Abstract
Increased urinary protein excretion is common after renal transplantation and portends worse outcome. In this study we assessed the prognostic contribution of several urinary proteins. Urinary total protein, albumin, retinol binding protein (RBP), α-1-microglobulin, IgG and IgM, were measured in banked urine samples from 221 individuals one-year after renal transplantation (age 52 ± 13 years, 55% male, 93 % Caucasian and 82 % living donor). Levels of all proteins measured were higher than in normal non-transplant populations. Patients with glomerular lesions had higher urinary albumin than those with normal histology, while those with Interstitial Fibrosis and Tubular Atrophy plus Inflammation (ci>0, cg=0, i>0) had higher levels of IgG, IgM, α-1-microglobulin and RBP. Concomitant normal levels of urinary albumin, IgM and RBP identified normal histology (specificity 91%, sensitivity 15 %,). Urinary levels of the specific proteins were highly correlated, could not differentiate among the histologic groups, and appeared to result from tubulointerstitial damage. Increased urinary excretion of the low molecular weight protein RBP was a sensitive marker of allografts at risk, predicting long-term graft loss independent of histology and urinary albumin. This study highlights the prognostic importance of tubulointerstitial disease for long-term graft loss.
Keywords: Retinol binding protein, α 1 microglobulin, IgG, IgM, Albumin, Protocol Biopsies, Spot urine, Creatinine ratio, Graft survival
Introduction
Over the past several decades, kidney transplantation has seen a remarkable decrease in acute rejection rates and increased one-year survival (1). The improved one-year allograft survival has not been mirrored by a similar increase long-term (2). Identifying renal allografts at increased risk beyond the first year post transplant is the first step in any attempt to implement a therapeutic strategy. Such markers of risk for long-term graft loss include serum creatinine at one-year (3), renal allograft histology on surveillance (protocol) biopsies (4, 5), and urine protein or albumin excretion (6, 7). Over the past decade, the clinical significance of low level proteinuria has become apparent (8), since low levels of one-year urinary total protein and albumin have both been identified as strong predictors of allograft loss (6, 9, 10). Our group previously reported that 24-hour urine total protein at one-year post transplant provided risk stratification beyond histology and graft function (6). A modest increase in urinary total protein excretion (150 to 500 mg/ day) was associated with a 2.5-fold increased risk of graft loss after adjustment for graft histology and function (6). Total urinary excretion of non-albumin proteins also predicts subsequent graft loss (11). The appearance of specific proteins also appears to have prognostic value. Urinary levels of the low molecular weight protein α-1 microglobulin are increased in renal transplant patients compared to controls, and even higher among those with acute rejection (12). Furthermore, elevated urinary α-1 microglobulin excretion at 6-months post transplant increased the risk for a subsequent decline of allograft function (13). Increased urinary excretion of another low molecular weight protein, RBP also identified allografts at risk for functional decline in the early post transplant period (14). Based upon these studies, we set out to investigate a panel of low and high molecular weight proteins to determine the relationship to allograft histology and the relative contribution for risk stratifying renal allografts at one-year post transplant.
Subjects and Methods
Patient Population
Spot urine samples were collected at protocol post-kidney transplant visits between 2005 and 2008 at the Mayo Clinic. Banked 1-year urine samples were studied from all consented patients who also had a 1-year renal biopsy. Patients on sirolimus were excluded, since this agent is associated with abnormal renal protein handling (15, 16). The Mayo Clinic Institutional Review Board approved this study.
Urine Samples
Urine from a clean catch morning specimen was centrifuged at 2000 revolutions per minute for 6 minutes. Aliquots of 2.5 ml were then stored at −80°C. Samples for this study were removed from the freezer, thawed and processed immediately. The urine creatinine and protein levels were all measured from one aliquot.
Measurement of Urinary Proteins
Urinary total protein (pyrogallol red, Wako Chemicals), albumin (immunoturbidimetric Roche assay), and creatinine (IDMS-traceable Roche enzymatic method) were measured on a Cobas 6000 / 501c analyzer (Roche Diagnostics) in the Mayo Renal Function Laboratory (17). IgG and IgM were measured using a commercially available enzyme linked immunosorbent assay (ELISA) kits from ALPCO (Salem, NH) and Cygnus Technologies, Inc. (Southport, NC), respectively. Urinary α 1-microglobulin and RBP were measured on a Siemens BN II nephelometer using kits from Siemens and The Binding Site, respectively. All urine protein values were corrected for creatinine to adjust for urine concentration.
Established reference ranges in a non-transplant population in our laboratory from healthy volunteer studies are: total urine protein < 50 milligram/gram (mg/g) creatinine; urine albumin < 17 mg/g creatinine in males and < 25 mg/g creatinine in females; urine RBP < 130 microgram/gram (mcg/g) creatinine if < 50 years of age and < 172 mcg/g creatinine if ≥ 50 years of age; and urine α 1-microglobulin < 13 mg/g creatinine if < 50 years of age and < 20 mg/g creatinine if ≥ 50 years of age; IgG ≤ 4.1mg/g creatinine; and IgM ≤ 0.09 mg/g creatinine.
Renal Histology
Biopsies in this cohort were obtained one-year post transplant as part of routine care. Importantly, these were surveillance biopsies and not obtained because of allograft dysfunction or other clinical risk factors. All biopsies were examined by light microscopy and when clinically indicated, immunofluorescence including C4d, electron microscopy and immunohistochemistry for BK virus were performed as previously described (6, 18). Dedicated renal pathologists interpreted biopsies per Banff Schema (19).
As a measure of chronic tubulointerstitial damage we defined a combined chronic score as chronic tubular + chronic interstitial (ct+ci). A combined acute scoreto reflect inflammatory burden, was defined as interstitial + tubular (i +t). In this study we organized the allograft biopsy pathological findings in two ways. The first we termed the histopathologic classification and divided biopsies into five groups: Normal, Interstitial Fibrosis and Tubular Atrophy (IFTA), Glomerular (GN), Inflammation, and Vascular. Normal biopsies were defined as no glomerular lesions and the i, t, ci, and ct scores all zero. IFTA was defined as a ci and/or ct > 0 and with normal glomeruli. GN was defined as any glomerular lesion. Vascular was defined as having extensive chronic vascular lesions or nephrosclerosis reported by the pathologist. These groups were mutually exclusive and as such a patient cannot be in more than one group.
The second classification was termed the histology risk grouping. This scheme was justified by the previous observation that IFTA with inflammation carried an increased risk of graft loss, unlike IFTA alone (4, 5). In this classification IFTA without i was defined as ct > 0 or ci > 0 but i =0, IFTA + i was defined as ct or ci> 0 and i>0, GN was defined as any glomerular lesion, and miscellaneous inflammation was defined as i>0 but ct =0. All groups were mutually exclusive. To assess progression of fibrosis, the difference in combined chronic score from one to two years was used [(2 year ct+ci) − (1 year ct + ci)].
Measurement of Renal Function
Renal function was assessed by an enzymatic, IDMS-traceable serum creatinine assay, eGFR estimated by the four variable MDRD equation (20), and GFR measured by cold iothalamate renal clearance (21).
Statistical Analysis
Differences between proportions were tested by the Chi-square test. Correlations were tested by Spearman’s ρ. Any overall differences in proteinuria by histological groups were assessed by the Kruskall Wallis test. Pairwise comparison of each histological group to normal was assessed by the Mann-Whitney test. End-points for graft survival were all cause graft loss (ACGL) and death censored graft loss (DCGL). The relationship of graft survival to urine proteins and histology was assessed by the Kaplan Meier method and the Log Rank test.
