Abstract
Obstructive azoospermia is a common cause of male infertility and can result from infection, congenital anomalies, or iatrogenic injury. Microsurgical vasal reconstruction is a suitable treatment for many cases of obstructive azoospermia, although some couples will require sperm retrieval paired with in-vitro fertilization. The various causes of obstructive azoospermia and recommended treatments will be examined. Microsurgical vasovasostomy and vasoepididymostomy will be discussed in detail.
The postoperative patency and pregnancy rates for surgical reconstruction of obstructive azoospermia and the impact of etiology, obstructive interval, sperm granuloma, age, and previous reconstruction on patency and pregnancy will be reviewed.
Keywords: Obstructive Azoospermia, Wolffian Duct Abnormalities, Iatrogenic Injury, Microsurgery, Vasovasostomy
INTRODUCTION
Obstructive azoospermia (OA) is defined as the absence of spermatozoa in the ejaculate despite normal spermatogenesis. OA is a common urologic condition and accounts for 6.1% (1) to 13.6% (2) of patients presenting for fertility evaluation. Vasectomy is a frequent cause of OA; however, alternate etiologies represent 19% (3) to 69% (4) of patients undergoing surgical exploration for OA. Infection, iatrogenic injury, and genetic and congenital conditions are all possible causes of OA. While some of these conditions are amenable to curative surgery, others will require sperm retrieval and in-vitro fertilization/intracytoplasmic sperm injection (IVF/ICSI).
Is correction of OA necessary when couples could elect to proceed directly to sperm retrieval and IVF/ICSI? While treatment should be tailored to the individual couple, there is an excellent rationale for recommending surgical reconstruction for OA. First, treatment may obviate the need for IVF/ICSI and thereby eliminate the risks and costs associated with advanced assisted reproductive techniques. Cost analyses reveal that vasectomy reversal is less expensive than IVF/ICSI (5-8). IVF/ICSI also subjects the spouse to risks, such as ovarian hyperstimulation syndrome, that are not present with spontaneous conception. The rate of birth defects is higher, albeit slightly, with IVF/ICSI. Multiple gestations occur in over 30% of all IVF/ICSI pregnancies (9) and carry risks to the mother and unborn children, such as prematurity and low birth weight.
In the following chapter, we will describe the various etiologies for obstructive azoospermia and discuss the treatment options. The factors that influence the success of vasal reconstruction will be reviewed, and the microsurgical techniques for vasovasostomy (VV) and vasoepididymostomy (VE) will be described in detail.
Etiologies
Ejaculatory duct obstruction
Ejaculatory duct obstruction (EDO) is a rare cause of OA and accounts for approximately 1% of patients presenting with male infertility. EDO is an evolving topic, and a discussion regarding partial vs. complete EDO and functional vs. anatomic obstruction is beyond the scope of this chapter. The diagnosis of complete EDO should be suspected when the patient has low-volume, acidic semen that contains no sperm. An absence of fructose in the semen supports the diagnosis, as fructose is present in the secretions from the seminal vesicles. Occasionally, pain at the time of ejaculation is reported. Physical examination may reveal enlarged seminal vesicles or a midline nodule in the prostate, but frequently, the rectal exam is unremarkable. Testicular volume is usually normal, and the vasa deferentia are present. Laboratory studies will confirm normal gonadotropin and testosterone levels. Retrograde ejaculation should be rule out by examining post-ejaculatory urine for sperm. Transrectal ultrasound is a useful tool for confirming the diagnosis and further defining the causative factor. A 7 to 10 mHz endocavitary probe provides excellent visualization of the prostate and other accessory sex organs. Dilation of the seminal vesicles to greater than 1.5 cm in the anteroposterior axis is consistent with EDO, and the presence of 10 or more sperm per high-powered field in the seminal vesicle aspirate confirms the diagnosis. To aid diagnosis, the patient should be instructed to ejaculate within the 24 hours prior to the ultrasound. Sonography can also demonstrate dilation of the ejaculatory ducts, calcifications within the ejaculatory ducts, or prostate, utricle, or Müllerian duct cysts that can occlude the ejaculatory ducts.
Traditional treatment consists of transurethral resection of the ejaculatory ducts (TURED). Yurdakul et al. retrospectively reviewed the outcomes of 12 azoospermic men with EDO who underwent TURED. Sperm appeared in the ejaculate of 11 of 12 patients. Of these 11 patients, 42% (n = 5) had a postoperative sperm concentration of>20 mil/ml. The authors reported spontaneous pregnancy in three couples, pregnancy by IUI in one couple, and one couple with sperm concentration less than five million per ml who obtained a pregnancy through ICSI using fresh ejaculated sperm (10). Emerging data suggests that vesiculoscopy paired with ejaculatory duct dilation and/or calculi extraction may also be a viable treatment option for patients with EDO (11,12).
Wolffian duct abnormalities
Congenital bilateral absence of the vas deferens (CBAVD) is often caused by a mutation in the cystic fibrosis transmembrane conductance regulator (CFTR) gene. This condition is suspected based on the absence of palpable vas deferens at the time of physical exam. The caput of the epididymis is present, and the testicles should be a normal size and consistency; however, the seminal vesicles are absent or hypoplastic in the majority of patients (13). CBAVD can also be associated with unilateral renal agenesis in a minority of patients (14).
Unilateral absence or hypoplasia of the vas deferens is derived from failure of organogenesis of the Wolffian ducts system, and its association with renal agenesis has been well described. Unilateral or bilateral vasal hypoplasia or unilateral absence of the vas may be an indicator of obstructive azoospermia, as a high percentage of these patients will have anomalies of the contralateral seminal vesicle. Raviv et al. published their experience with TRUS in the evaluation of low-volume azoospermic men and noted that 10 of 12 patients (83%) with unilateral absence of the vas demonstrated contralateral abnormalities of the seminal vesicles or ejaculatory ducts (15). Partial vasal agenesis has also been described. Anger and Goldstein published a series of three men found to have segmental dysplasia of the vas deferens during scrotal exploration for possible microsurgical reconstruction (16).
Surgical reconstruction may be a viable treatment for some patients with unilateral vasal agenesis or hypoplasia. CBAVD is not amenable to surgical reconstruction, but sperm is readily retrievable from these patients via percutaneous (PESA) or microsurgical (MESA) epididymal aspiration, testicular sperm aspiration (TESA), or simple open biopsy (TESE).
Young's syndrome
Young's syndrome is obstructive azoospermia associated with chronic sinopulmonary infections. Initially described in 1950 by Dr. David Young, the relative rarity of this condition in the modern era has caused some to call the existence of this syndrome into question (17). Mercury exposure is one proposed etiology for Young's syndrome, and in an elegant argument supporting this theory, Hendry et al. demonstrated the decreasing incidence of Young's syndrome in men born after mercury-containing teething powder and worm medications were banned in the United Kingdom (18). There is building evidence that modern day Young's syndrome may be genetic variations of Kartagener's syndrome (19,20) or CFTR gene mutations (21,22). Genetic testing should be performed in patients presenting with signs and symptoms of Young's syndrome. Surgical reconstruction, while technically feasible, has resulted in poor outcomes in traditional cases of Young's syndrome (18). Sperm retrieval paired with IVF/ICSI is the best option for these couples.
Infection
Epididymitis is a common genitourinary condition, and an infectious etiology should always be considered in men with this diagnosis. Gonorrhea, chlamydia, trichomonas, brucellosis, BCG, ureaplasma, mycoplasma, coliforms bacteria, adenovirus, and enterovirus have all been reported as causes of epididymitis. Regardless of the etiology, epididymitis can cause an intense inflammatory reaction, leading to secondary scarring and obstruction of the epididymis. Physical examination may reveal enlarged or indurated epididymides and a transition point suggesting the site of obstruction. Semen volumes are typically normal, and white cells are not necessarily present in the ejaculate or urine outside of the period of acute infection. In cases of tuberculosis, the vas deferens may be nodular and enlarged, and a low-volume ejaculate may be present when the disease involves the prostate and seminal vesicles.
Infection was the proposed etiology for obstructive azoospermia in 8-46% of patients undergoing vasal reconstruction in several large series (2,4,23,24). The incidence of post-infectious epididymal obstruction is thought to be low in developed countries due to prompt treatment, but it may account for a disproportionately large percentage of OA in the developing world (25). Twenty-three percent of infertile men presenting to a Nigerian teaching hospital had findings consistent with chronic infectious epididymitis, and 14% of infertile men had azoospermia attributed to post-infectious obstruction of the vas or epididymis (26). In a retrospective review of couples with male factor fertility evaluated at a tertiary hospital in Nigeria, Eke et al. reported sexually transmitted disease as the cause of infertility in 29.4% of men, with the majority of these men presenting with signs and/or symptoms consistent with active infection (27). OA due to infection was diagnosed in 8.6% of men with male factor infertility, and an additional 4.3% of men were diagnosed with an infection of the male accessory sex glands in a study of infertility in Western Siberia (28). A study of infertile couples in Mongolia found post-infectious obstructive azoospermia and male accessory gland infection in 8.4% and 6.7% of men, respectively (29). A high percentage of these men (44.2%) reported previous treatment for sexually transmitted infections (STI), with 59%, 9.1%, and 1.2% reporting treatment for gonorrhea, trichomonas, and chlamydia, respectively. Vigil et al. found chlamydia in 38.6% of males in couples presenting for fertility evaluation in Chile but detected no statistically significant differences in semen parameters between men with and without active chlamydia infections (30).
