Abstract
This study tested the hypothesis that adolescent-onset alcohol abuse (AOAA) would both mediate and moderate the effect of childhood conduct disorder on antisocial behaviour in late adolescence and early adulthood. A sample comprising 504 young men and women strategically recruited from the community were grouped using the criteria of the Diagnostic and Statistical Manual (DSM-IV, American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: APA), as follows: neither childhood conduct disorder (CCD) nor alcohol abuse/dependence; CCD but no alcohol abuse or dependence; alcohol abuse/dependence but no CCD; both CCD and alcohol abuse/dependence. The outcome measure was the sum of positive responses to 55 interview items capturing a variety of antisocial behaviours engaged in since age 15. Severity of lifetime alcohol-related and CCD problems served as predictor variables in regression analysis. Antisocial behaviour problems were greatest in individuals with a history of co-occurring conduct disorder (CD) and alcohol abuse/dependence. While CCD was strongly predictive of adult antisocial behaviour, this effect was both mediated and moderated (exacerbated) by AOAA.
Keywords: alcohol abuse, conduct disorder, antisocial behaviour
Introduction
It has long been documented that childhood conduct disorder (CCD) is a precursor of adult antisocial personality and behaviour (Kjelsberg, 2006), hence it is included in DSM-IV as a necessary condition for a diagnosis of antisocial personality disorder (APD; American Psychiatric Association [APA], 1994). However, as discussed below, the nature of the relationship between CCD and adult antisocial personality remains unclear, particularly in regard to what factors other than CCD are necessary for progression to adult antisocial personality.
A possible answer to this question was given in a hypothesis proposed by Howard (2006), according to which CCD initially leads to a progressive and accelerating use of alcohol and other drugs in adolescence. A vicious cycle then develops whereby increasing use of alcohol in adolescence results in increasing disinhibition and progressive misuse of alcohol. Exposure of the vulnerable adolescent brain to excessive amounts of alcohol and other substances putatively results in structural and functional changes in the brain, particularly in those prefrontal areas involved in emotional and behavioural self-regulation. As a consequence, on entering adulthood such individuals suffer deficits in self-regulation that place them at high risk of serious antisocial conduct.
Since this hypothesis was first proposed, evidence (reviewed below) has accrued to suggest that adolescent-onset alcohol abuse is a major risk factor for adult antisocial behaviour, including violence. Howard's (2006) hypothesis suggests that early-onset alcohol abuse is a critical intervening variable (as a mediator and/or as a moderator) in the relationship between conduct disorder (CD) and adult antisocial behaviour. This study set out to test the prediction that among a sample of young adults recruited from the community, those who engaged in the highest degree of antisocial behaviour in late adolescence and early adulthood would show a history of co-occurring CCD and adolescent-onset alcohol abuse (AOAA), and that AOAA would moderate and/or mediate the relationship between CCD and adult antisocial behaviour.
Adolescent-onset alcohol abuse is a risk factor for adult antisocial behaviour
Results from three longitudinal studies that have examined adolescent predictors of adult antisocial outcomes concur in showing that AOAA is an important risk factor for adult antisocial behaviour and violent offending in particular. In the Cambridge Study in Delinquent Development, heavy drinking at age 18 was one of the most important risk factors predicting which offenders would persist with crime after age 21 (Farrington, Ttofi, & Coid, 2009). In the Christchurch Health and Development Study, AOAA was found to predict violent offending both at the age groups of 15–21 and 21–25, even after controlling for confounding background and individual factors, including CCD (Wells, Horwood, & Fergusson 2004). In the Dunedin Multidisciplinary Health and Development Study, roughly one-half of male members of the birth cohort (1037 children born in 1972–1973 in Dunedin), who subsequently showed a pattern of life-course persistent antisocial behaviour, were alcohol dependent at age 18 (Moffitt, T. E., personal communication to first author). Consistent with this, studies have reported that measures of early alcohol use such as age of first drink were associated with heightened risk of delinquency and criminal behaviour and of disinhibitory psychopathology generally (Brems, Johnson, Neal, & Freemon, 2004; Zernicke, Cantrell, Finn, & Lucas, 2010). In a forensic sample of former adolescent psychiatric patients, younger age of onset of substance (including alcohol) abuse was significantly associated with later development of what the authors described as a complex personality disorder characterised by explosive and psychopathic traits (Gustavson et al., 2007). Consistent with this, AOAA has been found to be associated with APD (Bakken, Landheim, & Vaglum, 2004). In summary, therefore, AOAA appears to be an important risk factor for the adult manifestation of externalising, a predominantly heritable vulnerability that contributes to the development of diverse traits (e.g. rebelliousness, excitement seeking, problematic impulsivity) and problem behaviours including disinhibitory tendencies, antisocial deviance of different sorts and alcohol/drug problems (Krueger, Markon, Patrick, Benning, & Kramer, 2007).
Conduct disorder is a risk factor for adult antisocial behaviour
The association between CCD and adult antisocial behaviour has been well documented (Kjelsberg, 2006). Childhood-onset social and behavioural problems form the most relevant psychiatric symptom cluster in relation to pervasive adult violent behaviour (Soderstrom, Sjodin, Carlstedt, & Forsman, 2004). Despite its frequent co-morbidity with other childhood disorders, in particular Oppositional Defiant Disorder (ODD) and Attention Deficit-Hyperactivity Disorder (ADHD), CCD alone among these disorders was found to be associated with adult APD when psychiatric co-morbidity and other confounding factors were controlled (Fergusson, Boden, & Horwood, 2010).
