Abstract
The function of the right heart is to pump blood through the lungs, thus linking right heart physiology and pulmonary vascular physiology. Inflammation is a common modifier of heart and lung function, by elaborating cellular infiltration, production of cytokines and growth factors, and by initiating remodeling processes 1.
Compared to the left ventricle, the right ventricle is a low-pressure pump that operates in a relatively narrow zone of pressure changes. Increased pulmonary artery pressures are associated with increased pressure in the lung vascular bed and pulmonary hypertension 2. Pulmonary hypertension is often associated with inflammatory lung diseases, for example chronic obstructive pulmonary disease, or autoimmune diseases 3. Because pulmonary hypertension confers a bad prognosis for quality of life and life expectancy, much research is directed towards understanding the mechanisms that might be targets for pharmaceutical intervention 4. The main challenge for the development of effective management tools for pulmonary hypertension remains the complexity of the simultaneous understanding of molecular and cellular changes in the right heart, the lungs and the immune system.
Here, we present a procedural workflow for the rapid and precise measurement of pressure changes in the right heart of mice and the simultaneous harvest of samples from heart, lungs and immune tissues. The method is based on the direct catheterization of the right ventricle via the jugular vein in close-chested mice, first developed in the late 1990s as surrogate measure of pressures in the pulmonary artery5-13. The organized team-approach facilitates a very rapid right heart catheterization technique. This makes it possible to perform the measurements in mice that spontaneously breathe room air. The organization of the work-flow in distinct work-areas reduces time delay and opens the possibility to simultaneously perform physiology experiments and harvest immune, heart and lung tissues.
The procedural workflow outlined here can be adapted for a wide variety of laboratory settings and study designs, from small, targeted experiments, to large drug screening assays. The simultaneous acquisition of cardiac physiology data that can be expanded to include echocardiography5,14-17 and harvest of heart, lung and immune tissues reduces the number of animals needed to obtain data that move the scientific knowledge basis forward. The procedural workflow presented here also provides an ideal basis for gaining knowledge of the networks that link immune, lung and heart function. The same principles outlined here can be adapted to study other or additional organs as needed.
Keywords: Immunology, Issue 71, Medicine, Anatomy, Physiology, Cardiology, Surgery, Cardiovascular Abnormalities, Inflammation, Respiration Disorders, Immune System Diseases, Cardiac physiology, mouse, pulmonary hypertension, right heart function, lung immune response, lung inflammation, lung remodeling, catheterization, mice, tissue, animal model
Protocol
1. Preparation
- Prepare the following solutions and tubes (Table 1) as follows:
- Hanks solution, no calcium, magnesium or indicator with Penicillin (100 U/ml) / Streptomycin (100 mg/ml).
- Phosphate buffered saline (PBS), 1x, no calcium, no magnesium.
- Ethanol, 70 %, make 500 ml.
- Buffered formaldehyde, 7-10 % with PBS, make 500 ml.
- Anaesthesia solutions:
- Avertin. Carefully add 5 ml of 2-Methyl-2-butanol to 5 g of 2,2,2-Tribromoethanol. Once dissolved, keep stock solution at room temperature in the dark. Take 0.25 ml of the stock solution and dilute it with 10 ml of 1xPBS in glass bottom bottle. Wrap the bottle with aluminium foil, place at 37 °C until dissolved and then aliquot into 5 ml polypropylene tubes and keep in refrigerator. Warm one aliquot on the morning of the experiment.
- Barbiturate. Dilute stock solution with PBS to give 2.6% barbiturate solution. Place 3-4 ml aliquots in polypropylene tubes.
Organize three work-areas (Figure 1).
- Area A: Arrange the following items: study form to record study identification number, date, body weight, weights of right heart, left heart and septum; precision scale (0-50 g at 0.01 g precision) to determine body weight; micro scale to determine heart weights at 0.001 g precision; weigh boats; anaesthesia solutions (clearly marked); small dewar with liquid nitrogen; insulated container with ice; tubes and 24-well plate to collect blood and tissue specimens (Table 1); surgical instruments (Table 2, Figure 2); and solutions to clean the instruments (Table 1).
- Area B: Arrange the following items: dissecting microscope; right heart catheter connected to a pressure control unit that is connected to an amplifier and laptop computer. The catheter is placed into a beaker containing water. Arrange surgical instruments (Table 2), pieces of suture cut to optimal length and placed into a weigh boat; tape (autoclave tape is optimal) cut to optimal length and width and lined up on microscope or lab bench for easy access; cotton swabs and hair remover solution. Calibrate the catheter at the beginning of the study.
