Abstract
Aim
There is a wealth of evidence suggesting that patients with schizophrenia tend to respond to life stressors using less effective coping skills, which are in turn related to poor outcome. However, the contribution of coping strategies to outcome in youth at clinical high risk (CHR) for developing psychosis has not been investigated.
Methods
This longitudinal study followed CHR youth over a twelve-month period, using the Brief COPE questionnaire. CHR subjects (n=88) were compared at baseline to a healthy control sample (n=53), and then mixed models were used to explore the relationship of coping strategies to clinical and psychosocial outcomes in CHR subjects over time (n=102).
Results
Cross-sectional analyses revealed that, in comparison to healthy controls, CHR youth reported using more maladaptive coping strategies (p<.001) and fewer adaptive coping strategies (p<.01). Longitudinal analyses within the CHR group showed significant decreases in maladaptive coping and symptom severity over time, with corresponding improvements in social and role functioning. Adaptive coping was associated with better concurrent social functioning and less severe symptomatology (both p<.001). Over time, more maladaptive coping was associated with more severe positive and negative symptoms (both p < .005).
Conclusions
Youth at-risk for psychosis report using fewer adaptive and more maladaptive coping strategies relative to healthy controls. Over one year follow-up, more adaptive coping styles are associated with less severe clinical symptomatology and better social functioning. These findings suggest that teaching adaptive coping styles may be an important target for intervention in youth at high risk for psychosis.
Keywords: ultra high risk, psychosis prodrome, coping, psychosocial functioning
Introduction
The stress-vulnerability model of schizophrenia proposes that psychosocial stressors are a pervasive risk factor contributing to the onset of psychosis1, 2. According to this model, poor coping responses to these stressors are fundamental to the development, course and outcome of illness. Coping refers to the cognitive processes and behaviors in which one engages to tolerate or minimize stress3. In patients with schizophrenia, coping style is significantly correlated with both severity of clinical symptomatology and psychosocial functioning, and indeed mediates the relationship between them4. In addition, coping styles in schizophrenia patients are related to quality of life5, 6, distress about one’s illness7, cognitive abilities8, social functioning9, and negative mood changes during a laboratory psychosocial stress task10. In schizophrenia patients with a recent onset of illness, coping styles affect levels of self-efficacy11, cognitive performance11, psychosocial functioning12, clinical symptomatology13, and quality of life13. Collectively, these findings suggest that coping styles affect multiple domains of functioning and quality of life in individuals with psychotic disorder, including those whose symptoms have appeared only recently.
In an attempt to reduce the chronic and severe disability associated with schizophrenia, there have been increasing efforts to identify and provide interventions for individuals who are at clinical high risk (CHR) for developing the disorder14–16. Primary goals in early intervention research are to prevent deterioration in functioning, decrease severity of symptoms over time, and lower the amount of stress that individuals experience. Given the clear relevance of coping styles to symptoms and functioning in schizophrenia patients, examining coping styles in CHR individuals – and their relationship to changes in clinical symptomatology and psychosocial outcome – may ultimately contribute to the development of more effective intervention strategies.
Two studies investigating coping style in CHR individuals were recently published. The first showed that, in comparison to controls, CHR individuals report engaging in active coping less often17. Additionally, Lee and colleagues18 found that maladaptive coping was significantly related to negative symptoms in CHR individuals. However, both studies were cross-sectional in design and thus cannot address how coping may change over time, nor how coping styles may relate to changes in clinical symptomatology. Employing a longitudinal design, a recent study in an adolescent general population sample found that adaptive coping styles were related to a decrease in self-reported subclinical positive psychotic experiences over time, while maladaptive coping styles were related to an increase in such experiences19. However, these were not help-seeking individuals, and psychotic experiences were measured via a self-report questionnaire. Associations between symptoms and coping styles over time have yet to be examined in help-seeking individuals meeting criteria for a putative prodromal syndrome.
It is important to note that, unlike patients with established illness, those at risk for schizophrenia are typically adolescents, undergoing developmental changes that are accompanied by a host of distinct stressors20. Notably, poor coping strategies have been linked to lower levels of psychosocial health and increased behavioral problems in typically developing adolescents21, 22. At the same time, healthy adolescents tend to develop a wider repertoire of coping strategies and become more active in their coping styles as they get older (e.g. showing an increased use of strategies such as problem-solving or seeking emotional support23, 24). Thus, examining the developmental trajectory of coping styles in CHR individuals may also be important for understanding developmental effects on stress response.