Scrotal exploration and microsurgical reconstruction is a viable option for post-infectious epididymal obstruction, and the outcomes and surgical techniques are described later in this chapter. A notable exception is genitourinary tuberculosis. Outcomes for surgical reconstruction for tuberculosis are particularly poor due to scarring at multiple levels of the male reproductive tract (31). Once identified, prompt treatment for genitourinary tuberculosis should be initiated, as early treatment may resolve the inflammation and return sperm to the ejaculate (32). Sperm retrieval paired with IVF/ICSI should be considered for patients who remain azoospermic despite adequate treatment for tuberculosis (31).
Iatrogenic injury
Injury to the vas during surgical procedures has been well described and presents a unique challenge to fertility specialists. Vasal injury has been attributed to a variety of inguinal, scrotal, and pelvic surgeries, including herniorrhaphy, hydrocelectomy, appendectomy, and renal transplant. Trauma is a rare cause of vasal obstruction (4). The author has experience with one patient with proven paternity who was unreconstructable at the time of vasectomy reversal due to obstruction of the pelvic vas, which was presumably due to a history of multiple pelvic fractures suffered during a blast injury. Transection, compression, fibrosis, and ischemic injury are all possible mechanisms for vasal injury. There are no large series establishing the most common mechanisms of injury; however, transection of the vas is thought to account for no more than 25% of the cases of postsurgical obstruction based on surgical series and examination of pathological specimens (33,34).
Obstruction was attributed to iatrogenic injury in 8-19% of patients in several series examining the outcomes of VE (4,23,24). Sheynkin et al. reviewed 472 men who underwent scrotal exploration for obstructive azoospermia and found that 7.2% of men had findings consistent with iatrogenic injury to the vas deferens. Pediatric inguinal hernia repair was the most common cause (59%), followed by adult inguinal hernia repair (29%), renal transplant (6%), appendectomy (3%), and spermatocelectomy (3%) (35). Fifty-six percent of the cases had a history of bilateral procedures that were exclusively herniorrhaphy. A history of a unilateral surgery was noted in 44% of the cohort; however, all of these patients had a contralateral abnormalities that included vasal and/or epididymal obstruction, testicular atrophy, absent testis, congenital epididymal aplasia, and congenital absence of the vas deferens. The likelihood of vasal obstruction after inguinal hernia repair may be influenced by the surgical approach (laparoscopic vs. open), pediatric vs. adult hernia repair, the surgical method, and the material used to bolster the repair (36). Of particular concern to fertility specialists is the use of polypropylene mesh. Shin et al. described 14 patients from eight infertility centers diagnosed with vasal obstruction secondary to polypropylene mesh herniorrhaphy. Obstruction at the hernia repair was confirmed with vasography, and exploration revealed dense fibrosis encasing and in some cases obliterating the vas deferens (37). In theory, newer, lightweight mesh material causes less of an inflammatory reaction and may decrease the chances of vasal obstruction secondary to hernia repair (36).
Surgical reconstruction is possible in many cases of iatrogenic injury to the vas in the scrotum or inguinal canal; however, the surgeon should be prepared to perform VE and other complex repairs.
Elective sterilization
Prevalence of vasectomy varies by country and is influenced by affluence, religion, and culture. Vasal reconstruction is the preferred method for restoration of fertility after a vasectomy, and due to the popularity of vasectomy and frequency of divorce, the demand for this procedure will continue to grow. Reconstruction is less expensive than sperm retrieval paired with IVF/ICSI, avoids the risks associated with IVF/ICSI, and offers the possibility of natural conception and multiple pregnancies over time without additional expense (38). Sperm retrieval may be a reasonable option in couples likely to require IVF for concomitant female factor due to advanced age or tubal disease. In these cases, sperm can readily be obtained through PESA performed with local anesthetic or sedation.
Men with previous paternity and normal genitourinary exams do not require additional fertility evaluation before proceeding to surgery. Patients should be queried about previous inguinal, scrotal, or pelvic surgeries, as these procedures may complicate vasal reconstruction. The physical exam should confirm normal testicles bilaterally. Enlarged epididymides are common, and the location and size of the vasectomy defects should be noted. Couples should be counseled about the option of intraoperative sperm retrieval for cryopreservation, and it is our practice to recommend this step to couples with a higher likelihood of requiring VE.
INFLUENTIAL FACTORS
The majority of the literature exploring the factors that influence the success of vasal reconstruction is derived from the outcomes after vasectomy reversal. Some factors, such as age and obstructive interval, are likely to impact postoperative outcomes after vasal reconstruction for other etiologies of OA.
Obstructive interval
An obstructive interval of 10 years or longer was thought to portend a poor outcome after vasal reconstruction. Recent publications have reported minimal decline in patency among couples with obstructive intervals of 10 years or longer, though pregnancy rates are lower in couples with longer obstructive intervals. The Vasovasostomy Study Group reported that patency and pregnancy rates decreased with increasing time since the vasectomy; however, pregnancy rates declined more rapidly. When grouped by obstructive interval, patency and pregnancy rates were 97% and 76%, respectively, for less than three years, 88% and 53%, respectively, for 3 to 8 years, 79% and 44%, respectively, for 9 to 14 years, and 71% and 30%, respectively, for intervals of 15 years or more (39). In 2004, Boorjian reviewed 213 patients randomly selected from a single surgeon's 17-year operative experience of bilateral vasal reconstructions. Patency (defined as the presence of any intact sperm in the ejaculate) was achieved in 90% of patients, and there was no statistically significant difference in patency rates based on obstructive interval. Pregnancy rates, however, decreased dramatically from 85% for obstructive intervals of 15 years or less to 44% for intervals of more than 15 years (p<0.05) (40). Magheli reviewed a single surgeon's series of 334 vasectomy reversals and reported that patency and pregnancy rates were not influenced by the length of obstructive interval, although multivariate analysis revealed that longer obstructive intervals were associated with an increased tendency to perform VE (41). Kolettis found favorable patency and pregnancy rates in 74 patients with obstructive intervals of 10 years or longer drawn from the experiences of three surgeons. Patency and pregnancy rates were 74% and 40%, 87% and 36%, and 75% and 27% for obstructive intervals of 10 to 15 years, 16 to 19 years, and 20 or more years, respectively (42). The authors concluded that pregnancy rates after obstructive intervals of up to 20 years were on par with IVF/ICSI.
Age
Age of the female partner significantly impacts postoperative pregnancy rates, as female fertility potential drops profoundly in women over 40 years of age (41,43). Gerrard demonstrated a precipitous decline in postoperative pregnancy rates after age 40 in a series of 249 vasal reconstructions. Postoperative patency and pregnancy rates were 90% and 67%, respectively, for females age 20-24, 89% and 52%, respectively, for those age 25-29, 90% and 57%, respectively, for those age 30-34, 86% and 54%, respectively, for those age 35-39, and 83% and 14%, respectively, for those age 40 and older (44). Kolettis examined the outcomes of 46 vasectomy reversals in men with female partners aged 35 or older and found a marked decline in pregnancy rates when the female partner was 40 years of age or older. Overall patency and pregnancy rates were 81% and 35%, respectively, though the pregnancy rate was 46% for women 35 to 39 and only 14% for women 40 or older (45). Hinz examined 212 vasectomy reversals performed by a single surgeon and found female age to be an independent predictor of postoperative pregnancy on multivariate analysis, with age 40 and older associated with significantly poor pregnancy rates compared with the younger age groups (42% vs. 74%, respectively) (46).
In contrast, the age of the male does not appear to independently influence patency or pregnancy after vasectomy reversal. In some series, older male age is associated with longer obstructive intervals, which in turn may be associated with increased need to performed VE (41,47).
Couples with previous conceptions together
Several studies have demonstrated that a history of previous conception together increases a couple's chance of pregnancy after vasectomy reversal. The Vasovasostomy Study Group reported 86% patency and 75% pregnancy rates in couples citing death of a child as the reason for vasectomy reversal (39). Chan compared the outcomes of 27 couples with a history of previous children together to 100 historical controls. Postoperative patency and pregnancy rates for couple with previous children together were 100% and 86%, respectively. Patency was not significantly different between the study group and historical cohort, but the pregnancy rate in the study group far exceeded the 54% pregnancy rate in the historical controls. Notably, the mean age of the study group was statistically older than the historical control (37.2 vs. 29.9, p<0.01) (48). Hernandez and Sabanegh examined the outcomes of 41 couples undergoing repeat vasal reconstruction and found couples with a history of children together had a pregnancy rate of 80% compared with couples married to new partners, in whom the pregnancy rate was only 17% (49). In contrast, Kim et al. examined the outcomes of 44 couples undergoing repeat vasectomy reversal and found no significant difference in pregnancy rates between couples with a history of children together and couples married to new partners. The authors determined that female age of less than 35 years was the only significant predictor of pregnancy after repeat VV (50).