- Area C: Arrange the following items: magnifier lens; tracheal cannula; 1 ml syringes; suture cut to optimal length and placed into a weigh boat; small dewar with liquid nitrogen; insulated container with ice; tubes and 24-well plate to collect BAL and tissue specimens (Table 1); surgical instruments (Table 2); solutions to perform BAL and to clean the tracheal cannula and the instruments (Table 1).
2. Right Heart Catheterization
Weigh mouse using a precision scale by gently placing mouse into a weigh boat. Make sure to handle the animal gently and quietly. Record weight. The described protocol works best for mice that are 20 g or more because the diameter of the jugular vein has to accommodate the pressure catheter; it is possible to catheterize smaller mice (17 g or more) as long as the vein is large enough.
Anaesthetize the mouse by injection with Avertin depending on the body weight (10 μl/g), e.g. for 20 g give 200 μl, for 25 g give 250 μl, for 30 g give 300 μl. The exact injection volume needs to be adjusted depending on the mouse strain. Make sure to handle the animal gently and quietly because stress can alter the response to the anaesthetic.
Once the mouse is sedated, place on double-pleated tissue paper. Note the ID number on the paper. Gently rub hair removal lotion into the ventral aspect of the neck to clear the surgical field. Place the mouse back onto the paper and wait for 1-2 min.
Remove hair from the ventral aspect of the neck by gently stroking the hair against the direction of the hair growth with cotton swabs.
Carefully determine the sufficient depth of anaesthesia by checking for the absence of the toe reflex: the mouse does not react to pinching of its toes.
Working quickly and relaxed, the remainder of the right heart catheterization should not take more than 10 min, optimally 3-6 min. It is important that the tissue does not dry out because the catheter needs to glide into the vein and move inside of the vein on a layer of moisture. Consistent timing of the procedure is important for the generation of data that are comparable between groups.
Place mouse back on tissue paper and transfer with tissue paper onto styrofoam board. Fix paws and head into place using autoclave tape.
Make incision of skin from mandibles to sternum (breast-bone).
Carefully dissect the thyroid grand upwards towards the mandibles to expose the right jugular vein and trachea.
Place styrofoam board holding the mouse underneath the dissection microscope with the focus plane already in place and the lens at approximately 0.8x magnification (total magnification [lens x eye piece] is approximately 8x.
Carefully microdissect the right jugular vein by removing surrounding connective tissue with surgical forceps.
Place two pieces of suture on top of the right jugular vein. Tie the suture closest to the mandibles to close off blood flow in the vein to a tiny trickle, place the suture that is closest to the sternum / breast-bone at a loose knot around the vein. One can use the tiny trickle of blood to later find the hole in the vein, should this become necessary.
Breathe and relax (loosen the muscles in the neck and jaw) to keep your eyes on the vein through the eyepiece. This will ensure that your hands and fingers will move securely, smoothly and relaxed. While holding the vein with forceps at the side closest to the mandibles, cut a hole into the vein between the two sutures using micro-scissors operated by the other hand. Put down the micro-scissors, and keeping that hand relaxed, feel for the catheter. Gently retrieve the catheter holding it between thumb and first finger (Figure 3). Insert the catheter into the hole of the vein.
Gently advance the catheter into the right heart (Figure 3). Observe the marks at the catheter that give an approximate index of how far the catheter needs to be inserted and observe the monitor. Once the pressure curves are displayed, gently tighten the lower suture around the catheter. Because the catheter has tensile strength that gives it a coil, and because the breathing and heart beat of the mouse add motion, additionally affix the catheter using tape.
Record pressure measurements for 2 min for later analysis (Figure 4).
Open the suture holding the catheter, then gently retrieve catheter. Wipe the part behind the pressure transducer, place back into the beaker with water. Do not touch the pressure transducer.
Transfer the mouse on top of the tissue paper to area A for euthanasia, collection of blood and spleen tissue. Clean surgical instruments.
Start the procedure with the next animal. When the timing permits, inject the anaesthetic while waiting to record the pressure curve (2.15).
3. Collection of Blood and Spleen Samples
Inject barbiturate solution, 400 μl per mouse and wait for 1-2 min. This is routinely performed in our laboratory to avoid the possibility that the mice inadvertently recover from avertin-anaesthesia while being bled. Appropriate standardization of the experiment is achieved by injecting the same dose of barbiturate solution per mouse, and by waiting the same amount of time prior to harvest of blood. If permitted by the Institutional Animal Care and Use Committee and as long as the animals are carefully monitored for the depth of anaesthesia prior to exsanguination, this step can be omitted.
Make incision into the abdomen. Open the caudal vein (vena cava) and collect blood using a transfer pipette.
Remove the spleen, or a piece of the spleen into the Eppendorf tube and snap freeze in liquid nitrogen, or into the 24 well plate into a well containing Hanks buffer for later preparation of single cells.
