Abstract
This study examined relations among family environment, cortisol response, and behavior in the context of a randomized controlled trial with 92 children (M = 48 months) at risk for antisocial behavior. Previously, researchers reported an intervention effect on cortisol response in anticipation of a social challenge. The current study examined whether changes in cortisol response were related to later child aggression. Among lower warmth families, the intervention effect on aggression was largely mediated by the intervention effect on cortisol response. Although the intervention also resulted in significant benefits on child engaging behavior, cortisol response did not mediate this effect. These findings demonstrate meaningful associations between cortisol response and aggression among children at familial risk for antisocial behavior.
The way in which children respond to stress is an important aspect of development. Although experimental studies with animals have led to influential theoretical modeling of the role of human cortisol regulation in maladaptive outcomes (Champagne & Meaney, 2006; Francis, Caldji, Champagne, Plotsky, & Meaney, 1999; Levine, 1957; Liu et al., 1997; Meaney, 2001), only limited experimental work has been done with humans. In children, cross-sectional studies largely support a negative relation between cortisol response to a stressor and aggressive behavior (Blair, Granger, & Razza, 2005; Snoek, Van Goozen, Matthys, Buitelaar, & Van Engeland, 2004; van Goozen, Matthys, Cohen-Kettenis, Buitelaar, & van Engeland, 2000; van Goozen et al., 1998), although the exact nature of the relation has yet to be established (Dadds & Rhodes, 2008; Hart, Burock, London, Atkins, & Bonilla-Santiago, 2005; Rutter, 2008).
A rich literature demonstrates a relation between a blunted child cortisol response to stress and unresponsive or neglectful environments (Gunnar, Fisher, & the Early Experience, Stress and Prevention Network, 2006). However, as with the cortisol–behavior association, the nature of these cortisol–context relations is not well understood.
One model of the development of an abnormal stress response (e.g., Caldji, Diorio, & Meaney, 2000; Liu et al., 1997) suggests that mothers living under stressful conditions display abnormal stress responses, which may be transmitted directly to their offspring. Such maladaptive stress responsivity may lead to various negative outcomes, including aggression. Other models emphasize the complex manner in which genes and environment shape physiology and behavior through Gene × Environment interactions and Gene × Environment correlations (Rutter, Moffitt, & Caspi, 2006). For example, genes that shape maternal stress response could impact the environment by influencing parenting behavior, which, in turn, influences maternal–child interactions. This Gene × Environment effect could subsequently impact child stress response, which, in turn, may influence child behavior. From this perspective, relations among parent cortisol, parent behavior, child cortisol, and child behavior could each reflect the influence of both genes and the environment shared by parents and their offspring.
Experimental approaches provide unique opportunities to examine relations among family environment, child physiology, and behavior. The current study takes advantage of a randomized controlled prevention trial of an early family intervention among children at high risk for antisocial behavior. Previously, Brotman and colleagues demonstrated that the intervention impacts three aspects of parenting (responsive parenting, harsh parenting, and stimulation for learning), child engaging behaviors with unfamiliar peers, and child aggression (Brotman et al., 2005; Brotman et al., 2008), and that intervention effects on parenting are meaningfully related to the prevention of aggression during parent–child interactions (Brotman et al., 2009). Furthermore, the behavioral family intervention resulted in changes in children’s cortisol response in anticipation of a social challenge with unfamiliar peers (Brotman et al., 2007), demonstrating the malleability of the stress response system among children at high risk for antisocial behavior. These reports did not examine how the family environment relates to child stress response or the relations between child cortisol and aggressive behavior. The primary aim of this study is to examine if intervention effects on child cortisol are meaningfully related to later child aggressive behavior, observed during a parent–child interaction 16 months after the intervention. To explore the specificity of this relation, the study also examines intervention effects on child engaging behavior during the same parent–child interaction and whether changes in cortisol mediate any observed intervention effects.
Cortisol Response and Behavior
Stress regulation is implicated in the development of psychopathology (e.g., Alink et al., 2008). Cortisol response to a stressor has been identified as an important indicator of stress regulation, with consequences for child behavior. However, as noted above, considerable literature demonstrates the complex nature of associations among cortisol, context, and behavior. Although low cortisol reactivity to a stressor (i.e., hypocortisolism) has been linked to aggressive behavior (Gunnar & Vazquez, 2001), careful analysis demonstrates more complex associations. For example, unique subgroups of children may exhibit positive associations between cortisol responding and aggression (e.g., Dadds & Rhodes, 2008; Hart et al., 2005; Rutter, 2008). Cortisol does not exhibit a simple one-to-one correspondence with aggression but, rather, can show positive associations in some contexts and negative associations in others. Theories explaining the process in which cortisol is linked to aggression differ. The fearlessness theory (Raine, 1993) posits that low levels of cortisol arousal or reactivity lead children to be fearless, and such fearless children are more likely to initiate fights because they are not concerned about consequences. Stimulation seeking theory (Zuckerman, 1979) argues that some children experience a low arousal, negative state, which leads them to seek higher levels of arousal via aggressive behavior. A third theory proposes that insensitivity to social and emotional distress signals (e.g., fear) in peers predisposes children to certain types of aggression (Blair, 2003).
Relative to typically developing children, children at high risk for psychopathology (e.g., children with familial antisocial behavior, maltreated children, or those raised in orphanages) or those with clinical diagnoses of disruptive psychopathology exhibit low or flattened cortisol responses to challenging situations as well as to circadian changes (Fisher, Gunnar, Chamberlain, & Reid, 2000; Gunnar & Vazquez, 2001; Hart, Gunnar, & Cicchetti, 1995). Considerable empirical literature relates low cortisol reactivity to aggression and disruptive psychopathology (Snoek et al., 2004; van Goozen et al., 1998; van Goozen et al., 2000). This literature, summarized in a recent meta-analysis, finds a medium effect size (d = .57) of low cortisol stress response for children characterized as antisocial or with clinical diagnoses of conduct disorder or oppositional defiant disorder (van Goozen, Fairchild, Snoek, & Harold, 2007). Although preschoolers were not included in the meta-analytic study, a study by Blair et al. (2005) found a similar relation between highly aggressive behavior and blunted cortisol reactivity among preschoolers from low-income families.
Despite the findings from one meta-analysis (van Goozen et al., 2007), some empirical evidence suggests either no significant relation between cortisol reactivity and aggression (see meta-analysis by Alink et al., 2008) or even a positive relation of cortisol reactivity to aggression (e.g., Hart et al., 2005). This lack of a simple one-to-one correspondence between stress response and aggression may be due to multiple complicating factors, including child age and type of disruptive psychopathology (Alink et al., 2008; Dadds & Rhodes, 2008). For example, children who exhibit physical aggression that is predatory or instrumental may be more likely to have blunted cortisol responses to stress than children with reactive aggression or those with more general nonaggressive disruptive psychopathology (Dadds & Rhodes, 2008; Loney, Butler, Lima, Counts, & Eckel, 2006; McBurnett, King, & Scarpa, 2003). The current study examines observed child behavior (physical aggression and socially engaging behavior) during a standardized parent–child interaction paradigm and cortisol levels in response to a social challenge among a relatively homogenous age group of children (33–63 months) followed prospectively over a 24-month period.
Experimental Studies of Child Neurobiology and Behavior
Because the literature on the stress response and aggressive behavior in humans is largely based on cross-sectional studies, there have been few advances in understanding the causal relations between cortisol response and child aggression. As a result, a call has been made for greater use of experimental studies that can illuminate causal mechanisms underlying the link between neurobiology and behavior (Rutter, 2008; Tremblay, 2008). Experimental studies of interventions that alter both the stress response and child behavior provide unique opportunities to examine the nature of the relation between cortisol response and behavior. In theory, restoring a high-risk child’s physiological stress reaction to a typical, reactive state may lead to improved emotional and cognitive appraisal of a socially stressful situation, thus facilitating a less aggressive reaction and a potentially more positive, socially engaged reaction to stressful events (van Goozen et al., 2007).
Two experimental studies with maltreated children report changes in cortisol and child behavior (Dozier, Peloso, Lewis, Laurenceau, & Levine, 2008; Fisher, Stoolmiller, Gunnar, & Burraston, 2007). These studies considered diurnal patterns of cortisol secretion during typical days and did not examine the link between cortisol levels in response to stress and child behavior. A third study of older children (aged 8–13) with behavior disorders found that pretreatment cortisol response to stress moderated intervention outcomes on conduct problems (van de Wiel, van Goozen, Matthys, Snoek, & van Engeland, 2004). Since this study did not examine intervention effects on cortisol, the consequences of child stress response on child behavior remains unknown. In a prior report of immediate intervention outcomes on cortisol response in the current study sample, Brotman and colleagues found that intervention effects on cortisol levels in anticipation of a social challenge and engaged behavior with peers during the challenge were not related (Brotman et al., 2007). The current study extends this work and other prior experimental studies in this area by examining the links between immediate intervention effects on child cortisol response and longer term intervention effects on child engaging and aggressive behavior with the parent, with consideration of the family environment.
