Abstract
Objective
Widespread immunization confers both individual- and community-level protection against vaccine-preventable diseases. To better understand vaccine hesitancy, we assessed correlates of forgone vaccination for children and adolescents.
Method
We analyzed weighted data from the 2010 Child Health Assessment and Monitoring Program survey of North Carolina parents (n=1,847) of children ages 1–17.
Results
Overall, 12% of parents reported having refused or delayed a vaccine for their child. Forgone vaccination was more common for young children than for teenagers (16% versus 8%) and for children born before rather than on/after their due dates (16% versus 10%). Parents with high (versus low) scores on an index of healthy feeding practices were also more likely to report forgone vaccination (17% versus 5%). The most common reason for forgoing vaccines was concern about safety (34%). Other reasons included believing the child did not need (18%) or was too young (13%) for the vaccine, or that the child was sick (10%).
Conclusion
Forgoing vaccines is more common among parents who are socially-advantaged and highly attentive to their children’s health in other areas such as nutrition. Providers should reassure parents of premature or sick children that such circumstances are not typically contraindications to vaccination.
Keywords: child health, adolescent health, vaccination/statistics & numerical data, vaccine hesitancy, North Carolina
Although few parents in the United States categorically reject vaccination, many choose to refuse or delay certain vaccines for their children, leading to under-immunization (Smith et al., 2011). With regard to young children, recent research suggests that 13–40% of parents forgo (i.e., refuse or delay) at least one vaccine (Dempsey et al., 2011; Gust et al., 2008; Smith et al., 2010; Smith, et al., 2011). Even more parents may be “at risk” for forgoing vaccines given that concerns about early childhood immunization are common, even among those parents who comply with recommended guidelines (Dempsey et al., 2011; Kennedy et al., 2011). Although surveillance of forgone vaccination is limited, some measures indicate the problem is growing (Omer et al., 2006; Kempe et al., 2011). For example, an increasing number of parents are claiming nonmedical exemptions to school-based immunization requirements (Omer et al., 2006).
Less is known about forgone vaccination with regard to older children and vaccines in the adolescent platform: tetanus, diphtheria, and pertussis (Tdap); meningococcal vaccine; and human papillomavirus (HPV) vaccine. However, given that as many as one-third of parents of unvaccinated adolescents report having received a provider recommendation for these vaccines, parental refusal or delay is likely one reason for suboptimal uptake (Dorell et al., 2011). Under-immunization is most pronounced for HPV vaccine with only 35% of girls and 1% of boys completing the three dose series (CDC, 2012). Coverage for Tdap (78%) and meningococcal vaccine (71%) is higher, but still shows room for improvement (CDC, 2012).
In response to these issues, a small, but growing literature addresses the need for healthcare providers to identify “vaccine-hesitant” parents so as to more effectively communicate with them (Fredrickson et al., 2004; Smith et al., 2006). Because parents with vaccine-related doubts are more likely to delay or refuse immunization (Gaudino et al., 2012; Gust et al., 2008; Smith et al., 2011), one approach is to classify parents based on their vaccine-related attitudes using survey instruments and typologies (Keane et al., 2005; Opel et al., 2011). However, given the constraints of the clinical encounter, using these tools for universal screening may not be feasible. For this reason, providers can also benefit from more readily available indicators of vaccine refusal or delay, including factors related to families’ demographic characteristics, parenting style, or relationship with the healthcare provider. Knowing which vaccines and which concerns are most worrisome can also help providers focus their discussions.
To investigate these issues, we used data from a statewide survey of parents to: a) identify correlates of forgone vaccination; and b) assess which vaccines parents refused or delayed and their reasons for doing so.
METHODS
Sample
We used data from two linked telephone surveys conducted in 2010. The North Carolina Behavioral Risk Factor Surveillance System (BRFSS) survey is a population-based survey of adults (NC SCHS, 2011a). Households with BRFSS respondents who report living with a child under age 18 are eligible to participate in the Child Health Assessment and Monitoring Program (CHAMP) survey (NC SCHS, 2001b). CHAMP is administered in a follow-up phone call to the adult caregiver the BRFSS respondent identifies as being most knowledgeable about the health of a randomly-selected child in the household.