Granuloma
Much attention has been paid to the impact of the presence of sperm granuloma on the success of vasectomy reversal. The published literature provides conflicting results, but the balance of evidence suggests that sperm granuloma does not impact postoperative pregnancy rates and does not exert a strong influence on postoperative patency. The Vasovasostomy Study Group found no difference in postoperative patency or pregnancy when comparing patients with and without histologically confirmed sperm granulomas (39). Magheli found that the presence of sperm granuloma did not improve postoperative patency or pregnancy rates (41). Boorjian examined the outcomes of 213 vasectomy reversals and determined that the presence of sperm granuloma was associated with a lower incidence of VE but that it was not associated with an increase in patency or pregnancy rates (40). Conversely, Bolduc found the presence of a sperm granuloma correlated with patency in a series of 747 vasectomy reversals (51). Hinz reported the presence of a sperm granuloma improved patency but not pregnancy rates in a review of 351 vasectomy reversals (52).
Previous reconstruction
Repeat vasal reconstruction yields encouraging patency and pregnancy rates. Piack reported patency and natural birth rates of 92% and 52%, respectively, in 62 patients who underwent repeat vasal reconstruction after failed VV. Of note, unless technically unfeasible, the authors performed VV regardless of the quality of the intravasal fluid or presence of sperm (43). Hollingsworth reported patency and pregnancy rates of 85% and 44%, respectively, in 49 patients undergoing repeat vasectomy reversal. Unilateral or bilateral VE was performed in 34% of the patients. An obstructive interval of 10 years or more did not predict an increased need to perform VE or negatively impact the rates of patency or pregnancy after repeat reconstruction in this series (53). Hernandez and Sabanegh reported overall patency and pregnancy rates of 79% and 31%, respectively, in 41 couples who underwent repeat vasectomy reversal after one or more attempts at vasal reconstruction. Unilateral or bilateral VE was performed in 73% of these couples (49). Pasqualotto reported patency and spontaneous pregnancy in 66.7% and 25%, respectively, in 18 couples who underwent bilateral (n = 8) or isolated unilateral (n = 10) VE after failure of previous VE (54). The literature supports repeat vasal reconstruction, though the surgeon should be comfortable performing VE, as the need to perform VE is frequently reported.
SURGICAL TECHNIQUE
In 1977, Silber and Owen independently described the microsurgical approach to vasectomy reversal and thereby ushered in the modern era of vasal reconstruction. The microsurgical approach is the gold standard for vasal reconstruction, as the precise mucosal-to-mucosal anastomosis is believed to result in superior outcomes. Series comparing microsurgical, Loupe magnification, and unmagnified VV have revealed that patency and pregnancy rates are better when higher magnification is used (55-57). To date, there have only been two published reports to detail the outcomes of robot-assisted vasovasostomies in humans. Neither report included pregnancy rates, and patency after robot-assisted reconstruction was either inferior or on par with traditional microsurgery (58,59). Given these results and the expense of robot-assisted surgery, we advocate a traditional microsurgical approach to vasal reconstruction.
General or spinal anesthesia is typically favored for vasal reconstruction due to the possible length of these cases. Patients should be positioned in a supine position, the scrotal hair clipped, and the clippings thoroughly removed to prevent interference with visualization of the suture. The patient should be positioned and padded appropriately to prevent iatrogenic injuries, such as occipital alopecia, brachial plexus injuries, and myolysis. Sequential compression devices and prophylactic perioperative antibiotics are recommended.
Vasovasostomy
The vasectomy defect is identified and swept to the anterior scrotal wall (Figure 1). A small vertically oriented incision, typically no longer than 2 cm, is made through the anterior scrotal skin, and the dartos is divided until the vas deferens is identified. Healthy appearing portions of the vas immediately proximal and distal to the vasectomy defect or sperm granuloma are identified. Careful dissection with limited electrocautery is used to mobilize the vas deferens. Battery-powered thermal cautery units are a useful adjunct, as these devices have a very limited area of collateral tissue damage. To aid with retraction and identification, the vas may be encircled with vessel loops, or fine-stay sutures may be placed in the adventitia. The vascular pedicles of the vas are ligated at the expected level of the anastomosis using a fine suture, such as a 6-0 prolene (Figure 2). In the instances in which a longer distance must be bridged to affect a tension-free anastomosis, the distal vas can be mobilized on its vascular pedicle all the way into the inguinal canal, affording several additional centimeters of length (Figure 3).
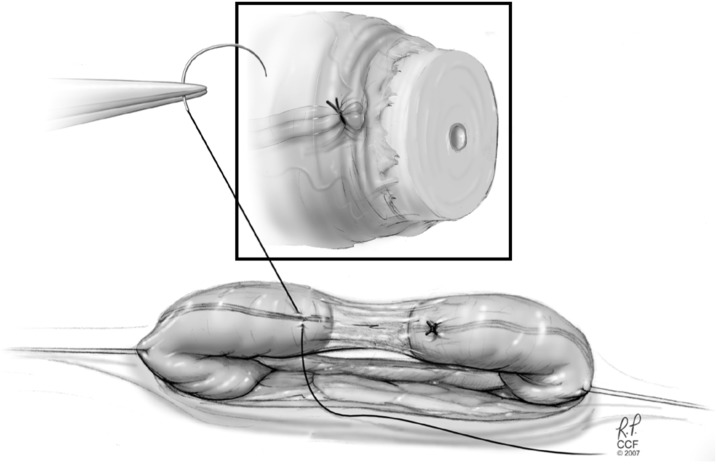
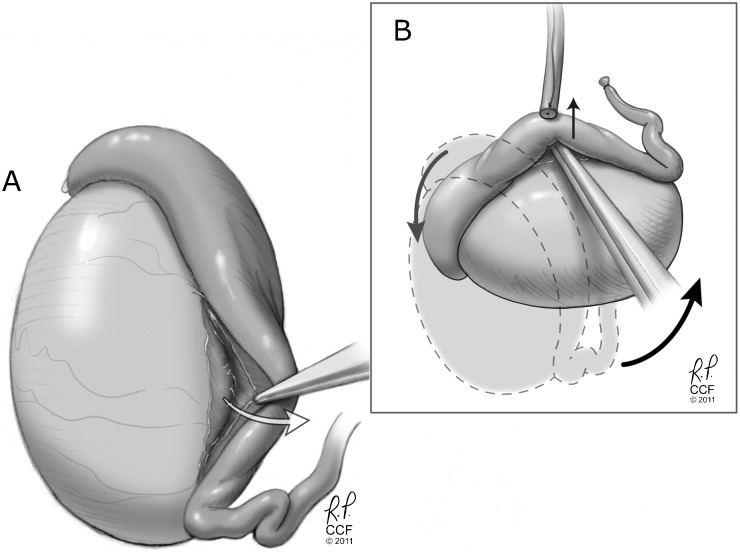
Figure 1.
Initial dissection of the vas. The incision can be minimized by fixing the vasectomy defect below the scrotal skin with a towel clamp or vas deferens clamp.
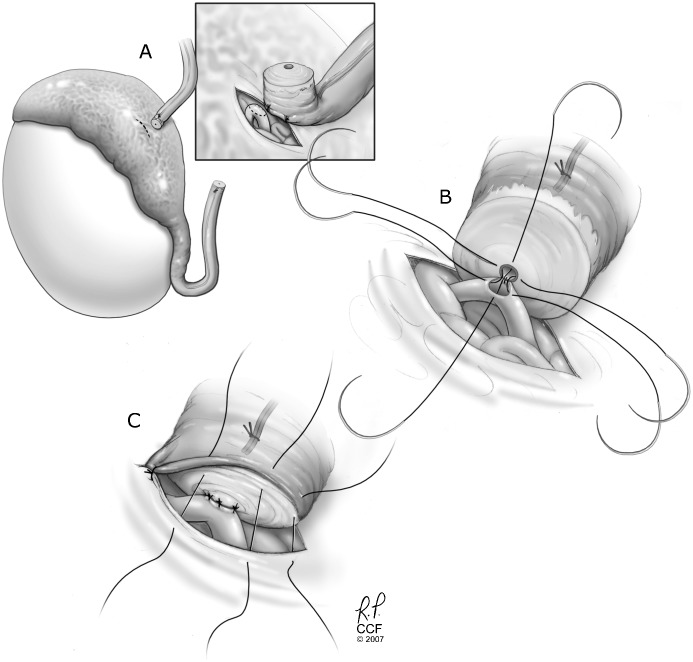
Figure 2.
Vascular control. Once the vas is isolated and mobilized, the vascular pedicle is ligated with 6-0 prolene just below the expected level of the anastomosis (inset). Monopolar electrocautery should be avoided in close proximity to the vas deferens.
Figure 3.
Mobilization of the distal vas. A tension-free anastomosis is essential. Gentle blunt dissection paired with judicious use of thermal cautery can be used to mobilize the distal vas to the external ring. When necessary, the scrotal incision can be extended cranially to aid in the dissection. In extreme cases, the inguinal canal can be opened, and the vas can be mobilized through the level of the internal ring. These maneuvers provide several centimeters of additional length.
