Abstract
Physical activity has been identified as a protective factor with regard to tobacco use, such that physically active adolescents are less likely to initiate smoking, and smokers are less physically active than non-smokers. These findings, along with the well-documented benefits of exercise on mood and well-being in adults, have stimulated interest in exercise-based smoking cessation interventions. However, little research has explored the relationship between physical activity and smoking characteristics within adolescent smokers. Also, gender differences in adolescents’ motives for smoking and exercise may have implications for intervention development, especially in clinical populations. The current study explored the relationship between physical activity and smoking in a sample of adolescent smokers (N = 191) and non-smokers (N = 48) receiving inpatient psychiatric treatment (61% female, mean age 15.3 years). Results indicated that smokers were less likely to be physically active than non-smokers. Additionally, there was a consistent pattern of gender differences in the relationship between smoking and physical activity within smokers. Specifically, physically active male smokers were less nicotine dependent and less prone to withdrawal, and had a trend toward greater motivation to quit, than their non-active counterparts. In contrast, physically active female smokers did not differ in dependence or withdrawal and were less motivated to quit than non-active female smokers. Taken together, these results suggest that within clinical populations of adolescent females, smoking and exercise may be used jointly as weight control strategies. Exercise-based interventions for smoking cessation for adolescent females, especially clinical populations, should address weight and body image concerns.
Keywords: exercise, tobacco, youth, psychiatric, inpatient
Introduction
Physical Activity and Smoking in Adolescents
Cigarette smoking is the leading cause of preventable death and disability in the United States (CDC, 2008; Mokdad, Marks, Stroup, & Gerberding, 2004). Given that initiation of smoking occurs mainly during adolescence (USDHHS, 2012), one focus of research has been the identification of risk and protective factors to inform the development of youth smoking prevention and cessation interventions. Physical activity has been identified in a number of studies as a protective factor within community samples of adolescents. Physically active adolescents are less likely to initiate smoking and progress to regular smoking (Audrain-McGovern, Rodriguez, & Moss, 2003), and adolescents who are current smokers are less likely than non-smokers to participate in sports (Larson, Story, Perry, Neumark-Sztainer, & Hannan, 2007; Lisha & Sussman, 2010) or engage in other regular exercise (Coulson, Eiser, & Eiser, 1997; Larson et al., 2007; Savage & Holcomb, 1997; Verkooijen, Nielsen, & Kremers, 2008; Wilson et al., 2005).
Importantly, some research has revealed gender differences in this relationship. Rodriguez, Dunton, Tscherne, and Sass (2008) found that participation in sports was associated with reduced likelihood of smoking one year later among males, but not females, and this effect was mediated by sport competence beliefs and depressive symptoms. However, other studies have indicated that the discrepancy in physical activity between smokers and non-smokers is more pronounced among females than males (Aaron et al., 1995; Burke et al., 1997; Kaczynski, Manske, Mannell, & Grewal, 2008; Wilson et al., 2005). Of course, there are also gender differences in general participation in physical activity, and this is an area where results are overwhelmingly consistent: adolescent males are more likely to be physically active than females, regardless of smoking status (e.g., Belcher et al., 2010; Cohen, Brownell, & Felix, 1990; Cumming, Standage, Gillison, & Malina, 2008; Jago, Anderson, Baranowski, & Watson, 2005; Mota & Esculcas, 2002).
The Relationship Between Smoking and Physical Activity Within Smokers
Given these findings, one might also expect to observe an inverse relationship between physical activity and smoking within smokers, such that heavier, more nicotine dependent smokers would be less physically active than lighter smokers. Indeed, one recent study found a negative correlation between activity level and smoking frequency among adolescents and young adults (Charilaou, Karekla, Constantinou, & Price, 2009). However, to our knowledge, no studies have examined the relationship between physical activity level and other indicators of nicotine dependence (e.g., score on nicotine dependence measure, withdrawal symptoms) and/or interest in smoking cessation (e.g., motivation and self-efficacy for quitting) within adolescent smokers. Examining relationships between physical activity, nicotine dependence, and cessation interest among adolescent smokers is warranted because of the potential implications for interventions. Engaging in an acute bout of aerobic exercise has shown consistent beneficial effects on mood, withdrawal symptoms, and craving in adult smokers (Taylor, Ussher, & Faulkner, 2007; Ussher, Taylor, & Faulkner, 2012), stimulating interest in exercise-based interventions for smoking cessation (Ussher et al., 2012); however, these effects have yet to be replicated in adolescent smokers (Everson, Daley, & Ussher, 2006).
Gender Differences in Motives for Exercise
Research with community samples has indicated that adolescent females are more likely than males to report that weight concerns motivate both their smoking (Potter, Pederson, Chan, Aubut, & Koval, 2004) and exercise (Penas-Lledo, Sancho, & Waller, 2002) behavior. For example, Peñas-Lledó, Sancho, and Waller (2002) found that whereas adolescent males appear to exercise for positive goals (e.g., fitness), adolescent females exercise to avoid perceived negative consequences (e.g., weight gain).Verkooijen et al. (2009) found that participation in exercise for friendship or competition strengthened the inverse association between exercise and smoking in adolescent males. On the other hand, participation for the reasons of losing weight or enhancing self-esteem weakened the inverse association among adolescent females. Lowry, Galuska, Fulton, Wechsler, and Kann (2002) reported that males who exercised for weight control were less likely to be smokers than those who did not exercise for weight control, but this relationship was not found in females. Furthermore, both physical activity and smoking were associated with trying to lose weight in females, but only physical activity was associated with trying to lose weight in males (Lowry et al., 2002). Finally, the only study to date to examine an exercise-based intervention for adolescent smoking cessation, which involved a community sample, found that adding an exercise component to an existing validated behavioral intervention improved smoking cessation rates in boys but not in girls (Horn et al., 2011). Taken together, these findings suggest that the relationship between smoking and physical activity within smokers may also differ by gender as a result of differences in motives for exercise. If a subgroup of female adolescents is using both smoking and exercise jointly as weight control strategies, we would not expect to find inverse relationships between physical activity and smoking characteristics (i.e., nicotine dependence, interest in cessation) in this group.
