Abstract
Purpose
To evaluate the relation of anisometropia with unilateral amblyopia, interocular acuity difference (IAD) and stereoacuity, among Head Start preschoolers, using both clinical notation and vector notation analyses.
Design
Multicenter, cross-sectional study.
Participants
3- to 5-year-old participants in the Vision In Preschoolers (VIP) Study (N=4040).
Methods
Secondary analysis of VIP data from participants who had comprehensive eye examinations including monocular visual acuity (VA) testing, stereoacuity testing, and cycloplegic refraction. VA was retested with full cycloplegic correction when retest criteria were met. Unilateral amblyopia was defined as IAD ≥2 lines in logarithm of the Minimum Angle of Resolution (logMAR). Anisometropia was defined as ≥0.25 D (diopter) difference in spherical equivalent (SE) or in cylinder power, and also two approaches using power vector notation. The percentage with unilateral amblyopia, mean IAD, and mean stereoacuity were compared between anisometropic and isometropic children.
Main Outcomes Measures
The percentage with unilateral amblyopia, mean IAD, and mean stereoacuity.
Results
Compared with isometropic children, anisometropic children had a higher percentage of unilateral amblyopia (8% vs. 2%), larger mean IAD (0.07 vs. 0.05 logMAR) and worse mean stereoacuity (145 vs.117 arc sec) (all p<0.0001). Larger amounts of anisometropia were associated with higher percentages of unilateral amblyopia, larger IAD, and worse stereoacuity (trend p<0.001). Percentage of unilateral amblyopia was significantly increased with spherical equivalent (SE) anisometropia >0.5 D, cylindrical anisometropia >0.25 D, the vertical/horizontal meridian (J0) or oblique meridian (J45) >0.125 D, or vector dioptric distance (VDD) >0.35 D (all p<0.001). VDD had higher ability in detecting unilateral amblyopia than cylinder, SE, J0 and J45 (p<0.001).
Conclusions
The presence of and amount of anisometropia were associated with the presence of unilateral amblyopia, larger IAD and worse stereoacuity. The threshold level of anisometropia at which unilateral amblyopia becomes significant was lower than current guidelines. VDD is more accurate than spherical equivalent anisometropia or cylindrical anisometropia in identifying preschoolers with unilateral amblyopia.
INTRODUCTION
Amblyopia is one of the leading causes of monocular vision loss in the United States with a prevalence of 1% to 4%.1,2 In addition, unilateral amblyopia puts the patient at increased risk of vision loss throughout life.2,3 Treatment of amblyopia at a young age is highly successful.4 Historically, there has been good agreement among eye care practitioners that detecting and treating amblyopia in early childhood is desirable to prevent permanent loss of vision. The US Preventive Services Task Force recommends screening “to detect amblyopia, strabismus, and defects in visual acuity in children younger than 5 years.” 5 The need for early detection of amblyopia and amblyogenic factors has been a driving force behind preschool vision screening.
Anisometropia is a recognized risk factor for amblyopia.6-10 The population-based Multi-ethnic Pediatric Eye Disease Study 6 found that 54 (78%) of 69 cases of amblyopia were attributed to anisometropia in African American and Hispanic children. The population-based Baltimore Pediatric Eye Disease Study 7 found 6 (32%) of 19 cases of amblyopia were associated with anisometropia in White and African American children. These studies support the hypothesis that screening for high risk refractive error should detect a large proportion of cases of amblyopia. However, because data on the likelihood of amblyopia at any given level of anisometropia are lacking, selecting referral criteria for screening tests of refractive error remains challenging. Also, the amount of anisometropia requiring treatment is based largely on expert clinical opinion and varies among different professional organizations. The American Optometric Association defines anisometropia as a “potentially amblyogenic factor” if the difference in refractive error between eyes exceeds 1.0 D (diopter) of hyperopia, 3.0 D of myopia, or 1.5 D of astigmatism.11 The American Academy of Ophthalmology in the ‘Preferred Practice Pattern’ recommends that anisometropia of the following levels should be treated or monitored to prevent the development of amblyopia: ≥1.5 D of hyperopia, ≥2.0 D of myopia, or ≥2.0 D of astigmatism.12 The American Association for Pediatric Ophthalmology and Strabismus (AAPOS) recommends an inter-ocular difference in sphere or cylinder more than 1.5 D to be considered an amblyogenic factor in preschool vision screening.13
One reason for the differences among the professional organizations on the level of anisometropia considered to be a risk factor for amblyopia, is the scarcity of empirical data comparing the percentages of children with amblyopia among different levels of anisometropia. A few studies have been conducted to illustrate the relation between level of anisometropia and risk or presence of amblyopia.14-17 However, the findings from these studies may not be generalizable to the screening of preschoolers, either because studies were not tailored to the preschool age group or were determined in a selected population. Furthermore, these studies were limited by sample size in that only a small number of subjects were available at certain severity levels of anisometropia to determine the threshold value. They were therefore, not powerful in determining the threshold level of anisometropia associated with an increased prevalence of amblyopia.
The Vision In Preschoolers (VIP) Study was a multi-center, cross-sectional study of 4040 Head Start 3- to 5-year-old children enrolled from five VIP clinical centers across the United States.8-9 All the preschoolers underwent a comprehensive, standardized eye examination by certified eye professionals. The rich dataset from the VIP Study provide an excellent opportunity to examine the relation between anisometropia with the presence and depth of amblyopia in preschoolers, and the relation between anisometropia with interocular acuity difference and stereoacuity. The purpose of this paper is to describe the relation between anisometropia and unilateral amblyopia in 3- to 5-year-old preschoolers, using both traditional measures of anisometropia and two approaches of power vector analyses of refractive error. In addition, we examined the relation between anisometropia with interocular acuity difference and stereoacuity.
METHODS
This is a secondary data analysis of the VIP data from participants of the VIP Study. Details of the VIP Study have been published previously,8-9 and only the details of the comprehensive eye examinations related to this paper are described here.
Comprehensive Eye Examinations
VIP participants were preschool children (3- to 5-year-old) enrolled in Head Start in the five VIP clinical centers (Berkeley, California; Boston, Massachusetts; Columbus, Ohio; Philadelphia, Pennsylvania; Tahlequah, Oklahoma). The local institutional review boards associated with each center approved the study protocol and informed consent documents. All Head Start children who failed their local Head Start screening and a random sample of those who did not fail the local Head Start screening were targeted for enrollment into the VIP Study. The enrolled children underwent a comprehensive, standardized eye examination performed by study-certified optometrists and ophthalmologists who were experienced in providing care to children. The comprehensive examination incorporated monocular threshold VA testing, cover testing, and cycloplegic refraction to determine whether a child had amblyopia or reduced VA, strabismus, or significant refractive error. Anterior segment evaluation and dilated fundus examination were also performed to detect possible causes of reduced VA.