Cox Proportional hazards model were used for adjusted analyses of predictors of graft survival. Urine proteins were entered as both continuous and dichotomized variables. Dichotomization was based on the upper limit of normal from our laboratory. For total protein we used both a normal reference value of < 50mg/g creatinine as well as < 200mg/g creatinine as previously described for the detection of chronic kidney disease (22).
Statistical significance was deemed present when p < 0.05. A Bonferroni correction was made for multiple post hoc tests with the following formula: 0.05/k where k is the number of comparisons performed.
Results
Patient Characteristics
Of the 227 patients with a 1-year post transplant biopsy and bio-banked urine, 6 were excluded because they were receiving sirolimus (known to influence proteinuria), leaving 221 for analysis. The baseline characteristics of this cohort are shown in Table 1. Pre-emptive transplantation, i.e., without prior dialysis, was performed in 97 (43.9%) of patients. For those dialyzed pre-transplant, the mean ± Standard Deviation (SD) duration was 23 ± 34 months. Maintenance immunosuppression was tacrolimus-based in 220 patients and cyclosporine in one. Mean follow-up was 53 ± 10 months.
Table 1.
Baseline Characteristics of the Study Cohort (N = 221)
| Demographics: | |
|---|---|
| Recipient age ± SD years | 51.6 (13.1) |
| Recipient male N (%) | 121 (54.8) |
| Recipient Caucasian N (%) | 206 (93.2) |
| Donor age ± SD years | 44.1 (13.1) |
| Donor male N (%) | 109 (49.3) |
| Live Donor N (%) | 182 (82.4) |
| Preemptive transplant N (%) | 97 (43.9) |
| First Transplant N (%) | 177 (80.1) |
| Follow-up ± SD months | 52.8 (10.4) |
| Renal Function Year 1: | |
| Cr ± SD mg/dL | 1.3 (0.3) |
| eGFR ± SD ml/min/SA | 53.7 (14.9) |
| iGFR ± SD ml/min | 65.7 (20.9) |
| iGFR ± SD ml/min/SA | 57.5 (17.1) |
| Histology at Implantation (n=216) | |
| i >0 N (%) | 0 (0%) |
| t > 0 N (%) | 0 (0%) |
| ci >0 N (%) | 12 (5.5%) |
| ct >0 N (%) | 38 (17.2) |
| Histology at year 1 (n=221) | |
| i >0 N (%) | 29 (13.1) |
| t > 0 N (%) | 22 (9.9) |
| ci >0 N (%) | 97 (43.9) |
| ct >0 N (%) | 117 (52.9) |
| Combined Acute Score ± SD | 0.3 (0.9) |
| Combined Chronic Score ± SD | 1.2 (1.3) |
| Glomerular Pathology N (%) | 33 (14.9) |
Urinary protein levels at One-Year post-transplant
Table 2 depicts individual urinary protein levels at one-year post transplant by histological category. Pathologic proteinuria was common. Albumin was significantly higher in the glomerular disease group (N=33) compared to normal biopsies (N=84). IgM was higher in the inflammation group (N=14), while IgM, IgG, α 1 microglobulin and RBP were significantly higher among IFTA + i cases (N=21). The vast majority (79%) of urine samples contained pathologic levels of total protein (> 50 mg/g; Table 3). Urinary levels of individual low and high MW proteins were also commonly increased (43–77% of samples depending on individual protein) (Table 3), and were significantly correlated with each other (r = 0.3 to 0.8, p<0.001 for all comparisons). When those patients with a histologic glomerular lesion were excluded the correlation coefficients only changed minimally (Data not shown).
Table 2.
| a: Concentration of Urine Proteins in Different Histological Groups at One-Year Post Transplant [median (25%,75%)] | ||||||
|---|---|---|---|---|---|---|
| Protein/Cr (mg/g) | Albumin/Cr (mg/g) | IgG (mg/g) | IgM (mg/g) | α1m (mg/g) | RBP (µg/g) | |
| All Patients (N= 221) | 84.7 (54.3, 164.0) | 16.2 (4.4, 56.8) | 2.5 (0.1,7.6) | 41.4 (9.3, 119.7) | 17 (9.9, 32.5) | 166.7 (91, 587.6) |
| Normal (N= 84) | 75.5 (52.6, 139.4) | 12.0 (0.1, 34.6) | 0.1 (0.1, 6.5) | 37.2 (0.0, 87.7) | 15.2 (6.8, 29.3) | 127.7 (73.1, 412.6) |
| IFTA (N= 79) | 85.7 (59.7, 189.7) | 19.7 (0.1, 189.7) | 3.1 (0.1, 8.5) | 50.3 (7.3, 152.7) | 19.9 (9.9, 31.8) | 198.3 (101.9, 689.9) |
| Inflammation (N= 14) | 142.9 (70.3, 281.1) | 24.9 (11.8, 101.1) | 5.1 (2.3, 34.6)* | 147.3 (86.3, 474.4)# | 39.2 (14.0, 60.1) | 624.4 (112.1, 2239.6) |
| GN (N= 33) | 100.3 (49.3, 355.1) | 24.9 (6.5, 136.1)# | 3.3 (0.1, 11.5) | 36.1 (17.2, 98.6) | 20.6 (3.5, 36.2) | 242.9 (75.8, 1363.4) |
| Vascular (N= 11) | 73.2 (54.9, 111.7) | 8.1 (6.0, 34.3) | 0.1 (0.1, 4.4) | 50.4 (0.0, 33.9) | 14.9 (10.0, 23.2) | 163.0 (80.5, 315.8) |
| Kruskall Wallis | 0.286 | 0.052 | 0.051 | 0.002 | 0.07 | 0.131 |
| b: Concentration of Urine Proteins for Different Histology Risk Groups at One-Year [median (25%, 75%)] | ||||||
| Protein/Cr (mg/g) | Albumin/Cr (mg/g) | IgG (mg/g) | IgM (mg/g) | α1m (mg/g) | RBP (µg/g) | |
| All Patients (N= 216) | 84.5 (54.3, 161.0) | 16.2 (3.6, 57.1) | 2.4 (0.1, 7.5) | 39.4 (7.8, 106.6) | 16.2 (9.7, 30.8) | 165.9 (90.6, 569.7) |
| Normal (N= 90) | 73.2 (52.5, 131.9) | 12.0 (0.1, 34.3) | 0.1 (0.1, 6.5) | 34.0 (0.0, 75.4) | 14.6 (6.4, 26.1) | 127.2 (76.0, 392.7) |
| IFTA (N= 72) | 87.5 (56.5, 188.2) | 18.1 (0.1, 60.9) | 2.9 (0.1, 7.6) | 36.3 (0.0, 116.9) | 19.6 (9.7, 29.8) | 166.8 (94.1, 662.9) |
| IFTA + i (N= 21) | 100.8 (68.1, 235.3)* | 32.3 (6.4, 73.6)* | 5.3 (0.1, 15.5)# | 106.6 (44.1, 214.0)# | 23.0 (13.7, 46.3)# | 256.3 (156.9 992.3)# |
| GN (N= 33) | 100.3 (49.3, 355.1) | 24.9 (6.5, 136.1)# | 3.3 (0.1, 11.5) | 36.1 (17.2, 98.6) | 20.6 (9.5, 36.2) | 242.9 (75.8, 1363.4) |
| Kruskall Wallis | 0.134 | 0.021 | 0.083 | 0.016 | 0.04 | 0.053 |
p < 0.013,
p < 0.05 Mann Whitney post Hoc compared to Normal.
p < 0.017,
p < 0.05 Mann Whitney post Hoc compared to Normal.