Smoking and Physical Activity in Psychiatric Populations
In reviewing exercise-based interventions for smoking cessation among adults, Ussher et al. (2012) noted the significant limitations of existing research and in particular highlighted the dearth of studies in subgroups of smokers that may especially benefit from exercise. For example, given the high comorbidity between smoking and psychiatric disorders (Lasser et al., 2000) and well-documented beneficial effects of exercise on well-being (Penedo & Dahn, 2005) and depressive symptoms (Carek, Laibstain, & Carek, 2011), smokers with psychiatric disorders might especially benefit from exercise-based interventions. However, elevated rates of eating disorders, weight concerns, and body image dissatisfaction, as well as smoking for weight control, are observed in adolescent females receiving psychiatric treatment (e.g., Abrantes, Strong, Ramsey, Lewinsohn, & Brown, 2006). Therefore, these females may be especially motivated by extrinsic reasons (i.e., weight control) to exercise and to use smoking and exercise jointly for weight control. Adding exercise as an adjunct to standard cessation approaches for this population may be ineffective if weight and body image concerns are not addressed.
The Current Study
In summary, most previous research examining the relationship between smoking and physical activity in adolescents has consisted of comparisons between smokers and non-smokers using community-based samples (Coulson et al., 1997; Larson et al., 2007; Lisha & Sussman, 2010; Wilson et al., 2005). Very little research has focused on the relationship between physical activity and smoking within smokers (e.g., severity of dependence, motivation and self-efficacy to quit) or on gender differences in the degree to which weight control is a motive for exercise and smoking. This research would have potential implications for adolescent smoking cessation interventions, especially among clinical populations of adolescent females within which weight control motives for these behaviors may be particularly salient.
In the current study, we conducted a secondary analysis of data collected at baseline for a clinical trial of a brief smoking cessation intervention for psychiatrically hospitalized adolescents (for results of the trial, see Brown et al., 2003), which also included a comparison group of non smoking patients (Ramsey et al., 2003). We examined the relationship between smoking and physical activity by gender, both between smokers and non-smokers and within smokers, and with respect to weight control motives for these behaviors. We hypothesized that smokers would be less physically active than non-smokers, and that we would find an inverse relationship between smoking characteristics (i.e., smoking frequency, severity of nicotine dependence and withdrawal symptoms, motivation and self-efficacy for smoking cessation) and physical activity within smokers. We expected that these differences would be more pronounced among males.
Method
Participants and Procedure
From February 1998 to April 2001, all patients admitted to the adolescent inpatient unit of a psychiatric hospital in the Northeast were approached regarding participation in a teen smoking intervention study with a total of 191 smokers enrolled (for complete methodological details and results of the trial, see Brown et al., 2003). Beginning in March 2000 until June 2001, non-smokers were also enrolled as a comparison group (n = 48), generating a total sample of 239 adolescents for this study (Ramsey et al., 2003). This study was approved by the Institutional Review Board of the hospital. Prior to participation, written assent was obtained from the adolescent, and written informed consent was obtained from a parent or guardian. Each of the measures described below was part of the baseline assessment for this intervention study and was administered by a trained research assistant during adolescents’ inpatient hospital stay.
Physical Activity Measures (Smokers and Non-Smokers)
Physical activity
An item from the Youth Risk Behavior Survey (YRBS, Brener, Collins, Kann, Warren, & Williams, 1995) assessed frequency of physical activity (PA). Participants’ PA status was considered physically active if they reported that they “exercised or participated in sports activities for at least 20 minutes” that made them “sweat and breathe hard” on at least 3 of the 7 days prior to hospitalization. Those who exercised 2 days or less were considered non-active.
Weight Control Motive for Exercise
A single yes/no item from the YRBS (Brener et al., 1995) assessed whether adolescents ever exercised “to lose weight or keep from gaining weight” during the past 30 days. Adolescents answered this item as part of a set of questions regarding frequency of various weight-control behaviors including dieting, purging, and taking diet pills.
Smoking Measures (Smokers Only)
Cigarettes Per Day
The Timeline Followback (TLFB) (Sobell & Sobell, 1996) assessed smoking quantity and frequency and was used to calculate each participant’s average number of cigarettes smoked per day during the 90 days prior to hospitalization.
Nicotine Dependence
Nicotine dependence was measured with a modified version of the Fagerström Tolerance Questionnaire (FTQ) (Prokhorov, Koehly, Pallonen, & Hudmon, 1998), which has been found to have adequate psychometric properties when used with adolescents.
