Abstract
Background
Recent studies have demonstrated that trunk control likely plays a role in anterior cruciate ligament (ACL) injury. Yet, the majority of ACL research remains focused on the lower limb, with limited information on the trunk position at the time of injury.
Hypotheses
Athletes experiencing a non-contact ACL-injury, after a one-legged landing, position their center-of-mass (COM) more posterior from the base-of-support (BOS) at initial ground contact, in comparison to uninjured athletes. The distance from the COM to the BOS (COM_BOS) is larger in female, as compared to male, athletes during one-legged landing.
Study Design
Case control study; Level of evidence, 3
Methods
Movie captures of 20 athletes performing a one-legged landing maneuver, resulting in a torn ACL were compared to matched (for gender, sport, and activity just prior to landing) movie captures of 20 athletes performing a similar maneuver that did not result in an ACL disruption (controls). The COM_BOS, trunkG angle, and limbG angle (both relative to the gravity vector) were measured in the sagittal plane at initial ground-foot contact. A two-way ANOVA (injury_status×gender) were used to examine the hypotheses.
Results
There was a significant difference in all 3 measures based on injury_status, but not on gender. COM_BOS, normalized by femur length, and limbG angle were greater (Δ=0.9, p<0.001 and Δ=16°, p=0.004, respectively) and the trunkG angle was smaller (12°, p=0.016) in the subjects that sustained an ACL-injury as compared to controls. The average COM was calculated as 38 cm more posterior relative to the BOS in the subjects who sustained an ACL-injury as compared to controls.
Conclusions
Landing with the COM far posterior to the BOS may be a risk factor for noncontact ACL-injury and potentially can be addressed in prevention programs.
Keywords: ACL-injury, injury prevention, gender differences
INTRODUCTION
Anterior cruciate ligament (ACL)-injuries are typically sports related, occur in active healthy young adults (15–24 years old), involve expensive intervention with long recoveries, and result in many athletes losing knee function and quality of life24,26,31. For these reasons a sustained and extensive research effort has been put forth to identify the risk factors associated with ACL-injuries as a first step in trying to prevent them2. This efforts has tended to focus on the lower limb5,11,15,27,30,37, yet more recent work has begun to focus on trunk orientation and control4,20,30,38.
The control of sagittal-plane trunk position may play a key role in ACL-injury, as it is central to balance control. The importance of trunk control in ACL-injury is evidenced by the phantom-foot mechanism in skiing, which partially attributes ACL-injury to a strong quadriceps contraction13. This mechanism was tested using a 2D sagittal plane model of landing during high-speed downhill skiing14. When a small balance disturbance caused a slight backwards fall, ACL forces large enough to cause failure were seen during the model’s attempt to restore balance. A recent descriptive videotape study supported this finding in noting that athletes who sustained an ACL-injury were leaning backwards at the time of injury7. Blackburn and Padua4 demonstrated that increased trunk extension (measured as the angle between the trunk and the thigh) during a two-legged drop landing increased the ground reaction and quadriceps forces. Similarly, Kulas and colleagues20 demonstrated that subjects who increased trunk extension (measured as the angle between the trunk and vertical line) in response to an additional trunk load during a 2-legged drop-test , implemented a quadriceps dominant strategy (i.e, there was an increase in quadriceps and a decrease in hamstring forces) upon landing. These 2D sagittal plane studies indicate that when the trunk is more extended during a landing maneuver, the quadriceps are recruited in an attempt to maintain balance.
In opposition to these modeling and lab-based studies, an earlier video-based study8 found that the hip angle (measured as the angle between the trunk and the thigh) was significantly more flexed at foot contact during a one-legged landing maneuver that resulted in an ACL disruption (provocative landing position), as compared to a safe landing position. Therefore, the actual orientation of the trunk relative to the leg may not be as important as the position of the trunk relative to the foot, which is influenced not only by the trunk angle, but the hip, knee, and ankle angles as well. If the gravitational vector from the body’s center of mass (COM, approximately located at the center of the trunk) does not lie within the base of support (BOS) then static posture is unstable18,19. In order to avoid a fall, the body’s posture must be altered so that the COM falls within the BOS. In a dynamic situation, the COM can fall outside the BOS, but if the distance is too great, then recovery is no longer possible, resulting in a fall.
This study tested the hypothesis that the distance from the COM to the BOS (COM_BOS) was larger at the time of initial ground contact in the provocative, as compared to the safe, landing position. In addition, the hypothesis that limb angle relative to vertical (limbG angle) was larger, but trunk angle relative to vertical (trunkG angle) was no different, in the provocative, as compared to the safe, landing position was also tested. The analysis was limited to the sagittal plane, as the trunk position in the frontal plane had previously been reported17. Since female athletes tend to injure their ACL more frequently than their male counterparts3 a tertiary hypothesis was tested: The COM_BOS and limb angle were larger in the female athletes as compared to the male athletes, during a one-legged landing maneuver.
METHODS
Twelve videotapes of athletes captured during an ACL-injury, acquired for a previous study8, formed the basis of the current study. Sixteen additional movies in digital format were acquired from collaborators and the public domain. For a video or movie clip to be included within the study it had to meet previously published inclusion criteria8. The same author (AU3) assessed both the original videos, as well as the additional movie clips (eight additional movie clips met the inclusion criteria), resulting in a total of 20 movie clips of athletes performing a one-legged landing maneuver that resulted in an ACL-injury (Table 1). All ACL-injuries were confirmed based on the medical record, except two. These two videos were acquired directly from the public domain and the ACL-injury was confirmed through media reports. The same author (AU3) assessed fifty sagittal view videotapes (12 were from a previous study8) or digital movie clips of athletes (controls) performing similar decelerating or landing maneuvers during game situations that did not result in an ACL tear (32 met the inclusion criteria). The activity being performed just prior to ground contact was categorized into one of three activities: 1) stopping from a run (run-stop), 2) a vertical jump, or 3) a horizontal jump. From these 32 control clips, 20 were selected so that the controls were matched for gender, sport, and activity just prior to landing. To lessen any potential for selection bias, the matching was done without reference to the video data and the athletes’ landing position did not factor into the acceptance or rejection of the video clip anytime during the selection process. This study was exempt from institutional review board approval, as assessed by the IRB of the National Institutes of Child Health and Human Services, NIH, as all movies were in the public domain.
Table 1. Study Participant Descriptions.
