Abstract
Background
Cirrhosis of the liver is the end stage of chronic liver disease. Among the many liver disorders that can lead to cirrhosis, some progress rapidly (years) and others more slowly (decades). In Germany, cirrhosis is often a consequence of fatty liver disease due to alcoholism or other causes, but can also be caused by hepatitis B and hepatitis C. Cirrhosis is more common in overweight persons and smokers. The underlying causes of cirrhosis determine its rate of progression and are the focus of preventive efforts and treatment. The prevalence of cirrhosis in Germany is rising; it now ranks among the top 20 causes of death in the country.
Methods
This article is based on a selective review of pertinent literature, including reviews and current guidelines.
Results
Strictly speaking, cirrhosis is a pathological diagnosis; it is, nevertheless, usually diagnosed clinically, by history, physical examination (e.g., cutaneous signs of liver disease), ancillary testing (e.g., ultrasonography, transient elastography) and laboratory analyses (e,g., APRI, which is the quotient of the GOT concentration and the platelet count). There are no laboratory cutoff values for the diagnosis of cirrhosis. Early detection of chronic liver disease, followed by individually tailored, risk-adapted treatment, is the best way to prevent it. Esophagogastroduodenoscopy can be performed early on to assess the risk of variceal bleeding. In most patients, the progression of fibrosis can be averted by early detection and appropriate treatment.
Conclusion
Screening for chronic liver disease should include history and physical examination, serum transaminase measurement, upper abdominal ultrasonography, and, in some cases, transient elastography.
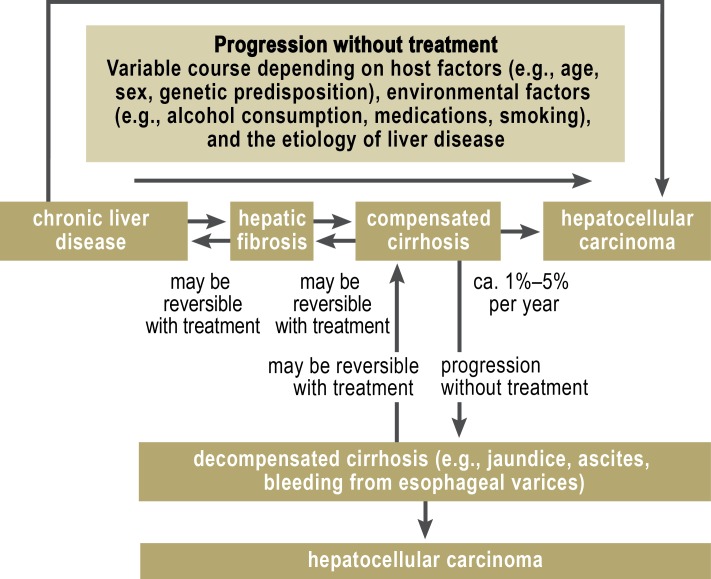
Cirrhosis is the final stage attained by various chronic liver diseases after years or decades of slow progression. There are, however, ways to prevent cirrhosis, because the diseases that most commonly lead to it progress slowly, and measures are available to prevent and treat them. Moreover, most cases of hepatocellular carcinoma (HCC) arise in a cirrhotic liver, so cirrhosis prevention is, in fact, also HCC prevention (Figure 1). The risk of developing HCC depends on the underlying disease: It is low, for example, when the underlying disease is autoimmune hepatitis (2.9% in 10 years) (1), and high when the underlying disease is chronic hepatitis B with a viral burden greater than 107copies/mL (19.8% in 13 years) (2). Aside from chronic viral hepatitis, fatty liver disease due to any of the very common underlying disorders (obesity, diabetes, alcohol abuse) commonly progresses to cirrhosis and thus merits both specialized medical treatment and close follow-up by the primary-care physician.
Figure 1.
The course of chronic liver disease:
Worsening hepatic fibrosis leads to cirrhosis, which can become decompensated and lead, in turn, to hepatocellular carcinoma. Timely intervention can prevent progression to the next disease stage. In particular, it can prevent hepatocellular carcinoma. Appropriate treatment can bring about the regression of disease from a worse stage to a better one. Even cirrhosis can regress, but hepatocellular carcinoma cannot.
This article, based on a selective review of the literature, deals with approaches to cirrhosis prevention that involve the proper diagnostic work-up for early detection of chronic liver disease, followed by risk-adapted treatment.
