Abstract
Background
Alopecia areata (AA) is believed to be an organ-specific autoimmune disease in which a mononuclear cell infiltrate develops in and around anagen hair follicles. There is no definitive therapy for AA.
Objective
We sought to determine whether the combination therapy of cyclosporine and psoralen plus ultraviolet A (PUVA) could be an effective treatment for severe AA.
Methods
A total of 41 patients with severe AA were treated with oral cyclosporine and topical PUVA. Cyclosporine was given at an initial daily dose of 200 mg for adult and 100 mg for children for periods of up to 16 weeks. Eight-methoxypsoralen (Methoxsalen) was applied topically 20 minutes prior to ultraviolet A (UVA) exposure, and the patients were irradiated with UVA twice a week for 16 weeks.
Results
Of the total 41 patients, 2 (7.3%) patients were lost to follow-up, and 1 (2.4%) patient discontinued the treatment due to abdominal discomfort. Six (14.6%) patients were treated for less than 12 weeks. Of remaining 32 patients, 3 (9.4%) showed excellent response, 3 (9.4%) showed good response, 12 (37.5%) showed fair response, and 14 (43.7%) showed poor response.
Conclusion
Although limited by its uncontrolled character, this study shows that the combination therapy with cyclosporine and PUVA may be an additional choice for severe and recalcitrant AA.
Keywords: Alopecia areata, Cyclosporine, PUVA therapy, Side effect
INTRODUCTION
Severe alopecia areata (AA) is a refractory condition. Although it is a medically benign condition, AA may cause considerable psychological and emotional distress for affected individuals, particularly for severe or chronic cases1. Conventional treatment including topical, intralesional, photochemotherapy, and systemic steroids, such as topical sensitizers (diphencyprone), anthralin, and minoxidil, are usually ineffective in severe AA2-8. Systemic corticosteroids are one of the most commonly used therapeutic modalities in patients with extensive AA9,10. However, potential adverse effects normally preclude their use in the long term11.
Cyclosporine, which is commonly used in post-transplantation patients, has a common cutaneous side-effect of hypertrichosis12,13. It also decreases the perifollicular lymphocytic infiltrates14. Although systemic cyclosporine appears to be effective in AA, the high recurrence rate after discontinuation and the side-effect profile make cyclosporine a poor choice for the treatment of AA12,15. A recent study reported the effect of combination therapy with cyclosporine and methylprednisolone in patients with severe AA, and the results showed 88.4% of patients with significant hair regrowth16.
In this study, we report on the use of cyclosporine in combination with psoralen plus ultraviolet A (PUVA) to treat 41 patients with severe AA.
MATERIALS AND METHODS
In this retrospective study, total 41 patients (17 female and 24 male) with severe AA (≥50% loss of scalp hair or ≥10 patches scattered over the scalp and body) received combination therapy between January 2007 and April 2008. This study was approved by the Institutional Review Board (IRB). Severe AA patients with impaired patient's quality of life and a significant psychological impact were enrolled. The average age of patients was 24 years (from 6 to 50 years), and mean duration of disease was 22 months (from 5 to 240 months). There were 5 cases of AA, 9 cases of alopecia totalis (AT) and 27 cases of alopecia universalis (AU). Patients with cardiovascular disease, hypertension, diabetes mellitus, thyroid disorder, peptic ulcer, or other serious medical illness and pregnancy were excluded. Prior to the treatment, patients were informed of study procedures, benefits, and complications (hypertension, nephrotoxicity, headache, skin carcinogenesis, postinflammatory hyperpigmentation etc.), and signed consent was obtained from each patient. All patients had been treated with topical sensitizers (diphencyprone), cryotherapy, phototherapy, oral steroid, or oral cyclosporine for more than 6 months with no satisfactory results. The patients underwent physical examination, with the taking of blood pressure and other investigations, including compete blood cell count, liver function test, renal function test, urinalysis, and checking of electrolytes. Patients were clinically evaluated at monthly intervals along with the measurement of blood pressure, liver function test, and renal function test. At each visit, we questioned the patient on the occurrence of any side effects.
Cyclosporine was given at an initial daily dose of 200 mg for adult and 100 mg for children for periods of up to 16 weeks. At the end of the sixteen-week period, the dose of cyclosporine was reduced gradually. Eight-methoxypsoralen (Methoxsalen) was applied topically 20 minutes prior to ultraviolet A (UVA) exposure, and the patients were irradiated with UVA twice a week for 16 weeks. The initial dose was 1 J per square cm (J/cm2), with the subsequent doses increased by 0.5 J/cm2 according to individual patient tolerance, up to a maximum of 15 J/cm2.