In 2010, the response rate for the North Carolina BRFSS was 61% (CDC, 2011). Of the 3,174 BRFSS respondents invited to participate in CHAMP, 2009 (63%) completed the survey. We excluded parents of children less than one year of age (n=79) from our analytic sample because several survey items of interest were not relevant to infants. We also excluded respondents if they were unsure whether they had ever delayed or refused a vaccine for their child (n=7), did not provide the child’s sex (n=2), or did not provide information on nutrition-related variables (n=74). Our sample consisted of the remaining 1,847 respondents. Because a majority of respondents in our sample (88%) reported being the biological parent of the child in question, we refer to respondents as “parents.” The University of North Carolina Institutional Review Board determined that this study did not require review.
Measures
One item on the CHAMP survey assessed this study’s primary outcome: “Have you ever postponed or refused to get a vaccine shot for [child’s name]?” For parents who responded “yes” to this item, interviewers asked respondents to give their reason(s) and to name which vaccine(s). Our measure of forgone vaccination combined vaccine refusal and delay because both behaviors are associated with under-immunization (Smith et al., 2011).
The survey also assessed factors related to forgone vaccination identified in the research literature, including parents’ relationship with their child’s healthcare provider, perceptions of their child’s health, and parenting behaviors. In terms of the parent-provider relationship, CHAMP assessed: 1) whether the child had a “personal” healthcare provider who knew him/her well; 2) how often in the last year providers spent enough time with the child; and 3) how often in the last year providers helped the parent feel like a partner in the child’s care. In terms of the child’s health status, CHAMP assessed: 1) the child’s general health; 2) whether the child was born before his/her due date; and 3) whether the child was limited in his/her ability compared to children of the same age.
With regard to parenting behaviors, CHAMP assessed whether the child had ever been breastfed. Using a 4-point response scale, the survey also assessed the child’s daily consumption of fruits, vegetables, and sweetened beverages as well as the weekly frequency of fast food meals and home-cooked family meals. To reduce collinearity in the final model, we combined the latter five items into an index of healthy child feeding practices. After reverse-coding variables related to fast food and sweetened beverage consumption, we calculated the sum of the items and collapsed the resulting totals into three categories: low (5–10), medium (11–15), and high (16–20).
We used demographic variables from both CHAMP and BRFSS. CHAMP assessed child’s sex, age, and race, as well as whether the child had health insurance, parent’s sex, and the highest level of education attained by anyone in the household. BRFSS assessed household income and location. We defined households within a metropolitan statistical area (MSA) as “urban or suburban” and those outside an MSA as “rural” (U.S. Census Bureau, 2011).
Statistical Analyses
We used logistic regression to identify bivariate correlates of forgone vaccination. We entered statistically significant correlates into a multivariate model. We chose not to stratify our analyses by child’s age because our study examined vaccine refusal or delay that occurred at any time in the child’s life. To further explore the association of child feeding practices with forgone vaccination, we used linear regression to examine the bivariate association separately for each component of the child feeding practices index. We analyzed data using Stata Version 12.0 (Statacorp, College Station, TX), incorporating sample weights to account for unequal probability of selection. We report unweighted frequencies and weighted proportions and odds ratios. All statistical tests were 2-tailed with a critical alpha of 0.05.
RESULTS
Sample characteristics
Participants were equally likely to be the parent of a son (50%) or a daughter (50%) (Table 1). The mean age of children was 9.7 years, and most were non-Hispanic white (62%) or black (22%). Most parents were female (85%). Half of respondents indicated an annual household income of $50,000 or more (50%), and about three quarters reported that someone in their household had attended college (78%).
Table 1.