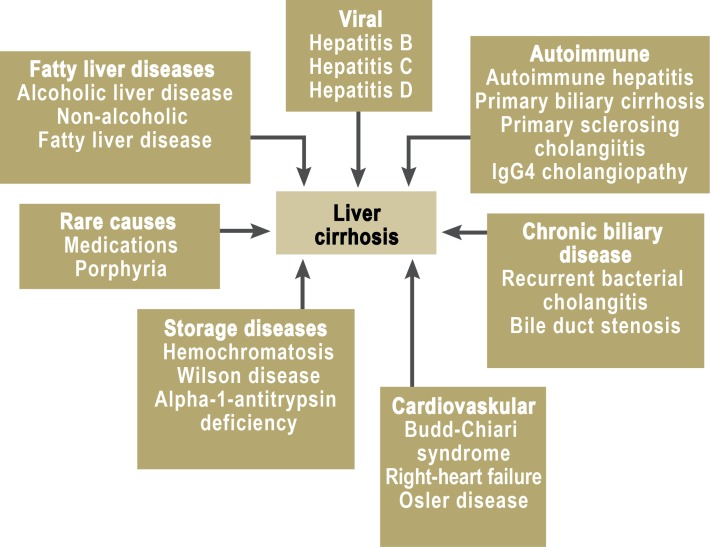
The etiology of cirrhosis
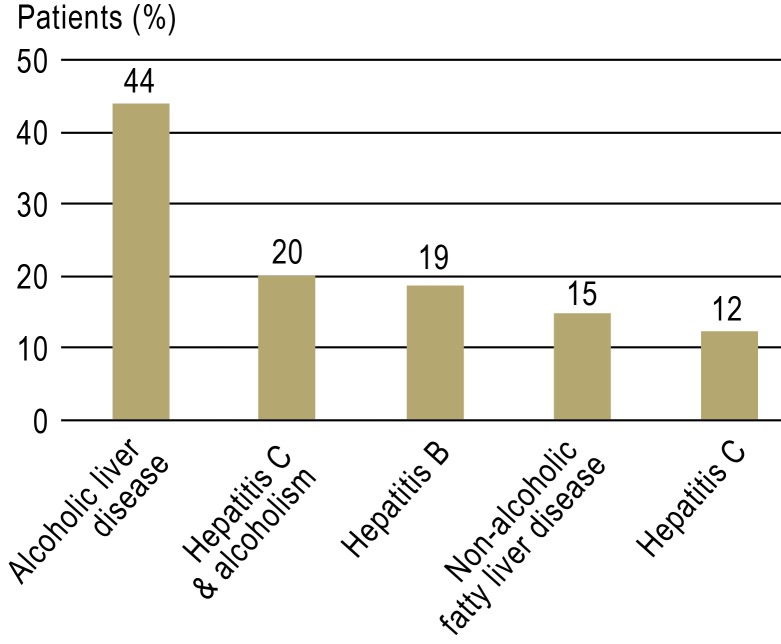
Cirrhosis can arise in consequence of an exogenous/toxic, infectious, toxic/allergic, immunopathological/autoimmune, or vascular process or an inborn error of metabolism (Figure 2). The commonest causes of cirrhosis in Germany are alcoholic and non-alcoholic fatty liver disease and viral hepatitis (B or C). Among these causes, the most common of all is alcoholic fatty liver disease, which caused 8619 deaths in Germany (8.9 deaths per 100 000 population) in 2009 and thus ranks among the country’s top 20 causes of death (3). Cirrhosis is rising in importance as a public health problem: the number of deaths from cirrhosis per 100 000 population doubled from 5 in 1980 to 9.9 in 2005 (3).
Figure 2.
Causes of liver cirrhosis
Autopsy studies have revealed fatty liver disease in 70% of overweight persons and in 35% of persons of normal weight. They have also revealed cirrhosis in 18.5% of overweight diabetics (4).
0.5% of the German population are chronically infected with the hepatitis B virus, and 0.5% with the hepatitis C virus (5). Cirrhosis and HCC due to chronic hepatitis C are among the main indications for liver transplantation in Western industrialized countries. From 1988 to 2010, viral hepatitis was the underlying cause of liver disease in 39% of liver transplant recipients—hepatitis B in one-third of cases, and hepatitis C in two-thirds (e1).
