Abstract
Azoospermia due to obstructive and non-obstructive mechanisms is a common manifestation of male infertility accounting for 10-15% of such cases. Known genetic factors are responsible for approximately 1/3 of cases of azoospermia. Nonetheless, at least 40% of cases are currently categorized as idiopathic and may be linked to unknown genetic abnormalities. It is recommended that various genetic screening tests are performed in azoospermic men, given that their results may play vital role in not only identifying the etiology but also in preventing the iatrogenic transmission of genetic defects to offspring via advanced assisted conception techniques. In the present review, we examine the current genetic information associated with azoospermia based on results from search engines, such as PUBMED, OVID, SCIENCE DIRECT and SCOPUS. We also present a critical appraisal of use of genetic testing in this subset of infertile patients.
Keywords: Azoospermia, Male Infertility, Genetic Testing, Genetic Diseases, Klinefelter Syndrome, Y Chromosome
INTRODUCTION
Infertility refers to failure of a couple to conceive following 12 months of unprotected regular intercourse, and this problem affects 10-15% of couples in the United States (1). Male factor infertility is partially or fully responsible for approximately 30-55% of cases of infertility (2,3). It was recently reported that 1 in 13 men of reproductive age requests medical assistance to have a child (4). Azoospermia, which is the complete absence of sperm in the ejaculate, accounts for 10-15% of male infertility cases and generally affects 1% of the male population (3,5,6). Azoospermia is divided into two major categories: obstructive azoospermia (OA), in which there is genital tract outflow obstruction, blocking passage of the sperm, and non-obstructive azoospermia (NOA), in which the testicle fails to produce mature sperm in the ejaculate. Although some reports indicate a higher incidence of NOA than OA (60 vs. 40%) (6) and (85.2 vs. 12.9%) (7), others have reported the opposite. (8). Genetic factors explain 21-29% of azoospermia (9), whereas 12-41% of azoospermic cases are idiopathic and most likely related to unknown genetic factors (7). Using a series of advanced diagnostic and assisted reproduction therapeutic tools, clinical pregnancy and live birth rates were reported to range from 26-57% and 18-55% for NOA and OA, respectively (10-16).
Azoospermia of a genetic origin is primarily caused by a wide array of genetic disorders, such as chromosomal abnormalities, monogenic disorders, multifactorial genetic diseases, and epigenetic disorders. These conditions constitute the genetic basis of reproductive failure. Table 1) summarizes the genetic basis of azoospermia at the post-testicular (obstructive azoospermia), pre-testicular and testicular (non-obstructive azoospermia) levels. The aim of this article is to review the genetic causes of azoospermia and to critically appraise the available types of genetic testing and the utility of such tests for the diagnosis and management of azoospermic males.
Table 1.
Genetic diseases and abnormalities that result in azoospermia at the post-testicular (obstructive azoospermia), pre-testicular and testicular (non-obstructive azoospermia) levels.
| Obstructive Azoospermia of Genetic Origin |
| Cystic Fibrosis |
| Congenital Bilateral Absence of the Vas Deferens |
| Congenital Unilateral Absence of the Vas Deferens (CUAVD) |
| Congenital Bilateral Epididymal Obstruction and Normal Vasa |
| Young Syndrome |
| Nonobstructive Azoospermia of Genetic Origin |
| Genetic Pre-testicular Causes of NOA |
| Hypothalamic HH |
| Congenital HH |
| Adult-onset genetic hypothalamic HH |
| Pituitary Disorders Associated with Hypogonadism |
| Generalized anterior pituitary hormone deficiency |
| Selective gonadotropin deficiency |
| Genetic Testicular Disorders |
| Affecting Spermatogenesis and Androgen Production |
| Klinefelter syndrome |
| XX male syndrome |
| Mutation in X-linked USP 26 |
| X-linked SOX3 mutation |
| Bilateral anorchia |
| Noonan syndrome |
| 45 X/46XY mosaicism (mixed gonadal dysgenesis) |
| Affecting Spermatogenesis |
| Y chromosome microdeletion |
| Autosome translocations |
| Monogenic disorders |
| Multifactorial disorders (e.g., cryptorchidism) |
| Affecting Androgen Production or Action |
| Androgen receptor mutation |
| Steroidogenic acute regulatory protein StAR mutation |
| 3BHSD type 2 deficiency |
| SRD5A2 mutation |
| Dysfunctional Cell Regulatory Pathways |
| Epigenetic Defects |
| Genetic Abnormities at the Primordial Germ Cell Level |
OBSTRUCTIVE AZOOSPERMIA OF GENETIC ORIGIN
Obstructive azoospermia comprises the genetic and acquired diseases that cause the obstruction of the reproductive tract pathway. The genetic causes of OA account for approximately 30% of cases (17). In a study that evaluated 179 men with OA, congenital bilateral absence of the vas deferens (CBAVD) was the most frequent condition linked to genetic abnormalities (17). Four genetic post-testicular diseases have been characterized and are described below. Young syndrome is another condition that is associated with OA and that may have a genetic background. Nevertheless, no definitive causative mutations have been discovered.
Cystic fibrosis
Cystic fibrosis (CF) is a life-threatening autosomal recessive disease that affects 1/2,500 Caucasian newborns and has a carrier frequency of 4% (18). CF is characterized by the presence of thick and viscid secretions in the lungs, pancreas, intestines, and liver. Such abnormal secretions result in the formation of plugs that obstruct the ductal lumens in these organs, causing dilatations, frequent infections, and fibrosis. The cause of the viscid secretions is a failure of epithelial cells to transport chloride, sodium ions and water to the lumen of the epithelial tubes. This failure is due to a mutation in the cystic fibrosis transmembrane conductance regulator (CFTR) gene, which encodes a chloride channel protein.
The CFTR gene is located on chromosome 7 q31.2 (19) and has been implicated in the formation of excurrent seminal ducts (20). The CFTR gene is 190 kb in length and consists of 27 exons. Over 1,800 mutations in this gene have been reported (20). The CFTR protein is a glycosylated transmembrane ATPase protein that functions as a plasma membrane channel for sugars, peptides, inorganic phosphate, chloride, and metal cations. CFTR is expressed in the epithelial cells of exocrine tissues, such as the lungs, the pancreas, sweat glands, the head of the epididymis and the vas deferens. This protein is composed of 1,480 amino acids and has a molecular weight of 168,173 Da. Several reports noted the role of CFTR in sperm maturation in the epididymis, as this protein is necessary for fluid absorption and the facilitation of sperm capacitation and fertilization ability (21-23).
The level of functionally active CFTR protein determines the clinical phenotypes of CFTR mutations. Normal individuals should have an active CFTR protein level of 50-100%, whereas individuals with CF exhibit CFTR activity that is lower than 10% of normal levels (24). Only 2-3% of men with classic CF are fertile, and the majority are infertile (98%) due to congenital bilateral absence or atresia of the vas deferens, which results in azoospermia (25). Epididymal malformations are also common manifestation of CF and are characterized by the absence of the body and tail and blind-ended efferent ductules. Seminal vesicles in these men exhibit a spectrum of anomalies, ranging from atresia, hypoplasia and cystic dilatation. Obstructed ejaculatory ducts are also common. Patients with CF may exhibit varying combinations of these abnormalities.
In most patients with CF, testicular histology indicates normal spermatogenesis. A subset of patients, however, exhibit impaired spermatogenesis, and such impairment may be attributed to the role of the CFTR protein in gametogenesis (26,27). Abnormal sperm morphology has also been described. It is attributed to defective spermiogenesis due to a lack of CFTR protein, which is also expressed in spermatozoa (28). The vast majority of patients with CF carry two major mutations in chromosome 7 (88%), whereas 11% exhibit compound heterozygous mutations, consisting of a severe mutation in one chromosome and a mild mutation in the other (18,29). The types of severe mutations that are frequently encountered in patients with CF encompass F508del (30%), G542X (3.4%) and G551D (2.4%) (30). The prevalence of these specific mutations vary with the ethnic background of the patient. For example, ▵F508 is the most common mutation in 70-90% of men with CF in North America and Northern Europe, compared with 50% in Southern Europe and less than 30% in Asians and Indians (31). CFTR mutations are also implicated in isolated seminal duct abnormalities. These abnormalities are referred to as primary genital or atypical forms of CF.
Congenital bilateral absence of the vas deferens
The congenital bilateral absence of the vas deferens (CBAVD) invariably results in azoospermia. CFTR is mutated in 60-90% of patients with CBAVD (32). CBAVD accounts for at least 6-25% of cases of obstructive azoospermia and approximately 2% of infertility cases (33,34). Men with CBAVD generally exhibit either a single or two mild mutations in the CFTR gene (12%) or a combination of a severe and a mild mutation (88%) (18,35,36). Five patterns of CFTR mutations have been described: i) class I, which is characterized by a defect in protein synthesis, with a premature termination that results in a nonsense or truncated protein; ii) class II, which is caused by a defect in protein processing and localization of CFTR protein to the apical plasma membrane, e.g., ΔF508; iii) class III, which is characterized by a defect in cAMP regulation of the channel opening, e.g., G551D (replacement of glycine with aspartic acid at position 551); iv) class IV, which is caused by a partial decline in chloride conductance; and v) class V, which is characterized by reduced levels of functional CFTR protein. Classes I, II and III have been associated with a complete lack of functional CFTR and severe CF manifestations, including pancreatic insufficiency. Class IV and V mutations cause a mild CF phenotype due to residual CFTR protein activity. Men with compound heterozygosity (i.e., a mild and a severe mutation, such as ΔF508) may have either CBAVD or a mild form of CF.
The common CFTR mutations found in men with CBAVD are the following: i) ΔF508, in which the three nucleotides that encode the phenylalanine at position 508 are missing in the protein's amino acid sequence. ΔF508 is a class II mutation observed in 21-40% of men with CBAVD; ii) polymorphisms within intron 8 (5T, 7T). Such polymorphisms reduce the production of the CFTR protein, resulting in a reduction in the splicing efficiency of the CFTR gene (accounts for 19-37% of CBAVD cases); iii) a missense R117H mutation in exon 4 (14% of CBAVD cases); and iv) a combination of ΔF508/R117H, which represents the most common mutation in patients with CBAVD (40%) (36,37).
A recent meta-analysis by Yu et al. revealed that 78% of men with CBAVD carry a minimum of one CFTR mutation. In the aforementioned study, 46% and 28% of men carried two mutations and a single mutation, respectively (38). Moreover, compound heterozygous ΔF508/5T and ΔF508/R117H mutations were present in 17% and 4% of CBAVD cases, respectively. The three most common mutations are 5T (25%), ΔF508 (17%), and R117H (3%) (38). Non-Caucasian men exhibit a higher incidence of single rather than double mutations (68 vs. 50%, p = 0.012), a higher frequency of 5T mutations (31 versus 20%, p = 0.009) and a lower frequency of ÄF508 mutations (8 versus 22%, p = 0.001) compared with Caucasian men (38).
Intracytoplasmic sperm injection (ICSI) is a useful method for the treatment of azoospermic men with the CFTR mutation. Partners who both carry the mutation should be advised to have a preimplantation genetic diagnosis (PGD) performed to avoid passing the abnormality to their offspring (39).
Congenital unilateral absence of the vas deferens (CUAVD)
This condition affects 0.5-1.0% of the male population and represents a heterogeneous disorder with respect to its etiology and clinical presentations. Whereas most men with CUAVD are fertile, a subgroup exhibits azoospermia or oligozoospermia. In the embryonic period, the vas deferens arises from the mesonephric duct. At the 7th week of development, this duct gives rise to the ureteric bud, which in turn induces the development of the kidney from the metanephros. An embryological insult to a single mesonephric duct at or prior to the seventh week of development can result in unilateral vasal aplasia and ipsilateral renal agenesis. It has been estimated that 79% of individuals with CUAVD have an absent ipsilateral kidney (40).
CFTR mutations have been observed in men with CUAVD who exhibit no renal agenesis. Kolettis et al. reported either single CFTR mutations, such as Negative/621_G-T, or compound heterozygous mutations, such as ΔF508/5T and ΔF508/7T/9T, in three out of four men with CUAVD and a distally obstructed contralateral vas deferens. The fourth patient, who was negative for a CFTR mutation, exhibited contralateral renal agenesis (41). In the aforementioned series, none of six men with CUAVD and patent contralateral vas exhibited mutations in the CFTR gene, although three of these patients had ipsilateral renal agenesis (41). Other authors have reported that CFTR mutations may be observed even in men with CUAVD who have normal patent contralateral vas. Radpour et al. demonstrated that in the absence of renal agenesis, five of seven (70%) Iranian men with CUAVD and a patent contralateral vas had either single or compound heterozygous CFTR mutations (42). Studies from Canada (43), Spain (44), Germany (45), France (37), and Portugal (43) also reported variable rates of CFTR mutations among men with CUAVD (20%, 27%, 60-100%, and 75%, respectively). However, a critical point with respect to these data sets, besides the small sample sizes, is the lack of information regarding the patency of the contralateral vas deferens.
Congenital bilateral epididymal obstruction and normal vasa
CFTR mutations have been implicated in bilateral epididymal obstruction in azoospermic men in the presence of normal, bilaterally palpable vasa. Mak et al. identified CFTR mutations in 14/56 (25%) men with idiopathic epididymis obstruction (46). The most common identified mutations were IVS8-5T, ΔF508, R117H and L206W. Similarly, Jarvi et al. reported that as many as 47% of patients with bilateral epididymal obstruction carried CFTR mutations, such as IVS8-5T, ΔF508, and R117H (47).
Young syndrome
Young syndrome is a rare disease primarily characterized by a constellation of three components, that is, bilateral epididymal obstruction with azoospermia, bronchiectasis, and chronic sinusitis. The estimated prevalence is unknown, with newly discovered cases being described as case reports. Unfortunately, the origin of this disease is also unknown, although childhood exposure to mercury and genetic etiologies have been suggested (48,49). Its familial incidence in one case and its association with medullary sponge kidney in another suggest its inheritability (50,51); however, mutations have not been identified. Male infertility is attributed to bilateral epididymal head dilatation and blockage by an expressible amorphous mass that is attributed to poor epididymal mucociliary clearance (49). The diagnosis of Young syndrome is made by the exclusion of the two other similar syndromes, namely, CF (screened for by testing for CFTR mutations) and immotile cilia syndrome, which is confirmed by prolonged nasal mucociliary clearance of the tested material (saccharine) (49,52). Functional rather than subtle ultrastructural epididymal and nasal ciliary defects are considered to be the basic mechanism of the disease, and epididymal aspirations revealed motile spermatozoa (52). Interestingly, epididymal obstruction often occurs in middle-aged men; therefore, previously successful parenthood may be anticipated in such syndromes (52,53).
NON-OBSTRUCTIVE AZOOSPERMIA OF GENETIC ORIGIN
Non-obstructive azoospermia (NOA) is a heterogeneous disorder that is characterized by various testicular tissue alterations. Such changes result in poor and/or absent spermatogenesis within the testes and the absence of sperm in the ejaculate. NOA accounts for approximately 60% of men with azoospermia and represents the most severe form of male factor infertility. Although NOA is caused by a multitude of factors, such as heat, radiation, drugs, varicocele, infections and cancer, genetic etiologies contribute significantly to the development of this disorder in 21-28% of cases (7,9,40),. NOA is didactically divided into two major categories, i.e., pre-testicular and testicular. The genetic pre-testicular etiology encompasses hereditary hypothalamic-pituitary abnormalities, which lead to insufficient gonadotropin action on testicular cells. This defect results in small testes that exhibit an immature histological pattern. In these cases, immature Sertoli cells or spermatogonia type A (which primarily reside in the center of seminiferous tubules) and the absence of Leydig cells are often observed.
Genetic testicular causes of NOA include the following: i) chromosomal abnormalities, ii) Y chromosome microdeletions, iii) failure of the primordial germ cells to reach the developing gonads, iv) lack of differentiation of the primordial germ cells to spermatogonia, and v) male germ line mutations that affect spermatogenesis. The lattermost cause is further divided into mutations that control transcription, signal transduction, apoptosis, cell response to stress factors, cytokines (cross-talk), immune sensitization of germ cells, meiotic divisions, and epigenetic factors. Genetic mutations of androgen receptors are also included in this category.
GENETIC PRE-TESTICULAR CAUSES OF NOA
Pre-testicular causes of NOA result from either hypothalamic or pituitary disorders.
Hypothalamic hypogonadotropic hypogonadism
Genetic hypothalamic disorders essentially fall under the classification of hypothalamic hypogonadotropic hypogonadism (HH), which encompasses a broad spectrum of diseases characterized by various genotypes. A deficiency of gonadotropin-releasing hormone (GnRH) or its receptor is the fundamental endocrine abnormality that is detected in this disease. GnRH is a decapeptide that is synthesized by a loose network of neurons located in the medial basal hypothalamus (MBH) and in the arcuate nucleus of the hypothalamus. A subset of GnRH neurons is observed outside of the hypothalamus in the olfactory organ, reflecting the common embryological origin of these neurons (54). Developmentally, GnRH neurons originate from the olfactory placode/vomeronasal organ of the olfactory system and migrate along the vomeronasal nerves to the hypothalamus. Here, these cells extend processes to the median eminence and the pituitary gland (55). GnRH is synthesized as a precursor, 92-amino acid hormone and is then cleaved into a 69-amino acid prohormone. This prohormone is further cleaved at the nerve terminals to form the active decapeptide (55). GnRH receptors are plasma membrane-associated receptors that promote increases in intracellular calcium concentrations, which acts as a second messenger, upon binding to GnRH (55).
The essential function of GnRH is to stimulate the secretion of LH and FSH from the anterior pituitary gland at the time of puberty (56). The hypothalamic pulse generator triggers the pulsatile release of GnRH and is considered to be a regulatory mechanism of the action of this hormone. Moreover, there is a brief postnatal surge of GnRH during the infantile period, which lasts for a few months and allows for the proper diagnosis of a suspected deficiency at an early age (57).
Genetic HH is primarily divided into two general categories based on the age of onset: congenital and adult-onset HH. Congenital HH is subdivided by the presence of an intact olfactory sense: anosmic HH (Kallmann syndrome) and congenital normosmic isolated HH (IHH). Prader-Willi syndrome is also a congenital disorder that presents with HH.
Congenital HH
This disease is primarily characterized by early-onset hypogonadism due to the dysfunctional release or action of GnRH. This defect results in delayed or absent pubertal development, with low sex steroid levels in the setting of low or normal gonadotropin levels. Normal hypothalamic pituitary gland anatomy on magnetic resonance imaging and the absence of other causes of HH, such as hemochromatosis, are prerequisites for diagnosis (58). The congenital incidence of HH is 1-10/100,000 live births, with approximately 2/3 being due to Kallmann syndrome and 1/3 to normosmic HH (59).
Kallmann syndrome (KS) is characterized by the presence of complete or partial anosmia in association with congenital HH. The failure of the migration of GnRH neurons from the olfactory placode to their destination in the hypothalamus and the olfactory lobe is the basic embryological defect that characterizes this syndrome (59). However, the genetic bases of this condition have not been fully elucidated. Sporadic (2/3) and familial (1/3) varieties of this condition have been described (60). Hereditary studies reveal that familial KS is heterogenetic, with variable modes of inheritance (autosomal dominant, autosomal recessive, and X-linked) being observed. X-linked inheritance is the most common mode. It is not only the genotypic characteristics but also the phenotypic features of this syndrome that are variable. A diverse spectrum of physical manifestations is observed. Males are affected five times more frequently than females, and its incidence in males is approximately 1/8,000 (61). Unfortunately, the genetic origin of only 50% of familial cases and 10% of sporadic cases has been clarified (62). Six known genes account for only 25-35% of all cases of KS (60). These genes are as follows: KAL-1, FGFR-1, PROK-2, PROKR-2, CHD-7, and FGF-8. However, other genetic abnormalities have been described, such as chromosomal translocation 46 XY, t(10,12) (63) and copy number variations (CNVs) (64). Regions in which CNVs are observed account for less than 12% of the human genome and are defined as large segments of DNA on a particular chromosome that have been deleted or duplicated (65,66). Five distinctive chromosomal regions have been implicated in Kallmann syndrome, and the majority of these CNVs involve the intronic regions of a particular gene, reflecting a possible disturbance in splicing mechanisms. These regions include the following: 1p21.1, 2q32.2, 8q21.13, 14q21.2, and Xp22.31 (64).
KAL-1 was the first gene that was discovered in Kallmann syndrome patients. This gene maps to the X chromosome (Xp22.32) and consists of 14 exons (59,67). It encodes an 840-amino acid protein that is referred to as anosmin 1. This is an extracellular adhesion protein that has a potential role in orchestrating GnRH neuron adhesion and axonal migration (59,67). The majority of the observed mutations in the KAL-1 gene are either nucleotide insertions or deletions that result in a frame shift mutation or a premature stop codon (59). However, in fewer than 20% of cases, these nucleotide insertions or deletions may cause amino acid substitution, disrupting the tertiary structure of anosmin 1 and attenuating its function (68). Rarely, contiguous gene syndrome, which includes the deletion of terminal regions of the short arm of the X chromosome (Xp22), may contribute to KS (69,70). Such deletions may cause, in addition to KS, short stature, chondrodysplasia punctata, mental retardation, and steroid sulfatase deficiency (69,70). The KAL-1 gene is responsible for the X-linked recessive mode of inheritance in familial KS and accounts for 10-20% of all cases of KS (71-73). Specifically, KAL-1 mutations account for 30-60% of familial cases and 10-15% of sporadic cases of KS (73-75). Nevertheless, this gene has not been observed in female KS patients or in isolated normosmic HH cases (76). Interestingly, several phenotypic characteristics have been associated with KAL-1 mutations, such as mid-facial clefting, unilateral renal agenesis in 30% of cases, specific neurological abnormalities such as synkinesis (mirror movement), cerebellar dysfunction, deafness, eye abnormalities and mental retardation (60).