Once the vasa are mobilized and vascular pedicles controlled, the operative microscope is brought over the operative field and focused. Patency and pregnancy rates are equivalent between anastomosis to the straight and convoluted portions of the proximal vas; therefore, the surgeon should concentrate on the identifying healthy-appearing vas (60,61). The proximal vas is incised with a small knife, such as a Beaver or supersharp eye blade. The division may be performed free-hand against a surface, such as a tongue blade, or with the aid of a cutting guide. The cut should be clean and perpendicular to the long axis of the vas. Gentle milking of the vas and/or epididymis may yield effluent that is examined for the presence and motility of sperm with a bench-top microscope. A touch prep of the effluent can be prepared by touching a sterile slide to the proximal vas. Alternatively, the effluent can be aspirated through a small angiocatheter attached with a sterile tuberculin syringe preloaded with a small amount of saline. The presence of numerous sperm, in whole or in part, or the presence of copious clear fluid, even in the absence of intravasal sperm, is associated with excellent postoperative patency (39),. When these findings are present, the surgeon should proceed with VV.
A healthy portion of the distal vas is then sharply divided perpendicular to its long axis, and the lumen is assessed. Some favor dilating the lumen with lacrimal duct probes or the tips of microforceps. In instances in which the surgeon is suspicious of obstruction distal to the vasostomy, either a saline vasogram or traditional radiographic vasogram can be performed. Patency can also be directly assessed by flushing the vas with methylene blue-tainted saline while performing simultaneous cystoscopy to visualize the ejaculatory ducts. The level of obstruction can be assessed by cannulating the distal vas with a 0-nylon.
The ends of the vas can be held in proximity with gentle traction on stay stitches or by use of a vasovasostomy clamp. When necessary, tissue adjacent to the vas can be approximated with a stitch to allow for a tension-free vasal anastomosis. A fine-point operative marker can be used to mark the sites of the anastomosis sutures, which is a step that can help ensure even spacing between the sutures during the anastomosis (65).
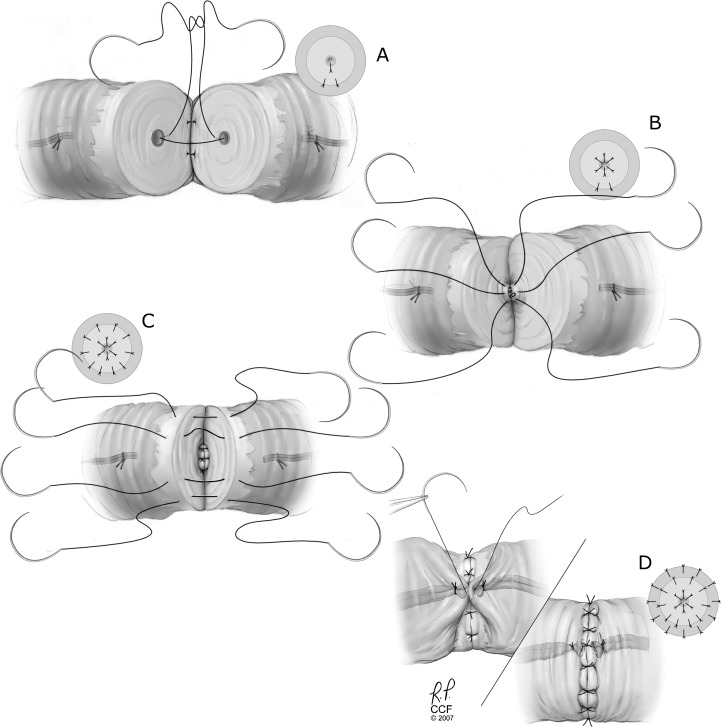
The vasal anastomosis can be performed with a one- or two-layer anastomosis. The formal two-layer and modified two-layer are the techniques most commonly described in the literature, and patency rates between the two techniques are comparable (39,66). The formal two-layer approach allows for direct mucosal-to-mucosal anastomosis. This technique may prove advantageous when there is a marked difference in the diameter of the lumens. The anastomosis begins by opposing the adventitia and muscularis of the vasal ends on the posterior side of the anastomosis with one to two interrupted 9-0 nylon stitches. Once the ends are approximated, interrupted 10-0 sutures are placed in the mucosal layer of the vas beginning on the far side of the anastomosis (Figure 4A). The stitches should be placed so that the knots reside outside the lumen. Shorter double-armed stitches may prove useful. Care is taken to gently approximate the delicate mucosal layers, and the first few stitches can be tied as they are placed. Six to eight luminal stitches are typically required to create a well-spaced anastomosis (Figure 4B). The second layer is completed by placing an additional 4 to 5 interrupted 9-0 nylon stitches through the serosal and muscularis layers of the anterior vas (Figure 4C). If desired, additional stitches can be used to oppose the perivasal tissues (Figure 4D).
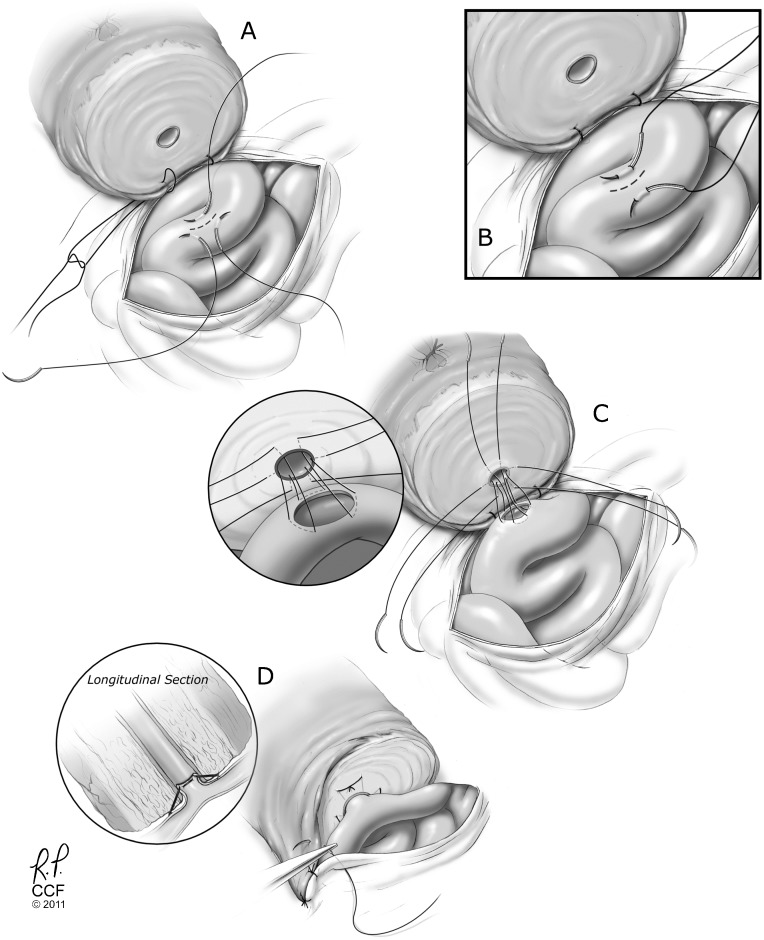
Figure 4.
Two-layer vasovasostomy.
The modified two-layer anastomosis diverges from the formal two-layer technique in the size of the suture and layers incorporated in the luminal stitches. Full-thickness 9-0 interrupted nylon stitches incorporating the serosa, muscularis and mucosa are used to approximate the two vasal ends (Figure 5A). The surgeon may begin the anastomosis on the deep side of the field and move circumferentially. Alternatively, one may begin on the near side of the anastomosis and rotate or “flip” the vas after the first two to three stitches are placed. A microsurgical vas clamp can assist with positioning and rotating the vasal ends. A total of four to six full-thickness stitches are typically required to create a well-spaced anastomosis. The stitches should be placed such that the knots will reside on the serosa. The first few stitches are tied immediately after placement, and the remaining two to three stitches are tied once all remaining stitches have been placed to allow visualization of the lumen and confirmation of good suture placement (Figure 5B). Once the lumens are approximated, a second layer of 9-0 stitches incorporating the adventitia and small amount of muscularis is then placed in between the full-thickness stitches to affect a water-tight anastomosis (Figure 5C).
Figure 5.
Modified two-layer vasovasostomy.
Vasoepididymostomy
The absence of effluent or poor quality effluent containing no recognizable sperm parts is consistent with obstruction of the proximal vas, and a VE should then be considered. Modern techniques for VE center upon identifying and then directly anastomosing a single patent epididymal tubule to the much larger and sturdier lumen of the vas deferens. The patient preparation and initial dissection for the VE are as described for the VV. Careful attention should be paid to patient positioning during VE, as iatrogenic injuries can be avoided through simple measures, such as ensuring correct positioning and padding.
The vertically oriented incision described in the VV technique is extended, and the testis is delivered. The tunica vaginalis is then opened, and the epididymis is inspected. On occasion, a transition point marking the level of epididymal obstruction can be readily identified proximal to where the epididymal tubules will be engorged. The presence of lipofuchsin, a blue-brown discoloration caused by the breakdown of extravasated sperm, may also indicate the level of obstruction, though in some instances, the level of obstruction will not be apparent by inspection alone.