Physical Symptoms
Participants were not allowed to smoke during the length of their inpatient stay, and current withdrawal symptoms were assessed with the Minnesota Withdrawal Scale (Hughes & Hatsukami, 1986), containing 11 symptoms (e.g., anxiety or nervousness, drowsiness) rated from 1 = not present to 6 = very severe. Participants also completed an 8-item measure of respiratory symptoms (e.g., cough frequently throughout the day, pain or tightness in chest), each symptom rated on frequency from 1 = every day to 5 = never.
Motivation to Quit
Participants ranked themselves on the 10-point Contemplation Ladder (e.g., 1 = I have decided to continue smoking; 5 = I often think about quitting, but I have no plans yet; 10 = I have already quit smoking) (Biener & Abrams, 1991). Participants also specified their smoking behavior intention after discharge from the hospital from the following options: 1 = smoke more than I used to, 2 = smoke as much as I used to, 3 = smoke a little less than I used to, 4 = smoke a lot less than I used to, 5 = quit smoking completely (Brown et al., 2003; MacPherson et al., 2007).
Self-Efficacy
Participants rated their confidence in quitting if they were to try to quit within the next month from 1 = not at all confident to 11 = very confident (Apodaca, Abrantes, Strong, Ramsey, & Brown, 2007).
Weight Control Motive for Smoking
Three 5-point Likert scale items from the Adolescent Decisional Balance Scale (Migneault, Pallonen, & Velicer, 1997) assessed strength of beliefs that smoking helps control weight and appetite (“If I stop smoking, I will gain weight”; “I often smoke to reduce my appetite when I get hungry”; “I started to smoke to control my weight”).
Statistical Analyses
All data analyses were conducted using SPSS® Statistics version 20.0.0. Distributions of dependent variables were screened for violations of parametric test assumptions and determined acceptable. The amount of missing data was small and most likely due to researcher error (e.g., item/scale not administered) or participant error (e.g., accidentally skipped item/scale). Missing data was dealt with using pairwise deletion.
Logistic regression was used to evaluate the effects of gender (male vs. female), smoking status (smoker vs. non-smoker) and their interaction on PA status (physically active vs. non-active) and on weight control motive for exercise (yes vs. no). All models were adjusted for age and diagnoses as these variables differed significantly by smoking status (see Results section below). Analysis of variance (ANOVA) was used to evaluate the effects of gender, PA status, and their interaction on continuous measures of smoking characteristics within smokers.
Results
Participant Demographics and Diagnoses
The total sample had a mean age of 15.27 years and was 61% female and 94% Caucasian. All smoking participants reported smoking at least one cigarette per week during the four weeks prior to hospitalization. A comparison of demographics, non-nicotine substance use, and diagnostic characteristics between smokers and non-smokers in this sample has been conducted (Ramsey et al., 2003). In brief, the two groups did not differ in gender or ethnicity, but smokers (mean = 15.38 years) were slightly older than non-smokers (mean = 14.85 years), p < .05. Smokers were more likely to have engaged in binge drinking and marijuana use, and were more likely to meet criteria for a non-nicotine substance use disorder (71% vs. 10%) and a disruptive behavior disorder (79% vs. 56%) as assessed with the Columbia Diagnostic Interview for Children (C-DISC) (Costello, Edelbrock, Duncan, Kalas, & Klaric, 1984), all p’s < .01. Smokers and non-smokers did not differ on rates of mood or anxiety disorders.
Smokers vs. Non-Smokers
Physical Activity (PA) Status
To determine whether there were gender or smoking status differences with regard to PA status, we conducted a series of logistic regression models. All models included PA status as the dependent variable and were adjusted for age and diagnoses. The first model included gender and revealed that gender was not a significant predictor of PA status B = −.36, Odds Ratio (OR) = 1.74, p = .19. A second model included smoking status and revealed a significant effect of smoking status, B = −.78, Odds Ratio (OR) = 4.03, p < .05 (.045), such that smokers were less likely to be physically active than non-smokers. A third model included gender, smoking status, and a gender x smoking status interaction. Results indicated no significant interaction between gender and smoking status on PA status, B = −.29, Odds Ratio (OR) = .18, p = .67.
Weight Control Motive for Exercise
We conducted a similar series of logistic regression models to determine whether there were gender or smoking status differences with regard to weight control motive for exercise. The first model included gender and revealed that gender was a significant predictor of weight control motive for exercise, B = 1.14, Odds Ratio (OR) = 14.78, p < .001, such that females were more likely to report exercising for weight control than males. The second model included smoking status and revealed that smoking status was not a significant predictor of weight control motive for exercise, B = −.29, Odds Ratio (OR) = .54, p = .46. A third model included gender, smoking status and a gender x smoking status interaction. Results indicated no significant interaction between gender and smoking status, B = −.28, Odds Ratio (OR) = .15, p = .70.
Physical Activity and Smoking Characteristics Within Smokers
Cigarettes Per Day
The ANOVA revealed no main effect of gender (p = .46) or PA status (p = .38) on number of cigarettes smoked per day. However, there was a trend for an interaction between gender and PA status, F(1, 187) = 3.87, p = .05. Simple effects analyses revealed a trend for physically active male smokers (M = 13.22, SD = 9.14) to smoke fewer cigarettes per day than non-active male smokers (M = 17.22, SD = 11.30) (p = .07); however, physically active (M = 14.94, SD = 9.74) and non-active (M = 13.41, SD = 7.94) female smokers did not differ in cigarettes per day (p = .37).
