Abstract
Background
Selective lumbar nerve root block (SNRB) is generally accepted as an effective treatment method for back pain with sciatica. However, it requires devices producing radioactive materials such as C-arm fluoroscopy. This study evaluated the usefulness of the longitudinal view of transverse process and needles for medial branch block as landmarks under ultrasonography.
Methods
We performed selective nerve root block for 96 nerve roots in 61 patients under the guidance of ultrasound. A curved probe was used to identify the facet joints and transverse processes. Identifying the lumbar nerve roots under the skin surface and ultrasound landmarks, the cephalad and caudal medial branch blocks were undertaken under the transverse view of sonogram first. A needle for nerve root block was inserted between the two transverse processes under longitudinal view, while estimating the depth with the needle for medial branch block. We then injected 1.0 mL of contrast medium and checked the distribution of the nerve root with C-arm fluoroscopy to evaluate the accuracy. The visual analog scale (VAS) was used to access the clinical results.
Results
Seven SNRBs were performed for the L2 nerve root, 15 for L3, 49 for L4, and 25 for L5, respectively. Eighty-six SNRBs (89.5%) showed successful positioning of the needles. We failed in the following cases: 1 case for the L2 nerve root; 2 for L3; 3 for L4; and 4 for L5. The failed needles were positioned at wrong leveled segments in 4 cases and inappropriate place in 6 cases. VAS was improved from 7.6 ± 0.6 to 3.5 ± 1.3 after the procedure.
Conclusions
For SNRB in lumbar spine, the transverse processes under longitudinal view as the ultrasound landmark and the needles of medial branch block to the facet joint can be a promising guidance.
Keywords: Lumbar spine, Spinal injections, Ultrasound
Selective nerve root block (SNRB) has a therapeutic potential for lower back pain accompanied by sciatica, and many studies have reported good results.1,2) Furthermore, SNRB can help to confirm the surgical level and range before the operation as a diagnostic tool. It also alleviates pain effectively to delay the operation. However, the traditional method, using computed tomography (CT) or C-arm fluoroscopy as a guidance, is not free from exposure to radiation. Also, the space required for the devices is not always available in the outpatient departments. Recently, the ultrasound guided SNRB has been introduced to overcome these disadvantage, so as to be applied easily in the outpatient department.3,4) However, its application is restricted due to the more difficult anatomical assessment to nerve roots as compared to the facet joint block. Regarding this limitation, we have attempted an ultrasound guided selective lumbar nerve root block. We evaluated the usefulness of longitudinal view of the transverse process and needles of medial branch block to facet joint as landmarks under ultrasonography.
METHODS