The diagnosis of liver cirrhosis
Cirrhosis is histologically characterized by fibrous septa between the portal fields; it comes in micro- and macronodular forms (6, 7). The condition is diagnosed by its characteristic findings on clinical examination, laboratory tests, and ancillary studies.
The typical findings in cirrhosis include
cutaneous signs of liver disease,
a firm liver on palpation, and
-
certain risk constellations such as:
The early signs of cirrhosis in B-ultrasonography include inhomogeneity of the hepatic tissue, irregularity of the hepatic surface, or enlargement of the caudate lobe. Portal hypertension leads to splenomegaly.
In advanced liver disease approaching the stage of cirrhosis, thrombocytopenia is seen, along with impaired hepatic biosynthesis (as shown by, e.g., low concentration of albumin and cholinesterase and an elevation of the international normalized ratio [INR]) and impairment of the detoxifying function of the liver (as shown by, e.g., elevated bilirubin concentration). The transaminase concentrations are generally in the normal range or only mildly elevated (6, 7). There is no well-defined threshold value of any laboratory test that can be used to determine when screening for cirrhosis should be performed.
Ancillary studies include upper abdominal ultrasonography and gastroscopy. Esophagogastroduodenoscopy (EGD) can be used to demonstrate esophageal varices, and to assess the risk that they will bleed; it should be performed whenever cirrhosis is initially diagnosed or suspected (6, 7).
Liver biopsy is unnecessary, or even contraindicated, if the diagnosis of cirrhosis has been clearly established from the clinical findings and imaging studies (e.g., evidence of decompensation, with ascites and impaired hepatic biosynthesis).
Liver biopsy is indicated if the etiology of liver disease is unclear, or if its stage cannot be determined from the findings of the tests mentioned above. In cases of suspected cirrhosis, transcutaneous liver biopsy is indicated if the clinical findings leave the diagnosis in doubt or if the biopsy is expected to yield information about the cause of cirrhosis that will affect the choice of treatment (8). To enable the reliable staging of hepatic fibrosis, the punch cylinders used for liver biopsy should be at least 15 mm long, and at least 10 portal fields should be examined per sectional level (9).
It should be borne in mind that, once hepatic disease has reached the stage of cirrhosis, histological determination of the original underlying etiology may be difficult or impossible.
Noninvasive diagnostic evaluation of cirrhosis
A number of laboratory and ultrasound-based methods have been developed recently for the noninvasive diagnostic evaluation of cirrhosis. These noninvasive methods often obviate the need for liver biopsy when the only question to be answered is the stage of fibrosis; nonetheless, the information they provide must always be considered in the light of the accompanying clinical findings (10).
Laboratory-based methods for estimating the extent of hepatic fibrosis can be divided into those based on routine liver function tests (11– 15, e2) and those based on particular laboratory values that are associated with fibrosis, such as the hyaluronic acid concentration (16). The AST-to-platelet ratio index (APRI) is easily calculated as the quotient of the AST (GOT) and the platelet count and serves as a screening index for advanced fibrosis and cirrhosis (17).
The diagnostic evaluation of cirrhosis with ultrasonography is based on the direct relation between the extent of fibrosis and the ultrasonographically determined degree of liver stiffness. Transient elastography and the acoustic radiation force impulse (ARFI) technique are now well-established methods for the staging of fibrosis in various liver diseases (Figures 3, e1, e2) (18, 19). These two techniques can be performed repeatedly on an outpatient basis, and they can also be combined (10).
Figure 3.
Macroscopic pathology of liver cirrhosis
Techniques for the measurement of liver stiffness and laboratory indices of hepatic fibrosis enable longitudinal assessment of the progression and regression of fibrosis in patients with chronic liver disease. Although ultrasonography can rule cirrhosis in or out in over 90% of cases (18, 19), its findings are less than 100% specific because of occasional incorrect measurements and false-positive findings (Table). There may be difficulty in interpreting values that do not cross the necessary thresholds for ruling advanced fibrosis, or cirrhosis, in or out; in such situations, the temporal course of the variable in question is its clinically relevant feature. It should also be borne in mind that the diagnostic threshold values vary depending on the underlying etiology of liver disease (20).