IFTA is Interstitial Fibrosis and Tubular Atrophy, GN is Glomerular
Table 3.
Proportion of subjects with abnormal Levels of Urine Proteins at 1-year and Allograft Histology N (%)
| Protein (>50mg/g) |
Protein (>200mg/g) |
Albumin | IgG | IgM | α1m | RBP | |
|---|---|---|---|---|---|---|---|
| Histopathologic Grouping | |||||||
| All Patients (N= 221) | 176 (79) | 44 (20) | 101 (46) | 96 (43) | 170 (77) | 126 (57) | 119 (54) |
| Normal (N= 84) | 67 (80) | 11 (13) | 32 (38) | 32 (38) | 59 (70) | 45 (54) | 39 (46) |
| IFTA (N= 79) | 63 (79) | 16 (20) | 37 (47) | 38 (48) | 61 (77) | 48 (61) | 47 (60) |
| Inflammation (N= 14) | 12 (86) | 6 (43) | 10 (71) | 8 (57) | 14 (100) | 10 (71) | 9 (64) |
| GN (N= 33) | 24 (73) | 10 (30) | 18 (55) | 15 (46) | 29 (88) | 20 (61) | 19 (58) |
| Vascular (N= 11) | 10 (91) | 1 (9) | 4 (36) | 3 (27) | 7 (64) | 3 (27) | 5 (46) |
| Histological Risk Grouping | |||||||
| All Patients (N= 216) | 172 (80) | 41 (19) | 98 (45) | 93 (43) | 165 (76) | 122 (57) | 116 (54) |
| Normal (N= 90) | 72 (80) | 11 (12) | 34 (38) | 33 (37) | 63 (70) | 46 (51) | 41 (46) |
| IFTA (N= 72) | 57 (79) | 14 (19) | 33 (46) | 33 (46) | 53 (74) | 42 (58) | 41 (57) |
| IFTA + i (N= 21) | 19 (91) | 6 (29) | 13 (62) | 12 (57) | 20 (95) | 14 (67) | 15 (71) |
| GN (N= 33) | 9 (27) | 10 (30) | 18 (55) | 15 (46) | 29 (88) | 20 (61) | 19 (58) |
IFTA is Interstitial Fibrosis and Tubular Atrophy, GN is Glomerular
All 101 patients with abnormal urinary albumin also had increased total urine protein (> 50mg/g creatinine). However, among the 120 patients with normal urinary albumin excretion, the majority (n=75; 63%) demonstrated increased total urinary protein excretion including increased levels of IgG (N=29; 39%), IgM (N=29, 39%), α-1 microglobulin (N=44, 59%) and RBP (N=39, 52%).
Graft Histology at One-Year
Eighty-four (38%) of the grafts were histologically normal without glomerular or interstitial pathology (ci and ct scores of 0). Seventy-nine (36%) of the grafts manifested IFTA. Glomerular pathology was present in 33 (15%) of the grafts including transplant glomerulopathy (N=14), IgA (N=6), membranous nephropathy (N=5), FSGS (N=5), mesangial GN (N=2), and membranoproliferative GN (N=1). Inflammation was present in 14 grafts consisting of acute cellular rejection in 8 (6 Borderline changes, one 1A, one1B), antibody mediated rejections in 2, BK nephropathy in 2, and one case each of interstitial nephritis and pyelonephritis. Eleven grafts were grouped as vascular having either significant nephrosclerosis and/or vascular changes including arteriosclerosis, significant arterial hyalinosis or neointimal fibrosis.
Five grafts were not placed in a histological risk category since they did not meet a predefined histological risk pattern. Of the remainder, 90 (42%) were considered normal, 72 (33%) were determined to have IFTA alone, 21 (10%) had IFTA + i, and 33 (15%) had a glomerular lesion (see above). The inflammatory groups had higher levels of IgM, IgG, α 1-microglobulin and RBP, while the GN group had higher levels of albumin (Table 2b). However, significant overlap precluded accurate differentiation between the groups based upon these markers alone. The urinary protein profile correlated significantly with Banff scores (i, t, ci, ct), the combined chronic score, and the combined acute score (Table 4). Furthermore, concomitant normal levels of urinary albumin, IgM and RBP related to normal histology (specificity 95%, sensitivity 16%). Table 5 shows the C statistic, the positive and negative predictive value and sensitivity/specificity of the various urinary proteins and renal histology.
Table 4.
Correlation of Urine Proteins at 1 year with Allograft Function and Histology r (p)
| Protein (mg/g) | Albumin (mg/g) | IgG (mg/g) | IgM (mg/g) | α1m (mg/g) | RBP (µg/g) | |
|---|---|---|---|---|---|---|
| Renal Function Year-1: | ||||||
| Cr mg/dL | 0.148 (0.032) | 0.172 (0.013) | 0.1 (0.149) | −0.013 (0.852) | 0.307 (<0.0001) | 0.253 (<0.0001) |
| eGFR ml/min | −0.117 (0.09) | −0.12 (0.083) | −0.022 (0.755) | −0.029 (0.671) | −0.234 (0.001) | −0.251 (<0.0001) |
| iGFR ml/min | −0.128 (0.069) | −0.117 (0.97) | −0.028 (0.691) | −0.131 (0.062) | −0.186 (0.008) | −0.244 (< 0.0001) |
| iGFR ml/min/1.73m2 | −0.156 (0.027) | −0.178 (0.012) | −0.064 (0.371) | −0.132 (0.062) | −0.272 (< 0.0001) | −0.272 (< 0.0001) |
| Year 1 Histology | ||||||
| i | 0.189 (0.0005) | 0.142 (0.035) | 0.171 (0.011) | 0.279 (< 0.0001) | 0.248 (< 0.0001) | 0.235 (<0.0001) |
| t | 0.207 (0.002) | 0.169 (0.012) | 0.234 (< 0.0001) | 0.267 (<0.0001) | 0.242 (< 0.0001) | 0.231 (<0.001) |
| ci | 0.229 (0.001) | 0.2 (0.003) | 0.184 (0.006) | 0.173 (0.01) | 0.198 (0.003) | 0.23 (<0.001) |
| ct | 0.205 (0.002) | 0.214 (0.001) | 0.168 (0.012) | 0.118 (0.08) | 0.146 (0.03) | 0.169 (0.012) |
| Combined Acute Score | 0.189 (0.005) | 0.147 (0.029) | 0.180 (0.007) | 0.296 (<0.0001) | 0.262 (<0.0001) | 0.243 (<0.0001) |
| Combined Chronic Score | 0.222 (0.001) | 0.214 (0.001) | 0.184 (0.006) | 0.147 (0.029) | 0.173 (0.01) | 0.201 (0.003) |
Cr: Creatinine, eGFR: estimated GFR by the four variable MDRD equation. iGFR: Iothalamate measured GFR by the cold method.
Table 5.