Differences between the two cohorts were tested using a two-tailed Chi-squared test.
| Injured | Controls | p-value | ||
|---|---|---|---|---|
| Gender | female male |
13 7 |
13 7 |
1.0 |
| Sport | basketball soccer football handball |
10 2 5 3 |
10 2 5 3 |
1.0 |
| Activity just prior to analysis |
run-stop vertical horizontal jump |
15 2 3 |
17 2 1 |
0.45 |
The video recordings and digital movies were edited using Adobe Premiere Pro (version 2.0, Adobe Systems, Inc., San Jose, CA) and iMovie HD (Apple, Cupertino, CA), respectively. For each movie the frame in which the foot initially contacted the ground (initial contact) was captured and stored for analysis. This frame was distinguished from the series of frames capturing foot fall, by having a least a single point on the foot stop its downward progression. Image J (National Institutes of Health, Bethesda, MD) was used for all measurements. For consistency, a single author (AU2), who was not involved in assessing the video quality, performed all measures. Four months after the initial analysis, the measures were repeated by AU2, who was blinded to the initial results.
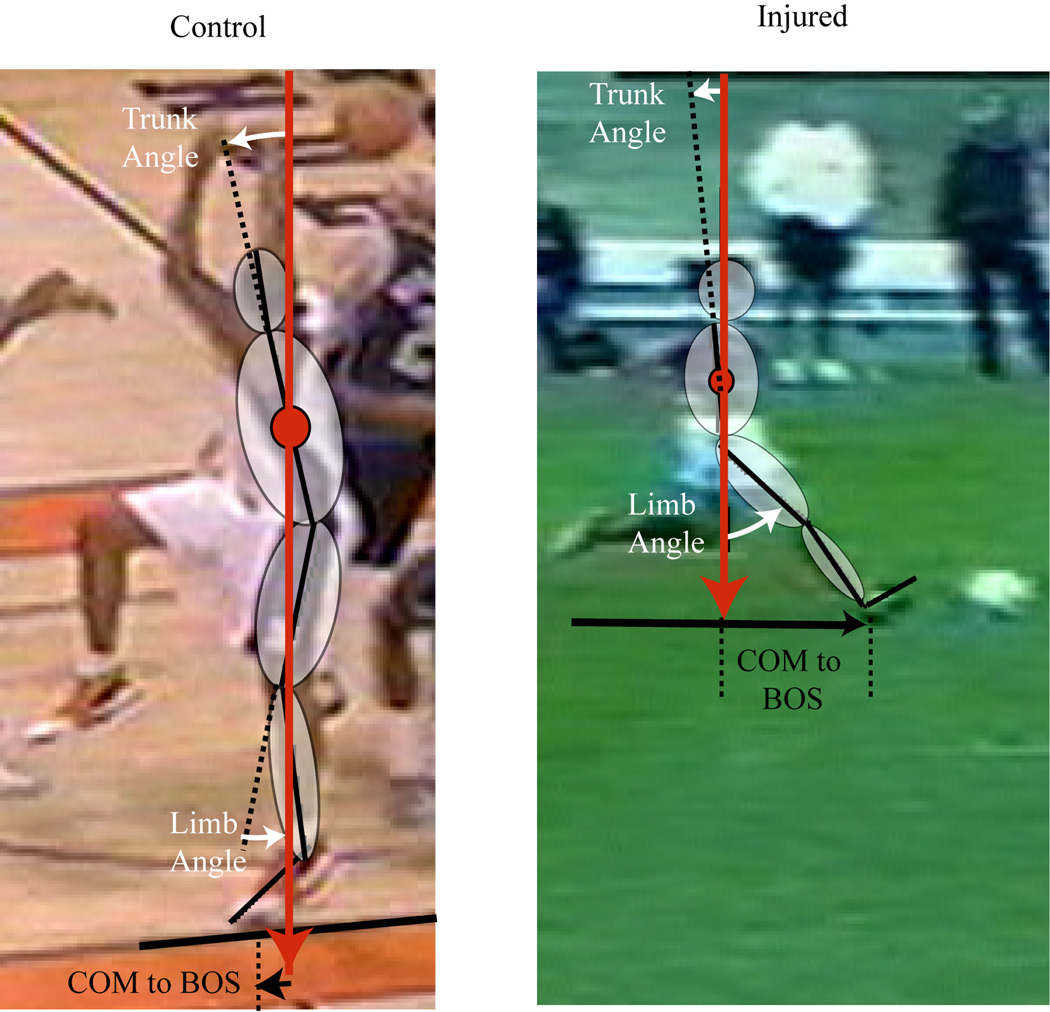
The first measure of interest was the COM_BOS. The COM was defined as the center of an ellipse delineating the athlete’s trunk (Figure 1). The major axis was the centerline of the trunk (represented as the line from the center of the hip joint to the center of the shoulder joint) and the minor axis ran from the anterior to the posterior aspect of the trunk. The BOS was defined as the point bisecting the line of contact between the shoe and the floor at initial contact. To account for small variations in camera angle across images, perpendicular lines on the field of play (e.g., the key in basketball) were used to denote the anterior and medial directions relative to the athlete. The COM_BOS (in pixels) was then taken along the anterior/posterior direction. Since the conversion from pixels to mm was not available, the COM_BOS was normalized by femur length (measured from the center of the knee joint to the center of the hip joint), which was measured from the identical image as the COM_BOS. This scaling accounted for the variations in magnification factors and variations in subject height. In addition, any slight rotation of the athlete away from the sagittal plane would have resulted in a foreshortening of the COM_BOS (by the cosine of the out-of-plane rotation angle). A similar foreshortening of the femur_length would have also occurred. Thus, dividing the COM_BOS by the femur_length minimized this error. Femur length was chosen over subject height as the scaling factor, because this single measure was not prone to cumulative measurement errors and has been correlated with body height21. Two angles (trunkG and limbG) were also measured. The trunkG angle was defined as the angle from the vertical to the centerline of the trunk. The limbG angle was defined as the angle between the vertical and the thigh (represented as the line from the center of the knee joint to the center of the hip joint). A positive trunkG and/or limbG angle indicated that the trunk and/or limb was rotated anteriorly relative to vertical.
Figure 1. Analysis of Control Landing (left) and landing that was proceeded by an ACL-injury (Right).