The fibroblast growth factor receptor 1 (FGFR-1 or KAL-2, 8p11.2-p11.1) gene is the second most common genetic mutation that is associated with KS (77,78). This gene encodes a tyrosine kinase-linked membrane glycoprotein receptor that binds to extracellular acidic and basic fibroblast growth factors (79). A potential function of fibroblast growth factor is to facilitate GnRH neuron migration, differentiation and survival (80,81). The dysfunction of the FGF receptor results in improper migration and localization of GnRH neurons, potentially explaining the contribution of this mutation to normosmic HH. FGFR-1 mutations are observed in 10% of patients with KS (78,82). Mutations in this gene are observed in 11% of sporadic cases and 8% of familial cases (83). More importantly, the observed mode of inheritance in familial KS is autosomal dominant, with variable expressivity, incomplete penetrance and an even male-to-female ratio (84). Variable expression of the FGFR-1 gene is reflected by the occurrence of anosmia alone, hypogonadism alone, or both in family members of the proband (i.e., the affected individual). Moreover, mutations in the FGFR-1 gene do not always result in KS (incomplete penetrance); this phenomenon may highlight the requirement of a loss of function mutation in the development of KS. More than 70% of mutations in FGFR-1 are missense point mutations that result in amino acid substitutions in the immunoglobulin-like or tyrosine kinase domains. Other mutations are either nonsense, frame shift or splice mutations (61). FGFR-1 mutation-induced KS is characterized by variably severe hypogonadism (from mild to complete) and certain morphogenic abnormalities, such as mid-facial clefting, synkinesis (20% of patients) and missing teeth (61).
Fibroblast growth factor 8 (FGF-8) is considered to be one of the ligands for FGFR-1 and is hypothesized to facilitate the migration and differentiation of GnRH neurons to the hypothalamus, as was described above. Mutations in the gene that encodes this protein can cause KS and normosmic HH (85,86). This gene has been mapped to chromosome 10q24 and is responsible for fewer than 2% of all cases of KS (60). An autosomal dominant mode of inheritance is also demonstrated in familial cases with variable penetrance. Other genes that may be affected in KS include PROK2, PROKR2, and CHD7. Prokineticin 2 is an 81-amino acid protein that is encoded by the PROK2 gene, which has been mapped to chromosome 3p13. This protein has a putative role in the chemoattraction of GnRH neurons in their migration to and differentiation in the hypothalamus (59). This protein acts by binding to a specific G-protein-linked receptor that is encoded by PROKR2 and is located at 20p12.3 (59,61,62). Frame-shift mutations in PROK2 and missense mutations in PROKR2 account for 5-10% of cases of KS (59,61). Mutations in either of these genes exhibit homozygous (autosomal recessive), heterozygous (autosomal dominant) and compound heterozygous modes of inheritance (87). Furthermore, these mutations are associated with variable phenotypic manifestations, such as fibrous dysplasia, severe obesity, sleep problems and synkinesis. Similarly, mutations in these genes have been described in normosmic HH (88). Chromodomain helicase DNA binding protein 7 (CHD7) is a member of a family of proteins whose function is to organize chromatin remodeling (packaging), a process that regulates gene expression (89,90). Tightly arranged chromatin is characterized by lower gene expression compared with loosely arranged chromatin. CHD7 is ubiquitously expressed in fetal tissues, the brain, the eyes, the inner ear, olfactory neural tissue and GnRH neurons. The gene that encodes this protein is located on chromosome 8q12.2 (62). Mutations in this gene have been linked to several diseases, such as KS, normosmic HH and CHARGE syndrome. CHARGE syndrome is associated with eye coloboma, heart defects, atresia of the nasal choana, retarded growth, genitourinary abnormalities, anosmia, and hypogonadism (KS) (89-91). The CHD7 protein is postulated to be an essential factor in the migration and differentiation of GnRH neurons. Seven mutations have been described for this gene in sporadic and familial KS and normosmic HH (59,92). CHD7 accounts for 6% of all cases of KS and 6% of sporadic KS cases. Moreover, familial KS due to CHD7 mutations exhibits an autosomal dominant mode of inheritance (92).
Normosmic HH, which is also referred to as isolated or idiopathic HH, is defined as a lack of GnRH secretion or function in the setting of i) normal or low pituitary gonadotropins and ii) the absence of anatomical or functional hypothalamic abnormalities. Patients with normosmic HH present with low levels of sex steroids, normal MRIs and a normal olfactory sense. This disease contributes to 40% of cases of hypothalamic HH. Two-thirds of cases of normosmic HH are considered to be sporadic, whereas 1/3 of cases are familial (60). This disease frequently overlaps with KS in terms of both clinical presentation and the involved genes. Familial cases exhibit X-linked, autosomal dominant and recessive modes of inheritance. The pathogenetic mechanism is attributed to a failure of differentiation or development of normally migrating GnRH neurons into the hypothalamus, resulting in a lack of GnRH secretion or apulsatile secretion (59). A wide array of causative mutations have been identified by nucleotide sequence studies. Nevertheless, the genetic etiology of this condition is unknown for more than 50% of patients. Genes that have been previously reported to be mutated in KS, including FGFR-1, FGF8, PROK2, PROKR2, and CHD7, have also been implicated in the pathogenesis of normosmic HH. The other implicated mutations include those in GnRH, GnRHR, KISS1R, TAC3, TACR3, and DAX1 (59,60,76). However, chromosomal abnormalities (generally sporadic) have been observed in 3% of patients with normosmic HH. Such abnormalities include 46,XY/46,X,inv(Y)(p11.2q11.2) and mos46,XY,t(3;12)(p13;p13)/46,XY (76,93).
Mutations in the GnRH gene were recently determined to be a rare cause of normosmic HH in two human studies of familial HH (94,95). The gene maps to chromosome 8q21-p11.2 and encodes a large 92-amino acid precursor protein. An autosomal recessive mode of inheritance for this trait has been described, and homozygous frame-shift mutations have been observed in probands (94,95). However, mutations in the gene that encodes the G-protein-coupled receptor for GnRH (GnRHR1) are the most common genetic abnormality that is detected in patients with this disorder, accounting for 5-40% of normosmic HH cases (3.5-16% of sporadic cases and as many as 40% of familial cases) (93). This gene maps to chromosome 4q13.2-3, spans over 18.9 kb and encodes a 328-amino acid protein (96). Autosomal recessive homozygous or compound heterozygous mutations have been reported in familial cases (97-103). The majority of GnRHR1 mutations are missense mutations that cause single amino acid substitutions. Such mutations result in variable functional effects, ranging from mild impairment to complete inactivation of the receptor (104,105).
Recent studies have identified other ligand proteins and their receptors, such as Kisspeptin and neurokinin B, the functions of which are to regulate the differentiation of GnRH neurons and to initiate their function during puberty. The Kisspeptin (KSS1) gene has been mapped to chromosome 1q32, and a missense mutation in this gene causes autosomal recessive inherited normosmic HH (62,106). Moreover, Kisspeptin receptor (KSSR1, chromosome 19p13.3) mutations also exhibit autosomal recessive patterns of inheritance, and both KISS1 and KISSR1 mutations contribute to fewer than 5% of normosmic HH cases (107). Mutations in neurokinin B (TAC3, chromosome 12q13-q21) and its receptor (TACR3, 4q25) have also been implicated in the pathogenesis of normosmic HH and exhibit autosomal recessive inheritance patterns (108-110). Convertase 1 is an endopeptidase that is encoded by the PCKS1 gene and is involved in i) the post-translational modification of precursor GnRH and ii) the release of mature and active GnRH (59). Mutations in the gene that encodes this protein have been linked to anosmic HH, diabetes and obesity (111). Finally, an X-linked mode of inheritance of normosmic HH has been linked to DAX1 mutations, which cause congenital X-linked adrenal hypoplasia (112).
Prader-Willi syndrome (PWS) is a complex genetic disorder that is associated with various degrees of systemic involvement. This condition is caused by the lack of expression of paternally derived imprinted genes on chromosome 15q11-q13. This lack of expression is due either to the deletion of these genes, maternal uniparental disomy of chromosome 15 or the disruption of the paternally inherited chromosome 15 (9,90). Genomic imprinting refers to a phenomenon in which certain genes are expressed in a parent in an origin-specific manner. In this situation, an allele from a given parent is silenced to allow for the expression of non-imprinted genes from the other parent. Genomic imprinting is observed in fewer than 1% of genes. Obesity, hyperphagia, growth retardation, mild to moderate mental retardation, dysmorphic facial features, and sleep abnormalities are the characteristic features of Prader-Willi syndrome. Hypothalamic HH is a consistent feature of all men with this syndrome (9). During infancy, 80-90% of affected children exhibit cryptorchidism, with a poorly developed scrotum and micropenis. Most adolescents will exhibit delayed or incomplete puberty; however, precocious puberty has been described in 4% of patients (9,24,90). Maternally derived supernumerary marker chromosome (SMC) 15 is the most frequently observed supernumerary chromosome marker in humans (50%). This dicentric chromosome fragment arises from the two homologous chromosomes 15 and is now referred to as dic(15). This genetic defect was formerly referred to as inverted duplication of chromosome 15 or inv dup(15). The size of the fragment is variable; long fragments may contain the PWS critical region and may lead to the development of PWS, whereas short fragments do not contain this critical region, in which case PWS is not observed. However, azoospermia and mild facial dysmorphism, such as mandibular anomalies, have been reported in men that carry the short fragment. Further genetic analysis of the genes on chromosome 15 is lacking but may aid in our understanding of the role of these genes in male infertility.
Adult-onset genetic hypothalamic HH
This disease category has recently been described and is restricted to men who successfully completed pubertal development (and who may already have children) and who subsequently exhibited disruption of the HPG axis. Testicular size in such patients is normal, but serum testosterone and gonadotropins levels are low. Moreover, an apulsatile pattern of LH secretion is observed in these patients. A single study of 10 men with adult-onset HH revealed a heterozygous PROKR2 mutation in one patient. However, a good prognosis is expected in these men following treatment with respect to their future fertility potential and androgenization status (9).
Pituitary disorders that are associated with hypogonadism
Male hypogonadism that is attributed to genetic pituitary diseases is rare, and such conditions are divided into two major categories: a) generalized or combined anterior pituitary hormone deficiency, and b) selective gonadotropin deficiency.
Generalized anterior pituitary hormone deficiency
Several mutations have been observed in men with combined anterior pituitary hormone deficiency (CPHD). Most of these mutations involve genes that code for signaling molecules and transcription factors. Transcription factors are DNA-binding proteins that facilitate the transcription of mRNA from DNA. The affected hormones in CPHD include growth hormone, prolactin, thyroid-stimulating hormone, and gonadotropins (LH and FSH). ACTH may or may not be involved. Such mutations may interfere with the early or late embryonic development of the pituitary gland from Rathke's pouch. Certain mutations may give rise to various syndromes, such as septo-optic hypoplasia and craniofacial abnormalities (113). In addition to phenotypic variability, the appearance of the pituitary gland on MRI is also variable in CPHD and ranges from enlarged in cases with PROP1 mutations (113,114) to normal or hypoplastic in patients with SOX2 mutations (114). Specifically, the implicated mutated transcription factor genes that cause hypogonadism are the following: PROP1 (most common), LHX and SOX2. Familial and sporadic cases that exhibit autosomal recessive patterns of inheritance are the most common forms of CPHD (114). To accurately differentiate between hypothalamic and pituitary HH, a GnRH stimulation test is performed. In hypothalamic disorders, significant increases in gonadotropin levels are observed, whereas no response is observed in patients with pituitary hypogonadism.
Selective gonadotropin deficiency
FSH and LH are glycoproteins that are secreted by anterior pituitary gonadotropes to stimulate testicular spermatogenesis and testosterone production, respectively. Each glycoprotein molecule is composed of α and β chains. The α chain represents a common chain for LH, FSH, human chorionic gonadotropin (hCG), and TSH, whereas the different β chains of these hormones confer immunological and biological hormone specificity. Selective gonadotropin deficiency includes mutations in the genes that code for the synthesis of FSH and LH and their receptors. Specifically, mutations that affect hormone synthesis generally involve the β chain genes, given that mutations in the α chain gene (CGA, 6q12-21) are generally embryonically lethal due to the lack of placental HCG synthesis (115).
FSH exerts its action through Sertoli cell receptors, stimulating their proliferation in the immature testis. FSH also stimulates and maintains spermatogenesis. FSH is composed of an α chain, which is composed of 92 amino acids and is non-covalently bound to the β chain (111 amino acids). Rare β subunit (chromosome 11p13) mutations result in isolated FSH deficiency, delayed or normal puberty and small or normal-sized testes in association with severe oligozoospermia or non-obstructive azoospermia (116-118). The β subunit gene is composed of three exons and two introns. To date, two missense and three stop codon mutations with autosomal recessive modes of inheritance have been detected (117),. In contrast, FSH β knockout mice are not infertile, indicating differential regulatory mechanisms in humans and mice (122,123). Furthermore, rare mutations in the gene that encodes the FSH receptor (FSHR), which is expressed in Sertoli cells, have variable effects on spermatogenesis. In a study of five men who were homozygous for FSHR mutations, none exhibited normal semen parameters. Specifically, three patients exhibited severe oligozoospermia and one exhibited moderate oligozoospermia; the fifth patient exhibited a low semen volume and teratozoospermia despite having a normal sperm count (124). The FSHR gene has been mapped to chromosome 2p21-16 and consists of 10 exons and 9 introns (125,126). This gene encodes the mature form of a G-protein-linked glycoprotein receptor, which is composed of 678 amino acids and is exclusively expressed in Sertoli cells (125). Single missense inactivating mutations that result in a valine to alanine substitution at position 189 (A189V) have been reported; these mutations exhibit an autosomal recessive mode of inheritance. Preliminary studies by Simoni et al. (127) and Ahda et al. (128) have revealed differences in the FSHR polymorphisms between fertile and infertile men. Further research is required to clarify the genetic background of FSHR mutations.
LH initiates male pubertal development through its effect on LH receptors on Leydig cells, which stimulate the release of testosterone. Although reported in only five men, recessively inherited missense mutations in the beta subunit (121 amino acids) of the LH gene (19q13.3) result in delayed or absent pubertal development and oligozoospermia or azoospermia (129-131). The hormonal profile of such patients indicates normal FSH levels, high LH immunoreactivity and low testosterone (129,130). The detected LH does not exhibit biological activity. A variety of autosomal recessive mutations (missense, insertion, deletion and nonsense) have been observed in the gene that encodes the G-protein-linked LH receptor. Such mutations result in variable phenotypic traits and infertility. Interestingly, LH glycoprotein receptors (674 amino acids) respond not only to LH but also to hCG and are thus occasionally referred to as LhCGRs. These receptors are present not only in Leydig cells but also in sperm, seminal vesicles, the skin, the thyroid and other organs, where they have an unidentified physiological significance. The gene for the LH receptor has been mapped to chromosome 2p21 and consists of 11 exons and 10 introns (132). This genomic location is close to that of the FSHR gene, and mutations in the LH receptor gene result in Leydig cell hypoplasia (LCH) or agenesis (115,133). LCH exhibits a wide spectrum of manifestations, ranging from male pseudohermophroditism in cases of 46,XY (female external genitalia, undescended abdominal testes, absent breast development) to selective, milder undervirilization defects, such as micropenis, hypospadias, and cryptorchidism (115).
Genetic testicular disorders (GTDs)
Genetic testicular disorders that cause male infertility can be divided into three categories according to the specific altered function: 1) genetic testicular disorders that primarily affect spermatogenesis and androgen production; 2) genetic testicular disorders that primarily affect spermatogenesis; and 3) genetic testicular disorders linked to androgen synthesis or action.
GTDs that affect spermatogenesis and androgen production
Klinefelter syndrome
KLFS is the most common cause of hypogonadism and infertility in males (1 in 500). Klinefelter syndrome is also the most common chromosomal aneuploidy that is observed in azoospermic men (10%) (134); specifically, azoospermia is detected in 74% of men with KLFS (134). The mechanisms of infertility associated with KLFS include a lack of the potential for testicular growth, premature degeneration of the primordial germ cells before puberty and the early or late maturation arrest of spermatogenesis at the primary spermatocyte stage. Later stages of sperm development can also be affected (39). Generally, two forms of KLFS are observed: non-mosaic, (47,XXY, 85% of cases) and mosaic (47,XXY/46,XY, 15% of cases). Twenty-five percent of patients with non-mosaic KLFS have sperm in their ejaculate (32). Rare cases of KLFS are caused by isochromosome Xq i(Xq) or X-Y translocations in 0.3-0.9% of males with X chromosome polysomies (135,136). Residual spermatogenesis is observed in men with both mosaic and non-mosaic forms of KLFS. In addition to very small (1-3 ml) and firm testes, gynecomastia (40%) and features of male hypogonadism are also present, such as sparse facial and pubic hair growth, loss of libido and erectile dysfunction. Low testosterone is observed in as many as 80% of men, an effect that is attributed to small testicular growth despite the presence of Leydig cell hyperplasia.
Several studies have demonstrated that KLFS patients exhibit a high incidence of aneuploid gametes, rendering them at risk for producing offspring with chromosomal abnormalities (137). Interestingly, the successful fathering of 60 children has been achieved by testicular sperm extraction (TESE) and ICSI in men with KLFS. Karyotype studies that were performed in approximately 50 children revealed no chromosomal abnormalities (138,139). These genetic findings have been further clarified in a study by Sciurano et al., who detected spermatogenesis foci in testicular biopsies of 6/11 men with nonmosaic KLFS (140). Whereas the majority of seminiferous tubules are devoid of germ cells, 8-24% do contain germ cells. Sciurano et al. examined the chromosomal complements of 92 meiotic spermatocytes using fluorescent in situ hybridization (FISH). These spermatocytes exhibited euploidy (normal chromosomal constituents) and the ability to form haploid gametes (140). These novel findings may explain the high rate of normal children who are born following testicular sperm extraction and ICSI in men with KLFS. Nonetheless, even with this high rate of normally born children, there is still a risk of genetic defects in the offspring; therefore, it is advised that a preimplantation genetic diagnosis (PGD) be offered prior to ART to ensure that the offspring are not aneuploid (39).
XX males
This genetic disorder is very rare, with an estimated prevalence of 1:10,000-1: 20,000 (141). The genetic event that causes this disorder involves the translocation of genetic material of the testis-determining region of SRY (or SOX A, a gene that lies on the Y chromosome) to the X chromosome during paternal meiosis. SRY encodes a transcription factor of approximately 204 amino acids (142). This translocation results in the successful differentiation of indeterminate gonads into testes; however, the lack of other genes involved in the initiation of spermatogenesis renders these males azoospermic. Furthermore, SRY-negative variants have also been described, which are characterized by severe undervirilization defects, such as undescended testes, hypospadias and bifid scrota (143). Phenotypically, these men are very similar (but with smaller statures) to patients with KLFS (144).
Mutations in X-linked USP26
The USP26 gene is a single-exon gene that maps to chromosome Xq26.2. This gene encodes the USP26 protease (913 amino acids), which is a deubiquitinating enzyme (145,146). The ubiquitination and deubiquitination of macromolecules are essential for the regulation of the cell cycle, maintenance of chromosomal structure and gene silencing (145). The removal of histones and the regulation of protein turnover during meiosis are important functions of this protein. More than twenty mutations in this gene have been reported. These mutations result in the severe impairment of spermatogenesis, and several result in hypogonadism (147). Studies have demonstrated a relationship between this gene and certain cases of non-obstructive azoospermia (148,149).
X-linked SOX3 mutations
The SOX genes are essential for development and control of embryonic ontogenesis in the human testes, neural tissues, cartilage, and neural crest cells. These genes are present only in vertebrates and give rise to SOX proteins that have a role in both the developing and adult gonads. These proteins share a common 79-amino acid DNA binding domain that is characteristic of a large protein superfamily that is referred to as the high mobility group (HMG) due to the high migration rate of these proteins in polyacrylamide gels (150). SOX proteins specifically bind to the DNA minor groove and regulate gene expression by acting either as transcriptional activators or repressors (150). The name SOX is derived from the first-discovered Y-linked SOX gene, i.e., sex-determining region Y (SRY). The other genes in this family are therefore referred to as SRY-box (SOX) genes. The SOX genes are divided into several groups, from A to H, with group A consisting only of the Y-linked SRY (150). SOX3 is X-linked (Xq26.3) and belongs to the SOX B1 group. The SOX3 gene is specifically expressed in developing testicular and neural tissues and encodes the SOX3 transcriptional activator (151,152). Solmon et al. and Woods et al. correlated genetic mutations in the SOX3 gene with hypopituitarism and mental retardation (153,154). Recessively inherited polymorphic mutations in SOX3 have been observed in men with idiopathic oligozoospermia and in mice with severely impaired sperm production and hypogonadism (155,156).
Bilateral anorchia
Bilateral anorchia is a rare congenital disease with an estimated prevalence of 1 in 20,000 males. This condition is characterized by the absence of testicular tissue in 46,XY individuals (157). Because male infants who are born with this disorder exhibit normal genital differentiation, the absence of testicular tissue is most likely attributed to testicular regression that occurs in the second half of gestation. A micropenis is observed in half of these cases (157). The exact etiology of this disease is unknown; however, a subset of cases exhibit familial clustering, suggesting a genetic etiology. Philibert et al. recently noted the role of mutated steroidogenic factor-1 (NR5A1), which is a member of the nuclear receptor family, in the disease etiology. These genes regulate the transcription of other genes that control the development of adrenal and gonadal tissues (158). NR5A1 has been mapped to chromosome 9q33 and has been correlated with other human diseases, such as male infertility, hypospadias, ovarian insufficiency, and others (158).
Noonan syndrome
Noonan syndrome is a relatively common heterogeneous genetic disorder that results in a wide array of clinical manifestations and genotypic abnormalities. Its incidence ranges from 1:1,000 to 1:2,500 live births, and it is inherited in an autosomal dominant manner (150). To date, nine genes have been implicated in Noonan or Noonan-associated syndromes (PTPN11, SOS1, KRAS, NRAS, RAF1, BRAF, SHOC2, MEK1, and CBL) (159). The basic cellular abnormalities that are caused by mutations in these genes are defective signal transduction pathways, particularly the RAS-GTPase and mitogen-activated protein kinase (MAPK) signaling cascades (159). The typical phenotypic features of Noonan syndrome include a short stature, a webbed neck, facial dysmorphism, congenital pulmonic stenosis and other manifestations. Unilateral and bilateral cryptorchidism are frequent in this syndrome and are observed in as many as 77% of patients (160). Moreover, delayed or absent pubertal development in males with this syndrome is attributed to testicular failure (161). Therefore, altered spermatogenesis with oligozoospermia or azoospermia is multifactorial due to the basic genetic defect itself and its association with cryptorchidism.
45X/46,XY mosaicism (mixed gonadal dysgenesis)
Normal male external genitalia are observed in 90% of males with 45,X/46,XY mosaicism; abnormal, ambiguous and female genitalia are observed in the other 10%. Mixed gonadal dysgenesis (a streak gonad on one side and a testis on the other) is observed in 10-30% of patients with this type of mosaicism (162). Abnormal gonadal development results in azoospermia and low testosterone levels (163).