The Brief COPE questionnaire, a short, well-validated measure that assesses how individuals respond to stressful events25, has been successfully used to examine coping patterns in schizophrenia patients4. Here we used the Brief COPE to identify the types of coping styles employed by CHR youth and to assess whether these coping strategies are different from their same-age peers. Based on prior findings in patients with schizophrenia (e.g.,4, 10) we first hypothesized that, in comparison to healthy participants, CHR individuals would implement fewer adaptive coping techniques and use more maladaptive coping strategies. Second, to better characterize how coping strategies are related to other clinical characteristics in CHR individuals, we examined the association between baseline coping styles and current symptomatology. In accordance with previous findings4, we hypothesized that lower levels of adaptive coping would be associated with more severe clinical symptomatology. Finally, we explored whether coping styles in CHR individuals changed over a one-year follow-up period, and how coping style was associated with clinical symptomatology and psychosocial functioning over that time frame. Specifically, we investigated whether: (a) baseline coping profiles were predictive of symptom trajectories; and (b) coping strategies were associated with concurrent symptoms over time.
Method
Participants
The total sample with brief COPE data consisted of 102 CHR individuals and 53 demographically comparable control participants, who were part of a longitudinal study of individuals at high-risk for developing psychosis at the University of California, Los Angeles. Note that the current sample was drawn from a larger longitudinal study of individuals at high risk and a healthy comparison group. Because the participants in our study are administered a large number of measures at each time point (clinical interviews, neurocognitive evaluation, neuroimaging, etc.), sometimes they do not complete every task at each timepoint. In particular, study participants often took home self-report questionnaires to fill out later (e.g., Brief COPE), but then did not return them to the clinic, resulting in some incomplete data at baseline. As a result, we have partially incomplete data at each timepoint, including baseline (baseline N: 88, six-month: 43, 12-month: 30). Because our analytic strategy (mixed model regression) is robust to missing data26, we were able to take advantage of data points for individuals who were missing coping data at the baseline timepoint. Although we only had 30 individuals with brief COPE data at the 12-month assessment, only 30 participants had actually dropped out of the overall study by that timepoint, which lessens our concern about differential attrition effects.
At baseline, all eligible individuals were ages 12–35 years, and CHR participants met criteria for one of three conditions, based on the Structured Interview for Prodromal Symptoms (SIPS27): 1) attenuated (subthreshold) psychotic symptoms; 2) transient, recent-onset psychotic symptoms; or 3) a substantial, recent drop in functioning in conjunction with schizotypal personality disorder diagnosis or a first-degree relative with a psychotic disorder. Axis I disorders were assessed via semi-structured diagnostic interviews [Kiddie Schedule for Affective Disorders and Schizophrenia (K-SADS28) for participants aged 12–15, or the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-P29), for participants over 15]. Participants were excluded from the study if they met criteria for an Axis I schizophrenia spectrum diagnosis (schizophrenia, schizoaffective disorder, or schizophreniform disorder). Control participants were recruited from the community through advertisements posted in newspapers and flyers. Inclusion criteria for controls required that they did not display evidence of either any major mental disorder or a prodromal syndrome, based on information gathered during the diagnostic interviews. Participants were also excluded if they had a neurological disorder which might affect performance on study tasks, insufficient fluency in English, an estimated IQ of <70, or if they endorsed substance or alcohol abuse and/or dependence within the past six months. Inter-rater reliability and case consensus procedures have been described in detail elsewhere30 and all raters demonstrated good reliability with kappa values ranging from .85 to 1.00.
At the baseline assessment, the breakdown of medication use in CHR individuals was as follows: 28% of CHR participants were taking no medication, 22% were taking antipsychotics, 36% were taking antidepressants, and 14% were taking other psychotropic medications (e.g., mood stabilizers, psychostimulants). Additionally, at the baseline assessment, 51% of CHR individuals (n=45) were not enrolled in any type of psychotherapy, while 49% of CHR individuals (n=43) reported that they were currently involved in ongoing, regularly attended therapy.
All participants underwent a verbal and written informed consent process. Subjects under the age of 18 years provided written assent, while their parent or guardian completed written consent. All procedures and informed consent materials were approved by the University of California, Los Angeles Institutional Review Board.
Clinical, Psychosocial Outcome, and Cognitive Measures
Clinicians rated positive, negative, disorganized and general symptom items from the SIPS (McGlashan, 2001) at each timepoint (baseline, 6- and 12-months). Social and role functioning were assessed using the Global Functioning Social (GSF) and Role (GRF) Scales, measures developed specifically to assess psychosocial functioning in younger individuals 31. The GSF evaluates how much time one spends with friends and family, how one deals with peer-related conflicts, and whether or not one seeks out others. The GRF assesses the level at which an individual is functioning in an academic or a work environment. Both scales have shown good construct validity, strong inter-rater reliability, and have successfully identified significant social and role impairment in CHR youth31. A Full Scale IQ estimate derived from two subtests from the Wechsler Abbreviated Scale of Intelligence (WASI), Vocabulary and Matrix Reasoning, was used as a measure of general intellectual functioning 32.