Early Family Environment and Stress Neurobiology
Stress-sensitive neurobiology is shaped by early experience, especially by caregiving (Gunnar & Quevedo, 2007). Family environmental factors that operate at key points in development might sculpt hypothalamic–pituitary–adrenal (HPA) axis regulation in children, much as environmental factors have been shown to play a role in HPA regulation in rodents and nonhuman primates (e.g., Caldji et al., 2000; Levine, 1957; Liu et al., 1997). Animal studies suggest both genetic and environmental factors involved in the transmission of abnormal stress regulation. Offspring at high risk for abnormal neuroendocrine stress regulation are characterized by having lower warmth parents (Meaney, 2001). Studies in young human children find evidence of parallel processes (Fisher, Gunnar, Dozier, Bruce, & Pears, 2006; Gunnar et al., 2006; Hane & Fox, 2006). Children from high-risk, stressful environments exhibit lower or flat diurnal cortisol levels compared to nonstressed children (“hypocortisolism”; Gunnar & Vazquez, 2001; Hart et al., 1995; Heim, Ehlert, & Hellhammer, 2000; Hertsgaard, Gunnar, Erickson, & Nachmias, 1995; Nachmias, Gunnar, Mangelsdorf, Parritz, & Buss, 1996). Although both positive and negative relations between quality of caregiving and child cortisol response to stress have been found among low-risk families (Blair & Diamond, 2008; Gunnar, Brodersen, Nachmias, Buss, & Rigatuso, 1996; Gunnar & Vazquez, 2001; Hane & Fox, 2006; Nachmias et al., 1996), studies of high-risk families consistently link suboptimal caregiving with low child cortisol response. For high-risk families, responsive parenting may serve as an important moderating risk or buffering factor for the development of hypocortisolism (i.e., low cortisol levels; Fisher et al., 2006; Gunnar & Vazquez, 2001).
In addition to the responsive nature of the caregiving environment, a small literature in humans suggests that parent stress responding and depression may be related to child cortisol response to stress in early childhood. A large twin study found modest similarity in afternoon basal cortisol levels between parents and children (Schreiber et al., 2006). A small study of diurnal levels of cortisol in typically developing children and their parents documented a positive correlation between diurnal levels of parent and child cortisol (Young, Vazquez, Jiang, & Pfeffer, 2006). Another study of low-risk families found a positive correlation between infant and mother diurnal cortisol, but the correlation was not significant between child and mother cortisol reactivity during a separation paradigm (Thompson & Trevathan, 2008).
Related to parent psychopathology, a small literature suggests that parent depression during early childhood may be related to child cortisol patterns (e.g., Lupien, King, Meaney, & McEwen, 2000). Parent depression in the first 2 years of life was found to predict child cortisol reactivity to a stressor at age 7 (Ashman, Dawson, Panagiotides, Yamada, & Wilkinson, 2002). In sum, parental warmth, parent stress response, and parent depression are likely to influence child cortisol response in early childhood. Yet, the aforementioned studies have not systematically characterized the family environment or examined parent and child factors among children from high-risk stressful environments. In the current study, therefore, we consider three aspects of the family environment (i.e., parental warmth, stress response, and depression) in relation to children’s cortisol and behavior in a high-risk sample.
The Current Study
The current study takes advantage of a randomized controlled trial of an early family intervention among preschoolers at familial risk for antisocial behavior. In a series of studies, the intervention has been found to promote responsive parenting and child engaging behavior with peers, reduce physical aggression during parent–child interactions, and alter cortisol response in anticipation of a social challenge with peers (Brotman et al., 2005; Brotman et al., 2007; Brotman et al., 2008). Guided by current models of developmental psychopathology, we evaluate whether increased cortisol response is related to intervention effects on aggressive behavior with parents. To yield a more complete picture and to evaluate the specificity of the cortisol–aggression connection, we will also evaluate relations among cortisol response and engaging behavior with parents.
Method
Participants
This study includes children and parents who participated in a randomized controlled trial of a family intervention aimed at preventing early conduct problems and later antisocial behavior. The trial methodology and characteristics of participants are detailed elsewhere (Brotman, Gouley, O’Neal, & Klein, 2004; Brotman et al., 2005; Brotman et al., 2008). Briefly, all family court records of youths under the age of 16 adjudicated in two boroughs in New York City were screened between 1997 and 2001 for the presence of preschool-age siblings. “Sibling” was defined as a child who was biologically related to, or lived with, the adjudicated youth for at least 1 year, and whose caregiver also raised the adjudicated youth. Families were eligible if siblings were between 33 and 63 months, the caregiver spoke English, and the family lived within the designated geographic area. Families were ineligible if caregivers had a current substance use or psychotic disorder determined by structured diagnostic interview, or if preschoolers had pervasive developmental disorders or severe or profound mental retardation as reported by parents or indicated by standardized cognitive testing. Forty-eight percent of eligible families (N = 92) agreed to participate and completed assessments. Seven of the 92 families had more than one preschool-age child; none of the siblings were included in this study. Forty-seven families were randomized to the intervention condition and 45 families to the control condition that received no intervention.
Sixty-eight percent of preschoolers were biological siblings of the adjudicated youths (12% full; 56% half), 3% adoptive siblings, and 28% biological nephews, nieces, or cousins raised as “siblings.” Eighty-three percent of caregivers (parents) were the preschoolers’ biological mothers, 2% biological fathers, 10% grandmothers, 3% adoptive mothers, and 2% other female relatives. Parent mean age was 36.3 years (SD = 9.2). Forty-five percent of parents had not completed high school and 59% of families had household incomes under $15,000. Fifty-three percent of preschoolers were girls; 65% were African American, 27% Latino, and 8% other or mixed race. Child mean age was 47.52 months (SD = 8.28) and the average child IQ score (DAS; Elliott, 1990) was 83.2 (SD = 12.9). The stressors experienced by the sample are described elsewhere (Brotman et al., 2004); in addition to socioeconomic disadvantage and sibling antisocial behavior, children were exposed to high rates of maternal psychopathology (based on semistructured diagnostic interviews) and stressful life events (based on maternal reports).
Preventive Intervention
The prevention program was adapted from the Incredible Years Series (IYS), an efficacious program developed and tested extensively by Webster-Stratton (e.g., Webster-Stratton & Hancock, 1998). The program aimed to improve parenting practices and preschoolers’ social competence with the goal of preventing later conduct problems. The program consisted of 6–8 months of active intervention (November–June), followed by a 3-month booster intervention (October–December) initiated approximately 4–6 months after the end of the intervention. The active intervention included 22 group sessions for parents, 22 group sessions for preschoolers, 22 guided parent–child interactions, and 10 home visits.
As per published IYS manuals, group leaders coached parents to use specific parenting skills (e.g., labeled praise, time out) and modeled, directed, and reinforced appropriate behavioral strategies. The program specifically encourages parents to use nonharsh, consistent, and appropriate disciplinary strategies, be less critical, and use positive reinforcement and play interactions to promote children’s social competence. Groups for preschoolers incorporated elements from the Incredible Years Dinosaur Social Skills and Problem-Solving Curriculum (Webster-Stratton, 1990), which has been shown to increase the efficacy of the Parent Program (Webster-Stratton, Reid, & Hammond, 2004). Child group leaders taught social skills, reinforced positive behaviors, and provided consequences for negative behaviors. Home visits were designed to help parents implement skills at home. Leaders from the parent and children’s groups together provided home visits following a curriculum corresponding to parent and preschool group lessons. Home visits created opportunities for developing and implementing behavior plans (e.g., placement of a time out chair in a crowded apartment).
The control condition consisted of assessments and monthly phone calls through which family service use and changes to family circumstances were evaluated. Parents were paid $5 for these monthly phone interviews. If families requested assistance with identifying social, educational, or mental health resources during these calls, a clinician followed up with information provided over the telephone.
Assessment Procedures
Participants were assessed four times, 8 months apart, over 24 months: baseline or preintervention (Time 1, Month 0), postintervention (Time 2, Month 8), 8-month follow-up (Time 3, Month 16), and 16-month follow-up (Time 4, Month 24; see Table 1). Previously, we reported main effects of the intervention on child cortisol response immediately postintervention (Brotman et al., 2007), and intervention effects on child aggression during a parent–child interaction at Time 4 (Brotman et al., 2008). The intervention took place between Time 1 and Time 2 and the booster sessions took place between Time 2 and Time 3; no intervention took place between Time 3 and Time 4. The length of time between assessments was not different for intervention and control conditions, t(77) = −0.42, p > .10. The preintervention assessment required three or four visits, and the three postintervention assessments required two visits each; one visit was at the study center and one was in the home.
Table 1.