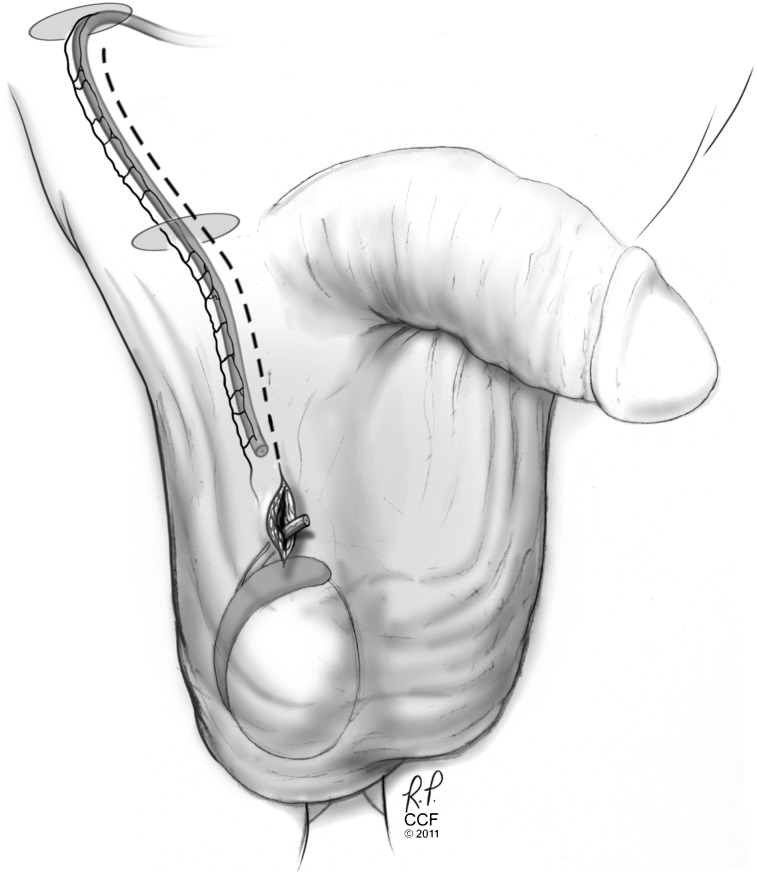
The distal vas may require additional mobilization to ensure a tension-free anastomosis. Additional length can be obtained by mobilizing the vas into the inguinal canal (Figure 3). Frequently, this maneuver can be performed through the scrotal incision, but when necessary, the vertically oriented incision can be extended to the level of the external inguinal ring. Care should be taken to ensure the vascular pedicle remains intact and that hemostasis is ensured. The caudal portion of the epididymis can also be mobilized by dividing the relatively avascular plane of the lateral sulcus at the junction of the epididymis and testis (Figure 6A). This maneuver will allow the tail of the epididymis to swing posteriorly. Additional distance can be bridged by rotating the entire testis and epididymis on its horizontal axis, in essence, inverting the testis and epididymis (Figure 6B). The testis should be inspected to assure adequate perfusion, but when carefully applied, these maneuvers should not jeopardize the blood supply.
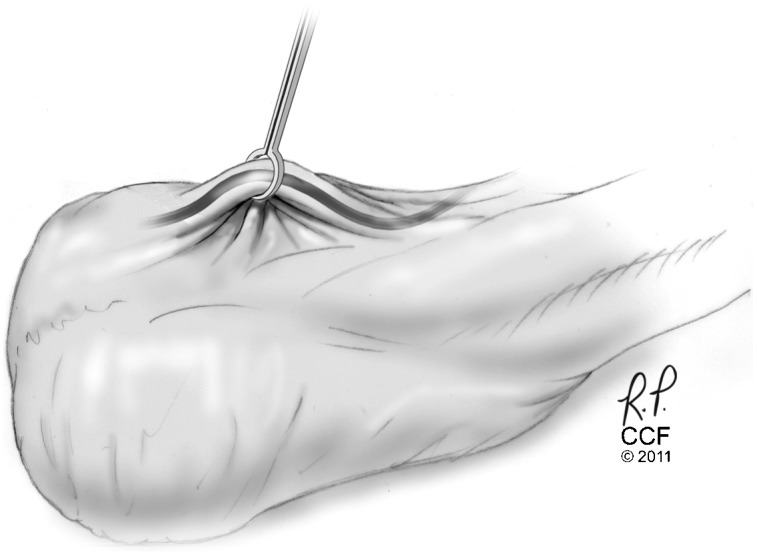
Figure 6.
Mobilization of the epididymis. A) Division of the tunica albuginea through the avascular potions of the lateral epididymal sulcus allows posterior rotation of the epididymal body. B) Additional length can be gained by pivoting the testis and epididymis superiorly and thereby swinging the epididymis into a cranial position. In extreme cases, the testis may be inverted.
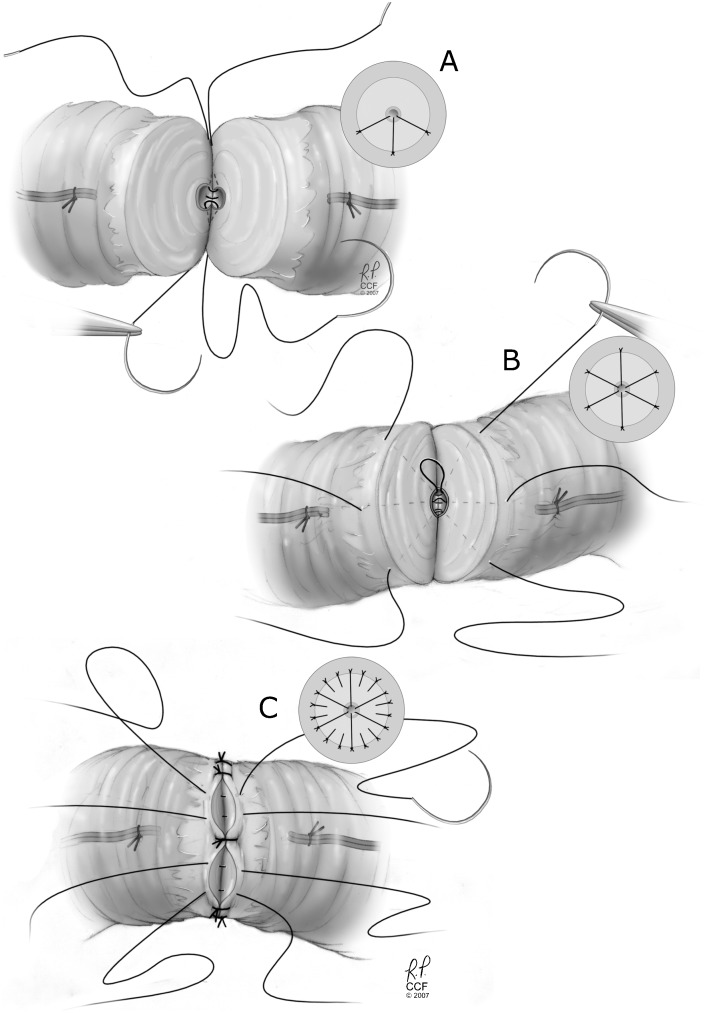
A tension-free anastomosis is critical to the success of a VE. The adventitia of the distal vas should be secured to the tunica albuginea in a location and orientation that allows for minimal angulation of the completed anastomosis. Bringing the distal vas through a separate, small aperture at the posterior-lateral reflection of the tunica vaginalis may provide the best lie for the vas deferens. Outcome studies for VE suggest better patency and pregnancy rates for more distal anastomoses. As such, exploration for a candidate tubule should begin as distally as is feasible. All modern VE techniques are modifications of the end-to-side anastomosis wherein the end of the vas deferens is anastomosed to the side of the epididymal tubule. A 5-mm incision is made through the tunica albuginea overlying the target tubules (Figure 7A). Careful sharp dissection under high magnification (25X) is used to mobilize a candidate tubule. Visualization is aided by gentle irrigation with saline through an angiocatheter. Judicious use of bipolar cautery or handheld low-temperature cautery units can aid with hemostasis. The adventitia of the vas is secured to the tunica albuginea of the epididymis with a 9-0 nylon stitch. The number of sutures and timing for opening the epididymis vary with the different anastomotic techniques. For conventional end-to-side anastomosis, a microknife or microscissors are used to make a ½- to 1-mm aperture in the side of a candidate tubule (Figure 7A). A 10-0 nylon suture is placed through the lip of the tubule to aid in identification of the mucosal edge. Alternately, dilute methylene blue can be painted on the tubule to highlight the mucosal edge. The effluent is then assessed and whole, preferably motile, sperm should be found. An additional two to three 10-0 sutures are evenly spaced around the tubotomy to triangulate or quadrangulate the epididymal opening (Figure 7B). Single-arm or double-armed sutures may be used in accordance with the surgeon's preference, and all knots should lie outside the lumen. The 10-0 sutures are passed through their corresponding sectors in the vasal mucosa, and the sutures are tied while supporting the vas in close proximity to the epididymal tubule. Additional supporting 9-0 nylon sutures are placed circumferentially between the adventitia and tunica albuginea (Figure 7C).
Figure 7.
Conventional end-to-side vasoepididymostomy.
The epididymal tubule can also be drawn into the vasal lumen using an intussusception technique. Precise needle placement may be easier with this technique, as the needles are all placed before the tubule is opened and has decompressed. As with conventional end-to-side anastomosis, a candidate tubule is selected and then widely mobilized so that it can be drawn into the vasal lumen. The adventitia of the vas is secured to the tunica albuginea of the epididymis with an interrupted 9-0 nylon suture. The first needle of a double-armed 10-0 nylon stitch is passed in and out of the wall of the tubule, but the throw is not completed, thus anchoring the body of the needle in the epididymal tubule (Figure 8A). An additional one to two sutures are similarly passed depending on whether the 2-suture or triangulation technique is used (Figures 8A and B). The epididymal tubule is then sharply incised, and the fluid is assessed. The needle throws are then completed by drawing the needle completely through the epididymal wall. Each double-armed needle is then passed inside to out through the mucosa of the vas in its corresponding sector (Figure 8C). The 10-0 sutures are gently pulled to invaginate and then are tied to secure the epididymal aperture inside the lumen of the vas (Figure 8D). Additional 9-0 nylon sutures are placed to secure the vas to the tunica albuginea. The tunica vaginalis, dartos, and skin are closed in accordance with standard practice with careful attention to proper hemostasis.