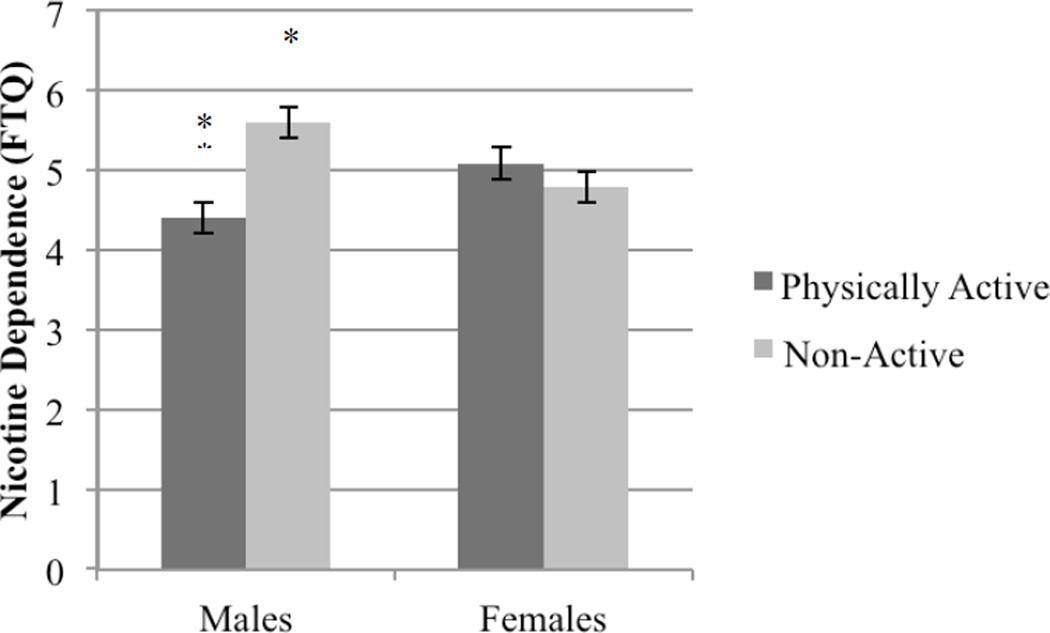
Nicotine Dependence
The ANOVA revealed no main effect of gender (p = .81) or PA status (p = .11) on nicotine dependence (FTQ). However, there was a significant interaction between gender and PA status, F(1, 182) = 7.47, p = .007 (see Figure 1). Simple effects analyses revealed that physically active male smokers were significantly less nicotine dependent than non-active male smokers (p = .006); however, physically active and non-active female smokers did not differ significantly in nicotine dependence (p = .37).
Figure 1.
Significant interaction of gender and physical activity status on nicotine dependence (FTQ score), p = .007. Simple effects analyses revealed that physically active males were less nicotine dependent than non-active males, p = .006.
Withdrawal and Respiratory Symptoms
For withdrawal symptoms, the ANOVA showed a main effect of gender, F(1, 180) = 7.39, p = .007, and a trend for a main effect of PA status, F(1, 180) = 3.85, p = .05, such that female and non-active smokers reported worse current withdrawal symptoms. There was no interaction between gender and PA status F(1, 180) = 2.75, p = .10. However, simple effects analyses revealed that physically active male smokers experienced less withdrawal than non-active male smokers (p = .02), but withdrawal symptoms did not differ by PA status for female smokers (p = .81). For respiratory symptoms, there were main effects of both gender, F(1, 185) = 9.50, p = .002, and PA status, F(1, 185) = 6.41, p = .01, but no significant interaction (p = .93). Female and non-active smokers experienced worse respiratory symptoms.
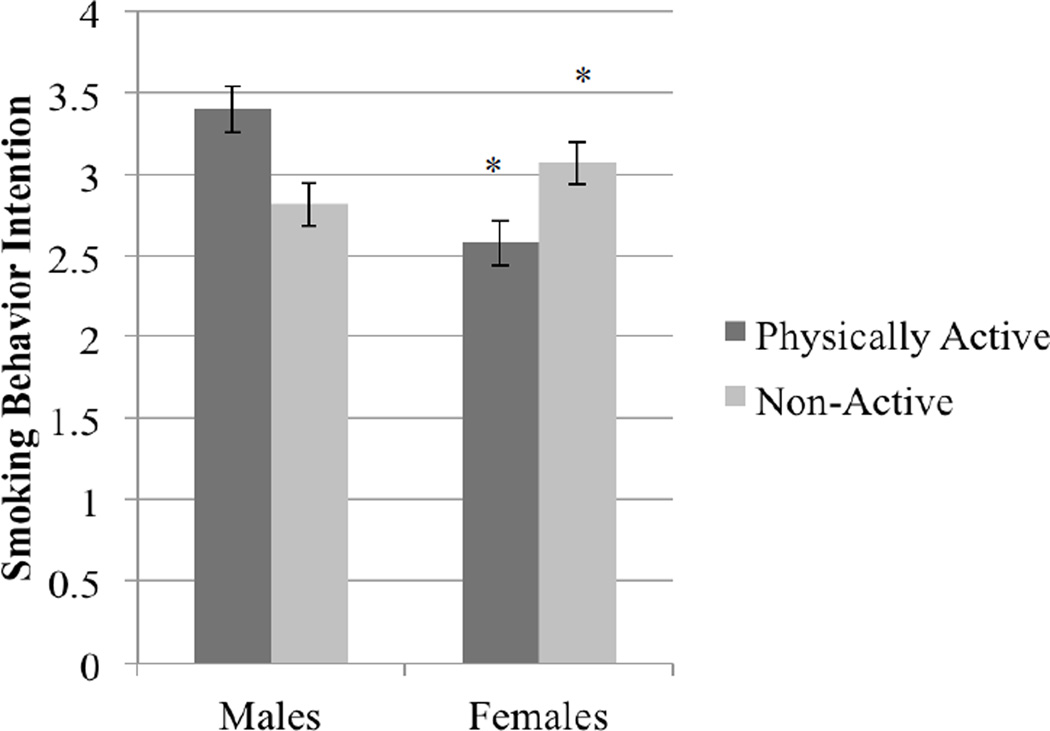
Motivation to Quit
ANOVA results indicated no main effects of gender or PA status on the Contemplation Ladder (p = .47 and p = .79 respectively). However, there was a significant crossover interaction between gender and PA status, F(1, 186) = 6.58, p = .01 (see Figure 2). Simple effects analyses revealed the following trends: physically active females were significantly less motivated than non-active females (p = .06), whereas males showed the opposite pattern such that physically active males were more motivated than non-active males (p = .08). Similarly, ANOVA results indicated no main effects of gender or PA status (p = .14 and p = .81 respectively) on smoking behavior intention but a significant crossover interaction between gender and PA status, F(1, 183) = 8.08, p = .005 (see Figure 2). Simple effects analyses revealed the following: physically active females had significantly weaker intention to reduce or quit smoking after discharge relative to non-active female smokers (p = .03), whereas males showed a trend for the opposite pattern (physically active males had stronger intention to reduce or quit after discharge than non-active males) (p = .05).
Figure 2.
Significant interaction of gender and physical activity status on smoking behavior intention after hospital discharge (ranged from 1-5; 1 = smoke more than I used to, 5 = quit smoking completely), p = .005. Simple effects analyses revealed that physically active females had significantly weaker intention to reduce or quit smoking than non-active females, p = .03; for males the relationship was in the opposite direction, p = .05.
Self-Efficacy