Efficacy was graded by direct clinical examination and photographs. Response to treatment was evaluated as follows: excellent response, more than a 50% extent of hair regrowth; good response, hair regrowth of 25% to 50%; fair response, hair regrowth of 10% to 25%; and poor response, hair regrowth of 0% to 10%. Improvements mean sum of excellent, good, and fair responses.
RESULTS
The results from this study are presented in Table 1. Of the total 41 patients, 2 (7.3%) patients were lost to follow-up, 1 (2.4%) patient discontinued the treatment due to abdominal discomfort, and 6 (14.6%) patients were treated for less than 12 weeks. Of the remaining 32 patients, 19 (59.4%) patients had improvements: 3 (9.4%) of excellent responses; 5 (15.6%) of good responses; and 11 (34.4%) of fair responses. Thirteen (40.6%) patients showed poor response.
Table 1.
Demographics, duration of treatment, response, and duration until new hair growth (n=41)
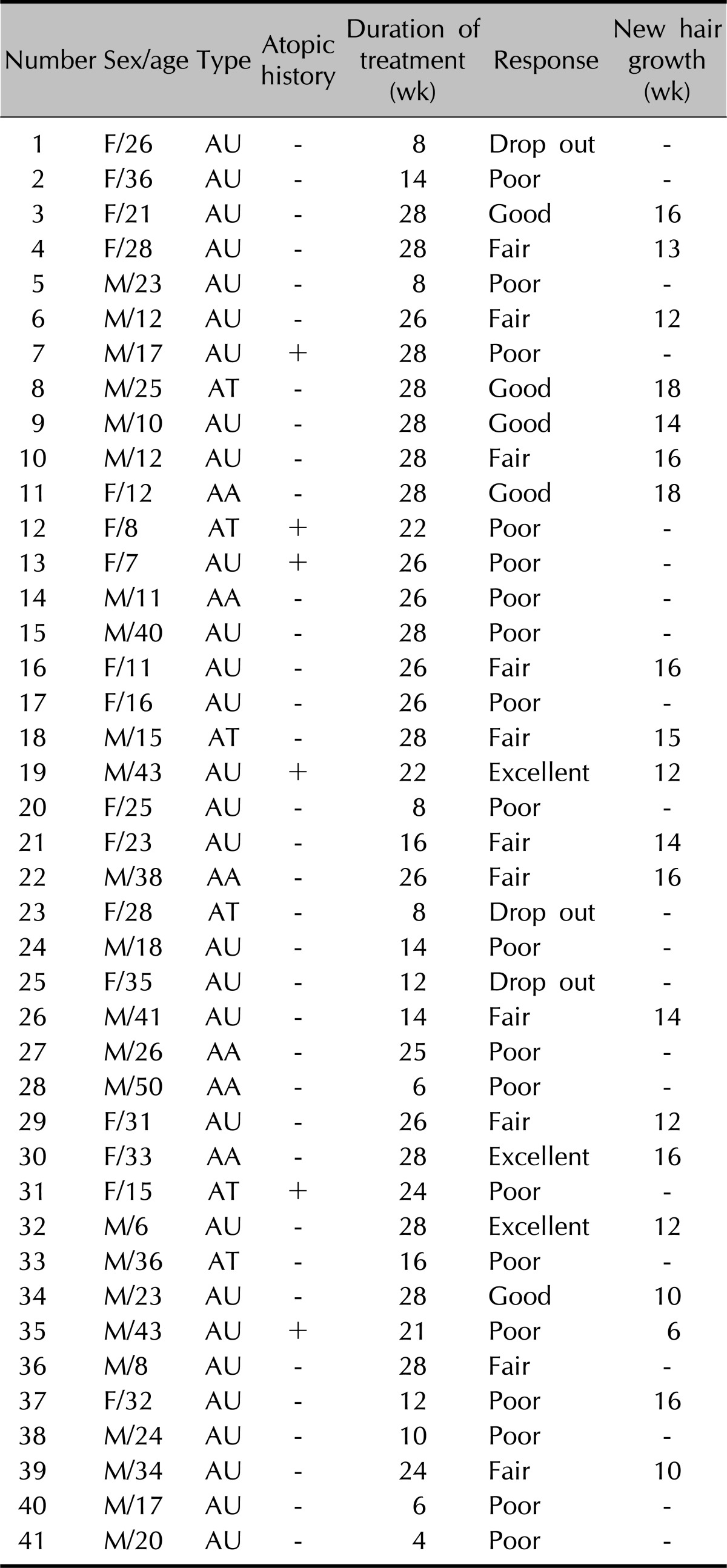
F: female, M: male, AU: alopecia universalis, AT: alopecia totalis, AA: alopecia areata.