Problems with the CCD/adult antisocial personality relationship
The nature of the CCD-adult antisocial personality relationship is problematic for at least three reasons. First, CCD appears to predispose to the development of a wide range of adult disorders (Kjelsberg, 2006) and to the entire spectrum of personality disorders rather than just APD (Bernstein, Cohen, Skodol, Bezirganian, & Brook, 1996; Blackburn, 2007). Second, although the rate of progression from CCD to adult APD has been estimated at around 50% (Kendall et al., 2009), variable rates of progression have been reported ranging from 30% (Burke, Waldman, & Lahey, 2010; Robins, 1978) to as high as 61% in adolescents with concurrent substance abuse problems (Myers, Stewart, & Brown, 1998). Third, it remains unclear to what extent the presence of CCD makes a clinically meaningful difference to adult antisocial personality. Past studies (e.g. Black & Braun, 1998) suggested that persons meeting only the adult criteria for APD suffer essentially the same disorder as those meeting both adult and child APD criteria (a DSM APD diagnosis requires that at least three of both child and adult criteria are met). This is questioned by results of two recent studies. First, Howard, Huband, and Duggan (in press) reported an association between severe CCD and adult antisocial personality when the latter co-occurred with borderline personality disorder. Second, results of a recent study highlighted the role played by CCD in serious adult antisocial behaviour, suggesting the existence of a clinically meaningful distinction between antisocial adults with and without antecedent childhood CD (Walters & Knight, 2010). As noted by these authors, research on the transition from CCD to adult antisocial personality is needed in order to clarify the relationship between them. Clearly factors other than CCD, including (as reviewed above) AOAA, are at play in determining a shift in the developmental trajectory towards APD.
The present study
The frequent co-occurrence of CCD and alcohol (and other drug) abuse makes it difficult to tease apart their separate and conjoint influence on adult antisocial behaviour (DeBrito & Hodgins, 2009). Notwithstanding, Finn et al. (2009) were able to identify, among a community sample of 477 young adults at high risk for drug and alcohol use, substantial numbers of individuals who, while meeting DSM diagnostic criteria for CCD, had no significant history of alcohol dependence or abuse. Other groups in the sample comprised those with a history of both CCD and early alcohol abuse/dependence; those with alcohol abuse/dependence only; and those with neither alcohol abuse/dependence nor CCD. In short, this sample presented with a wide range of symptoms in both the CD and alcohol abuse/dependence domains, while additionally showing a wide range of antisocial behaviours during late adolescence and early adulthood.
Here, we report the testing, in the Finn et al. (2009) sample, of three predictions arising from Howard's (2006) hypothesis that early-onset alcohol abuse is a critical intervening variable in the relationship between CD and adult antisocial behaviour. First, it was predicted that a group comprising those with co-occurring alcohol abuse/dependence and CCD would outscore those with a diagnosis of CCD alone on a measure of antisocial behaviours engaged in during late adolescence and early adulthood (since age 15). Second, consistent with the idea that AOAA is, at least in part, the mechanism through which CCD exerts its effect on adult antisocial behaviour, it was predicted that adolescent alcohol abuse would significantly mediate the influence of CCD on later antisocial behaviour. The third and final prediction was that adolescent alcohol abuse would moderate (i.e. exacerbate) the relationship between CCD and later antisocial behaviour.
Method
Participants
Details of recruitment are given in Finn et al. (2009) and will be briefly summarised. Participants were strategically recruited through advertisements placed in local newspapers and around the community, a relatively small mid-west American college town with about 100,000 residents in the county. The advertisements were designed to attract respondents who varied from low to high levels of impulsive and disinhibited traits and alcohol use, and to ensure sufficient variation and range in severity of lifetime problems with alcohol, marijuana, other drugs, CCD and adult antisocial behaviour. This approach has been effective in attracting responses from individuals varying in disinhibited traits and from alcohol dependent, antisocial, and generally disinhibited participants (Bauer & Hesselbrock, 1993; Finn, Mazas, Justus, & Steinmetz, 2002). The range of ads/flyers targeted `daring, rebellious, defiant individuals', `carefree, adventurous individuals who haveled exciting and impulsive lives', `impulsive individuals', `heavy drinkers wanted for psychological research', persons with a `drinking problem', persons who `got into a lot of trouble as a child', persons `interested in psychological research', `quiet, reflective and introspective persons' and `social drinkers'. Participants were initially screened by telephone and excluded from the study if they: (a) were not between 18 and 30 years of age; (b) could not read and speak English; (c) had never consumed alcohol; (d) had less than a 6th grade level of education; (e) reported having suffered from any serious head injury; (f) had a history of psychosis. Of 507 participants who underwent the diagnostic interview (see below), three decided to withdraw their data, resulting in a final sample size of 504.
The following groups were selected using DSM-IV criteria as per Finn et al. (2009): those with neither CD nor a history of alcohol abuse or dependency (neither CCD nor AA/D, N ¼ 112, 54 males); those with a history of CD but no alcohol abuse or dependency (CCD only, N ¼ 42, 20 males); those with a history of alcohol abuse or dependency but no history of CD (AA/D only, N ¼ 168, 93 males); and those with a history of both CCD and alcohol abuse or dependency (CCD þ AA/D, N ¼ 182, 104 males). It should be noted that, unlike in Finn et al (2009), participants with a history of alcohol abuse, in addition to those with alcohol dependence, were excluded from the control (neither CCD nor AA/D) and CCD only groups.
