronger risks of infection and hospitalization compared with fistulas. The proportion of access-related fatal infections in available studies was not reported, and in one study, only 23% of all infection-related hospitalizations were considered directly caused by access infection,17 suggesting that catheter and graft colonization does not entirely explain the increased mortality, infection, and hospitalization associated with these access types. In addition, rates of bacteremia are 10 times higher in observational studies than they are in clinical trials,11 suggesting that, in observational studies, persons with poorer prognosis (including those individuals who start dialysis acutely) are over-represented among catheter users; this finding may explain the adverse outcomes observed in persons using catheters.
Although the associations between vascular access type and adverse patient outcomes are large and consistent in available studies, this review highlights that data for outcomes associated with vascular access are substantially biased by treatment selection. Persons who receive a fistula that matures sufficiently for dialysis are likely to differ in important ways from persons for whom a fistula cannot be established before dialysis initiation because of insufficient predialysis planning, inadequate vascular anatomy, or short life expectancy.18 Patient characteristics that drive clinical decisions about vascular access insertion (e.g., poor prognosis, heart failure, or peripheral vascular disease) also influence patient survival, regardless of the vascular access type achieved. Fistulas have a high risk of maturation failure, often require several interventions to attain suitability for hemodialysis, and are frequently impossible or not attempted in persons with poor prognosis. Accordingly, in the context of treatment selection bias, our data show that persons who can successfully have a fistula created and used have better clinical outcomes, but the relative benefits and harms of access strategies for other persons remain uncertain. Although guidelines strongly promote the fistula as the first and optimal access type for all persons starting or treated with hemodialysis, insufficient information is available to evaluate the merits of this strategy. Given that approximately 40% of fistulas fail to attain maturity for dialysis and may require repetitive interventions to achieve function, indiscriminately recommending fistula first may result in inappropriate use of resources and services.19
Given the methodological limitations in available studies primarily caused by selection bias, additional research is necessary to inform clinical practice when caring for a person for whom a fistula may not be appropriate or possible. Selection bias in the current evidence cannot be addressed by statistical techniques that control for known and measured confounders.20 Observational studies that evaluate patient outcomes based on treatment intent (comparing outcomes of persons in whom a fistula is the first approach, regardless of whether a fistula is achieved, with the outcomes of persons for whom a graft or catheter is the first treatment option) may provide relevant additional data. Although a large randomized trial comparing fistula versus grafts or catheters in all incident hemodialysis persons may not be considered appropriate or feasible before such information is available, equipoise may already exist as to whether early consideration of an arteriovenous graft or central venous catheter would be noninferior or even superior to fistula prioritization strategies in persons at high risk (or prior history) of fistula maturation failure.
This study has strengths, including rigorous methodology, the magnitude and consistency of the associations that we observed, and its relevance to current practice and policy-making, but it also has important limitations, primarily because of the primary source data. First, our conclusions are supported by low-quality evidence from observational studies that are vulnerable to confounding by measured and unmeasured variables. We used univariate metaregression to control for confounding by risk of bias. Associations found in larger and more recent studies were weaker. Study-level adjustment for confounding variables did not materially alter risk estimates, suggesting that residual confounding (particularly from patient selection) was likely present.21 Second, we found large between-study heterogeneity, indicating that associations significantly varied between studies. We controlled for specific study and participant characteristics, but we could not explain residual heterogeneity. Despite marked heterogeneity, the direction of association with mortality was consistent in 49 of 51 (96%) comparisons, with higher risks in catheter users than users of arteriovenous accesses and higher risks in graft users than fistula users. Finally, although data suggest that achieving a fistula or graft improves clinical outcomes, we could not identify specific patient characteristics that might predict smaller absolute benefits of a fistula instead of a graft or catheter, leaving open the question of who may or may not benefit from aggressive fistula promotion.
In summary, several important clinical outcomes are associated with the type of vascular access used for hemodialysis. The strongest associations with adverse events are observed in persons using catheters, with the lowest risk being observed in persons using fistulas. Available evidence is profoundly limited by selection bias. Given the high mortality rate of hemodialysis patients and the potential impact of vascular access on clinical outcomes, additional research should now focus on defining the characteristics of patient populations, where equipoise may exist between different access options, including patients who do not achieve a functioning fistula. Clinical trials evaluating the impact of different access strategies on clinical outcomes in such populations should be a research priority.