Transfer the mouse on top of the tissue paper to work-area C for collection of BAL, lung draining lymph node, lung, and heart tissues. Clean surgical instruments.
4. Collection of Lung and Heart Samples
Dissect the trachea free of muscle and connective tissue. Placing forceps under the trachea, pull suture through. Gently generate sufficient stretch to cut a hole. Maintaining the gentle stretch, insert the tracheal cannula using a slightly turning motion, and suture cannula into place. For the insertion of the tracheal cannula, make sure that the trachea is moist, if necessary add a drop of Hanks solution. Throughout the procedure, breathe, relax neck and jaw muscles, to keep hand movements secure and smooth.
Dissect open the rib cage by carefully removing the breast-bone starting from the abdominal end. Do not disturb the contents of the thorax because this will make it very hard to find the lymph node.
Perform bronchoalveolar lavage (BAL) by gently inserting 1 ml of Hanks buffer, gently turn the syringe and retrieve BAL fluid. Repeat 3 times, close tube and place on ice. Throughout the procedure, keep eyes on the end of the tracheal cannula that connects to the syringe. Glance to thorax to observe the inflation and deflation of the lungs.
Harvest lung lymph node by holding rib cage wall with one set of forceps, finding and retrieving the lymph node with another forceps. Place lymph node into 24 well plate. It is important to know where to search: starting from the neck, find the entrance of the rib cage from the right side of the mouse and look above the spine (Figure 5).
Harvest heart and place on tissue paper. Isolate the right heart by carefully dissecting alongside the septum. Transfer to work-area A to weigh, record the weight and place into eppendorf tubes to snap freeze in liquid nitrogen.
Place suture around the left lung lobe to close the main bronchus. Dissect the left lung lobe free, place into eppendorf tube and snap freeze in liquid nitrogen, or place into a well of a 24 well plate containing Hanks solution for later isolation of single cell suspensions.
Insert approx. 0.5 ml buffered formaldehyde solution through the tracheal cannula into the remaining lung lobes. After inflation, dissect the lung lobes out of the thorax and place into 50 ml tube containing formaldehyde solution. For an alternative study design, the lungs can be inflated with optimal cutting media (OCT, diluted 1:4 with PBS) and frozen in a mold containing undiluted OCT for later preparation of frozen sections. Another study design might necessitate obtaining snap frozen lung tissue and single cell suspensions from the lungs. In that case, no inflation is necessary: dissect the remaining lung lobes; retrieve them from the thorax and place into the 24 well plate into a well containing Hanks buffer.
Remove tracheal cannula, clean by rinsing with Hanks buffer, clean surgical instruments.
5. Analysis of Pressure Curves Generated from the Right Heart Catheter
The recorded right ventricular pressure data are analyzed using LabChart 7 software with no knowledge of the group identity of each recording. More than 20 curves are selected randomly and the difference between maximum and minimum ventricular pressure for each curve measured (ΔP). The average ΔP is calculated to give the right ventricular systolic pressure.
Representative Results
The primary outcome for obtaining right heart pressure curves is achieved by the correct position of the right heart catheter. The shape of the pressure time curves is critical because the correct placement of the catheter inside of the right ventricle will result in pressure plateaus (Figure 4). Spiky curves, instead, indicate a catheter that is moved by the breathing or heart beat motion against the wall of the right ventricle. To detect potential problems with the stage of survival of the animals, the standard deviation of the ΔP, and the heart rate needs to be calculated. Both values are expected to be not significantly different between treatment groups. Furthermore, the expectation is that the ΔP values and the heart rate do not show a drift across the recording time. For example, slowly increasing ΔP values would indicate hypoxic pulmonary vasoconstriction 18-20. Decreasing heart rate would indicate that the level of anaesthesia is too high leading to the death of the animal. In our laboratory different people perform the procedure. Across all groups of mice we routinely achieve 90-95 % success rates in obtaining right ventricular pressure data.
While learning the procedure, it is best to start with older female mice (25-30 g and more) that have a larger jugular vein and tend to have less subcutaneous fat deposits than male mice. The best way to ascertain the placement of the catheter is to euthanize the animal as soon as the catheter is secured inside of the vein. Dissect the animal starting from the heart to directly visualize the placement of the catheter. This will greatly facilitate problem solving.