Timeline of Assessments
| Time 1 | Time 2 | Time 4 |
|---|---|---|
| 0 months | 8 months | 24 months |
| 4 years old | 4 years 8 months old | 6 years old |
| Preintervention (baseline) | Immediate postintervention | 16 months postintervention |
| Child cortisol reactivity | Child cortisol reactivity | Child aggression |
| Parent cortisol reactivity | Child engaging behavior | |
| Parent depression | ||
| Parent warmth |
Measures
Child cortisol in anticipation of a social challenge
Neuroendocrine functioning was measured by collecting salivary cortisol samples prior to an unfamiliar peer situation (prechallenge cortisol). Cortisol assessments were collected at baseline prior to randomization (Time 1) and repeated in an identical fashion immediately after intervention (Time 2). Samples were collected using a sterile cotton roll held by dental floss. The child mouthed the roll until it was wet. The sample was then placed in a vial and kept in a freezer until transported on ice to the laboratory. Food intake was controlled during the collection process.
The social challenge involved entry into an unfamiliar peer group for 30 min of play at a nursery school several blocks from the study center. Observations were scheduled with the school to correspond with planned free play. Approximately, 40 children (ages 34–60 months) from diverse socioeconomic and ethnic backgrounds were enrolled in the school. During free play, children were free to move from station to station (e.g., blocks, pretend house, art table) in a large room designed for this purpose. At least one teacher and three assistants from the school staffed free play.
Prior to leaving the study office for the school, a research assistant unaware of intervention status and study hypotheses explained to the child (in front of the parent) that he or she was “going to a school to play with some other children.” Thus, children were informed about an impending potentially stressful experience prior to cortisol sampling. Two or three research assistants escorted the child and parent to the school (a 10– to 15–min walk). On arrival, and in the presence of the parent, a salivary cortisol sample was collected. The sample was collected approximately 15–20 min after the child was told about the challenge task. Because cortisol release in preschoolers occurs as early as 10 min from the stimulus presentation, we consider this cortisol sample to be an index of the child’s anticipation of the challenge. After the cortisol sample was taken at the school, the child was then required to separate from the parent and accompanied to the play area by one or two research assistants who observed the child during 30 min of free play. Assessment procedures, including timing of cortisol collection, were identical for intervention and control conditions and for both assessment points. For Times 1 and 2, children’s cortisol samples were collected between 10:00 and 11:30 a.m. or between 2:00 and 4:00 p.m., with the majority collected in the afternoon. Although individual children were not assessed at the same exact time at both assessments, major differences in levels based on diurnal patterns are not expected in this time range from late morning to early afternoon. Further details of the observational paradigm and intervention effects on behavior observed during this procedure are presented elsewhere (Brotman, Gouley, & Chesir-Teran, 2005; Brotman et al., 2005).
Children’s cortisol levels in anticipation of the social challenge may reflect the child’s response to a number of cues including separation from the parent, entry into a social peer situation, or a general transition. To further understand the challenge data, we also collected cortisol samples at home over the course of the day to evaluate diurnal patterns. We examined intervention effects on diurnal patterns but did not find an effect. Details on the diurnal patterns and the relation between cortisol in anticipation of a social challenge and cortisol levels over the course of the day at home are reported in Brotman et al. (2007).
Observed child behavior during parent–child interaction
Child behaviors with the parent were observed by raters unaware of intervention status during semistructured, parent–child interactions at the home and study center at Times 1–4. For this study, we utilize data from Times 1 and 4 only. At each assessment point, two parent–child interaction measures were obtained, a 10-min session at the family’s home (5-min child-directed free play and 5-min parent-directed puzzle task), and a 15-min session at the study center (7-min child-directed free play, 5-min parent-directed puzzle task, and 3-min cleanup). Home and center-based assessments took place approximately 1 week apart. Home assessments were coded live and assessments in the study center were videotaped and coded at a later time. Different raters coded home and center-based observations and were uninvolved in other aspects of the study.
The Dyadic Parent–Child Interaction Coding System–Revised (DPICS–R; Robinson & Eyberg, 1981; Webster-Stratton, 1985) was used to record the frequency of discrete aggressive behaviors in both settings. Observed child physical aggression was derived from the two DPICS–R codes of physical aggression: child physical negative (i.e., child is physically aggressive toward parent) and child destructive (i.e., child destroys, damages, or attempts to damage objects). The two codes of physical aggression were significantly related (r = .43, p < .001) and combined. Reliability estimates consider average reliability across assessment time points. To estimate interrater reliability, approximately 20% of observations (in each setting, at each time point, and in each condition) were coded by two raters. Interrater agreement, calculated via single-measure intraclass correlation coefficients with a one-way random-effects model (Shrout & Fleiss, 1979), was .85 for direct home observations and .84 for videotaped center observations. Mean level aggression scores across home and center settings were not significantly different and were highly correlated (r = .67, p < .001). At each time point, we created a composite index of physical aggression by combining ratings across the two settings. The total physical aggression score reflects the number of times the child aggressed toward his or her parent or destroyed objects over a total of 25 min. The estimated reliability of the composite across all time points was .88 (Lord & Novick, 1968).
Although the primary focus of this study is on aggressive behavior, we also examined engaging behavior with the parent to gain a more complete picture of behavioral outcomes. Of note, although we have reported immediate intervention effects on engaging behavior with peers (Brotman, Gouley, Chesir-Teran, & Dennis, 2005), we have not previously examined longer term intervention effects (Time 4) on engaging behavior with the parent. The Global Impressions of Parent–Child Interactions (GIPCI; Brotman, 1998) was used to make global ratings of child positive, engaging behavior with the parent. GIPCI ratings were made on a 5-point scale using descriptions of prototypic behaviors. Child positive engagement was the average of the following three GIPCI scales: child emotion (i.e., positive emotional tone of the child behaviors), child play with the parent (i.e., child shares and encourages activity with parent, shows appropriate verbal skills and cooperation), and reverse-coded child disconnection (i.e., child is withdrawn, aimless, requires encouragement to play and relate to parent). The three codes of positive engagement were significantly related (rs = .53–.69) and were combined. We combined home and study center observations because both were related (r = .38 at Time 1 and r = .44 at Time 4). Test–retest reliability for the combined scale ranged from .47 to .61. The ICC for the combined composite is .75. The estimated reliability of the composite was .83 (Lord & Novick, 1968).
Parent warmth
The Home Observation for the Measurement of the Environment–Early Childhood Version (HOME–EC; Caldwell & Bradley, 1984) was used to assess aspects of the home environment and parenting. The observation of the parent–child relationship occurred in the home over the course of an approximately 2-hr visit. For the current study, we used warmth data at Time 1. Items are rated by interviewers as present (1) or absent (0). We employed the conventional Caldwell and Bradley HOME Warmth scale (Caldwell & Bradley, 1984). It is a seven-item scale including the following items: “Parent holds child close 10–15 min per day”; “Parent converses with child at least twice during visit”; “Parent answers child’s questions or requests verbally”; “Parent usually responds verbally to child’s speech”; “Parent praises child’s qualities twice during visit”; “Parent caresses, kisses, or cuddles child during visit”; and “Parent helps child demonstrate some achievement during visit.” The summary score was the mean of all seven items. Internal consistency was moderate (α = .61). Approximately one third of the sample had scores of 1 on all seven items (i.e., all seven items were observed in the home). For the remainder of the sample (67%), scores ranged from 0 to 6.
Parent depression
We assessed parent depression using the Structured Clinical Interview for DSM–IV nonpatient version (SCID–NP; Williams et al., 1992) by trained clinical psychologists. An independent clinician reviewed all clinical interviews for diagnostic decision making by interviewers. Psychometric properties of the SCID are adequate in other samples (Williams et al., 1992).
Parent cortisol in anticipation of a challenge
Parent neuroendocrine functioning was measured by collecting salivary cortisol samples prior to the administration of a Wechsler Adult Intelligence Scale–Vocabulary subtest and a Wide Range Achievement Test–Reading subtest (i.e., prechallenge cortisol). Cortisol assessments were collected prior to randomization (Time 1) on the same day and within a 1-hr time period of when the child provided his or her sample. Parents were informed that they were going to be asked to complete a test of their vocabulary and reading skills. Saliva samples were taken approximately 10 min after the instructions were given; as such, we consider this cortisol sample to be an index of the parent’s anticipation of the challenge. The literature supports that cognitive testing should serve as a stressful challenge for adults in a similar fashion as the peer entry paradigm is stressful for young children. A cognitive test may be perceived as especially challenging for parents in this sample since their mean level of cognitive functioning and achievement was well below average (Brotman et al., 2004). Samples were collected using a sterile cotton roll held by dental floss. The parent mouthed the roll until it was wet. The sample was then placed in a vial and kept in a freezer until transported on ice to the laboratory. Food intake was controlled during the collection process. The assessment of parent cortisol was designed so that it would yield information that would be helpful in interpreting child cortisol levels. As with child cortisol, parent cortisol was also collected from parents at home at four time points over the course of the day (the same day and time points as the child). We do not report these data here, but we evaluated these diurnal levels to aid interpretation of challenge data. Diurnal levels are available from the authors.