The ANOVA revealed no main effect of PA status p = .96) on the confidence for quitting within the next month, but a significant main effect of gender, F(1, 186) = 6.19, p = .01, such that females were less confident than males. There was also a significant crossover interaction between gender and PA status, F(1, 186) = 4.91, p = .03 (see Figure 2). Simple effects analyses revealed a trend for physically active females to have lower confidence than non-active females (p = .07), whereas there was no difference in confidence between physically active and non-active males (p = .17).
Weight Control Motive for Smoking
The ANOVA revealed no main effect of PA status on weight-control smoking expectancies (p = .32). There was a trend for a main effect of gender, F(1, 187) = 3.40, p = .07, such that females had greater weight-control smoking expectancies than males. There was no interaction between gender and PA status, F(1, 187) = 2.70, p = .10; however, simple effects analyses revealed that physically active females had stronger weight control expectancies than physically active males (p = .02) whereas among non-active smokers there was no gender difference in strength of weight control expectancies (p = .88).
Discussion
The current study explored the relationship between smoking and physical activity in male and female adolescents receiving inpatient psychiatric treatment. Comparison of smokers versus non-smokers was largely consistent with past research on community samples. That is, within this clinical sample of adolescents, smokers were less likely to be physically active than non-smokers. Smokers and non-smokers in this sample differed significantly in age and diagnoses; however, these differences did not appear to account for the discrepancy in physical activity.
Similarly, our findings with respect to the relationship between physical activity and smoking characteristics within male smokers extend extant research in that an inverse relationship was demonstrated. Specifically, compared to non-active male smokers, physically active male smokers were less severely nicotine dependent and less prone to withdrawal symptoms. There were also trends for physically active male smokers to smoke fewer cigarettes per day and to report greater motivation for quitting. However, the observed relationship between smoking and physical activity in females was largely in the opposite direction. That is, relative to non-active female smokers, physically active female smokers reported lower motivation to quit and a trend for lower self-efficacy to quit relative to non-active female smokers. Physically active female smokers did not differ from non-active female smokers in smoking frequency, severity of nicotine dependence, or withdrawal. Irrespective of PA status, female smokers reported worse withdrawal and respiratory symptoms and lower self-efficacy than male smokers.
We also observed gender differences in the degree to which weight control was a motive for physical activity and smoking. Females were more likely than males to report that they exercised to control their weight, regardless of smoking status. Physically active female smokers also held stronger expectations that smoking would help them control their weight than physically active male smokers, whereas expectations that smoking helps control weight did not differ among non-active male and female smokers. Taken together, our findings indicate that within this clinical population, decreased motivation for smoking cessation among physically active female smokers as compared to non-active female smokers may reflect use of smoking and exercise jointly as weight control strategies.