GTDs that affect spermatogenesis
Y chromosome microdeletion
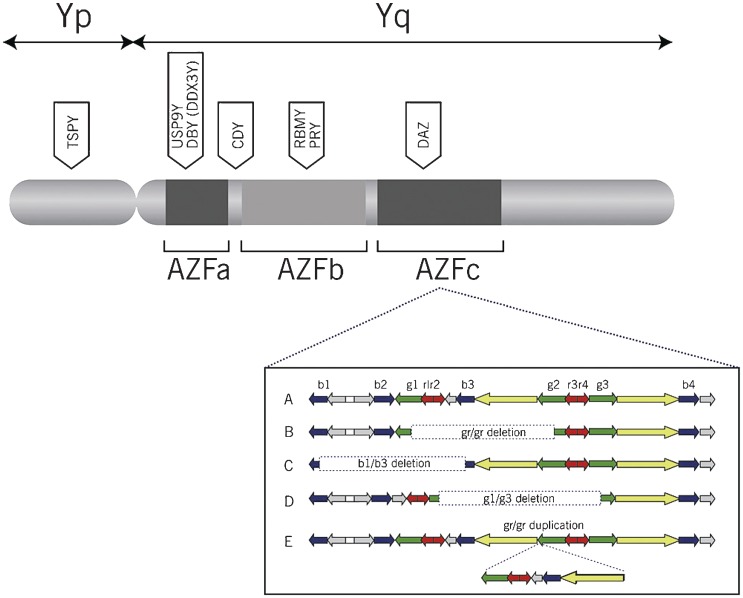
The long and short arms of the Y chromosome contain many genes that regulate spermatogenesis and testes development, respectively. Microdeletions on the long arm of the Y chromosome (Yq) are well correlated with male infertility. Yq microdeletions are detected in approximately 13% of men with non-obstructive azoospermia and in 5% of men with severe oligozoospermia (sperm counts lower than 5 million/mL) (164,165). A microdeletion is defined as a chromosomal deletion that spans several genes but that is small in size and cannot be detected using conventional cytogenetic methods (e.g., karyotyping). Y chromosome microdeletions are clustered in intervals 5 and 6 of the long arm of the Y chromosome. This region at Yq11 is referred to as the “Azoospermia Factor” (AZF) region. The AZF region is further subdivided into three subregions that are termed AZFa, AZFb, and AZFc (Figure 1). The most common aberrations in the AZF region are multiple gene deletions in the AZFb and AZFc sub regions (166), which can produce a wide range of infertility phenotypes. The genes on the Y chromosome are generally divided into three types: “X transposed”, X degenerated, and amplicons. Eight palindromes are recognized in the AZF region and six of these are related to male fertility. Six of the genes that are located in the AZF regions are expressed exclusively in the testes and are therefore referred to as “AZF candidate genes”.
Figure 1.
Schematic representation of the Y chromosome that depicts the AZF region, the AZF subregions and the primary genes within each subregion. Adapted from: O'Flynn, O'Brien KL, Varghese AC, Agarwal A. The genetic causes of male factor infertility: a review, pages 1-12, copyright 2010, Fertil Steril 93, with permission from Elsevier via the Copyright Clearance Center (Order Detail ID: 62879217).
The AZFa region is the smallest portion of the AZF and spans approximately 400-600 kb of DNA. It is located in the proximal portion of interval 5. The AZFa region is characterized by a non-repetitive structure and a low deletion frequency. This subregion contains three genes: USP9Y, DBY (DDX3Y) and UTY. Two protein-coding genes are directly related to male infertility: USP9Y and DBY (recently termed DDX3Y). Complete and partial deletions of AZFa have been described. Complete deletions that remove both genes cause Sertoli cell-only syndrome (SCOS) and bilateral small-sized testes (167,168). It is estimated that 9-55% of SCOS cases are caused by deletions in the AZFa region (169-171). Partial deletions have also been reported, with particular involvement of USP9Y. The DBY gene is the major single-copy gene in the AZFa region and belongs to the DEAD BOX RNA helicase family. This family consists of a group of genes that encode proteins that specifically regulate RNA transcription, translation, and splicing in the G1 phase of the cell cycle. DBY expression is observed in the male germ line, whereas its expression in other tissues is uncertain (172). DBX, a DBY homologue, belongs to the same family as DBY and is expressed in male germ cells. Its expression pattern has been elucidated by immunohistochemistry techniques. The DBY gene and protein are specifically expressed in premeiotic germ cells, whereas the DBX gene and protein are expressed in postmeiotic germ cells (172). This differential distribution explains why deletions of the DBY gene can result in SCOS and azoospermia. The USP9Y gene is a single-copy gene that encodes a ubiquitin-specific protease (a deubiquitinating enzyme). This enzyme binds to ubiquitin-protein conjugates and hydrolyzes the ubiquitin peptide chain. Such action confers stability to cellular proteins and protects them from cellular degradation by the proteasome complex (173). The expression of USP9Y is restricted to spermatids in humans and mice (174,175). USP9Y expression in male germ cell lines may lead to the stability of certain cellular proteins that are synthesized in primordial germ cells (PGCs) and that are important for germ cell survival. Point mutations in the USP9Y gene result in maturation arrest at the spermatid stage (176), oligozoospermia (177), oligoasthenozoospermia, and asthenozoospermia (178).
The AZFb subregion spans approximately 6 Mb and is located in the distal portion of interval 5 and the proximal portion of interval 6 (subinterval 5O-6B) (179). The meiotic arrest of spermatogenesis at the primary spermatocyte stage is usually observed when AZFb is deleted. AZFb contains 32 genes and overlaps with AZFc (179). As such, AZFb deletions often remove certain genes from the AZFc region (e.g., DAZ1 and DAZ2), as well as one copy each of BPY2, CDY1, and PRY. The primary protein-encoding genes in AZFb are RBMY and PRY. Six copies of RBMY are located in the distal portion of AZFb and are only expressed in germ cells (180). RBMY encodes four types of testis-specific RNA-binding proteins that are involved in mRNA processing, transport, and splicing (181). Due to its proximity to AZFc, certain deletions within AZFc can remove several copies of RBMY genes. Two copies of PRY are located in the AZFb region and presumably regulate apoptosis (167). Hypospermatogenesis is observed when all of the AZFb genes are deleted except for RBMY and PRY. Conversely, spermatogenesis is completely arrested when both the RBMY and PRY genes are deleted (182,183).
AZFc spans over 3.5 Mb and contains a large number of amplicons that are arranged as direct repeats, inverted repeats, or palindromes. Examples of these repeats include b, g, r, and P repeats. Seven distinct gene families, encompassing 23 genes, are observed in the AZFc region. These families include PRY (two copies), TTY (eight copies), BPY (three copies), DAZ (four copies), GOLGA2LY (two copies), CSPYG4LY (two copies), and CDY (two copies). Deletions in the AZFc region alone or deletions in this region that are combined with deletions in other AZF regions are the most common types and account for as many as 87% of Yq microdeletions. The incidence of these deletions is 1/4,000 males. Although AZFa and AZFb deletions result in azoospermia, deletions in the AZFc region can result in either azoospermia or oligozoospermia (184). AZFc deletions can explain approximately 12% of non-obstructive azoospermia and 6% of severe oligozoospermia cases (185). Two scenarios have been described regarding the cause of complete AZFc deletions, namely, a new deletion in addition to a preexisting partial deletion or a complete deletion of a preexisting normal gene. AZFc deletions may jeopardize Y chromosome integrity, resulting in its loss and sex reversal. As such, AZFc deletions predispose one's offspring to the 45,X0 karyotype (186) and to the mosaic phenotype 45,X/46,XY (187).
Two types of AZFc deletions have been described. The classic AZFc deletion is denoted by b2/b4. This deletion encompasses four DAZ genes, resulting in azoospermia. Partial or sub-deletions are denoted by gr/gr, b1/b3, and b2/b3. The gr/gr subdeletion removes nearly half of the AZFc region and results in different phenotypes in various populations. Such variability suggests that other confounding factors may be involved, such as ethnicity and environmental effects on gene expression. Although certain studies have recognized gr/gr deletions as a risk factor for impaired spermatogenesis (168),, others failed to conclusively demonstrate this relationship (191-193). The deletion of b1/b3 removes the proximal portion of AZFc. Two of the six copies of RBMY1, the two functional copies of PRY (194), one of the three copies of BPY2 and two of the four DAZ genes are deleted. Nevertheless, large 1.8-Mb deletions have been observed in normozoospermic fertile individuals (195), whereas other researchers have identified this deletion in azoospermic men (196,197). The deletion of b2/b3 removes nearly half of the AZFc region (1.8-Mb DNA segment) and 12 genes, including two copies of DAZ and two copies of BPY. With respect to b1/b2, no conclusive impact on spermatogenesis has been determined (198,199).
The coding genes in AZFc include DAZ and CDY. DAZ plays important roles throughout germ cell development from embryonic life to adulthood; there are four copies of this gene on the Y chromosome (210,211). Postnatally, DAZ encodes proteins that have RNA recognition motifs (RRMs), which are involved in the regulation of RNA translation (200) and control of meiosis. DAZ is essential for the maintenance of the PGC during embryogenesis (201). DAZ2 and DAZ3 each have a single RRM, whereas DAZ1 has two and DAZ4 has three RRMs. There are two autosomal homologues of DAZ: DAZL on chromosome 3q24.3 and BOULE on chromosome 2q33. DAZ gene expression was observed to be reduced in azoospermic patients (202), and partial deletions of DAZ genes appear to be related to oligozoospermia. Two copies of the chromodomain protein Y-linked (CDY) gene are located in the AZFc region. CDY is expressed exclusively in germ cells, where it encodes a protein that contains a chromodomain and a histone acetyltransferase catalytic domain, which is primarily observed in the nucleus of late spermatids. (167). This protein regulates histone hyperacetylation, which is essential to proceed from a histone- to a protamine-based chromatin structure in spermatid nuclei.
Other Y chromosome genes, excluding those that are clustered in intervals 5 and 6 of the long arm, may participate in spermatogenesis. Copies of the TSPY gene have been detected on both Yp and Yq. The protein product of this gene is expressed in spermatogonia and is believed to play a role in the timing of spermatogenesis by signaling to spermatogonia to enter meiosis (168,203). A study of copy number variations of the TSPY gene revealed that more copies were present in infertile patients (204). This finding warrants further investigation of TSPY to characterize its role in azoospermia.
Autosome translocations
Translocations can cause loss of genetic material at gene breakpoints, thereby corrupting the genetic message (205). Autosomal translocations were determined to be 4-10 times more likely in infertile males than in normal males (206,207). Robertsonian translocations, which occur when two acrocentric chromosomes fuse, are the most frequent structural chromosomal abnormalities in humans (32). Although the prevalence of Robertsonian translocations is only 0.8% in infertile males, this prevalence is 9 times higher than that in the general population (39,208). Such translocations can result in a variety of sperm production phenotypes, from normal spermatogenesis to azoospermia (39). Robertsonian translocations are more common in oligozoospermic and azoospermic men, with rates of 1.6 and 0.09%, respectively (209,210). Given the risk of passing on the translocations to offspring, preimplantational genetic screening may be advisable for couples who undergo ART (41).
Monogenic disorders
DAZL is a single-copy gene that is located on chromosome 3. DAZL belongs to the DAZ gene family and is the autosomal homologue of the DAZ gene that is located on the Y chromosome. DAZL is expressed in fetal primordial germ cells, fetal gonocytes and adult male and female germ cells in both the nucleus and cytoplasm. The DAZL protein may regulate protein synthesis and meiosis (211). Although mice with DAZL null mutations are sterile in both sexes and the male germ cells of these animals are arrested at the leptotene stage, no conspicuous mutations in human DAZL that result in sterility have been recognized. Nevertheless, Teng et al., when examining a group of azoospermic and oligozoospermic men in Taiwan, reported that a subset of these men were heterozygous for the single nucleotide polymorphism 386A_G (212). However, these results have not been confirmed in Caucasian men (228), and more studies are required in different populations to examine the role of DAZL mutations and polymorphisms in azoospermia.
The methylenetetrahydrofolate reductase (MTHFR) gene, which is located on the short arm of chromosome 1, encodes an enzyme that catalyzes the conversion of 5,10-methylenetetrahydrofolate to 5-methyltetrahydrofolate. This reaction is important for methionine and S-adenosylmethionine (SAM) synthesis from homocysteine, which is a toxic product, as well as for the synthesis of thymidine. SAM serves as a methyl donor for DNA methyltransferase, which controls DNA methylation, an important process in germ cell development. A recent meta-analytic study revealed that individuals who were homozygous for the single nucleotide polymorphism (SNP) 1298CC (i.e., the CC vs. AA genotype) or who carried a recessive allele (CC vs. AA/AC) were at an increased risk of azoospermia (OR = 1.66 for CC vs. AA; OR = 1.67 for CC vs. AA/AC genotype) (213). This SNP inserts an alanine at position 429. In another meta-analysis, the presence of a MTHFR 677T mutation, in which a valine substitution occurs at amino acid 222 and thus encodes a thermolabile enzyme with reduced activity, is associated with a significantly increased risk of azoospermia (214).
Multifactorial disorders
Cryptorchidism causes an infertile phenotype and appears to be influenced by genetic factors. Mutations in the INSL3 gene (insulin-like 3 on chromosome 19) and its receptor LGR8 (relaxin/insulin-like family peptide receptor 2 on chromosome 13) occur in approximately 5% of men with cryptorchidism and have been linked to the disease (215). Additionally, the first phase of normal testicular descent is controlled by INSL3 (216). The INSL3 gene may also participate in testicular dysgenesis syndrome (TDS) (217), which comprises a variety of disorders that may present alone or in combination. Such disorders include cryptorchidism, hypospadias, an elevated risk of testicular cancer, and infertility. It has been suggested that TDS results from a combination of genetic, environmental, and lifestyle factors (218).
GTDs that affect androgen action or production
Androgen receptor mutations
The androgen receptor (AR) gene is a single-copy gene that is located on Xq11-q12. This gene encodes a cytoplasmic protein that binds specifically to testosterone, and the resultant complex can activate the expression of certain DNA segments. AR is essential for meiosis, in which spermatocytes are converted into round spermatids, and for the appearance of secondary sex characteristics. The AR gene consists of eight exons. Exon 1 encodes the transactivation domain, which activates transcription; exons 2-3 encode the DNA binding domain (DBD); exons 5-8 encode the ligand-binding domain (LBD); and exon 4 encodes the hinge region that connects the DBD and the LBD. From 2004 to the present, the number of reported mutations in the AR gene increased from 605 to 1,029; these mutations have been linked to prostate cancer, male infertility and breast cancer (219). Point mutations, insertions or deletions, and altered CAG repeats can severely impair the amount, structure and function of the AR gene, causing androgen insensitivity syndrome (AIS). The phenotypic manifestation of AIS includes ambiguous genitalia, partial labialscrotal fusions, hypospadias, bifid scrota and gynaecomastia (220). Testosterone and LH levels are consistently elevated in patients with AIS. Although no mutations have been identified in more than 40% of patients, others reported point mutations and polymorphisms in the AR gene in azoospermic men who exhibit normal external genitalia. Alterations in two polymorphic trinucleotide repeats (CAG and GGC) in the 5' region of exon 1 have been implicated in male infertility and azoospermia. Mirfakhraie et al. identified the transversion of 1510C→A in exon 1 of the AR gene in a single patient with SCOS (221). Hose et al. discovered the novel mutation 212A→G in the CAG repeat that resulted in a glutamine-arginine substitution in men with SCOS (222). Although GGC polymorphisms or repeat length alterations are inversely correlated with the transactivation ability of the receptor (223), no marked effects on male fertility potential have been observed.
Steroidogenic acute regulatory protein (StAR) mutations
Testosterone is the most important male androgen, and the major site of its production is the Leydig cells, which account for 75% of testosterone synthesis. Steroidogenic acute regulatory protein (StAR) facilitates the transfer of cholesterol from the outer to the inner mitochondrial membranes; this is the rate-limiting step of testosterone synthesis (224). Congenital lipoid hyperplasia is a rare disease that is caused by frame-shift, missense and nonsense mutations in the StAR gene. This gene spans 8 kb, consists of seven exons and six introns and maps to 8p11.2 (225). Because StAR is the first essential step in the synthesis of all of the steroid hormones in all steroid-synthesizing cells, the classic deficiency of StAR results in a lack of corticosteroids, mineralocorticoids and testosterone. Males with the classic form are born with feminized external genitalia. Given that the condition is life-threatening, the delayed administration of proper hormonal replacement may lead to fatal outcomes shortly after birth. However, a non-classic form has also been described and is characterized by partial protein activity. In such a form, males may be born with external genitalia; nonetheless, they may exhibit compromised fertility potential and azoospermia (226).
3BHSD type 2 deficiency
3BHSD type 2 is one of the intracellular adrenal and gonadal enzymes that is necessary for the synthesis of all steroids. Mutations in the 3BHSD type 2 gene (located at 1p11-13) result in the salt-losing or non-salt-losing forms, which are characterized by female-like genitalia at birth in 46,XY males. These males may develop secondary sexual characteristics at puberty (227).
SRD5A2 mutation
SRD5A2 is a gene that maps to 2p23 and encodes 5-alpha reductase type 2. This enzyme is present in the external genitalia and prostate. Autosomal recessive homozygous mutations in this gene result in feminized external genitalia in 46,XY males. At the time of puberty, signs of masculinization develop due to the activity of 5-alpha reductase type 1 (SRD5A1) in the skin and liver. However, other features, such as prostatic hypoplasia, less body hair and a female frontal hair line, remain. These men are often infertile due to prostatic underdevelopment. Nevertheless, fertility has been reported in certain men due to partial enzymatic activity, which can be conferred by different types of mutations. Epidemiologically, this disease has been reported more frequently in an isolated area in the Dominican Republic (228).
Dysfunctional cell regulatory pathways
Genetic defects at the levels of germ or Sertoli cells in azoospermic men may result from impaired cellular regulatory pathways, culminating in the loss of the germ cells or the arrest of spermatogenesis (229-286). First, exaggerated apoptotic signals due to mutations in the genes that encode for enzymes with crucial roles in apoptosis, such as inducible nitric oxide synthase (iNOS), Fas, FasL, and active caspase 3, affect germ cell proliferation and may result in azoospermia with the SCOS phenotype (245-250). Second, impaired cross-talk or increased immune injury due to mutations in the genes that encode interleukins may lead to maturation arrest or SCOS (229-232). Third, the disruption of Sertoli cell cytoskeletal integrity can result in an inefficient supportive role for spermatogenesis. An intact germ cell cytoskeleton is essential for the regulation of germ cell development; maturation arrest and SCOS are observed when the cell cytoskeleton is disrupted (233-243). Fourth, the cell cycle in mitosis or meiosis should pass through four important phases: G1, S, G2 and M. A defect in any of these phases can result in cell cycle arrest or apoptosis (244-249). Fifth, impaired signal transduction may undermine the response of testicular cells to activating factors, such as hormones and growth factors (248-257). Finally, selective defects in the genes encoding transcription factors in germ and/or supporting cells, such as DAX-1 and nuclear export factor (NF2), have been implicated in NOA (283,284).
Epigenetic defects
Disturbed germ cell nuclear histone acetylation and single-stranded DNA break repair have been implicated in SCOS and maturation arrest (258).
Genetic abnormalities at the primordial germ cell level
The specification, formation, and migration of primordial germ cells toward the developing gonads are all under complex genetic control (287-290). Moreover, several genes regulate the settlement process of primordial germ cells within the testes, the protection of these cells from apoptosis, the formation of gonocytes and the differentiation of germ cells into spermatogonia (291). Spermatogonia undergo proliferative phases that are regulated by many external and internal factors that are encoded by specific genes. Certain genes are activated in each germ cell stage, whereas others are repressed. Selective mutations in the genes that regulate human primordial cell lines are likely to affect male fertility status and may also explain certain cases of non-obstructive azoospermia.
GENETIC TESTING IN AZOOSPERMIA
There are three groups of genetic tests used to detect genetic diseases in azoospermic men: a) cytogenetic tests that detect chromosomal aneuploidy and structural alterations, such as conventional karyotyping; b) polymerase chain reaction to detect Y chromosome microdeletions; and c) specific gene sequencing for mutational analysis of a specific gene.
Conventional karyotyping involves the collection of heparinized peripheral blood samples (approximately 5 ml) from the patient and the isolation of a plasma lymphocyte suspension. Lymphocytes are then transferred to culture media (RPMI) containing a mitotic stimulator (PHA) and incubated for 72 hours. After 70 hours, cell division is arrested at the metaphase stage using colchicine. The cells are then subjected to hypotonic treatment (KCl) and fixed with Karnovsky fixative overnight at 4°C. Finally, the cells are spread on a clean, grease-free wet slide and subjected to GTG banding for karyotyping (292). The standard protocols are available in various practical guidelines and should be optimized for different laboratory conditions (293). Cytogenetic analysis is the most frequently used diagnostic test in the evaluation of patients with azoospermia (294,295).
The Y chromosome microdeletion (YCMD) assay is a PCR-based blood test that detects the presence or absence of defined sequence-tagged sites (STSs). This technique therefore enables the detection of the presence or absence of any clinically relevant microdeletion. Yq microdeletion analysis is generally performed using multiplex polymerase chain reaction (PCR) to amplify the AZFa, AZFb, and AZFc loci in the long arm of the Y chromosome. The set of PCR primers that are used to amplify the AZF regions is important in the identification of deletions (296). The PCR should be performed at least twice in the presence of an internal control (SRY), as well as positive and negative controls, to confirm the presence of deletions. PCR is a rapid method for the detection of submicroscopic Y chromosome deletions, which conventional cytogenetic analysis is unable to resolve. To obtain uniform results, it is necessary to follow the same guidelines for the entire examined population. The European Association of Andrology (EAA) recommends the use of a set of seven markers in men with idiopathic infertility who present with severe oligozoospermia or azoospermia: six STSs in the AZF locus, and one STS (sY14) in the SRY locus, the latter of which is the internal control. Y chromosome infertility is inherited in a Y-linked manner.
For specific gene sequencing and mutational analyses, the “dye terminator sequence” method is performed. This method is a high-throughput, automated, more efficient and more rapid method than the original Sanger method of sequencing. The principle, which is similar to that of Sanger's method, depends on the premature termination of four separate sequencing reactions that contain all four of the standard deoxynucleotides (dATP, dGTP, dCTP, and dTTP) and the DNA polymerase. To each reaction is added only one of the four dideoxynucleotides (ddATP, ddGTP, ddCTP, or ddTTP), which are chain-terminating nucleotides that lack the 3'-OH group required for the formation of a phosphodiester bond between two nucleotides. Thus, DNA strand extension is terminated, resulting in DNA fragments of varying lengths. Next, these labeled DNA fragments are separated by gel electrophoresis on a denaturing polyacrylamide-urea gel and read in a specific manner from the shortest to the longest (297).