Coping Measure
Coping abilities were assessed using the Brief Cope25, a 28-item questionnaire that assesses how an individual deals with difficult situations. This questionnaire has shown good reliability and validity in adults25, and has also been used with adolescents (e.g., 33). Participants are presented with 28 questions and asked to report how they have generally responded to stressful events in the past 12 months. A four point Likert Scale (0–3) is used to determine how often an individual engages in a given behavior, with zero referring to “not at all” and three meaning “all of the time”. The 28 items comprise two separate scales reflecting maladaptive (e.g., blaming one’s self for the occurrence of the event) and adaptive (e.g., choosing to reinterpret the event in a positive fashion) coping styles (see 4 for details).
Statistical Analyses
All statistical analyses were performed using SPSS software v. 18 (SPSS Inc., Chicago, Illinois). The primary cross-sectional analysis of coping strategies used multiple linear regression models with maladaptive and adaptive coping scores as the outcomes, group (patients, controls) as the between-subjects factor and IQ, age, and gender as covariates. We explored interactions between diagnostic group and demographic variables to investigate whether differences between CHR and healthy youth varied as a function of these factors. Pearson correlations were used to examine the relationship between baseline coping style, clinical and psychosocial measures in each group.
Longitudinal analyses within the CHR group alone were used to determine: (1) whether there were changes in coping, symptoms and psychosocial function over time and (2) whether the symptom and functioning variables were associated with coping strategies over time. To examine developmental trajectories of coping strategies (adaptive and maladaptive), functioning (social and role) and clinical symptomatology (SIPS positive, negative, disorganized and general symptoms) we fit mixed models with each of these variables as the outcome and time (baseline, six months, twelve months) as a within-subject factor. To determine whether poorer initial coping skills were predictive of poorer outcome trajectories, we added baseline adaptive and maladaptive coping scores and their interactions with time to the trajectory models for clinical symptomatology and psychosocial factors. Next, to examine whether the clinical outcome trajectories tracked with the coping trajectories over time we refit the mixed models for symptoms and functioning with concurrent coping scores as time-varying covariates. As a secondary analysis, we examined the effects of type of medication prescribed and psychological treatment status as both baseline and time-varying covariates.
Results
The baseline cross-sectional analysis used the 88 CHR individuals (M=58, F=30) and 53 control participants (M=27, F=26) who had coping scores at this timepoint. As shown in Table 1, the groups were comparable on all demographic factors (all p-values > .09) but differed on IQ, with controls having significantly higher IQ than CHR patients (t139=3.00; p=.003).
Table 1.
Baseline Comparison Demographic Information
| CHR Individuals (n=88) | Healthy Comparison Participants (n=53) | ||
|---|---|---|---|
|
| |||
| Age, in years (+/− SD) | 17.9 (3.4) | 17.8 (4.4) | p=.70 |
|
| |||
| Parental Education (+/− SD) | 15.6 (3.0) | 16.4 (2.9) | p=.11 |
|
| |||
| Gender (N, % female) | 30 (35%) | 26 (49%) | p=.10 |
|
| |||
| Race (N) | p=.57 | ||
| African-American | 4 | 4 | |
| Pacific Islander | 6 | 4 | |
| Caucasian | 48 | 22 | |
| Native American | 0 | 1 | |
| Latino | 20 | 15 | |
| Other | 10 | 7 | |
|
| |||
| Prodromal Syndrome (N) | NA | ||
| Attenuated Positive Symptoms | 63 | ||
| Brief Intermittent Psychosis | 15 | ||
| Genetic Risk and Deterioration | 8 | ||
| Genetic Risk and Deterioration + | 2 | ||
| Attenuated Positive Symptoms | |||
|
| |||
| Medications (N) | NA | ||
| No medications | 25 | ||
| Antipsychotics | 19 | ||
| Antidepressants | 32 | ||
| Other | 12 | ||
|
| |||
| WASI IQ, 2 subtests (+/− SD) | 104.5 (15.5) | 112.1 (12.9) | p=.003 |
3.1 Cross-Sectional Analyses
In the cross-sectional model for adaptive coping, there was a significant interaction between group and IQ (F(1,135)=9.1,p=.003) and significant main effects for group (F(1,135)=7.6,p=.007), age (F(1,135)=11.9,p=.001) and IQ (F(1,135)= 7.7,p=.006), but not gender (F(1,135)=.9,p=.34). Follow-up tests of the raw correlations in the individual groups showed that as IQ levels increased, reported levels of adaptive coping also increased in controls (r=.44, p=.001), but not CHR patients (r=-.02,p=.86). In both CHR patients and controls, older individuals reported higher levels of adaptive coping (r= .27, p=.013; r= .36, p=.008, respectively).
For maladaptive coping, there were no significant interactions, but there were significant main effects for group (F(1,136)=47.21, p<.001; mean difference (patients-controls)=6.17) and gender (F(1,136)=4.2, p=.042; mean difference (females-males)=1.68). CHR individuals reported using significantly more maladaptive coping strategies than controls. Females reported using higher levels of maladaptive coping strategies in comparison to males.