Assessment materials
Diagnostic interview
Participants were interviewed using the Semi-Structured Assessment for the Genetics of Alcoholism (SSAGA), a reliable and valid structured diagnostic interview originally developed for use in genetic linkage studies (Bucholz et al., 1994) and subsequently used in literally hundreds of studies of substance use and related disorders, such as ASPD and CCD (Finn et al., 2002, 2009; Henry et al., 2011; Hesselbrock, Easton, Bucholz, Schuckit, & Hesselbrock, 1999; Mazas, Finn, & Steinmetz, 2000; Meier, Slutsky, Heath, & Martin, 2011; Zernicke, et al., 2010). SSAGA has excellent reliability (inter-rater and test–retest) (e.g. Bucholz et al., 1994; Meier et al., 2011). Kappa reliability coefficients vary from .70–.90 for substance use disorders and .70–.75 for ASPD and CCD (Bucholz et al, 1994; Meier et al., 2011). The validity of the SSAGA has been demonstrated in a number of studies that have compared it with other diagnostic interviews (e.g. Hesselbrock et al. 1999) and have measured outcomes, core aspects of psychopathology, or genetic markers (e.g. Cao et al., 2011; Henry et al., 2011; Mazas et al., 2000). SSAGA was used to determine whether responses from potential participants satisfied DSM-IV (APA, 1994) criteria for AD, CCD, marijuana abuse/dependence and drug abuse/dependence. All diagnoses were based on standard DSM-IV (APA, 1994) criteria. Although multiple interviewers were not used, 25% of cases were selected whose SSAGA responses and diagnoses were checked by a second and third independent assessor. Any disagreement (approximately 3% of cases) was discussed with P.R.F. and a best-estimate diagnosis was ascertained in such cases. The severity of lifetime problems associated with alcohol use, childhood conduct, adult (since age 15) antisocial behaviour, marijuana dependence, marijuana use, and other drug use were measured by summing positive responses to relevant subsets of SSAGA questions in the respective diagnostic sections. The main outcome measure investigated here was antisocial behaviour engaged in since age 15,1 a broad category captured by positive responses to 55 interview items relating to a variety of antisocial behaviours. These included: fighting, bullying, causing physical injury, felony convictions, injuring animals, cheating, lying, stealing, forgery, breaking and entering, threats/use of force to obtain money, property damage, physical injury, pimping, dishonesty, failure to pay debts, abuse/neglect of children, neglect of work responsibilities, vagrancy, promiscuity/lack of fidelity, recklessness and anger proneness. Only when these items were endorsed as having occurred in the absence of concomitant alcohol or drug intoxication were they counted as positive responses. Positive responses to these 55 items were summed to give an antisocial problem count. Zernicke et al. (2010) found this measure to correlate positively with measures of drug and alcohol dependence and with personality measures of impulsivity and social deviance. It can therefore be said to tap the general externalising factor proposed to account for shared variance among diverse impulse control disorders within DSM and to be associated with problematic traits and behaviours, e.g. aggression, drug and alcohol use, impulsivity and excitement seeking (Krueger et al., 2007).
Assessment of intellectual functioning
Intellectual functioning was assessed using the Shipley Institute for Living Scale (Zachary, 1986). It comprises two sub-scales: a Vocabulary Test consisting of 40 items asking participants to underline the one word out of four which is most similar to the prompting word; and an Abstract Thinking Test consisting of 20 items asking participants to fill in each `blank' at the end of the line with a letter or number to complete the pattern. Pro-rated IQ was obtained from these scores.
Data analysis
Comparison of antisocial outcomes between the groups
The mean antisocial behaviour problem counts were calculated for each of the four groups. Due to the uneven group sizes, antisocial problem counts were compared between groups using a Mann–Whitney U test, notwithstanding limitations (e.g. lack of power) of using a non-parametric test to compare groups.
Investigating the relationships among conduct disorder, alcohol abuse/dependence and antisocial outcomes
Regression analyses were performed to investigate whether and to what degree alcohol abuse problems would account for significant variance in antisocial behaviour problems over and above that accounted for by CD. The Variance Inflation Factor (VIF) and tolerance statistics indicated that there was no undue collinearity within the data, with VIF values under 10 and tolerance values over 0.2 (Field, 2009). Moderation and/or mediation effects were examined using Modgraph-I2 (Jose, 2008) and Medgraph-I3 (Jose, 2003).
Results
Group antisocial problem behaviour counts
The mean antisocial behaviour problem counts for each of the groups are shown in Table 1. The lowest scores were obtained by those with neither a history of CD nor alcohol abuse/dependency: comparison of their mean score with each of the other three groups yielded significant difference in each case (all ps 5 .02, with Bonferroni correction for multiple comparisons). Critically, and in line with the hypothesis, the CCD þ AA/AD group showed the highest level of antisocial behaviour: their mean antisocial problem count was significantly (p 5 .001) higher than that of the CCD alone group.
Table 1.