Table 2) summarizes the currently available genetic tests for azoospermic men who seek fertility counseling.
Table 2.
Table 2 - Genetic testing that is currently available for the investigation of azoospermia
| Phenotype | Genetic point of interest | Type of testing |
| Post-testicular azoospermia (obstructive azoospermia) | CFTR gene | Mutational analysis of the CFTR gene in cases of CAVD, congenital epididymal obstruction and normal vasa, and Young syndrome |
| Long arm of the Y chromosome | Polymerase chain reaction to detect Y chromosome microdeletion | |
| Testicular azoospermia (non-obstructive azoospermia) | Autosome and sexual chromosomes | Cytogenetic analysis to detect chromosomal aneuploidy and structural alterations |
| Androgen receptor gene | CAG repeat/AR mutation analysis for androgen insensitivity syndrome (AIS) | |
| X-linked USP 26, X-linked SOX3, LH and FSH receptors, X-linked TAF7L, DAZL, MTHFR, ER1, ER2, and FSH | Mutational analysis of the specific gene | |
| KAL1, FGFR, PROK2, PROKR2, FGF8, CDH7, KISS1, GPR54, TAC3, TACR3, GnRH, and GnRHR | Mutational analysis of genes related to Kallmann syndrome and normosmic HH | |
| Pre-testicular azoospermia (HH) | PROP1, LHX, and SOX2 | Mutational analysis of genes related to generalized pituitary insufficiency |
| FSH and LH genes, and FSH and LH receptor genes | Mutational analysis of the genes that code for the secretion of FSH and LH, and their receptors, in cases of selective gonadotropin deficiency | |
| Complex/multifactorial genetic disorders | NR5A1 gene | Mutational analysis of the specific gene in cases of bilateral anorchia |
| INSL3 gene and its receptor | Mutational analysis of the specific genes in cryptorchidism | |
| PTPN11, SOS1, KRAS, NRAS, RAF1, BRAF, SHOC2, MEK1, and CBL genes | Mutational analysis of the specific genes in Noonan syndrome | |
| Chromosome 15 | Cytogenetic/FISH analysis to detect deletions, maternal uniparental disomy of chromosome 15q11-q13 or the disruption of paternally inherited chromosome 15 in Prader-Willi syndrome | |
| Steroid 5-alpha-reductase 2 (SRD5A2) gene | Mutation analysis of the specific gene in cases of SRD5A2 deficiency |
CAVD: congenital agenesis of the vas deferens; CFTR: cystic fibrosis transmembrane regulator protein, FISH: fluorescence in situ hybridization; FSH: follicle-stimulating hormone; LH: luteinizing hormone; GnRH: gonadotropin-releasing hormone; HH: hypogonadotropic hypogonadism.
EXPERT COMMENTARY
The aim of this article was to review the current knowledge of the genetic basis of azoospermia and to highlight the requirement for genetic testing in such conditions. Thousands of single or multiple genes are involved in establishing the male fertility potential, and many others are yet to be revealed. Currently, genetic testing ranges from the chromosomal level to specific gene mutations. Single gene disorders are important for understanding the etiology of male infertility. Moreover, testing can aid in the improved management of couples who seek genetic counseling prior to conception.
The initial evaluation of infertile men generally commences with history taking and a thorough physical examination. These steps are followed by an initial seminal fluid analysis and, if required, endocrine profile testing and imaging analysis. Until approximately two decades ago, the understanding of the genetic basis of infertility was of limited value for it provided only a diagnosis. In the current era of ART, however, genetic testing have emerged as tools of paramount importance in helping clinicians not only to explore the specific genetic background of a disease but also to take the necessary precautions to prevent the transmission of the disease to the offspring via assisted conception. Certain genetic defects are associated with increased morbidity, childhood cancer and genital ambiguity. As such, genetic testing in azoospermic males allows couples to make educated decisions regarding their choice to use a sperm donor or to opt for advanced assisted conception techniques. Such techniques can be coupled with preimplantation genetic diagnosis (PGD) if an abnormal result is obtained. Compiling the data from the initial evaluation that include history and physical examination may segregate azoospermic men into four major groups based on their probability of harboring male fertility-related genetic diseases. For the first group, who present with a history and a physical examination that is consistent with cryptorchidism, Noonan syndrome, bilateral anorchia or Prader-Willi syndrome, certain genetic tests are available; however, these tests are not routinely used. In the second group, azoospermic men with clear evidence of seminal duct obstruction based on physical examination (CBAVD, Young syndrome) require testing for CFTR mutations. The third group encompasses men with non-obstructive azoospermia. For such individuals, after the exclusion of acquired testicular pathologies and a history of exposure to gonadotoxins, such as radiation and chemotherapy, genetic testing, including karyotype and Yq microdeletion analyses, should be set as minimum standards (Table 2). Lastly, for men with feminized or ambiguous external genitalia, the genetic workup should also include androgen receptor genetic analysis.
Chromosomal defects are the most common genetic abnormalities in infertile men with azoospermia and may account for as many as 15% of cases (298-302). The most common chromosomal aberrations that are associated with severe spermatogenic defects are sex chromosome aneuploidies and chromosomal translocations. Among the various cytogenetic abnormalities, Klinefelter syndrome is the major cytogenetic/sex chromosome/numerical anomaly that is detected in infertile men, followed by translocations, deletions and inversions. Cytogenetic abnormalities may predispose to malsegregation and/or abnormal embryonic development (303). Moreover, the occurrence of aneuploid embryos after IVF and ICSI will not only decrease the success rate of the treatment (304) but also increase the risk of both an unbalanced translocation and altered amount of genetic material in the offspring. Thus, PGD may be useful for certain couples undergoing IVF treatment.
Y microdeletion screening is mandatory in infertile men with azoospermia of unknown origin who opt for ART. Y chromosome microdeletions are observed in as many as 15% of men with NOA (59,296,297). Yq microdeletion screening may not only identify the cause of azoospermia but also predict the probability of sperm retrieval in ART candidates. In cases that involve AZFa and/or AZFb microdeletions, sperm retrieval is currently not recommended because there is no evidence that testicular sperm can be found, irrespective of the retrieval method (56-59). Conversely, sperm can be retrieved from the testes in approximately 70% of cases that involve AZFc Yq microdeletions (56-59,305). In such cases, ICSI can be performed. The probability of fatherhood by ICSI is unaltered by the presence of AZFc microdeletions (305). However, ART-derived male offspring will inherit the Yq microdeletion, potentially resulting in subsequent infertility. The probability of whole Y chromosome deletion also increases in such cases, which may lead to genital ambiguity in the offspring (306). Female fetuses from a father with a Y chromosome deletion have no increased risk of congenital abnormalities or infertility. Given that males with deletion of the AZF regions of the long arm of the Y chromosome are infertile, the deletions are generally de novo and are therefore absent from the father of the proband. Rarely, within a family, the same deletion of the Y chromosome can cause infertility in certain males but not in others; thus, certain fertile males with a deletion in the AZF regions have fathered sons who are infertile (57-59). In pregnancies that are conceived via assisted reproduction and that are known to include the risk of producing a male with a Y chromosome deletion, specific prenatal testing or preimplantation testing may be performed to determine the sex of the fetus and/or the presence of the Y chromosome deletion (292).
Mutations in the cystic fibrosis gene are the most common genetic mutations that result in azoospermia. Congenital bilateral absence of the vas deferens (CBAVD) is a syndromic disorder that is characterized by the absence of the vas deferens and accounts for at least 6% of cases of obstructive azoospermia and approximately 2% of infertility cases. CFTR mutations are responsible for CBAVD in at least 95% of men, and CFTR analysis is one of the most important genetic tests in infertility cases (obstructive azoospermia) (307). Patients with CAVD due to CFTR mutations are at risk of having both male and female offspring with cystic fibrosis and male offspring with CAVD, given the relatively high carrier rate of CFTR mutations (e.g., 4% in the Caucasian population) (259). Screening for CFTR mutations may also be recommended for men with Young syndrome and for those with unilateral vasal agenesis before attempting to conceive (40). Ideally, both partners should be screened prior to assisted reproductive techniques (ART) to determine the risk of transmitting CFTR mutations to the offspring (41). Up-to-date information on CFTR mutations can be found at http://www. genet.sickkids.on.ca/cftr/app, which is a CFTR mutation database. Different techniques, such as Western-blotting, in situ hybridization, fluorescence in situ hybridization, single-strand conformation polymorphism analysis, heteroduplex analysis, PCR, and real time PCR followed by direct sequencing, have been developed to screen for CFTR mutations. PGD has been regarded as a useful tool to identify the presence of CFTR mutations in in vitro-derived embryos, assuming that both the male and female partners have been screened for genetic mutations.
In azoospermia, genetic testing using karyotyping, Yq chromosome microdeletion analysis and CFTR mutation screening reveals a genetic etiology in approximately 30% of cases. A summary of the current recommendations for genetic testing in azoospermia is presented in Table 3).
Table 3.
Table 3 - The current recommendations for genetic testing in azoospermia based on clinical phenotypes
| Genetic test | Phenotype | Recommendation |
| Cytogenetic analysis | Non-obstructive azoospermia | Mandatory |
| Yq microdeletion analysis | Non-obstructive azoospermia | Mandatory |
| Cystic fibrosis transmembrane conductance regulator (CFTR) mutation analysis | Obstructive azoospermia and congenital absence of the vas deferens (CAVD) or congenital bilateral epididymal obstruction and normal vasa | Highly Recommended |
| KAL1 mutation analysis | Kallmann syndrome (KS) | Recommended |
| CAG repeat/AR mutation analysis | Androgen insensitivity syndrome (AIS) | Recommended |
| Steroid 5-alpha-reductase 2 (SRD5A2) mutation analysis | SRD5A2 deficiency | Recommended |
| Lutenizing hormone (LH ) receptor mutation analysis | Pseudohermaphroditism , azoospermia, micropenis, delayed puberty and arrest of spermatogenesis | Suggested |
| Gonadotropin-releasing hormone (GnRH) mutation analysis | Low serum LH and FSH levels | Suggested |
| DAZL/MTHFR mutation analysis | Non-obstructive azoospermia | Suggested |
Incorporating novel techniques, such as genomics, proteomics, and metabolomics, into infertility research may assist in the creation of a complete portrait of the genes that are involved in infertility and would allow for improvements in ART and the development of more targeted solutions (297). Microarrays are emerging as valuable tools for the determination of the gene expression profiles of infertile phenotypes (308). Microarray technology is also useful in the examination of spermatogenesis. An analysis of gene expression over time may be performed to identify the genes that are involved in each spermatogenic stage. Genomic analyses can also be used to determine differentially transcribed genes (309). An enhanced understanding of transcriptional regulation could aid geneticists in the discovery of the mechanisms by which different expression patterns impact a patient's fertility status. However, because the results of gene expression microarray studies are variable, it would be necessary to determine global gene expression patterns of RNA samples from the testis before this type of analysis become clinically relevant. Grouping the expressed genes into functional categories may allow the characterization of a gene expression signature for normal human spermatogenesis, which could be used as a diagnostic marker. Proteins are identified using two-dimensional electrophoresis and mass spectrometry techniques, and the results are used to create proteome maps in relation to sperm and seminal plasma (310,311). The identification of protein biomarkers for male factor infertility will allow for unbiased comparisons of fertile and infertile males and will clarify the pathophysiology of the disease. An advantageous characteristic of genomic and proteomic technology is that the results provide a definitive characterization of infertile phenotypes. The use of technologies such as genomics and proteomics is a step toward creating personalized medical diagnoses by determining the individual causes of infertility (309). Finally, metabolomics involves the measurement of metabolite expression. Metabolites are small biomarkers that indicate the functionality of a cell and characterize certain diseases or physiological states. The determination of the human metabolome will reveal the functional phenotype of the system being examined, whether it is a single cell or an entire organism. Mass spectroscopy, nuclear magnetic resonance spectroscopy, and other chromatography methods can be used to create metabolite profiles. Pathway or cluster analyses are used to identify subsets of metabolites that can facilitate more accurate diagnosis (309-311). By identifying differences in the metabolome of infertile phenotypes, novel noninvasive methods for the diagnosis and treatment of male factor infertility can be developed.
KEY POINTS
Approximately 2,000 genes have been implicated in male fertility. There is a genetic basis for both the hypothalamic pituitary gonadal axis control of sperm production and the molecular events that characterize this process. Moreover, genes control the formation of the ductal system and orchestrate sperm function during fertilization.
Currently, genetic abnormalities explain approximately 1/3 of azoospermia cases. Although 12-41% of azoospermic cases are idiopathic, it is likely that these cases have unknown genetic causes.
Azoospermia of genetic origin primarily encompasses men with any of a wide variety of genetic disorders, including chromosomal abnormalities, monogenic disorders, multifactorial genetic diseases, and epigenetic disorders.
Sex and numerical chromosomal abnormalities (Klinefelter syndrome and Robertsonian translocations), gene deletions (Yq chromosome microdeletions) and mutations (CF mutations) are the most common abnormalities in the context of azoospermia.
Three groups of genetic tests are used to detect genetic diseases in azoospermic men: cytogenetic tests (karyotyping) to detect chromosomal aneuploidy and structural alterations, PCR to detect Y chromosome microdeletions, and specific gene sequencing analyses (mutational analysis of a specific gene).
A high frequency of CFTR mutations is detected in men with obstructive azoospermia who present with congenital bilateral or unilateral absence of the vas deferens and bilateral epididymal obstruction.
Non-obstructive azoospermia is primarily due to pretesticular and testicular defects; each of these conditions has a multitude of genetic causes.
Depending on whether the azoospermia is obstructive (OA) or non-obstructive (NOA), one can determine which genes require analysis. CFTR gene analysis is recommended in OA, whereas karyotyping and Yq microdeletion analyses are recommended in NOA.
Yq microdeletion screening may not only identify the cause of azoospermia but also predict the probability of sperm retrieval in ART candidates. ART-derived male offspring will inherit the Yq microdeletion, potentially resulting in subsequent infertility.
Genetic testing in infertile males allows couples to make educated decisions regarding whether to use a sperm donor or to opt for advanced ART and a preimplantation genetic diagnosis if an abnormal result is revealed.
The inability to identify a specific genetic etiology in idiopathic azoospermia carries an increased risk of the transmission of the same trait to the offspring.
Incorporating novel techniques, such as genomics, proteomics, and metabolomics, into infertility research could assist in the creation of a complete portrait of the genes that are involved in infertility and would allow for improvements in ART and the development of more targeted solutions.
Footnotes
No potential conflict of interest was reported.
REFERENCES
- 1.Bhasin S, de Kretser DM, Baker HW. Clinical review 64: Pathophysiology and natural history of male infertility. J Clin Endocrinol Metab. 1994;79(6):1525–9. doi: 10.1210/jcem.79.6.7989450. [DOI] [PubMed] [Google Scholar]
- 2.Bablok L, Dziadecki W, Szymusik I, Wolczynski S, Kurzawa R, Pawelczyk L, et al. Patterns of infertility in Poland - multicenter study. Neuro Endocrinol Lett. 32(6):799–804. [PubMed] [Google Scholar]
- 3.Jarow JP, Sharlip ID, Belker AM, Lipshultz LI, Sigman M, Thomas AJ, et al. Best practice policies for male infertility. J Urol. 2002;167(5):2138–44. [PubMed] [Google Scholar]
- 4.Anderson JE, Farr SL, Jamieson DJ, Warner L, Macaluso M. Infertility services reported by men in the United States: national survey data. Fertil Steril. 2009;91(6):2466–70. doi: 10.1016/j.fertnstert.2008.03.022. [DOI] [PubMed] [Google Scholar]
- 5.Jarvi K, Lo K, Fischer A, Grantmyre J, Zini A, Chow V, et al. CUA Guideline: The workup of azoospermic males. Can Urol Assoc J. 4(3):163–7. doi: 10.5489/cuaj.10050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jarow JP, Espeland MA, Lipshultz LI. Evaluation of the azoospermic patient. J Urol. 1989;142(1):62–5. doi: 10.1016/s0022-5347(17)38662-7. [DOI] [PubMed] [Google Scholar]
- 7.Hernandez Uribe L, Hernandez Marin I, Cervera-Aguilar R, Ayala AR. [Frequency and etiology of azoospermia in the study of infertile couples] Ginecol Obstet Mex. 2001;69:322–6. [PubMed] [Google Scholar]
- 8.Coat C, Perrin A, Talagas M, Tetefort R, Amice J, Valeri A, et al. [Azoospermia: management and results: a series of 90 cases] Prog Urol. 21(13):946–54. doi: 10.1016/j.purol.2011.06.004. [DOI] [PubMed] [Google Scholar]
- 9.Lee JY, Dada R, Sabanegh E, Carpi A, Agarwal A. Role of genetics in azoospermia. Urology. 77(3):598–601. doi: 10.1016/j.urology.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 10.Ghazzawi IM, Sarraf MG, Taher MR, Khalifa FA. Comparison of the fertilizing capability of spermatozoa from ejaculates, epididymal aspirates and testicular biopsies using intracytoplasmic sperm injection. Hum Reprod. 1998;13(2):348–52. doi: 10.1093/humrep/13.2.348. [DOI] [PubMed] [Google Scholar]
- 11.Verza S, Jr, Esteves SC. Sperm defect severity rather than sperm Source is associated with lower fertilization rates after intracytoplasmic sperm injection. Int Braz J Urol. 2008;34(1):49–56. doi: 10.1590/s1677-55382008000100008. [DOI] [PubMed] [Google Scholar]