3.1.2. Relationship Between Baseline Coping Style, Clinical Symptomatology and Psychosocial Outcome
The relationships between baseline coping style and concurrent clinical symptomatology and outcome variables were also tested within each group. More adaptive coping was associated with significantly fewer negative symptoms (r=-.31, p=.003) in CHR individuals. Additionally, the more adaptive coping reported by CHR individuals, the higher their level of social functioning as measured by the GSF (r=-.32, p=.003). The controls did not show significant relationships between adaptive coping and any of the clinical or psychosocial measures (all p>.16). No relationships between maladaptive coping and clinical or psychosocial variables were observed in either group (all p>.12).
3.1.3. Medication and Psychological Treatment Cross-Sectional Analyses
There were no significant baseline differences in the CHR sample in adaptive (F(3,84)=.36, p=.43) or maladaptive coping style (F(3,84)=.36, p=.78) based on type of medication prescribed (groups=no medications, antipsychotics, anti-depressants, other). Additionally there were no significant differences in coping styles between CHR individuals engaged in psychological treatment at baseline and those who were not (adaptive coping: F(1,87)=2.2, p=.14; maladaptive coping F(1,87)=.17, p=.68).
3.2 Longitudinal Analyses
In the CHR sample, individuals who dropped out of the study before the 6 or 12 month assessment (N=30) showed no difference at baseline on any outcomes of interest (all p-values > .30) from those who went on to complete the study or were still in active follow-up at the time of this analysis (N=58), providing support for the idea that data are missing at random, as assumed for mixed models employed in the longitudinal analyses 26. Because the primary focus of the study was on the relationship of coping style to symptoms and functioning in CHR individuals, we did not examine longitudinal relationships between coping style, symptoms and functioning in healthy controls.
3.2.1 Change in Coping, Clinical, and Psychosocial Measures Over Time
To examine the developmental trajectories of the major coping, symptom and psychosocial measures in the CHR group we fit mixed models with each of these variables as the outcome and time (0, 6, 12 months) as a within-subjects factor. There was no evidence of a change in adaptive coping strategies over the study period (F(2, 81)=.44,p=.64). However, maladaptive coping (F(2,80)=3.4,p=.038), positive symptoms (F(2,148)=13.7,p<.001), negative symptoms (F(2,116)=11.4,p<.001), disorganized symptoms (F(2,122)=4.4,p=0.014), and general symptoms (F(2,120)=8.7,p<.001) all decreased significantly. Correspondingly there were significant improvements over time in social functioning (F(2,120)=13.9,p<.001) and role functioning (F(2,116)=7.2,p=.001). In all cases, follow-up tests suggested that the significant changes occurred between 0–6 months; however, this significant finding may be due to the fact that there was a much smaller sample size at the 12-month timepoint.
3.2.2. Baseline and Concurrent Coping as Predictors of Pyschosocial and Clinical Outcomes
To determine whether worse baseline coping strategies were predictive of a poorer trajectory, or progression over time, we added baseline adaptive and maladaptive coping scores and their interactions with time to the trajectory models for the clinical and psychosocial variables. None of the coping style by time interactions was significant, meaning that we were not able to successfully predict clinical and psychosocial progression as a function of baseline coping. There were, however, main effects of coping in many of the models, as detailed below, meaning that overall better baseline coping strategies were associated with better outcomes. There were also no significant main effects or time interactions of baseline medication type and psychosocial treatment status when these covariates were added to the models.
To further examine the longitudinal relationship between coping style and outcomes, we added the adaptive and maladaptive coping scores as time-varying covariates to the trajectory models. This allowed us to examine the association between coping scores and concurrent symptoms and functioning. We found that greater use of adaptive coping strategies tracked with significantly better social functioning (F(1,140)=11.5,p=.001), and lower levels of negative (F(1,147)=14.7, p<.001) and disorganized symptoms over time (F(1,146)=8.2, p=.005). Similarly, we found significant associations between increased use of maladaptive coping strategies and higher concurrent levels of positive (F(1,142)=9.3, p=.003), negative (F(1,151)=9.86, p=.002), disorganized (F(1,151)=5.1, p=.025) and general symptoms (F(1,148)=16.6, p=.003).
Medication type and treatment status were also added as time-varying covariates to the above models. Though we did not find any interactions between type of medication prescribed, treatment status, time, and/or coping styles, we found several main effects of medication type when it was included as a time-varying covariate. Perhaps most importantly, the significant results that we identified between coping styles and psychosocial and clinical variables maintained when including medication and therapy status in the model.