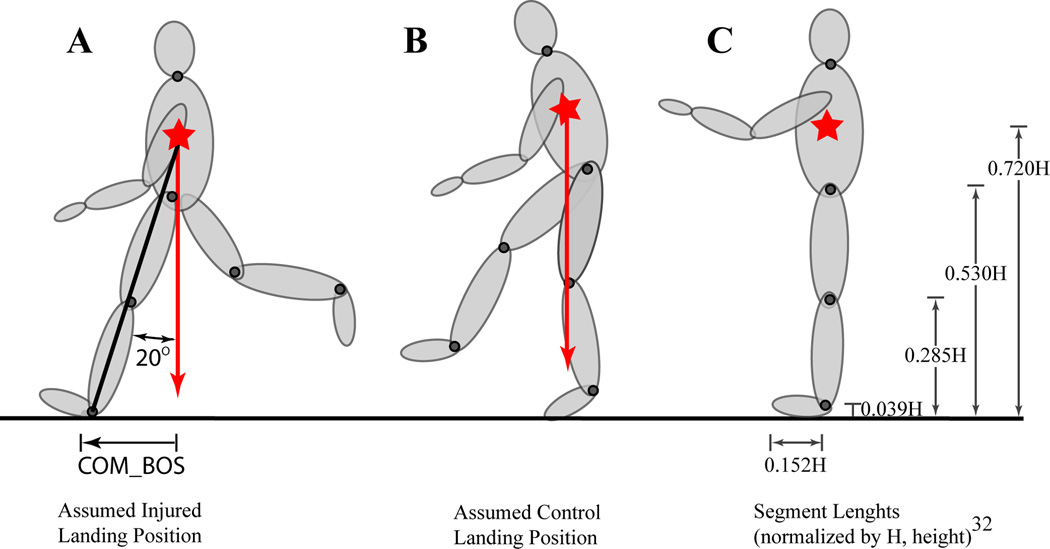
An a priori power analysis revealed that seven subjects were needed for both the injured and control groups (alpha = 0.05, beta = 0.80). This was based on the assumption that the difference in the COM_BOS between the injured and control populations would be 0.246*height (Figure 2), and that the variation in both populations would be equal to 75% of the average value of COM_BOS. Thus, the original video tapes8 (ninjured = 12 and ncontrol = 12) were sufficient to test the main hypothesis, but the additional digital videos were added in order to match the two cohorts and investigate difference across subpopulations.
Figure 2. Power Analysis.
A: Assumed provocative landing position: In order to perform the power calculations it was assumed that the line between the hip and the heel is 20° from the vertical (gravitational direction). Then the COM_BOS was calculated as the distance from the COM to the heel of the foot multiplied by the sin of 20° (0.246*H = 0.720*H * sin (20°)). B. Assumed safe landing position: In the control position, it was assumed that that the COM was directly over the BOS. C: Segment Lengths: Segment lengths normalized by height as provided by Winter36. The key measurements used in the current study:
Trunk_to_heel = 0.720H
Femur_length = 0.245H = (0.530H-0.285H)
Foot Length = 0.152H
Foot Length = .0.618*femur_length = 0.152H*(femur_length/0.246H)
A two-way analysis of variance (2×2 ANOVA, SPSS 15.0, IBM Corporation, Somers, NY) was used to assess main and interaction effects of injury_status and gender on three variables (COM_BOS, limbG angle, and trunkG angle). Intraclass correlation coefficients, using a two-way mixed effects model, were used to examine intra-rater reliability. A discriminant analysis determined if any single variable could distinguish injury_status. A p-value less than 0.05 was considered significant.