- 12.Aboulghar MA, Mansour RT, Serour GI, Fahmy I, Kamal A, Tawab NA, et al. Fertilization and pregnancy rates after intracytoplasmic sperm injection using ejaculate semen and surgically retrieved sperm. Fertil Steril. 1997;68(1):108–11. doi: 10.1016/s0015-0282(97)81484-7. [DOI] [PubMed] [Google Scholar]
- 13.Palermo GD, Schlegel PN, Hariprashad JJ, Ergun B, Mielnik A, Zaninovic N, et al. Fertilization and pregnancy outcome with intracytoplasmic sperm injection for azoospermic men. Hum Reprod. 1999;14(3):741–8. doi: 10.1093/humrep/14.3.741. [DOI] [PubMed] [Google Scholar]
- 14.Schwarzer JU, Fiedler K, Hertwig I, Krusmann G, Wurfel W, Muhlen B, et al. Male factors determining the outcome of intracytoplasmic sperm injection with epididymal and testicular spermatozoa. Andrologia. 2003;35(4):220–6. doi: 10.1046/j.1439-0272.2003.00563.x. [DOI] [PubMed] [Google Scholar]
- 15.Ghanem M, Bakr NI, Elgayaar MA, El Mongy S, Fathy H, Ibrahim AH. Comparison of the outcome of intracytoplasmic sperm injection in obstructive and non-obstructive azoospermia in the first cycle: a report of case series and meta-analysis. Int J Androl. 2005;28(1):16–21. doi: 10.1111/j.1365-2605.2005.00491.x. [DOI] [PubMed] [Google Scholar]
- 16.Semiao-Francisco L, Braga DP, Figueira Rde C, Madaschi C, Pasqualotto FF, Iaconelli A, Jr, et al. Assisted reproductive technology outcomes in azoospermic men: 10 years of experience with surgical sperm retrieval. Aging Male. 2010;13(1):44–50. doi: 10.3109/13685530903342203. [DOI] [PubMed] [Google Scholar]
- 17.Tuttelmann F, Werny F, Cooper TG, Kliesch S, Simoni M, Nieschlag E. Clinical experience with azoospermia: aetiology and chances for spermatozoa detection upon biopsy. Int J Androl. 2011;34(4):291–8. doi: 10.1111/j.1365-2605.2010.01087.x. [DOI] [PubMed] [Google Scholar]
- 18.Radpour R, Gourabi H, Dizaj AV, Holzgreve W, Zhong XY. Genetic investigations of CFTR mutations in congenital absence of vas deferens, uterus, and vagina as a cause of infertility. J Androl. 2008;29(5):506–13. doi: 10.2164/jandrol.108.005074. [DOI] [PubMed] [Google Scholar]
- 19.Rommens JM, Iannuzzi MC, Kerem B, Drumm ML, Melmer G, Dean M, et al. Identification of the cystic fibrosis gene: chromosome walking and jumping. Science. 1989;245(4922):1059–65. doi: 10.1126/science.2772657. [DOI] [PubMed] [Google Scholar]
- 20.Radpour R, Gourabi H, Gilani MA, Dizaj AV. Molecular study of (TG)m(T)n polymorphisms in Iranian males with congenital bilateral absence of the vas deferens. J Androl. 2007;28(4):541–7. doi: 10.2164/jandrol.106.002337. [DOI] [PubMed] [Google Scholar]
- 21.Wong PY. CFTR gene and male fertility. Mol Hum Reprod. 1998;4(2):107–10. doi: 10.1093/molehr/4.2.107. [DOI] [PubMed] [Google Scholar]
- 22.Patrizio P, Salameh WA. Expression of the cystic fibrosis transmembrane conductance regulator (CFTR) mRNA in normal and pathological adult human epididymis. J Reprod Fertil Suppl. 1998;53:261–70. [PubMed] [Google Scholar]
- 23.Chan HC, Ruan YC, He Q, Chen MH, Chen H, Xu WM, et al. The cystic fibrosis transmembrane conductance regulator in reproductive health and disease. J Physiol. 2009;587(Pt 10):2187–95. doi: 10.1113/jphysiol.2008.164970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Huynh T, Mollard R, Trounson A. Selected genetic factors associated with male infertility. Hum Reprod Update. 2002;8(2):183–98. doi: 10.1093/humupd/8.2.183. [DOI] [PubMed] [Google Scholar]
- 25.Taussig LM, Lobeck CC, di Sant'Agnese PA, Ackerman DR, Kattwinkel J. Fertility in males with cystic fibrosis. N Engl J Med. 1972;287(12):586–9. doi: 10.1056/NEJM197209212871204. [DOI] [PubMed] [Google Scholar]
- 26.Mocanu E, Shattock R, Barton D, Rogers M, Conroy R, Sheils O, et al. All azoospermic males should be screened for cystic fibrosis mutations before intracytoplasmic sperm injection. Fertil Steril. 2010;94(6):2448–50. doi: 10.1016/j.fertnstert.2010.02.029. [DOI] [PubMed] [Google Scholar]
- 27.Cruger DG, Agerholm I, Byriel L, Fedder J, Bruun-Petersen G. Genetic analysis of males from intracytoplasmic sperm injection couples. Clin Genet. 2003;64(3):198–203. doi: 10.1034/j.1399-0004.2003.00128.x. [DOI] [PubMed] [Google Scholar]
- 28.Tsai MF, Jih KY, Shimizu H, Li M, Hwang TC. Optimization of the degenerated interfacial ATP binding site improves the function of disease-related mutant cystic fibrosis transmembrane conductance regulator (CFTR) channels. J Biol Chem. 2010;285(48):37663–71. doi: 10.1074/jbc.M110.172817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Claustres M, Guittard C, Bozon D, Chevalier F, Verlingue C, Ferec C, et al. Spectrum of CFTR mutations in cystic fibrosis and in congenital absence of the vas deferens in France. Hum Mutat. 2000;16(2):143–56. doi: 10.1002/1098-1004(200008)16:2<143::AID-HUMU7>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 30.Tsui LC. Mutations and sequence variations detected in the cystic fibrosis transmembrane conductance regulator (CFTR) gene: a report from the Cystic Fibrosis Genetic Analysis Consortium. Hum Mutat. 1992;1(3):197–203. doi: 10.1002/humu.1380010304. [DOI] [PubMed] [Google Scholar]
- 31.Morral N, Llevadot R, Casals T, Gasparini P, Macek M, Jr, Dork T, et al. Independent origins of cystic fibrosis mutations R334W, R347P, R1162X, and 3849 + 10kbC–>T provide evidence of mutation recurrence in the CFTR gene. Am J Hum Genet. 1994;55(5):890–8. [PMC free article] [PubMed] [Google Scholar]
- 32.Ferlin A, Raicu F, Gatta V, Zuccarello D, Palka G, Foresta C. Male infertility: role of genetic background. Reprod Biomed Online. 2007;14(6):734–45. doi: 10.1016/s1472-6483(10)60677-3. [DOI] [PubMed] [Google Scholar]
- 33.Oates RD, Amos JA. The genetic basis of congenital bilateral absence of the vas deferens and cystic fibrosis. J Androl. 1994;15(1):1–8. [PubMed] [Google Scholar]
- 34.Patrizio P, Leonard DG. Mutations of the cystic fibrosis gene and congenital absence of the vas deferens. Results Probl Cell Differ. 2000;28:175–86. doi: 10.1007/978-3-540-48461-5_7. [DOI] [PubMed] [Google Scholar]
- 35.Gervais R, Dumur V, Rigot JM, Lafitte JJ, Roussel P, Claustres M, et al. High frequency of the R117H cystic fibrosis mutation in patients with congenital absence of the vas deferens. N Engl J Med. 1993;328(6):446–7. doi: 10.1056/NEJM199302113280619. [DOI] [PubMed] [Google Scholar]
- 36.Ratbi I, Legendre M, Niel F, Martin J, Soufir JC, Izard V, et al. Detection of cystic fibrosis transmembrane conductance regulator (CFTR) gene rearrangements enriches the mutation spectrum in congenital bilateral absence of the vas deferens and impacts on genetic counselling. Hum Reprod. 2007;22(5):1285–91. doi: 10.1093/humrep/dem024. [DOI] [PubMed] [Google Scholar]
- 37.Jezequel P, Dubourg C, Le Lannou D, Odent S, Le Gall JY, Blayau M, et al. Molecular screening of the CFTR gene in men with anomalies of the vas deferens: identification of three novel mutations. Mol Hum Reprod. 2000;6(12):1063–7. doi: 10.1093/molehr/6.12.1063. [DOI] [PubMed] [Google Scholar]
- 38.Yu J, Chen Z, Ni Y, Li Z. CFTR mutations in men with congenital bilateral absence of the vas deferens (CBAVD): a systemic review and meta-analysis. Hum Reprod. 27(1):25–35. doi: 10.1093/humrep/der377. [DOI] [PubMed] [Google Scholar]
- 39.Georgiou I, Syrrou M, Pardalidis N, Karakitsios K, Mantzavinos T, Giotitsas N, et al. Genetic and epigenetic risks of intracytoplasmic sperm injection method. Asian J Androl. 2006;8(6):643–73. doi: 10.1111/j.1745-7262.2006.00231.x. [DOI] [PubMed] [Google Scholar]
- 40.Donohue RE, Fauver HE. Unilateral absence of the vas deferens. A useful clinical sign. JAMA. 1989;261(8):1180–2. [PubMed] [Google Scholar]
- 41.Kolettis PN, Sandlow JI. Clinical and genetic features of patients with congenital unilateral absence of the vas deferens. Urology. 2002;60(6):1073–6. doi: 10.1016/s0090-4295(02)01973-8. [DOI] [PubMed] [Google Scholar]
- 42.Radpour R, Gourabi H, Gilani MA, Dizaj AV. Correlation between CFTR gene mutations in Iranian men with congenital absence of the vas deferens and anatomical genital phenotype. J Androl. 2008;29(1):35–40. doi: 10.2164/jandrol.107.002972. [DOI] [PubMed] [Google Scholar]
- 43.Mak V ZJ, Tsui L-C, Durie P, Zini A, Martin S, Longley TB Jarvi KA. Proportion of cystic fibrosis gene mutations not detected by routine testing in men with obstructive azoospermia. J Am Med Assoc. 1999;281(23):2217–24. doi: 10.1001/jama.281.23.2217. [DOI] [PubMed] [Google Scholar]
- 44.Casals T, Bassas L, Egozcue S, Ramos MD, Gimenez J, Segura A, et al. Heterogeneity for mutations in the CFTR gene and clinical correlations in patients with congenital absence of the vas deferens. Hum Reprod. 2000;15(7):1476–83. doi: 10.1093/humrep/15.7.1476. [DOI] [PubMed] [Google Scholar]
- 45.Dork T, Dworniczak B, Aulehla-Scholz C, Wieczorek D, Bohm I, Mayerova A, et al. Distinct spectrum of CFTR gene mutations in congenital absence of vas deferens. Hum Genet. 1997;100(3-4):365–77. doi: 10.1007/s004390050518. [DOI] [PubMed] [Google Scholar]
- 46.Mak V, Zielenski J, Tsui LC, Durie P, Zini A, Martin S, et al. Proportion of cystic fibrosis gene mutations not detected by routine testing in men with obstructive azoospermia. JAMA. 1999;281(23):2217–24. doi: 10.1001/jama.281.23.2217. [DOI] [PubMed] [Google Scholar]
- 47.Jarvi K, Zielenski J, Wilschanski M, Durie P, Buckspan M, Tullis E, et al. Cystic fibrosis transmembrane conductance regulator and obstructive azoospermia. Lancet. 1995;345(8964):1578. doi: 10.1016/s0140-6736(95)91131-6. [DOI] [PubMed] [Google Scholar]
- 48.Hendry WF, Levison DA, Parkinson MC, Parslow JM, Royle MG. Testicular obstruction: clinicopathological studies. Ann R Coll Surg Engl. 1990;72(6):396–407. [PMC free article] [PubMed] [Google Scholar]
- 49.Arya AK, Beer HL, Benton J, Lewis-Jones I, Swift AC. Does Young's syndrome exist. J Laryngol Otol. 2009;123(5):477–81. doi: 10.1017/S0022215109004307. [DOI] [PubMed] [Google Scholar]
- 50.Teichtahl H, Temple-Smith PD, Johnson JL, Southwick GJ, de Kretser DM. Obstructive azoospermia and chronic sinobronchial disease (Young's syndrome) in identical twins. Fertil Steril. 1987;47(5):879–81. doi: 10.1016/s0015-0282(16)59186-9. [DOI] [PubMed] [Google Scholar]
- 51.Umeki S, Soejima R, Kawane H. Young's syndrome accompanied by medullary sponge kidney. Respiration. 1989;55(1):60–4. doi: 10.1159/000195707. [DOI] [PubMed] [Google Scholar]
- 52.Handelsman DJ, Conway AJ, Boylan LM, Turtle JR. Young's syndrome. Obstructive azoospermia and chronic sinopulmonary infections. N Engl J Med. 1984;310(1):3–9. doi: 10.1056/NEJM198401053100102. [DOI] [PubMed] [Google Scholar]
- 53.Meschede D, Dworniczak B, Nieschlag E, Horst J. Genetic diseases of the seminal ducts. Biomed Pharmacother. 1998;52(5):197–203. doi: 10.1016/S0753-3322(98)80016-4. [DOI] [PubMed] [Google Scholar]
- 54. Geracioti TD SJ, Ekhator NN. Pfaff DW A A, Etgen A M, Fahrbach S E, Rubin R T, Neuroregulatory peptides of central nervous system origin: from laboratory to clinic Hormones, Brain and Behavior 2009New York: Elsevier Inc. Academic Press; 2541–96. [Google Scholar]
- 55.Schwarting GA, Wierman ME, Tobet SA. Gonadotropin-releasing hormone neuronal migration. Semin Reprod Med. 2007;25(5):305–12. doi: 10.1055/s-2007-984736. [DOI] [PubMed] [Google Scholar]
- 56.Knobil E. The electrophysiology of the GnRH pulse generator in the rhesus monkey. J Steroid Biochem. 1989;33(4B):669–71. doi: 10.1016/0022-4731(89)90476-7. [DOI] [PubMed] [Google Scholar]
- 57.van Tijn DA, Schroor EJ, Delemarre-van de Waal HA, de Vijlder JJ, Vulsma T. Early assessment of hypothalamic-pituitary-gonadal function in patients with congenital hypothyroidism of central origin. J Clin Endocrinol Metab. 2007;92(1):104–9. doi: 10.1210/jc.2006-0689. [DOI] [PubMed] [Google Scholar]
- 58.Layman LC, Reindollar RH. Diagnosis and Treatment of Pubertal Disorders. Adolesc Med. 1994;5(1):37–56. [PubMed] [Google Scholar]
- 59.Bianco SD, Kaiser UB. The genetic and molecular basis of idiopathic hypogonadotropic hypogonadism. Nat Rev Endocrinol. 2009;5(10):569–76. doi: 10.1038/nrendo.2009.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Pallais JC AM, Pitteloud N. Kallmann Syndrome, Genes Review NCBI Bookshelf Bookshelf US national Library of Medicine, National Institute of Health; 2011. Available from: US national Library of Medicine, National Institute of Health Web site. http://0-www.ncbi.nlm.nih.gov.library.ccf.org/books/NBK1334/ [Google Scholar]
- 61.Dode C, Hardelin JP. Kallmann syndrome. Eur J Hum Genet. 2009;17(2):139–46. doi: 10.1038/ejhg.2008.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Behre HM NE, Partsch CJ, et al. Nieschlag E B H, Nieschlag S, edDiseases of the hypothalamus and the pituitary gland Andrology Male Reproductive Health and Dysfunction Verlag Berlin Heidelberg 2010Germany: Springer; 169–92.In: [Google Scholar]
- 63.Bhagavath B, Podolsky RH, Ozata M, Bolu E, Bick DP, Kulharya A, et al. Clinical and molecular characterization of a large sample of patients with hypogonadotropic hypogonadism. Fertil Steril. 2006;85(3):706–13. doi: 10.1016/j.fertnstert.2005.08.044. [DOI] [PubMed] [Google Scholar]
- 64.Trarbach EB. Copy number variation associated with Kallmann syndrome: new genetics insights from genome-wide studies. Asian J Androl. 2011;13(2):203–4. doi: 10.1038/aja.2010.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Iafrate AJ, Feuk L, Rivera MN, Listewnik ML, Donahoe PK, Qi Y, et al. Detection of large-scale variation in the human genome. Nat Genet. 2004;36(9):949–51. doi: 10.1038/ng1416. [DOI] [PubMed] [Google Scholar]
- 66.Redon R, Ishikawa S, Fitch KR, Feuk L, Perry GH, Andrews TD, et al. Global variation in copy number in the human genome. Nature. 2006;444(7118):444–54. doi: 10.1038/nature05329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.del Castillo I, Cohen-Salmon M, Blanchard S, Lutfalla G, Petit C. Structure of the X-linked Kallmann syndrome gene and its homologous pseudogene on the Y chromosome. Nat Genet. 1992;2(4):305–10. doi: 10.1038/ng1292-305. [DOI] [PubMed] [Google Scholar]
- 68.Kim SH, Hu Y, Cadman S, Bouloux P. Diversity in fibroblast growth factor receptor 1 regulation: learning from the investigation of Kallmann syndrome. J Neuroendocrinol. 2008;20(2):141–63. doi: 10.1111/j.1365-2826.2007.01627.x. [DOI] [PubMed] [Google Scholar]
- 69.Ballabio A, Andria G. Deletions and translocations involving the distal short arm of the human X chromosome: review and hypotheses. Hum Mol Genet. 1992;1(4):221–7. doi: 10.1093/hmg/1.4.221. [DOI] [PubMed] [Google Scholar]
- 70.Parenti G, Rizzolo MG, Ghezzi M, Di Maio S, Sperandeo MP, Incerti B, et al. Variable penetrance of hypogonadism in a sibship with Kallmann syndrome due to a deletion of the KAL gene. Am J Med Genet. 1995;57(3):476–8. doi: 10.1002/ajmg.1320570323. [DOI] [PubMed] [Google Scholar]
- 71.Albuisson J, Pecheux C, Carel JC, Lacombe D, Leheup B, Lapuzina P, et al. Kallmann syndrome: 14 novel mutations in KAL1 and FGFR1 (KAL2) Hum Mutat. 2005;25(1):98–9. doi: 10.1002/humu.9298. [DOI] [PubMed] [Google Scholar]
- 72.Pedersen-White JR, Chorich LP, Bick DP, Sherins RJ, Layman LC. The prevalence of intragenic deletions in patients with idiopathic hypogonadotropic hypogonadism and Kallmann syndrome. Mol Hum Reprod. 2008;14(6):367–70. doi: 10.1093/molehr/gan027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Oliveira LM, Seminara SB, Beranova M, Hayes FJ, Valkenburgh SB, Schipani E, et al. The importance of autosomal genes in Kallmann syndrome: genotype-phenotype correlations and neuroendocrine characteristics. J Clin Endocrinol Metab. 2001;86(4):1532–8. doi: 10.1210/jcem.86.4.7420. [DOI] [PubMed] [Google Scholar]
- 74.Izumi Y, Tatsumi K, Okamoto S, Ogawa T, Hosokawa A, Matsuo T, et al. Analysis of the KAL1 gene in 19 Japanese patients with Kallmann syndrome. Endocr J. 2001;48(2):143–9. doi: 10.1507/endocrj.48.143. [DOI] [PubMed] [Google Scholar]
- 75.Georgopoulos NA, Pralong FP, Seidman CE, Seidman JG, Crowley WF, Jr, Vallejo M. Genetic heterogeneity evidenced by low incidence of KAL-1 gene mutations in sporadic cases of gonadotropin-releasing hormone deficiency. J Clin Endocrinol Metab. 1997;82(1):213–7. doi: 10.1210/jcem.82.1.3692. [DOI] [PubMed] [Google Scholar]
- 76.Layman LC. Hypogonadotropic hypogonadism. Endocrinol Metab Clin North Am. 2007;36(2):283–96. doi: 10.1016/j.ecl.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 77.Pitteloud N, Meysing A, Quinton R, Acierno JS, Jr, Dwyer AA, Plummer L, et al. Mutations in fibroblast growth factor receptor 1 cause Kallmann syndrome with a wide spectrum of reproductive phenotypes. Mol Cell Endocrinol. 2006;254-255:60–9. doi: 10.1016/j.mce.2006.04.021. [DOI] [PubMed] [Google Scholar]
- 78.Dode C, Levilliers J, Dupont JM, De Paepe A, Le Du N, Soussi-Yanicostas N, et al. Loss-of-function mutations in FGFR1 cause autosomal dominant Kallmann syndrome. Nat Genet. 2003;33(4):463–5. doi: 10.1038/ng1122. [DOI] [PubMed] [Google Scholar]
- 79.Groth C, Lardelli M. The structure and function of vertebrate fibroblast growth factor receptor 1. Int J Dev Biol. 2002;46(4):393–400. [PubMed] [Google Scholar]
- 80.Gill JC, Moenter SM, Tsai PS. Developmental regulation of gonadotropin-releasing hormone neurons by fibroblast growth factor signaling. Endocrinology. 2004;145(8):3830–9. doi: 10.1210/en.2004-0214. [DOI] [PubMed] [Google Scholar]
- 81.Bottcher RT, Niehrs C. Fibroblast growth factor signaling during early vertebrate development. Endocr Rev. 2005;26(1):63–77. doi: 10.1210/er.2003-0040. [DOI] [PubMed] [Google Scholar]
- 82.Pitteloud N, Acierno JS, Jr, Meysing A, Eliseenkova AV, Ma J, Ibrahimi OA, et al. Mutations in fibroblast growth factor receptor 1 cause both Kallmann syndrome and normosmic idiopathic hypogonadotropic hypogonadism. Proc Natl Acad Sci U S A. 2006;103(16):6281–6. doi: 10.1073/pnas.0600962103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sato N, Katsumata N, Kagami M, Hasegawa T, Hori N, Kawakita S, et al. Clinical assessment and mutation analysis of Kallmann syndrome 1 (KAL1) and fibroblast growth factor receptor 1 (FGFR1, or KAL2) in five families and 18 sporadic patients. J Clin Endocrinol Metab. 2004;89(3):1079–88. doi: 10.1210/jc.2003-030476. [DOI] [PubMed] [Google Scholar]
- 84.Salenave S, Chanson P, Bry H, Pugeat M, Cabrol S, Carel JC, et al. Kallmann's syndrome: a comparison of the reproductive phenotypes in men carrying KAL1 and FGFR1/KAL2 mutations. J Clin Endocrinol Metab. 2008;93(3):758–63. doi: 10.1210/jc.2007-1168. [DOI] [PubMed] [Google Scholar]
- 85.Falardeau J, Chung WC, Beenken A, Raivio T, Plummer L, Sidis Y, et al. Decreased FGF8 signaling causes deficiency of gonadotropin-releasing hormone in humans and mice. J Clin Invest. 2008;118(8):2822–31. doi: 10.1172/JCI34538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Trarbach EB, Abreu AP, Silveira LF, Garmes HM, Baptista MT, Teles MG, et al. Nonsense mutations in FGF8 gene causing different degrees of human gonadotropin-releasing deficiency. J Clin Endocrinol Metab. 2010;95(7):3491–6. doi: 10.1210/jc.2010-0176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Trarbach EB, Silveira LG, Latronico AC. Genetic insights into human isolated gonadotropin deficiency. Pituitary. 2007;10(4):381–91. doi: 10.1007/s11102-007-0061-7. [DOI] [PubMed] [Google Scholar]