Sample characteristics, 2010 Child Health Assessment and Monitoring Program (CHAMP) survey, North Carolina, USA (n=1847).
| n (%) | |
|---|---|
| Child’s sex | |
| Male | 936 (50) |
| Female | 911 (50) |
| Child’s age (years) | |
| 1–6 | 582 (36) |
| 7–12 | 599 (35) |
| 13–17 | 666 (29) |
| Child’s race | |
| Non-Hispanic white | 1271 (62) |
| Non-Hispanic black | 310 (22) |
| Other | 266 (16) |
| Child covered by health insurance | |
| No/don’t know | 108 (5) |
| Yes | 1739 (95) |
| Parent’s sex | |
| Male | 299 (15) |
| Female | 1548 (85) |
| Annual household income | |
| < $50,000 | 751 (42) |
| ≥ $50,000 | 938 (50) |
| Not reported | 158 (8) |
| Highest education in household | |
| High school or less | 392 (22) |
| Some college or more | 1455 (78) |
| Urbanicity | |
| Rural | 445 (26) |
| Urban/suburban | 1402 (74) |
Note: Table shows raw frequencies and weighted percentages. Percentages may not total 100% due to rounding.
Correlates of forgone vaccination
Overall, 12% of parents reported having ever refused or delayed a vaccine for their child. In multivariate analysis, forgone vaccination was more common for young children (ages 1–6) than for older children (ages 13–17) (16% versus 8%). Female respondents reported forgone vaccination more often than did male respondents (13% versus 7%). The practice was also more common among respondents living in households with high versus low educational attainment (14% versus 5%). Although bivariate analyses indicated that child’s race and annual household income correlated with refusal or delay, these variables did not retain statistical significance in the multivariate model (Table 2).
Table 2.
Correlates of forgone vaccination, 2010 Child Health Assessment and Monitoring Program (CHAMP) survey, North Carolina, USA (n=1847).
| Parents Reporting Refusal/Delay of Vaccine for Child | Bivariate | Multivariate | |
|---|---|---|---|
| n/N (%) | OR (95% CI) | OR (95% CI) | |
| Demographics | |||
| Child’s sex | |||
| Male | 101/936 (11) | 1 | |
| Female | 123/911 (14) | 1.36 (0.96–1.93) | |
| Child’s age (years) | |||
| 1–6 | 105/582 (16) | 1 | 1 |
| 7–12 | 61/599 (12) | 0.69 (0.46–1.04) | 0.74 (0.48–1.15) |
| 13–17 | 58/666 (8) | 0.48 (0.31–0.75)** | 0.61 (0.39–0.95)* |
| Child’s race | |||
| Non-Hispanic white | 175/1271 (14) | 1 | 1 |
| Non-Hispanic black | 27/310 (10) | 0.67 (0.40–1.12) | 0.87 (0.51–1.49) |
| Other | 22/266 (8) | 0.54 (0.31–0.95)* | 0.73 (0.40–1.35) |
| Child covered by health insurance | |||
| No/don’t know | 9/108 (8) | 1 | |
| Yes | 215/1739 (12) | 1.65 (0.75–3.61) | |
| Parent’s sex | |||
| Male | 19/299 (7) | 1 | 1 |
| Female | 205/1548 (13) | 2.14 (1.14–4.03)* | 2.17 (1.16–4.08)* |
| Annual household income | |||
| < $50,000 | 73/751 (9) | 1 | 1 |
| ≥ $50,000 | 136/938 (15) | 1.72 (1.18–2.52)** | 1.21 (0.79–1.84) |
| Not reported | 15/158 (8) | 0.86 (0.41–1.82) | 0.79 (0.37–1.71) |
| Highest education in household | |||
| High school or less | 22/392 (5) | 1 | 1 |
| Some college or more | 202/1455 (14) | 3.21 (1.87–5.53)** | 2.45 (1.30–4.63)** |
| Urbanicity | |||
| Rural | 43/445 (10) | 1 | |
| Urban/suburban | 181/1402 (13) | 1.29 (0.83–2.02) | |
| Relationship with child’s healthcare provider | |||
| Personal healthcare provider | |||
| No/don’t know | 35/323 (9) | 1 | |
| Yes | 189/1524 (13) | 1.48 (0.93–2.35) | |