Monocular threshold VA testing was conducted with crowded, single H, O, T and V optotypes using the Electronic Vision Assessment (EVA) system at 10 ft, according to the protocol established by the Amblyopia Treatment Study.18 Children who wore spectacles were tested while wearing their spectacles. Both eyes of a child were retested with full cycloplegic correction if: (1) VA <20/50 for 3-year-old, VA <20/40 for 4- to 5-year-old, or an IAD ≥2 lines; AND (2) hyperopia ≥2.0 D, or myopia ≥0.5 D, or astigmatism ≥1.0 D was present in either eye. About 17% of children in VIP Phase I and 20% of children in VIP Phase II required a VA retest.
The final visual acuity score of an eye was based on the re-test for eyes that were retested, and based on the initial test for eyes that were not re-tested.
Both a cover-uncover test and an alternating cover test were performed at distance (10 ft) and near (16 inches) to evaluate ocular alignment. Cycloplegic retinoscopy was performed 30 to 40 minutes after instillation of cycloplegic drops. Retinoscopy was performed with the child wearing retinoscopy spectacles corresponding to the examiner’s working distance, while the child watched a children’s video presented at 10 ft.
In VIP Phase I-year 1, stereoacuity was tested using the Random Dot E test at 50, 100 and 150 cm corresponding to 502, 252, and 168 arc sec disparity. In VIP Phase 1-year 2 and Phase II, stereoacuity was tested at 40cm using the Stereo Smile Test with six smile stereoacuity cards including card A (demo), card B (480 sec arc), card C (240 sec arc), card D (120 sec arc), card E (60 sec arc) and a blank card (random dot pattern without disparity).
The research followed the tenets of the Declaration of Helsinki and was approved by the institutional review board of each clinical center. Written informed consent was obtained from parents prior to examination of each child.
Amblyopia Determination
We defined unilateral amblyopia solely based on the interocular difference in final VA without regard to the presence or absence of amblyogenic factors. We defined unilateral amblyopia as ≥2 lines difference in logarithm of the Minimum Angle of Resolution (logMAR) of the best-corrected interocular VA. Because the VIP study protocol did not specify retesting a child with best correction when the IAD was <2 lines and VA in each eye was in the normal range for the child’s age, these children were classified as non-amblyopic under the assumption that the IAD would remain <2 lines upon retesting. Children with IAD ≥ 2 lines who were not re-tested with correction (because their small amount of refractive error did not meet re-test criteria as defined above) were excluded from analysis, because it is unknown whether re-testing with correction would have resulted in a smaller IAD.
Anisometropia Definition
Anisometropia was classified by both the traditional clinical notation using spherical equivalent (SE) and cylinder power, and power vector notations using methods by Thibos and by Harris.21-22 SE is calculated as the sphere power plus half the cylinder power (preserving sign of the cylinder power). Using clinical notation, anisometropia was defined as an interocular difference ≥0.25 D in SE for spherical equivalent anisometropia and as an interocular difference ≥0.25 D in cylinder for cylindrical anisometropia. Hyperopic anisometropia was defined as a SE ≥ +0.25 D in each eye, and an interocular difference ≥0.25 D in SE. Myopic anisometropia was defined SE ≥ 0.25 D in each eye, and an interocular difference ≥0.25 D in SE. If a child met the definitions of more than one type of anisometropia, we assumed that the type of anisometropia that was inducing the amblyopia was the type with the larger magnitude. Therefore, a child was classified into the one anisometropia group corresponding to the largest interocular difference.
The above definitions of anisometropia used only sphere and cylinder and did not consider axis. To take the axis into consideration, we also defined anisometropia using the power vector notation of Thibos et al 19 and of Harris 20. Using the Thibos method, we first converted the clinical notation of refractive error (S, C X β, where S is sphere, C is cylinder, and β is axis) into the rectangular Fourier form [M, J0, J45]. Here M is the sphere equivalent with M=SE, J0 represents power at axis 0°/180° with J0=(-C/2)cos2β, and J45 represents power at 45°/135° with J45=(-C/2)sin2β. We calculated the interocular difference for each of J0 and J45 and determined the amount of anisometropia based on the larger interocular difference of J0 and J45. Using the Harris method,20 we calculated the vector dioptric distance (VDD) between two eyes as VDD=sqrt(2) x sqrt[(M0-M1)2 + (J00-J01)2 +(J450-J451) 2], where the subscript 0 represents left eye, and 1 represents right eye. VDD provides a full description of the difference in refractive error between the two eyes. For both types of vector notation analyses, a group of children without anisometropia (control group), similar to the isometropic group in the clinical notation analyses, was defined. Groups of children with different severities of anisometropia were then compared to a control group. For vector notation of both Thibos and Harris, subjects in the control group had zero interocular difference of M, J0 and J45 (i.e., with zero of VDD). Because analyses of M anisometropia was equivalent to the analyses of SE anisometropia presented in the clinical notation analyses and because J0/J45 analyses was included to focus on the cylinder and axis components of anisometropia, data from children with large SE anisometropia (SE ≥ 1.00 D) were excluded from the vector analysis of Thibos et al,19 the same analysis approach as that taken by Dobson et al. 17
Statistical Analysis
Visual acuity and stereoacuity results were transformed to logarithmic values for all statistical analyses. For analysis of stereoacuity data, we restricted our analysis to the stereoacuity measured using Stereo Smile test, as Stereo Smile test has more disparity levels and provide better measure of stereoacuity than Random Dot E test, as small stereoacuity deficits may not be detected by Random Dot E test. For preschoolers (6.0%) who were not able to resolve the largest disparity level (480 arc sec) of Stereo Smile test, a value of 1600 arc sec was assigned on the stereoacuity test, by following the same approach used by other investigators.17,21 Additional sensitivity analyses were also performed by assigning 1000 arc sec and 10000 arc sec to children who could not resolve the largest disparity level.21
To evaluate whether the presence of anisometropia was associated with presence of unilateral amblyopia, larger IAD, and worse stereoacuity, the chi-square test was used for comparing the percentage of unilateral amblyopia, and the two group t-test was used for comparing the mean IAD and stereoacuity between the anisometropia and isometropia groups.