The patients had visited our hospital for chronic lower back pain and radiating pain to the leg, from September 2010 to February 2011. They were diagnosed lumbar spinal stenosis, based on the medical history, physical examination, radiography, magnetic resonance imaging (MRI) or CT. Sixty-one patients showed no satisfactory improvement of symptoms following medication, physical therapy, and rehabilitation programs for more than 6 weeks. Ultrasound-guided selective nerve root block was done in 96 nerve roots for 61 patients. There were 26 male and 35 female. The mean age of the patients was 60.4 years (range, 35 to 83 years). They were selected for the lumbar nerve root for nerve block, based on clinical symptoms and radiological pathology, including foraminal stenosis on MRI or CT. During the procedure, the patients were in the prone position, and the lumbar lordotic curve was countervailed. A surface landmark of the spinous process, iliac crest line, and needle target points were marked using anteroposterior lumbar radiograph after the spinous process, and the posterior iliac crest line of patients were palpated (Fig. 1). To develop the necessary ultrasound views, the spinous processes were first examined under high-resolution ultrasound with 5-MHz curved transducer (LogiQ P5, GE Medical Systems, Milwaukee, WI, USA). Ultrasound-guided identification of the desired segment for nerve block was not described exactly, in contrast to C-arm fluoroscopy. Longitudinal facet views were obtained by curved tranducer to identify the different spinal segments (Fig. 2). The physicians were well aware of the anatomical landmark of the lateral facet and the transverse process for pedicle screw placement in the lumbar spine. The facet joint is a useful ultrasonic landmark for the identification of anatomical level. We identified the target level by counting up the facet joint from the lumbosacral facet joint or counting down from the twelfth rib. After finding the location of the desired target level, the transverse axial images were obtained by rotating the probe 90 degrees. The spinous process, facet joint, and transverse process were delineated by transverse sonograms at each level. The target point for the medial branch block was defined as on the upper edge of the transverse process. Confirming lumbar nerve roots under the surface and ultrasound landmarks, the cephalad and caudal medial branch block to the nerve root was undertaken in the transverse view of sonogram, using 21 gauge needle. The needle for the medial branch block was inserted approximately 30 degrees to the skin and exactly in line with the transducer and echo plane as short axis in plane approach (Fig. 3). A needle of length equal to that for medial branch block was inserted for SNRB, between the two transverse processes under longitudinal view. The angle of the needles was the same for medial branch block as short axis out of plane approach (Fig. 4). At this point we estimated the depth of the needle for SNRB, comparing with the needles for medial branch block, and we inserted the needle 10 mm deeper than medial branch block. Then we injected 1 mL contrast medium and evaluated the position of the needles and distribution of the contrast medium with C-arm fluoroscopy (Fig. 5). We used a mixture of 1 mL of 2% lidocaine and 1 mL of triamcinolone acetate (40 mg/mL). The clinical assessment was performed by visual analog scale (VAS) at one to three days after the procedure at the outpatient clinic. Independent t-tests were used to compare between pre- and postoperative VAS. Statistical analysis was carried out using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). Significance was set at p < 0.05.
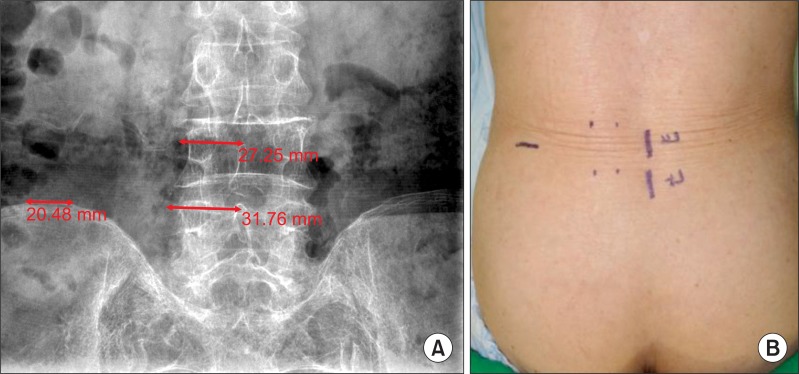
Fig. 1.
(A) Distance from the spinous process to the needle target point was measured on the radiograph. (B) Surface landmarks such as spinous process, iliac crest, and needle target point were marked.
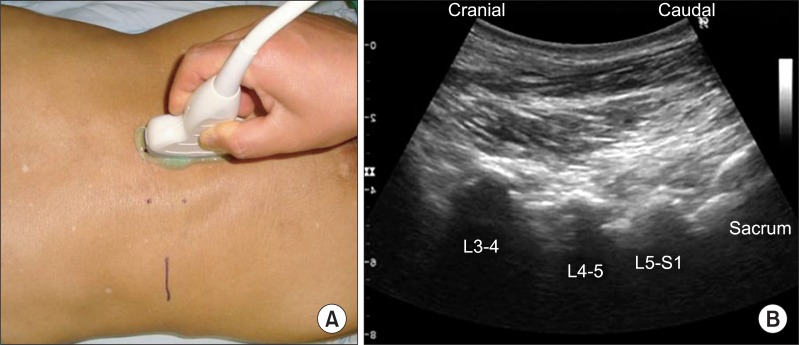
Fig. 2.