| Felt like partner in care in past year | |||
| Never/sometimes | 16/175 (10) | 1 | |
| Usually/always | 203/1637 (12) | 1.30 (0.68–2.46) | |
| Not reported | 5/35 (19) | 2.11 (0.63–7.12) | |
| Providers spent enough time in past year | |||
| Never/sometimes | 21/187 (9) | 1 | |
| Usually/always | 198/1614 (12) | 1.39 (0.78–2.48) | |
| Not reported | 5/46 (16) | 1.90 (0.59–6.12) | |
| Health of child | |||
| General health | |||
| Fair/poor | 4/52 (14) | 1 | |
| Good/very good/excellent | 220/1795 (12) | 0.89 (0.28–2.85) | |
| Born before due date | |||
| No/don’t know | 115/1173 (10) | 1 | 1 |
| Yes | 109/674 (16) | 1.72 (1.21–2.45)** | 1.43 (1.00–2.05)* |
| Limited ability to do things | |||
| No/don’t know | 209/1738 (12) | 1 | |
| Yes | 15/109 (16) | 1.37 (0.66–2.87) | |
| Parenting behaviors | |||
| Ever breastfed childa | |||
| No | 42/491 (9) | 1 | 1 |
| Yes | 170/1125 (15) | 1.76 (1.12–2.78)* | 1.20 (0.75–1.94) |
| Not reported | 12/231 (8) | 0.93 (0.43–2.01) | 1.00 (0.46–2.14) |
| Healthy child feeding practices index scoreb | |||
| Low (5–10) | 15/193 (5) | 1 | 1 |
| Medium (11–15) | 101/1013 (10) | 2.25 (1.09–4.62)* | 1.81 (0.84–3.92) |
| High (16–20) | 108/641 (17) | 4.11 (2.00–8.44)** | 2.81 (1.27–6.22)* |
Note: OR: odds ratio. CI: confidence interval. Table shows raw frequencies and weighted estimates.
Item administered only to respondents who were biological parents (n=1617).
Index scores reflect the total of 5 items that assessed the child’s consumption of fruit, vegetables, home-cooked family meals, fast food meals, and sweetened beverages. Each item was worth 4 points with higher scores corresponding to healthier practices.
p < 0.05
p < 0.0
Beyond demographic characteristics, forgone vaccination was more common for children born before versus on or after their due dates (16% versus 10%). Forgone vaccination also correlated with high versus low scores on the index of healthy child feeding practices (17% versus 5%). In exploratory bivariate analyses, 4 of 5 items in the index achieved statistical significance: fruit consumption, vegetable consumption, sweetened beverage consumption, and frequency of home-cooked family meals (Table 3). Breastfeeding correlated with foregone vaccination in bivariate analyses, but did not retain statistical significance in the multivariate model.
Table 3.
Forgone vaccination for items in the healthy child feeding practices index, 2010 Child Health Assessment and Monitoring Program (CHAMP) survey, North Carolina, USA (n=1847).
| n/N (%) | p | |
|---|---|---|
| Fruit servings per day | 0.00 | |
| 0 | 12/154 (7) | |
| 1 | 65/638 (9) | |
| 2 | 78/615 (14) | |
| 3 or more | 69/440 (15) | |
| Vegetable servings per day | 0.04 | |
| 0 | 10/102 (8) | |
| 1 | 63/516 (11) | |
| 2 | 80/766 (12) | |
| 3 or more | 71/463 (16) | |
| Home-cooked family meals per week | 0.01 | |
| 0–2 | 20/177 (10) | |
| 3–5 | 50/421 (9) | |
| 6–7 | 62/580 (11) | |
| 8 or more | 92/669 (15) | |
| Fast food meals per weeka | 0.27 | |
| 0 | 86/556 (15) | |
| 1 | 76/682 (11) | |
| 2 | 36/385 (11) | |
| 3 or more | 26/224 (11) | |
| Sweetened beverages per daya | 0.00 | |
| 0 | 123/644 (19) | |
| 1 | 45/548 (9) | |
| 2 | 29/335 (9) | |
| 3 or more | 27/320 (7) |
Note: Table shows bivariate associations with forgone vaccination. Data are raw frequencies and weighted percentages.