The first outcome for obtaining BAL fluid is the correct placement of the tracheal cannula. This is indicated by the inflation of the lungs when Hanks buffer is instilled, and deflation of the lungs when the buffer is removed. The expected recovery is 70-80 % of the instilled volume in control animals, less (down to 50 %) in animals that have lung inflammation. Foam on top of the recovered BAL fluid indicates the presence of surfactant. Blood contamination of the recovered BAL fluid either occurs because of the presence of significant lung inflammation, or because instillation and recovery of the wash fluid was too fast. It is of note that some acute measures of injury within the lungs can be induced by the BAL procedure. If the experimental design is to understand these acute injury parameters and examination of BAL is also important, then one lung lobe needs to be tied off and removed prior to conducting BAL.
In the procedure shown here, we harvest lung tissues for histology without standardized inflation and perfusion of the lungs. In cases where exact histological morphometry is the major read-out, the lungs should be inflated via the trachea, and perfusion should be performed via the pulmonary artery, all under standardized pressure.
In the protocol shown, the heart is dissected to provide the Fulton index as measure of right heart hypertrophy (weight of right ventricle / weight of left ventricle and septum). In addition, new methods are being developed that are based on histological evaluation of the right heart. Emerging histological measures of right heart hypertrophy are a) the number of nuclei within a defined area of randomly selected right heart, and b) counts of vessels, and fibrotic index per area of heart.
In our laboratory, the correct recovery of lung draining mediastinal and tracheobronchial lymph nodes (Figure 5) is routinely verified by flow cytometry because these tissues are very small in control mice. However, depending on the microbiome in the housing facility and the age of the animals, the size of the lymph nodes in unchallenged, control mice may be sufficiently large for only visual confirmation. When verifying by flow cytometry, lymph node cells need to be distinguished from thymocytes. By accident, the thymus can easily be sampled together with the lymph node because the thymus and the lymph nodes are located close to each other and are contained within the rib cage. The distinction is that the thymus is located close to the breast-bone and the lymph node close to the spine. Further challenging is that the thymus is very big, containing many more cells than the small lymph nodes. Thymocytes can easily be distinguished from lymph node cells by using flow cytometry and CD3, CD4, and CD8 markers. Lymph nodes have characteristically CD3+ cells, the majority of which are either positive for CD4 or CD8. In contrast, the majority of thymocytes are positive for all three markers (CD3+, CD4+, CD8+). Further in depth information on the localization of mouse lymph nodes can be found in the manuscript by van den Broeck et al.21.
Consistent timing of each main procedural step (heart catheterization, recovery of blood and spleen, harvest of BAL, lung and heart tissues) is critical for the generation of data that allows for robust comparison between treatment groups. Therefore, it is recommended that at least two, and best three, investigators collaborate to accomplish the experiment. Furthermore, it is critical that the investigators perform the procedure without knowledge of the group identity of the animals. Therefore, the identification of the data has to be made in a manner that obscures the group identity. Finally, it is also important that the order in which the animals are analyzed is randomized. For example, a simple identifier is the date of the experiment and consecutive numbering of the animals. If there are for example 4 groups of animals (A-D), assign identification and study the animals in the following order: date_1: Aa, date_2: Ba, date_3: Ca, date_4: Da, date_5: Ab, date_6: Bb, date_7: Cb, and so on.
This experimental flow allows for an in-depth, simultaneous study of the molecular mechanisms that control lung inflammation and right heart function. The simultaneous data and sample collection achieves better insights into molecular networks, and a reduction in the number of animals needed to obtain novel biological knowledge.
| Type of tube / beaker | Solution (volume) | Utilization |
| Processing of blood | ||
| Eppendorf, 1.5 ml | Blood for serum | |
| EDTA coated 2.0 ml | Blood for plasma | |
| Eppendorf, 0.5 ml | Freeze serum or plasma | |
| Processing of BAL | ||
| Polypropylene, round bottom, 4.5 ml | Collect bronchoalveolar lavage | |
| Polypropylene, round bottom, 4.5 ml | Freeze BAL supernatant | |
| 96-well plate, skirted | BAL cells | |
| Processing of tissue | ||
| Polypropylene, 50 ml | Formaldehyde, 7.5 ml | Fix lung tissue |
| Eppendorf, 1.5 ml | Snap freeze lung lobe | |
| Eppendorf, 1.5 ml | Snap freeze right heart | |
| Eppendorf, 1.5 ml | Snap freeze left heart | |
| 24-well plate | Hanks buffer, 0.5-1 ml | Quick-storage of lung lobes for later isolation of single cells |
| 24-well plate | Hanks buffer, 0.5-1 ml | Quick storage of spleens for later isolation of single cells |
| 24-well plate | Hanks buffer, 0.5-1 ml | Quick storage of lymph nodes for later isolation of single cells |
| For the procedures | ||
| Glass beaker, 300 ml | Autoclaved water | Moisturizing and cleaning catheter |
| Polypropylene tube, 50 ml | Hanks buffer, 50 ml | Perform BAL |
| Polypropylene tube, 50 ml | Hanks buffer, 50 ml | Wash tracheal cannula |
| Polypropylene tube, 50 ml | Disinfectant solution | Cleaning instruments |
| Polypropylene tube, 50 ml | 70 % ethanol | Cleaning instruments |
| Polypropylene tube, 50 ml | Tap water | Cleaning instruments |
Table 1. Preparation and organization of tubes and solutions.