Discussion
This study revealed several novel findings regarding the relationships between coping style, clinical symptomatology and psychosocial outcome in youth at clinical high-risk for psychosis. Cross-sectional analyses revealed that relative to healthy controls, CHR youth reported using significantly fewer adaptive coping strategies and more maladaptive coping strategies. In addition, there were effects of both IQ and development; in particular, higher IQ was associated with higher levels of adaptive coping in controls, but not in CHR patients. In contrast, increasing age was associated with higher levels of adaptive coping in both CHR patients and controls, indicating that both groups are more likely to implement adaptive coping strategies as they grow older.
In our longitudinal analyses of CHR individuals, adaptive coping did not significantly change over the 12-month period, but there were significant decreases in reported maladaptive coping strategies, along with significant improvements in psychosocial functioning and decreases in clinical symptomatology. Over time, adaptive coping was associated with better social functioning and less severe negative and disorganized symptoms. Additionally, over the 12-month period, more maladaptive coping strategies were associated with more severe clinical symptomatology. Finally, our time-varying covariate analysis of coping styles indicated that overall better coping strategies were associated with better concurrent outcomes.
These results are consistent with those of previous coping studies in patients with established schizophrenia diagnoses4, 10, and extend them into the critical period prior to onset of full psychosis. In comparison to same-age, healthy participants. CHR individuals are less likely to engage in adaptive coping strategies, and more likely to engage in maladaptive behaviors. These results suggest that, like those with a diagnosis of schizophrenia, CHR youth may not possess the skills to effectively cope with stressful situations. Additionally, when CHR individuals do attempt to cope with stressful situations, they may use strategies that may be detrimental to their functioning or exacerbate symptomatology.
These findings are also consistent with and build upon two recent cross-sectional studies. Pruessner and colleagues17 found that CHR individuals showed reduced levels of active coping, a specific type of adaptive coping measured by the Brief COPE, which we also found to be reduced in CHR individuals. Furthermore, similar to our findings, Lee and colleagues18 showed that maladaptive coping was significantly related to negative symptoms in CHR individuals. However, both of these studies included smaller sample sizes and did not include a longitudinal component, two strengths of the current study. Additionally, in a recent population-based study of adolescents, Lin and colleagues19 found that increased use of emotion-oriented coping styles (described as self-oriented emotional reactions, self-preoccupation and fantasizing) was associated with an increase in subclinical psychotic experiences, which is consistent with our finding of a significant relationship between maladaptive coping and positive symptoms over time in CHR individuals. The present study, however, establishes this relationship in a help-seeking population.
When observing relationships between baseline coping style and concurrent outcome variables, two significant findings emerged. Individuals who reported engaging in more adaptive coping styles had fewer negative symptoms and higher levels of social functioning. However, we did not identify a relationship between positive symptoms and coping styles, which Meyer4 observed in patients with chronic schizophrenia. This difference may be due to the fact that our study participants are not experiencing full-blown positive psychotic symptoms, with the present findings suggesting that the association between coping style and negative symptoms and social functioning emerges prior to the association between coping and positive symptoms. In support of our findings, two previous studies examining individuals at CHR who do not convert to psychosis, including some individuals with attenuated positive symptoms which remitted entirely over the course of follow-up, continued to display impaired social functioning34, 35. Thus, the association between coping style and negative symptoms and social functioning may therefore prove a valuable early target for relatively early-stage clinical intervention, as discussed below.
Certain limitations of this study must be noted. First, it would have been optimal to observe longitudinal changes in a healthy control sample, to determine whether the changes seen CHR individuals’ coping styles in a 12-month period are developmentally appropriate. However, due to low rates of completion of the coping measurement at the six (74%) and twelve (90%) month points for healthy controls, this analysis was not possible. Given that there were no significant differences in baseline clinical or demographic variables between CHR individuals who dropped out and those who remained in the study, we do not believe that our results are driven by a selection bias, but this possibility cannot be definitively ruled out. Another limitation of our study is that we did not directly assess the number and type of stressful events in the participants’ lives, and how these events may have contributed to how effectively an individual was coping. For example, if a CHR individual is distressed by his/her psychotic symptoms, he/she may cope differently with this stressor than another (e.g., difficulty with academics). Larger samples and a more fine-grained characterization of life stress would be necessary to show such conditional associations. Notably, we did not find that baseline coping style predicted subsequent symptomatic and functional trajectories. It is possible that our study was under-powered to detect significant coping by time interactions. However, the lack of findings may also be due to the fact that coping styles are not static traits with predictive value for symptom levels and functioning in CHR individuals. Instead, our findings suggest that coping styles correspond to one’s current functioning level or severity of symptoms, and are likely to represent important factors in a dynamic process of attempting to mediate one’s vulnerability to stress. For instance, given that CHR patients’ cumulative experience of “daily hassles” correlates with plasma cortisol level, which in turn predicts symptoms of depression and anxiety36 and may even precipitate psychotic symptoms37, it is reasonable to imagine that the experience of stress worsens symptoms, which degrades adaptive coping, in turn increasing stress, and on in a feed-forward cycle - consistent with the results of our time-varying covariate analysis. Intervention designed to slow or stop this cycle by bolstering an individual’s adaptive coping resources may in turn slow symptom exacerbation. In fact, similarly conceptualized approaches are in wide use to prevent relapse among remitted schizophrenia patients38. Alternatively, the self-reported use of adaptive and maladaptive coping patterns may track with concurrent symptoms because what is measured in an instrument such as the Brief Cope is analogous to what is measured in instruments for symptoms and functioning. Finally, due to the sample size limitations, we did not examine coping in relation to conversion to psychosis in CHR individuals.