RESULTS
Matching was completely successful for the first two criteria (Table 1). But due to the difficulty in obtaining control movie clips that fit the inclusion criteria, two controls categorized as horizontal jump were matched with 2 injured subjects categorized as run-stop (all other parameters matched). No significant differences in any of the matching criteria were found between groups.
For the COM_BOS, limbG angle, and trunkG angle, the intraclass correlations coefficients were 0.956 (95% CI: 0.917-0.977), 0.988 (95% CI: 0.977-0.994), and 0.967 (95% CI: 0.937-0.983), respectively.
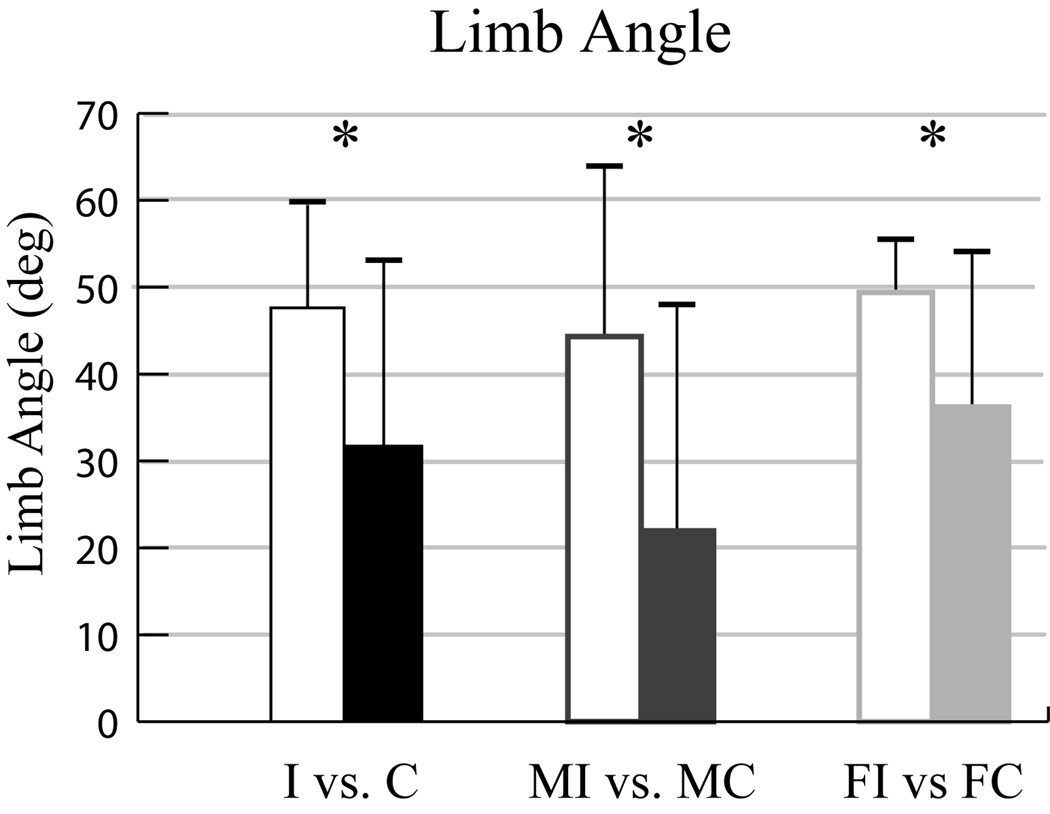
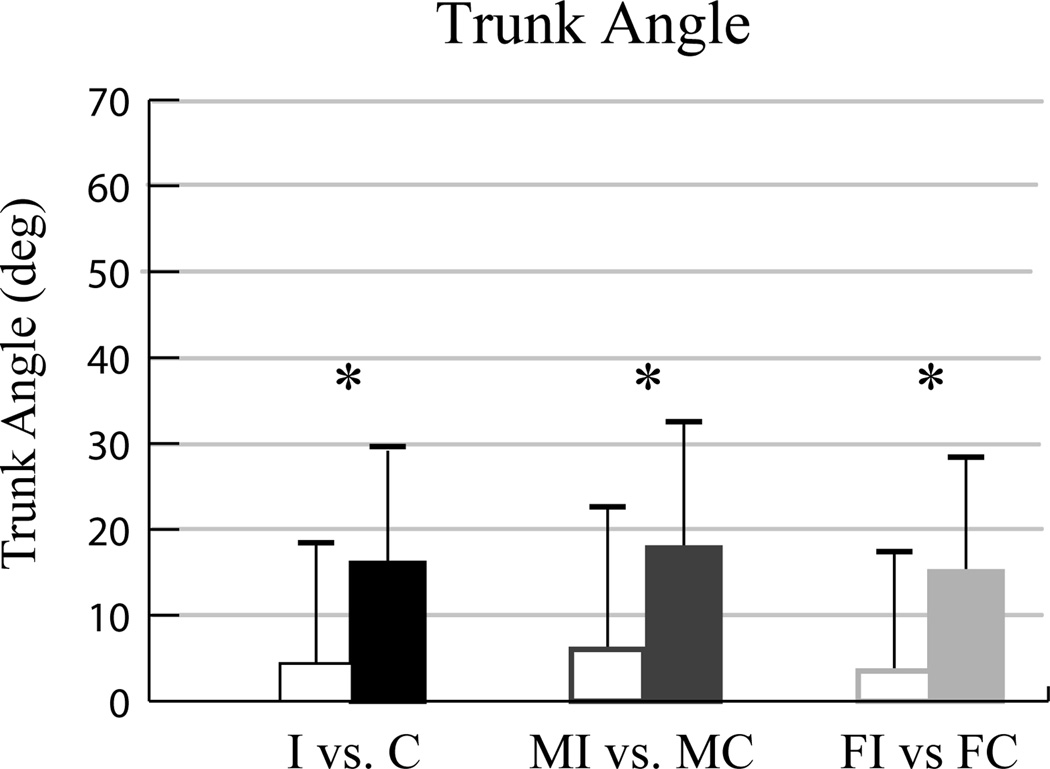
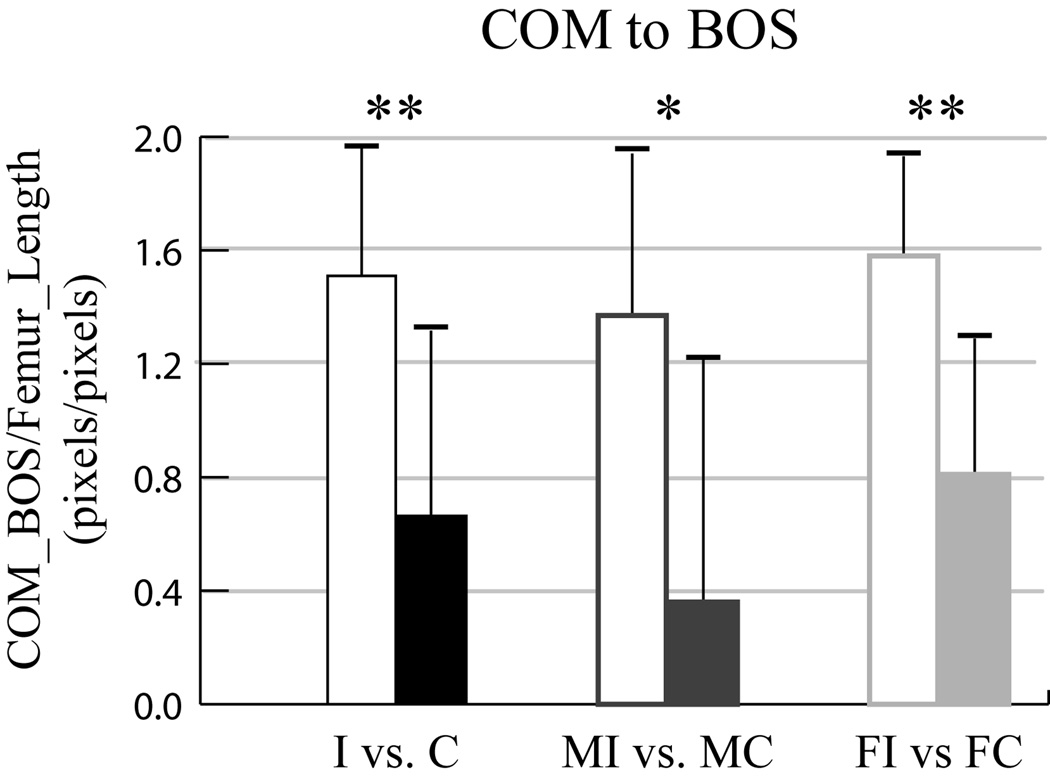
Injury_status was a significant main effect for COM_BOS, limbG angle, and trunkG angle (Table 2). The COM_BOS, normalized by femur length, was greater in the ACL-injured population (Δ=0.9, p <0.001, Figure 3). If an average height of 177.8 cm (5’ 10”) and a femur length of 0.245*height (Figure 2) is assumed for both groups, then on average the COM was 38 cm more posterior relative to the BOS in the subjects who sustained an ACL-injury as compared to controls [177.8*0.245*(COM_BOSControls - COM_BOSInjured), Table 2]. The limbG angle (Figure 4) was greater (Δ=16°, p=0.004) and the trunkG angle (Figure 5) was smaller (Δ=12°, p=0.016) in the ACL-injured, as compared to the control, population. Interestingly, the same trends existed if each sport was evaluated separately, but due to power issues, significant differences were only found for basketball.
Table 2. Results.