Items reverse-coded to create index.
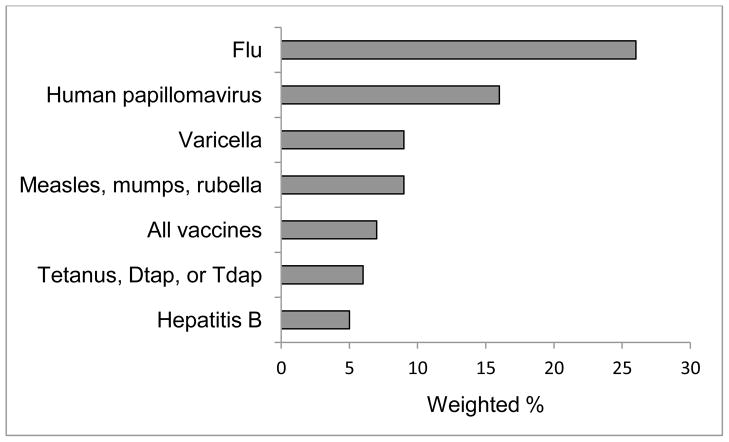
Forgone vaccines: types and reasons
Among parents who reported forgoing a vaccine for their child (n=224), the most commonly cited vaccines were flu (26%) and human papillomavirus (16%) (Figure 1). Most parents named one (56%) or two (13%) vaccines, and very few (7%) responded “all.” A total of 55 parents did not name a vaccine, including 41 non-respondents (17%) and 14 parents (5%) who responded with “don’t know.” The most commonly stated reason for forgoing vaccine was concern about safety or side effects (34%). Other concerns included believing the child did not need (18%) or was too young (13%) for the vaccine, that the child was sick at the time of the visit (10%), or needing more information (7%). Most parents named one (67%) or two (31%) reasons.
Figure 1.
Vaccines refused or delayed. Data from the 2010 Child Health Assessment and Monitoring Program (CHAMP) survey, North Carolina, USA (n=224)a.
a 55 parents did not name a specific vaccine.
DISCUSSION
A sizeable minority of parents in our North Carolina sample reported forgone vaccination, with more parents of young children (16%) reporting the behavior. Our statewide estimate for young children is similar to findings of several previous national studies, including those by Dempsey et al. (2011) and Gust et al. (2008), which placed the prevalence of forgone vaccination at 13% and 19%, respectively. To our knowledge, we are the first to report the prevalence of forgone vaccination for older children (12%) or teens (8%). Although our cross-sectional study design prevents us from determining why parents of teens less often reported having ever refused or delayed a vaccine, recall bias may have been a contributing factor since parents of older children likely had more difficulty remembering instances of forgone vaccination that occurred in early childhood. Alternatively, these data are also consistent with the conclusion that forgoing vaccination is becoming more common. Longitudinal research is needed to more fully characterize the epidemiology of forgone vaccination, particularly with regard to trends in the prevalence of vaccine refusal and delay.
Perhaps our most notable finding is the association between forgone vaccination and indicators of healthy child feeding practices, including increased fruit and vegetable consumption, and decreased sweetened beverage consumption. This relationship may reflect a broader endorsement of a “natural” parenting style and desire to protect children from preservatives or other chemicals seen as being prevalent in vaccines and processed foods. Alternatively, healthier eating practices may be indicative of higher socioeconomic status, which prior research has linked to forgone vaccination (Smith et al., 2010; Smith et al., 2011). Though we controlled for income and education, we may not have fully controlled for socioeconomic status as a confounder of the relationship between feeding practices and forgone vaccination. As in previous studies (Smith et al., 2010; Smith et al., 2011), we found that forgone vaccination was more common among parents with higher levels of education. Thus, unlike most other health disparities, forgone vaccination appears to be more common among parents who have social and material resources to carefully attend to their children’s health.