- 88.Cole LW, Sidis Y, Zhang C, Quinton R, Plummer L, Pignatelli D, et al. Mutations in prokineticin 2 and prokineticin receptor 2 genes in human gonadotrophin-releasing hormone deficiency: molecular genetics and clinical spectrum. J Clin Endocrinol Metab. 2008;93(9):3551–9. doi: 10.1210/jc.2007-2654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Vissers LE, van Ravenswaaij CM, Admiraal R, Hurst JA, de Vries BB, Janssen IM, et al. Mutations in a new member of the chromodomain gene family cause CHARGE syndrome. Nat Genet. 2004;36(9):955–7. doi: 10.1038/ng1407. [DOI] [PubMed] [Google Scholar]
- 90.Semple RK, Topaloglu AK. The recent genetics of hypogonadotrophic hypogonadism - novel insights and new questions. Clin Endocrinol (Oxf) 2010;72(4):427–35. doi: 10.1111/j.1365-2265.2009.03687.x. [DOI] [PubMed] [Google Scholar]
- 91.Lalani SR, Safiullah AM, Fernbach SD, Harutyunyan KG, Thaller C, Peterson LE, et al. Spectrum of CHD7 mutations in 110 individuals with CHARGE syndrome and genotype-phenotype correlation. Am J Hum Genet. 2006;78(2):303–14. doi: 10.1086/500273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kim HG, Kurth I, Lan F, Meliciani I, Wenzel W, Eom SH, et al. Mutations in CHD7, encoding a chromatin-remodeling protein, cause idiopathic hypogonadotropic hypogonadism and Kallmann syndrome. Am J Hum Genet. 2008;83(4):511–9. doi: 10.1016/j.ajhg.2008.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bedecarrats GY, Kaiser UB. Mutations in the human gonadotropin-releasing hormone receptor: insights into receptor biology and function. Semin Reprod Med. 2007;25(5):368–78. doi: 10.1055/s-2007-984743. [DOI] [PubMed] [Google Scholar]
- 94.Bouligand J, Ghervan C, Tello JA, Brailly-Tabard S, Salenave S, Chanson P, et al. Isolated familial hypogonadotropic hypogonadism and a GNRH1 mutation. N Engl J Med. 2009;360(26):2742–8. doi: 10.1056/NEJMoa0900136. [DOI] [PubMed] [Google Scholar]
- 95.Chan YM, de Guillebon A, Lang-Muritano M, Plummer L, Cerrato F, Tsiaras S, et al. GNRH1 mutations in patients with idiopathic hypogonadotropic hypogonadism. Proc Natl Acad Sci U S A. 2009;106(28):11703–8. doi: 10.1073/pnas.0903449106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kaiser UB, Dushkin H, Altherr MR, Beier DR, Chin WW. Chromosomal localization of the gonadotropin-releasing hormone receptor gene to human chromosome 4q13.1-q21.1 and mouse chromosome 5. Genomics. 1994;20(3):506–8. doi: 10.1006/geno.1994.1211. [DOI] [PubMed] [Google Scholar]
- 97.de Roux N, Young J, Misrahi M, Genet R, Chanson P, Schaison G, et al. A family with hypogonadotropic hypogonadism and mutations in the gonadotropin-releasing hormone receptor. N Engl J Med. 1997;337(22):1597–602. doi: 10.1056/NEJM199711273372205. [DOI] [PubMed] [Google Scholar]
- 98.Layman LC, Cohen DP, Jin M, Xie J, Li Z, Reindollar RH, et al. Mutations in gonadotropin-releasing hormone receptor gene cause hypogonadotropic hypogonadism. Nat Genet. 1998;18(1):14–5. doi: 10.1038/ng0198-14. [DOI] [PubMed] [Google Scholar]
- 99.Costa EM, Bedecarrats GY, Mendonca BB, Arnhold IJ, Kaiser UB, Latronico AC. Two novel mutations in the gonadotropin-releasing hormone receptor gene in Brazilian patients with hypogonadotropic hypogonadism and normal olfaction. J Clin Endocrinol Metab. 2001;86(6):2680–6. doi: 10.1210/jcem.86.6.7551. [DOI] [PubMed] [Google Scholar]
- 100.de Roux N, Young J, Brailly-Tabard S, Misrahi M, Milgrom E, Schaison G. The same molecular defects of the gonadotropin-releasing hormone receptor determine a variable degree of hypogonadism in affected kindred. J Clin Endocrinol Metab. 1999;84(2):567–72. doi: 10.1210/jcem.84.2.5449. [DOI] [PubMed] [Google Scholar]
- 101.Caron P, Chauvin S, Christin-Maitre S, Bennet A, Lahlou N, Counis R, et al. Resistance of hypogonadic patients with mutated GnRH receptor genes to pulsatile GnRH administration. J Clin Endocrinol Metab. 1999;84(3):990–6. doi: 10.1210/jcem.84.3.5518. [DOI] [PubMed] [Google Scholar]
- 102.Seminara SB, Beranova M, Oliveira LM, Martin KA, Crowley WF, Jr, Hall JE. Successful use of pulsatile gonadotropin-releasing hormone (GnRH) for ovulation induction and pregnancy in a patient with GnRH receptor mutations. J Clin Endocrinol Metab. 2000;85(2):556–62. doi: 10.1210/jcem.85.2.6357. [DOI] [PubMed] [Google Scholar]
- 103.Beranova M, Oliveira LM, Bedecarrats GY, Schipani E, Vallejo M, Ammini AC, et al. Prevalence, phenotypic spectrum, and modes of inheritance of gonadotropin-releasing hormone receptor mutations in idiopathic hypogonadotropic hypogonadism. J Clin Endocrinol Metab. 2001;86(4):1580–8. doi: 10.1210/jcem.86.4.7395. [DOI] [PubMed] [Google Scholar]
- 104.Bedecarrats GY, Linher KD, Kaiser UB. Two common naturally occurring mutations in the human gonadotropin-releasing hormone (GnRH) receptor have differential effects on gonadotropin gene expression and on GnRH-mediated signal transduction. J Clin Endocrinol Metab. 2003;88(2):834–43. doi: 10.1210/jc.2002-020806. [DOI] [PubMed] [Google Scholar]
- 105.Pitteloud N, Boepple PA, DeCruz S, Valkenburgh SB, Crowley WF, Jr, Hayes FJ. The fertile eunuch variant of idiopathic hypogonadotropic hypogonadism: spontaneous reversal associated with a homozygous mutation in the gonadotropin-releasing hormone receptor. J Clin Endocrinol Metab. 2001;86(6):2470–5. doi: 10.1210/jcem.86.6.7542. [DOI] [PubMed] [Google Scholar]
- 106.Silveira LG, Noel SD, Silveira-Neto AP, Abreu AP, Brito VN, Santos MG, et al. Mutations of the KISS1 gene in disorders of puberty. J Clin Endocrinol Metab. 2010;95(5):2276–80. doi: 10.1210/jc.2009-2421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Messager S, Chatzidaki EE, Ma D, Hendrick AG, Zahn D, Dixon J, et al. Kisspeptin directly stimulates gonadotropin-releasing hormone release via G protein-coupled receptor 54. Proc Natl Acad Sci U S A. 2005;102(5):1761–6. doi: 10.1073/pnas.0409330102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Topaloglu AK, Reimann F, Guclu M, Yalin AS, Kotan LD, Porter KM, et al. TAC3 and TACR3 mutations in familial hypogonadotropic hypogonadism reveal a key role for Neurokinin B in the central control of reproduction. Nat Genet. 2009;41(3):354–8. doi: 10.1038/ng.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Guran T, Tolhurst G, Bereket A, Rocha N, Porter K, Turan S, et al. Hypogonadotropic hypogonadism due to a novel missense mutation in the first extracellular loop of the neurokinin B receptor. J Clin Endocrinol Metab. 2009;94(10):3633–9. doi: 10.1210/jc.2009-0551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Gianetti E, Tusset C, Noel SD, Au MG, Dwyer AA, Hughes VA, et al. TAC3/TACR3 mutations reveal preferential activation of gonadotropin-releasing hormone release by neurokinin B in neonatal life followed by reversal in adulthood. J Clin Endocrinol Metab. 2010;95(6):2857–67. doi: 10.1210/jc.2009-2320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Jackson RS, Creemers JW, Ohagi S, Raffin-Sanson ML, Sanders L, Montague CT, et al. Obesity and impaired prohormone processing associated with mutations in the human prohormone convertase 1 gene. Nat Genet. 1997;16(3):303–6. doi: 10.1038/ng0797-303. [DOI] [PubMed] [Google Scholar]
- 112.Muscatelli F, Strom TM, Walker AP, Zanaria E, Recan D, Meindl A, et al. Mutations in the DAX-1 gene give rise to both X-linked adrenal hypoplasia congenita and hypogonadotropic hypogonadism. Nature. 1994;372(6507):672–6. doi: 10.1038/372672a0. [DOI] [PubMed] [Google Scholar]
- 113.Mendonca BB, Osorio MG, Latronico AC, Estefan V, Lo LS, Arnhold IJ. Longitudinal hormonal and pituitary imaging changes in two females with combined pituitary hormone deficiency due to deletion of A301,G302 in the PROP1 gene. J Clin Endocrinol Metab. 1999;84(3):942–5. doi: 10.1210/jcem.84.3.5537. [DOI] [PubMed] [Google Scholar]
- 114.Kelberman D, Dattani MT. Hypopituitarism oddities: congenital causes. Horm Res. 2007;68 Suppl 5:138–44. doi: 10.1159/000110610. [DOI] [PubMed] [Google Scholar]
- 115.Themmen APN, Huhtaniemi IT. Mutations of gonadotropins and gonadotropin receptors: elucidating the physiology and pathophysiology of pituitary-gonadal function. Endocr Rev. 2000;21(5):551–83. doi: 10.1210/edrv.21.5.0409. [DOI] [PubMed] [Google Scholar]
- 116.Layman LC, Porto AL, Xie J, da Motta LA, da Motta LD, Weiser W, et al. FSH beta gene mutations in a female with partial breast development and a male sibling with normal puberty and azoospermia. J Clin Endocrinol Metab. 2002;87(8):3702–7. doi: 10.1210/jcem.87.8.8724. [DOI] [PubMed] [Google Scholar]
- 117.Lindstedt G, Nystrom E, Matthews C, Ernest I, Janson PO, Chatterjee K. Follitropin (FSH) deficiency in an infertile male due to FSHbeta gene mutation. A syndrome of normal puberty and virilization but underdeveloped testicles with azoospermia, low FSH but high lutropin and normal serum testosterone concentrations. Clin Chem Lab Med. 1998;36(8):663–5. doi: 10.1515/CCLM.1998.118. [DOI] [PubMed] [Google Scholar]
- 118.Diez JJ, Iglesias P, Sastre J, Salvador J, Gomez-Pan A, Otero I, et al. Isolated deficiency of follicle-stimulating hormone in man: a case report and literature review. Int J Fertil Menopausal Stud. 1994;39(1):26–31. [PubMed] [Google Scholar]
- 119.Layman LC, Lee EJ, Peak DB, Namnoum AB, Vu KV, van Lingen BL, et al. Delayed puberty and hypogonadism caused by mutations in the follicle-stimulating hormone beta-subunit gene. N Engl J Med. 1997;337(9):607–11. doi: 10.1056/NEJM199708283370905. [DOI] [PubMed] [Google Scholar]
- 120.Kottler ML, Chou YY, Chabre O, Richard N, Polge C, Brailly-Tabard S, et al. A new FSHbeta mutation in a 29-year-old woman with primary amenorrhea and isolated FSH deficiency: functional characterization and ovarian response to human recombinant FSH. Eur J Endocrinol. 2010;162(3):633–41. doi: 10.1530/EJE-09-0648. [DOI] [PubMed] [Google Scholar]
- 121.Matthews CH, Borgato S, Beck-Peccoz P, Adams M, Tone Y, Gambino G, et al. Primary amenorrhoea and infertility due to a mutation in the beta-subunit of follicle-stimulating hormone. Nat Genet. 1993;5(1):83–6. doi: 10.1038/ng0993-83. [DOI] [PubMed] [Google Scholar]
- 122.Kumar TR, Wang Y, Lu N, Matzuk MM. Follicle stimulating hormone is required for ovarian follicle maturation but not male fertility. Nat Genet. 1997;15(2):201–4. doi: 10.1038/ng0297-201. [DOI] [PubMed] [Google Scholar]
- 123.Zirkin BR, Awoniyi C, Griswold MD, Russell LD, Sharpe R. Is FSH required for adult spermatogenesis. J Androl. 1994;15(4):273–6. [PubMed] [Google Scholar]
- 124.Tapanainen JS, Aittomaki K, Min J, Vaskivuo T, Huhtaniemi IT. Men homozygous for an inactivating mutation of the follicle-stimulating hormone (FSH) receptor gene present variable suppression of spermatogenesis and fertility. Nat Genet. 1997;15(2):205–6. doi: 10.1038/ng0297-205. [DOI] [PubMed] [Google Scholar]
- 125.Gromoll J, Pekel E, Nieschlag E. The structure and organization of the human follicle-stimulating hormone receptor (FSHR) gene. Genomics. 1996;35(2):308–11. doi: 10.1006/geno.1996.0361. [DOI] [PubMed] [Google Scholar]
- 126.Heckert LL, Daley IJ, Griswold MD. Structural organization of the follicle-stimulating hormone receptor gene. Mol Endocrinol. 1992;6(1):70–80. doi: 10.1210/mend.6.1.1738373. [DOI] [PubMed] [Google Scholar]
- 127.Simoni M, Gromoll J, Hoppner W, Kamischke A, Krafft T, Stahle D, et al. Mutational analysis of the follicle-stimulating hormone (FSH) receptor in normal and infertile men: identification and characterization of two discrete FSH receptor isoforms. J Clin Endocrinol Metab. 1999;84(2):751–5. doi: 10.1210/jcem.84.2.5500. [DOI] [PubMed] [Google Scholar]
- 128.Ahda Y, Gromoll J, Wunsch A, Asatiani K, Zitzmann M, Nieschlag E, et al. Follicle-stimulating hormone receptor gene haplotype distribution in normozoospermic and azoospermic men. J Androl. 2005;26(4):494–9. doi: 10.2164/jandrol.04186. [DOI] [PubMed] [Google Scholar]
- 129.Weiss J, Axelrod L, Whitcomb RW, Harris PE, Crowley WF, Jameson JL. Hypogonadism caused by a single amino acid substitution in the beta subunit of luteinizing hormone. N Engl J Med. 1992;326(3):179–83. doi: 10.1056/NEJM199201163260306. [DOI] [PubMed] [Google Scholar]
- 130.Lofrano-Porto A, Barra GB, Giacomini LA, Nascimento PP, Latronico AC, Casulari LA, et al. Luteinizing hormone beta mutation and hypogonadism in men and women. N Engl J Med. 2007;357(9):897–904. doi: 10.1056/NEJMoa071999. [DOI] [PubMed] [Google Scholar]
- 131.Daly AFSR, Menage J, et al. Abstracts 88th Annu Meet Endocr Soc. Boston: 2006. Identification of a family harboring a novel LH beta-subunit mutation associated with hypogonadism. [Google Scholar]
- 132.Rousseau-Merck MF, Misrahi M, Atger M, Loosfelt H, Milgrom E, Berger R. Localization of the human luteinizing hormone/choriogonadotropin receptor gene (LHCGR) to chromosome 2p21. Cytogenet Cell Genet. 1990;54(1-2):77–9. doi: 10.1159/000132962. [DOI] [PubMed] [Google Scholar]
- 133.Berthezene F, Forest MG, Grimaud JA, Claustrat B, Mornex R. Leydig-cell agenesis: a cause of male pseudohermaphroditism. N Engl J Med. 1976;295(18):969–72. doi: 10.1056/NEJM197610282951801. [DOI] [PubMed] [Google Scholar]
- 134.Foresta C, Garolla A, Bartoloni L, Bettella A, Ferlin A. Genetic abnormalities among severely oligospermic men who are candidates for intracytoplasmic sperm injection. J Clin Endocrinol Metab. 2005;90(1):152–6. doi: 10.1210/jc.2004-1469. [DOI] [PubMed] [Google Scholar]
- 135.Meschede D, Lemcke B, Behre HM, De Geyter C, Nieschlag E, Horst J. Clustering of male infertility in the families of couples treated with intracytoplasmic sperm injection. Hum Reprod. 2000;15(7):1604–8. doi: 10.1093/humrep/15.7.1604. [DOI] [PubMed] [Google Scholar]
- 136.Gianotten J, Westerveld GH, Leschot NJ, Tanck MW, Lilford RJ, Lombardi MP, et al. Familial clustering of impaired spermatogenesis: no evidence for a common genetic inheritance pattern. Hum Reprod. 2004;19(1):71–6. doi: 10.1093/humrep/deh008. [DOI] [PubMed] [Google Scholar]
- 137.Ron-El R, Strassburger D, Gelman-Kohan S, Friedler S, Raziel A, Appelman Z. A 47,XXY fetus conceived after ICSI of spermatozoa from a patient with non-mosaic Klinefelter's syndrome: case report. Hum Reprod. 2000;15(8):1804–6. doi: 10.1093/humrep/15.8.1804. [DOI] [PubMed] [Google Scholar]
- 138.Schiff JD, Palermo GD, Veeck LL, Goldstein M, Rosenwaks Z, Schlegel PN. Success of testicular sperm extraction [corrected] and intracytoplasmic sperm injection in men with Klinefelter syndrome. J Clin Endocrinol Metab. 2005;90(11):6263–7. doi: 10.1210/jc.2004-2322. [DOI] [PubMed] [Google Scholar]
- 139.Staessen C, Tournaye H, Van Assche E, Michiels A, Van Landuyt L, Devroey P, et al. PGD in 47,XXY Klinefelter's syndrome patients. Hum Reprod Update. 2003;9(4):319–30. doi: 10.1093/humupd/dmg029. [DOI] [PubMed] [Google Scholar]
- 140.Sciurano RB, Luna Hisano CV, Rahn MI, Brugo Olmedo S, Rey Valzacchi G, Coco R, et al. Focal spermatogenesis originates in euploid germ cells in classical Klinefelter patients. Hum Reprod. 2009;24(9):2353–60. doi: 10.1093/humrep/dep180. [DOI] [PubMed] [Google Scholar]
- 141.Schweikert HU, Weissbach L, Leyendecker G, Schwinger E, Wartenberg H, Kruck F. Clinical, endocrinological, and cytological characterization of two 46, XX males. J Clin Endocrinol Metab. 1982;54(4):745–52. doi: 10.1210/jcem-54-4-745. [DOI] [PubMed] [Google Scholar]
- 142.Behlke MA, Bogan JS, Beer-Romero P, Page DC. Evidence that the SRY protein is encoded by a single exon on the human Y chromosome. Genomics. 1993;17(3):736–9. doi: 10.1006/geno.1993.1395. [DOI] [PubMed] [Google Scholar]
- 143.Abbas NE, Toublanc JE, Boucekkine C, Toublanc M, Affara NA, Job JC, et al. A possible common origin of "Y-negative" human XX males and XX true hermaphrodites. Hum Genet. 1990;84(4):356–60. doi: 10.1007/BF00196234. [DOI] [PubMed] [Google Scholar]
- 144.Dada R, Ahmad ME, Talwar R, Kucheria K. Clinical and Genetic study in a XX (SRY negative) male. Medicine on-line 2002. Available from: http://www.priory.com/med/xx.htm Accessed August 6, 2012. [Google Scholar]
- 145.Glickman MH, Ciechanover A. The ubiquitin-proteasome proteolytic pathway: destruction for the sake of construction. Physiol Rev. 2002;82(2):373–428. doi: 10.1152/physrev.00027.2001. [DOI] [PubMed] [Google Scholar]
- 146.Wei L, Shi YC, Cui YX, Huang YF. [Mutation of the USP26 gene in spermatogenesis dysfunction] Zhonghua Nan Ke Xue. 2010;16(1):65–7. [PubMed] [Google Scholar]
- 147.Stouffs K, Tournaye H, Liebaers I, Lissens W. Male infertility and the involvement of the X chromosome. Hum Reprod Update. 2009;15(6):623–37. doi: 10.1093/humupd/dmp023. [DOI] [PubMed] [Google Scholar]
- 148.Stouffs K, Lissens W, Tournaye H, Van Steirteghem A, Liebaers I. Possible role of USP26 in patients with severely impaired spermatogenesis. Eur J Hum Genet. 2005;13(3):336–40. doi: 10.1038/sj.ejhg.5201335. [DOI] [PubMed] [Google Scholar]
- 149.Paduch DA, Mielnik A, Schlegel PN. Novel mutations in testis-specific ubiquitin protease 26 gene may cause male infertility and hypogonadism. Reprod Biomed Online. 2005;10(6):747–54. doi: 10.1016/s1472-6483(10)61119-4. [DOI] [PubMed] [Google Scholar]
- 150.Kiefer JC. Back to basics: Sox genes. Dev Dyn. 2007;236(8):2356–66. doi: 10.1002/dvdy.21218. [DOI] [PubMed] [Google Scholar]
- 151.Graves JA. Interactions between SRY and SOX genes in mammalian sex determination. Bioessays. 1998;20(3):264–9. doi: 10.1002/(SICI)1521-1878(199803)20:3<264::AID-BIES10>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 152.Graves JA. Evolution of the mammalian Y chromosome and sex-determining genes. J Exp Zool. 1998;281(5):472–81. [PubMed] [Google Scholar]
- 153.Solomon NM, Ross SA, Forrest SM, Thomas PQ, Morgan T, Belsky JL, et al. Array comparative genomic hybridisation analysis of boys with X-linked hypopituitarism identifies a 3.9 Mb duplicated critical region at Xq27 containing SOX3. J Med Genet. 2007;44(4):e75. doi: 10.1136/jmg.2007.049049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Woods KS, Cundall M, Turton J, Rizotti K, Mehta A, Palmer R, et al. Over- and underdosage of SOX3 is associated with infundibular hypoplasia and hypopituitarism. Am J Hum Genet. 2005;76(5):833–49. doi: 10.1086/430134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Raverot G, Lejeune H, Kotlar T, Pugeat M, Jameson JL. X-linked sex-determining region Y box 3 (SOX3) gene mutations are uncommon in men with idiopathic oligoazoospermic infertility. J Clin Endocrinol Metab. 2004;89(8):4146–8. doi: 10.1210/jc.2004-0191. [DOI] [PubMed] [Google Scholar]
- 156.Weiss J, Meeks JJ, Hurley L, Raverot G, Frassetto A, Jameson JL. Sox3 is required for gonadal function, but not sex determination, in males and females. Mol Cell Biol. 2003;23(22):8084–91. doi: 10.1128/MCB.23.22.8084-8091.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Zenaty D, Dijoud F, Morel Y, Cabrol S, Mouriquand P, Nicolino M, et al. Bilateral anorchia in infancy: occurence of micropenis and the effect of testosterone treatment. J Pediatr. 2006;149(5):687–91. doi: 10.1016/j.jpeds.2006.07.044. [DOI] [PubMed] [Google Scholar]