Figure 8.
Intussusception end-to-side vasoepididymostomy.
OUTCOMES
Microsurgical vasectomy reversal delivers excellent patency and pregnancy outcomes. The Vasovasostomy Study Group reported overall patency of 86% and pregnancy in 52% of patients in their series of 1,469 microsurgical vasectomy reversals (39). Bolduc et al. reviewed 747 microsurgical vasovasostomies and reported overall patency of 86% and a pregnancy rate of 53% (51). Hinz et al. reviewed 212 vasectomy reversals performed by a single surgeon and reported overall patency of 93% and a pregnancy rate of 72% (46). Adherence to good microsurgical techniques with special attention to selecting healthy vas segments, ensuring a tension-free anastomosis, and performing precise mucosal-to-mucosal anastomosis will result in excellent outcomes for couples electing vasectomy reversal.
The results of vasal reconstruction for etiologies other than vasectomy are limited, though the majority of the literature suggests that while surgery may be challenging, postoperative patency is acceptable in the instances wherein reconstruction is technically feasible. Tuberculosis is a notable exception, as the extensive inflammatory reaction is not amenable to surgical reconstruction (see above). VE and/or complex repairs requiring transseptal, inguinal, or pelvic approaches are frequently required for success. Simultaneous sperm retrieval and cryopreservation should be discussed with couples.
Berardinucci and Jarvi reviewed the etiologies, intraoperative findings, and outcomes of 80 men without a history of vasectomy who underwent surgical exploration for obstructive azoospermia. All patients had normal ejaculatory volume or transrectal ultrasound not diagnostic for EDO, at least one palpable vas deferens, and active spermatogenesis, as documented by testicular biopsy. The etiologies for obstruction were idiopathic in 73% (n = 59), infectious in 18% (n = 14), and surgical in 8% (n = 7) of subjects. Twenty-eight patients (35%) had findings that precluded surgical repair, which included 24 patients with either bilateral or unilateral intra-testicular obstruction defined as the absence of sperm in the epididymal fluid. The remaining 52 patients underwent reconstruction consisting of unilateral VE in 22 patients, bilateral VE in 27 patients, and cross VVs in three patients. Overall patency was 62%. The likelihood of reconstruction and subsequent patency were higher for patients with obstruction attributed to an infectious or surgical etiology compared with those with an idiopathic cause (93% and 77%, respectively, for those with infectious causes, 79% and 60%, respectively, for those with surgical causes, and 58% and 55%, respectively, for those with idiopathic causes) (23).
Kim et al. reported 49 patients with no history of vasectomy who underwent bilateral or isolated unilateral VE. Etiologies of obstruction included idiopathic 43% (n = 21), inflammatory 39% (n = 19), unreported 12% (n = 2), congenital 4% (n = 2), and traumatic 2% (n = 1) causes. Overall patency was 81%, and the pregnancy rate was 37%; however, the outcomes were not stratified by etiology. The authors noted that a more proximal anastomosis (caput) favored patency, while a more distal anastomosis favored pregnancy (3). Similarly, Ho et al. reviewed the outcomes of 22 patients with OA not attributable to surgery or vasectomy who underwent VE. Overall patency was 57%, while patency was 60% for post-infectious obstruction and 50% for idiopathic obstruction (25). Shiff et al. reviewed the outcomes of four surgical techniques in 153 men undergoing VE. Of the men with postoperative semen analysis, the etiology for obstruction was vasectomy in 45, infection in 47, iatrogenic injury in eight, and unknown etiology in two of the subjects. Patency was higher in men with iatrogenic etiology for obstruction (75% iatrogenic vs. 44% for vasectomy, 45% for infection, and 0% for unknown), though the difference did not reach statistical significance (24).
Hopps and Goldstein reported eight patients with a history of hydrocelectomy who underwent reconstruction for OA due to injury to the epididymis (n = 6) or scrotal vas (n = 2). The injury was bilateral in four patients, while the remaining four had a unilateral injury that was associated with a contralateral abnormality, such as atrophy, absence of the testis, or obstruction from hernia repair. Sperm was detected in the ejaculate in five of six patients who submitted a semen sample, though only one spontaneous pregnancy was reported, and three of the remaining couples elected to proceed to IVF. (67) These outcomes prompted the authors to recommend couples be counseled about the likelihood of VE and option of sperm retrieval paired with IVF/ICSI in lieu of reconstruction when hydrocelectomy or spermatocelectomy is suspected as the cause for obstructive azoospermia.
OA after herniorrhaphy can represent a difficult challenge. Shyenkin reported overall patency and natural pregnancy rates of 65% and 39%, respectively, in a review of 34 patients who underwent vasal reconstruction after iatrogenic injury to the vas deferens, the majority of which were attributed to prior herniorrhaphy (35). Pasqualotto reported overall patency and pregnancy rates of 65% and 40%, respectively, in 13 men who underwent open microsurgical vasal reconstruction for azoospermia or severe oligospermia attributed to herniorrhaphy (68). Of note, six patients required a second procedure, and half of these men remained azoospermic despite repeat reconstruction, which is an outcome that speaks to the technical difficulty of the anastomosis in this situation. Shaeer and Shaeer reviewed their experience with laparoscopic mobilization of the pelvic vas after unilateral or bilateral post-herniorrhaphy vasal obstruction confirmed by vasography. Once mobilized, the freed end of the vas is tunneled through the conjoint tendon and/or abdominus rectus, and an open microsurgical vasal reconstruction is then performed. The authors reported an overall patency of 68%, with bilateral repairs faring better than unilateral repairs (80% patency vs. 60% patency, respectively) (69).
Sabanegh and Thomas reported equivalent patency but lower mean sperm concentrations in cross transseptal vasoepididymostomies performed in four patients with unilateral vasal agenesis, as opposed to six patients with other etiologies (70). The mean postoperative sperm concentration was 37.8 mil/ml in agenesis patients vs. 136 mil/ml in the remaining patients (p<0.05) (70). In a series of 18 patients requiring repeat vasoepididymostomies; however, patients with congenital etiologies fared slightly better, with postoperative patency of 85.7% compared with patients with inflammatory or post-vasectomy obstruction (patency 43% and 75%, respectively) (54).
Microsurgery reconstruction is a viable option in many causes of obstructive azoospermia and remains the gold standard for vasal reconstruction. Postoperative patency and pregnancy rates are excellent after VV. Vasoepididymostomy or other complex repairs may be required, especially if vasectomy is not the cause of the obstruction or if the surgery is a repeat reconstruction. Reasonable patency and pregnancy rates are reported after complex repairs and repeat reconstructions. CBAVD and obstruction due to tuberculosis should be treated with sperm retrieval.
Footnotes
No potential conflict of interest was reported.