Characteristics of the four groups.
| Group | ||||
|---|---|---|---|---|
|
| ||||
| NoCCD/noAA/D (N ¼ 112) | CCD-alone (N ¼ 42) | AA/D-alone (N ¼ 168) | CCD þ AA/D (N ¼ 182) | |
| Mean age (SD) | 21.2 (2.2) | 21.7 (3.1) | 22.0 (2.9) | 22.6 (3.2) |
| Mean Shipley IQ (SD) | 108.5 (8.2) | 104.5 (10.3) | 105.3 (7.7) | 102.4 (12.2) |
| Mean age of onset of alcohol abuse/dependency (SD) | -* | -* | 17.6 (2.4) | 15.9 (2.6) |
| Mean antisocial problem behaviour count (SD) | 3.20 (2.87) | 16.24 (6.97) | 11.42 (6.45) | 21.08 (7.21) |
| Mean alcohol abuse problem count (SD) | 2.99 (3.5) | 15.71 (14.76) | 34.07 (17.87) | 42.18 (17.16) |
| Mean conduct disorder problem count (SD) | 4.22 (3.47) | 17.52 (5.70) | 12.14 (5.43) | 20.21 (4.69) |
| Marijuana abuse problem count (SD) | 0.42 (2.54) | 9.33 (10.14) | 10.24 (11.51) | 17.15 (11.74) |
| Drug abuse problem count (SD) | 0.03 (0.28) | 16.88 (27.83) | 13.76 (26.18) | 25.80 (31.11) |
Notes: NoCCD/noAA/D ¼ a history of neither conduct disorder nor alcohol abuse or dependence; CCD-alone ¼ a history of childhood conduct disorder, AA/D-alone ¼ a history of alcohol abuse or dependence without a history of conduct disorder; CCD þ AA/D ¼ a history of childhood conduct disorder with a history of alcohol abuse or dependence.
Alcohol abuse/dependency was an exclusion criterion for these groups
Did adolescent alcohol abuse mediate between childhood conduct disorder and adult antisocial behaviour?
The question of whether alcohol abuse might mediate at least part of the relationship between CD and antisocial behaviour was examined next. Using MedGraph-I, a significant Sobel's z-score was obtained, z ¼ 5.54, p 5 .001, and the size of the indirect to total ratio indicated that about 12% of the total effect was explained by the indirect effect through alcohol abuse. This result suggested that a significant amount of the resulting antisocial behaviour could be predicted by individuals who initially displayed CD, and then engaged in subsequent alcohol use.
Did adolescent alcohol abuse moderate (i.e. exacerbate) the relationship between childhood conduct disorder and adult antisocial behaviour?
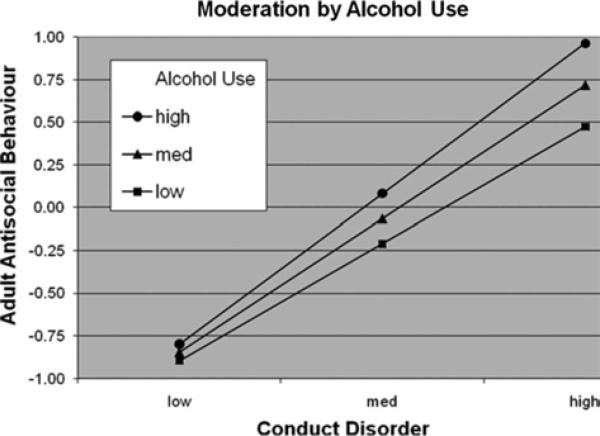
A further analysis was carried out to examine whether alcohol abuse might moderate the relationship between CD and antisocial behaviour. To this end, we used a regression-based moderation analysis (MacKinnon, 2008), following the recommendation that this be employed in cases where predictor variables are continuous (Cohen, Cohen, West, & Aiken, 2003). The person-based continuous variables of CD and alcohol abuse scores were centred before the interaction term was created. The regression analysis indicated that all three terms were significant predictors of adult antisocial behaviour: CD, b ¼ .78, p 5 .001; alcohol abuse, b ¼ .15, p 5 .001; and the interaction, b ¼ .10, p 5 .001. The interaction graphed by ModGraph-I is presented in Figure 1. The pattern indicates that alcohol abuse exercised an exacerbating effect on the CD to antisocial behaviour relationship. As may be seen from Figure 1, the group with the steepest slope was the high alcohol abuse group, signifying that for individuals with serious alcohol abuse levels, the relationship between CD problems and later antisocial behaviour problems was the strongest. Simple slope analyses verified that slope steepness increased with number of alcohol abuse problems: high AA slope ¼ .88, t ¼ 18.82, p 5 .001; medium AA slope ¼ .78, t ¼ 19.58, p 5 .001; and low AA slope ¼ .69, t ¼ 16.10, p 5 .001. It is notable that those with the highest levels of both alcohol abuse and CD problems showed the highest level of antisocial behaviour problems.
Figure 1.
The moderating effect of alcohol abuse on the relationship between conduct disorder and adult antisocial behaviour.
Notes: The measure of adult antisocial behaviour was standardised so that negative frequency counts were possible. The high, medium and low groups for both childhood conduct disorder and alcohol abuse were based on individuals falling one standard deviation above the mean, at the mean and one standard deviation below the mean, respectively (Aiken & West, 1991).
Discussion
While confirming results of previous studies indicating that CCD is a major influence on adult antisocial behaviour (Copeland, Miller-Johnson, Keeler, Angold, & Costello, 2007; Kratzer & Hodgins, 1997), results of the present study suggest that its effect is both to some degree mediated by, as well as moderated by, early-onset alcohol abuse. As predicted, the group characterised by a combination of CCD and alcohol abuse showed a level of antisocial problem behaviour that was significantly higher than that shown by those manifesting CCD alone. The moderation analysis indicated that problematic alcohol use added significantly to the variance in adult antisocial behaviour, over and above that accounted for by CCD alone, and that problematic alcohol use significantly amplified the effect of CCD on adult antisocial behaviour. It may be seen from Figure 1 that the combination of childhood conduct problems and early-onset alcohol abuse appeared to place individuals at the highest risk of adult antisocial behaviour.