These findings may have implications for interventions. Whereas there is longstanding interest in exercise-based smoking cessation interventions for adults that continues to increase (Ussher et al., 2012), research on exercise-based smoking cessation interventions for adolescents is in its infancy. To date, there is only one randomized trial (Horn et al., 2011). This three group study compared an exercise-based intervention (FIT) in combination with a well-established intervention for adolescent smoking cessation (Not on Tobacco, N-O-T) to N-O-T alone and to a brief intervention control condition within a community sample of adolescents. Results indicated a significant gender difference, such that males who received N-O-T + FIT were four times more likely to quit than males who only received N-O-T, whereas the addition of FIT to N-O-T had no benefit for females. The authors suggested that perhaps FIT was more “culturally suitable” for males. These findings, along with the findings of the current study, suggest that physical activity interventions for adolescent smokers may need to be tailored by gender. Interventions for females, especially within clinical populations, should take into account gender differences in motives for physical activity and smoking and consider incorporating content to address issues of weight concern and body image that may motivate continued smoking. Certain types of physical activity interventions may be more likely to improve body image among adolescent females, for example, aerobic dance (Burgess, Grogan, & Burwitz, 2006). Discussion and skill-building with respect to resisting the influence of the media, thin-ideal internalization, and body comparison, and increasing emphasis on non-appearance related positive traits can also reduce body dissatisfaction (Richardson & Paxton, 2010; Stice, Shaw, & Marti, 2007)
Limitations and Conclusion
The current study has a number of limitations that must be acknowledged. First, with respect to our methodology, all analyses were cross-sectional, which did not allow determination of causality with respect to the relationship between smoking and physical activity. Also, the number of non-smokers (N = 48) was small relative to the number of smokers (N = 191), which limited power to detect differences between smokers and non-smokers. Second, physical activity status was determined based on adolescents’ self-report of the week prior to hospitalization. Self-report measures of physical activity are less reliable and are likely to be overestimates relative to more objective measures (Adamo, Prince, Tricco, Connor-Gorber, & Tremblay, 2009); furthermore, the week prior to psychiatric hospitalization may not have been a “typical” week. Third, the measure of weight control motive for exercise was a single item, was answered by all participants regardless of PA status, and was embedded in a series of questions about frequency of pathological weight control behaviors (e.g., purging), which may have affected responses. Finally, data were collected from primarily Caucasian adolescents who were receiving inpatient psychiatric treatment within a single private psychiatric hospital in the northeastern United States. Psychiatric hospitalization is usually preceded by a crisis (e.g., suicide attempt); adolescents who are hospitalized are likely to be experiencing severe psychopathology. Therefore, results may not generalize to other geographic locations, more diverse samples, other psychiatric treatment settings (e.g., outpatient settings), or community samples.
Despite these limitations, this study is the first to examine the relationship between cigarette smoking and physical activity in a psychiatric sample of adolescents and, thus, makes a contribution to growing literature in this area. The physical and mental health benefits of physical activity are well-documented and significant. Adolescence is a critical developmental period where interventions to address health risk behaviors can have important benefits to adult functioning and outcomes. Physical activity interventions may play an important role in promoting healthy behaviors in youth. However, the results of this study highlight the importance of considering gender differences as well as exercise and smoking motives when developing effective approaches for smoking cessation in adolescents.
Highlights.
Physical activity and smoking are inversely related in community samples of youth.
We examined this relationship in psychiatrically hospitalized adolescents.
Physical activity and smoking were negatively related among males.
Physical activity and smoking were positively related among females.
Interventions for female smokers should address weight and body image concerns.
Acknowledgements
This research was supported by Grant CA 77082 from the National Cancer Institute to Richard A. Brown, Ph.D. and a grant from the Brown University Department of Psychiatry and Human Behavior to Susan E. Ramsey, Ph.D.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aaron DJ, Dearwater SR, Anderson R, Olsen T, Kriska AM, Laporte RE. Physical activity and the initiation of high-risk health behaviors in adolescents. Medicine and Science in Sports and Exercise. 1995;27:1639–1645. [PubMed] [Google Scholar]
- Abrantes AM, Strong DR, Ramsey SE, Lewinsohn PM, Brown RA. Characteristics of dieting and non-dieting adolescents in a psychiatric inpatient setting. Journal of Child and Family Studies. 2006;15:418–432. [Google Scholar]