All values are listed as an average ± one standard deviation (SD). The 2×2 design ANOVA indicated that injury_status was a significant factor, but gender was not and there were no interaction effects.
| INJURED | CONTROLS | |||||
|---|---|---|---|---|---|---|
| ALL | Male | Female | ALL | Male | Female | |
| COM_BOS /femur | 1.5 ± 0.5 | 1.4 ± 0.6 | 1.6 ± 0.4 | 0.7 ± 0.7 | 0.4 ± 0.9 | 0.8 ± 0.5 |
| Limb Angle (deg) | 48 ± 12 | 44 ± 19 | 49 ± 6 | 31 ± 22 | 22 ± 26 | 36 ± 18 |
| Trunk Angle (deg) | 4 ± 14 | 6 ± 17 | 4 ± 14 | 16 ± 13 | 18 ± 14 | 15 ± 13 |
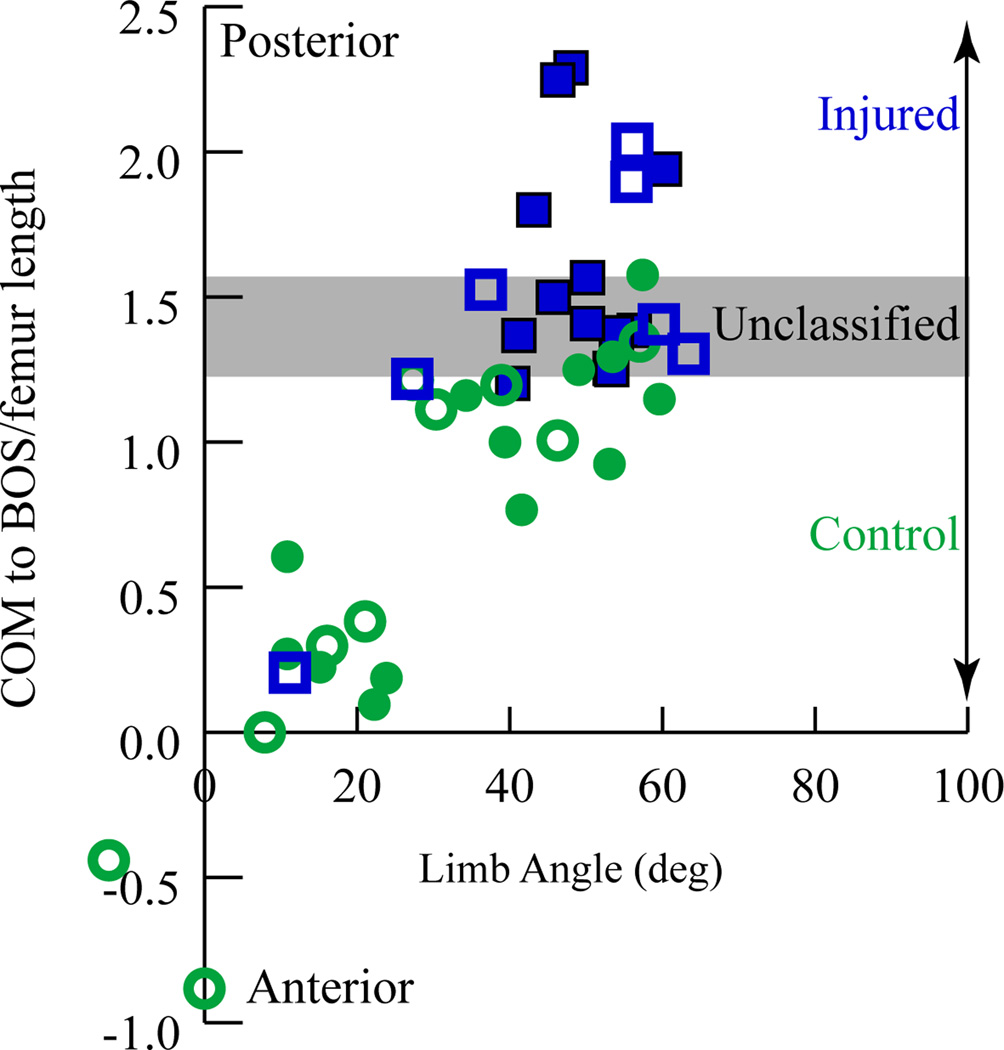
Figure 4. LimbG relative to the gravitational vector.
I = injured C= Controls, M = males, F= Females. Injury status was a significant main effect (p=0.004), but gender was not (p=0.098). There were no significant interaction effects (p=0.425).
Figure 5. TrunkG angle relative to the gravitational vector.
I = injured C= Controls, M = males, F= Females. Injury status was a significant main effect (p=0.016), but gender was not (p=0.571). There were no significant interaction effects (p=0.980).
Gender was not a significant main effect for any variable and there was no interaction effect between injury_status and gender for any of the three variables of interest. Specifically, differences did not exist when comparing male versus female athletes within or across the two cohorts.
The value of COM_BOS discriminated between athletes who sustained an ACL-injury and athletes that did not with 80% accuracy (Figure 6, Wilks’ Lamba, p<0.001). The limbG angle did less well in discriminating the groups (72%), whereas the trunkG angle could not discriminate the groups (70%). Using a combination of these variables did not improve the accuracy of discrimination.
Figure 6. Discriminant Analysis.
COM_BOS plotted versus limbG angle. The data from athletes who sustained an ACL-injury are represented by blue squares. The subjects in the control group are represented by green circles. Hollow symbols represent male subjects and filled symbols represent female subjects. The discriminant analysis determined that COM_BOS could predict membership in a group to within 80% accuracy (1 injured case and 7 control cases were misclassified). Neither the limbG nor the trunkG angle could discriminate to the same level.
DISCUSSION
This study demonstrates that having the COM far posterior to the BOS, a large limbG angle, and a small trunkG angle at initial ground contact are important components of the noncontact ACL-injury mechanism. These results extend our previously defined provocative and safe landing positions8 in the sagittal plane. In the provocative position, the athletes tend to land flat-footed, with the hip flexed, knee extended, and the COM far posterior to their BOS. In the safe position, athletes land on their forefoot with the hip in a neutral position, the knee slightly more flexed, and the COM close to the BOS, based on a sagittal plane analysis. These results may be useful in screening athletes who are at risk for ACL-injury and for implementing a prevention program that trains athletes to land with the foot closer to the body. In addition, training athletes to fall safely when landing with the COM far posterior to the BOS, instead of reflexively activating their hip flexors and knee extensors, may help prevent ACL-injuries. Future studies are needed to determine if neuromuscular interventions that focus on improving core35 stability and trunk positioning can help reduce the incidence of ACL-injuries.
Previous video tape studies8,17 have failed to demonstrate significant coronal plane alignment (knee abduction, hip abduction, or trunk angle) differences at initial contact between the safe and provocative landing positions when comparing injured athletes to controls. Yet, other studies have demonstrated that increased knee abduction16 and lateral trunk bend17 during landing may be a risk factor for non-contact ACL injury in female athletes. Interestingly, the current study did not show significant differences between male and female athletes for any variable, indicating that a more posteriorly place trunk may be a generalized risk factor across genders.