These findings have important implications for the development of clinical interventions for CHR individuals. We found that, regardless of medication being prescribed or type of psychosocial treatment one is engaged in, maladaptive coping styles decreased over time. This finding suggests that maladaptive coping styles may be more malleable and easier to target than adaptive coping styles. Additionally, given that we found a strong relationship between adaptive coping and social functioning in CHR individuals, it may be effective to implement social skills training programs, which teach adaptive coping styles (e.g., problem-solving in interpersonal situations) and may lead to improvement in social functioning. Social skills training programs have shown promising results for both schizophrenia patients39 and typically developing adolescents40.
Future studies are warranted to determine why CHR individuals are less likely to use adaptive coping strategies, but more likely to engage in maladaptive ones. A recently published study on CHR youth shows, perceptions of one’s ability to cope with stressful situations, along with the appraisals of stressful life events experienced, may influence the type of coping style that one employs41. Furthermore, investigating the relationship between coping styles, appraisal of stressful life events, and symptomatology may provide us with more a better understanding of the stress-vulnerability model in schizophrenia. Alternatively, other factors, such as self-efficacy, have been found to account for a significant amount of the variance in coping styles of individuals with schizophrenia11, which may also be the case for CHR individuals.
To our knowledge, this is the first study to examine the relationship between coping styles with clinical symptomatology and psychosocial functioning in CHR individuals over time. These findings suggest that implementing interventions to teach adaptive coping styles and simultaneously reduce maladaptive coping styles in CHR individuals may also affect psychosocial functioning and clinical symptomatology. Identifying the coping strategies used by CHR individuals may aid in targeting specific interventions that may be useful in preventing the onset of psychosis.
Figure 1.
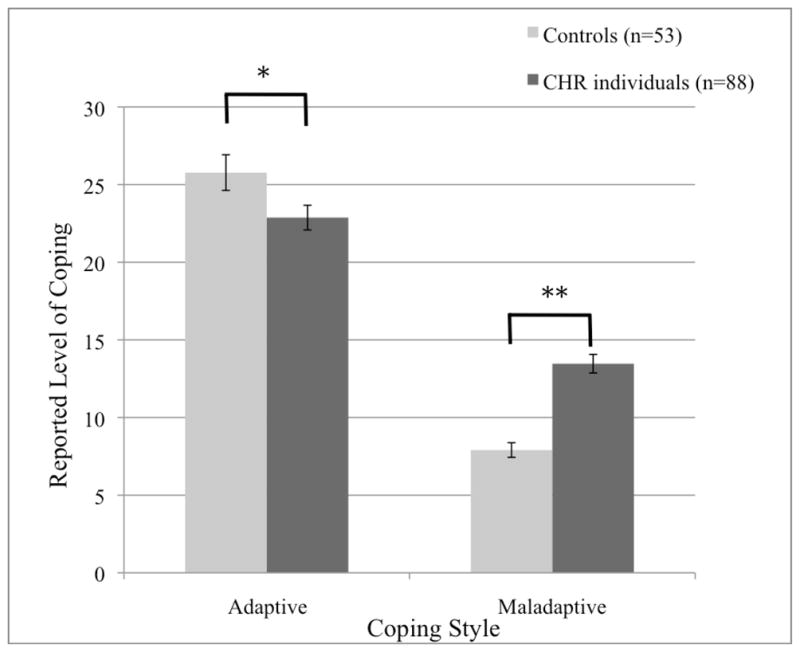
Baseline Coping Styles of CHR Individuals vs. Healthy Controls
*p<.01, **p<.001
Acknowledgments
Funding for this study was provided by NARSAD Young Investigator Award (Maxine and Jack Zarrow Investigator Award to CEB), National Institute of Mental Health grants K23MH74644 (CEB), MH65079 (TDC) and NIMH P50 MH066286 (TDC and CEB), UCLA Graduate Summer Research Mentorship Program for MEJ, as well as donations from the International Mental Health Research Organization (IMHRO) and Staglin Music Festival for Mental Health to the UCLA Foundation.