Table. Diagnostic algorithm for chronic liver disease.
| Screening measures | Step 1:General laboratory testing | Step 2:Specific laboratory testing | Step 3:Molecular and invasive studies |
| History (identification of risk constellations) | ALT, AST, GGT, AP, bilirubin | Hepatitis serology(HBsAg, anti-HCV) | Ceruloplasmin, copper in 24-hour urine sample, genetic testing for Wilson disease |
| Physical examination | Complete blood count, platelet count, routine coagulation studies | Autoantibody testing(ANA, SMA, LKM, SLA, p-ANCA, AMA) | HFE mutation |
| Serum ALT and GGT | Total protein, albumin, serum electrophoresis | Quantitative immunoglobulins(IgA, IgG, IgM) | A1-antitrypsin genotype (PIZZ) |
| Ultrasonography | Cholesterol, triglycerides, glucose | Ferritin, transferrin saturation, iron | Liver biopsy, MRCP, ERC (for suspected PSC) |
ALT, alanine aminotransferase; AST, aspartate aminotransferase; GGT, gamma-glutamyl transferase; AP, alkaline phosphatase; HBsAg, hepatitis B surface antigen; anti-HCV, anti-hepatitis-C antibodies; ANA, antinuclear antibodies; SMA, smooth-muscle antibodies; LKM, liver/kidney microsome antibodies; SLA, antibodies against soluble liver antigen; p-ANCA, perinuclear anti-neutrophil cytoplasmic antibodies; AMA, anti-mitochondrial antibodies; HFE, the “high-iron” gene responsible for hereditary hemochromatosis; MRCP, magnetic resonance cholangiopancreatography; ERC, endoscopic retrograde cholangiography; PSC, primary sclerosing cholangiitis
Individual risk stratification for the development of cirrhosis
The course by which cirrhosis develops from a chronic liver disease is not linear; rather, it is modulated by the influence of various disease-specific, host-specific, and environmental factors. Knowledge of these factors enables individual risk stratification, which, in turn, serves as the basis for personalized treatment.
In non-alcoholic fatty liver disease, the risk of progression of fibrosis can be estimated from the findings of an initial biopsy. If marked inflammatory changes are found, the predicted time to the development of advanced fibrosis is only 4.2 years; in the absence of inflammatory changes, the predicted time to the development of cirrhosis is more than 13 years. 15% to 20% of persons with non-alcoholic fatty liver disease develop significant fibrosis within a decade (21). If the patient declines a liver biopsy, the presence of cirrhosis can be assessed by ultrasonography instead.
Genetic modulation of the progression of chronic liver disease is illustrated by the role of the patatin-like phospholipase-domain-containing gene 3 (PNPLA-3, adiponutrin) in nutritional-toxic liver disease, i.e., alcoholic and non-alcoholic fatty liver disease. Polymorphisms in this gene are associated both with susceptibility to fatty liver diseases and with the risk of progression, including progression to HCC (22, 23).
In chronic hepatitis C, progression to cirrhosis depends mainly on the patient’s age and level of alcohol consumption. In the absence of appropriate treatment, chronic hepatitis C progresses slowly in young patients, but the risk of advanced fibrosis and cirrhosis rises rapidly from age 40 onward. If the patient also drinks alcohol to excess, the risk of progression is multiplied by a further factor. Thus, patients with chronic hepatitis C should receive timely treatment to prevent progression to cirrhosis (24). In chronic hepatitis B, the risk of cirrhosis depends to a large extent on the burden of viral infection (i.e., the amount of HBV-DNA in the serum): the disease is most likely to progress when the viral burden exceeds 2000 IU/mL. According to current guidelines, this variable plays a major role in the decision whether to initiate antiviral treatment (25, 26).
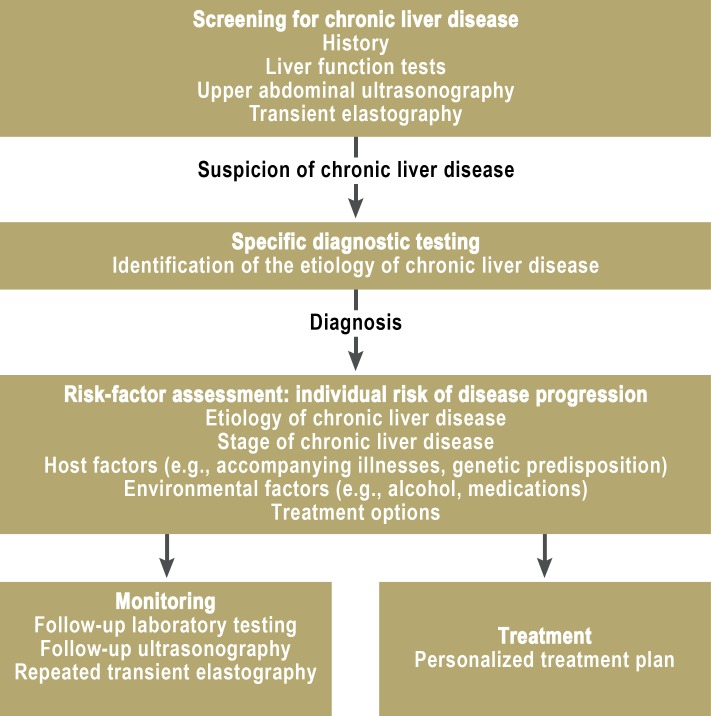
Preventing cirrhosis by early diagnosis of chronic liver disease
Cirrhosis is the end stage of chronic liver diseases that progress over years or decades. It can thus be prevented by appropriate screening for chronic liver diseases so that they can be treated in time (Figure 4).