| Instrument | Description | Use |
| Scissors | rounded or straight 5.5 inch, round or sharp ends | Area A |
| Scissors | rounded 4.0 inches, sharp ends | |
| Forceps | 4.5 inch, bent, with flat, grasping ends | |
| Forceps | 4.0 inch, bent, with flat, grasping ends | |
| Scissors | Slim Blades/Angled- 9 cm | Area B |
| Micro-scissors | Vannas Spring Scissors - 2 mm Blades | |
| Forceps | forceps (Dumon #5 Fine) | |
| Forceps | 4.0 inch, bent, with flat, grasping ends | |
| Forceps | 4.0 inch, straight, with flat, grasping ends | |
| Suture | Braided Silk Suture 6-0 | |
| Catheter | Pressure catheter | |
| Scissors | rounded or straight 5.5 inch, round or sharp ends | Area C |
| Scissors | rounded 4.0 inches, sharp ends | |
| Forceps | 4.5 inch, bent, with flat, grasping ends | |
| Forceps | 4.0 inch, bent, with flat, grasping ends | |
| Cannula | Tracheal cannula | |
| Suture | Braided Silk Suture 4-0 |
Table 2. Organization of instruments, suture, catheter, tracheal cannula.
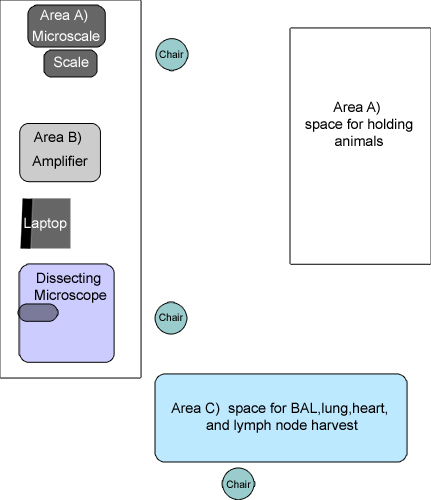 Figure 1. Schematic sketch of the work-areas. A) Work-area A for recording, weighing, collection of blood and spleen tissue and temporary holding space for the animals. B) Work-area B for right heart catheterization. C) Work-area C for harvest of BAL, lungs, lung lymph node, and heart tissues.
Figure 1. Schematic sketch of the work-areas. A) Work-area A for recording, weighing, collection of blood and spleen tissue and temporary holding space for the animals. B) Work-area B for right heart catheterization. C) Work-area C for harvest of BAL, lungs, lung lymph node, and heart tissues.
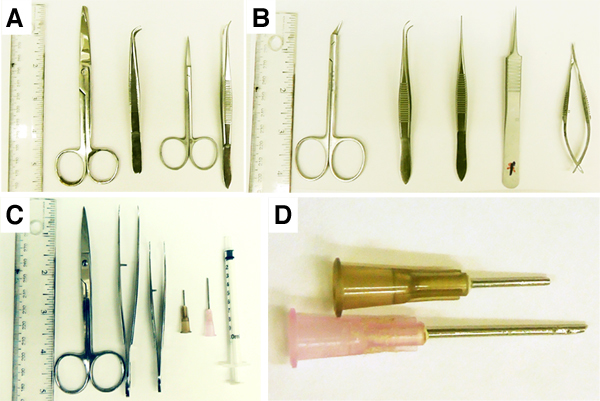 Figure 2. Instruments used for the procedure. A) Instruments for work-area A; B) instruments for right heart catheterization (work-area B); C) instruments for work-area C. D) Tracheal cannulas. The ruler shows the size of the instruments.
Figure 2. Instruments used for the procedure. A) Instruments for work-area A; B) instruments for right heart catheterization (work-area B); C) instruments for work-area C. D) Tracheal cannulas. The ruler shows the size of the instruments.