To evaluate whether larger amounts of anisometropia were associated with an increased prevalence of unilateral amblyopia, we categorized children into several severity levels of anisometropia and performed a test of trend in proportions. If the trend test showed a statistically significant association, we then determined the threshold level of anisometropia that is associated with presence of unilateral amblyopia by comparing the percentage of unilateral amblyopia between each severity level of anisometropia with that of the isometropic group. We summarized the association of anisometropia with amblyopia using odds ratios (ORs) and their 95% confidence interval (95% CI), calculated from logistic regression models. To test whether the relation of anisometropia with unilateral amblyopia differs by age, a test of interaction between anisometropia and age was performed, followed by a stratified analysis by age if the interaction was found to be statistically significant.
To evaluate the ability of the different measures of anisometropia (clinical notation, power vector notations) in detecting unilateral amblyopia, we performed the analysis of Receiver Operating Characteristic (ROC) by calculating the area under the ROC curve (AUC) and compared AUC between pairs of different measures.22
To evaluate whether the larger amounts of anisometropia were associated with increased IAD and stereoacuity, we performed a test of trend using analysis of variance. If test of trend is statistically significant, we proceeded with post-hoc comparisons between each severity level of anisometopia as compared to the isometropic group to determine the threshold level associated with increased IAD and worse stereoacuity. For these comparisons, we used the Hochberg procedure 23 (a less conservative, more powerful procedure than Bonferroni method) to adjust the p-values for multiple comparisons and to control the overall type I error of 0.05 (two-sided). All the statistical analyses were performed in SAS v9.2 (SAS Institute Inc, Cary, NC).
RESULTS
Study Subjects
A total of 4040 preschoolers were enrolled into VIP Phases 1 and 2. 160 (4.0%) subjects were excluded due to having an IAD of ≥2 lines but not re-tested because their refractive error did not meet re-test criteria, 146 (3.6%) subjects were excluded due to the presence of strabismus, and 6 (0.2%) were excluded due to missing visual acuity or refractive error data. The remaining 3728 (92.3%) subjects constitute the population used in the analysis for this paper. Unilateral amblyopia as defined in the methods was observed in 217 (5.8%) children.
Anisometropia Measured with Clinical Notation and Unilateral Amblyopia
Among the 3728 children, 1163 (31.2%) children were isometropic (ISO), 1214 (32.6%) had SE anisometropia (≥0.25 D in SE), 1284 (34.4%) had cylindrical anisometropia (≥0.25 D in cylinder), and 67 children had the same amount of SE anisometropia and cylindrical anisometropia. This latter group of children was classified as having neither spherical nor cylindrical anisometropia and were excluded for the primary analysis of SE anisometropia or cylindrical anisometropia. Among the 1214 children with SE anisometropia, 1113 children had hyperopic anisometropia, 49 children had myopic anisometropia, and 52 children had antimetropia. Compared to the isometropic children, those with anisometropia had a significantly higher percentage of unilateral amblyopia (7.5% vs. 2.2%, p<0.001) with an odds ratio (OR) of 3.7 (95% CI: 2.4 – 5.6).
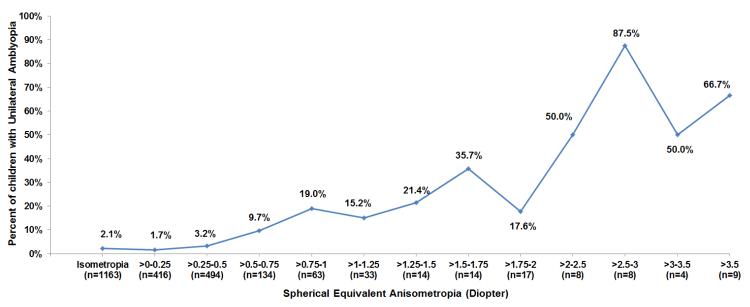
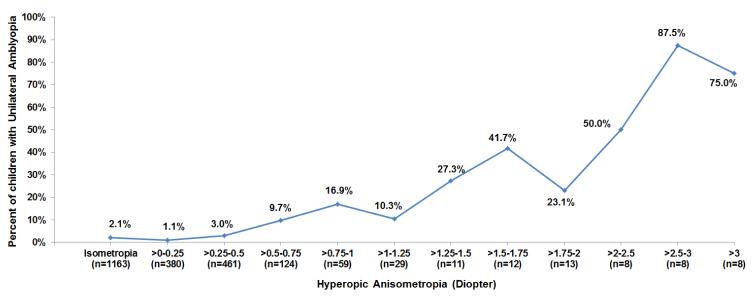
SE anisometropia was significantly associated with unilateral amblyopia (OR=3.3, 95% CI=2.1 – 5.3; Table 1). The presence of unilateral amblyopia significantly increased when SE anisometropia was >0.50 D in SE (OR=4.9, 95% CI=2.4 – 9.8). The presence of unilateral amblyopia increased with increasing amounts of SE anisometropia (trend p<0.001, Figure 1A, available at http://aaojournal.org). Among the 83 children with both SE anisometropia and unilateral amblyopia, the amount of SE anisometropia was significantly correlated with greater interocular acuity difference (Spearman correlation = 0.42, p<0.0001). Compared to the isometropic group, the OR for the presence of unilateral amblyopia ranged from 4.9 for SE anisometropia >0.5 to 0.75 D, to 42 for SE anisometropia >1.75 D. Similar relations held when only the 1113 children with hyperopic anisometropia were considered (Table 1, Figure 1B, available at http://aaojournal.org).
Table 1.