REFERENCES
- 1.Aziz N, Agarwal A, Nallella KP, Thomas AJ., Jr Relationship between epidemiological features and aetiology of male infertility as diagnosed by a comprehensive infertility service provider. Reprod Biomed. 2006;12(2):209–14. doi: 10.1016/s1472-6483(10)60863-2. [DOI] [PubMed] [Google Scholar]
- 2.Jequier AM. Obstructive azoospermia: a study of 102 patients. Clin Reprod Fertil. 1985;3(1):21–36. [PubMed] [Google Scholar]
- 3.Kim ED, Winkel E, Orejuela F, Lipshultz LI. Pathological epididymal obstruction unrelated to vasectomy: results with microsurgical reconstruction. J Urol. 1998;160(6 Pt 1):2078–80. doi: 10.1097/00005392-199812010-00037. [DOI] [PubMed] [Google Scholar]
- 4.Chan PTK, Brandell RA, Goldstein M. Prospective analysis of outcomes after microsurgical intussusception vasoepididymostomy. BJU Int. 2005;96(4):598–601. doi: 10.1111/j.1464-410X.2005.05691.x. [DOI] [PubMed] [Google Scholar]
- 5.Pavlovich CP, Schlegel PN. Fertility options after vasectomy: a cost-effectiveness analysis. Fertil Steril. 1997;67(1):133–41. doi: 10.1016/s0015-0282(97)81870-5. [DOI] [PubMed] [Google Scholar]
- 6.Donovan JF, Jr, DiBaise M, Sparks AE, Kessler J, Sandlow JI. Comparison of microscopic epididymal sperm aspiration and intracytoplasmic sperm injection/in-vitro fertilization with repeat microscopic reconstruction following vasectomy: is second attempt vas reversal worth the effort. Hum Reprod. 1998;13(2):387–93. doi: 10.1093/humrep/13.2.387. [DOI] [PubMed] [Google Scholar]
- 7.Kolettis PN, Thomas AJ., Jr Vasoepididymostomy for vasectomy reversal: a critical assessment in the era of intracytoplasmic sperm injection. J Urol. 1997;158(2):467–70. doi: 10.1016/s0022-5347(01)64504-x. [DOI] [PubMed] [Google Scholar]
- 8.Lee R, Li PS, Goldstein M, Tanrikut C, Schattman G, Schlegel PN. A decision analysis of treatments for obstructive azoospermia. Hum Reprod. 2008;23(9):2043–9. doi: 10.1093/humrep/den200. [DOI] [PubMed] [Google Scholar]
- 9.Clinic Summary Report [Internet] [cited 2011 Sep 15] Available from: https://www.sartcorsonline.com/rptCSR_PublicMultYear.aspx?ClinicPKID = 0. [Google Scholar]
- 10.Yurdakul T, Gokce G, Kilic O, Piskin MM. Transurethral resection of ejaculatory ducts in the treatment of complete ejaculatory duct obstruction. Int Urol Nephrol. 2008;40(2):369–72. doi: 10.1007/s11255-007-9273-z. [DOI] [PubMed] [Google Scholar]
- 11.Xu B, Niu X, Wang Z, Li P, Qin C, Li J, et al. Novel methods for the diagnosis and treatment of ejaculatory duct obstruction. BJU Int. 2011;108(2):263–6. doi: 10.1111/j.1464-410X.2010.09775.x. [DOI] [PubMed] [Google Scholar]
- 12.Wang H, Ye H, Xu C, Liu Z, Gao X, Hou J, et al. Transurethral Seminal Vesiculoscopy Using a 6F Vesiculoscope for Ejaculatory Duct Obstruction. J Androl. 2012;33(4):637–43. doi: 10.2164/jandrol.111.013912. [DOI] [PubMed] [Google Scholar]
- 13.Kuligowska E, Fenlon HM. Transrectal US in male infertility: spectrum of findings and role in patient care. Radiology. 1998;207(1):173–81. doi: 10.1148/radiology.207.1.9530314. [DOI] [PubMed] [Google Scholar]
- 14.Daudin M, Bieth E, Bujan L, Massat G, Pontonnier F, Mieusset R. Congenital bilateral absence of the vas deferens: clinical characteristics, biological parameters, cystic fibrosis transmembrane conductance regulator gene mutations, and implications for genetic counseling. Fertil Steril. 2000;74(6):1164–74. doi: 10.1016/s0015-0282(00)01625-3. [DOI] [PubMed] [Google Scholar]
- 15.Raviv G, Mor Y, Levron J, Shefi S, Zilberman D, Ramon J, et al. Role of transrectal ultrasonography in the evaluation of azoospermic men with low-volume ejaculate. J Ultrasound Med. 2006;25(7):825–9. doi: 10.7863/jum.2006.25.7.825. [DOI] [PubMed] [Google Scholar]
- 16.Anger JT, Goldstein M. Intravasal “toothpaste” in men with obstructive azoospermia is derived from vasal epithelium, not sperm. J Urol. 2004;172(2):634–6. doi: 10.1097/01.ju.0000131486.34917.2f. [DOI] [PubMed] [Google Scholar]
- 17.Arya AK, Beer HL, Benton J, Lewis-Jones I, Swift AC. Does Young's syndrome exist. J Laryngol Otol. 2009;123(5):477–81. doi: 10.1017/S0022215109004307. [DOI] [PubMed] [Google Scholar]
- 18.Hendry WF, A'Hern RP, Cole PJ. Was Young's syndrome caused by exposure to mercury in childhood. BMJ. 1993;307(6919):1579–82. doi: 10.1136/bmj.307.6919.1579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ichioka K, Kohei N, Okubo K, Nishiyama H, Terai A. Obstructive azoospermia associated with chronic sinopulmonary infection and situs inversus totalis. Urology. 2006;68(1):204.e5–7. doi: 10.1016/j.urology.2006.01.072. [DOI] [PubMed] [Google Scholar]
- 20.Shiraishi K, Ono N, Eguchi S, Mohri J, Kamiryo Y, Takihara H. Young's syndrome associated with situs inversus totalis. Arch Androl. 2004;50(3):169–72. doi: 10.1080/01485010490425511. [DOI] [PubMed] [Google Scholar]
- 21.Hirsh A, Williams C, Williamson B. Young's syndrome and cystic fibrosis mutation delta F508. Lancet. 1990;342(8863):118. doi: 10.1016/0140-6736(93)91321-c. [DOI] [PubMed] [Google Scholar]
- 22.Goeminne PC, Dupont LJ. The sinusitis-infertility syndrome: Young's saint, old devil. Eur Respir J. 2010;35(3):698. doi: 10.1183/09031936.00163809. [DOI] [PubMed] [Google Scholar]
- 23.Berardinucci D, Zini A, Jarvi K. Outcome of microsurgical reconstruction in men with suspected epididymal obstruction. J Urol. 1998;159(3):831–4. [PubMed] [Google Scholar]
- 24.Schiff J, Chan P, Li PS, Finkelberg S, Goldstein M. Outcome and late failures compared in 4 techniques of microsurgical vasoepididymostomy in 153 consecutive men. J Urol. 2005;174(2):651–5. doi: 10.1097/01.ju.0000165573.53109.92. [DOI] [PubMed] [Google Scholar]
- 25.Ho KL, Wong MH, Tam PC. Microsurgical vasoepididymostomy for obstructive azoospermia. Hong Kong Med J. 2009;15(6):452–7. [PubMed] [Google Scholar]
- 26.Ahmed A, Bello A, Mbibu NH, Maitama HY, Kalayi GD. Epidemiological and aetiological factors of male infertility in northern Nigeria. Niger J Clin Pract. 2010;13(2):205–9. [PubMed] [Google Scholar]
- 27.Eke AC, Okafor CI, Ezebialu IU. Male infertility management in a Nigerian tertiary hospital. Int J Gynaecol Obstet. 2011;114(1):85–6. doi: 10.1016/j.ijgo.2011.01.023. [DOI] [PubMed] [Google Scholar]
- 28.Philippov OS, Radionchenko AA, Bolotova VP, Voronovskaya NI, Potemkina TV. Estimation of the prevalence and causes of infertility in western Siberia. Bull. World Health Organ. 1998;76(2):183–7. [PMC free article] [PubMed] [Google Scholar]
- 29.Bayasgalan G, Naranbat D, Tsedmaa B, Tsogmaa B, Sukhee D, Amarjargal O, et al. Clinical patterns and major causes of infertility in Mongolia. J Obstet Gynaecol Res. 2004;30(5):386–93. doi: 10.1111/j.1447-0756.2004.00217.x. [DOI] [PubMed] [Google Scholar]
- 30.Vigil P, Morales P, Tapia A, Riquelme R, Salgado AM. Chlamydia trachomatis infection in male partners of infertile couples: incidence and sperm function. Andrologia. 2002;34(3):155–61. doi: 10.1046/j.1439-0272.2002.00472.x. [DOI] [PubMed] [Google Scholar]
- 31.Paick J, Kim SH, Kim SW. Ejaculatory duct obstruction in infertile men. BJU Int. 2000;85(6):720–4. doi: 10.1046/j.1464-410x.2000.00600.x. [DOI] [PubMed] [Google Scholar]
- 32.Shah RS. Obstructive azoospermia following genital tuberculosis may be reversible with medical therapy. 1600 AUA 2004 Abstract. Available from: http://www.abstracts2view.com/aua_archive/view.php?nu = 2004001503. [Google Scholar]
- 33.Ridgway PF, Shah J, Darzi AW. Male genital tract injuries after contemporary inguinal hernia repair. BJU Int. 2002;90(3):272–6. doi: 10.1046/j.1464-410x.2002.02844.x. [DOI] [PubMed] [Google Scholar]
- 34.Steigman CK, Sotelo-Avila C, Weber TR. The incidence of spermatic cord structures in inguinal hernia sacs from male children. Am J Surg Pathol. 1999;23(8):880–5. doi: 10.1097/00000478-199908000-00004. [DOI] [PubMed] [Google Scholar]
- 35.Sheynkin YR, Hendin BN, Schlegel PN, Goldstein M. Microsurgical repair of iatrogenic injury to the vas deferens. J Urol. 1998;159(1):139–41. doi: 10.1016/s0022-5347(01)64036-9. [DOI] [PubMed] [Google Scholar]