Analyses
Attrition and imputation strategies
Time 1, 2, and 4 data were utilized for the current study. There was modest attrition by Time 2 (87% retained) and Time 4 (77% retained). There were no differences by intervention status in the percentage of children and parents missing data at any time. Furthermore, there were no baseline differences between those with complete data versus those with missing data at later times, and there were no significant baseline score by intervention status interactions in predicting missingness. Given these results, we assume that the data are missing at random (Schafer & Graham, 2002).
As per Little and Rubin (2002), we used the SAS Multiple Imputation (SAS Institute, Cary, NC) procedure with 10 replicated imputations to impute data for all study variables; the imputation made use of the joint distribution of all available measures of parent and child functioning. Imputations were conducted separately for the control and intervention groups to account for the possibility of different missing data patterns by group (Little & Rubin, 2002). SAS PROC MIANALYZE was used to combine the results of the 10 imputations for the final inference. This combination of multiple imputations provides estimates of standard errors that take into account the fact that some data were imputed. Of note, we did not impute missing data for observed child physical aggression because the distribution of scores was highly skewed, even after log transformation. The imputation methods are optimal for normally distributed variables and are not appropriate for highly skewed variables. Therefore, we used the approach of carrying the last time point forward to replace the missing values for this variable. All analyses yielded highly similar results regardless of using the imputed or nonimputed data set.
Analytic approach
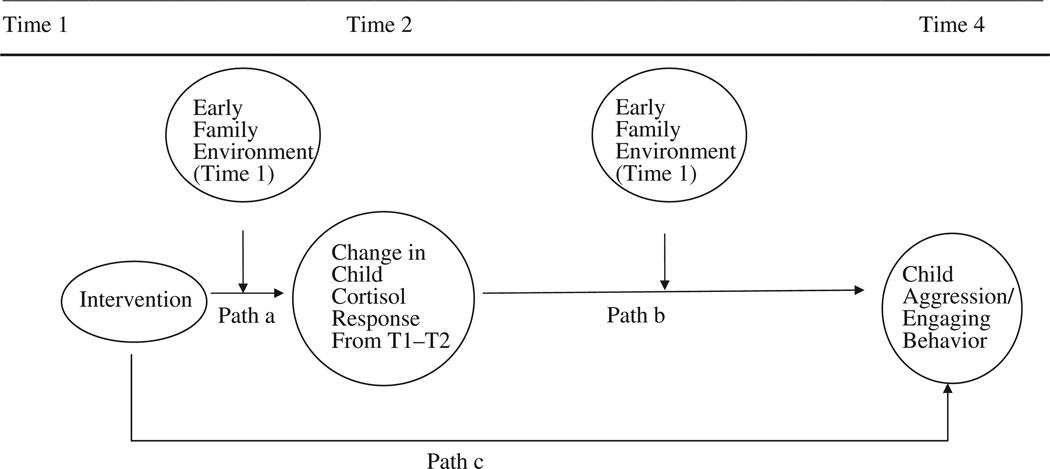
Correlations were estimated and tested to determine the concurrent relations among aspects of the family environment, child cortisol response, and child behavior. We tested a mediation process in which child cortisol response was expected to mediate the intervention effect on later child outcomes (i.e., aggression, engaging behavior): The intervention effect on child cortisol response was expected to be related to the intervention effect on child outcomes. We employed the “joint significance test” strategy in which mediation is inferred if there is evidence that both paths a (intervention effect on cortisol) and b (change in cortisol and later behavior) in Figure 1 are significant (MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002). We also carried out the conventional Sobel test described by Baron and Kenny to test the significance of the mediation model (1986).
Figure 1.
Hypothesized mediation model.
To test the percent of the intervention effect accounted for by the mediator, we used an equation that is appropriate for a nonlinear mediation model. In a linear-based mediation model, the total intervention effect (c) is equal to the sum of the part that is explained by the mediator (paths a and b) and the part that does not involve the mediator (c′). In a nonlinear mediation model, like our model, c is not equal to the total intervention effect (i.e., c is not equal to the sum of the part explained by the mediator [a and b] and the part that does not explain the mediator [c′]; Fleiss, Levin, & Paik, 2003). For this reason, we compute the total effect as the indirect effect/total effect = (a × b)/[(a × b) + c′].
Poisson regression analysis, a log-linear approach appropriate for low frequency behavior counts with skewed distributions (Fleiss et al., 2003), was used to test the relation between cortisol change and aggression. The Poisson regression model was carried out using a generalized estimating equation approach (Diggle, Heagerty, Liang, & Zeger, 2002; Liang & Zeger, 1986; Zeger, Liang, & Albert, 1988) with a log-link function (Diggle et al., 2002). PROC GENMOD in SAS® (SAS Institute, Cary, NC.) was used to perform the analyses.
A mediation model is ideally tested in a design demonstrating time precedence in which the intervention occurs before the mediator and the mediator occurs before the outcome (Cole & Maxwell, 2003; Kraemer, Wilson, Fairburn, & Agras, 2002; Sobel, 1990). Note that we only examined the outcomes at Time 4, rather than modeling change over multiple time points, due to the temporal limitations of testing a mediation model.
Upon inspection of the distribution of child aggression scores across the range of parental warmth, we found that there was essentially no child aggression at Time 1 or Time 4 among the families with scores of 1 on warmth (33% of the sample). Among the high-warmth families (warmth = 1), only 1 child in the control group and 1 in the intervention group had nonzero scores at baseline. At Time 4, 2 children in the control condition had nonzero aggression scores and all children in the intervention had 0 aggression scores. As a result, we eliminated the families with scores of 1 on warmth from the mediation analyses relating child cortisol to aggression.
Results
Preliminary Analyses
Descriptive means and standard deviations for the sample by intervention are presented in Tables 2 and 3. Because both tables are intended to provide information necessary for interpretation of the mediation analyses on aggression, all descriptive information is presented with the removal of the families with scores of 1 on warmth at baseline. As shown in Table 2, no baseline (Time 1) intervention group differences were found for any of the child or family variables.
Table 2.
Descriptives (Mean and Standard Deviation) by Intervention Status
| Control (N = 24) | Intervention (N = 33) | |||
|---|---|---|---|---|
| Time 1 | Time 2 | Time 1 | Time 2 | |
| Child cortisol | 0.07 (0.31) | −0.09 (0.33) | 0.07 (0.32) | 0.27 (0.50) |
| Parent cortisol | 0.11 (0.27) | 0.05 (0.29) | ||
| Parent warmth | 0.66 (0.18) | 0.67 (0.16) | ||
| Parent depression | 42% | 35% | ||
| Time 1 | Time 4 | Time 1 | Time 4 | |
| Child aggressive behavior | 0.24 (0.79) | 1.05 (3.73) | 0.86 (2.41) | 0.26 (0.71) |
| Child engaging behavior | 3.96 (0.50) | 4.02 (0.56) | 3.81 (0.38) | 3.91 (0.44) |
Note. Table does not include families with warmth = 1.
Table 3.
Descriptives and Correlations Among Baseline Early Family Environment, Child Cortisol Response, and Child Behavior
| N | M (SD) | Child cortisol |
Parent cortisol |
Parent warmth |
Parent depression |
Child aggression |
|
|---|---|---|---|---|---|---|---|
| Child cortisol | 44 | 0.07 (0.31) | |||||
| Parent cortisol | 47 | 0.08 (0.28) | .25 | ||||
| Parent warmth | 57 | 0.66 (0.17) | .08 | .21 | |||
| Parent depression | 56 | 0.39 (0.49) | −.08 | .01 | −.14 | ||
| Child aggression | 57 | 0.50 (1.69) | −.17 | −.07 | −.21 | −.04 | |
| Child engaging | 57 | 3.90 (0.45) | −.22 | .21 | .24† | .25† | −.24† |
Note. N for correlations in the low warmth group ranged from 40 to 57. Table does not include families with warmth = 1.
p < .10.
Relations Among the Family Environment, Cortisol Response, and Child Behavior
Table 3 shows concurrent, baseline relations among aspects of the family environment (parent cortisol response, warmth, and depression), child cortisol response, and child behavior.
Intervention Effect on Cortisol (Path a)
Previously, Brotman et al. (2007) reported intervention effects on cortisol for the entire sample. Since we removed a subset of families with high warmth scores from the mediation analyses, we first needed to replicate the intervention effect on cortisol among the remaining families. Results indicate that the intervention had a significant effect on cortisol, Estimate (SE) = .49 (.20), p < .05. Similar to findings previously reported for the full sample, cortisol levels increased in the intervention condition (.07 to .27) and decreased in the control group (.07 to −.09; see Table 2). Even after removing the high-warmth families from these analyses, maternal warmth at baseline significantly moderated the intervention effect on cortisol, Estimate Intervention × Warmth (SE) = 1.83 (.61), p < .01. The pattern of findings shows that the intervention had a stronger effect on cortisol among the families with lower warmth scores at baseline.