Association of spherical equivalent anisometropia, hyperopic anisometropia and myopic anisometropia with unilateral amblyopia
| Interocular difference in spherical equivalent (Diopter) |
N | Unilateral Amblyopia n (%) |
Odds Ratio (95% CI)* |
|---|---|---|---|
| Isometropia | 1163 | 25 (2.15%) | 1.00 |
| Spherical equivalent anisometropia | |||
| Any | 1214 | 83 (6.48%) | 3.34 (2.12, 5.26) |
| =0.25 | 416 | 7 (1.68%) | 0.78 (0.34,1.82) |
| >0.25 - 0.5 (Mean=0.46) | 494 | 16 (3.24%) | 1.52 (0.81, 2.88) |
| >0.5 – 0.75 (Mean=0.71) | 134 | 13 (9.70%) | 4.89 (2.44, 9.81) |
| >0.75 – 1.75 (Mean=1.16) | 124 | 25 (20.2%) | 11.5 (6.37, 20.8) |
| >1.75 – 12.3 (Mean=3.07) | 46 | 22 (47.8%) | 41.7 (20.7, 84.1) |
| Hyperopic anisometropia | |||
| Any | 1113 | 71 (6.38%) | 3.10 (1.95, 4.93) |
| =0.25 | 380 | 4 (1.05%) | 0.48 (0.17, 1.40) |
| >0.25 - 0.5 (Mean=0.46) | 461 | 14 (3.04%) | 1.43 (0.73, 2.77) |
| >0.5 – 0.75 (Mean=0.70) | 124 | 12 (9.68%) | 4.88 (2.39, 9.97) |
| >0.75 – 1.75 (Mean=1.15) | 111 | 21 (18.9%) | 10.6 (5.72, 19.7) |
| >1.75 – 5.25 (Mean=2.68) | 37 | 20 (54.1%) | 53.6 (25.1, 114) |
| Myopic anisometropia | |||
| Any | 49 | 9 (18.4%) | 10.2 (4.49, 23.4) |
| =0.25 | 14 | 1 (7.14%) | 3.50 (0.44, 27.8) |
| >0.25 – 1.0 (Mean=0.63) | 24 | 4 (16.7%) | 9.10 (2.90, 28.6) |
| >1.0 – 12.3 (Mean=3.91) | 11 | 4 (36.4%) | 26.0 (7.15, 94.6) |
CI = Confidence Interval.
Compared with isometropic group.
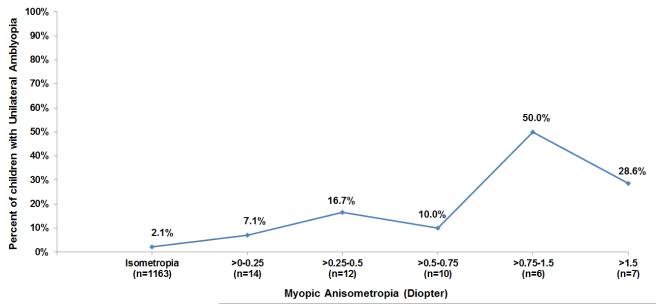
Figure 1.
Percent of children with unilateral amblyopia by levels of spherical equivalent anisometropia (Figure 1A), hyperopic anisometropia (Figure 1B), and myopic anisometropia (Figure 1C).
Although relatively uncommon, myopic anisometropia was strongly associated with amblyopia (OR=10, 95% CI=4.5-23; Table 1). The presence of unilateral amblyopia was statistically significantly increased when myopic anisometropia was >0.25 D. Compared with the ISO group, the odds ratio was 9.1 for myopic anisometropia of >0.25 to 1.0 D and was 26 for myopic anisometropia >1.0 D (p-values 0.002 and <0.001, respectively).
Cylindrical anisometropia was significantly associated with unilateral amblyopia (OR=3.8, 95% CI=2.4-5.9; Table 2). The presence of unilateral amblyopia was statistically significantly increased when cylindrical anisometropia was greater than 0.25 D (OR=2.8, 95% CI=1.6 – 4.8). The presence of unilateral amblyopia increased with increased amounts of cylindrical anisometropia (trend p<0.001). Among the 98 children with both cylindrical anisometropia and unilateral amblyopia, the amount of cylindrical anisometropia was significantly correlated with greater interocuar acuity difference (Spearman correlation = 0.31, p=0.002). Compared to the ISO group, the OR of unilateral amblyopia ranged from 2.8 for cylindrical anisometropia >0.25 to 0.5 D to 23.8 for cylindrical anisometropia >1.5 D (all p-values <0.001).
Table 2.
Association of cylindrical anisometropia with unilateral amblyopia
| Interocular difference in cylinder (Diopter) |
N (N=2447) |
Unilateral Amblyopia (N=123) n (%) |
Odds Ratio (95% CI)* |
|---|---|---|---|
| Isometropia | 1163 | 25 (2.15%) | 1.00 |
|
Any cylindrical
anisometropia |
1284 | 98 (7.63%) | 3.76 (2.41, 5.88) |
| =0.25 | 486 | 15 (3.09%) | 1.45 (0.76, 2.77) |
| >0.25 - 0.5 (Mean=0.50) | 473 | 27 (5.71%) | 2.76 (1.58, 4.80) |
| >0.5 – 1.00 (Mean=0.86) | 218 | 23 (10.6%) | 5.37 (2.99, 9.65) |
| >1.00 – 1.50 (Mean=1.38) | 72 | 21 (29.2%) | 10.7 (9.84, 35.7) |
| >1.50 – 8.50 (Mean=2.37) | 35 | 12 (34.3%) | 23.8 (10.6, 53.0) |
CI= Confidence Interval.
Compared with isometropic group.
Anisometropia Measured with Vector Analysis and Unilateral Amblyopia
When anisometropia was measured with the vector components of Thibos, 21 increased amounts of anisometropia (based on the larger value of J0/J45) were significantly associated with an increased percentage of unilateral amblyopia (trend p<0.001, Table 3, available at http://aaojournal.org). The presence of unilateral amblyopia was statistically significantly increased when the interocular difference in J0/J45 was >0.125 D. Compared to the group of children with zero interocular difference in J0/J45, the OR of unilateral amblyopia ranged from 3.1 for J0/J45 >0.125 D to 0.25 D, to 15.5 for J0/J45 >1.0 D. Similar relations with unilateral amblyopia held for J0 (power at axis 0°/180°) alone and J45 (power at axis 45°/135°) alone (data not shown).
Table 3.
Association of interocular difference in J0/J45 (whichever is greater) with unilateral amblyopia
| Interocular Difference in J0/J45 (Diopter) |
N§ | Unilateral Amblyopia n (%) |
Odds Ratio (95% CI)* |
|---|---|---|---|
| Control group † | 1062 | 20 (1.88%) | |
| >0 – 0.125 (Mean=0.12) | 601 | 17 (2.83%) | 1.52 (0.79, 2.92) |
| >0.125 – 0.25 (Mean=0.23) | 624 | 35 (5.61%) | 3.10 (1.77, 5.41) |
| >0.25 – 0.50 (Mean=0.40) | 338 | 23 (6.80%) | 3.80 (2.06, 7.02) |
| >0.50 – 0.75 (Mean=0.65) | 123 | 22 (17.9%) | 11.4 (5.99, 21.5) |
| >0.75 – 1.00 (Mean=0.87) | 66 | 14 (21.2%) | 14.0 (6.71, 29.3) |
| >1.00 – 2.91 (Mean=1.55) | 61 | 14 (23.0%) | 15.5 (7.38, 32.6) |
CI = Confidence Interval.