A consensus is beginning to form around the concept that ACL-injury is likely due to a combination of forces. The critical force appears to be a compressive force on the lateral aspect of the knee6,8,23,37, resulting in a sliding of the lateral femoral condyle on the lateral tibial plateau with resultant ACL disruption, often referred to as a buckling of the leg, instead of the normal knee flexion to absorb the ground reaction forces. Landing in an unstable posture may contribute to the ACL disruption by lowering the level of impulsive force required to buckle the leg and cause an ACL tear. The control subjects land with the ankle plantarflexed8 and the COM less than a single foot length posterior from the BOS. Thus, they are close to a stable static posture and ankle dorsiflexion would extend the BOS towards the heel, creating a stable posture. In contrast, on average, the ACL-injured athletes land with the COM more than two foot lengths posterior to the BOS with a dorsiflexed ankle8, creating a less stable position. To stabilize their posture, these athletes would likely try to flex their trunk forward by activating their quadriceps and trunk flexors13,14. This vigorous quadriceps contraction would lower the impulse force necessary to tear the ACL, by adding a compressive force, as well as, a secondary anterior shear force on the tibia25,33. This activation likely occurs prior to landing as the athletes prepare to stabilize their COM at the time of ground contact10.
At the time of foot contact the trunk’s momentum would naturally rotate the trunk forward, even without core muscle or quadriceps activation. Since the foot lands in a dorsiflexed position (near the end range of motion) in the injured athletes8, the rotation of the tibia cannot assist in this forward rotation. Thus, the upper body and thigh rotate forward, while the lower leg and foot remain fairly stationary. This forward rotation of the upper relative to the lower leg would foster a forward translation of the tibia6, enhancing the likelihood of ACL rupture.
The discriminant analysis demonstrated that positioning of the body’s COM is a likely risk factor for ACL-injury, but that it also likely works in conjunction with other factors to cause injury. No control subject landed with the COM_BOS greater than 1.6 (Figure 6), thus the position of the trunk relative to the base of support is likely a primary risk factor for ACL-injury when the COM_BOS is large. In the range of 1.2-1.6 ACL-injury both occurred and did not occur. In this range the posterior position of the trunk likely combines with other factors in order to result in injury. When the trunk is positioned close to the base of support (COM_BOS < 1.2) ACL-injury did not occur, with one exception. In this range the location of the COM is not a critical factor and other factors are the most likely cause of injury.
The COM_BOS was the measurement of interest for the current study because it provides a more complete description of the dynamic balance stability, as it is the cumulative effect of both lower limb and trunk position. Two previous sagittal-plane studies examined the effect of trunk angle during two-legged drop-landing in healthy controls. These studies concluded that landing with the more extended trunk increased landing and quadriceps forces4 and increased the anterior shear forces on the tibia20. In contrast, a previous study8, from which the current study evolved, demonstrated that a flexed hip, measured similarly to the afore mentioned trunk angle, was present during a landing maneuver that led to ACL disruption. The divergence in results can be explained by the difference in the task evaluated. In the drop-landing task4,20 the limbG angle is quite small, placing the COM close to the BOS. Thus, trunk extension brings the trunk further from the feet, decreasing stability and increasing the external knee flexor moment. To prevent knee collapse, the quadriceps force is increased. In the provocative position8, the limbG angle is large, the hip is flexed, placing the athletes leg anterior to their body, moving the COM far posterior to the BOS. This likely triggers strong core35 and quadriceps muscle contraction in response to the unstable posture, which may have a deleterious effect on the ACL.
In a study by Zazulak and colleagues38 it was demonstrated that athletes who sustain ACL tears have greater pre-injury deficits in proprioceptive repositioning of the trunk compared to uninjured athletes. Due to the small number of individuals that advanced to an ACL-injury (4 females and 2 males) in their prospective study, the role gender played in the relationship of these variables to ACL-injury was not reported. Nonetheless, poor trunk control may have led athletes to allow their COM to be positioned in an unstable position posterior to the BOS, which contributed to the ACL rupture, irrespective of gender.
As with many imaging studies, an exact measure of the accuracy was not available for the current study. For example, in radiological studies the accuracy is typically assumed to be one half the pixel resolution. On average, the femur length was 37.7 pixels for both populations. The difference in the COM_BOS across cohorts was 0.9, which on average would be 32.4 pixels, or 32 times the resolution. If the femur length was again assumed to be 37.5cm, the average resolution was 1 cm. If an accuracy 4 times worse than a radiological study was assumed for the current methods, the accuracy would be 2mm, well below the 38cm reported for the ΔCOM_BOS. The possible acceptance videos where the athletes were slightly rotated away from the sagittal plane would have added variability into the measures. Yet, even if a “worse-case scenario” was assumed, in which: 1) all the control subjects were rotated 30° away from the sagittal plane, 2) all the injury-videos were captured in a purely sagittal plane, and 3) the scaling by femur_length did not compensate at all for this rotation; the difference in the COM_BOS between cohorts dropped to 0.8 and remained significant. Only when the scenario was changed to a 50° angle did the difference between cohorts become insignificant.
There were several potential limitations to this study. The movie clips were collected as a convenience sample and may not be representative of all noncontact ACL-injury mechanisms. Yet, the observed motions likely represented some of the most common noncontact mechanisms of ACL-injury. It was not possible to determine the exact moment at which the ACL-injury occurred, creating possible millisecond differences in the timing of the first sequence picked as the foot touched the ground to the point of injury. However, it was likely that the ACL-injury occurred within 50 msec of ground contact22. There were also possible difficulties identifying anatomic landmarks in clothed individuals with no markers, yet the inter- and intra-rater reliability was excellent. Lastly, although every effort was made to eliminate bias throughout the experiment, there remained a minor potential for selection bias, as the inclusion criteria was based on a qualitative analysis. However, the quantitative measurements acquired (with the use of matched controls to reduce these potential errors) were a considerable improvement over previous descriptive studies based purely on visual estimates of body position. The further strengths of the study were the intentional focus on the sagittal plane to explore concepts that were raised in previous 2D sagittal analyses of controls4,20, eliminating redundancy with previous video-based studies that reported frontal plane kinematics17, the strong statistical differences between the ACL-injured and control cohorts, and the evaluation of posture during an event that directly resulted in ACL-injury. Lastly, this work represents the largest quantitative video analysis study to date and the only one to match the two cohorts.