Inspection of Table 1 indicates that the AA/D-alone group's antisocial problem count was roughly three times higher than that of the control (noCCD/noAA/D) group, confirming that AOAA increases the risk of adult antisocial behaviour even in the absence of CCD (Farrington et al., 2009; Wells et al., 2004). Evidence further suggests that progression from CCD to adult APD depends on co-morbidity with other disorders, and with co-morbid substance abuse in particular (Myers et al., 1998). While the literature clearly indicates that CCD is a powerful antecedent of adult antisocial personality in general (Copeland, Shanahan, Costello, & Angold, 2009), and of adult violence in particular (Fergusson et al., 2010; Soderstrom et al., 2004), nonetheless its presence does not guarantee progression to APD at age 18 and beyond. The current results suggest that AOAA is a critical factor in determining that the developmental trajectory points towards APD as the final adult outcome.
The present results are consistent with evidence linking AOAA both with APD (Bakken et al., 2004) and with a range of variables associated with the adult manifestation of externalising, including violent recidivism and life-time aggression (Gustavson et al., 2007). Consistent with Howard's (2006) hypothesis that early-onset alcohol abuse is a critical factor in the development of adult antisocial behaviour, results further suggest that CCD and adolescent alcohol abuse exert both independent and interactive effects on the development of adult antisocial behaviour. This hypothesis further proposed that by impairing the function of prefrontal cortex during adolescence, a critical period in its development, AOAA leads to deficits in the neuropsychological substrates of goal-directed behaviour and emotional self-regulation, leading to chronic antisocial behaviour in adulthood (Howard, 2009). While evidence suggests that adolescent alcohol abuse results in structural changes in the brain (De Bellis et al., 2005, 2008), it will need to be demonstrated that these changes are causally related to adult antisocial behaviour.
Limitations of the research
Several caveats should be mentioned here to aid in the careful evaluation of the present study's findings. First, in our regression analysis, following inspection of the residuals some concerns were raised regarding how well the model fitted the sample data. The pattern of residuals indicated that 1.2% of the cases had standardised residuals with absolute values greater than 2.58, a value in excess of that expected in a normal distribution. Whilst the Cook's distances, Mahalanobis distances and DFBeta values did not raise any concerns about the influence of individual cases, eight of the cases had leverage values over the recommended cut off point (0.003). Inspection of the problem counts for CD, alcohol abuse/dependence and antisocial behaviour for these eight individuals indicated that some of the sample deviated substantially from the model; most commonly, some had very high alcohol abuse but low or average antisocial behaviour. The presence of these individuals suggests that there may be protective factors for some people who abuse alcohol that prevent them from engaging in antisocial behaviour. Low trait impulsivity might be one such protective factor and interestingly inspection of these eight individuals' impulsivity scores (Eysenck & Eysenck, 1977) revealed that two of them had very low impulsivity scores (6 or less).
Second, it is clear from inspection of Table 1 that the combination of CCD with AOAA, compared with each considered singly, was associated with substance abuse problems in general, including problems with marijuana abuse. It is possible, indeed likely, that alcohol abuse may have acted in synergy with abuse of other substances to exert detrimental effects in terms of subsequent antisocial behaviour. Moreover, since adult antisocial behaviour was here – somewhat liberally but in keeping with the DSM-IV definition of adult antisocial behaviour – defined as that occurring since age 15, alcohol abuse will undoubtedly have overlapped in time with engagement in antisocial behaviour. Nonetheless, behaviours associated with drug or alcohol intoxication were excluded from the antisocial behaviour problem count, and results of moderation analysis using MedGraph analysis clearly indicated that the effect of CCD on antisocial problem count was significantly mediated by subsequent alcohol abuse. This suggests that the outcome (antisocial behaviour) was consequent upon prior alcohol abuse.
Third, the study was cross-sectional and assessment of symptoms was retrospective, and therefore relied on interviewees being truthful in their responses and accurate in their recollections. This applies particularly to assessment of individuals' alcohol abuse history and their CCD symptoms. It has previously been noted that self-report can result in both false-positive and false-negative errors, particularly for recalled childhood behaviours (Rueter, Chao, & Conger, 2000).
Fourth, this study has not considered the possibility that other personality disorders could have co-occurred with antisocial personality in this sample, particularly in those individuals characterised by both CCD and AOAA who showed the highest level of adult antisocial behaviour. Co-morbidity of borderline personality disorder is particularly relevant here, since adult antisocial behaviour has been reported to be associated with greater severity of CD symptoms when it co-occurs with borderline personality disorder than when it occurs in the absence of such co-morbidity (Howard et al., in press). It would therefore be reasonable to suppose that, had borderline symptoms been examined in the current sample, greater borderline pathology might have been found in the CD þ AOAA group. This would have implications for the development of antisocial behaviour. It might suggest, for example, that CCD combined with AOAA pushes the developmental trajectory towards an adult outcome of APD/borderline co-morbidity. While this suggestion is speculative, it is consistent with evidence that early-onset alcohol abuse is associated with both APD and borderline personality disorder (Gustavson et al., 2007; Thatcher, Cornelius, & Clark, 2005).