Concise Methods
Data Sources and Searches
We systematically searched MEDLINE and EMBASE (from inception to September 25, 2012) without language restriction using search strategies designed by a specialist librarian (Supplemental Table 6). We also hand-searched the reference lists of all identified relevant publications and contacted experts in the field. Citations were independently screened for eligibility by two reviewers based on title and abstract. We retrieved the full text of any study that seemed relevant or when there was uncertainty as to the eligibility based on title and abstract alone. Two reviewers then independently selected studies fulfilling the inclusion criteria based on full-text review.
Study Selection
We included cohort studies published in any language comparing types of hemodialysis access (two or more of fistula, graft, or catheter) in persons treated with or planning to shortly commence hemodialysis that reported any of the following relevant person outcomes: all-cause mortality, fatal or nonfatal cardiovascular events, fatal or nonfatal infection, and all-cause hospitalization. We used broad inclusion criteria for studies, including varying definitions for vascular access (e.g., any configuration and location of fistulas and grafts and any material and structure of grafts and catheters). We included clinical events as defined by the investigators. We excluded narrative review articles and original articles that reported only vascular access outcomes and studies comparing outcomes by subtypes of the same access category (e.g., femoral versus jugular venous catheters, side-to-side versus end-to-side fistulas, and synthetic versus bovine grafts).
Data Extraction and Quality Assessment
Two independent reviewers extracted, classified, and coded data for baseline characteristics (age, time on dialysis, sex, and prevalence of diabetes and cardiovascular disease), vascular access type (fistula, graft, or catheter) and subtype (temporary and permanent catheters, femoral and jugular or subclavian location, synthetic and native vessel graft, and proximal or distal location of the fistula), and study design (publication year, study size, duration of follow-up, prospective collection of data, inclusion or exclusion of prevalent patients, exposure defined as the access in use at hemodialysis commencement versus after 3 months, and exposure defined as the access at initial follow-up versus time-varying access) using standardized data extraction forms. Two independent authors also evaluated the risk of bias in included studies, exploring domains of participation, selection, or attrition, exposure and outcome measurement, confounding, and analysis bias using previously validated methods22,23 (Supplemental Table 6). Whenever more than one publication provided data from the same cohort population, we included in the analyses only data from the larger study or the study with the most complete data to avoid data duplication. Disagreements were resolved by discussions with two authors (P.R. and M.T.J.) that were arbitrated by a third author (G.F.M.S.).
Statistical Approach
We defined the exposure as the type of vascular access. We prespecified analyses for outcomes comparing catheter versus fistula, graft versus catheter, and fistula versus graft. The primary outcome was all-cause mortality. Secondary outcomes were fatal and nonfatal cardiovascular events (myocardial infarction, congestive heart failure, and stroke), fatal and nonfatal infection, and all-cause hospitalization. We extracted RRs, incidence rate ratios, hazard ratios, or odds ratios for the association between vascular access type and outcomes. We calculated risks when only crude event data were reported. We added 0.5 to all 2 × 2 table cells with a zero count. When only P values were reported, we calculated 95% CIs by deriving the standard errors of the log-RRs from the two-sided P value. We selected the results from full statistical models that adjusted for the largest number of potential confounders. We pooled the natural logarithm of RRs for dichotomous outcomes across studies using the random effects model by DerSimonian and Laird.24 We used standard methods to convert point estimates and variances of odds ratios to RRs.25,26 When two comparisons were reported for an outcome in a study, we derived the third mathematically. When reported, we extracted and analyzed risk estimates separately for clinically important subgroups (e.g., persons with and without diabetes and incident and prevalent dialysis patients). We used the I2 statistic27,28 to test for heterogeneity in risk estimates between studies. We did additional prespecified subgroup and random effects univariate metaregression to explore heterogeneity between risk estimates in individual studies according to each of the following study-level covariates: age, sex, prevalence of diabetes, follow-up duration, sample size, publication year, inclusion of prevalent patients, definition of the exposure based on the vascular access at 3 months after dialysis initiation (as opposed to access at commencement of hemodialysis), outcome models built on time-varying access versus initial access, subtype of access within each comparison (temporary or tunneled catheters, proximal or distal fistulas, and bovine or synthetic graft), and risk of bias. For comparative and subgroup analyses, we required a minimum of three independent estimates per group to justify analyses. We used standard methods to detect and quantify publication bias.29,30 Because studies provided several risk estimates using different statistical models, subgroups, or published versions, we did sensitivity analyses by including these multiple risk estimates from the same data source in separate pooled analyses. We also repeated analyses and excluded studies enrolling participants who required complex surgical procedures, children, or HIV-positive persons. We did all analysis using R (packages ‘meta’ and ‘metafor’; http://CRAN.R-project.org/).