In conclusion, athletes captured on video while tearing their ACL landed with the COM far posterior to the BOS, as compared to controls. This position likely increases the rectus femoris contraction at initial impact in order to prevent a backwards fall. A strong quadriceps contraction lowers the impulse force necessary to tear the ACL, by adding a compressive force as well as a smaller, secondary anterior shear force on the tibia5,25,34. Therefore, observation of consistent landing with the COM far posterior to the BOS may be helpful as a screening test for athletes at risk for noncontact ACL-injury. Future work is needed to determine if training athletes to avoid this dangerous position helps reduce the risk of an ACL-injury.
Figure 3. Posterior Displacement of the COM relative to the BOS Normalized by Femur Length.
I = injured C= Controls, M = males, F= Females. Injury status was a significant main effect (p<0.001), but gender was not (p=0.080). There were no significant interaction effects (p=0.530).
ACKNOWLEDGEMENT
This research was supported by the Intramural Research Program of the NIH, and the Clinical Center at the NIH. The authors would like to thank Dr. Ching-yi Shieh of the Epidemiology and Biostatistics Department (Rehabilitation Medicine, NIH) for her statistical analysis support. Any opinions, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the National Institutes of Health or the US Public Health Service.
Contributor Information
William Sipprell, Email: William.sipprell@gmail.com.
Frances T. Sheehan, Email: fsheehan@cc.nih.gov.
References
- 1.Adachi N, Nawata K, Maeta M, Kurozawa Y. Relationship of the menstrual cycle phase to anterior cruciate ligament injuries in teenaged female athletes. Arch Orthop Trauma Surg. 2008 May;128(5):473–478. doi: 10.1007/s00402-007-0461-1. PMID:17909824. [DOI] [PubMed] [Google Scholar]
- 2.Alentorn-Geli E, Myer GD, Silvers HJ, et al. Prevention of non-contact anterior cruciate ligament injuries in soccer players. Part 1: Mechanisms of injury and underlying risk factors. Knee Surg Sports Traumatol Arthrosc. 2009 Jul;17(7):705–729. doi: 10.1007/s00167-009-0813-1. PMID:19452139. [DOI] [PubMed] [Google Scholar]
- 3.Arendt E, Dick R. Knee injury patterns among men and women in collegiate basketball and soccer. NCAA data and review of literature. Am J Sports Med. 1995 Nov-Dec;23(6):694–701. doi: 10.1177/036354659502300611. PMID:8600737. [DOI] [PubMed] [Google Scholar]
- 4.Blackburn JT, Padua DA. Sagittal-plane trunk position, landing forces, and quadriceps electromyographic activity. J Athl Train. 2009 Mar-Apr;44(2):174–179. doi: 10.4085/1062-6050-44.2.174. PMID:19295962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boden B, Sheehan FT, Torg JS, Hewett TE. Noncontact Anterior Cruciate Ligament Injuries: Mechanisms and Risk Factors. J Am Acad Orthop Surg. 2010 doi: 10.5435/00124635-201009000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boden BP, Breit I, Sheehan FT. Tibiofemoral alignment: contributing factors to noncontact anterior cruciate ligament injury. J Bone Joint Surg Am. 2009 Oct;91(10):2381–2389. doi: 10.2106/JBJS.H.01721. PMID:19797573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boden BP, Dean GS, Feagin JA, Jr, Garrett WE., Jr Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000 Jun;23(6):573–578. doi: 10.3928/0147-7447-20000601-15. PMID:10875418. [DOI] [PubMed] [Google Scholar]
- 8.Boden BP, Torg JS, Knowles SB, Hewett TE. Video analysis of anterior cruciate ligament injury: abnormalities in hip and ankle kinematics. Am J Sports Med. 2009 Feb;37(2):252–259. doi: 10.1177/0363546508328107. PMID:19182110. [DOI] [PubMed] [Google Scholar]
- 9.Borotikar BS, Newcomer R, Koppes R, McLean SG. Combined effects of fatigue and decision making on female lower limb landing postures: central and peripheral contributions to ACL injury risk. Clin Biomech (Bristol, Avon) 2008 Jan;23(1):81–92. doi: 10.1016/j.clinbiomech.2007.08.008. PMID:17889972. [DOI] [PubMed] [Google Scholar]
- 10.Chappell JD, Creighton RA, Giuliani C, Yu B, Garrett WE. Kinematics and electromyography of landing preparation in vertical stop-jump: risks for noncontact anterior cruciate ligament injury. Am J Sports Med. 2007 Feb;35(2):235–241. doi: 10.1177/0363546506294077. PMID:17092926. [DOI] [PubMed] [Google Scholar]
- 11.DeMorat G, Weinhold P, Blackburn T, Chudik S, Garrett W. Aggressive quadriceps loading can induce noncontact anterior cruciate ligament injury. Am J Sports Med. 2004 Mar;32(2):477–483. doi: 10.1177/0363546503258928. PMID:14977677. [DOI] [PubMed] [Google Scholar]
- 12.Dienst M, Schneider G, Altmeyer K, et al. Correlation of intercondylar notch cross sections to the ACL size: a high resolution MR tomographic in vivo analysis. Arch Orthop Trauma Surg. 2007 May;127(4):253–260. doi: 10.1007/s00402-006-0177-7. PMID:16807752. [DOI] [PubMed] [Google Scholar]
- 13.Ettlinger CF, Johnson RJ, Shealy JE. A method to help reduce the risk of serious knee sprains incurred in alpine skiing. Am J Sports Med. 1995 Sep-Oct;23(5):531–537. doi: 10.1177/036354659502300503. PMID:8526266. [DOI] [PubMed] [Google Scholar]
- 14.Gerritsen KG, Nachbauer W, van den Bogert AJ. Computer simulation of landing movement in downhill skiing: anterior cruciate ligament injuries. J Biomech. 1996 Jul;29(7):845–854. doi: 10.1016/0021-9290(95)00167-0. PMID:8809615. [DOI] [PubMed] [Google Scholar]
- 15.Gilchrist J, Mandelbaum BR, Melancon H, et al. A randomized controlled trial to prevent noncontact anterior cruciate ligament injury in female collegiate soccer players. Am J Sports Med. 2008 Aug;36(8):1476–1483. doi: 10.1177/0363546508318188. PMID:18658019. [DOI] [PubMed] [Google Scholar]
- 16.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005 Apr;33(4):492–501. doi: 10.1177/0363546504269591. PMID:15722287. [DOI] [PubMed] [Google Scholar]