Figure 4.
Prevention of liver cirrhosis
Chronic liver diseases do not usually cause any symptoms. Measuring the serum concentrations of alanine aminotransferase (ALT—an indicator of hepatic inflammation) and gamma-glutamyl transferase (GGT—an indicator of cholestasis and impaired hepatic metabolism) is indicated as a screening measure for patients initially presenting to a primary-care physician, even if asymptomatic. The physician should also inquire into all the main risk factors for chronic liver disease, including the components of metabolic syndrome as precipitants of non-alcoholic fatty liver disease, the use of harmful substances (e.g., alcohol), the prolonged ingestion of hepatotoxic medications, and risk factors for parenterally transmitted viral hepatitis. Patients who engage in behavior that puts them at risk for chronic liver disease are often not aware of the fact, and subtle clinical manifestations are easily overlooked by physicians as well. As a result, 44% of patients initially presenting to a specialized gastroenterological clinic already have liver cirrhosis (e3).
10% to 25% of adults in Germany have an elevated serum ALT concentration. High transaminase levels are usually a sign of clinically relevant liver disease (27) and are associated with significantly increased mortality from liver disease (hazard ratio 8.2, 95% confidence interval 2.1–31.9) (28). A serum GGT concentration above 67 IU/L is an early indicator of an elevated risk of occupational disability (29).
Whenever possible, patients should not only have their transaminases measured, but should also undergo upper abdominal ultrasonography. A study from the German state of Mecklenburg–West Pomerania showed that an elevation of the GGT concentration in men was associated with an increase in mortality by a factor of 1.49; if ultrasonography revealed a fatty liver as well, mortality was increased by a factor of 1.98 (30).
If the screening tests point to liver disease, a further diagnostic algorithm may be applied to determine the specific type of disease that is present (Table).
Wherever special ultrasonographic techniques such as transient elastography are available, they can be used as additional tests to screen for liver disease and monitor its course. Liver stiffness greater than 8 kPa implies that chronic liver disease is present, even if the patient feels well and has normal liver function tests (31).
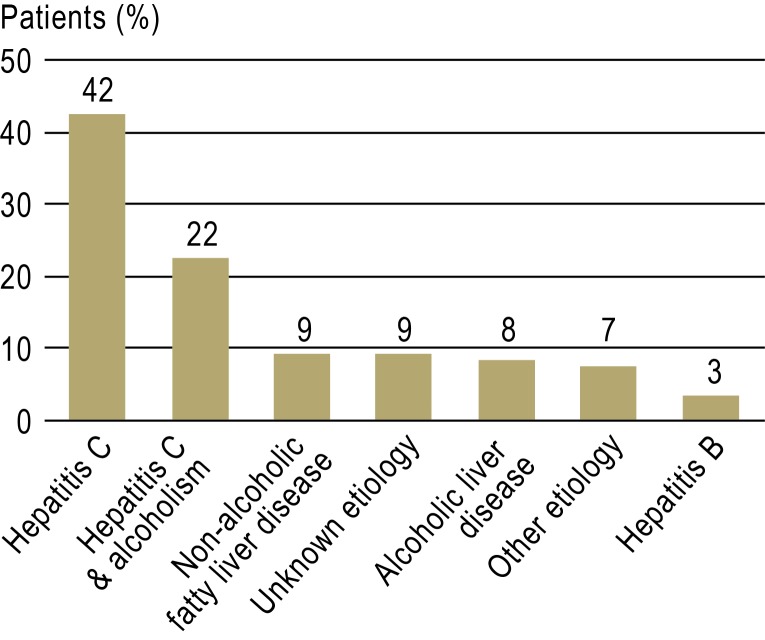
Pathological findings in transaminase screening or ultrasonography imply that an etiological diagnostic algorithm should be applied (7) and that the patient should be referred to a gastroenterologist or hepatologist if indicated. A study from the USA revealed that only 21% of patients for whom liver transplantation might have been an option were actually referred to a center where they could be evaluated for it, and only 8% of such patients were treated by specialists in addition to their family physician (e4). Meanwhile, it has been found that gastroenterologists in private practice treat mainly patients with newly diagnosed hepatitis C, while highly prevalent conditions such as non-alcoholic or alcoholic fatty liver disease account for only 8% to 9% of their caseload (Figure 5). The latter conditions actually confer a much higher risk of cirrhosis than hepatitis C does (Figure 6) (32). Among patients with cirrhosis who develop hepatocellular carcinoma, 29% were not treated by a gastroenterologist, hepatologist, or oncologist before the carcinoma was diagnosed, and 21% are not treated by a specialist of any of these types afterward, either (e5).