The average duration until growth of new hair was 13.8 weeks (6 to 18 weeks). Six (18.7%) patients had relapse during the observation period of 12 months.
Side-effects of the therapy were noted in 9 (28.1%) patients. Gastrointestinal disturbance (n=5) was the most common side effect, and other side effects included hypertrichosis (n=2), headache (n=1), and hypertension (n=1). Except for 1 discontinued case, all the side effects related to therapy were gradually endurable during the first 1 month and subsided in the 1 year follow-up period.
DISCUSSION
AA is a tissue restricted autoimmune disorder with an unpredictable and relapsing course. The hair loss is most often localized and patchy, and extensive forms of AA are less common. AA involving more than 50% hair loss was seen in 11% of patients in one study17.
At present, all treatments for AA are palliative, only controlling the condition. All local treatments may help the treated area, but do not prevent further spread of the condition. In addition, any mode of treatment may need to be used for long periods because of the chronic nature of AA9. Extensive AA is more difficult to treat and more resistant to conventional modalities such as topical steroids, topical sensitizer, PUVA therapy, minoxidil, and immunomodulators10,13,18.
Weissmann et al.19 reported that PUVA had induced regrowth of hair in all cases of AA treated. The use of PUVA is based on the concept that the mononuclear cells that surround the affected hair follicles may play a direct pathogenic role, and that PUVA therapy can eradicate this inflammatory cell infiltrate20-22. Relapses of AA are frequent. Hair regrowth after oral PUVA treatment was reported to require a mean energy of 505 J/cm2 in 38% of patients with AT23.
Cyclosporine is a common therapy used in patients undergoing organ transplantation, which exerts its effect via specific inhibition of T-cell activity. A common cutaneous side-effect is dose-dependent hypertrichosis, which occurs in approximately 80% of patients, possibly as a result of prolongation of the anagen phase of the hair cycle12,13. It also decreases the perifollicular lymphocytic infiltrates through inhibition of primary helper T cell activation. Oral cyclospoine was effective in the DEBR model for AA. All rats had a full pelt by 5 weeks of treatments with 10 mg/kg/d, 5 d/wk for 7 weeks24. Gupta et al.15 first reported the treatment of AA in humans with oral cyclosporine using doses of 6 mg/kg/d for 3 months. Six patients experienced some hair regrowth, with excellent results in two patients. However, all patients relapsed within 3 months after the treatment was stopped. Shapiro et al.25 used oral cyclosporine 5 mg/kg/d in combination with oral prednisone 5 mg/d for 6 months. Two of eight patients experienced cosmetically acceptable regrowth, but they both relapsed after discontinuation of the therapy. Three patients had to discontinue medications because of side-effects including generalized edema, hypertension, abnormal liver function test, abnormal lipid levels, and hypertrichosis.
We attempted treatment of severe AA with oral cyclosporine and topical PUVA, and 59.4% of patients had improvements (Fig. 1, 2). The side-effects were seen in 28.1% of the patients; however they were not serious enough to warrant discontinuing the therapy in any of our patients. Only one patient wanted to stop the therapy due to abdominal discomfort. Most of the side-effects occurred during the first 2 weeks and became endurable within 1 month.
Fig. 1.
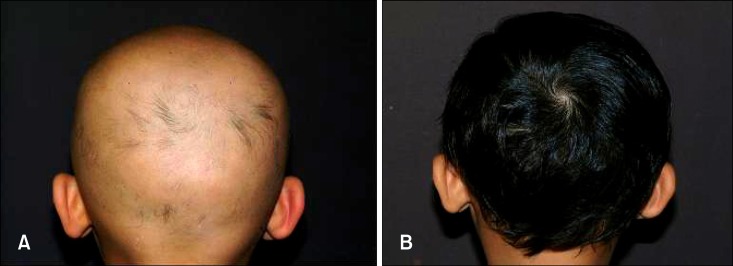
A 6-year-old boy with alopecia universalis of 4 years' duration: (A) Baseline, (B) 24 weeks after the treatment.
Fig. 2.