Defined as zero interocular differences of M, J0 and J45.
Compared with control group.
Children who had spherical equivalent difference ≥1.0 diopter were excluded from this analysis.
When anisometropia was measured with VDD, increased amounts of VDD were significantly associated with increased presence of unilateral amblyopia (trend p<0.001, Table 4). The presence of unilateral amblyopia was statistically significantly increased when VDD was >0.35 D. Compared to the group with zero VDD, the OR of unilateral amblyopia ranged from 2.4 for VDD >0.35 to 0.6 D, to 99 for VDD >4.0 D.
Table 4.
Association of vector dioptric distance with unilateral amblyopia
| VDD (Diopter) | N | Unilateral Amblyopia n (%) |
Odds Ratio (95% CI)* |
|---|---|---|---|
| Control Group † | 1062 | 20 (1.88%) | 1.00 |
| >0 - 0.35 (Mean=0.30) | 844 | 18 (2.13%) | 1.14 (0.60, 2.16) |
| >0.35 - 0.6 (Mean=0.51) | 625 | 27 (4.32%) | 2.35 (1.31, 4.23) |
| >0.6 - 0.8 (Mean=0.72) | 493 | 24 (4.87%) | 2.67 (1.46, 4.87) |
| >0.8 – 1.2 (Mean=1.02) | 323 | 32 (9.91%) | 5.73 (3.23, 10.2) |
| >1.2 – 2 (Mean=1.50) | 249 | 48 (19.3%) | 12.4 (7.23, 21.4) |
| >2 – 4 (Mean=2.64) | 103 | 29 (28.2%) | 20.4 (11.0, 37.8) |
| >4 – 17.3 (Mean=7.08) | 29 | 19 (65.5%) | 99.0 (40.9, 240) |
CI = Confidence Interval; VDD = Vector Dioptric Distance.
Defined as zero interocular differences of M, J0 and J45.
Compared with isometropic group.
Comparison on Measures of Anisometropia for Identifying Unilateral Amblyopia
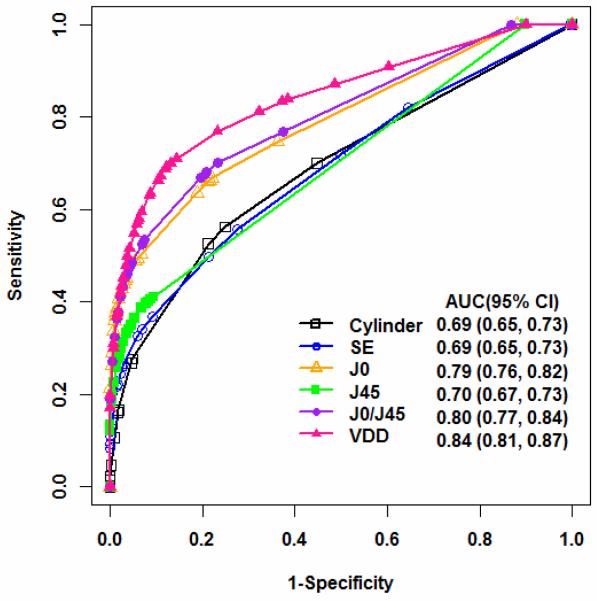
Using ROC analysis (Figure 2), the VDD has an AUC of 0.84 in detecting unilateral amblyopia. This is significantly better than the traditional clinical notation of anisometropia using SE (AUC=0.69) or cylinder power (AUC=0.69). It is also better than the Thibos notation of anisometropia using J0 (AUC=0.79), J45 (AUC=0.70), or larger value of J0/J45 (AUC=0.80). Using VDD >=0.75 D for defining positive unilateral amblyopia leads to a sensitivity of 0.64 and specificity of 0.81.
Figure 2.
Receiver Operating Characteristic (ROC) curves and area under ROC curve (AUC) for detecting unilateral amblyopia using interocular difference of spherical equivalent, cylinder, J0, J45, the larger inter-ocular difference of J0 and J45 (J0/J45), and vector dioptric distance (VDD). The AUC from VDD is significantly higher than that from using other measures of anisometropia (p<0.001). ROC = Receiver Operating Characteristic; AUC = area under ROC curve; VDD = vector dioptric distance; CI= confidence interval.
Age Effect on the Association between Anisometropia and Unilateral Amblyopia
The association of the amount of cylindrical anisometropia with unilateral amblyopia differs between 3-year-old preschoolers and 4- to 5-year-old preschoolers (p<0.0001 for test of interaction). When stratifying the analysis by age group, we found the percentage of amblyopia in 3-year-olds was more than twice as large as in 4- to 5-year-olds when cylindrical anisometropia was >0.25 to 1.0 D (Table 5, available at http://aaojournal.org). However, the percentages were nearly equal in the two age groups when cylindrical anisometropia was >1.0 D in two age groups. For all other types of anisometropia, the relation with amblyopia did not differ by age (p ≥0.25 for all tests of interaction).
Table 5.
The association between cylindrical anisometropia and unilateral amblyopia by age of children
| 3-Year-Old (N=772) | 4- to 5-Year-old(N= 1919) | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Interocular difference in cylinder |
N | Mean interocular difference in cylinder |
Unilateral Amblyopia n (%) |
Odds Ratio (95% CI)* |
N | Mean interocular difference in cylinder |
Unilateral Amblyopia n (%) |
Odds Ratio (95% CI)* |
| Isometropia | 261 | 0 | 7 (2.68%) | 1.00 | 902 | 0 | 18 (2.00%) | 1.00 |
|
| ||||||||
|
Cylindrical
anisometropia |
267 | 0.55 | 28 (10.5%) | 4.25 (1.82, 9.92) | 1017 | 0.57 | 70 (6.88%) | 3.63 (2.15, 6.14) |
| =0.25 | 105 | 0.25 | 3 (2.86%) | 1.07 (0.27, 4.21) | 381 | 0.25 | 12 (3.15%) | 1.60 (0.76, 3.35) |
| >0.25 - 0.5 | 98 | 0.5 | 10 (10.2%) | 4.12 (1.52, 11.2) | 375 | 0.5 | 17 (4.53%) | 2.33 (1.19, 4.58) |
| >0.5 – 1.00 | 45 | 0.88 | 9 (20.0%) | 9.07 (3.18, 25.9) | 173 | 0.86 | 14 (8.09%) | 4.32 (2.11, 8.87) |
| >1.00 – 8.5 | 19 | 1.70 | 6(31.6%) | 16.8 (4.92, 57.0) | 88 | 1.71 | 27 (30.7%) | 21.7 (11.4, 41.7) |
CI= Confidence Interval.