Predictive value for normal histology of the various urinary protein measurements
| ROC C statistic | Positive Predictive Value |
Negative Predictive Value |
Sensitivity | Specificity | |
|---|---|---|---|---|---|
| Total Protein <50m/g | 0.568 | 38% | 62% | 20% | 80% |
| Total Protein <200m/g | 0.560 | 41% | 75% | 66% | 24% |
| Albumin Normal | 0.586 | 43% | 68% | 62% | 50% |
| IgG Normal | 0.569 | 42% | 67% | 62% | 47% |
| IgM Normal | 0.560 | 49% | 65% | 30% | 81% |
| α-1-microglobulin Normal | 0.574 | 41% | 64% | 46% | 59% |
| RBP Normal | 0.584 | 44% | 67% | 54% | 58% |
| All Individual Proteins Normal | 0.517 | 55% | 63% | 7% | 96% |
| IgM, RBP, Albumin Normal | 0.534 | 52% | 64% | 15% | 91% |
Urinary proteins’ relationship to graft function at One-Year
Urinary levels of low molecular weight proteins correlated most strongly with current (one-year) graft function. In this cross sectional cohort there was a strong positive correlation between urinary RBP or α-1 microglobulin and serum creatinine, and a negative correlation of these two low molecular weight proteins with eGFR, corrected measured GFR and uncorrected measured GFR. Urinary albumin and total protein correlated with serum creatinine and corrected measured GFR, but not with eGFR or uncorrected GFR. IgG and IgM had no significant correlations with graft function (Table 4).