Previously, we reported long-term intervention effects on parent responsiveness for the entire sample (Brotman et al., 2008). For this study, we reexamined the intervention effect on parental warmth within the smaller sample (without the highest warmth families and with a slightly different measure so that it was consistent with the baseline measure of warmth considered in this study) and then conducted a post hoc analysis of the relation between intervention effects on parental warmth and child cortisol. As expected, the intervention significantly increased warmth (β = .15, SE = .06, p = .01), and there was a positive, although nonsignificant, association between change in warmth and change in cortisol (r = .24, p = .21), such that increases in warmth were associated with increases in cortisol response.
Cortisol Change and Later Aggression (Path b)
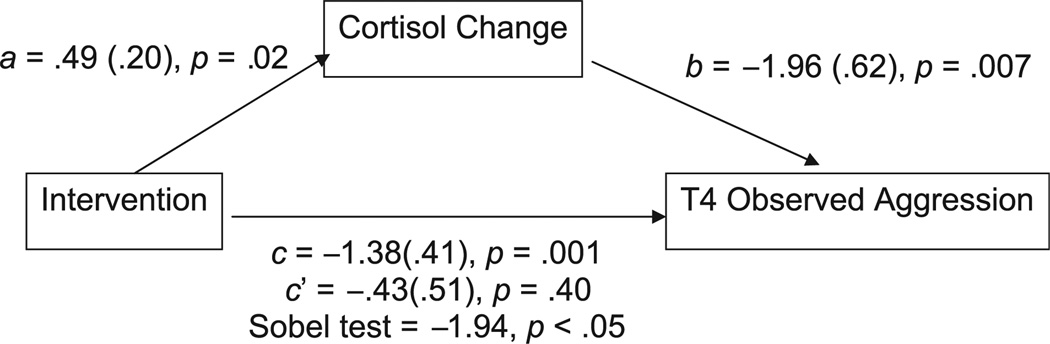
There was a significant relation of change in cortisol from pre- to postintervention with child aggression at Time 4, Estimate (SE) = −1.96 (.62), p = .007 (see Figure 2). The relation between cortisol change and later aggression was not moderated by warmth, Estimate intervention ½ warmth (SE) = 1.88 (1.35), p = .17.
Figure 2.
Estimates for indirect intervention effect for lower warmth group (warmth < 1).
Note. N = 57; subsample of high warmth (warmth score = 1) has been removed. a = intervention effect on cortisol change; b = cortisol change on aggression; c = total intervention effect on aggression; c′ = total intervention effect on aggression, adjusting for the mediator (cortisol change).
Taken together, these results meet the joint significance test for mediation of child aggression because both paths a (intervention effects on cortisol) and b (change in cortisol and later behavior) were significant (MacKinnon et al., 2002).
Intervention Effect on Child Aggression (Path c)
Brotman and colleagues previously reported that there was a significant intervention effect on Time 4 aggression across the entire sample (Brotman et al., 2008). After the removal of the high warmth families, there was a significant intervention effect on Time 4 aggression, c = −1.38 (.41), p = .001 (see Figure 2). This effect was not moderated by warmth, Estimate Intervention × Warmth (SE) = 8.03 (5.91), p = .20.
Intervention and Child Aggression Adjusted for Mediator (Path c′)
The results from the previous three sections show that the mediation link between the intervention, cortisol, and later aggression was supported (paths a and b were significant; see Figure 1). In this section, we test paths c and c′ (whether the effect of intervention on aggression is no longer significant after adjusting for the mediator). As described above, the intervention effect on aggression (path c) was significant, c = −1.38 (.41), p = .001. As expected in complete mediation, regression analyses showed that after adjusting for the mediator (change in cortisol), the intervention was no longer significantly correlated with later aggression, c′ = −.43 (.51), p = .40.
Post hoc analyses revealed that changes in cortisol accounted for 69% of the intervention effect on child aggression. We find further support for the mediating role of cortisol on aggression using the Sobel test (Sobel test = −1.94, p < .05; see Figure 2).
To summarize, after removing the highest warmth families because their children did not display aggression at baseline or Time 4, there was an intervention effect on cortisol (that was strongest for the lower warmth families) and intervention-induced change in cortisol response mediated the intervention effect on aggression. Over two thirds of the intervention effect on Time 4 aggression during a parent–child interaction was accounted for by the intervention effect on cortisol response in anticipation of a social challenge.
Child Engaging Behavior
Across the entire sample, we documented a significant intervention effect on later child engaging behavior with the parent, 16 months after the intervention, Estimate (SE) = .26 (.08), p = .003. To be able to compare results from the mediation analyses with those for child aggression, we limited the analyses of engaging behavior to the lower warmth sample only. The intervention effect on engaging behavior was not significant among lower warmth families, Estimate (SE) = .12 (.15), p = .41, and a change in cortisol from pre- to postintervention was not related to child engaging behavior at T4, Estimate (SE) = .09 (.42), p = .33; since path b was not significant, mediation did not occur for engaging behavior via cortisol change.
Discussion
The current study takes advantage of an experimental trial with young children at high risk for antisocial behavior to further understand the complex nature of relations among the family environment, neurobiological regulation of stress, and developmental psychopathology. In earlier work with this high-risk sample, we found that family intervention that successfully prevented aggression during early childhood (Brotman et al., 2008) also resulted in normalized stress response (Brotman et al., 2007). The current study extends these findings by examining associations between immediate intervention effects on cortisol response and intervention effects on later aggression, with consideration of the family environment. Study findings underscore the importance of parental warmth for the development of cortisol response during early childhood, suggest that the cortisol response system is plastic (amenable to change as a result of psychosocial intervention) in children from high-risk families and those further characterized by lower maternal warmth, and indicate that cortisol response in anticipation of a social stressor predicts later child aggression. Among the subset of families considered in this study of meditational processes, the long-term prevention effect on child aggression was largely explained by immediate intervention effects on cortisol levels. These findings hold important theoretical and practical implications for the development of the stress response, developmental psychopathology, and its prevention.
Although low cortisol has been associated with disruptive psychopathology, studies demonstrating this link remain largely correlational in nature and, for the most part, have been conducted with children already exhibiting problems (Alink et al., 2008). Furthermore, studies linking child cortisol and behavior have not typically characterized the family environment in which these associations are found. The current study investigates the connection between child cortisol and aggression, while also considering family environment. It links intervention-related increases in cortisol in anticipation of a social challenge to the prevention of physical aggression among children at high risk for maladjustment. Findings are consistent with the theoretical proposition that prevention of aggressive behavior, among children at high risk for atypical stress responding, is dependent on changing the stress response system (van Goozen et al., 2007).
The results of this study beg future in-depth probing of the underlying mechanisms linking changes in cortisol to reduced aggression. Of particular interest in this study is how children’s anticipation of a social challenge with peers relates to later aggressive behavior during a parent–child play interaction. A theoretical model worth testing is whether or not child physiological stress response impacts cognitive and emotional processes leading to aggression (van Goozen et al., 2007). In theory, restoring a child’s physiological stress response to a typical, reactive state may lead to improved emotional and cognitive appraisal of a socially stressful situation, and these skills generalize across settings and over time, resulting in less aggressive reactions (van Goozen et al., 2007). An alternative but related explanation of results may be that children’s increased, more typical, reaction to stress may make them more sensitive to stress cues in relationships, which may, in turn, make them less aggressive toward others. Perhaps such increased sensitivity to social stress leads children to be more fearful of the negative consequences of misbehavior, resulting in lower rates of aggression (Raine, 1993). It has also been posited that heightened stress reactivity occurs due to increased “biological sensitivity to context” with negative consequences in an adverse context and positive consequences in a supportive context (Boyce & Ellis, 2005; Ellis & Boyce, 2008). An intervention could act as a supportive context for families. Perhaps, in this sample, a positive behavioral outcome (i.e., low levels of aggressive behavior) as a consequence of increased stress reactivity was especially possible due to the supportive context an intervention offers to a family.
The current study points to the importance of how the early family environment relates to child cortisol response to a stressor. This study’s result linking parent and child cortisol response is too preliminary to speculate as to whether or not the association is due to genetic or learned causes; however, it will be important to identify mechanisms leading children to develop cortisol reactivity patterns that are similar to their parents. Future studies may want to examine whether the most direct route to understanding child neurobiology is not via parent psychopathology or parenting, but via parent neurobiology. In addition to the clustering of parent depression, warmth, cortisol, and child engaging behavior and associations between parent and child cortisol, preliminary, post hoc analyses suggested that among lower warmth families, where changes in both responsive parenting and cortisol levels were observed, responsive parenting and child cortisol response changed in a parallel fashion. Together, the sum picture of such correlational results suggests the importance of research testing causal pathways explaining the link between family environment and child neuroendocrine response during the important developmental period of early childhood.