- 158.Philibert P, Zenaty D, Lin L, Soskin S, Audran F, Leger J, et al. Mutational analysis of steroidogenic factor 1 (NR5a1) in 24 boys with bilateral anorchia: a French collaborative study. Hum Reprod. 2007;22(12):3255–61. doi: 10.1093/humrep/dem278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Tartaglia M, Gelb BD, Zenker M. Noonan syndrome and clinically related disorders. Best Pract Res Clin Endocrinol Metab. 2011;25(1):161–79. doi: 10.1016/j.beem.2010.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Sharland M, Burch M, McKenna WM, Paton MA. A clinical study of Noonan syndrome. Arch Dis Child. 1992;67(2):178–83. doi: 10.1136/adc.67.2.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Kelnar CJ. Noonan syndrome: the hypothalamo-adrenal and hypothalamo-gonadal axes. Horm Res. 2009;72 Suppl 2:24–30. doi: 10.1159/000243775. [DOI] [PubMed] [Google Scholar]
- 162.Caglayan AO, Demiryilmaz F, Kendirci M, Ozyazgan I, Akalin H, Bittmann S. Mixed gonadal dysgenesis with 45,X/46,X,idic(Y)/46,XY,idic(Y) karyotype. Genet Couns. 2009;20(2):173–9. [PubMed] [Google Scholar]
- 163.Telvi L, Lebbar A, Del Pino O, Barbet JP, Chaussain JL. 45,X/46,XY mosaicism: report of 27 cases. Pediatrics. 1999;104(2 Pt 1):304–8. doi: 10.1542/peds.104.2.304. [DOI] [PubMed] [Google Scholar]
- 164.Reijo R, Lee TY, Salo P, Alagappan R, Brown LG, Rosenberg M, et al. Diverse spermatogenic defects in humans caused by Y chromosome deletions encompassing a novel RNA-binding protein gene. Nat Genet. 1995;10(4):383–93. doi: 10.1038/ng0895-383. [DOI] [PubMed] [Google Scholar]
- 165.McLachlan RI, Mallidis C, Ma K, Bhasin S, de Kretser DM. Genetic disorders and spermatogenesis. Reprod Fertil Dev. 1998;10(1):97–104. doi: 10.1071/r98029. [DOI] [PubMed] [Google Scholar]
- 166.Ferlin A, Arredi B, Speltra E, Cazzadore C, Selice R, Garolla A, et al. Molecular and clinical characterization of Y chromosome microdeletions in infertile men: a 10-year experience in Italy. J Clin Endocrinol Metab. 2007;92(3):762–70. doi: 10.1210/jc.2006-1981. [DOI] [PubMed] [Google Scholar]
- 167.Vogt PH. Azoospermia factor (AZF) in Yq11: towards a molecular understanding of its function for human male fertility and spermatogenesis. Reprod Biomed Online. 2005;10(1):81–93. doi: 10.1016/s1472-6483(10)60807-3. [DOI] [PubMed] [Google Scholar]
- 168.Nuti F, Krausz C. Gene polymorphisms/mutations relevant to abnormal spermatogenesis. Reprod Biomed Online. 2008;16(4):504–13. doi: 10.1016/s1472-6483(10)60457-9. [DOI] [PubMed] [Google Scholar]
- 169.Foresta C, Ferlin A, Garolla A, Moro E, Pistorello M, Barbaux S, et al. High frequency of well-defined Y-chromosome deletions in idiopathic Sertoli cell-only syndrome. Hum Reprod. 1998;13(2):302–7. doi: 10.1093/humrep/13.2.302. [DOI] [PubMed] [Google Scholar]
- 170.Kamp C, Huellen K, Fernandes S, Sousa M, Schlegel PN, Mielnik A, et al. High deletion frequency of the complete AZFa sequence in men with Sertoli-cell-only syndrome. Mol Hum Reprod. 2001;7(10):987–94. doi: 10.1093/molehr/7.10.987. [DOI] [PubMed] [Google Scholar]
- 171.Blagosklonova O, Fellmann F, Clavequin MC, Roux C, Bresson JL. AZFa deletions in Sertoli cell-only syndrome: a retrospective study. Mol Hum Reprod. 2000;6(9):795–9. doi: 10.1093/molehr/6.9.795. [DOI] [PubMed] [Google Scholar]
- 172.Ditton HJ, Zimmer J, Kamp C, Rajpert-De Meyts E, Vogt PH. The AZFa gene DBY (DDX3Y) is widely transcribed but the protein is limited to the male germ cells by translation control. Hum Mol Genet. 2004;13(19):2333–41. doi: 10.1093/hmg/ddh240. [DOI] [PubMed] [Google Scholar]
- 173.D'Andrea A, Pellman D. Deubiquitinating enzymes: a new class of biological regulators. Crit Rev Biochem Mol Biol. 1998;33(5):337–52. doi: 10.1080/10409239891204251. [DOI] [PubMed] [Google Scholar]
- 174.Vogt PH, Falcao CL, Hanstein R, Zimmer J. The AZF proteins. Int J Androl. 2008;31(4):383–94. doi: 10.1111/j.1365-2605.2008.00890.x. [DOI] [PubMed] [Google Scholar]
- 175.Qureshi SJ, Ross AR, Ma K, Cooke HJ, Intyre MA, Chandley AC, et al. Polymerase chain reaction screening for Y chromosome microdeletions: a first step towards the diagnosis of genetically-determined spermatogenic failure in men. Mol Hum Reprod. 1996;2(10):775–9. doi: 10.1093/molehr/2.10.775. [DOI] [PubMed] [Google Scholar]
- 176.Tyler-Smith C. An evolutionary perspective on Y-chromosomal variation and male infertility. Int J Androl. 2008;31(4):376–82. doi: 10.1111/j.1365-2605.2008.00889.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Brown GM, Furlong RA, Sargent CA, Erickson RP, Longepied G, Mitchell M, et al. Characterisation of the coding sequence and fine mapping of the human DFFRY gene and comparative expression analysis and mapping to the Sxrb interval of the mouse Y chromosome of the Dffry gene. Hum Mol Genet. 1998;7(1):97–107. doi: 10.1093/hmg/7.1.97. [DOI] [PubMed] [Google Scholar]
- 178.Krausz C, Degl'Innocenti S, Nuti F, Morelli A, Felici F, Sansone M, et al. Natural transmission of USP9Y gene mutations: a new perspective on the role of AZFa genes in male fertility. Hum Mol Genet. 2006;15(18):2673–81. doi: 10.1093/hmg/ddl198. [DOI] [PubMed] [Google Scholar]
- 179.Repping S, Skaletsky H, Lange J, Silber S, Van Der Veen F, Oates RD, et al. Recombination between palindromes P5 and P1 on the human Y chromosome causes massive deletions and spermatogenic failure. Am J Hum Genet. 2002;71(4):906–22. doi: 10.1086/342928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Skaletsky H, Kuroda-Kawaguchi T, Minx PJ, Cordum HS, Hillier L, Brown LG, et al. The male-specific region of the human Y chromosome is a mosaic of discrete sequence classes. Nature. 2003;423(6942):825–37. doi: 10.1038/nature01722. [DOI] [PubMed] [Google Scholar]
- 181.Elliott DJ. The role of potential splicing factors including RBMY, RBMX, hnRNPG-T and STAR proteins in spermatogenesis. Int J Androl. 2004;27(6):328–34. doi: 10.1111/j.1365-2605.2004.00496.x. [DOI] [PubMed] [Google Scholar]
- 182.Ferlin A, Moro E, Rossi A, Dallapiccola B, Foresta C. The human Y chromosome's azoospermia factor b (AZFb) region: sequence, structure, and deletion analysis in infertile men. J Med Genet. 2003;40(1):18–24. doi: 10.1136/jmg.40.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Vogt PH. Human chromosome deletions in Yq11, AZF candidate genes and male infertility: history and update. Mol Hum Reprod. 1998;4(8):739–44. doi: 10.1093/molehr/4.8.739. [DOI] [PubMed] [Google Scholar]
- 184.Page DC. 2003 Curt Stern Award address. On low expectation exceeded; or, the genomic salvation of the Y chromosome. Am J Hum Genet. 2004;74(3):399–402. doi: 10.1086/382659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Kuroda-Kawaguchi T, Skaletsky H, Brown LG, Minx PJ, Cordum HS, Waterston RH, et al. The AZFc region of the Y chromosome features massive palindromes and uniform recurrent deletions in infertile men. Nat Genet. 2001;29(3):279–86. doi: 10.1038/ng757. [DOI] [PubMed] [Google Scholar]
- 186.Siffroi JP, Le Bourhis C, Krausz C, Barbaux S, Quintana-Murci L, Kanafani S, et al. Sex chromosome mosaicism in males carrying Y chromosome long arm deletions. Hum Reprod. 2000;15(12):2559–62. doi: 10.1093/humrep/15.12.2559. [DOI] [PubMed] [Google Scholar]
- 187.Patsalis PC, Sismani C, Quintana-Murci L, Taleb-Bekkouche F, Krausz C, McElreavey K. Effects of transmission of Y chromosome AZFc deletions. Lancet. 2002;360(9341):1222–4. doi: 10.1016/s0140-6736(02)11248-7. [DOI] [PubMed] [Google Scholar]
- 188.Sassone-Corsi P. Transcriptional checkpoints determining the fate of male germ cells. Cell. 1997;88(2):163–6. doi: 10.1016/s0092-8674(00)81834-6. [DOI] [PubMed] [Google Scholar]
- 189.Kimmins S, Kotaja N, Davidson I, Sassone-Corsi P. Testis-specific transcription mechanisms promoting male germ-cell differentiation. Reproduction. 2004;128(1):5–12. doi: 10.1530/rep.1.00170. [DOI] [PubMed] [Google Scholar]
- 190.Falender AE, Freiman RN, Geles KG, Lo KC, Hwang K, Lamb DJ, et al. Maintenance of spermatogenesis requires TAF4b, a gonad-specific subunit of TFIID. Genes Dev. 2005;19(7):794–803. doi: 10.1101/gad.1290105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Akinloye O, Gromoll J, Callies C, Nieschlag E, Simoni M. Mutation analysis of the X-chromosome linked, testis-specific TAF7L gene in spermatogenic failure. Andrologia. 2007;39(5):190–5. doi: 10.1111/j.1439-0272.2007.00789.x. [DOI] [PubMed] [Google Scholar]
- 192.Stouffs K, Willems A, Lissens W, Tournaye H, Van Steirteghem A, Liebaers I. The role of the testis-specific gene hTAF7L in the aetiology of male infertility. Mol Hum Reprod. 2006;12(4):263–7. doi: 10.1093/molehr/gal020. [DOI] [PubMed] [Google Scholar]
- 193.Li X. Sex chromosomes and sex chromosome abnormalities. Clin Lab Med. 2011;31(4):463–79, vii. doi: 10.1016/j.cll.2011.08.013. [DOI] [PubMed] [Google Scholar]
- 194.Stouffs K, Lissens W, Verheyen G, Van Landuyt L, Goossens A, Tournaye H, et al. Expression pattern of the Y-linked PRY gene suggests a function in apoptosis but not in spermatogenesis. Mol Hum Reprod. 2004;10(1):15–21. doi: 10.1093/molehr/gah010. [DOI] [PubMed] [Google Scholar]
- 195.Repping S, van Daalen SK, Korver CM, Brown LG, Marszalek JD, Gianotten J, et al. A family of human Y chromosomes has dispersed throughout northern Eurasia despite a 1.8-Mb deletion in the azoospermia factor c region. Genomics. 2004;83(6):1046–52. doi: 10.1016/j.ygeno.2003.12.018. [DOI] [PubMed] [Google Scholar]
- 196.Cong XW, Tu XD, Yan AZ, Zeng J. [Partial AZfc region deletions of the Y chromosome in spermatogenic dysfunction patients] Zhonghua Nan Ke Xue. 2010;16(7):594–8. [PubMed] [Google Scholar]
- 197.Shaqalaih AJ, Abu Halima MS, Ashour MJ, Sharif FA. Screening for Y-chromosome microdeletions in a population of infertile males in the Gaza Strip. J Exp Clin Assist Reprod. 2009;6:7. [PMC free article] [PubMed] [Google Scholar]
- 198.Eloualid A, Rhaissi H, Reguig A, Bounaceur S, El Houate B, Abidi O, et al. Association of spermatogenic failure with the b2/b3 partial AZFc deletion. PLoS One. 2012;7(4):e34902. doi: 10.1371/journal.pone.0034902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Fernandes S, Paracchini S, Meyer LH, Floridia G, Tyler-Smith C, Vogt PH. A large AZFc deletion removes DAZ3/DAZ4 and nearby genes from men in Y haplogroup N. Am J Hum Genet. 2004;74(1):180–7. doi: 10.1086/381132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Yen HW, Jakimiuk AJ, Munir I, Magoffin DA. Selective alterations in insulin receptor substrates-1, -2 and -4 in theca but not granulosa cells from polycystic ovaries. Mol Hum Reprod. 2004;10(7):473–9. doi: 10.1093/molehr/gah066. [DOI] [PubMed] [Google Scholar]
- 201.Reynolds N, Cooke HJ. Role of the DAZ genes in male fertility. Reprod Biomed Online. 2005;10(1):72–80. doi: 10.1016/s1472-6483(10)60806-1. [DOI] [PubMed] [Google Scholar]
- 202.Lavery R, Glennon M, Houghton J, Nolan A, Egan D, Maher M. Investigation of DAZ and RBMY1 gene expression in human testis by quantitative real-time PCR. Arch Androl. 2007;53(2):71–3. doi: 10.1080/01485010600915228. [DOI] [PubMed] [Google Scholar]
- 203.Lardone MC, Parodi DA, Valdevenito R, Ebensperger M, Piottante A, Madariaga M, et al. Quantification of DDX3Y, RBMY1, DAZ and TSPY mRNAs in testes of patients with severe impairment of spermatogenesis. Mol Hum Reprod. 2007;13(10):705–12. doi: 10.1093/molehr/gam057. [DOI] [PubMed] [Google Scholar]
- 204.Vodicka R, Vrtel R, Dusek L, Singh AR, Krizova K, Svacinova V, et al. TSPY gene copy number as a potential new risk factor for male infertility. Reprod Biomed Online. 2007;14(5):579–87. doi: 10.1016/s1472-6483(10)61049-8. [DOI] [PubMed] [Google Scholar]
- 205.Carrell DT. Contributions of spermatozoa to embryogenesis: assays to evaluate their genetic and epigenetic fitness. Reprod Biomed Online. 2008;16(4):474–84. doi: 10.1016/s1472-6483(10)60454-3. [DOI] [PubMed] [Google Scholar]
- 206.Chandley AC, Edmond P, Christie S, Gowans L, Fletcher J, Frackiewicz A, et al. Cytogenetics and infertility in man. I. Karyotype and seminal analysis: results of a five-year survey of men attending a subfertility clinic. Ann Hum Genet. 1975;39(2):231–54. doi: 10.1111/j.1469-1809.1975.tb00126.x. [DOI] [PubMed] [Google Scholar]
- 207.Elliott DJ, Cooke HJ. The molecular genetics of male infertility. Bioessays. 1997;19(9):801–9. doi: 10.1002/bies.950190910. [DOI] [PubMed] [Google Scholar]
- 208.De Braekeleer M, Dao TN. Cytogenetic studies in male infertility: a review. Hum Reprod. 1991;6(2):245–50. [PubMed] [Google Scholar]
- 209.Johnson MD. Genetic risks of intracytoplasmic sperm injection in the treatment of male infertility: recommendations for genetic counseling and screening. Fertil Steril. 1998;70(3):397–411. doi: 10.1016/s0015-0282(98)00209-x. [DOI] [PubMed] [Google Scholar]
- 210.Meschede D, Lemcke B, Exeler JR, De Geyter C, Behre HM, Nieschlag E, et al. Chromosome abnormalities in 447 couples undergoing intracytoplasmic sperm injection–prevalence, types, sex distribution and reproductive relevance. Hum Reprod. 1998;13(3):576–82. doi: 10.1093/humrep/13.3.576. [DOI] [PubMed] [Google Scholar]
- 211.Tuttelmann F, Rajpert-De Meyts E, Nieschlag E, Simoni M. Gene polymorphisms and male infertility–a meta-analysis and literature review. Reprod Biomed Online. 2007;15(6):643–58. doi: 10.1016/s1472-6483(10)60531-7. [DOI] [PubMed] [Google Scholar]
- 212.Teng YN, Lin YM, Lin YH, Tsao SY, Hsu CC, Lin SJ, et al. Association of a single-nucleotide polymorphism of the deleted-in-azoospermia-like gene with susceptibility to spermatogenic failure. J Clin Endocrinol Metab. 2002;87(11):5258–64. doi: 10.1210/jc.2002-020016. [DOI] [PubMed] [Google Scholar]
- 213.Shen O, Liu R, Wu W, Yu L, Wang X. Association of the methylenetetrahydrofolate reductase gene A1298C polymorphism with male infertility: a meta-analysis. Ann Hum Genet. 2012;76(1):25–32. doi: 10.1111/j.1469-1809.2011.00691.x. [DOI] [PubMed] [Google Scholar]
- 214.Wu W, Shen O, Qin Y, Lu J, Niu X, Zhou Z, et al. Methylenetetrahydrofolate reductase C677T polymorphism and the risk of male infertility: a meta-analysis. Int J Androl. 2012;35(1):18–24. doi: 10.1111/j.1365-2605.2011.01147.x. [DOI] [PubMed] [Google Scholar]
- 215.Ferlin A, Foresta C. Insulin-like factor 3: a novel circulating hormone of testicular origin in humans. Ann N Y Acad Sci. 2005;1041:497–505. doi: 10.1196/annals.1282.074. [DOI] [PubMed] [Google Scholar]
- 216.Zimmermann S, Steding G, Emmen JM, Brinkmann AO, Nayernia K, Holstein AF, et al. Targeted disruption of the Insl3 gene causes bilateral cryptorchidism. Mol Endocrinol. 1999;13(5):681–91. doi: 10.1210/mend.13.5.0272. [DOI] [PubMed] [Google Scholar]
- 217.Wang PJ, McCarrey JR, Yang F, Page DC. An abundance of X-linked genes expressed in spermatogonia. Nat Genet. 2001;27(4):422–6. doi: 10.1038/86927. [DOI] [PubMed] [Google Scholar]
- 218.Olesen IA, Sonne SB, Hoei-Hansen CE, Rajpert-DeMeyts E, Skakkebaek NE. Environment, testicular dysgenesis and carcinoma in situ testis. Best Pract Res Clin Endocrinol Metab. 2007;21(3):462–78. doi: 10.1016/j.beem.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 219.Gottlieb B, Beitel LK, Nadarajah A, Paliouras M, Trifiro M. The androgen receptor gene mutations database: 2012 update. Hum Mutat. 2012;33(5):887–94. doi: 10.1002/humu.22046. [DOI] [PubMed] [Google Scholar]
- 220.Galani A, Kitsiou-Tzeli S, Sofokleous C, Kanavakis E, Kalpini-Mavrou A. Androgen insensitivity syndrome: clinical features and molecular defects. Hormones (Athens) 2008;7(3):217–29. doi: 10.14310/horm.2002.1201. [DOI] [PubMed] [Google Scholar]
- 221.Mirfakhraie R, Kalantar SM, Mirzajani F, Montazeri M, Salsabili N, Houshmand M, et al. A novel mutation in the transactivation-regulating domain of the androgen receptor in a patient with azoospermia. J Androl. 2011;32(4):367–70. doi: 10.2164/jandrol.110.010645. [DOI] [PubMed] [Google Scholar]
- 222.Hose KA, Haffner K, Fietz D, Gromoll J, Eckert T, Kliesch S, et al. A novel sequence variation in the transactivation regulating domain of the human androgen receptor. Fertil Steril. 2009;92(1):390 e9–e11. doi: 10.1016/j.fertnstert.2009.02.068. [DOI] [PubMed] [Google Scholar]
- 223.Tut TG, Ghadessy FJ, Trifiro MA, Pinsky L, Yong EL. Long polyglutamine tracts in the androgen receptor are associated with reduced trans-activation, impaired sperm production, and male infertility. J Clin Endocrinol Metab. 1997;82(11):3777–82. doi: 10.1210/jcem.82.11.4385. [DOI] [PubMed] [Google Scholar]
- 224.Stocco DM. StAR protein and the regulation of steroid hormone biosynthesis. Annu Rev Physiol. 2001;63:193–213. doi: 10.1146/annurev.physiol.63.1.193. [DOI] [PubMed] [Google Scholar]
- 225.Bose HS, Pescovitz OH, Miller WL. Spontaneous feminization in a 46,XX female patient with congenital lipoid adrenal hyperplasia due to a homozygous frameshift mutation in the steroidogenic acute regulatory protein. J Clin Endocrinol Metab. 1997;82(5):1511–5. doi: 10.1210/jcem.82.5.3962. [DOI] [PubMed] [Google Scholar]
- 226.Metherell LA, Naville D, Halaby G, Begeot M, Huebner A, Nurnberg G, et al. Nonclassic lipoid congenital adrenal hyperplasia masquerading as familial glucocorticoid deficiency. J Clin Endocrinol Metab. 2009;94(10):3865–71. doi: 10.1210/jc.2009-0467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Pang S. The molecular and clinical spectrum of 3beta-hydroxysteroid dehydrogenase deficiency disorder. Trends Endocrinol Metab. 1998;9(2):82–6. doi: 10.1016/s1043-2760(98)00015-0. [DOI] [PubMed] [Google Scholar]
- 228.Leshin M, Griffin JE, Wilson JD. Hereditary male pseudohermaphroditism associated with an unstable form of 5 alpha-reductase. J Clin Invest. 1978;62(3):685–91. doi: 10.1172/JCI109176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Abu Elheija M, Dyomin V, Ganaiem M, Lunenfeld E, Vardy NS, Huleihel M. Distinct expression of interleukin-1alpha, interleukin-1beta, and interleukin-1 receptor antagonist in testicular tissues and cells from human biopsies with normal and abnormal histology. J Interferon Cytokine Res. 2011;31(4):401–8. doi: 10.1089/jir.2010.0059. [DOI] [PubMed] [Google Scholar]
- 230.Gonzalez CR, Matzkin ME, Frungieri MB, Terradas C, Ponzio R, Puigdomenech E, et al. Expression of the TGF-beta1 system in human testicular pathologies. Reprod Biol Endocrinol. 2010;8:148. doi: 10.1186/1477-7827-8-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Rozwadowska N, Fiszer D, Jedrzejczak P, Kosicki W, Kurpisz M. Interleukin-1 superfamily genes expression in normal or impaired human spermatogenesis. Genes Immun. 2007;8(2):100–7. doi: 10.1038/sj.gene.6364356. [DOI] [PubMed] [Google Scholar]
- 232.Adly MA, Abdelwahed Hussein MR. Expression of CD1d protein in human testis showing normal and abnormal spermatogenesis. Ultrastruct Pathol. 2011;35(3):124–9. doi: 10.3109/01913123.2010.546944. [DOI] [PubMed] [Google Scholar]
- 233.Miyakawa H, Miyamoto T, Koh E, Tsujimura A, Miyagawa Y, Saijo Y, et al. Single-Nucleotide Polymorphisms in the SEPTIN12 Gene May Be a Genetic Risk Factor for Japanese Patients With Sertoli Cell-Only Syndrome. J Androl. 2012;33(3):483–7. doi: 10.2164/jandrol.110.012146. [DOI] [PubMed] [Google Scholar]
- 234.Relle M, Cash H, Brochhausen C, Strand D, Menke J, Galle PR, et al. New perspectives on the renal slit diaphragm protein podocin. Mod Pathol. 2011;24(8):1101–10. doi: 10.1038/modpathol.2011.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Adly MA, Hussein MR. Expression of cytokeratin 10 protein in the human testis showing normal and abnormal spermatogenesis. Ultrastruct Pathol. 2011;35(5):209–13. doi: 10.3109/01913123.2011.598255. [DOI] [PubMed] [Google Scholar]