(A) Longitudinal facet views were obtained by curved transducer to identify the different spinal segments. (B) The longitudinal facet view shows L3-4, L4-5, and L5-S1 facet joints.
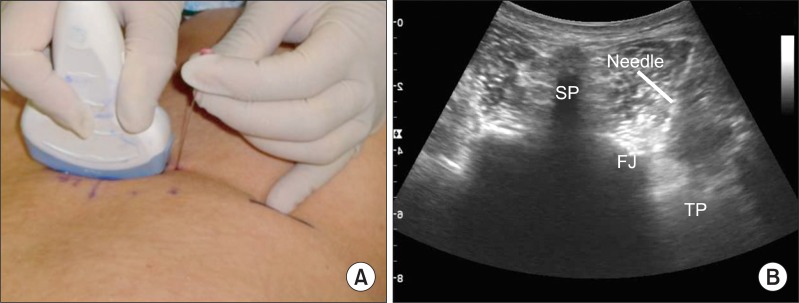
Fig. 3.
(A) Medial branch block to the facet joint was performed on the transverse view as short axis in plane approach. (B) The needle is targeted just lateral to the facet joint. SP: spinous process, FJ: facet joint, TP: transverse process.
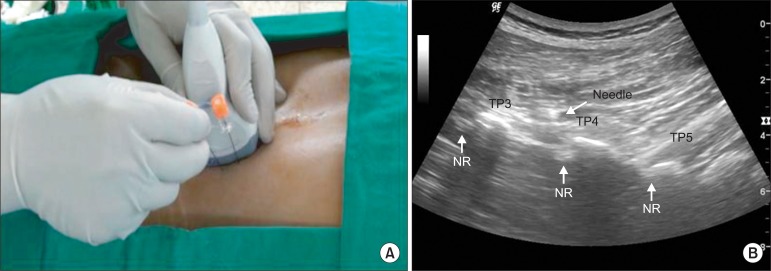
Fig. 4.
(A) The needle for selective nerve root (NR) block was inserted at the same angle with the needle for medial branch block as short axis out of plane approach. (B) The NRs are seen just caudal to the each transverse process (TP) and the needle is approaching the L3 NR.
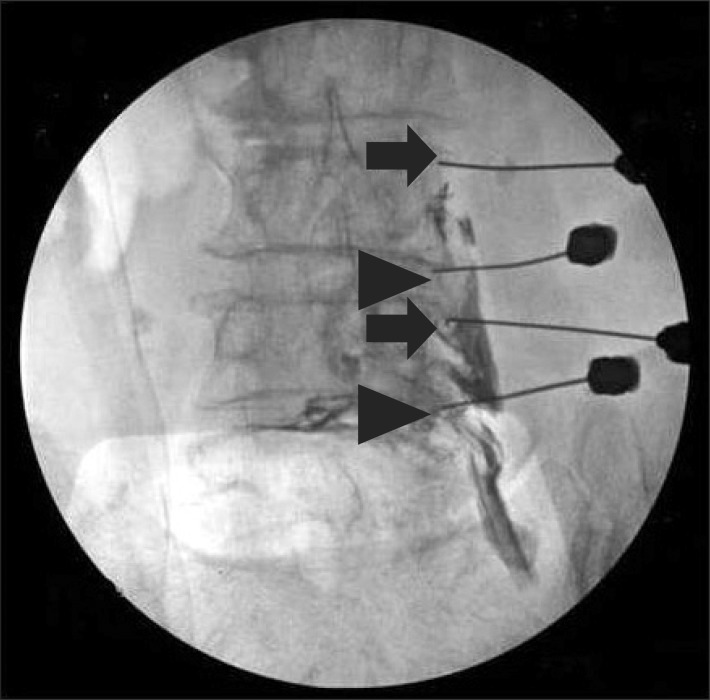
Fig. 5.