Given that the link between neurobiological change and aggression occurred among lower warmth families in this study, the intervention effect on cortisol and aggression suggests that care-giving is an important element of a compensatory resilience process (see Luthar, Cicchetti, & Becker, 2000) promoting healthy early neurobiological growth among high-risk children. Results suggest that the early family environment of warmth is a significant contextual factor in explaining change in cortisol response and the consequence of such cortisol change on child aggression. Results contribute to the small literature demonstrating biological outcomes from early intervention with young children (Brotman et al., 2007; Dozier et al., 2008; Fisher et al., 2007; Raine et al., 2001). Our findings underscore the importance of considering characteristics of the family environment (e.g., parental warmth) within studies that examine biological and behavioral outcomes from family intervention (Cicchetti & Gunnar, 2008). In intervention children from lower warmth families, cortisol levels in anticipation of a social challenge were found to increase over an 8-month period, from approximately ages 4–5 years. In contrast, in control children from lower warmth families, cortisol levels decreased over this same developmental period. These findings support a developmental model in which moderately low levels of parent warmth place children who are at familial risk for antisocial behavior at even further risk for an atypical stress response. In these lower warmth families, preventive intervention that enhances parenting practices and child social competence (Brotman et al., 2005) may protect against this risk; immediately following intervention, children from lower warmth intervention families exhibited increases in cortisol relative to controls. It is important that future research more definitively establishes the developmental trajectory of normal cortisol response patterns over time among young children and the specific challenge conditions that elicit such a response. Translation of basic research to preventive interventions is dependent on future research, which details the stress buffering mechanisms in the family environment leading to positive neurobiological and behavioral outcomes in high-risk children (Gunnar et al., 2006).
This study also extends previous research (e.g., Fisher et al., 2006) by characterizing the family environment and the subgroups that benefit from intervention. Additional post hoc results suggested that among lower warmth families, the intervention altered both parent warmth and child cortisol, and these changes may be related. Further research is needed to more fully understand how change in parenting may lead to change in child neuroendocrine functioning and behavior. The unique importance of warmth for the development of the neurobiological system is strongly supported by animal studies (e.g., Caldji et al., 2000; Liu et al., 1997), especially an elegant experimental literature of rodent maternal care on rat pup stress response. Unlike the physical process underlying rodent parent warmth (i.e., licking and grooming of their offspring), the measure of human parental warmth as assessed in this study largely consisted of verbal behaviors. It is not known whether findings are specific to verbal behaviors or whether inclusion of physical behaviors (e.g., hugging, physical proximity) would provide a more complete picture of this process. As these lower warmth families were also characterized by parent depression and hypocortisolism, future exploration of the construct of warmth and its relation to other aspects of parenting behavior and neurobiology in high-risk families appears warranted.
Future studies should also consider additional outcomes of child functioning and parent–child relations. In the current study, increased cortisol in anticipation of a social challenge was related to lower rates of aggressive behavior during parent–child interactions. It is possible that higher cortisol levels may be related to other outcomes, including negative outcomes such as poor physical health. In this study, aggression, not child engaging behaviors, was related to child cortisol change. Perhaps other positive child outcomes, such as child emotion coping or academic success, would be affected by change in child cortisol response. Also, in empirical studies of cortisol and aggression, it has been argued that it is best to examine cortisol under stressful conditions (i.e., cortisol reactivity) rather than relying on diurnal cortisol (van Goozen et al., 2007); the cortisol patterns unique to aggressive behavior may be specific to or more easily detected in stressful or challenging conditions (McBurnett, Lahey, Rathouz, & Loeber, 2000; Pajer, Gardner, Rubin, Perel, & Neal, 2001; Popma et al., 2006; van Goozen et al., 2000). Therefore, future studies may want to determine what kinds of outcomes are uniquely affected by change in cortisol response to challenge versus diurnal patterns of cortisol. Similarly, the specific context of the cortisol stressor could predict different subtypes of aggression. For instance, if the cortisol response paradigm tested reactivity or lack of reactivity to others’ distress, rather than reactivity to novel peers as in this study, then the lack of reactivity to others’ distress might better predict emotional callousness (Dadds & Rhodes, 2008).
In addition to further understanding relations among family environment, child cortisol response, and behavior, this study provides further evidence in support of early family intervention for high-risk children. Specifically, new findings on child outcomes in this study include intervention effects on observed child engaging behavior, 16 months after intervention.
There are a number of important study limitations that are worthy of consideration. First, we had to eliminate families with the highest scores on warmth from the mediation analyses. As a consequence, none of the findings can be generalized to families characterized by high warmth. Future studies should conduct mediation and moderation analyses of intervention effects on aggression to formally test many of the proposed hypotheses. In addition, the generalizability of study findings is limited due to the unique nature of the sample. In terms of the sample characteristics, attempts to replicate the current findings should consider whether similar effects on cortisol can be documented among children living in environments involving different forms of stress. The current findings should encourage attempts to examine effects on physiology in much larger samples, where unique subgroups can be examined more comprehensively. Despite the need for replication, the current findings demonstrate statistically significant mediating effects. This suggests the potential value of conducting future work examining mechanisms linking context, behavior, and stress response in children. Such future work might include longer term outcomes assessed over multiple time points.
As with the initial report on intervention effects on cortisol response (Brotman et al., 2007), the current study is limited by the lack of a low-risk comparison group. Including such a group, studied with identical methods, is key given the robust effects of context on both behavior and cortisol. However, the association between increased cortisol response and lower rates of aggression suggest that intervention effects on cortisol response were positive and that the intervention worked to normalize the stress response. The study is also limited by its reliance on one measure of parent warmth. It would have been desirable to have a more comprehensive measure of this construct that includes both verbal and physical aspects of warmth. Also, we do not know whether study findings generalize to child behavior outside the home environment. That is, we did not measure behavior with peers, and, therefore, it is not known whether the relation between cortisol and behavior is limited to the context of parent–child interactions.
Much remains to be explained about the role of the early family environment, stress response, and the prevention of psychopathology in high-risk children. It is imperative that prevention studies continue to examine neurobiological as well as behavioral systems and outcomes (Cicchetti & Gunnar, 2008). Additionally, we would urge investigators to consider many aspects of the caregiving environment as potential moderators of these mediational processes (Fairchild & MacKinnon, 2009). Such steps would advance the field considerably in understanding the complex interplay of the early family environment, neurobiological functioning and the development, and prevention of aggression and psychopathology.
Acknowledgments
This research was supported in part by a NARSAD Young Investigator Award to the first author and a grant from the National Institute of Mental Health (NIMH R01 MH55188) to the second author. We acknowledge the research staff of the Institute for Prevention Science, Tom Cooper and staff of the Nathan Kline Institute for assistance with the processing of cortisol assays, and the families and children who participated. We would also like to acknowledge the substantial contributions that Drs. Rachel Klein, Eva Petkova, and Patrick Shrout have made to this research.
Contributor Information
Colleen R. O’Neal, NYU Child Study Center, New York University, School of Medicine
Laurie Miller Brotman, NYU Child Study Center, New York University, School of Medicine.
Keng-Yen Huang, NYU Child Study Center, New York University, School of Medicine.
Kathleen Kiely Gouley, NYU Child Study Center, New York University, School of Medicine.
Dimitra Kamboukos, NYU Child Study Center, New York University, School of Medicine.