Compared with the isometropic group.
Anisometropia with IAD
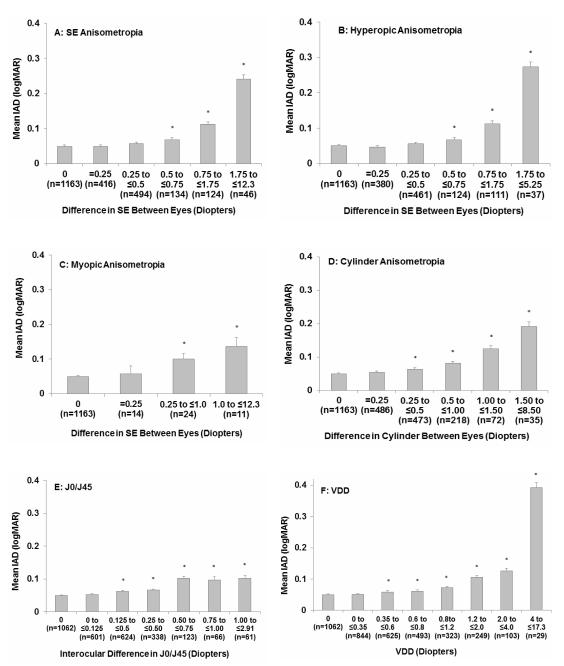
The mean IAD in the anisometropic children was significantly larger than isometropic children (0.07 vs. 0.05 logMAR, p<0.001). The mean IAD as a function of amount of anisometropia are shown for SE anisometropia (Figure 3A), hyperopic anisometropia (Figure 3B), myopic anisometropia (Figure 3C), and cylindrical anisometropia (Figure 3D). A significant increase in IAD occurred when SE anisometropia of >0.5 D, hyperopic anisometropia >0.5 D, myopic anisometropia >0.25 D, or cylindrical anisometropia >0.25 D were present. For each type of anisometropia, a larger amount of anisometropia was associated with a larger mean IAD, demonstrating clear a dose-response relationship (all trend p-values <0.001). Using the vector notation, interocular difference of J0/J45 >0.125 D (Figure 3E) or VDD >0.35 D (Figure 3F) was associated with significantly larger IAD (p<0.001).
Figure 3.
The mean interocular acuity difference in logarithm of the Minimum Angle of Resolution (logMAR) for each severity levels of spherical equivalent anisometropia (Figure 3A), hyperopic anisometropia (Figure 3B), myopic anisometropia (Figure 3C), cylindrical anisometropia (Figure 3D), J0/J45 (Figure 3E), and vector dioptric distance (VDD) (Figure 3F), as compared with the isometropic group. * indicated that mean interocular acuity difference in this anisometropia severity level was significantly different from the isometropic group (multiple comparison adjusted p<0.05 using Hochberg procedure). Bar,1 standard error. IAD = interocular acuity difference; SE= spherical equivalent; logMAR = logarithm of the Minimum Angle of Resolution; VDD = vector dioptric distance.
Anisometropia with Stereoacuity
Using the traditional clinical notation for anisometropia, the mean stereoacuity in the anisometropic children was significantly worse than that of the isometropic children (119 vs.94 arc sec, p<0.001). Larger amounts of anisometropia were associated with worse stereoacuity for each type of anisometropia, in a clear dose-response manner (Figure 4). The stereoacuity was significantly decreased when SE anisometropia was >0.5 D (Figure 4A), hyperopic anisometropia was >0.5 D (Figure 4B), myopic anisometropia was >0.25 D (Figure 4C) or cylindrical anisometropia was >0.5 D (Figure 4D). Using vector notation for anisometropia, the stereoacuity was statistically significantly decreased when the interocular difference of J0/J45 was >0.25 D (Figure 4E) or when VDD was >0.6 D (Figure 4F). The above results were based on assigning a value of 1600 arc sec stereoacuity to those (6.0% preschooler) who could not resolve the largest stereoacuity disparity level (480 arc sec) of Stereo Smile test. The sensitivity analyses, by assigning either 1000 arc sec or 10000 arc sec to these children, showed similar results (data not shown).
Figure 4.
The mean stereoacuity from stereo smile test for each severity levels of spherical equivalent anisometropia (Figure 4A), hyperopic anisometropia (Figure 4B), myopic anisometropia (Figure 4C), cylindrical anisometropia (Figure 3D), J0/J45 (Figure 4E), and vector dioptric distance (VDD) (Figure 4F), as compared with the isometropic group. * indicated that mean stereoacuity in this anisometropia severity level was significantly different from the isometropic group (multiple comparison adjusted p<0.05 from Hochberg procedure). Bar,1 standard error. SE = spherical equivalent; VDD = vector dioptric distance.
DISCUSSION
Using both traditional clinical notation and power vector notation as measures of anisometropia, we found that the presence of and the amount of anisometropia were significantly associated with presence of unilateral amblyopia, larger IAD and worse stereoacuity. The presence of unilateral amblyopia among preschoolers was increased when anisometropia exceeded the following criteria: SE anisometropia or hyperopic anisometropia >0.5 D, myopic anisometropia >0.25 D, cylindrical anisometropia >0.25 D, J0/J45 >0.125 D or VDD >0.6 D.