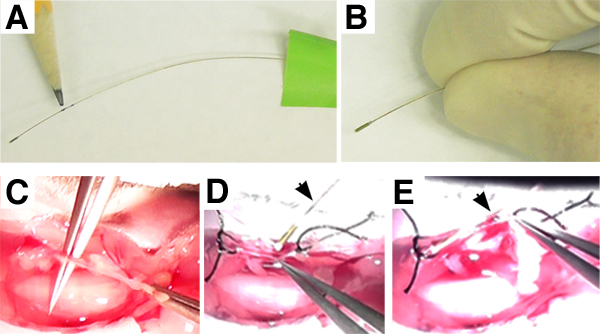 Figure 3. Right heart catheter. Right heart catheter shown with marks and tape (A), or held by hand (B). The pencil points to the marks made on the catheter (A). Insertion of the catheter (C-E): cleaning of the right jugular vein (C); sutured vein held with forceps, catheter is being advanced towards a hole previously made into the vein (D); catheter following insertion into the vein (E). Arrows point to the catheter (D, E).
Figure 3. Right heart catheter. Right heart catheter shown with marks and tape (A), or held by hand (B). The pencil points to the marks made on the catheter (A). Insertion of the catheter (C-E): cleaning of the right jugular vein (C); sutured vein held with forceps, catheter is being advanced towards a hole previously made into the vein (D); catheter following insertion into the vein (E). Arrows point to the catheter (D, E).
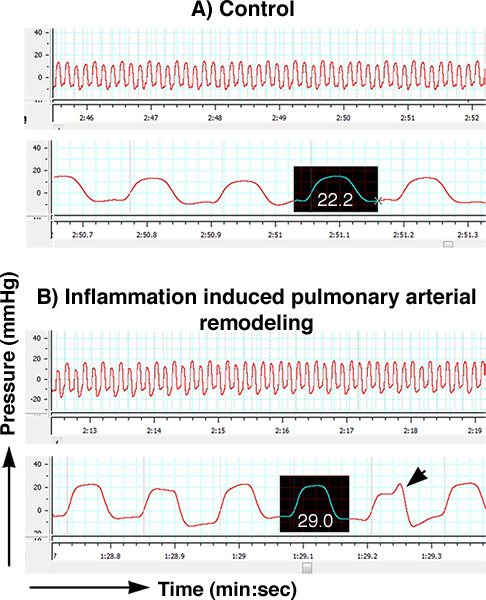 Figure 4. Sample trace of pressure changes in the right heart. The traces show pressure changes (mmHg) over time (min : sec); the software displays each of the curves at two different speeds. The traces of a control mouse (A); and a mouse with inflammation induced pulmonary arterial remodeling and hypertension (B) are shown. Curves used for the measurement of the right systolic ventricular pressure are highlighted. Note the clear pressure plateaus in the highlighted curves. The arrow points to a curve that has a spike indicating a technical error. These spiky types of curves cannot be used for measurement of right ventricular systolic pressures. Click here to view larger figure.
Figure 4. Sample trace of pressure changes in the right heart. The traces show pressure changes (mmHg) over time (min : sec); the software displays each of the curves at two different speeds. The traces of a control mouse (A); and a mouse with inflammation induced pulmonary arterial remodeling and hypertension (B) are shown. Curves used for the measurement of the right systolic ventricular pressure are highlighted. Note the clear pressure plateaus in the highlighted curves. The arrow points to a curve that has a spike indicating a technical error. These spiky types of curves cannot be used for measurement of right ventricular systolic pressures. Click here to view larger figure.
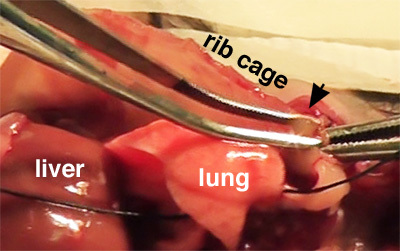 Figure 5. Location of a mediastinal / tracheobronchial lymph node relative to rib cage and spine. The arrow points to the lymph node.
Figure 5. Location of a mediastinal / tracheobronchial lymph node relative to rib cage and spine. The arrow points to the lymph node.
Discussion
The experimental flow outlined here allows for rapid and simultaneous measurement of right ventricular systolic pressure and harvest of samples for the analysis of the responses in the lungs, heart and the immune system in mice. The procedure combines heart physiology measurements, micro-dissection and subsequent tissue harvest for live cell studies, histological analysis, or omics-analysis of the tissues. The complete procedure takes less than 20 min per mouse. Because of the work-area-organized workflow, 2-3 animals can be studied simultaneously. Therefore, the procedure is suitable for small, targeted experiments 12 and large scale screens performed in a wide range of settings, from a small laboratory to a large pharmaceutical study.
The combination of heart physiology measurements and tissue harvest opens the possibility to perform analysis designed to detect biological networks that control or synchronize heart, lung and immune function, utilizing transgenic and KO mouse resources. An important advantage of the simultaneous procedure flow is the reduction in the number of animals needed per study. Another application of this procedural workflow is the possibility to study other or additional organs from the same animal as needed.