Esther J. Calzada, NYU Child Study Center, New York University, School of Medicine
Daniel S. Pine, National Institute of Mental Health
References
- Alink L, van IJzendoorn MH, Bakermans-Kranenburg MJ, Mesman J, Juffer F, Koot HM. Cortisol and externalizing behavior in children and adolescents: Mixed meta-analytic evidence for the inverse relation of basal cortisol and cortisol reactivity with externalizing behavior. Developmental Psychobiology. 2008;50:427–450. doi: 10.1002/dev.20300. [DOI] [PubMed] [Google Scholar]
- Ashman SB, Dawson G, Panagiotides H, Yamada E, Wilkinson CW. Stress hormone levels of children of depressed mothers. Development and Psychopathology. 2002;14:333–349. doi: 10.1017/s0954579402002080. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Blair RJ. Neurobiological basis of psychopathy. British Journal of Psychiatry. 2003;182:5–7. doi: 10.1192/bjp.182.1.5. [DOI] [PubMed] [Google Scholar]
- Blair C, Diamond A. Biological processes in prevention and intervention: The promotion of self-regulation as a means of preventing school failure. Development and Psychopathology. 2008;20:899–911. doi: 10.1017/S0954579408000436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair C, Granger D, Razza RP. Cortisol reactivity is positively related to executive function in preschool children attending Head Start. Child Development. 2005;76:554–567. doi: 10.1111/j.1467-8624.2005.00863.x. [DOI] [PubMed] [Google Scholar]
- Boyce WT, Ellis BJ. Biological sensitivity to context: I. An evolutionary-developmental theory of the origins and functions of stress reactivity. Development and Psychopathology. 2005;17:271–301. doi: 10.1017/s0954579405050145. [DOI] [PubMed] [Google Scholar]
- Brotman LM. GIPCI: Unpublished manual. New York: University School of Medicine; 1998. [Google Scholar]
- Brotman LM, Gouley KK, Chesir-Teran D. Assessing peer entry and play in preschoolers at risk for maladjustment. Journal of Clinical Child and Adolescent Psychology. 2005;34:671–680. doi: 10.1207/s15374424jccp3404_9. [DOI] [PubMed] [Google Scholar]
- Brotman LM, Gouley KK, Chesir-Teran D, Dennis T, Klein RG, Shrout P. Prevention for preschoolers at high risk for conduct problems: Immediate outcomes on parenting practices and child social competence. Journal of Clinical Child & Adolescent Psychology. 2005;34:724–734. doi: 10.1207/s15374424jccp3404_14. [DOI] [PubMed] [Google Scholar]
- Brotman LM, Gouley KK, Huang K-Y, Kamboukos D, Fratto C, Pine DS. Effects of a psychosocial family-based preventive intervention on cortisol response to a social challenge in preschoolers at high risk for antisocial behavior. Archives of General Psychiatry. 2007;64:1172–1179. doi: 10.1001/archpsyc.64.10.1172. [DOI] [PubMed] [Google Scholar]
- Brotman LM, Gouley KK, Huang K-Y, Rosenfelt A, O’Neal CR, Klein RG, et al. Preventive intervention for preschoolers at high risk for antisocial behavior: Long-term effects on child physical aggression and parenting practices. Journal of Child Clinical and Adolescent Psychology. 2008;37:386–396. doi: 10.1080/15374410801955813. [DOI] [PubMed] [Google Scholar]
- Brotman LM, Gouley KK, O’Neal C, Klein RG. Preschool-aged siblings of adjudicated youths: Multiple risk factors for conduct problems. Early Education & Development. 2004;15:387–406. [Google Scholar]
- Brotman LM, O’Neal CR, Huang K-Y, Gouley KK, Rosenfelt A, Shrout P. An experimental test of parenting practices as a mediator or early childhood physical aggression. Journal of Child Psychiatry and Psychology. 2009;50:235–245. doi: 10.1111/j.1469-7610.2008.01929.x. [DOI] [PubMed] [Google Scholar]
- Caldji C, Diorio J, Meaney MJ. Variations in maternal care in infancy regulate the development of stress reactivity. Biological Psychiatry. 2000;48:1164–1174. doi: 10.1016/s0006-3223(00)01084-2. [DOI] [PubMed] [Google Scholar]
- Caldwell BM, Bradley RH. Home Observation for Measurement of the Environment–Revised Edition. Little Rock: University of Arkansas at Little Rock; 1984. [Google Scholar]
- Champagne FA, Meaney MJ. Stress during gestation alters postpartum maternal care and the development of the offspring in a rodent model. Biological Psychiatry. 2006;59:1227–1235. doi: 10.1016/j.biopsych.2005.10.016. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Gunnar MR. Integrating biological measures into the design and evaluation of preventive interventions. Development and Psychopathology. 2008;20:737–743. doi: 10.1017/S0954579408000357. [DOI] [PubMed] [Google Scholar]
- Cole DA, Maxwell SE. Testing mediational models with longitudinal data: Questions and tips in the use of structural equation modeling. Journal of Abnormal Psychology. 2003;112:558–577. doi: 10.1037/0021-843X.112.4.558. [DOI] [PubMed] [Google Scholar]
- Dadds MR, Rhodes R. Aggression in young children with concurrent callous-unemotional traits: Can the neurosciences inform progress and innovation in treatment approaches? Philosophical Transactions of the Royal Society B: Biological Sciences. 2008;363:2567–2576. doi: 10.1098/rstb.2008.0029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diggle P, Heagerty P, Liang K-Y, Zeger S. Analyses of longitudinal data. Oxford, UK: Oxford University Press; 2002. [Google Scholar]
- Dozier M, Peloso E, Lewis E, Laurenceau JP, Levine S. Effects of an attachment-based intervention on the cortisol production of infants and toddlers in foster care. Development and Psychopathology. 2008;20:845–859. doi: 10.1017/S0954579408000400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott SN. Differential Abilities Scale. San Antonio, TX: Psychological Corporation; 1990. [Google Scholar]
- Ellis BJ, Boyce WT. Biological sensitivity to context. Current Directions in Psychological Science. 2008;17:183–187. [Google Scholar]
- Fairchild AJ, MacKinnon DP. A general model for testing mediation and moderation effects. Prevention Science. 2009;10:87–99. doi: 10.1007/s11121-008-0109-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher PA, Gunnar MR, Chamberlain P, Reid JB. Preventative intervention for maltreated preschoolers: Impact on children’s behavior, neuroendocrine activity, and foster parent functioning. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:1356–1364. doi: 10.1097/00004583-200011000-00009. [DOI] [PubMed] [Google Scholar]
- Fisher PA, Gunnar MR, Dozier M, Bruce J, Pears KC. Effects of therapeutic interventions for foster children on behavioral problems, caregiver attachment, and stress regulatory neural systems. Annals of the New York Academy of Sciences. 2006;1094:215–225. doi: 10.1196/annals.1376.023. [DOI] [PubMed] [Google Scholar]
- Fisher PA, Stoolmiller M, Gunnar MR, Burraston BO. Effects of a therapeutic intervention for foster preschoolers on diurnal cortisol activity. Psychoneuroendocrinology. 2007;32:892–905. doi: 10.1016/j.psyneuen.2007.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleiss J, Levin B, Paik M. 3rd ed. Hoboken, NJ: Wiley; 2003. [Google Scholar]
- Francis DD, Caldji C, Champagne F, Plotsky PM, Meaney MJ. The role of corticotropin-releasing factor-norepinephrine systems in mediating the effects of early experience on the development of behavioral and endocrine responses to stress. Biological Psychiatry. 1999;46:1153–1166. doi: 10.1016/s0006-3223(99)00237-1. [DOI] [PubMed] [Google Scholar]
- Gunnar MR, Brodersen L, Nachmias M, Buss K, Rigatuso J. Stress reactivity and attachment security. Developmental Psychobiology. 1996;29:191–204. doi: 10.1002/(SICI)1098-2302(199604)29:3<191::AID-DEV1>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- Gunnar MR, Fisher PA the Early Experience, Stress and Prevention Network. Bringing basic research on early experience and stress neurobiology to bear on preventive interventions for neglected and maltreated children. Development and Psychopathology. 2006;18:651–677. [PubMed] [Google Scholar]
- Gunnar MR, Quevedo K. The neurobiology of stress and development. Annual Review of Psychology. 2007;58:145–173. doi: 10.1146/annurev.psych.58.110405.085605. [DOI] [PubMed] [Google Scholar]
- Gunnar MR, Vazquez DM. Low cortisol and a flattening of expected daytime rhythm: Potential indices of risk in human development. Development and Psychopathology. 2001;13:515–538. doi: 10.1017/s0954579401003066. [DOI] [PubMed] [Google Scholar]
- Hane AA, Fox NA. Ordinary variations in maternal caregiving influence human infants’ stress reactivity. Psychological Science. 2006;17:550–556. doi: 10.1111/j.1467-9280.2006.01742.x. [DOI] [PubMed] [Google Scholar]
- Hart D, Burock D, London B, Atkins R, Bonilla-Santiago G. The relation of personality types to physiological, behavioural, and cognitive processes. European Journal of Personality. 2005;19:391–407. [Google Scholar]
- Hart J, Gunnar M, Cicchetti D. Salivary cortisol in maltreated children: Evidence of relations between neuroendocrine activity and social competence. Development & Psychopathology. 1995;7:11–26. [Google Scholar]
- Heim C, Ehlert U, Hellhammer DH. The potential role of hypocortisolism in the pathophysiology of stress-related bodily disorders. Psychoneuroendocrinology. 2000;25:1–35. doi: 10.1016/s0306-4530(99)00035-9. [DOI] [PubMed] [Google Scholar]