Disclosures
None.
Acknowledgments
The authors thank Ms. Diane Lorenzetti (librarian) and Ms. Divya Karsanji and Ms. Wendy Spragins (research assistants) from the University of Calgary for assistance with preparation of this study. The authors also thank Mr. Dykeman and Mr. Lowerison for technical support for figure preparation in R.
This work was supported by a grant from the University of Calgary, Division of Nephrology, awarded to P.R. and M.T.J. and an unrestricted educational grant from Diaverum, a provider of renal services.
Part of this work has been presented in the form of an abstract at the American Society of Nephrology Meeting held in San Diego, California, October 30 to November 4, 2012.
The funding sources had no role in any stage of the design and conduct of the study, the collection, management, analysis, and interpretation of data in the study, or the preparation, review, or approval of the manuscript.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
This article contains supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2012070643/-/DCSupplemental.
References
- 1.United States Renal Data System : Annual Data Report, 2011. Available at: http://www.usrds.org/adr.aspx Accessed April 20, 2012
- 2.Besarab A: Resolved: Fistulas are preferred to grafts as initial vascular access for dialysis. Pro. J Am Soc Nephrol 19: 1629–1631, 2008 [DOI] [PubMed] [Google Scholar]
- 3.Vascular Access 2006 Work Group : Clinical practice guidelines for vascular access. Am J Kidney Dis 48[Suppl 1]: S176–S247, 2006 [DOI] [PubMed] [Google Scholar]
- 4.Jindal K, Chan CT, Deziel C, Hirsch D, Soroka SD, Tonelli M, Culleton BF, Canadian Society of Nephrology Committee for Clinical Practice Guidelines : Hemodialysis clinical practice guidelines for the Canadian Society of Nephrology. J Am Soc Nephrol 17[Suppl 1]: S1–S27, 2006 [DOI] [PubMed] [Google Scholar]
- 5.Tordoir J, Canaud B, Haage P, Konner K, Basci A, Fouque D, Kooman J, Martin-Malo A, Pedrini L, Pizzarelli F, Tattersall J, Vennegoor M, Wanner C, ter Wee P, Vanholder R: EBPG on vascular access. Nephrol Dial Transplant 22[Suppl 2]: ii88–ii117, 2007 [DOI] [PubMed] [Google Scholar]
- 6.The AV Fistula First Breakthrough Initiative Coalition: Arteriovenous Fistula First Website, 2012. Available at: http://www.fistulafirst.org Accessed April 20, 2012
- 7.Healthy People—US Department of Health & Human Services Public Health Service: Topics and Objectives 2020 CKD-11: Improving Vascular Access for Hemodialysis Patients, 2012. Available at: http://healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=6 Accessed April 20, 2012
- 8.NHS: Payment by Results (PbR)—Renal Dialysis, 2012. Available at: http://www.kidneycare.nhs.uk/document.php?o=574 Accessed April 20, 2012
- 9.Dember LM, Beck GJ, Allon M, Delmez JA, Dixon BS, Greenberg A, Himmelfarb J, Vazquez MA, Gassman JJ, Greene T, Radeva MK, Braden GL, Ikizler TA, Rocco MV, Davidson IJ, Kaufman JS, Meyers CM, Kusek JW, Feldman HI, Dialysis Access Consortium Study Group : Effect of clopidogrel on early failure of arteriovenous fistulas for hemodialysis: A randomized controlled trial. JAMA 299: 2164–2171, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ethier J, Mendelssohn DC, Elder SJ, Hasegawa T, Akizawa T, Akiba T, Canaud BJ, Pisoni RL: Vascular access use and outcomes: An international perspective from the Dialysis Outcomes and Practice Patterns Study. Nephrol Dial Transplant 23: 3219–3226, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lok CE: Fistula first initiative: Advantages and pitfalls. Clin J Am Soc Nephrol 2: 1043–1053, 2007 [DOI] [PubMed] [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, Altman DG: Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann Intern Med 151: 264–269, 2009 [DOI] [PubMed] [Google Scholar]