References
- 1.Nuechterlein KH, Dawson ME, Gitlin M, et al. Developmental Processes in Schizophrenic Disorders: longitudinal studies of vulnerability and stress. Schizophr Bull. 1992;18:387–425. doi: 10.1093/schbul/18.3.387. [DOI] [PubMed] [Google Scholar]
- 2.Nuechterlein KH, Dawson ME. A heuristic vulnerability/stress model of schizophrenic episodes. Schizophr Bull. 1984;10:300–12. doi: 10.1093/schbul/10.2.300. [DOI] [PubMed] [Google Scholar]
- 3.Lazarus RS, Folkman S. Stress, appraisal, and coping. New York, NY: Springer Publishing Company, Inc; 1984. [Google Scholar]
- 4.Meyer B. Coping with Severe Mental Illness: Relations of the Brief COPE with Symptoms, Functioning, and Well-Being. Journal of Psychopathology and Behavioral Assessment. 2001;23:265–77. doi: 10.1023/A:1010929402770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rudnick A, Martins J. Coping and schizophrenia: a re-analysis. Arch Psychiatr Nurs. 2009;23:11–5. doi: 10.1016/j.apnu.2008.02.009. [DOI] [PubMed] [Google Scholar]
- 6.Brenner K, St-Hilaire A, Liu A, Laplante DP, King S. Cortisol response and coping style predict quality of life in schizophrenia. Schizophrenia research. 2011;128:23–9. doi: 10.1016/j.schres.2011.01.016. [DOI] [PubMed] [Google Scholar]
- 7.Cooke M, Peters E, Fannon D, et al. Insight, distress and coping styles in schizophrenia. Schizophrenia research. 2007;94:12–22. doi: 10.1016/j.schres.2007.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lysaker PH, Bryson GJ, Marks K, Greig TC, Bell MD. Coping style in schizophrenia: associations with neurocognitive deficits and personality. Schizophr Bull. 2004;30:113–21. doi: 10.1093/oxfordjournals.schbul.a007056. [DOI] [PubMed] [Google Scholar]
- 9.Boschi S, Adams RE, Bromet EJ, Lavelle JE, Everett E, Galambos N. Coping with psychotic symptoms in the early phases of schizophrenia. Am J Orthopsychiatry. 2000;70:242–52. doi: 10.1037/h0087710. [DOI] [PubMed] [Google Scholar]
- 10.Horan WP, Blanchard JJ. Emotional responses to psychosocial stress in schizophrenia: the role of individual differences in affective traits and coping. Schizophrenia research. 2003;60:271–83. doi: 10.1016/s0920-9964(02)00227-x. [DOI] [PubMed] [Google Scholar]
- 11.Ventura J, Nuechterlein KH, Subotnik KL, Green MF, Gitlin MJ. Self-efficacy and neurocognition may be related to coping responses in recent-onset schizophrenia. Schizophrenia research. 2004;69:343–52. doi: 10.1016/j.schres.2003.09.002. [DOI] [PubMed] [Google Scholar]
- 12.Boschi S, Adams RE, Bromet EJ, Lavelle JE, Everett E, Galambos N. Coping with psychotic symptoms in the early phases of schizophrenia. Am J Orthopsychiatry. 2000;70:242–52. doi: 10.1037/h0087710. [DOI] [PubMed] [Google Scholar]
- 13.Thompson KN, McGorry PD, Harrigan SM. Recovery style and outcome in first-episode psychosis. Schizophrenia research. 2003;62:31–6. doi: 10.1016/s0920-9964(02)00428-0. [DOI] [PubMed] [Google Scholar]
- 14.Yung AR, McGorry PD. The prodromal phase of first-episode psychosis: past and current conceptualizations. Schizophr Bull. 1996;22:353–70. doi: 10.1093/schbul/22.2.353. [DOI] [PubMed] [Google Scholar]
- 15.McGorry PD, Yung AR. Early intervention in psychosis: an overdue reform. Aust N Z J Psychiatry. 2003;37:393–8. doi: 10.1046/j.1440-1614.2003.01192.x. [DOI] [PubMed] [Google Scholar]
- 16.Cannon TD, Cornblatt B, McGorry P. The empirical status of the ultra high-risk (prodromal) research paradigm. Schizophr Bull. 2007;33:661–4. doi: 10.1093/schbul/sbm031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pruessner M, Iyer SN, Faridi K, Joober R, Malla AK. Stress and protective factors in individuals at ultra-high risk for psychosis, first episode psychosis and healthy controls. Schizophrenia research. 2011;129:29–35. doi: 10.1016/j.schres.2011.03.022. [DOI] [PubMed] [Google Scholar]
- 18.Lee SY, Kim KR, Park JY, et al. Coping strategies and their relationship to psychopathologies in people at ultra high-risk for psychosis and with schizophrenia. J Nerv Ment Dis. 2011;199:106–10. doi: 10.1097/NMD.0b013e3182083b96. [DOI] [PubMed] [Google Scholar]
- 19.Lin A, Wigman JT, Nelson B, et al. The relationship between coping and subclinical psychotic experiences in adolescents from the general population -a longitudinal study. Psychol Med. 2011:1–12. doi: 10.1017/S0033291711000560. [DOI] [PubMed] [Google Scholar]