The procedure outlined here generates right heart pressure data very rapidly, within 5-10 min of anaesthesia induction. This makes it possible to study the animals while they are breathing room air spontaneously. A limitation of the approach is that it is invasive: the animals are anaesthetized, they are placed onto their backs, and a catheter is passed via the jugular vein through the atrium into the right ventricle. The limitation is also the advantage of this procedure because the data represent direct measurements of pressure changes over time in the right ventricle. Further technical improvements, particularly relying on miniaturizing the pressure catheters, may allow to place permanent, indwelling catheters in mice that allow for the direct recording of the pulmonary artery pressure over several weeks time, as is being performed in rats 22-24 and other larger animals. If insertion of a heart-catheter through the jugular vein in close-chested, spontaneously breathing animals is not possible, an alternative recording of right ventricular systolic pressure changes can be made in ventilated animals by opening of the thorax and placing the pressure catheter through an incision directly into the right ventricle 25. Non-invasive measurements of right heart function can be made using echocardiography. This procedure can either be performed prior to right heart catheterization, or mice can be examined by echocardiography for multiple times to study disease progression prior to the invasive measurements5,14-17.
Another application of this procedure is to obtain additional data. As an example, using a catheter that can measure flows and pressure, right heart output could be simultaneously recorded together with right heart pressure changes. The procedure outlined here can also be used to further understand the physiologic, cellular and molecular changes that are triggers of pulmonary hypertension other than the immune response, for example, genetic mutations 8,10, cigarette smoke exposure 26, or microbial infections 27-29.
Disclosures
No conflicts of interest declared.
Acknowledgments
This work was funded by the National Institutes of Health 1R21HL092370-01 (GG), 1R01 HL095764-01 (GG); R01HL082694 (JW); American Heart Association, Founders affiliate (0855943D, GG); Stony Wold - Herbert Fund, New York (SHP).
References
- Price LC, et al. Inflammation in pulmonary arterial hypertension. Chest. 2012;141:210–221. doi: 10.1378/chest.11-0793. [DOI] [PubMed] [Google Scholar]
- Olschewski H, et al. Cellular pathophysiology and therapy of pulmonary hypertension. J. Lab. Clin. Med. 2001;138:367–377. doi: 10.1067/mlc.2001.119285. [DOI] [PubMed] [Google Scholar]
- Hassoun PM, et al. Inflammation, growth factors, and pulmonary vascular remodeling. J. Am. Coll. Cardiol. 2009;54:S10–S19. doi: 10.1016/j.jacc.2009.04.006. [DOI] [PubMed] [Google Scholar]
- Rabinovitch M. Molecular pathogenesis of pulmonary arterial hypertension. J. Clin. Invest. 2008;118:2372–2379. doi: 10.1172/JCI33452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steudel W, et al. Sustained pulmonary hypertension and right ventricular hypertrophy after chronic hypoxia in mice with congenital deficiency of nitric oxide synthase 3. J. Clin. Invest. 1998;101:2468–2477. doi: 10.1172/JCI2356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaidi SH, You XM, Ciura S, Husain M, Rabinovitch M. Overexpression of the serine elastase inhibitor elafin protects transgenic mice from hypoxic pulmonary hypertension. Circulation. 2002;105:516–521. doi: 10.1161/hc0402.102866. [DOI] [PubMed] [Google Scholar]
- Guignabert C, et al. Tie2-mediated loss of peroxisome proliferator-activated receptor-gamma in mice causes PDGF receptor-beta-dependent pulmonary arterial muscularization. Am. J. Physiol. Lung Cell Mol. Physiol. 2009;297:L1082–L1090. doi: 10.1152/ajplung.00199.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West J, et al. Pulmonary hypertension in transgenic mice expressing a dominant-negative BMPRII gene in smooth muscle. Circ. Res. 2004;94:1109–1114. doi: 10.1161/01.RES.0000126047.82846.20. [DOI] [PubMed] [Google Scholar]
- Cook S, et al. Increased eNO and pulmonary iNOS expression in eNOS null mice. Eur. Respir. J. 2003;21:770–773. doi: 10.1183/09031936.03.00121203. [DOI] [PubMed] [Google Scholar]