Graft Survival
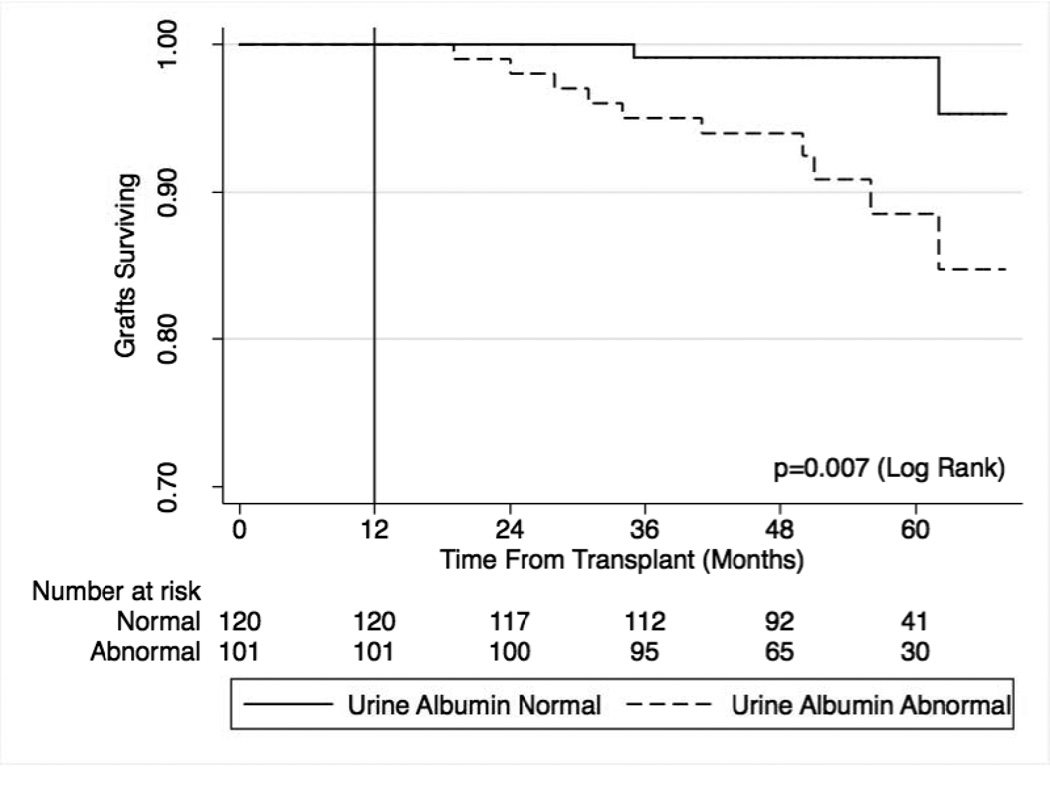
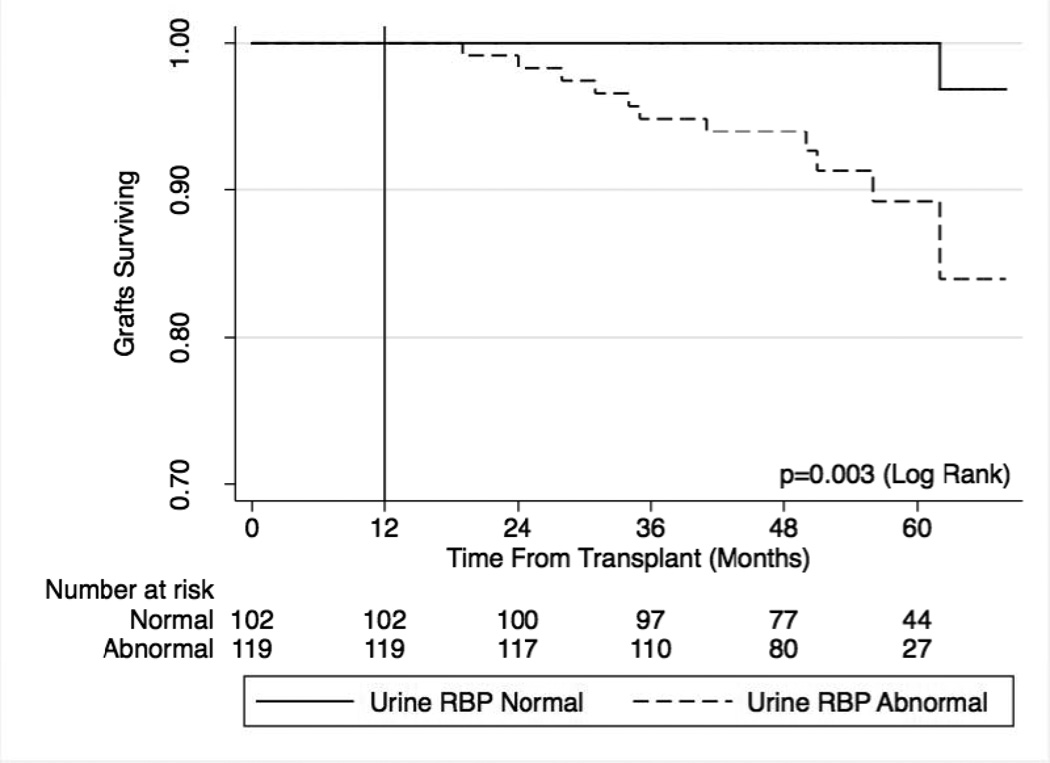
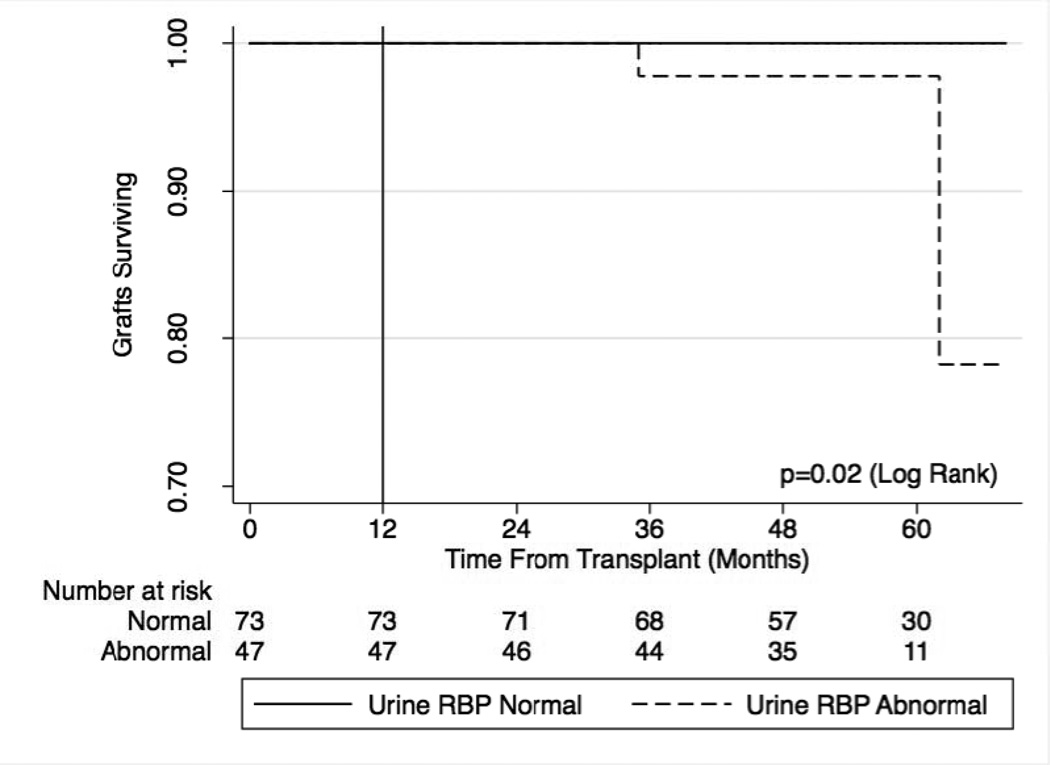
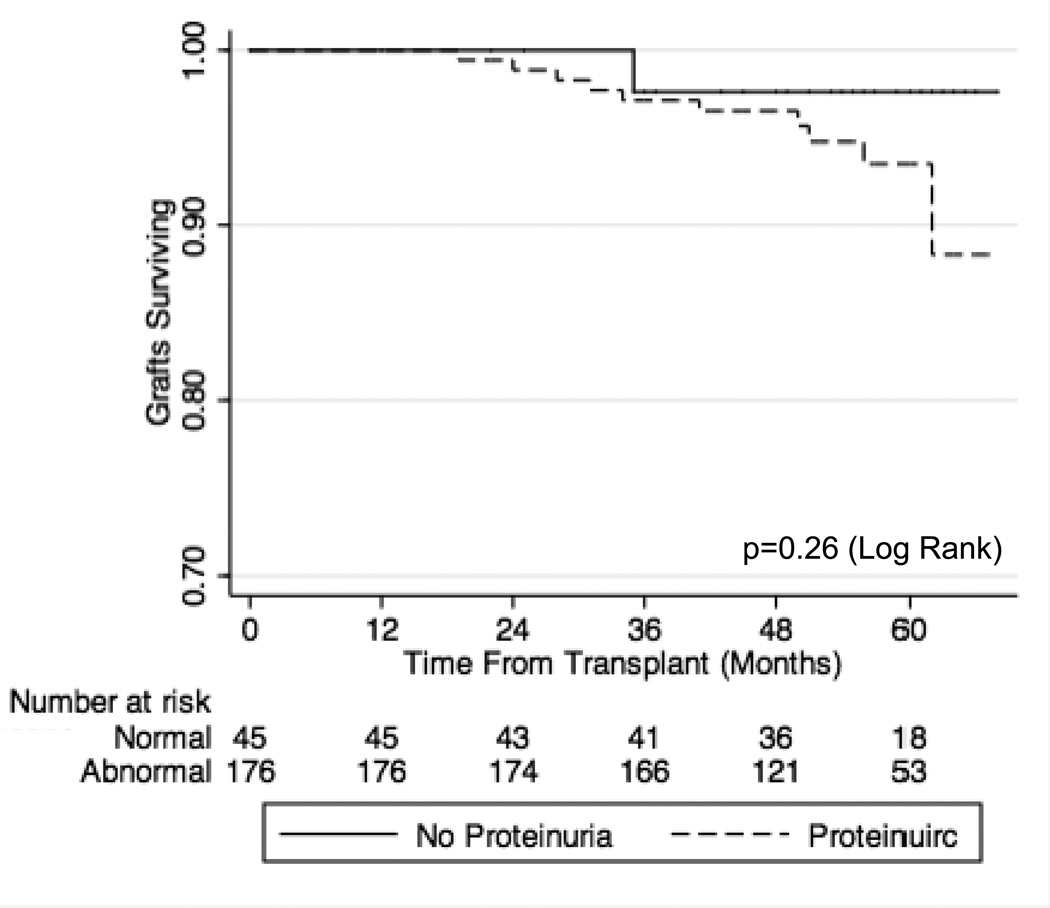
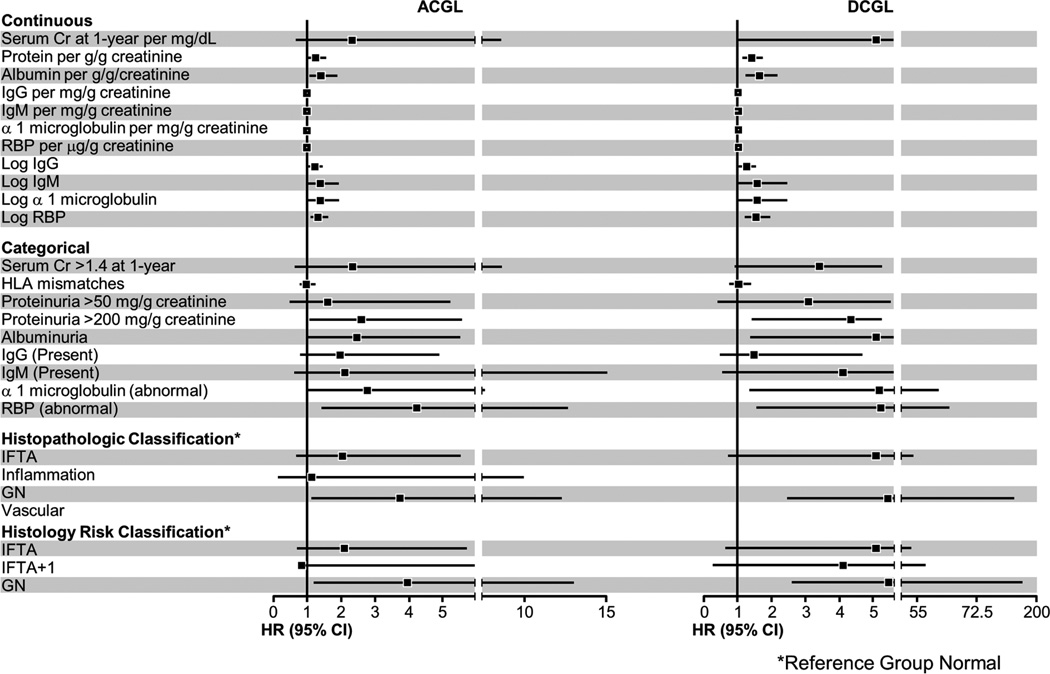
During 52.8 ±10.4 months of follow-up, 21 grafts were lost, 12 of which were not due to patient death. The univariate relationship between urinary protein excretion, histology and graft survival is shown in Table 6. Unadjusted and adjusted values are shown in Table 7. Fig 1 depicts a Kaplan Meier plot of death censored graft survival for patients with normal and abnormal urine albumin, while Fig 2 depicts death censored graft survival for patients with normal and abnormal urine RBP. Increased urinary excretion of either protein predicted worse long-term outcome. Fig 3 compares those with normal and abnormal RBP among the group with normal urinary albumin, demonstrating that increased urinary RBP provides additional independent prognostic information. Fig 4 shows death censored graft survival in patients with normal and abnormal urine total protein. Fig 5 summarizes in graphical form factors affecting graft survival.