- 17.Hewett TE, Torg JS, Boden BP. Video analysis of trunk and knee motion during non-contact anterior cruciate ligament injury in female athletes: lateral trunk and knee abduction motion are combined components of the injury mechanism. Br J Sports Med. 2009 Jun;43(6):417–422. doi: 10.1136/bjsm.2009.059162. PMID:19372088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Horak FB, Nashner LM. Central programming of postural movements: adaptation to altered support-surface configurations. J Neurophysiol. 1986 Jun;55(6):1369–1381. doi: 10.1152/jn.1986.55.6.1369. PMID:3734861. [DOI] [PubMed] [Google Scholar]
- 19.Iqbal K, Pai Y. Predicted region of stability for balance recovery: motion at the knee joint can improve termination of forward movement. J Biomech. 2000 Dec;33(12):1619–1627. doi: 10.1016/s0021-9290(00)00129-9. PMID:11006386. [DOI] [PubMed] [Google Scholar]
- 20.Kulas A, Zalewski P, Hortobagyi T, DeVita P. Effects of added trunk load and corresponding trunk position adaptations on lower extremity biomechanics during drop-landings. J Biomech. 2008;41(1):180–185. doi: 10.1016/j.jbiomech.2007.06.027. PMID:17678932. [DOI] [PubMed] [Google Scholar]
- 21.Luo W, Stanhope SJ, Sheehan FT. Using two palpable measurements improves the subject-specific femoral modeling. J Biomech. 2009 Aug 25;42(12):2000–2005. doi: 10.1016/j.jbiomech.2009.05.006. PMID:19520371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McLean SG, Huang X, van den Bogert AJ. Investigating isolated neuromuscular control contributions to non-contact anterior cruciate ligament injury risk via computer simulation methods. Clin Biomech (Bristol, Avon) 2008 Aug;23(7):926–936. doi: 10.1016/j.clinbiomech.2008.03.072. PMID:18485552. [DOI] [PubMed] [Google Scholar]
- 23.Meyer EG, Baumer TG, Slade JM, Smith WE, Haut RC. Tibiofemoral contact pressures and osteochondral microtrauma during anterior cruciate ligament rupture due to excessive compressive loading and internal torque of the human knee. Am J Sports Med. 2008 Oct;36(10):1966–1977. doi: 10.1177/0363546508318046. PMID:18490469. [DOI] [PubMed] [Google Scholar]
- 24.Moller E, Weidenhielm L, Werner S. Outcome and knee-related quality of life after anterior cruciate ligament reconstruction: a long-term follow-up. Knee Surg Sports Traumatol Arthrosc. 2009 Jul;17(7):786–794. doi: 10.1007/s00167-009-0788-y. PMID:19360401. [DOI] [PubMed] [Google Scholar]
- 25.Nisell R. Mechanics of the knee. A study of joint and muscle load with clinical applications. Acta Orthop Scand Suppl. 1985;216:1–42. PMID:3865491. [PubMed] [Google Scholar]
- 26.Oiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009 Jul;37(7):1434–1443. doi: 10.1177/0363546509338827. PMID:19567666. [DOI] [PubMed] [Google Scholar]
- 27.Ramesh R, Von Arx O, Azzopardi T, Schranz PJ. The risk of anterior cruciate ligament rupture with generalised joint laxity. J Bone Joint Surg Br. 2005 Jun;87(6):800–803. doi: 10.1302/0301-620X.87B6.15833. PMID:15911662. [DOI] [PubMed] [Google Scholar]
- 28.Schmitz RJ, Ficklin TK, Shimokochi Y, et al. Varus/valgus and internal/external torsional knee joint stiffness differs between sexes. Am J Sports Med. 2008 Jul;36(7):1380–1388. doi: 10.1177/0363546508317411. PMID:18535251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009 Feb;37(2):246–251. doi: 10.1177/0363546508325665. PMID:19109531. [DOI] [PubMed] [Google Scholar]
- 30.Shimokochi Y, Yong Lee S, Shultz SJ, Schmitz RJ. The relationships among sagittal-plane lower extremity moments: implications for landing strategy in anterior cruciate ligament injury prevention. J Athl Train. 2009 Jan-Feb;44(1):33–38. doi: 10.4085/1062-6050-44.1.33. PMID:19180216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Swirtun LR, Renstrom P. Factors affecting outcome after anterior cruciate ligament injury: a prospective study with a six-year follow-up. Scand J Med Sci Sports. 2008 Jun;18(3):318–324. doi: 10.1111/j.1600-0838.2007.00696.x. PMID:18067527. [DOI] [PubMed] [Google Scholar]
- 32.Uhorchak JM, Scoville CR, Williams GN, Arciero RA, St Pierre P, Taylor DC. Risk factors associated with noncontact injury of the anterior cruciate ligament: a prospective four-year evaluation of 859 West Point cadets. Am J Sports Med. 2003 Nov-Dec;31(6):831–842. doi: 10.1177/03635465030310061801. PMID:14623646. [DOI] [PubMed] [Google Scholar]
- 33.van Eijden TM, de Boer W, Weijs WA. The orientation of the distal part of the quadriceps femoris muscle as a function of the knee flexion-extension angle. J Biomech. 1985;18(10):803–809. doi: 10.1016/0021-9290(85)90055-7. PMID:4066722. [DOI] [PubMed] [Google Scholar]
- 34.Vaneijden TMGJ, Weijs WA, Kouwenhoven E, Verburg J. Forces Acting on the Patella during Maximal Voluntary Contraction of the Quadriceps Femoris Muscle at Different Knee Flexion-Extension Angles. Acta Anatomica. 1987 Aug;129(4):310–314. doi: 10.1159/000146421. PMID:ISI:A1987J631500011. [DOI] [PubMed] [Google Scholar]
- 35.Willson JD, Dougherty CP, Ireland ML, Davis IM. Core stability and its relationship to lower extremity function and injury. J Am Acad Orthop Surg. 2005 Sep;13(5):316–325. doi: 10.5435/00124635-200509000-00005. PMID:16148357. [DOI] [PubMed] [Google Scholar]
- 36.Winter DA. Biomechanics and Motor Control of Human Movement. 4ed. Hoboken: John Wiley & Sons; 2005. Segment Dimensions; p. 59. [Google Scholar]
- 37.Yeow CH, Cheong CH, Ng KS, Lee PV, Goh JC. Anterior cruciate ligament failure and cartilage damage during knee joint compression: a preliminary study based on the porcine model. Am J Sports Med. 2008 May;36(5):934–942. doi: 10.1177/0363546507312645. PMID:18227229. [DOI] [PubMed] [Google Scholar]
- 38.Zazulak BT, Hewett TE, Reeves NP, Goldberg B, Cholewicki J. The effects of core proprioception on knee injury: a prospective biomechanical-epidemiological study. Am J Sports Med. 2007 Mar;35(3):368–373. doi: 10.1177/0363546506297909. PMID:17267766. [DOI] [PubMed] [Google Scholar]