A final limitation of this study is that it examined the effect of only two variables, CCD and AOAA, on the antisocial outcome. While this was consistent with testing the hypothesis at hand, it must of course be admitted that the effects on antisocial behaviour of many other relevant variables were neglected (e.g. psychosocial: Farrington, 2010). Moreover, Howard's (2006) hypothesis needs to be broadened to take account of findings suggesting that exposure to alcohol at earlier developmental stages can exert detrimental effects that predispose to disordered conduct in childhood, e.g. through a binge pattern of maternal alcohol consumption (Sayal et al., 2009). Clearly, the factors posited in this hypothesis are but a small part of a much larger picture in which exposure of the developing brain to excessive amounts of alcohol, from conception through adolescence, may place the individual at increased risk of engaging in antisocial behaviour as an adult.
Implications
Notwithstanding its limitations, results of this study have two significant implications. Firstly, it has been suggested that greater understanding of subgroups within the broad category of antisocial children might assist in devising and targeting interventions (Hill, 2003). In so far as early-onset alcohol use has been shown here to exacerbate the effect of CCD on adult antisocial behaviour, conduct disordered children who show incipient signs of excessive alcohol use should be particularly targeted for early intervention to prevent progression of their alcohol use to abuse and dependence. Secondly, since AOAA will often be present in the history of antisocial individuals, results of studies claiming to show that antisocial/psychopathic samples, in comparison with controls, differ on measures of brain structure or function should be interpreted with great caution. Findings claiming to find structural differences between antisocial and control samples typically do not take account of a history of early alcohol abuse (e.g. Raine, Lee, Yang, & Colletti, 2010). Any abnormality in brain structure or function found in adult antisocial samples could be attributable either to hereditary, congenital or early brain trauma factors, or to the effects of early exposure to alcohol, or indeed to both (McMurran & Howard, 2009).
Conclusion
These results generally support the hypothesis that early-onset alcohol abuse interacts with CCD in the genesis of adult antisocial behaviour (Howard, 2006, 2009). Further work will be required to verify that both CCD and adolescent alcohol abuse exert their conjoint effects by impairing brain substrates of emotional and behavioural self-regulation.
Acknowledgements
The authors are grateful to Jesolyn Lucas, Data Manager in the Department of Psychological and Brain Sciences, Indiana University, for help with providing relevant data. This research was supported by a NIH/NIAAA grant # R01 AA13650 to Peter R Finn.
Footnotes
Antisocial behaviour since age 15 was adopted in conformity with the DSM-IV definition of adult antisocial behaviour (APA, 1994).
Modgraph is a programme that allows entry of statistical information obtained from multiple regression output in order to compute the equations that yield cell means necessary for the graphical display of statistical interactions.
Medgraph is a programme designed to use statistical information generated from multiple regression analyses about covariance relationships among three variables to compute whether statistically significant mediation (using the Sobel's formula) has been obtained.
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Sage; Newbury Park, CA: 1991. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. APA; Washington, DC: 1994. [Google Scholar]
- Bakken K, Landheim AS, Vaglum P. Early and late onset groups of substance misusers: Differences in primary and secondary psychiatric disorders. Journal of Substance Use. 2004;9:224–234. [Google Scholar]
- Bauer LO, Hesselbrock VM. EEG, autonomic and subjective correlates of the risk for alcoholism. Journal of Studies on Alcohol. 1993;54:577–589. doi: 10.15288/jsa.1993.54.577. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Cohen P, Skodol A, Bezirganian S, Brook JS. Childhood antecedents of adolescent personality disorders. American Journal of Psychiatry. 1996;153:907–913. doi: 10.1176/ajp.153.7.907. [DOI] [PubMed] [Google Scholar]
- Black DW, Braun D. Antisocial patients: a comparison of those with and those without childhood conduct disorder. Annals of Clinical Psychiatry. 1998;10:53–57. doi: 10.1023/a:1026110915087. [DOI] [PubMed] [Google Scholar]
- Blackburn R. Personality disorder and antisocial deviance: Comments on the debate on the structure of the psychopathy checklist-revised. Journal of Personality Disorders. 2007;21:142–159. doi: 10.1521/pedi.2007.21.2.142. [DOI] [PubMed] [Google Scholar]
- Brems C, Johnson M, Neal D, Freemon M. Childhood abuse history and substance use among men and women receiving detoxification services. American Journal of Drug and Alcohol Abuse. 2004;30:799–821. doi: 10.1081/ada-200037546. [DOI] [PubMed] [Google Scholar]
- Bucholz KK, Cadoret R, Cloninger CR, Dinwiddie SH, Hesselbrock VM, Nurnberger JI, Jr., Schuckit MA. A new, semi-structured psychiatric interview for use in genetic linkage studies: A report on the reliability of the SSAGA. Journal of Studies on Alcohol. 1994;55:149–158. doi: 10.15288/jsa.1994.55.149. [DOI] [PubMed] [Google Scholar]