We found forgone vaccination was more common among parents of children born before their due dates, and a reason parents often gave for forgoing vaccines was that their child was sick at the time of the healthcare visit. By contrast, we did not find forgone vaccination to be more common among children who were generally unwell or limited in their abilities. Taken together, these findings suggest that temporary periods of relative vulnerability may be more relevant to understanding forgone vaccination when compared to states of longer-term sickness or disability. We speculate that such times of acute stress may cause parents to overestimate the risks of vaccines while underestimating their benefits.
For babies born prematurely or with low birth weight, the American Academy of Pediatrics (2009a) recommends a routine immunization schedule with only a few exceptions. Timely immunization is particularly important for low birth weight infants given their increased susceptibility to vaccine preventable diseases. Nevertheless, under-immunization of this population starts at birth and persists through six months of age (Batra et al., 2009). Intervention is likely needed with not only parents, but also healthcare providers, to communicate the increased importance of immunization for preterm infants.
In the case of children who are sick at the time of the healthcare visit, parents and providers may similarly need more guidance about how to make immunization-related decisions. In general, current guidelines recommend vaccinating children with mild illnesses or low-grade fevers while moderate or severe illnesses constitute “precautions” requiring a case-by-case assessment of risks and benefits (AAP, 2009b). Unfortunately, some providers lack knowledge of vaccine-related contraindications and take an overly conservative approach to vaccinating sick children (Cohen et al., 2003). As a result, parents’ understandable tendency to forgo vaccines for sick children may be exacerbated by the advice of excessively cautious providers, resulting in missed opportunities.
We were surprised to find that forgone vaccination was not associated with variables related to the quality of the patient-provider relationship. Given the extent to which prior research emphasizes the importance of trust (Benin et al., 2006; Gust et al., 2008; Senier, 2008 Smith et al., 2011), we suspect that our measures may not have fully assessed this domain. In particular, two items related to whether the provider spent enough time with the child or made the parent feel like a partner in care were specific to the year prior to the survey. If parents’ opinions about their providers changed over time, or if parents changed providers to receive more satisfactory care, these items would not capture an association between relationship quality and forgone vaccination occurring in an earlier time period.
This cross-sectional study relied on parental reports of lifetime forgone vaccination, and as previously mentioned, parents of older children may have under-reported the behavior due to difficulties remembering forgone vaccination during early childhood. We were also limited by the construction of our outcome measure which combined vaccine refusals with intentional delays. This combined measure allowed us to compare our findings to prior research (Smith et al., 2011; Dempsey et al, 2011), but prevented us from assessing correlates of refusals and delays separately. We were similarly unable to differentiate short or medically-indicated delays from those which were long-term or otherwise avoidable. Finally, our sample was limited to respondents with access to landline telephones in North Carolina, and although we weighted our data to account for differential response rates, the generalizability of our findings to households without landlines and to parents residing in different states remains to be established (Miles et al., 2010). These limitations are offset by the study’s strengths which include a large, population-based sample and a good response rate.
Conclusions
Forgone vaccination poses an ironic problem for preventive medicine because the parents who most often refuse or delay vaccines would seem to be the ones best equipped for getting their children preventive care. For example, in our sample of children with relatively high access to care, parents refused or delayed vaccination despite higher levels of education or attention to diet, suggesting that social privilege and engagement in health issues are perversely at odds with vaccination behavior. Our study suggests that forgone vaccination may be more common in periods of relative vulnerability, and these times of acute illness may lead parents to overestimate the short-term risks of vaccination while undervaluing its benefits. Whatever the case, providers should reassure parents of sick or premature children that such conditions are not usually contraindications for vaccination. By preventing forgone vaccination, providers stand to protect their individual patients as well as their broader communities from vaccine preventable diseases.