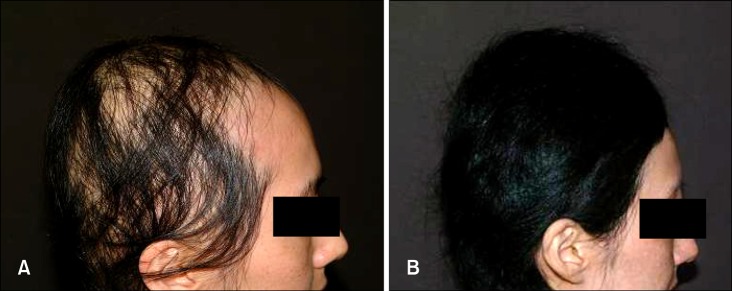
A 33-year-old woman with patchy alopecia areata of 3 years' duration: (A) Baseline, (B) 16 weeks after the treatment.
Despite the fact that the treatment regimen tested in this study was well-tolerated with no serious adverse events, potential side-effects must be taken into account. We should be mindful of the synergistic carcinogenesis of this combination therapy by the increasing Treg cells and UV damage, especially in young patients and those with a disease history of malignancy. Because patients with transplantation treated with cyclosporine experience increases in squamous cell carcinomas of the skin, and PUVA is known to cause an increase in cutaneous squamous cell carcinomas, using these two treatment modalities together may result in markedly increased cutaneous tumorigenesis26. The study period was relatively short for the evaluation of AA, as AA is a tissue-restricted autoimmune disorder with an unpredictable and relapsing course. As such, the long-term efficacy and side-effects of this treatment need to be evaluated by further investigation, along with the comparison of cyclosporine and PUVA therapy. Nevertheless, considering that the severe AA can impair patient's quality of life and has a significant psychological impact, the combination therapy of oral cyclosporine and PUVA in a short period under the full explanation and agreement may be an additional choice in severe and recalcitrant AA.
ACKNOWLEDGMENT
This study was supported by a Korea Research Foundation Grant funded by the Korea Government (2010-0021960).
References
- 1.García-Hernández MJ, Ruiz-Doblado S, Rodriguez-Pichardo A, Camacho F. Alopecia areata, stress and psychiatric disorders: a review. J Dermatol. 1999;26:625–632. doi: 10.1111/j.1346-8138.1999.tb02063.x. [DOI] [PubMed] [Google Scholar]
- 2.Feldmann KA, Kunte C, Wollenberg A, Wolfe H. Is topical tacrolimus effective in alopecia areata universalis? Br J Dermatol. 2002;147:1031–1032. doi: 10.1046/j.1365-2133.2002.500210.x. [DOI] [PubMed] [Google Scholar]
- 3.Taylor CR, Hawk JL. PUVA treatment of alopecia areata partialis, totalis and universalis: audit of 10 years' experience at St John's Institute of Dermatology. Br J Dermatol. 1995;133:914–918. doi: 10.1111/j.1365-2133.1995.tb06925.x. [DOI] [PubMed] [Google Scholar]
- 4.Higgins E, du Vivier A. Topical immunotherapy: unapproved uses, dosages, or indications. Clin Dermatol. 2002;20:515–521. doi: 10.1016/s0738-081x(02)00272-9. [DOI] [PubMed] [Google Scholar]
- 5.Tobin DJ, Gardner SH, Lindsey NJ, Hoffmann R, Happle R, Freyschmidt-Paul P. Diphencyprone immunotherapy alters anti-hair follicle antibody status in patients with alopecia areata. Eur J Dermatol. 2002;12:327–334. [PubMed] [Google Scholar]
- 6.Seiter S, Ugurel S, Tilgen W, Reinhold U. High-dose pulse corticosteroid therapy in the treatment of severe alopecia areata. Dermatology. 2001;202:230–234. doi: 10.1159/000051642. [DOI] [PubMed] [Google Scholar]
- 7.Sharma VK. Pulsed administration of corticosteroids in the treatment of alopecia areata. Int J Dermatol. 1996;35:133–136. doi: 10.1111/j.1365-4362.1996.tb03281.x. [DOI] [PubMed] [Google Scholar]
- 8.Assouly P, Reygagne P, Jouanique C, Matard B, Marechal E, Reynert P, et al. Intravenous pulse methylprednisolone therapy for severe alopecia areata: an open study of 66 patients. Ann Dermatol Venereol. 2003;130:326–330. [PubMed] [Google Scholar]
- 9.Madani S, Shapiro J. Alopecia areata update. J Am Acad Dermatol. 2000;42:549–566. [PubMed] [Google Scholar]