- Burke JD, Waldman I, Lahey BB. Predictive validity of childhood oppositional disorder and conduct disorder: Implications for the DSM-V. Journal of Abnormal Psychology. 2010;119:739–751. doi: 10.1037/a0019708. doi:10.1037/a0019708. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3rd ed. Lawrence Erlbaum Associates; Mahway, NJ: 2003. [Google Scholar]
- Cao J-X, Hu JY, Xiang-Mei X, Yian Haile CA, Kosten TR, Zhang XY. Association between the 5-HTR1B gene polymorphisms and alcohol dependence in a Han Chinese population. Brain Research. 2011;1376:1–9. doi: 10.1016/j.brainres.2010.12.039. [DOI] [PubMed] [Google Scholar]
- Copeland WE, Miller-Johnson S, Keeler G, Angold A, Costello EJ. Childhood psychiatric disorders and young adult crime: A prospective, population-based study. American Journal of Psychiatry. 2007;164:1668–1675. doi: 10.1176/appi.ajp.2007.06122026. [DOI] [PubMed] [Google Scholar]
- Copeland WE, Shanahan L, Costello EJ, Angold A. Childhood and adolescent psychiatric disorders as predictors of young adult disorders. Archives of General Psychiatry. 2009;66:764–772. doi: 10.1001/archgenpsychiatry.2009.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Bellis MD, Van Voorhees E, Hooper SR, Gibler N, Nelson L, Hege SG, MacFall J. Diffusion tensor measures of the corpus callosum in adolescents with adolescent onset alcohol use disorders. Alcohol:. Clinical and Experimental Research. 2008;32:395–404. doi: 10.1111/j.1530-0277.2007.00603.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Bellis MO, Narasimhan A, Thatcher DL, Kashavan MS, Soloff P, Clark DB. Prefrontal cortex, thalamus, and cerebellar volumes in adolescents and young adults with adolescent-onset alcohol use disorders and comorbid mental disorders. Alcoholism: Clinical and Experimental Research. 2005;27:1590–1600. doi: 10.1097/01.alc.0000179368.87886.76. [DOI] [PubMed] [Google Scholar]
- DeBrito SA, Hodgins S. Antisocial personality disorder. In: McMurran M, Howard RC, editors. Personality, personality disorder and violence. John Wiley & Sons Ltd.; Chichester: 2009. pp. 133–153. [Google Scholar]
- Eysenck SB, Eysenck HJ. The place of impulsiveness in a dimensional system of personality description. British Journal of Social and Clinical Psychology. 1977;16:57–68. doi: 10.1111/j.2044-8260.1977.tb01003.x. [DOI] [PubMed] [Google Scholar]
- Farrington DP. The developmental evidence base: Psychosocial research. In: Towl GJ, Crighton DA, editors. Forensic psychology. Blackwell Publishing Ltd.; Oxford: 2010. pp. 113–132. [Google Scholar]
- Farrington DP, Ttofi MM, Coid JW. Development of adolescence-limited, late-onset, and persistent offenders from age 8 to age 48. Aggressive Behavior. 2009;35:150–163. doi: 10.1002/ab.20296. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Boden JM, Horwood J. Classification of behaviour disorders in adolescence: Scaling methods, predictive validity, and gender differences. Journal of Abnormal Psychology. 2010;119:699–712. doi: 10.1037/a0018610. [DOI] [PubMed] [Google Scholar]
- Field A. Discovering statistics using SPSS. 3rd ed. Sage Publications Ltd.; London: 2009. [Google Scholar]
- Finn PR, Mazas C, Justus A, Steinmetz JE. Early-onset alcoholism with conduct disorder: go/no-go learning deficits, working memory capacity, and personality. Alcoholism: Clinical and Experimental Research. 2002;26:186–206. [PubMed] [Google Scholar]
- Finn PR, Rickert ME, Miller MA, Lucas J, Bogg T, Bobova L, Cantrell H. Reduced cognitive ability in alcohol dependence: Examining the role of covarying externalizing psychopathology. Journal of Abnormal Psychology. 2009;118:100–116. doi: 10.1037/a0014656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustavson C, Stahlberg O, Sjodin A-K, Forsman A, Nilsson T, Anckarsater H. Age at onset of substance abuse: A crucial covariate of psychopathic traits and aggression in adult offenders. Psychiatry Research. 2007;153:195–198. doi: 10.1016/j.psychres.2006.12.020. [DOI] [PubMed] [Google Scholar]
- Henry KL, McDonald JN, Oetting ER, Silk Walker P, Walker RD, Beauvais F. Age of onset of first alcohol intoxication and subsequent alcohol use among urban American Indian adolescents. Psychology of Addictive Behaviors. 2011;25:48–56. doi: 10.1037/a0021710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hesselbrock M, Easton C, Bucholz KK, Schuckit M, Hesselbrock V. A validity study of the SSAGA – A comparison with the SCAN. Addiction. 1999;94:1361–1370. doi: 10.1046/j.1360-0443.1999.94913618.x. doi:10.1046/j.1360-0443.1999.94913618. [DOI] [PubMed] [Google Scholar]
- Hill J. Early identification of individuals at risk for antisocial personality disorder. British Journal of Psychiatry Supplement. 2003;44:S11–S14. doi: 10.1192/bjp.182.44.s11. [DOI] [PubMed] [Google Scholar]
- Howard RC. How is personality disorder linked to dangerousness? A putative role for early-onset alcohol abuse. Medical Hypotheses. 2006;67:702–708. doi: 10.1016/j.mehy.2006.03.050. [DOI] [PubMed] [Google Scholar]
- Howard RC. The neurobiology of affective dyscontrol: Implications for understanding `dangerous and severe personality disorder'. In: McMurran M, Howard RC, editors. Personality, personality disorder and violence. J. Wiley & Sons; Chichester: 2009. pp. 157–174. [Google Scholar]