- 13.García Cortés MJ, Viedma G, Sánchez Perales MC, Borrego FJ, Borrego J, Pérez del Barrio P, Gil Cunquero JM, Liébana A, Pérez Bañasco V: Fistulae or catheter for elderly who start hemodialysis without permanent vascular access? Nefrologia 25: 307–314, 2005 [PubMed] [Google Scholar]
- 14.Hazinedaroğlu SM, Tüzüner A, Ayli D, Demirer S, Duman N, Yerdel MA: Femoral vein transposition versus femoral loop grafts for hemodialysis: A prospective evaluation. Transplant Proc 36: 65–67, 2004 [DOI] [PubMed] [Google Scholar]
- 15.Jones SM, Ravani P, Hemmelgarn BR, Muruve D, Macrae JM: Morphometric and biological characterization of biofilm in tunneled hemodialysis catheters. Am J Kidney Dis 57: 449–455, 2011 [DOI] [PubMed] [Google Scholar]
- 16.Wasse H, Speckman RA, McClellan WM: Arteriovenous fistula use is associated with lower cardiovascular mortality compared with catheter use among ESRD patients. Semin Dial 21: 483–489, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Allon M, Depner TA, Radeva M, Bailey J, Beddhu S, Butterly D, Coyne DW, Gassman JJ, Kaufman AM, Kaysen GA, Lewis JA, Schwab SJ, HEMO Study Group : Impact of dialysis dose and membrane on infection-related hospitalization and death: Results of the HEMO Study. J Am Soc Nephrol 14: 1863–1870, 2003 [DOI] [PubMed] [Google Scholar]
- 18.Ravani P, Barrett B, Mandolfo S, Brunori G, Cancarini G, Imbasciati E, Malberti F: Factors associated with unsuccessful utilization and early failure of the arterio-venous fistula for hemodialysis. J Nephrol 18: 188–196, 2005 [PubMed] [Google Scholar]
- 19.Palmer SC, McGregor DO, Macaskill P, Craig JC, Elder GJ, Strippoli GF: Meta-analysis: Vitamin D compounds in chronic kidney disease. Ann Intern Med 147: 840–853, 2007 [DOI] [PubMed] [Google Scholar]
- 20.Palmer SC, Strippoli GF: How to read critically a prognostic cohort study. Nephrology (Carlton) 15: 676–682, 2010 [DOI] [PubMed] [Google Scholar]
- 21.Ioannidis JP, Haidich AB, Pappa M, Pantazis N, Kokori SI, Tektonidou MG, Contopoulos-Ioannidis DG, Lau J: Comparison of evidence of treatment effects in randomized and nonrandomized studies. JAMA 286: 821–830, 2001 [DOI] [PubMed] [Google Scholar]
- 22.Hayden JA, Côté P, Bombardier C: Evaluation of the quality of prognosis studies in systematic reviews. Ann Intern Med 144: 427–437, 2006 [DOI] [PubMed] [Google Scholar]
- 23.Busse J, Guyatt G: An instrument for assessing risk of bias in cohort studies, 2012. Available at: http://www.evidencepartners.com/resources/ Accessed April 20, 2012
- 24.DerSimonian R, Laird N: Meta-analysis in clinical trials. Control Clin Trials 7: 177–188, 1986 [DOI] [PubMed] [Google Scholar]
- 25.Zhang J, Yu KF: What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA 280: 1690–1691, 1998 [DOI] [PubMed] [Google Scholar]
- 26.Miettinen O: Estimability and estimation in case-referent studies. Am J Epidemiol 103: 226–235, 1976 [DOI] [PubMed] [Google Scholar]
- 27.Higgins JP, Thompson SG: Quantifying heterogeneity in a meta-analysis. Stat Med 21: 1539–1558, 2002 [DOI] [PubMed] [Google Scholar]
- 28.Higgins JP, Thompson SG, Deeks JJ, Altman DG: Measuring inconsistency in meta-analyses. BMJ 327: 557–560, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Begg CB, Mazumdar M: Operating characteristics of a rank correlation test for publication bias. Biometrics 50: 1088–1101, 1994 [PubMed] [Google Scholar]
- 30.Duval S, Tweedie R: Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56: 455–463, 2000 [DOI] [PubMed] [Google Scholar]
- 31.Polkinghorne KR, McDonald SP, Atkins RC, Kerr PG: Vascular access and all-cause mortality: A propensity score analysis. J Am Soc Nephrol 15: 477–486, 2004 [DOI] [PubMed] [Google Scholar]
- 32.Foley RN, Chen SC, Collins AJ: Hemodialysis access at initiation in the United States, 2005 to 2007: Still “catheter first”. Hemodial Int 13: 533–542, 2009 [DOI] [PubMed] [Google Scholar]