- Adamo KB, Prince SA, Tricco AC, Connor-Gorber S, Tremblay M. A comparison of indirect versus direct measures for assessing physical activity in the pediatric population: a systematic review. International Journal of Pediatric Obesity. 2009;4:2–27. doi: 10.1080/17477160802315010. [DOI] [PubMed] [Google Scholar]
- Apodaca TR, Abrantes AM, Strong DR, Ramsey SE, Brown RA. Readiness to change smoking behavior in adolescents with psychiatric disorders. Addictive Behaviors. 2007;32:1119–1130. doi: 10.1016/j.addbeh.2006.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Audrain-McGovern J, Rodriguez D, Moss HB. Smoking progression and physical activity. Cancer Epidemiology, Biomarkers and Prevention. 2003;12:1121–1129. [PubMed] [Google Scholar]
- Belcher BR, Berrigan D, Dodd KW, Emken BA, Chou CP, Spruijt-Metz D. Physical activity in US youth: effect of race/ethnicity, age, gender, and weight status. Medicine and Science in Sports and Exercise. 2010;42:2211–2221. doi: 10.1249/MSS.0b013e3181e1fba9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biener L, Abrams DB. The Contemplation Ladder: validation of a measure of readiness to consider smoking cessation. Health Psychology. 1991;10:360–365. doi: 10.1037//0278-6133.10.5.360. [DOI] [PubMed] [Google Scholar]
- Brener ND, Collins JL, Kann L, Warren CW, Williams BI. Reliability of the Youth Risk Behavior Survey Questionnaire. American Journal of Epidemiology. 1995;141:575–580. doi: 10.1093/oxfordjournals.aje.a117473. [DOI] [PubMed] [Google Scholar]
- Brown RA, Ramsey SE, Strong DR, Myers MG, Kahler CW, Lejuez CW, et al. Effects of motivational interviewing on smoking cessation in adolescents with psychiatric disorders. Tobacco Control. 2003;(12 Suppl 4):IV3–IV10. doi: 10.1136/tc.12.suppl_4.iv3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgess G, Grogan S, Burwitz L. Effects of a 6-week aerobic dance intervention on body image and physical self-perceptions in adolescent girls. Body Image. 2006;3:57–66. doi: 10.1016/j.bodyim.2005.10.005. [DOI] [PubMed] [Google Scholar]
- Burke V, Milligan RA, Beilin LJ, Dunbar D, Spencer M, Balde E, et al. Clustering of health-related behaviors among 18-year-old Australians. Preventive Medicine. 1997;26:724–733. doi: 10.1006/pmed.1997.0198. [DOI] [PubMed] [Google Scholar]
- Carek PJ, Laibstain SE, Carek SM. Exercise for the treatment of depression and anxiety. International Journal of Psychiatry in Medicine. 2011;41:15–28. doi: 10.2190/PM.41.1.c. [DOI] [PubMed] [Google Scholar]
- CDC. Smoking-Attributable Mortality, Years of Potential Life Lost, and Productivity Losses - United States, 2000–2004. Morbidity and Mortality Weekly Report. 2008;57:1226–1228. [PubMed] [Google Scholar]
- Charilaou M, Karekla M, Constantinou M, Price S. Relationship between physical activity and type of smoking behavior among adolescents and young adults in Cyprus. Nicotine & Tobacco Research. 2009;11:969–976. doi: 10.1093/ntr/ntp096. [DOI] [PubMed] [Google Scholar]
- Cohen RY, Brownell KD, Felix MR. Age and sex differences in health habits and beliefs of schoolchildren. Health Psychology. 1990;9:208–224. doi: 10.1037//0278-6133.9.2.208. [DOI] [PubMed] [Google Scholar]
- Costello AJ, Edelbrock C, Duncan MK, Kalas R, Klaric S. Development and testing of the NIMH Diagnostic Interview Schedule for Children on a clinical population: Final report. Rockville, MD: Center for Epidemiological Studies, National Institute for Mental Health; 1984. [Google Scholar]
- Coulson NS, Eiser C, Eiser JR. Diet, smoking and exercise: interrelationships between adolescent health behaviours. Child: Care, Health and Development. 1997;23:207–216. doi: 10.1111/j.1365-2214.1997.tb00964.x. [DOI] [PubMed] [Google Scholar]
- Cumming SP, Standage M, Gillison F, Malina RM. Sex differences in exercise behavior during adolescence: is biological maturation a confounding factor? Journal of Adolescent Health. 2008;42:480–485. doi: 10.1016/j.jadohealth.2007.10.005. [DOI] [PubMed] [Google Scholar]
- Everson ES, Daley AJ, Ussher M. Does exercise have an acute effect on desire to smoke, mood and withdrawal symptoms in abstaining adolescent smokers? Addictive Behaviors. 2006;31:1547–1558. doi: 10.1016/j.addbeh.2005.11.007. [DOI] [PubMed] [Google Scholar]
- Horn K, Dino G, Branstetter SA, Zhang J, Noerachmanto N, Jarrett T, et al. Effects of physical activity on teen smoking cessation. Pediatrics. 2011;128:e801–e811. doi: 10.1542/peds.2010-2599. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Hatsukami D. Signs and symptoms of tobacco withdrawal. Archives of General Psychiatry. 1986;43:289. doi: 10.1001/archpsyc.1986.01800030107013. [DOI] [PubMed] [Google Scholar]
- Jago R, Anderson CB, Baranowski T, Watson K. Adolescent patterns of physical activity differences by gender, day, and time of day. American Journal of Preventive Medicine. 2005;28:447–452. doi: 10.1016/j.amepre.2005.02.007. [DOI] [PubMed] [Google Scholar]
- Kaczynski AT, Manske SR, Mannell RC, Grewal K. Smoking and physical activity: a systematic review. American Journal of Health Behavior. 2008;32:93–110. doi: 10.5555/ajhb.2008.32.1.93. [DOI] [PubMed] [Google Scholar]
- Larson NI, Story M, Perry CL, Neumark-Sztainer D, Hannan PJ. Are diet and physical activity patterns related to cigarette smoking in adolescents? Findings from Project EAT. Preventing Chronic Disease. 2007;4:A51. [PMC free article] [PubMed] [Google Scholar]
- Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: A population-based prevalence study. Journal of the American Medical Association. 2000;284:2606–2610. doi: 10.1001/jama.284.20.2606. [DOI] [PubMed] [Google Scholar]
- Lisha NE, Sussman S. Relationship of high school and college sports participation with alcohol, tobacco, and illicit drug use: a review. Addictive Behaviors. 2010;35:399–407. doi: 10.1016/j.addbeh.2009.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowry R, Galuska DA, Fulton JE, Wechsler H, Kann L. Weight management goals and practices among U.S. high school students: associations with physical activity, diet, and smoking. Journal of Adolescent Health. 2002;31:133–144. doi: 10.1016/s1054-139x(01)00408-6. [DOI] [PubMed] [Google Scholar]
- MacPherson L, Strong DR, Kahler CW, Abrantes AM, Ramsey SE, Brown RA. Association of post-treatment smoking change with future smoking and cessation efforts among adolescents with psychiatric comorbidity. Nicotine & Tobacco Research. 2007;9:1297–1307. doi: 10.1080/14622200701651734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Migneault JP, Pallonen UE, Velicer WF. Decisional balance and stage of change for adolescent drinking. Addictive Behaviors. 1997;22:339–351. doi: 10.1016/s0306-4603(96)00252-3. [DOI] [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. Journal of the American Medical Association. 2004;291:1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Mota J, Esculcas C. Leisure-time physical activity behavior: structured and unstructured choices according to sex, age, and level of physical activity. International Journal of Behavioral Medicine. 2002;9:111–121. doi: 10.1207/s15327558ijbm0902_03. [DOI] [PubMed] [Google Scholar]
- Penas-Lledo E, Sancho L, Waller G. Eating attitudes and the use of alcohol, tobacco, and exercise among male and female adolescents. Eating Behavior. 2002;3:101–111. doi: 10.1016/s1471-0153(01)00047-2. [DOI] [PubMed] [Google Scholar]
- Penedo FJ, Dahn JR. Exercise and well-being: a review of mental and physical health benefits associated with physical activity. Current Opinion in Psychiatry. 2005;18:189–193. doi: 10.1097/00001504-200503000-00013. [DOI] [PubMed] [Google Scholar]
- Potter BK, Pederson LL, Chan SS, Aubut JA, Koval JJ. Does a relationship exist between body weight, concerns about weight, and smoking among adolescents? An integration of the literature with an emphasis on gender. Nicotine & Tobacco Research. 2004;6:397–425. doi: 10.1080/14622200410001696529. [DOI] [PubMed] [Google Scholar]
- Prokhorov AV, Koehly LM, Pallonen UE, Hudmon KS. Adolescent nicotine dependence measured by the modified Fagerstrom tolerance questionnaire at two time points. Journal of Child and Adolescent Substance Abuse. 1998;7:35–47. [Google Scholar]
- Ramsey SE, Strong DR, Stuart GL, Weinstock MC, Williams LA, Tarnoff G, et al. Substance use and diagnostic characteristics that differentiate smoking and nonsmoking adolescents in a psychiatric setting. Journal of Nervous and Mental Disease. 2003;191:759–762. doi: 10.1097/01.nmd.0000095130.33301.f9. [DOI] [PubMed] [Google Scholar]
- Richardson SM, Paxton SJ. An evaluation of a body image intervention based on risk factors for body dissatisfaction: a controlled study with adolescent girls. International Journal of Eating Disorders. 2010;43:112–122. doi: 10.1002/eat.20682. [DOI] [PubMed] [Google Scholar]
- Rodriguez D, Dunton GF, Tscherne J, Sass J. Physical activity and adolescent smoking: A moderated mediation model. Mental Health and Physical Activity. 2008;1:17–25. [Google Scholar]
- Savage MP, Holcomb DR. Physical activity levels and self-reported risk-taking behavior among rural Australian and american 7th–9th grade adolescents. International Quaterly of Community Health Education. 1997;17:345–360. doi: 10.2190/KGPG-6C8E-TN5Y-8RCK. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline followback: A calendar method for assessing alcohol and drug use. Toronto, Canada: Addiction Research Foundation; 1996. [Google Scholar]
- Stice E, Shaw H, Marti CN. A meta-analytic review of eating disorder prevention programs: encouraging findings. Annual Review of Clinical Psychology. 2007;3:207–231. doi: 10.1146/annurev.clinpsy.3.022806.091447. [DOI] [PubMed] [Google Scholar]
- Taylor AH, Ussher MH, Faulkner G. The acute effects of exercise on cigarette cravings, withdrawal symptoms, affect and smoking behaviour: a systematic review. Addiction. 2007;102:534–543. doi: 10.1111/j.1360-0443.2006.01739.x. [DOI] [PubMed] [Google Scholar]
- USDHHS. Preventing tobacco use among youth and young adults: a report of the Surgeon General. 2012. [PubMed] [Google Scholar]
- Ussher MH, Taylor A, Faulkner G. Exercise interventions for smoking cessation. Cochrane Database of Systematic Reviews. 2012;1:CD002295. doi: 10.1002/14651858.CD002295.pub4. [DOI] [PubMed] [Google Scholar]
- Verkooijen KT, Nielsen GA, Kremers SP. The Association between leisure time physical activity and smoking in adolescence: an examination of potential mediating and moderating factors. International Journal of Behavioral Medicine. 2008;15:157–163. doi: 10.1080/10705500801929833. [DOI] [PubMed] [Google Scholar]
- Verkooijen KT, Nielsen GA, Kremers SPJ. Leisure time physical activity motives and smoking in adolescence. Psychology of Sport and Exercise. 2009;10 [Google Scholar]
- Wilson DB, Smith BN, Speizer IS, Bean MK, Mitchell KS, Uguy LS, et al. Differences in food intake and exercise by smoking status in adolescents. Preventive Medicine. 2005;40:872–879. doi: 10.1016/j.ypmed.2004.10.005. [DOI] [PubMed] [Google Scholar]