- Howard RC, Huband N, Duggan C. Adult antisocial syndrome with co-morbid borderline pathology: Association with severe childhood conduct disorder. Annals of Clinical Psychiatry. 2011 [PubMed] [Google Scholar]
- Jose PE. ModGraph-I: A programme to compute cell means for the graphical display of moderational analyses: The internet version. Version 2.0. Victoria University of Wellington; Wellington, New Zealand: 2008. Retrieved from http://www.victoria.ac.nz/psyc/staff/paul-jose-files/modgraph/modgraph.php. [Google Scholar]
- Jose PE. MedGraph-I: A programme to graphically depict mediation among three variables: The internet version. version 2.0. Victoria University of Wellington; Wellington, New Zealand: 2003. Retrieved from http://www.victoria.ac.nz/staff/paul-jose-files/medgraph/medgraph.php. [Google Scholar]
- Kendall T, Pilling S, Tyrer P, Duggan C, Burbeck R, Meader N, Taylor C. Borderline and antisocial personality disorders: Summary of NICE guidance. British Medical Journal. 2009;338:93. doi: 10.1136/bmj.b93. doi:10.1136/bmj.b93. [DOI] [PubMed] [Google Scholar]
- Kjelsberg E. Exploring the link between conduct disorder in adolescence and personality disorders in adulthood. Psychiatric Times. 2006;23:22–24. [Google Scholar]
- Kratzer L, Hodgins S. Adult outcomes of child conduct problems: A cohort study. Journal of Abnormal Child Psychology. 1997;25:65–81. doi: 10.1023/a:1025711525255. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Markon KE, Patrick CJ, Benning SD, Kramer MD. Linking antisocial behavior, substance use, and personality: An integrative quantitative model of the adult externalizing spectrum. Journal of Abnormal Psychology. 2007;116:645–666. doi: 10.1037/0021-843X.116.4.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP. Introduction to statistical mediation analysis. Lawrence Erlbaum Associates; New York, NY: 2008. [Google Scholar]
- Mazas CA, Finn PR, Steinmetz JE. Decision-making biases, antisocial personality, and early-onset alcoholism. Alcoholism: Clinical and Experimental Research. 2000;24:1036–1040. [PubMed] [Google Scholar]
- McMurran M, Howard RC. Personality, personality disorder and violence: Implications for future research. In: McMurran M, Howard RC, editors. Personality, personality disorder and violence. J. Wiley & Sons; Chichester: 2009. pp. 299–311. [Google Scholar]
- Meier MH, Slutsky WS, Heath AC, Martin NG. Sex differences in the genetic and environmental influences on childhood conduct disorder and adult antisocial behavior. Journal of Abnormal Psychology. 2011;120:377–388. doi: 10.1037/a0022303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers MG, Stewart DG, Brown SA. Progression from conduct disorder to antisocial personality disorder following treatment for adolescent substance abuse. American Journal of Psychiatry. 1998;155:479–485. doi: 10.1176/ajp.155.4.479. [DOI] [PubMed] [Google Scholar]
- Raine A, Lee L, Yang Y, Colletti P. Neurodevelopmental marker for limbic maldevelopment in antisocial personality disorder and psychopathy. British Journal of Psychiatry. 2010;197:186–192. doi: 10.1192/bjp.bp.110.078485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins LN. Sturdy childhood predictors of antisocial behaviour: Replications from longitudinal studies. Psychological Medicine. 1978;8:611–622. doi: 10.1017/s0033291700018821. [DOI] [PubMed] [Google Scholar]
- Rueter MA, Chao W, Conger RD. The effect of systematic variation in retrospective conduct disorder reports on antisocial personality disorder diagnoses. Journal of Consulting and Clinical Psychology. 2000;68:307–312. [PubMed] [Google Scholar]
- Sayal K, Heron J, Golding J, Alati R, Smith GD, Gray R, Emond A. Binge pattern of alcohol consumption during pregnancy and childhood mental health outcomes: Longitudinal population-based study. Pediatrics. 2009;123:289–296. doi: 10.1542/peds.2008-1861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soderstrom H, Sjodin A-K, Carlstedt A, Forsman A. Adult psychopathic personality with childhood-onset hyperactivity and conduct disorder: A central problem constellation in forensic psychiatry. Psychiatry Research. 2004;121:271–280. doi: 10.1016/s0165-1781(03)00270-1. [DOI] [PubMed] [Google Scholar]
- Thatcher DL, Cornelius JR, Clark DB. Adolescent alcohol use disorders predict borderline personality. Addictive Behaviors. 2005;30:1709–1724. doi: 10.1016/j.addbeh.2005.07.008. [DOI] [PubMed] [Google Scholar]
- Walters GD, Knight RA. Antisocial personality disorder with and without antecedent conduct disorder: Does it make a difference? Journal of Personality Disorders. 2010;24:258–271. doi: 10.1521/pedi.2010.24.2.258. [DOI] [PubMed] [Google Scholar]
- Wells JE, Horwood LJ, Fergusson DM. Drinking patterns in mid-adolescence and psychosocial outcomes in late adolescence and early adulthood. Addiction. 2004;99:1529–1541. doi: 10.1111/j.1360-0443.2004.00918.x. [DOI] [PubMed] [Google Scholar]
- Zachary RA. Shipley Institute of Living Scale: Revised manual. Western Psychological Services; Los Angeles, CA: 1986. [Google Scholar]
- Zernicke KA, Cantrell H, Finn PR, Lucas J. The association between earlier age of first drink, disinhibited personality, and externalizing psycho-pathology in young adults. Addictive Behaviors. 2010;35:414–418. doi: 10.1016/j.addbeh.2009.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]