Data on the level of anisometropia sufficient to induce unilateral amblyopia are sparse, particularly for the preschool age group. The major professional organizations concerned with the eyecare of children have based their guidelines primarily on consensus. So far, only two previous large-scale population-based studies have evaluated the association of anisometropia with amblyopia in preschoolers.6,7 To date, the VIP study provides the largest sample size (in terms of both number of children studied and number of children with amblyopia) to study the association between anisometropia and amblyopia. Similar evaluations of the association of anisometropia and amblyopia were conducted in studies by Weakley and Dobson et al,14,17 but in different, selected populations. Weakley studied the incidence of amblyopia (defined as at least one full Snellen line of acuity difference between two eyes) in a clinic-based sample of anisometropic and non-anisometropic patients between 3 to 14 years of age, and found that the “levels of anisometropia at which amblyopia becomes significant closely parallel the recent guidelines of American Academy of Ophthalmology in the Preferred Practice Pattern, which were previously supported primarily by clinical impression and experience.” 14 Because refractive error changes with age, the associations between refractive error and amblyopia in Weakley’s study, may not accurately predict the same associations among preschoolers. Dobson et al studied the association of anisometropia and amblyopia in a school-aged population from a Native American tribe with a high prevalence of astigmatism using the same definition of amblyopia (≥2 logMAR lines in interocular acuity difference), and found that hyperopic anisometropia ≥1.0 D or cylindrical anisometropia ≥ 2.0 D or VDD > 1.41 D was significantly associated with increase in IAD and presence of amblyopia.17 However, because the study was conducted in a selected population with a high prevalence of astigmatism and little spherical error, the threshold values from Dobson’s study may not apply to the general preschool population. More recently, Donahue et al found that among children participating in a statewide preschool photoscreening program, children with greater degrees of anisometropia had higher prevalence and greater depth of amblyopia. In addition, age affected the association.15,16 Younger children with anisometropia (defined as >1.0 D interocular difference in any meridian) had a lower prevalence and depth of amblyopia than older children, with prevalence ranging from 14% in 1-year-olds to 76% in 5-year-olds. All these studies are limited by sample size in that only a small number of subjects were available in certain severity levels of anisometropia to determine the threshold value. These studies are likely to be less precise in determining the threshold level of anisometropia associated with a clinically significant increase in the presence of amblyopia.
We found statistically significantly higher proportions of children with unilateral amblyopia when the degree of anisometropia was considerably lower than the levels considered amblyogenic by the professional organizations and those identified from the Weakley and Dobson studies (Table 6, available at http://aaojournal.org). Our lower thresholds are due, at least in part, to our larger sample size. For example, in Weakley’s study, the proportion with unilateral amblyopia was higher among children with spherical hyperopic anisometropia >0.5 to 1.0 D (8%) than among the isometropic group (4%) but the difference was not statistically significant. The VIP data presented here provide evidence that smaller degrees of anisometropia are associated with unilateral amblyopia. Thus, preschool children without strabismus who have an inter-ocular difference in visual acuity and anisometropia above the thresholds identified in this study may benefit from treatment for anisometropic amblyopia.
Table 6.
Anisometropic levels thought to be potentially amblyogenic in preschool and school-aged children
| Source | Age range (years) |
Sphere | Hyperopia | Myopia | Cylinder |
|---|---|---|---|---|---|
| American Academy of Ophthalmology 12 |
≥ 2 | ≥ 1.5 D | ≥ 1.5 D | ≥ 2.0 D | |
| American Optometric Association 11 |
≥ 1.0 D | ≥ 3.0 D | ≥ 1.5 D | ||
| American Association for Pediatric Ophthalmology and Strabismus 13 |
Preschool age |
> 1.5 D | >1.5 D | ||
| Weakley et al Study14 | ≥ 3 | ≥ 1.0 D | ≥ 3.0 D | ≥ 1.5 D | |
| Dobson et al Study 17 | 4 to 13 | ≥ 1.0 D | ≥ 2.0 D | ||
| Current study | 3 to 5 | > 0.5 D | > 0.25 D | > 0.25 D |
D= Diopter.
For each type of anisometropia defined here, we found that larger amounts of anisometropia were associated with higher percentages of unilateral amblyopia and greater interocular acuity difference. In addition, we found larger degrees of anisometropia were associated with worse stereoacuity. This dose-response relation is consistent with the findings of Donahue’s study from a statewide preschool photoscreening program.15,16 However, our finding that the proportion with unilateral amblyopia is higher in 3-year-old children than in 4- to 5-year-old children with moderate cylindrical anisometropia is not consistent with the findings by Donahue that older children had a higher percentage of amblyopia than younger children given the same amount of anisometropia.
We measured the degree of anisometropia using two forms of power vector analysis, the Thibos approach using a rectangular Fourier form and the Harris approach using Vector VDD. We found that VDD had significantly better power (AUC=0.84) for detecting unilateral amblyopia than the traditional clinical notation of anisometropia using spherical equivalent that ignores the axis (AUC=0.69), and the Thibo’s notation of J0/J45 that considers the axis (AUC=0.80). Even though the computation of VDD is not as straightforward as spherical equivalent, the substantial gain in the accuracy of detecting amblyopia using VDD may justify its wider use in both clinical care and clinical research.
The study is limited by the fact that in the VIP Study, visual acuity measurements were not made using the child’s best correction for the initial test, and only children who met specific criteria were retested with full cycloplegic correction, i.e., those with (1) VA <20/50 if 3 years old, VA <20/40 if 4 or 5 years old, an IAD ≥ 2 lines; AND (2) hyperopia ≥ 2.0 D, myopia≥ 0.5 D, or astigmatism ≥ 1.0 D. However, in our analyses, we assumed that children with IAD <2 lines from the initial VA test without full refraction would still have an IAD <2 lines if they were tested with full refraction. We analyzed VA data from all 782 children who underwent both initial VA testing without cycloplegic correction and VA re-test with cycloplegic correction because the VA re-test criteria were met. We found that re-test VA under cycloplegic correction usually led to a smaller IAD (0.21 LogMAR in IAD from the initial test without cycloplegic correction, and 0.15 LogMAR from the re-test with cycloplegic correction). The VA re-test also led to a lower % with unilateral amblyopia (39.6% in initial test, and 34.5% in re-test). Because the VA re-test rate was higher in anisometropic children than non-anisometropic children (22.1% vs. 7.4%), and the VA re-test under cycloplegic correction was associated with smaller IAD and a lower % with unilateral amblyopia, we could only have under-estimated rather than over-estimated that the association of anisometropia with unilateral amblyopia and IAD. The study also excluded 160 (4.0%) children who had an IAD ≥ 2 lines yet were not re-tested with full correction because their refractive error did not meet re-test criteria. However, because the distribution of spherical equivalent anisometropia levels of these excluded children was very similar to those who were included in our statistical analysis (p=0.51), we don’t think excluding these 160 children introduces any substantial bias. The VIP participants were enrolled from Head Start centers in the United States and therefore all live in low-income families. If the association between anisometropia and unilateral amblyopia is found to differ by socio-economic group, the VIP results may not apply to all preschoolers.