Table 6.
Relationship between Urinary Proteins and Graft Histology to Graft Survival
| Variable | All Cause Graft Loss HR [p] Events N=21 |
Death Censored Graft Loss [p] Events N=12 |
|
|---|---|---|---|
| Continuous | |||
| Serum Cr at 1-year per mg/dL | 2.34 [0.204] | 5.06 [0.058] | |
| Protein per g/g creatinine | 1.27 [0.023] | 1.39 [0.002] | |
| Albumin per g/g creatinine | 1.41 [0.016] | 1.62 [0.001] | |
| Log IgG | 1.22 [0.019] | 1.23 [0.075] | |
| Log IgM | 1.39 [0.046] | 1.55 [0.059] | |
| Log α 1 microglobulin | 1.39 [0.046] | 1.55 [0.059] | |
| Log RBP | 1.33 [0.004] | 1.52 [0.001] | |
| Categorical | |||
| Serum Cr > 1.4 at 1-year | 1.36 [0.509] | 3.39 [0.077] | |
| HLA mismatches | 0.99 [0.922] | 1.01 [0.937] | |
| Proteinuria > 50 mg/g creatinine | 1.62 [0.440] | 3.08 [0.282] | |
| Proteinuria > 200 mg/g creatinine | 2.59 [0.034] | 4.31 [0.012] | |
| Albuminuria | 2.47 [0.051] | 6.16 [0.019] | |
| IgG (Abnormal) | 2.30 [0.07] | 2.29 [0.162] | |
| IgM (Abnormal) | 2.04 [0.255] | 4.16 [0.173] | |
| α 1 microglobulin (abnormal) | 2.78 [0.048] | 10.35 [0.026] | |
| RBP (abnormal) | 4.24 [0.01] | 11.98 [0.018] | |
| Histopathologic Classification* | |||
| IFTA | 2.05 [0.199] | 5.89 [0.106] | |
| Inflammation | 1.16 [0.89] | - | |
| GN | 3.73 [0.03] | 20.50 [0.005] | |
| Vascular | - | - | |
| Histologic Risk Classification* | |||
| IFTA | 2.12 [0.188] | 5.46 [0.129] | |
| IFTA+ I | 0.83 [0.866] | 4.08 [0.320] | |
| GN | 3.96 [0.024] | 21.6 [0.005] | |
Reference Group Normal
Cr: Creatinine, IFTA: Interstitial Fibrosis and Tubular Atrophy, GN: Glomerular, eGFR: estimated GFR by the four variable MDRD equation, iGFR: Iothalamate measured GFR by the cold method. HR: Hazard Ratio
Table 7.
Unadjusted and adjusted predictors of graft loss.
| All Cause Graft Loss HR [p] (21 Events) | |
|---|---|
| RBP | |
| Log RBP | 1.33 [0.004] |
| Log RBP adjusted for albumin | 1.30 [0.019] |
| Log RBP adjusted for GN | 1.35 [0.009] |
| Log RBP adjusted for GN and Ablumin | 1.34 [0.028] |
| GN | |
| GN | 3.73 [0.030] |
| GN adjusted for albumin and RBP | 3.01 [0.028] |
| Log α 1 microglobulin | |
| Log α 1 microglobulin unadjusted | 1.39 [0.046] |
| Log α 1 microglobulin adjusted for albumin | 1.32 [0.102] |
|
Death Censored Graft Loss [p] (12 Events) | |
| RBP | |
| Log RBP | 1.52 [0.001] |
| Log RBP adjusted for albumin | 1.41 [0.013] |
| Log RBP adjusted for GN | 1.70 [<0.001] |
GN: Glomerular, RBP: Retinol Binding Protein, HR: Hazard Ratio
Figure 1.
Kaplan Meier plots comparing death censored graft survival between patients with normal (—) and abnormal (----) urine albumin excretion.
Figure 2.
Kaplan Meier plots comparing death censored graft survival between patients with normal (—) and abnormal (----) urinary retinol binding protein (RBP) excretion.
Figure 3.
Kaplan Meier plots comparing death censored graft survival between patients with normal (—) and abnormal (----) urinary retinol binding protein (RBP) excretion in the subset of patients (N=120) with normal urine albumin.
Figure 4.
Kaplan Meier plots comparing death censored graft survival between patients with normal (—) and abnormal (----) urinary total protein. Normal < 50mg/g.
Figure 5.
Hazard Ratio and 95% confidence intervals of the various factors to all cause graft loss (ACGL) and death censored graft loss (DCGL).
Notable in this cohort is, among 25 patients with normal urinary excretion of albumin, IgM and RBP none lost their graft during follow-up.
Discussion
In this study we confirmed that proteinuria is common one year after transplantation, with 79% having > 50 mg/g creatinine and 20% > 200 mg/g creatinine. Urinary levels of the individual proteins albumin, α1-microglobulin, RBP, IgG and IgM were also frequently increased (46–77% of the patients). Pathologic proteinuria was common even in patients with grafts that were deemed to have normal histology, being present in 12–80% depending on protein type. The appropriate threshold for pathologic proteinuria and its prognostic significance remains uncertain among patients with renal allografts (23). Although this study cannot definitively answer this question, the results do suggest that 50mg/g creatinine may be too conservative, since this lower level did not discriminate all cause graft loss or death censored graft loss.
All members of the panel of urinary proteins measured in this study had strong correlations with each other, despite the fact that they range in size from low molecular weight (MW) proteins that are freely filtered (e.g. RBP ~21 kDa), to higher MW proteins that should not be easily filtered (e.g., IgM ~180 kDa for the monomer and ~ 900 kDa for the pentamer). It is of interest, that even when allografts with glomerular lesions were excluded, the level of correlation changed only minimally. This observation, together with the significant correlations between urinary excretion of high and low molecular weight proteins, suggests that disordered tubular protein trafficking may be an important underlying feature. Indeed the low molecular weight urinary proteins RBP and α-1 microglobulin are known to be freely filtered then reabsorbed in the proximal tubule (24, 25). Even though albumin is larger and not as freely filtered by a normal glomerulus, some still passes through and the health of the proximal tubule determines the fraction found in the urine (26, 27). Therefore, small increases in urinary albumin may result from proximal tubular damage, and urinary albumin often increases in parallel with RBP and α-1 microglobulin in states marked by proximal tubular dysfunction.
The correlation of urinary IgG with other smaller molecular weight proteins that we observed is contrary to the findings of Bazzi and colleagues who reported that urinary excretion of IgG correlated with α-1 microglobulin, but not with albumin (28). It is important to note that that study was completed in patients with membranous nephropathy. In those patients with marked glomerular pathology heavy proteinuria composed overwhelmingly of albumin is common, and thus the correlation of urinary albumin with lower molecular weight proteins may be lost. Previous studies demonstrated that urinary excretion of IgM indicates lost glomerular selectivity and the presence of large pores in the glomerular filtration barrier (29). In the renal allograft, however, we postulate that urinary IgM may not just mark glomerular injury and loss of filtration barrier selectivity, but may also result from local production of IgM in the renal interstitium. This locally produced IgM could seep into renal tubules and appear in the urine. Furthermore, processes that stimulate increased interstitial IgM production may also injure tubules, the end result being that urinary IgM correlates with other markers of tubular injury in a transplant population. The finding that urinary IgM and IgG correlated with indicators of interstitial inflammation and injury (Banff i, t, ct, ci, combined acute and chronic scores; Table 6) supports this hypothesis. Furthermore, among allografts with IFTA + i, IgG and IgM levels were significantly higher than among those with normal histology 5.3 (0.1, 15.5) vs. 2.4 (0.1, 7.5) and 106.6 (44.1, 214.0) vs. 39.4 (7.8, 106.6), respectively; p<0.013 for all comparisons. Indeed, all proteins measured correlated with acute and chronic interstitial Banff scores on the one-year biopsy, further implicating a tubular/interstitial cause of the proteinuria.