The position of the needles and distribution of the contrast medium were evaluated with C-arm fluoroscopy. The two arrows indicate needles for medial branch block and the two arrowheads for selective nerve root block.
RESULTS
Seven SNRBs were performed at the L2 nerve root (foramen between the L2 and L3), 15 at the L3, 49 at the L4, and 25 at the L5, respectively. Of total 96 needles, 86 SNRBs (89.5%) showed successful positioning of the needles. We failed one case at the L2-3 level, and 2 at L3-4, 3 at L4-5, and 4 at L5-S1. The failed needles were positioned in wrong leveled segments in 4 cases and inappropriate place in 6 cases. VAS was improved from 7.6 ± 0.6 to 3.5 ± 1.3 after the procedure (p = 0.001). Before injecting the mixture of medicine, we corrected the wrong-positioned needles to the appropriate places under C-arm fluoroscopy. We had all patients rest in the recovery room for an hour before leaving the hospital. No case showed any complication such as aggravation of the pain, numbness, headache, dizziness, and allergic reaction.
DISCUSSION
The use of ultrasonography has recently been increasing in musculoskeletal intervention treatment.4-6) However, there are some limitations in using ultrasound for SNRB. The most challenging part in the use of ultrasound is in placing the needle in the exact position and estimating the depth of the nerve roots. Loizides et al.7) reported that all 10 needles were correctly placed using costal process and inter-transverse ligament as landmarks by in-plane method in their cadaveric study. However, it is not easy to obtain inter-transverse ligament clearly in practical situations. Chumnanvej et al.8) reported that successful needle position under ultrasound was resulted in 63% for SNRB. But they did not mention the approaching method of the needle, and reported that facet echo edge was identified by ultrasound. It is not easy to have a clear view for facet echo edge in all patients, and it is more difficult to place the needle tip at the facet echo edge under ultrasound. We think this is the reason for their low success rate of 63%. In order to overcome this limitation, we undertook the SNRB on the longitudinal ultrasound view for short axis out of plane approach. This could show both the caudal and cephalad transverse processes at one plane, and it was easier to apprehend the structural correlation during the procedure than transverse view. Additionally, prior to SNRB, we performed medial branch block as the needle for another guide. We took the same length of needle for SNRB and medial branch block, and inserted the needle for SNRB at the same angle (approximately 30°) of the needle for medial branch block. Preoperatively, we measured the distance from the basal portion of the transverse process to posterior margin of the vertebral disc on magnetic resonance imaging; and the mean distance was 5.7 ± 1.6 cm. We could estimate the depth of the needle comparing the head of the needles. The needle for SNRB was inserted deeper by 5 to 10 mm than medial branch block. To make a decision for the final depth of the needle, it is possible to get an image for motion echo of final needle tip in ultrasound by a small movement of the needle tip.
Most previous studies which performed ultrasound guided SNRB assumed successful positioning of the needle depending on whether the symptoms were relieved or not.9) The relief of symptoms could be obtained by systemic drug effect even if the needle was not placed at the appropriate position, leading to inadequate estimation of the accuracy. Hence, we evaluated the accuracy by checking the placement of the needle and distribution of the contrast medium, especially the tip, with C-arm fluoroscopy after injecting contrast medium under ultrasonic view. Eighty-six roots (89.5%) could be guided successfully for SNRB by ultrasound.
In comparison with CT or C-arm fluoroscopy, ultrasonography newly draws attentions for some of its advantages. First, there is no exposure to radiation. Although the radiation dose during the nerve block by CT or C-arm fluoroscopy for single procedure is ignorable, the physicians are repeatedly exposed to radiation during many procedures besides C-arm fluoroscopy, including nerve blocks. Thus when the total radiation dose for one year is examined, the level is of a concern. It can be argued that the hand region of orthopedic surgeons who use the irradiator may be excessively damaged by the radiation.10) Lee et al.11) reported on a hand lesion that was damaged due to radiation in Korea. The second advantage is that the additional equipments necessary for the protection against radiation are not required; and with the small size of the equipment which easily movable, the procedure can be performed in outpatient clinics.