In summary, we analyzed the cross-sectional data from a large group of children who participated in VIP and found that smaller amounts of anisometropia than currently used in many guidelines based on expert opinion are associated with presence of unilateral amblyopia. These degrees of anisometropia are also associated with larger interocular acuity difference and lower stereoacuity, in a dose-response manner. While the choice of the threshold of anisometropia for referral for evaluation of amblyopia will depend on the desired levels of sensitivity and specificity, these data provide an evidence base for making the decision.
Supplementary Material
Acknowledgments
This study is supported by grants from the National Eye Institute, National Institutes of Health, Department of Health and Human Services, Bethesda, MD: U10EY12534; U10EY12545; U10EY12547; U10EY12550; U10EY12644; U10EY12647; U10EY12648 and R21EY018908.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: None.
REFERENCES
- 1.Simons K. Preschool vision screening: rationale, methodology and outcome. Surv Ophthalmol. 1996;41:3–30. doi: 10.1016/s0039-6257(97)81990-x. [DOI] [PubMed] [Google Scholar]
- 2.Simons K. Amblyopia characterization, treatment, and prophylaxis. Surv Ophthalmol. 2005;50:123–66. doi: 10.1016/j.survophthal.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 3.Rahi J, Logan S, Timms C, et al. Risk, causes, and outcomes of visual impairment after loss of vision in the non-amblyopic eye: a population-based study. Lancet. 2002;360:597–602. doi: 10.1016/s0140-6736(02)09782-9. [DOI] [PubMed] [Google Scholar]
- 4.Williams C, Northsone K, Harrad RA, et al. Amblyopia treatment outcomes after screening before or at age 3 years: follow-up from randomised trial. BMJ. 2002;324:1549. doi: 10.1136/bmj.324.7353.1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.U.S. Preventive Services Task Force Screening for visual impairment in children younger than age 5 years: recommendation statement. Ann Fam Med. 2004;2:263–6. doi: 10.1370/afm.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Multi-ethnic Pediatric Eye Disease Study Group Prevalence of amblyopia and strabismus in African American and Hispanic children ages 6 to 72 months: the Multi-ethnic Pediatric Eye Disease Study. Ophthalmology. 2008;115:1229–36. doi: 10.1016/j.ophtha.2007.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Friedman DS, Repka MX, Katz J, et al. Prevalence of amblyopia and strabismus in white and African children age 6 through 71 months: the Baltimore Pediatric Eye Disease Study. Ophthalmology. 2009;116:2128–34. doi: 10.1016/j.ophtha.2009.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vision In Preschoolers Study Group Comparison of preschool vision screening tests as administered by licensed eye care professionals in the Vision In Preschoolers Study. Ophthalmology. 2004;111:637–50. doi: 10.1016/j.ophtha.2004.01.022. [DOI] [PubMed] [Google Scholar]
- 9.Vision In Preschoolers Study Group Preschool vision screening tests administered by nurse screeners compared to lay screeners in the Vision in Preschoolers Study. Invest Ophthalmol Vis Sci. 2005;46:2639–48. doi: 10.1167/iovs.05-0141. [DOI] [PubMed] [Google Scholar]
- 10.von Noorden GK. Factors involved in the production of amblyopia. Br J Ophthalmol. 1974;58:158–64. doi: 10.1136/bjo.58.3.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Optometric Association n Consensus Panel On Care of the Patient With Amblyopia . Optometric Clinical Practice Guideline. Care of the Patient with Amblyopia. American Optometric Association; St. Louis, MO: [Accessed July 15, 2012]. 2004. Available at: http://www.aoa.org/documents/CPG-4.pdf. [Google Scholar]
- 12.American Academy of Ophthalmology Pediatric Ophthalmology/Strabismus Panel . Amblyopia. American Academy of Ophthalmology; San Francisco, CA: [Accessed July 15, 2012]. 2007. Preferred Practice Pattern Guidelines. Available at: http://one.aao.org/CE/PracticeGuidelines/PPP.aspx. [Google Scholar]
- 13.Donahue SP, Arnold RW, Ruben JB, AAPOS Vision Screening Committee Preschool vision screening: what should we detect and how should we report it? Uniform guidelines for reporting results of preschool vision screening studies. J AAPOS. 2003;7:314–6. doi: 10.1016/s1091-8531(03)00182-4. [DOI] [PubMed] [Google Scholar]
- 14.Weakley DR., Jr The association between nonstrabismic anisometropia, amblyopia, and subnormal binocularity. Ophthalmology. 2001;108:163–71. doi: 10.1016/s0161-6420(00)00425-5. [DOI] [PubMed] [Google Scholar]
- 15.Donahue SP. Relationship between anisometropia, patient age, and the development of amblyopia. Am J Ophthalmol. 2006;142:132–40. doi: 10.1016/j.ajo.2006.02.040. [DOI] [PubMed] [Google Scholar]
- 16.Leon A, Donahue SP, Morrison DG, et al. The age-dependent effect of anisometropia magnitude on anisometropic amblyopia severity. J AAPOS. 2008;12:150–6. doi: 10.1016/j.jaapos.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 17.Dobson V, Miller JM, Clifford-Donaldson CE, Harvey EM. Associations between anisometropia, amblyopia, and reduced stereoacuity in a school-aged population with a high prevalence of astigmatism. Invest Ophthalmol Vis Sci. 2008;49:4427–36. doi: 10.1167/iovs.08-1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Holmes JM, Beck RW, Repka MX, et al. Pediatric Eye Disease Investigator Group. The Amblyopia Treatment Study visual acuity testing protocol. Arch Ophthalmol. 2001;119:1345–53. doi: 10.1001/archopht.119.9.1345. [DOI] [PubMed] [Google Scholar]
- 19.Thibos LN, Wheeler W, Horner D. Power vectors: an application of Fourier analysis to the description and statistical analysis of refractive error. Optom Vis Sci. 1997;74:367–75. doi: 10.1097/00006324-199706000-00019. [DOI] [PubMed] [Google Scholar]
- 20.Harris WF. The mean and variance of samples of dioptric powers: the basic calculations. Clin Exp Optom. 1990;73:89–92. [Google Scholar]
- 21.Wallace DK, Lazar EL, Melia M, et al. Pediatric Eye Disease Investigator Group. Stereoacuity in children with anisometropic amblyopia. J AAPOS. 2011;15:455–61. doi: 10.1016/j.jaapos.2011.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–45. [PubMed] [Google Scholar]
- 23.Hochberg Y. A sharper Bonferroni procedure for multiple significance testing. Biometrika. 1988;75:800–3. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.