- 36.Junge K, Binnebösel M, Rosch R, Ottinger A, Stumpf M, Mühlenbruch G, et al. Influence of mesh materials on the integrity of the vas deferens following Lichtenstein hernioplasty: an experimental model. Hernia. 2008;12(6):621–6. doi: 10.1007/s10029-008-0400-2. [DOI] [PubMed] [Google Scholar]
- 37.Shin D, Lipshultz LI, Goldstein M, Barmé GA, Fuchs EF, Nagler HM, et al. Herniorrhaphy with polypropylene mesh causing inguinal vasal obstruction: a preventable cause of obstructive azoospermia. Ann Surg. 2005;241(4):553–8. doi: 10.1097/01.sla.0000157318.13975.2a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Baker K, Sabanegh ES., Jr Sandlow J I, The Role of Microsurgical Reconstruction in the Era of ICSI Microsurgery for Fertility Specialists: A Practical Text 2013New York: Springer Science+Business Media; p.153–66. [Google Scholar]
- 39.Belker AM, Thomas AJ, Fuchs EF, Konnak JW, Sharlip ID. Results of 1,469 microsurgical vasectomy reversals by the Vasovasostomy Study Group. J Urol. 1991;145(3):505–11. doi: 10.1016/s0022-5347(17)38381-7. [DOI] [PubMed] [Google Scholar]
- 40.Boorjian S, Lipkin M, Goldstein M. The impact of obstructive interval and sperm granuloma on outcome of vasectomy reversal. J Urol. 2004;171(1):304–6. doi: 10.1097/01.ju.0000098652.35575.85. [DOI] [PubMed] [Google Scholar]
- 41.Magheli A, Rais-Bahrami S, Kempkensteffen C, Weiske WH, Miller K, Hinz S. Impact of obstructive interval and sperm granuloma on patency and pregnancy after vasectomy reversal. Int J Androl. 2010;33(5):730–5. doi: 10.1111/j.1365-2605.2009.01007.x. [DOI] [PubMed] [Google Scholar]
- 42.Kolettis PN, Sabanegh ES, D'amico AM, Box L, Sebesta M, Burns JR. Outcomes for vasectomy reversal performed after obstructive intervals of at least 10 years. Urology. 2002;60(5):885–8. doi: 10.1016/s0090-4295(02)01888-5. [DOI] [PubMed] [Google Scholar]
- 43.Paick J-S, Park JY, Park DW, Park K, Son H, Kim SW. Microsurgical vasovasostomy after failed vasovasostomy. J Urol. 2003;169(3):1052–5. doi: 10.1097/01.ju.0000052666.97595.f6. [DOI] [PubMed] [Google Scholar]
- 44.Gerrard ER, Sandlow JI, Oster RA, Burns JR, Box LC, Kolettis PN. Effect of female partner age on pregnancy rates after vasectomy reversal. Fertil Steril. 2007;87(6):1340–4. doi: 10.1016/j.fertnstert.2006.11.038. [DOI] [PubMed] [Google Scholar]
- 45.Kolettis PN, Sabanegh ES, Nalesnik JG, D'Amico AM, Box LC, Burns JR. Pregnancy outcomes after vasectomy reversal for female partners 35 years old or older. J Urol. 2003;169(6):2250–2. doi: 10.1097/01.ju.0000063780.74931.d6. [DOI] [PubMed] [Google Scholar]
- 46.Hinz S, Rais-Bahrami S, Kempkensteffen C, Weiske WH, Schrader M, Magheli A. Fertility rates following vasectomy reversal: importance of age of the female partner. Urol Int. 2008;81(4):416–20. doi: 10.1159/000167839. [DOI] [PubMed] [Google Scholar]
- 47.Parekattil SJ, Kuang W, Agarwal A, Thomas AJ. Model to predict if a vasoepididymostomy will be required for vasectomy reversal. J Urol. 2005;173(5):1681–4. doi: 10.1097/01.ju.0000154608.08496.f2. [DOI] [PubMed] [Google Scholar]
- 48.Chan PTK, Goldstein M. Superior outcomes of microsurgical vasectomy reversal in men with the same female partners. Fertil Steril. 2004;81(5):1371–4. doi: 10.1016/j.fertnstert.2003.09.066. [DOI] [PubMed] [Google Scholar]
- 49.Hernandez J, Sabanegh ES. Repeat vasectomy reversal after initial failure: overall results and predictors for success. J Urol. 1999;161(4):1153–6. doi: 10.1016/s0022-5347(01)61616-1. [DOI] [PubMed] [Google Scholar]
- 50.Kim SW, Ku JH, Park K, Son H, Paick J-S. A different female partner does not affect the success of second vasectomy reversal. J Androl. 2005;26(1):48–52. [PubMed] [Google Scholar]
- 51.Bolduc S, Fischer MA, Deceuninck G, Thabet M. Factors predicting overall success: a review of 747 microsurgical vasovasostomies. Can Urol Assoc J. 2007;1(4):388–94. doi: 10.5489/cuaj.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hinz S, Rais-Bahrami S, Weiske WH, Kempkensteffen C, Schrader M, Miller K, et al. Prognostic value of intraoperative parameters observed during vasectomy reversal for predicting postoperative vas patency and fertility. World J Urol. 2009;27(6):781–85. doi: 10.1007/s00345-009-0397-x. [DOI] [PubMed] [Google Scholar]
- 53.Hollingsworth MR, Sandlow JI, Schrepferman CG, Brannigan RE, Kolettis PN. Repeat vasectomy reversal yields high success rates. Fertil Steril. 2007;88(1):217–9. doi: 10.1016/j.fertnstert.2006.11.077. [DOI] [PubMed] [Google Scholar]
- 54.Pasqualotto FF, Agarwal A, Srivastava M, Nelson DR, Thomas AJ. Fertility outcome after repeat vasoepididymostomy. J Urol. 1999;162(5):1626–8. [PubMed] [Google Scholar]
- 55.Jee SH, Hong YK. One-layer vasovasostomy: microsurgical versus loupe-assisted. Fertil Steril. 2010;94(6):2308–11. doi: 10.1016/j.fertnstert.2009.12.013. [DOI] [PubMed] [Google Scholar]
- 56.Dewire DM, Lawson RK. Experience with macroscopic vasectomy reversal at the Medical College of Wisconsin. Wis Med J. 1994;93(3):107–9. [PubMed] [Google Scholar]
- 57.Lee L, McLoughlin MG. Vasovasostomy: a comparison of macroscopic and microscopic techniques at one institution. Fertil Steril. 1980;33(1):54–5. doi: 10.1016/s0015-0282(16)44478-x. [DOI] [PubMed] [Google Scholar]
- 58.Parekattil SJ, Atalah HN, Cohen MS. Video technique for human robot-assisted microsurgical vasovasostomy. J Endourol. 2010;24(4):511–4. doi: 10.1089/end.2009.0235. [DOI] [PubMed] [Google Scholar]
- 59.Parekattil SJ, Cohen MS. Robotic microsurgery 2011: male infertility, chronic testicular pain, postvasectomy pain, sports hernia pain and phantom pain. Curr Opin Urol. 2011;21(2):121–6. doi: 10.1097/MOU.0b013e3283435ac4. [DOI] [PubMed] [Google Scholar]
- 60.Sandlow JI, Kolettis PN. Vasovasostomy in the convoluted vas deferens: indications and outcomes. J Urol. 2005;173(2):540–2. doi: 10.1097/01.ju.0000149981.89230.50. [DOI] [PubMed] [Google Scholar]
- 61.Patel SR, Sigman M. Comparison of outcomes of vasovasostomy performed in the convoluted and straight vas deferens. J Urol. 2008;179(1):256–9. doi: 10.1016/j.juro.2007.08.169. [DOI] [PubMed] [Google Scholar]
- 62.Kolettis PN, Burns JR, Nangia AK, Sandlow JI. Outcomes for vasovasostomy performed when only sperm parts are present in the vasal fluid. J Androl. 2006;27(4):565–7. doi: 10.2164/jandrol.05190. [DOI] [PubMed] [Google Scholar]
- 63.Kolettis PN, D'Amico AM, Box L, Burns JR. Outcomes for vasovasostomy with bilateral intravasal azoospermia. J Androl. 2003;24(1):22–4. [PubMed] [Google Scholar]
- 64.Sigman M. The relationship between intravasal sperm quality and patency rates after vasovasostomy. J Urol. 2004;171(1):307–9. doi: 10.1097/01.ju.0000102322.90257.8b. [DOI] [PubMed] [Google Scholar]
- 65.Goldstein M, Li PS, Matthews GJ. Microsurgical vasovasostomy: the microdot technique of precision suture placement. J Urol. 1998;159(1):188–90. doi: 10.1016/s0022-5347(01)64053-9. [DOI] [PubMed] [Google Scholar]
- 66.Fischer MA, Grantmyre JE. Comparison of modified one- and two-layer microsurgical vasovasostomy. BJU Int. 2000;85(9):1085–8. doi: 10.1046/j.1464-410x.2000.00668.x. [DOI] [PubMed] [Google Scholar]
- 67.Hopps CV, Goldstein M. Microsurgical reconstruction of iatrogenic injuries to the epididymis from hydrocelectomy. J Urol. 2006;176(5):2077–9. discussion 2080. doi: 10.1016/j.juro.2006.07.042. [DOI] [PubMed] [Google Scholar]
- 68.Pasqualotto FF, Pasqualotto EB, Agarwal A, Thomas AJ., Jr Results of microsurgical anastomosis in men with seminal tract obstruction due to inguinal herniorrhaphy. Rev Hosp Clin Fac Med Sao Paulo. 2003;58(6):305–9. doi: 10.1590/s0041-87812003000600003. [DOI] [PubMed] [Google Scholar]
- 69.Shaeer OKZ, Shaeer KZ. Pelviscrotal vasovasostomy: refining and troubleshooting. J Urol. 2005;174(5):1935–7. doi: 10.1097/01.ju.0000176738.55343.75. [DOI] [PubMed] [Google Scholar]
- 70.Sabanegh E, Jr, Thomas AJ., Jr Effectiveness of crossover transseptal vasoepididymostomy in treating complex obstructive azoospermia. Fertil Steril. 1995;63(2):392–5. doi: 10.1016/s0015-0282(16)57374-9. [DOI] [PubMed] [Google Scholar]