Highlights.
We assessed forgone vaccination for a statewide sample of children (ages 1–17).
Overall, 12% of parents reported having refused or delayed vaccine for their child.
The most commonly forgone vaccines were flu and human papillomavirus.
Forgone vaccination correlated with more education and healthier feeding practices.
Forgone vaccination was also more common among parents whose child was born early.
Acknowledgments
This study was supported by GlaxoSmithKline, the Cancer Control Education Program at UNC Lineberger Comprehensive Cancer Center (R25 CA57726), and a NRSA in Primary Medical Care at the University of Minnesota (T32HP22239). NB has received HPV vaccine-related grants from or been on advisory boards for GlaxoSmithKline and Merck.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Melissa B. Gilkey, Email: gilkey@email.unc.edu.
Annie-Laurie McRee, Email: almcree@umn.edu.
Noel T. Brewer, Email: ntb@unc.edu.
References
- American Academy of Pediatrics. Pickering LK, Baker CJ, Kimberlin DW, Long SS, editors. Active and passive immunization. [accessed June 2012];Red Book: 2009 Report of the Committee on Infectious Diseases. (28). 2009a Available at: http://aapredbook.aappublications.org/cgi/content/full/2009/1/1.7.1.
- American Academy of Pediatrics. Pickering LK, Baker CJ, Kimberlin DW, Long SS, editors. Guide to contraindications and precautions to immunizations. [accessed June 2012];Red Book: 2009 Report of the Committee on Infectious Diseases. (28). 2009a Available at: http://aapredbook.aappublications.org/cgi/content/full/2009/1/6.6.
- Batra JS, Eriksen EM, Zangwill KM, Lee M, Marcy M, Ward JI. Evaluation of vaccine coverage for low birth weight infants during the first year of life in a large managed care population. Pediatrics. 2009;123:951–958. doi: 10.1542/peds.2008-0231. [DOI] [PubMed] [Google Scholar]
- Benin AL, Wisler-Scher DJ, Colson E, Shapiro ED, Homnboe ES. Qualitative analysis of mothers’ decision-making about vaccines for infants: the importance of trust. Pediatrics. 2006;117:1532–1541. doi: 10.1542/peds.2005-1728. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. [accessed June 2012];Behavioral Risk Factor Surveillance System: 2010 summary data quality report. 2011 Available at: ftp://ftp.cdc.gov/pub/Data/Brfss/2010_Summary_Data_Quality_Report.pdf.
- Centers for Disease Control and Prevention. National and state vaccination coverage among adolescents aged 13–17 years - United States, 2011. MMWR. 2012;61:671–677. [PubMed] [Google Scholar]
- Cohen NJ, Lauderdale DS, Shete PB, Seal JB, Daum RS. Physician knowledge of catch-up regimens and contraindications for childhood immunizations. Pediatrics. 2003;111:925–932. doi: 10.1542/peds.111.5.925. [DOI] [PubMed] [Google Scholar]
- Dempsey AF, Schaffer S, Singer D, Butchart A, Davis M, Freed GL. Alternative vaccination schedule preferences among parents of young children. Pediatrics. 2011;128:848–856. doi: 10.1542/peds.2011-0400. [DOI] [PubMed] [Google Scholar]
- Dorell C, Yankey D, Strasser S. Parent-reported reasons for nonreceipt of recommended adolescent vaccinations, National Immunization Survey: Teen, 2009. Clin Pediatr. 2011;50:1116–1124. doi: 10.1177/0009922811415104. [DOI] [PubMed] [Google Scholar]
- Fredrickson DD, Davis TC, Arnold CL, Kennen EM, Humiston SG, Cross JT, Bocchini JA. Childhood immunization refusal: provider and patient perceptions. Fam Med. 2004;36:431–439. [PubMed] [Google Scholar]