- West J, et al. Mice expressing BMPR2R899X transgene in smooth muscle develop pulmonary vascular lesions. Am. J. Physiol. Lung Cell Mol. Physiol. 2008;295:L744–L755. doi: 10.1152/ajplung.90255.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tu L, et al. Autocrine fibroblast growth factor-2 signaling contributes to altered endothelial phenotype in pulmonary hypertension. Am. J. Respir. Cell Mol. Biol. 2011;45:311–322. doi: 10.1165/rcmb.2010-0317OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daley E, et al. Pulmonary arterial remodeling induced by a Th2 immune response. J. Exp. Med. 2008;205:361–372. doi: 10.1084/jem.20071008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song Y, et al. Inflammation, endothelial injury, and persistent pulmonary hypertension in heterozygous BMPR2-mutant mice. Am. J. Physiol. Heart Circ. Physiol. 2008;295:677–690. doi: 10.1152/ajpheart.91519.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thibault HB, et al. Noninvasive assessment of murine pulmonary arterial pressure: validation and application to models of pulmonary hypertension. Circulation. Cardiovascular imaging. 2010;3:157–163. doi: 10.1161/CIRCIMAGING.109.887109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otto C, et al. Pulmonary hypertension and right heart failure in pituitary adenylate cyclase-activating polypeptide type I receptor-deficient mice. Circulation. 2004;110:3245–3251. doi: 10.1161/01.CIR.0000147235.53360.59. [DOI] [PubMed] [Google Scholar]
- Burton VJ, et al. Attenuation of leukocyte recruitment via CXCR1/2 inhibition stops the progression of PAH in mice with genetic ablation of endothelial BMPR-II. Blood. 2011;118:4750–4758. doi: 10.1182/blood-2011-05-347393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujita M, et al. Pulmonary hypertension in TNF-alpha-overexpressing mice is associated with decreased VEGF gene expression. J. Appl. Physiol. 2002;93:2162–2170. doi: 10.1152/japplphysiol.00083.2002. [DOI] [PubMed] [Google Scholar]
- Motley HL, Cournand A, Werko L, Himmelstein A, Dresdale D. The Influence of Short Periods of Induced Acute Anoxia Upon Pulmonary Artery Pressures in Man. Am. J. Physiol. 1947;150:315–320. doi: 10.1152/ajplegacy.1947.150.2.315. [DOI] [PubMed] [Google Scholar]
- Liljestrand G. Regulation of Pulmonary Arterial Blood Pressure. Arch. Intern. Med. 1948;81:162–172. doi: 10.1001/archinte.1948.00220200050006. [DOI] [PubMed] [Google Scholar]
- Euler USV, Liljestrand G. Observations on the pulmonary arterial blood pressure in the cat. Acta Physiol. Scand. 1946;12:301–320. [Google Scholar]
- Van den Broeck W, Derore A, Simoens P. Anatomy and nomenclature of murine lymph nodes: Descriptive study and nomenclatory standardization in BALB/cAnNCrl mice. Journal of immunological. 2006;312:12–19. doi: 10.1016/j.jim.2006.01.022. [DOI] [PubMed] [Google Scholar]
- Rabinovitch M, et al. Angiotensin II prevents hypoxic pulmonary hypertension and vascular changes in rat. Am. J. Physiol. 1988;254:500–508. doi: 10.1152/ajpheart.1988.254.3.H500. [DOI] [PubMed] [Google Scholar]
- Rabinovitch M, Gamble W, Nadas AS, Miettinen OS, Reid L. Rat pulmonary circulation after chronic hypoxia: hemodynamic and structural features. Am. J. Physiol. 1979;236:818–827. doi: 10.1152/ajpheart.1979.236.6.H818. [DOI] [PubMed] [Google Scholar]
- Rabinovitch M, et al. Changes in pulmonary blood flow affect vascular response to chronic hypoxia in rats. Circ. Res. 1983;52:432–441. doi: 10.1161/01.res.52.4.432. [DOI] [PubMed] [Google Scholar]
- Kugathasan L, et al. The angiopietin-1-Tie2 pathway prevents rather than promotes pulmonary arterial hypertension in transgenic mice. J. Exp. Med. 2009;206:2221–2234. doi: 10.1084/jem.20090389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bearer C, Emerson RK, ORiordan MA, Roitman E, Shackleton C. Maternal tobacco smoke exposure and persistent pulmonary hypertension of the newborn. Environ. Health Persp. 1997. pp. 105–202. [DOI] [PMC free article] [PubMed]
- Graham BB, et al. Schistosomiasis-induced experimental pulmonary hypertension: role of interleukin-13 signaling. Am. J. Pathol. 2010;177:1549–1561. doi: 10.2353/ajpath.2010.100063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butrous G, Ghofrani HA, Grimminger F. Pulmonary vascular disease in the developing world. Circulation. 2008;118:1758–1766. doi: 10.1161/CIRCULATIONAHA.107.727289. [DOI] [PubMed] [Google Scholar]
- Crosby A, et al. Praziquantel reverses pulmonary hypertension and vascular remodeling in murine schistosomiasis. Am. J. Respir. Crit. Care Med. 2011;184:467–473. doi: 10.1164/rccm.201101-0146OC. [DOI] [PubMed] [Google Scholar]