- 20.Spear LP. The adolescent brain and age-related behavioral manifestations. Neurosci Biobehav Rev. 2000;24:417–63. doi: 10.1016/s0149-7634(00)00014-2. [DOI] [PubMed] [Google Scholar]
- 21.Piko B. Gender differences and similarities in adolescents’ ways of coping. The Psychological Record. 2001;51:223–35. [Google Scholar]
- 22.Hampel P, Petermann F. Perceived stress, coping, and adjustment in adolescents. J Adolesc Health. 2006;38:409–15. doi: 10.1016/j.jadohealth.2005.02.014. [DOI] [PubMed] [Google Scholar]
- 23.Griffith MA, Dubow EF, Ippolito MF. Developmental and Cross-Situational Differences in Adolescents’ Coping Strategies. Journal of Youth and Adolescence. 2000;29:183–204. [Google Scholar]
- 24.Blanchard-Fields F, Irion JC. The relation between locus of control and coping in two contexts: age as a moderator variable. Psychol Aging. 1988;3:197–203. doi: 10.1037//0882-7974.3.2.197. [DOI] [PubMed] [Google Scholar]
- 25.Carver CS. You want to measure coping but your protocol’s too long: consider the brief COPE. Int J Behav Med. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 26.Edwards LJ. Modern statistical techniques for the analysis of longitudinal data in biomedical research. Pediatr Pulmonol. 2000;30:330–44. doi: 10.1002/1099-0496(200010)30:4<330::aid-ppul10>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 27.McGlashan TH. Structured Interview for Prodromal Syndromes (SIPS) New Haven: Yale University; 2001. [Google Scholar]
- 28.Kaufman J, Birmaher B, Brent D, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36:980–8. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 29.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders: Patient Edition. 1997. In press. [Google Scholar]
- 30.Meyer SE, Bearden CE, Lux SR, et al. The psychosis prodrome in adolescent patients viewed through the lens of DSM-IV. J Child Adolesc Psychopharmacol. 2005;15:434–51. doi: 10.1089/cap.2005.15.434. [DOI] [PubMed] [Google Scholar]
- 31.Cornblatt BA, Auther AM, Niendam T, et al. Preliminary findings for two new measures of social and role functioning in the prodromal phase of schizophrenia. Schizophr Bull. 2007;33:688–702. doi: 10.1093/schbul/sbm029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wechsler D. Wechsler Abbreviated Scale of Intelligence. 1999 In press. [Google Scholar]
- 33.Wilson GS, Pritchard ME, Revalee B. Individual differences in adolescent health symptoms: the effects of gender and coping. J Adolesc. 2005;28:369–79. doi: 10.1016/j.adolescence.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 34.Addington J, Cornblatt BA, Cadenhead KS, et al. At clinical high risk for psychosis: outcome for nonconverters. The American journal of psychiatry. 2011;168:800–5. doi: 10.1176/appi.ajp.2011.10081191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schlosser DA, Jacobson S, Chen Q, et al. Recovery From an At-Risk State: Clinical and Functional Outcomes of Putatively Prodromal Youth Who Do Not Develop Psychosis. Schizophr Bull. 2011 doi: 10.1093/schbul/sbr098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thompson KN, Phillips LJ, Komesaroff P, et al. Stress and HPA-axis functioning in young people at ultra high risk for psychosis. J Psychiatr Res. 2007;41:561–9. doi: 10.1016/j.jpsychires.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 37.Phillips LJ, McGorry PD, Garner B, et al. Stress, the hippocampus and the hypothalamic-pituitary-adrenal axis: implications for the development of psychotic disorders. Aust N Z J Psychiatry. 2006;40:725–41. doi: 10.1080/j.1440-1614.2006.01877.x. [DOI] [PubMed] [Google Scholar]
- 38.Hogarty GE. Prevention of relapse in chronic schizophrenic patients. J Clin Psychiatry. 1993;54 (Suppl):18–23. [PubMed] [Google Scholar]
- 39.Horan WP, Kern RS, Shokat-Fadai K, Sergi MJ, Wynn JK, Green MF. Social cognitive skills training in schizophrenia: an initial efficacy study of stabilized outpatients. Schizophrenia research. 2009;107:47–54. doi: 10.1016/j.schres.2008.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Thompson KL, Bundy KA, Wolfe WR. Social skills training for young adolescents: cognitive and performance components. Adolescence. 1996;31:505–21. [PubMed] [Google Scholar]
- 41.Phillips LJ, Edwards J, McMurray N, Francey S. Comparison of Experiences of Stress and Coping Between Young People at Risk of Psychosis and a Non-Clinical Cohort. Behavioural and cognitive psychotherapy. 2011:1–20. doi: 10.1017/S1352465811000397. [DOI] [PubMed] [Google Scholar]