- Gaudino JA, Robison S. Risk factors association with parents claiming personal-belief exemptions to school immunization requirements: community and other influences on more skeptical parents in Oregon, 2006. Vaccine. 2012;30:1132–1142. doi: 10.1016/j.vaccine.2011.12.006. [DOI] [PubMed] [Google Scholar]
- Gust DA, Darling N, Kennedy A, Schwartz B. Parents with doubts about vaccines: which vaccines and reasons why. Pediatrics. 2008;122:718–725. doi: 10.1542/peds.2007-0538. [DOI] [PubMed] [Google Scholar]
- Keane MT, Walter MV, Patel BI, Moorthy S, Stevens RB, Bradley KM, Buford JF, Anderson EL, Anderson LP, et al. Confidence in vaccination: a parent model. Vaccine. 2004;23:2486–2493. doi: 10.1016/j.vaccine.2004.10.026. [DOI] [PubMed] [Google Scholar]
- Kempe A, Daley MF, McCauley MM, Crane LA, Suh CA, Kennedy AM, Basket MM, Stokley SK, Dong F, et al. Prevalence of parental concerns about childhood vaccines: the experience of primary care physicians. Am J Prev Med. 2011;40:548–555. doi: 10.1016/j.amepre.2010.12.025. [DOI] [PubMed] [Google Scholar]
- Kennedy A, LaVail K, Nowak G, Basket M, Landry S. Confidence about vaccines in the Unites States: understanding parents’ perceptions. Health Aff. 2011;6:1151–1159. doi: 10.1377/hlthaff.2011.0396. [DOI] [PubMed] [Google Scholar]
- Miles DR, Herrick H, Ford CA. North Carolina Department of Health and Human Services, Division of Public Health. The North Carolina Child Health Assessment and Monitoring Program: survey methodology and data collection. Statistical Primer: A Publication of the State Center for Health Statistics. 2010;18:1–14. [Google Scholar]
- North Carolina State Center for Health Statistics. [accessed June 2012];Behavioral Risk Factor Surveillance System (BRFSS) 2011a Available at: http://www.epi.state.nc.us/SCHS/brfss/
- North Carolina State Center for Health Statistics. [accessed June 2012];Child Health Assessment and Monitoring Program (CHAMP) 2011b Available at: http://www.epi.state.nc.us/SCHS/champ/
- Omer SB, Pan WKY, Halsey NA, Stockley S, Moulton LH, Navar AM, Pierce M, Salmon DA. Nonmedical exemptions to school immunization requirements: secular trends and association of state policies with pertussis incidence. JAMA. 2006;296:1757–1763. doi: 10.1001/jama.296.14.1757. [DOI] [PubMed] [Google Scholar]
- Opel DJ, Mangione-Smith R, Taylor JA, Korfiatis C, Wiese C, Catz S, Martin DP. Hum Vaccin. 2011;7:419–425. doi: 10.4161/hv.7.4.14120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senier L. “It’s your most precious thing”: worst-case thinking, trust, and parental decision making about vaccination. Social Inquiry. 2008;78:207–229. [Google Scholar]
- Smith PJ, Humiston SG, Marcuse EK, Zhao Z, Dorell CG, Howes C, Hibbs B. Parental delay or refusal of vaccine doses, childhood vaccination coverage at 24 months of age, and the Health Belief Model. Public Health Rep. 2011;126(Suppl 2):135–146. doi: 10.1177/00333549111260S215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith PJ, Humiston SG, Parnell T, Vannice KS, Salmon DA. The association between intentional delay of vaccine administration and timely childhood vaccine coverage. Public Health Rep. 2010;125:534–541. doi: 10.1177/003335491012500408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith PJ, Kennedy AM, Wooten K, Gust DA, Pickering LK. Association between health care providers’ influence on parents who have concerns about vaccine safety and vaccination coverage. Pediatrics. 2006;118:1287–1292. doi: 10.1542/peds.2006-0923. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. [accessed June 2012];Metropolitan and micropolitan statistical areas. 2011 Available at: http://www.census.gov/population/metro/