Despite such advantages, the acoustic impedance of bone is high, and thus it has limitations in taking a good quality image of spinal structures. In addition, the reproducibility among doctors is low.12) These drawbacks may be overcome with practice and further development of ultrasound equipment in the future.
In conclusion, the transverse processes under longitudinal view as ultrasound landmark and the needles of medial branch block to the facet joint can be a promising guidance for SNRB in lumbar spine. It can be performed with 89.5% effectiveness, and we expect it to be performed in the outpatient departments without the concern for the radiation exposure.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Sato M, Simizu S, Kadota R, Takahasi H. Ultrasound and nerve stimulation-guided L5 nerve root block. Spine (Phila Pa 1976) 2009;34(24):2669–2673. doi: 10.1097/BRS.0b013e3181b43c62. [DOI] [PubMed] [Google Scholar]
- 2.Riew KD, Park JB, Cho YS, et al. Nerve root blocks in the treatment of lumbar radicular pain: a minimum five-year follow-up. J Bone Joint Surg Am. 2006;88(8):1722–1725. doi: 10.2106/JBJS.E.00278. [DOI] [PubMed] [Google Scholar]
- 3.Gray AT. Ultrasound-guided regional anesthesia: current state of the art. Anesthesiology. 2006;104(2):368–373. doi: 10.1097/00000542-200602000-00024. [DOI] [PubMed] [Google Scholar]
- 4.Marhofer P, Greher M, Kapral S. Ultrasound guidance in regional anaesthesia. Br J Anaesth. 2005;94(1):7–17. doi: 10.1093/bja/aei002. [DOI] [PubMed] [Google Scholar]
- 5.Peterson MK, Millar FA, Sheppard DG. Ultrasound-guided nerve blocks. Br J Anaesth. 2002;88(5):621–624. doi: 10.1093/bja/88.5.621. [DOI] [PubMed] [Google Scholar]
- 6.Kapral S, Krafft P, Eibenberger K, Fitzgerald R, Gosch M, Weinstabl C. Ultrasound-guided supraclavicular approach for regional anesthesia of the brachial plexus. Anesth Analg. 1994;78(3):507–513. doi: 10.1213/00000539-199403000-00016. [DOI] [PubMed] [Google Scholar]
- 7.Loizides A, Gruber H, Peer S, Brenner E, Galiano K, Obernauer J. A new simplified sonographic approach for pararadicular injections in the lumbar spine: a CT-controlled cadaver study. AJNR Am J Neuroradiol. 2011;32(5):828–831. doi: 10.3174/ajnr.A2389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chumnanvej S, Wetchagama N, Kounsongtham V. Accuracy of needle-tip localization by ultrasound guidance lumbar selective nerve root block: a prospective clinical study of 78 lumbar nerve roots block. J Med Assoc Thai. 2011;94(12):1451–1456. [PubMed] [Google Scholar]
- 9.Riew KD, Yin Y, Gilula L, et al. The effect of nerve-root injections on the need for operative treatment of lumbar radicular pain: a prospective, randomized, controlled, double-blind study. J Bone Joint Surg Am. 2000;82(11):1589–1593. doi: 10.2106/00004623-200011000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Watson-Jones R. Fracture and joint injuries. New York: Churchill Livingstone; 1982. pp. 278–279. [Google Scholar]
- 11.Lee EW, Chun JM, Ahn BW, Park YW, Lee SY, Paik NC. A study of hand lesion exposed by radiation. J Korean Orthop Assoc. 1991;26(3):841–846. [Google Scholar]
- 12.Hashimoto BE, Kramer DJ, Wiitala L. Applications of musculoskeletal sonography. J Clin Ultrasound. 1999;27(6):293–318. doi: 10.1002/(sici)1097-0096(199907/08)27:6<293::aid-jcu1>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]