There was significant variation of urinary albumin, IgG, IgM, α-1 microglobulin and RBP between the histologic categories at 1 year Urinary albumin was higher than normal in the glomerular group 24.9 (6.5, 136.1) vs. 16.2 (4.4, 56.8) mg/g creatinine; p < 0.013 while IgM and IgG were higher in the inflammation group 147.3 (86.3, 474.4) vs. 41.4 (9.3, 119.7); p < 0.013 and 5.1 (2.3, 34.6) vs. 2.5 (0.1,7.6) p <0.05. Urinary IgG, however, did not meet the Bonferroni corrected p < 0.013 threshold for multiple comparisons as a differentiating feature of these 2 groups. Overall, our study suggests that urinary protein profiles alone could not predict histological findings, in agreement with previous observations (6, 30).
During the period of our study 21 grafts were lost, 12 of which were not due to patient death. Despite the modest number of graft losses, we observed a relationship between the measured proteins and graft loss (Tables 6 & 7). This and previous studies (6, 9, 10, 12, 31, 32) demonstrate that urinary proteins relate to graft loss and this is statistically independent of graft histology and function (6). Urinary RBP excretion has previously been correlated with graft survival (14, 32). Our data demonstrate for the first time that urinary RBP excretion at 1-year predicts subsequent graft loss independent of histology and urinary albumin. This is exemplified in that among the 120 patients with normal urinary albumin at one year, no patient with normal urine RBP lost their graft. The only two grafts lost had abnormal RBP. One of these grafts had IgA and the other was deemed to be histologically normal at the one-year point. These grafts were lost at 62 and 35 months post transplant respectively. The IgA developed progressive proliferation and decline in function the other developed recurrent fibrillary glomerulonephritis. These two cases point to RBP being more sensitive and precedes development of albuminuria and histological changes.
Limitations of our study include a predominately Caucasian population, a large proportion of living donor source and pre-emptive transplants. This may limit external validity to other more diverse patient populations with a higher proportion of deceased donor allografts and non-Caucasians. We believe, however, that this is a minor limitation. This more homogenous population may in fact be strength since it limits unknown confounders. Strengths of the study include the cross sectional nature. All the allografts were assessed at the same time point post transplant. The correction of urinary proteins to urine creatinine to overcome variation in urine concentration is an added strength in contrast to previous studies (14, 32). This may explain our ability to observe the strong correlations between RBP and graft interstitial fibrosis and atrophy that was not detected in a previous study (32). Another strength is the relatively large panel of proteins tested in a cohort that is well characterized histologically by protocol biopsies and functionally by iothalamate clearance.
In conclusion, this study demonstrates that increased excretion of urinary proteins of diverse size is extremely common one-year post renal transplant. Furthermore, levels of these proteins correlate highly. This pathological proteinuria appears to be a consequence of tubulo-interstitial damage. Abnormal levels of urinary proteins precede histological changes in some cases. The low molecular weight protein RBP appears to be a sensitive marker of at risk allografts, and provides prognostic information beyond histology or albumin alone. This study also highlights the prognostic importance of tubulointerstitial disease for long-term graft loss.
Acknowledgments
This work was supported by funds from the Division of Nephrology and Hypertension, the William J von Liebig Transplant Center and the Renal Function Laboratory of Mayo Clinic Rochester, MN. The project described was also supported by UL1 TR000135 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The authors would like to thank Mr. Timothy Borland for laboratory support; Dr. Irfan Kundi for sample processing; the transplant coordinators for their dedication and our patients for whom this works is performed.
Abbreviations
- RBP
Retinol Binding Protein
- mcg/g
microgram/gram
- mg/g
milligram/gram
- IFTA
Interstitial Fibrosis and Tubular Atrophy
- GN
Glomerular
- ACGL
All Cause Graft Loss
- DCGL
Death Censored Graft Loss
- SD
Standard Deviation
- MW
Molecular Weight
Footnotes
Part of this work was presented in abstract form at the 2010 American Transplant Congress, San Diego, California and the 2012 International Transplant Congress, Berlin, Germany.
Disclosure:
The authors of this manuscript have no conflicts of interest to disclose as described by the American Journal of Transplantation.
References
- 1.Zand MS. Immunosuppression and immune monitoring after renal transplantation. Semin Dial. 2005;18(6):511–519. doi: 10.1111/j.1525-139X.2005.00098.x. [DOI] [PubMed] [Google Scholar]
- 2.Meier-Kriesche HU, Schold JD, Kaplan B. Long-term renal allograft survival: have we made significant progress or is it time to rethink our analytic and therapeutic strategies? Am J Transplant. 2004;4(8):1289–1295. doi: 10.1111/j.1600-6143.2004.00515.x. [DOI] [PubMed] [Google Scholar]
- 3.Hariharan S, McBride MA, Cherikh WS, Tolleris CB, Bresnahan BA, Johnson CP. Post-transplant renal function in the first year predicts long-term kidney transplant survival. Kidney Int. 2002;62(1):311–318. doi: 10.1046/j.1523-1755.2002.00424.x. [DOI] [PubMed] [Google Scholar]
- 4.Cosio FG, Grande JP, Wadei H, Larson TS, Griffin MD, Stegall MD. Predicting subsequent decline in kidney allograft function from early surveillance biopsies. Am J Transplant. 2005;5(10):2464–2472. doi: 10.1111/j.1600-6143.2005.01050.x. [DOI] [PubMed] [Google Scholar]
- 5.Park WD, Griffin MD, Cornell LD, Cosio FG, Stegall MD. Fibrosis with Inflammation at One Year Predicts Transplant Functional Decline. Journal of the American Society of Nephrology. 2010;21(11):1987–1997. doi: 10.1681/ASN.2010010049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Amer H, Fidler ME, Myslak M, Morales P, Kremers WK, Larson TS, et al. Proteinuria after kidney transplantation, relationship to allograft histology and survival. Am J Transplant. 2007;7(12):2748–2756. doi: 10.1111/j.1600-6143.2007.02006.x. [DOI] [PubMed] [Google Scholar]
- 7.Halimi JM, Buchler M, Al-Najjar A, Laouad I, Chatelet V, Marliere JF, et al. Urinary albumin excretion and the risk of graft loss and death in proteinuric and non-proteinuric renal transplant recipients. American Journal of Transplantation. 2007;7(3):618–625. doi: 10.1111/j.1600-6143.2007.01665.x. [DOI] [PubMed] [Google Scholar]