- 236.Ooba T, Ishikawa T, Yamaguchi K, Kondo Y, Sakamoto Y, Fujisawa M. Expression and distribution of laminin chains in the testis for patients with azoospermia. J Androl. 2008;29(2):147–52. doi: 10.2164/jandrol.107.003210. [DOI] [PubMed] [Google Scholar]
- 237.Matsuo Y, Nomata K, Eguchi J, Aoki D, Hayashi T, Hishikawa Y, et al. Immunohistochemical analysis of connexin43 expression in infertile human testes. Acta Histochem Cytochem. 2007;40(3):69–75. doi: 10.1267/ahc.07001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Lee JH, Choi KW, Lee SJ, Gye MC. Expression of beta-catenin in human testes with spermatogenic defects. Arch Androl. 2005;51(4):271–6. doi: 10.1080/014850190923387. [DOI] [PubMed] [Google Scholar]
- 239.Dobashi M, Fujisawa M, Naito I, Yamazaki T, Okada H, Kamidono S. Distribution of type IV collagen subtypes in human testes and their association with spermatogenesis. Fertil Steril. 2003;80 Suppl 2:755–60. doi: 10.1016/s0015-0282(03)00775-1. [DOI] [PubMed] [Google Scholar]
- 240.Defamie N, Berthaut I, Mograbi B, Chevallier D, Dadoune JP, Fenichel P, et al. Impaired gap junction connexin43 in Sertoli cells of patients with secretory azoospermia: a marker of undifferentiated Sertoli cells. Lab Invest. 2003;83(3):449–56. doi: 10.1097/01.lab.0000059928.82702.6d. [DOI] [PubMed] [Google Scholar]
- 241.Ravel C, El Houate B, Chantot S, Lourenco D, Dumaine A, Rouba H, et al. Haplotypes, mutations and male fertility: the story of the testis-specific ubiquitin protease USP26. Mol Hum Reprod. 2006;12(10):643–6. doi: 10.1093/molehr/gal063. [DOI] [PubMed] [Google Scholar]
- 242.Zhang XD, Yin LL, Zheng Y, Lu L, Zhou ZM, Sha JH. Expression of a novel beta adaptin subunit mRNA splice variant in human testes. Asian J Androl. 2005;7(2):179–88. doi: 10.1111/j.1745-7262.2005.00025.x. [DOI] [PubMed] [Google Scholar]
- 243.Gye MC, Kim ST. Expression of cathepsin L in human testis under diverse infertility conditions. Arch Androl. 2004;50(3):187–91. doi: 10.1080/01485010490425223. [DOI] [PubMed] [Google Scholar]
- 244.Cheng YS, Kuo PL, Teng YN, Kuo TY, Chung CL, Lin YH, et al. Association of spermatogenic failure with decreased CDC25A expression in infertile men. Hum Reprod. 2006;21(9):2346–52. doi: 10.1093/humrep/del163. [DOI] [PubMed] [Google Scholar]
- 245.Aarabi M, Modarressi MH, Soltanghoraee H, Behjati R, Amirjannati N, Akhondi MM. Testicular expression of synaptonemal complex protein 3 (SYCP3) messenger ribonucleic acid in 110 patients with nonobstructive azoospermia. Fertil Steril. 2006;86(2):325–31. doi: 10.1016/j.fertnstert.2005.12.070. [DOI] [PubMed] [Google Scholar]
- 246.Dan L, Lifang Y, Guangxiu L. Expression and possible functions of a novel gene SPATA12 in human testis. J Androl. 2007;28(4):502–12. doi: 10.2164/jandrol.106.001560. [DOI] [PubMed] [Google Scholar]
- 247.Cheng LJ, Li JM, Chen J, Ge YH, Yu ZR, Han DS, et al. NYD-SP16, a novel gene associated with spermatogenesis of human testis. Biol Reprod. 2003;68(1):190–8. doi: 10.1095/biolreprod.102.004242. [DOI] [PubMed] [Google Scholar]
- 248.Abdou AG, Hammam MA, Farag AG, Farouk S, Fawzy M. Immunohistochemical expression of cyclin A in testicular biopsies of fertile and infertile men: correlation with the morphometry of seminiferous tubules. Andrologia. 2011;43(1):57–64. doi: 10.1111/j.1439-0272.2009.01018.x. [DOI] [PubMed] [Google Scholar]
- 249.Schrader M, Muller-Tidow C, Ravnik S, Muller M, Schulze W, Diederichs S, et al. Cyclin A1 and gametogenesis in fertile and infertile patients: a potential new molecular diagnostic marker. Hum Reprod. 2002;17(9):2338–43. doi: 10.1093/humrep/17.9.2338. [DOI] [PubMed] [Google Scholar]
- 250.Medrano JV, Marques-Mari AI, Aguilar CE, Riboldi M, Garrido N, Martinez-Romero A, et al. Comparative analysis of the germ cell markers c-KIT, SSEA-1 and VASA in testicular biopsies from secretory and obstructive azoospermias. Mol Hum Reprod. 2010;16(11):811–7. doi: 10.1093/molehr/gaq044. [DOI] [PubMed] [Google Scholar]
- 251.Feng HL, Sandlow JI, Sparks AE, Sandra A, Zheng LJ. Decreased expression of the c-kit receptor is associated with increased apoptosis in subfertile human testes. Fertil Steril. 1999;71(1):85–9. doi: 10.1016/s0015-0282(98)00401-4. [DOI] [PubMed] [Google Scholar]
- 252.Sandlow JI, Feng HL, Cohen MB, Sandra A. Expression of c-KIT and its ligand, stem cell factor, in normal and subfertile human testicular tissue. J Androl. 1996;17(4):403–8. [PubMed] [Google Scholar]
- 253.Li T, Hu J, He GH, Li Y, Zhu CC, Hou WG, et al. Up-regulation of NDRG2 through nuclear factor-kappa B is required for Leydig cell apoptosis in both human and murine infertile testes. Biochim Biophys Acta. 2012;1822(2):301–13. doi: 10.1016/j.bbadis.2011.11.013. [DOI] [PubMed] [Google Scholar]
- 254.Adly MA, Hussein MR. Immunohistological profile of the Ras homologous B protein (RhoB) in human testes showing normal spermatogenesis, spermatogenic arrest and Sertoli cell only syndrome. Pathol Oncol Res. 2010;16(3):427–33. doi: 10.1007/s12253-009-9232-3. [DOI] [PubMed] [Google Scholar]
- 255.Huang X, Zhang J, Lu L, Yin L, Xu M, Wang Y, et al. Cloning and expression of a novel CREB mRNA splice variant in human testis. Reproduction. 2004;128(6):775–82. doi: 10.1530/rep.1.00036. [DOI] [PubMed] [Google Scholar]
- 256.Hu Z, Xia Y, Guo X, Dai J, Li H, Hu H, et al. A genome-wide association study in Chinese men identifies three risk loci for non-obstructive azoospermia. Nat Genet. 2012;44(2):183–6. doi: 10.1038/ng.1040. [DOI] [PubMed] [Google Scholar]
- 257.Fiszer D, Bialas M, Rozwadowska N, Kosicki W, Jedrzejczak P, Kurpisz M. Crem activator isoforms in normal and impaired human spermatogenesis analyzed by real time RT-PCR. Arch Androl. 2007;53(5):257–65. doi: 10.1080/01485010701569866. [DOI] [PubMed] [Google Scholar]
- 258.Faure AK, Pivot-Pajot C, Kerjean A, Hazzouri M, Pelletier R, Peoc'h M, et al. Misregulation of histone acetylation in Sertoli cell-only syndrome and testicular cancer. Mol Hum Reprod. 2003;9(12):757–63. doi: 10.1093/molehr/gag101. [DOI] [PubMed] [Google Scholar]
- 259.Wilcken B, Wiley V, Sherry G, Bayliss U. Neonatal screening for cystic fibrosis: a comparison of two strategies for case detection in 1.2 million babies. J Pediatr. 1995;127(6):965–70. doi: 10.1016/s0022-3476(95)70040-4. [DOI] [PubMed] [Google Scholar]
- 260.Lee JH, Choi KW, Lee SJ, Gye MC. Expression of beta-catenin in human testes with spermatogenic defects. Arch Androl. 2005;51(4):271–6. doi: 10.1080/014850190923387. [DOI] [PubMed] [Google Scholar]
- 261.Dobashi M, Fujisawa M, Naito I, Yamazaki T, Okada H, Kamidono S. Distribution of type IV collagen subtypes in human testes and their association with spermatogenesis. Fertil Steril. 2003;80 Suppl 2:755–60. doi: 10.1016/s0015-0282(03)00775-1. [DOI] [PubMed] [Google Scholar]
- 262.Defamie N, Berthaut I, Mograbi B, Chevallier D, Dadoune JP, Fenichel P, et al. Impaired gap junction connexin43 in Sertoli cells of patients with secretory azoospermia: a marker of undifferentiated Sertoli cells. Lab Invest. 2003;83(3):449–56. doi: 10.1097/01.lab.0000059928.82702.6d. [DOI] [PubMed] [Google Scholar]
- 263.Ravel C, El Houate B, Chantot S, Lourenco D, Dumaine A, Rouba H, et al. Haplotypes, mutations and male fertility: the story of the testis-specific ubiquitin protease USP26. Mol Hum Reprod. 2006;12(10):643–6. doi: 10.1093/molehr/gal063. [DOI] [PubMed] [Google Scholar]
- 264.Zhang XD, Yin LL, Zheng Y, Lu L, Zhou ZM, Sha JH. Expression of a novel beta adaptin subunit mRNA splice variant in human testes. Asian J Androl. 2005;7(2):179–88. doi: 10.1111/j.1745-7262.2005.00025.x. [DOI] [PubMed] [Google Scholar]
- 265.Gye MC, Kim ST. Expression of cathepsin L in human testis under diverse infertility conditions. Arch Androl. 2004;50(3):187–91. doi: 10.1080/01485010490425223. [DOI] [PubMed] [Google Scholar]
- 266.Cheng YS, Kuo PL, Teng YN, Kuo TY, Chung CL, Lin YH, et al. Association of spermatogenic failure with decreased CDC25A expression in infertile men. Hum Reprod. 2006;21(9):2346–52. doi: 10.1093/humrep/del163. [DOI] [PubMed] [Google Scholar]
- 267.Aarabi M, Modarressi MH, Soltanghoraee H, Behjati R, Amirjannati N, Akhondi MM. Testicular expression of synaptonemal complex protein 3 (SYCP3) messenger ribonucleic acid in 110 patients with nonobstructive azoospermia. Fertil Steril. 2006;86(2):325–31. doi: 10.1016/j.fertnstert.2005.12.070. [DOI] [PubMed] [Google Scholar]
- 268.Dan L, Lifang Y, Guangxiu L. Expression and possible functions of a novel gene SPATA12 in human testis. J Androl. 2007;28(4):502–12. doi: 10.2164/jandrol.106.001560. [DOI] [PubMed] [Google Scholar]
- 269.Cheng LJ, Li JM, Chen J, Ge YH, Yu ZR, Han DS, et al. NYD-SP16, a novel gene associated with spermatogenesis of human testis. Biol Reprod. 2003;68(1):190–8. doi: 10.1095/biolreprod.102.004242. [DOI] [PubMed] [Google Scholar]
- 270.Abdou AG, Hammam MA, Farag AG, Farouk S, Fawzy M. Immunohistochemical expression of cyclin A in testicular biopsies of fertile and infertile men: correlation with the morphometry of seminiferous tubules. Andrologia. 2011;43(1):57–64. doi: 10.1111/j.1439-0272.2009.01018.x. [DOI] [PubMed] [Google Scholar]
- 271.Schrader M, Muller-Tidow C, Ravnik S, Muller M, Schulze W, Diederichs S, et al. Cyclin A1 and gametogenesis in fertile and infertile patients: a potential new molecular diagnostic marker. Hum Reprod. 2002;17(9):2338–43. doi: 10.1093/humrep/17.9.2338. [DOI] [PubMed] [Google Scholar]
- 272.Sato Y, Yoshida K, Shinka T, Nozawa S, Nakahori Y, Iwamoto T. Altered expression pattern of heat shock transcription factor, Y chromosome (HSFY) may be related to altered differentiation of spermatogenic cells in testes with deteriorated spermatogenesis. Fertil Steril. 2006;86(3):612–8. doi: 10.1016/j.fertnstert.2006.01.053. [DOI] [PubMed] [Google Scholar]
- 273.Son WY, Han CT, Hwang SH, Lee JH, Kim S, Kim YC. Repression of hspA2 messenger RNA in human testes with abnormal spermatogenesis. Fertil Steril. 2000;73(6):1138–44. doi: 10.1016/s0015-0282(00)00496-9. [DOI] [PubMed] [Google Scholar]
- 274.Adly MA, Assaf HA, Hussein MR. Heat shock protein 27 expression in the human testis showing normal and abnormal spermatogenesis. Cell Biol Int. 2008;32(10):1247–55. doi: 10.1016/j.cellbi.2008.07.009. [DOI] [PubMed] [Google Scholar]
- 275.Medrano JV, Marques-Mari AI, Aguilar CE, Riboldi M, Garrido N, Martinez-Romero A, et al. Comparative analysis of the germ cell markers c-KIT, SSEA-1 and VASA in testicular biopsies from secretory and obstructive azoospermias. Mol Hum Reprod. 2010;16(11):811–7. doi: 10.1093/molehr/gaq044. [DOI] [PubMed] [Google Scholar]
- 276.Feng HL, Sandlow JI, Sparks AE, Sandra A, Zheng LJ. Decreased expression of the c-kit receptor is associated with increased apoptosis in subfertile human testes. Fertil Steril. 1999;71(1):85–9. doi: 10.1016/s0015-0282(98)00401-4. [DOI] [PubMed] [Google Scholar]
- 277.Sandlow JI, Feng HL, Cohen MB, Sandra A. Expression of c-KIT and its ligand, stem cell factor, in normal and subfertile human testicular tissue. J Androl. 1996;17(4):403–8. [PubMed] [Google Scholar]
- 278.Li T, Hu J, He GH, Li Y, Zhu CC, Hou WG, et al. Up-regulation of NDRG2 through nuclear factor-kappa B is required for Leydig cell apoptosis in both human and murine infertile testes. Biochim Biophys Acta. 2012;1822(2):301–13. doi: 10.1016/j.bbadis.2011.11.013. [DOI] [PubMed] [Google Scholar]
- 279.Adly MA, Hussein MR. Immunohistological profile of the Ras homologous B protein (RhoB) in human testes showing normal spermatogenesis, spermatogenic arrest and Sertoli cell only syndrome. Pathol Oncol Res. 2010;16(3):427–33. doi: 10.1007/s12253-009-9232-3. [DOI] [PubMed] [Google Scholar]
- 280.Huang X, Zhang J, Lu L, Yin L, Xu M, Wang Y, et al. Cloning and expression of a novel CREB mRNA splice variant in human testis. Reproduction. 2004;128(6):775–82. doi: 10.1530/rep.1.00036. [DOI] [PubMed] [Google Scholar]
- 281.Hu Z, Xia Y, Guo X, Dai J, Li H, Hu H, et al. A genome-wide association study in Chinese men identifies three risk loci for non-obstructive azoospermia. Nat Genet. 2012;44(2):183–6. doi: 10.1038/ng.1040. [DOI] [PubMed] [Google Scholar]
- 282.Fiszer D, Bialas M, Rozwadowska N, Kosicki W, Jedrzejczak P, Kurpisz M. Crem activator isoforms in normal and impaired human spermatogenesis analyzed by real time RT-PCR. Arch Androl. 2007;53(5):257–65. doi: 10.1080/01485010701569866. [DOI] [PubMed] [Google Scholar]
- 283.Kojima Y, Sasaki S, Hayashi Y, Umemoto Y, Morohashi K, Kohri K. Role of transcription factors Ad4bp/SF-1 and DAX-1 in steroidogenesis and spermatogenesis in human testicular development and idiopathic azoospermia. Int J Urol. 2006;13(6):785–93. doi: 10.1111/j.1442-2042.2006.01403.x. [DOI] [PubMed] [Google Scholar]
- 284.Stouffs K, Tournaye H, Van der Elst J, Liebaers I, Lissens W. Is there a role for the nuclear export factor 2 gene in male infertility. Fertil Steril. 2008;90(5):1787–91. doi: 10.1016/j.fertnstert.2007.08.071. [DOI] [PubMed] [Google Scholar]
- 285.Faure AK, Pivot-Pajot C, Kerjean A, Hazzouri M, Pelletier R, Peoc'h M, et al. Misregulation of histone acetylation in Sertoli cell-only syndrome and testicular cancer. Mol Hum Reprod. 2003;9(12):757–63. doi: 10.1093/molehr/gag101. [DOI] [PubMed] [Google Scholar]
- 286.Maymon BB, Cohen-Armon M, Yavetz H, Yogev L, Lifschitz-Mercer B, Kleiman SE, et al. Role of poly(ADP-ribosyl)ation during human spermatogenesis. Fertil Steril. 2006;86(5):1402–7. doi: 10.1016/j.fertnstert.2006.03.063. [DOI] [PubMed] [Google Scholar]
- 287.Saitou M, Payer B, O'Carroll D, Ohinata Y, Surani MA. Blimp1 and the emergence of the germ line during development in the mouse. Cell Cycle. 2005;4(12):1736–40. doi: 10.4161/cc.4.12.2209. [DOI] [PubMed] [Google Scholar]
- 288.Yamaji M, Seki Y, Kurimoto K, Yabuta Y, Yuasa M, Shigeta M, et al. Critical function of Prdm14 for the establishment of the germ cell lineage in mice. Nat Genet. 2008;40(8):1016–22. doi: 10.1038/ng.186. [DOI] [PubMed] [Google Scholar]
- 289.Ying Y, Zhao GQ. Cooperation of endoderm-derived BMP2 and extraembryonic ectoderm-derived BMP4 in primordial germ cell generation in the mouse. Dev Biol. 2001;232(2):484–92. doi: 10.1006/dbio.2001.0173. [DOI] [PubMed] [Google Scholar]
- 290.Di Carlo A, De Felici M. A role for E-cadherin in mouse primordial germ cell development. Dev Biol. 2000;226(2):209–19. doi: 10.1006/dbio.2000.9861. [DOI] [PubMed] [Google Scholar]
- 291.Saunders PT, Turner JM, Ruggiu M, Taggart M, Burgoyne PS, Elliott D, et al. Absence of mDazl produces a final block on germ cell development at meiosis. Reproduction. 2003;126(5):589–97. doi: 10.1530/rep.0.1260589. [DOI] [PubMed] [Google Scholar]
- 292.Dada R, Thilagavathi J, Venkatesh S, Esteves SC, Agarwal A. Genetic testing in male infertility. Open Reprod Sci J. 2011;3:42–56. [Google Scholar]
- 293. Dada R, Shamsi M B, Venkatesh S, Genetics of male Infertility 2010New Delhi: Jaypee Brothers Medical Publishers (P) Ltd [Google Scholar]
- 294.Dada R, Kumar R, Shamsi MB, et al. Genetic screening in couples experiencing recurrent assisted procreation failure. Indian J Biochem Biophys. 2008;45:116–20. [PubMed] [Google Scholar]
- 295.Lee JY, Dada R, Sabanegh E, Carpi A, Agarwal A. Role of Genetics in Azoospermia. Urology. 2011;77(3):598–601. doi: 10.1016/j.urology.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 296.Simoni M, Bakker E, Eurlings MC, et al. Laboratory guidelines for molecular diagnosis of Y-chromosomal microdeletions. Int J Androl. 1999;22(5):292–9. doi: 10.1046/j.1365-2605.1999.00193.x. [DOI] [PubMed] [Google Scholar]
- 297. Hamada A, Esteves SC, Agarwal A. Dubey A , Genetics and Male Infertility 2012New Delhi: Jaypee Brothers Medical Publishers; p. 113–160.Infertility - Diagnosis, Management & IVF. 1st edition [Google Scholar]
- 298.Nakamura Y, Kitamura M, Nishimura K, et al. Chromosomal variants among 1790 infertile men. Int J Urol. 2001;8(2):49–52. doi: 10.1046/j.1442-2042.2001.00242.x. [DOI] [PubMed] [Google Scholar]
- 299.Balkan M, Tekes S, Gedik A. Cytogenetic and Y chromosome microdeletion screening studies in infertile males with Oligozoospermia and Azoospermia in Southeast Turkey. J Assist Reprod Genet. 2008;25(11-12):559–65. doi: 10.1007/s10815-008-9272-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Akgul M, Ozkinay F, Ercal D, et al. Cytogenetic abnormalities in 179 cases with male infertility in Western Region of Turkey: report and review. J Assist Reprod Genet. 2009;26(2-3):119–22. doi: 10.1007/s10815-009-9296-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Rives N, Joly G, Machy A, Simeon N, Leclerc P, Mace B. Assessment of sex chromosome aneuploidy in sperm nuclei from 47,XXY and 46,XY/47,XXY males: comparison with fertile and infertile males with normal karyotype. Mol Hum Reprod. 2000;6(2):107–12. doi: 10.1093/molehr/6.2.107. [DOI] [PubMed] [Google Scholar]
- 302.Martinez-Garza SG, Gallegos-Rivas MC, Vargas-Maciel M, Rubio-Rubio JM, de Los Monteros-Rodríguez ME, Gonzáles-Ortega C, et al. Genetic screening in infertile Mexican men: chromosomal abnormalities, Y chromosome deletions, and androgen receptor CAG repeat length. J Androl. 2008;29(6):654–60. doi: 10.2164/jandrol.107.004309. [DOI] [PubMed] [Google Scholar]
- 303.Conn CM, Cozzi J, Harper JC, Winston RM, Delhanty JD. Preimplantation genetic diagnosis for couples at high risk of Down syndrome pregnancy owing to parental translocation or mosaicism. J Med Genet. 1999;36(1):45–50. [PMC free article] [PubMed] [Google Scholar]
- 304.Scriven PN, Flinter FA, Braude PR, Ogilvie CM. Robertsonian translocations--reproductive risks and indications for preimplantation genetic diagnosis. Hum Reprod. 2001;16(11):2267–73. doi: 10.1093/humrep/16.11.2267. [DOI] [PubMed] [Google Scholar]
- 305.Stahl PJ, Masson P, Mielnik A, Marean MB, Schlegel PN, Paduch DA. A decade of experience emphasizes that testing for Y microdeletions is essential in American men with azoospermia and severe oligozoospermia. Fertil Steril. 2010;94(5):1753–1756. doi: 10.1016/j.fertnstert.2009.09.006. [DOI] [PubMed] [Google Scholar]
- 306.Komori S, Kato H, Kobayashi S, Koyama K, Isojima S. Transmission of Y chromosomal microdeletions from father to son through intracytoplasmic sperm injection. J Hum Genet. 2002;47(9):465–8. doi: 10.1007/s100380200066. [DOI] [PubMed] [Google Scholar]
- 307.Carrell DT, De Jonge C, Lamb DJ. The genetics of male infertility: a field of study whose time is now. Arch Androl. 2006;52(4):269–74. doi: 10.1080/01485010500503603. [DOI] [PubMed] [Google Scholar]
- 308.Lin YH, Lin YM, Teng YN, Hsieh TY, Lin YS, Kuo PL. Identification of ten novel genes involved in human spermatogenesis by microarray analysis of testicular tissue. Fertil Steril. 2006;86:1650–8. doi: 10.1016/j.fertnstert.2006.04.039. [DOI] [PubMed] [Google Scholar]
- 309.Ellis PJ, Furlong RA, Conner SJ, Kirkman-Brown J, Afnan M, Barratt C, et al. Coordinated transcriptional regulation patterns associated with infertility phenotypes in men. J Med Genet. 2007;44:498–508. doi: 10.1136/jmg.2007.049650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Johnston DS, Wooters J, Kopf GS, Qiu Y, Roberts KP. Analysis of the human sperm proteome. Ann N YAcad Sci. 2005;1061:190–202. doi: 10.1196/annals.1336.021. [DOI] [PubMed] [Google Scholar]
- 311.Pilch B, Mann M. Large-scale and high-confidence proteomic analysis of human seminal plasma. Genome Biol. 2006;7:R40. doi: 10.1186/gb-2006-7-5-r40. [DOI] [PMC free article] [PubMed] [Google Scholar]