- 10.MacDonald Hull SP, Wood ML, Hutchinson PE, Sladden M, Messenger AG British Association of Dermatologists. Guidelines for the management of alopecia areata. Br J Dermatol. 2003;149:692–699. doi: 10.1046/j.1365-2133.2003.05535.x. [DOI] [PubMed] [Google Scholar]
- 11.Kar BR, Handa S, Dogra S, Kumar B. Placebo-controlled oral pulse prednisolone therapy in alopecia areata. J Am Acad Dermatol. 2005;52:287–290. doi: 10.1016/j.jaad.2004.10.873. [DOI] [PubMed] [Google Scholar]
- 12.Kahan BD. Cyclosporine. N Engl J Med. 1989;321:1725–1738. doi: 10.1056/NEJM198912213212507. [DOI] [PubMed] [Google Scholar]
- 13.Taylor M, Ashcroft AT, Messenger AG. Cyclosporin A prolongs human hair growth in vitro. J Invest Dermatol. 1993;100:237–239. doi: 10.1111/1523-1747.ep12468979. [DOI] [PubMed] [Google Scholar]
- 14.Gupta AK, Ellis CN, Nickoloff BJ, Goldfarb MT, Ho VC, Rocher LL, et al. Oral cyclosporine in the treatment of inflammatory and noninflammatory dermatoses. A clinical and immunopathologic analysis. Arch Dermatol. 1990;126:339–350. [PubMed] [Google Scholar]
- 15.Gupta AK, Ellis CN, Cooper KD, Nickoloff BJ, Ho VC, Chan LS, et al. Oral cyclosporine for the treatment of alopecia areata. A clinical and immunohistochemical analysis. J Am Acad Dermatol. 1990;22:242–250. doi: 10.1016/0190-9622(90)70032-d. [DOI] [PubMed] [Google Scholar]
- 16.Kim BJ, Min SU, Park KY, Choi JW, Park SW, Youn SW, et al. Combination therapy of cyclosporine and methylprednisolone on severe alopecia areata. J Dermatolog Treat. 2008;19:216–220. doi: 10.1080/09546630701846095. [DOI] [PubMed] [Google Scholar]
- 17.Sharma VK, Dawn G, Kumar B. Profile of alopecia areata in Northern India. Int J Dermatol. 1996;35:22–27. doi: 10.1111/j.1365-4362.1996.tb01610.x. [DOI] [PubMed] [Google Scholar]
- 18.Chantal B, Jerry S. The treatment of alopecia areata. Dermatol Ther. 2001;14:306–316. [Google Scholar]
- 19.Weissmann I, Hofmann C, Wagner G, Plewig G, Braun-Falco O. PUVA-therapy for alopecia areata. An investigative study. Arch Dermatol Res. 1978;262:333–336. doi: 10.1007/BF00447370. [DOI] [PubMed] [Google Scholar]
- 20.Tosti A, De Padova MP, Minghetti G, Veronesi S. Therapies versus placebo in the treatment of patchy alopecia areata. J Am Acad Dermatol. 1986;15:209–210. doi: 10.1016/s0190-9622(86)70158-8. [DOI] [PubMed] [Google Scholar]
- 21.Gu SQ, Ros AM, Thyresson N, Wasserman J. Blood lymphocyte subpopulations and antibody dependent, cell-mediated cytotoxicity (ADCC) in alopecia areata and universalis. Acta Derm Venereol. 1981;61:125–129. [PubMed] [Google Scholar]
- 22.Giannetti A, Di Silverio A, Castellazzi AM, Maccario R. Evidence for defective T cell function in patients with alopecia areata. Br J Dermatol. 1978;98:361. doi: 10.1111/j.1365-2133.1978.tb06165.x. [DOI] [PubMed] [Google Scholar]
- 23.Lassus A, Kianto U, Johansson E, Juvakoski T. PUVA treatment for alopecia areata. Dermatologica. 1980;161:298–304. doi: 10.1159/000250381. [DOI] [PubMed] [Google Scholar]
- 24.Oliver RF, Lowe JG. Oral cyclosporin A restores hair growth in the DEBR rat model for alopecia areata. Clin Exp Dermatol. 1995;20:127–131. doi: 10.1111/j.1365-2230.1995.tb02669.x. [DOI] [PubMed] [Google Scholar]
- 25.Shapiro J, Lui H, Tron V, Ho V. Systemic cyclosporine and low-dose prednisone in the treatment of chronic severe alopecia areata: a clinical and immunopathologic evaluation. J Am Acad Dermatol. 1997;36:114–117. doi: 10.1016/s0190-9622(97)70342-6. [DOI] [PubMed] [Google Scholar]
- 26.Rosmarin DM, Lebwohl M, Elewski BE, Gottlieb AB National Psoriasis Foundation. Cyclosporine and psoriasis: 2008 National Psoriasis Foundation Consensus Conference. J Am Acad Dermatol. 2010;62:838–853. doi: 10.1016/j.jaad.2009.05.017. [DOI] [PubMed] [Google Scholar]