- 8.Halimi JM, Laouad I, Buchler M, Al-Najjar A, Chatelet V, Houssaini TS, et al. Early low-grade proteinuria: causes, short-term evolution and long-term consequences in renal transplantation. Am J Transplant. 2005;5(9):2281–2288. doi: 10.1111/j.1600-6143.2005.01020.x. [DOI] [PubMed] [Google Scholar]
- 9.Amer H, Cosio FG. Significance and management of proteinuria in kidney transplant recipients. J Am Soc Nephrol. 2009;20(12):2490–2492. doi: 10.1681/ASN.2008091005. [DOI] [PubMed] [Google Scholar]
- 10.Halimi JM, Buchler M, Al-Najjar A, Laouad I, Chatelet V, Marliere JF, et al. Urinary albumin excretion and the risk of graft loss and death in proteinuric and non-proteinuric renal transplant recipients. Am J Transplant. 2007;7(3):618–625. doi: 10.1111/j.1600-6143.2007.01665.x. [DOI] [PubMed] [Google Scholar]
- 11.Halimi JM, Matthias B, Al-Najjar A, Laouad I, Chatelet V, Marliere JF, et al. Respective predictive role of urinary albumin excretion and nonalbumin proteinuria on graft loss and death in renal transplant recipients. Am J Transplant. 2007;7(12):2775–2781. doi: 10.1111/j.1600-6143.2007.02010.x. [DOI] [PubMed] [Google Scholar]
- 12.Teppo AM, Honkanen E, Ahonen J, Gronhagen-Riska C. Changes of urinary alpha1-microglobulin in the assessment of prognosis in renal transplant recipients. Transplantation. 2000;70(8):1154–1159. doi: 10.1097/00007890-200010270-00005. [DOI] [PubMed] [Google Scholar]
- 13.Teppo AM, Honkanen E, Finne P, Tornroth T, Gronhagen-Riska C. Increased urinary excretion of alpha1-microglobulin at 6 months after transplantation is associated with urinary excretion of transforming growth factor-beta1 and indicates poor long-term renal outcome. Transplantation. 2004;78(5):719–724. doi: 10.1097/01.tp.0000131816.51366.6b. [DOI] [PubMed] [Google Scholar]
- 14.Hosaka B, Park SI, Felipe CR, Garcia RG, Machado PG, Pereira AB, et al. Predictive value of urinary retinol binding protein for graft dysfunction after kidney transplantation. Transplant Proc. 2003;35(4):1341–1343. doi: 10.1016/s0041-1345(03)00380-4. [DOI] [PubMed] [Google Scholar]
- 15.Straathof-Galema L, Wetzels JF, Dijkman HB, Steenbergen EJ, Hilbrands LB. Sirolimus-associated heavy proteinuria in a renal transplant recipient: evidence for a tubular mechanism. Am J Transplant. 2006;6(2):429–433. doi: 10.1111/j.1600-6143.2005.01195.x. [DOI] [PubMed] [Google Scholar]
- 16.Letavernier E, Legendre C. mToR inhibitors-induced proteinuria: mechanisms, significance, and management. Transplantation reviews (Orlando, Fla. 2008;22(2):125–130. doi: 10.1016/j.trre.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 17.Watanabe N, Kamei S, Ohkubo A, Yamanaka M, Ohsawa S, Makino K, et al. Urinary protein as measured with a pyrogallol red-molybdate complex, manually and in a Hitachi 726 automated analyzer. Clin Chem. 1986;32(8):1551–1554. [PubMed] [Google Scholar]
- 18.Myslak M, Amer H, Morales P, Fidler ME, Gloor JM, Larson TS, et al. Interpreting post-transplant proteinuria in patients with proteinuria pre-transplant. Am J Transplant. 2006;6(7):1660–1665. doi: 10.1111/j.1600-6143.2006.01361.x. [DOI] [PubMed] [Google Scholar]
- 19.Racusen LC, Solez K, Colvin RB, Bonsib SM, Castro MC, Cavallo T, et al. The Banff 97 working classification of renal allograft pathology. Kidney Int. 1999;55(2):713–723. doi: 10.1046/j.1523-1755.1999.00299.x. [DOI] [PubMed] [Google Scholar]
- 20.Levey AS, Coresh J, Greene T, Stevens LA, Zhang YL, Hendriksen S, et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006;145(4):247–254. doi: 10.7326/0003-4819-145-4-200608150-00004. [DOI] [PubMed] [Google Scholar]
- 21.Wilson DM, Bergert JH, Larson TS, Liedtke RR. GFR determined by nonradiolabeled iothalamate using capillary electrophoresis. Am J Kidney Dis. 1997;30(5):646–652. doi: 10.1016/s0272-6386(97)90488-1. [DOI] [PubMed] [Google Scholar]
- 22.Vassalotti JA, Stevens LA, Levey AS. Testing for Chronic Kidney Disease: A Position Statement From the National Kidney Foundation. American Journal of Kidney Diseases. 2007;50(2):169–180. doi: 10.1053/j.ajkd.2007.06.013. [DOI] [PubMed] [Google Scholar]
- 23.Knoll GA. Proteinuria in kidney transplant recipients: prevalence, prognosis, and evidence-based management. Am J Kidney Dis. 2009;54(6):1131–1144. doi: 10.1053/j.ajkd.2009.06.031. [DOI] [PubMed] [Google Scholar]
- 24.Kirsztajn GM, Nishida SK, Silva MS, Ajzen H, Moura LA, Pereira AB. Urinary retinol-binding protein as a prognostic marker in glomerulopathies. Nephron. 2002;90(4):424–431. doi: 10.1159/000054730. [DOI] [PubMed] [Google Scholar]
- 25.Zhuang HS, Wang QE, Wu F. [Study on the chemiluminescence (CL) analysis for the determination of pyrogallol in water environment] Guang Pu Xue Yu Guang Pu Fen Xi. 2004;24(8):927–929. [PubMed] [Google Scholar]
- 26.Comper WD, Haraldsson B, Deen WM. Resolved: normal glomeruli filter nephrotic levels of albumin. J Am Soc Nephrol. 2008;19(3):427–432. doi: 10.1681/ASN.2007090997. [DOI] [PubMed] [Google Scholar]
- 27.Deen WM, Lazzara MJ. Glomerular filtration of albumin: how small is the sieving coefficient? Kidney Int Suppl. 2004;92:S63–S64. doi: 10.1111/j.1523-1755.2004.09216.x. [DOI] [PubMed] [Google Scholar]
- 28.Bazzi C, Petrini C, Rizza V, Arrigo G, Beltrame A, Pisano L, et al. Urinary excretion of IgG and alpha(1)-microglobulin predicts clinical course better than extent of proteinuria in membranous nephropathy. Am J Kidney Dis. 2001;38(2):240–248. doi: 10.1053/ajkd.2001.26080. [DOI] [PubMed] [Google Scholar]
- 29.Bakoush O, Segelmark M, Torffvit O, Ohlsson S, Tencer J. Urine IgM excretion predicts outcome in ANCA-associated renal vasculitis. Nephrol Dial Transplant. 2006;21(5):1263–1269. doi: 10.1093/ndt/gfk074. [DOI] [PubMed] [Google Scholar]
- 30.Schaub S, Mayr M, Honger G, Bestland J, Steiger J, Regeniter A, et al. Detection of subclinical tubular injury after renal transplantation: comparison of urine protein analysis with allograft histopathology. Transplantation. 2007;84(1):104–112. doi: 10.1097/01.tp.0000268808.39401.e8. [DOI] [PubMed] [Google Scholar]
- 31.First MR, Vaidya PN, Maryniak RK, Weiss MA, Munda R, Fidler JP, et al. Proteinuria following transplantation. Correlation with histopathology and outcome. Transplantation. 1984;38(6):607–612. [PubMed] [Google Scholar]
- 32.de Matos AC, Camara NO, de Oliveira AF, Franco MF, Moura LA, Nishida S, et al. Functional and morphologic evaluation of kidney proximal tubuli and correlation with renal allograft prognosis. Transpl Int. 2010;23(5):493–499. doi: 10.1111/j.1432-2277.2009.01005.x. [DOI] [PubMed] [Google Scholar]