- Hertsgaard L, Gunnar M, Erickson MG, Nachmias M. Adrenocortical responses to the strange situation in infants with disorganized/disoriented attachment relationships. Child Development. 1995;66:1100–1106. [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59:877–884. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- Levine S. Infantile experience and resistance to physiological stress. Science. 1957;126:405–406. doi: 10.1126/science.126.3270.405. [DOI] [PubMed] [Google Scholar]
- Liang K-Y, Zeger S. Longitudinal data analysis for discrete and continuous outcomes using Generalized Linear Models. Biometrika. 1986;84:3–32. [PubMed] [Google Scholar]
- Little R, Rubin D. Statistical analysis with missing data. Hoboken, NJ: Wiley; 2002. [Google Scholar]
- Liu D, Diorio J, Tannenbaum B, Caldji C, Francis D, Freedman A, et al. Maternal care, hippocampal glucocorticoid receptors, and hypothalamic-pituitary-adrenal responsesto stress. Science. 1997;277:1659–1662. doi: 10.1126/science.277.5332.1659. [DOI] [PubMed] [Google Scholar]
- Loney BR, Butler MA, Lima EN, Counts CA, Eckel LA. The relation between salivary cortisol, callous-unemotional traits, and conduct problems in an adolescent, non-referred sample. Journal of Child Psychology and Psychiatry. 2006;47:30–36. doi: 10.1111/j.1469-7610.2005.01444.x. [DOI] [PubMed] [Google Scholar]
- Lord FM, Novick MR. Statistical theories of mental test scores. Reading, MA: Addison-Wesley; 1968. [Google Scholar]
- Lupien SJ, King S, Meaney MJ, McEwen BS. Child’s stress hormone levels correlate with mother’s socioeconomic status and depressive state. Biological Psychiatry. 2000;48:976–980. doi: 10.1016/s0006-3223(00)00965-3. [DOI] [PubMed] [Google Scholar]
- Luthar SS, Cicchetti D, Becker B. The construct of resilience: A critical evaluation and guidelines for future work. Child Development. 2000;71:543–562. doi: 10.1111/1467-8624.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBurnett K, King J, Scarpa A. The HPA and the development of aggressive, antisocial, and substance abuse disorders. In: Cicchetti D, Walker E, editors. Neurodevelopmental mechanisms in psychopathology. New York: Cambridge University Press; 2003. pp. 324–344. [Google Scholar]
- McBurnett K, Lahey BB, Rathouz PJ, Loeber R. Low salivary cortisol and persistent aggression in boys referred for disruptive behavior. Archives of General Psychiatry. 2000;57:38–43. doi: 10.1001/archpsyc.57.1.38. [DOI] [PubMed] [Google Scholar]
- Meaney MJ. Maternal care, gene expression, and the transmission of individual differences in stress reactivity across generations. Annual Review of Neuroscience. 2001;24:1161–1192. doi: 10.1146/annurev.neuro.24.1.1161. [DOI] [PubMed] [Google Scholar]
- Nachmias M, Gunnar M, Mangelsdorf S, Parritz RH, Buss K. Behavioral inhibition and stress reactivity: The moderating role of attachment security. Child Development. 1996;67:508–522. [PubMed] [Google Scholar]
- Pajer K, Gardner W, Rubin RT, Perel J, Neal S. Decreased cortisol levels in adolescent girls with conduct disorder. Archives of General Psychiatry. 2001;58:297–302. doi: 10.1001/archpsyc.58.3.297. [DOI] [PubMed] [Google Scholar]
- Popma A, et al. Hypothalamus pituitary adrenal axis and autonomic activity during stress in delinquent male adolescents and controls. Psychoneuroendocrinology. 2006;31:948–957. doi: 10.1016/j.psyneuen.2006.05.005. [DOI] [PubMed] [Google Scholar]
- Raine A. Features of borderline personality and violence. Journal of Clinical Psychology. 1993;49:277–281. doi: 10.1002/1097-4679(199303)49:2<277::aid-jclp2270490222>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- Raine A, Venables PH, Dalais C, Mellingen K, Reynolds C, Mednick SA. Early educational and health enrichment at age 3–5 years is associated with increased autonomic and central nervous system arousal and orienting at age 11 years: Evidence from the Mauritius Child Health Project. Psychophysiology. 2001;38:254–266. [PubMed] [Google Scholar]
- Robinson EA, Eyberg SM. The dyadic parent–child interaction coding system: Standardization and validation. Journal of Consulting and Clinical Psychology. 1981;49:245–250. doi: 10.1037//0022-006x.49.2.245. [DOI] [PubMed] [Google Scholar]
- Rutter M. Introduction. Philosophical Transactions of the Royal Society B: Biological Sciences. 2008;363:2485–2489. doi: 10.1098/rstb.2008.0038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter M, Moffitt TE, Caspi A. Gene-environment interplay and psychopathology: Multiple varieties but real effects. Journal of Child Psychology and Psychiatry. 2006;47:226–261. doi: 10.1111/j.1469-7610.2005.01557.x. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Schreiber JE, Shirtcliff E, VanHulle C, Lemery-Chalfant K, Klein MH, Kalin NH, et al. Environmental influences on family similarity in afternoon cortisol levels: Twin and parent-offspring designs. Psychoneuroendocrinology. 2006;31:1131–1137. doi: 10.1016/j.psyneuen.2006.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrout PE, Fleiss JL. Intraclass correlations: Uses in assessing rater reliability. Psychological Bulletin. 1979;86:420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- Snoek H, Van Goozen S, Matthys W, Buitelaar JK, Van Engeland H. Stress responsivity in children with externalizing behavior disorders. Development and Psychopathology. 2004;16:389–406. doi: 10.1017/s0954579404044578. [DOI] [PubMed] [Google Scholar]
- Sobel ME. Effect analysis and causation in linear structural equation models. Psychometrika. 1990;55:495–515. [Google Scholar]
- Thompson LA, Trevathan WR. Cortisol reactivity, maternal sensitivity, and learning in 3-month-old infants. Infant Behavior and Development. 2008;31:92–106. doi: 10.1016/j.infbeh.2007.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tremblay RE. Understanding development and prevention of chronic physical aggression: Towards experimental epigenetic studies. Philosophical Transactions of the Royal Society B: Biological Sciences. 2008;363:2613–2622. doi: 10.1098/rstb.2008.0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van de Wiel NMH, van Goozen SHM, Matthys W, Snoek H, van Engeland H. Cortisol and treatment effect in children with disruptive behavior disorders: A preliminary study. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:1011–1018. doi: 10.1097/01.chi.0000126976.56955.43. [DOI] [PubMed] [Google Scholar]
- van Goozen S, Fairchild G, Snoek H, Harold GT. The evidence for a neurobiological model of childhood antisocial behavior. Psychological Bulletin. 2007;133:149–182. doi: 10.1037/0033-2909.133.1.149. [DOI] [PubMed] [Google Scholar]
- van Goozen SH, Matthys W, Cohen-Kettenis PT, Buitelaar JK, van Engeland H. Hypothalamic-pituitary-adrenal axis and autonomic nervous system activity in disruptive children and matched controls. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:1438–1445. doi: 10.1097/00004583-200011000-00019. [DOI] [PubMed] [Google Scholar]
- van Goozen SH, Matthys W, Cohen-Kettenis PT, Gispen-de Wied C, Wiegant VM, van Engeland H. Salivary cortisol and cardiovascular activity during stress in oppositional-defiant disorder boys and normal controls. Biological Psychiatry. 1998;43:531–539. doi: 10.1016/S0006-3223(97)00253-9. [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C. Comparisons of behavior transactions between conduct-disordered children and their mothers in the clinic and at home. Journal of Abnormal Child Psychology. 1985;13:169–183. doi: 10.1007/BF00910640. [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C. Incredible years dinosaur social skills and problem-solving curriculum. Seattle, WA: Incredible Years Press; 1990. [Google Scholar]
- Webster-Stratton C, Hancock L. Training for parents of young children with conduct problems: Content, methods, and therapeutic processes. In: Schaefer CE, Beriesmeister JM, editors. Handbook of parenting training. New York: Wiley; 1998. pp. 98–152. [Google Scholar]
- Webster-Stratton C, Reid M, Hammond M. Treating children with early-onset conduct problems: Intervention outcomes for parent, child, and teacher training. Journal of Clinical Child & Adolescent Psychology. 2004;33:105–124. doi: 10.1207/S15374424JCCP3301_11. [DOI] [PubMed] [Google Scholar]
- Williams JB, Gibbon M, First MB, Spitzer RL, Davies M, Borus J, et al. The Structured Clinical Interview for DSM–III–R (SCID): II. Multisite test–test reliability. Archives of General Psychiatry. 1992;49:630–636. doi: 10.1001/archpsyc.1992.01820080038006. [DOI] [PubMed] [Google Scholar]
- Young EA, Vazquez D, Jiang H, Pfeffer CR. Saliva cortisol and response to dexamethasone in children of depressed parents. Biological Psychiatry. 2006;60:831–836. doi: 10.1016/j.biopsych.2006.03.077. [DOI] [PubMed] [Google Scholar]
- Zeger S, Liang K-Y, Albert P. Models for longitudinal data: A generalized estimating equation approach. Biometrics. 1988;44:1049–1060. [PubMed] [Google Scholar]
- Zuckerman M. Sensation seeking: Beyond the optimal level of arousal. Hillsdale, NJ: Erlbaum; 1979. [Google Scholar]