Figure 5.
Relative frequency of newly diagnosed liver diseases in gastroenterological private practice in the USA (32)
Figure 6.
Relative frequency of liver cirrhosis by underlying newly diagnosed liver disease in gastroenterological private practice in the USA (32)
Preventing cirrhosis by treating chronic liver disease
It is advisable for a specialist (gastroenterologist or hepatologist) to be involved in the care of the patient at an early stage and to assist in the development of an appropriate treatment plan, because
chronic liver diseases progress slowly, and
their timely diagnosis and treatment can prevent both cirrhosis and hepatocellular carcinoma.
Treatment of the underlying disease can often halt or even reverse the progression of early-stage cirrhosis. Some examples of beneficial treatment approaches are:
antiviral therapy in cirrhosis due to hepatitis B or C (24, 25, 33);
immune suppression in autoimmune hepatitis (1);
treatment of iron overload in hemochromatosis and copper overload in Wilson disease (34, 35);
abstinence from alcohol in alcoholic cirrhosis (36).
Clearly, the etiology of cirrhosis in any particular case is highly relevant to the prognosis. Thus, appropriate screening should be performed (37). Mathematical models reveal that screening followed by treatment with highly potent HBV polymerase inhibitors (entecavir or tenofovir) is cost-effective, even in countries with a low prevalence of hepatitis B (0.3%-0.4%, as in Germany) (38). These medications can not only halt the progression of hepatitis B, but actually reverse it in 74% of cases; they can reconvert clinically decompensated to compensated cirrhosis (e6). Thus, cirrhosis need no longer be regarded as the irreversible end stage of chronic liver disease, but rather as one stage in a dynamic process whose further course (progression or reversion of fibrosis) depends on the provision of appropriate treatment and the avoidance of further harmful influences. Alongside abstinence from alcohol, all persons with chronic liver disease should abstain from smoking, which can also promote the progression of fibrosis (39). On the other hand, the consumption of two or more cups of coffee daily is associated with slower progression of fibrosis (40).
Conclusion
Screening for chronic liver disease can be performed inexpensively and easily with clinical history-taking, measurement of transaminase concentrations, upper abdominal ultrasonography, and transient elastography (where available). Abnormal findings should prompt specific diagnostic testing to determine the etiology of the underlying disease. In most patients, the dynamic process of progressive fibrosis, which could ultimately lead to cirrhosis, can be interrupted by the timely recognition of the risk, followed by appropriate treatment.
Key Messages.
The most common and most important causes of liver cirrhosis in Germany are fatty liver diseases that arise from two widespread conditions, the metabolic syndrome and alcoholism. Genetic risk factors play an important part in determining the risk that an individual will develop cirrhosis.
Cirrhosis can be prevented with individualized, risk-adapted treatment based on the early detection of chronic liver disease.
Cirrhosis can be diagnosed early without great effort or expense (identification of clinical risk constellations, physical examination, laboratory testing including complete blood count and liver function tests, ultrasonography).
Noninvasive testing is being increasingly used to detect hepatic fibrosis and to stage liver disease.
Appropriate treatment can stabilize cirrhosis or even reverse it.
To prevent cirrhosis is to prevent hepatocellular carcinoma as well.
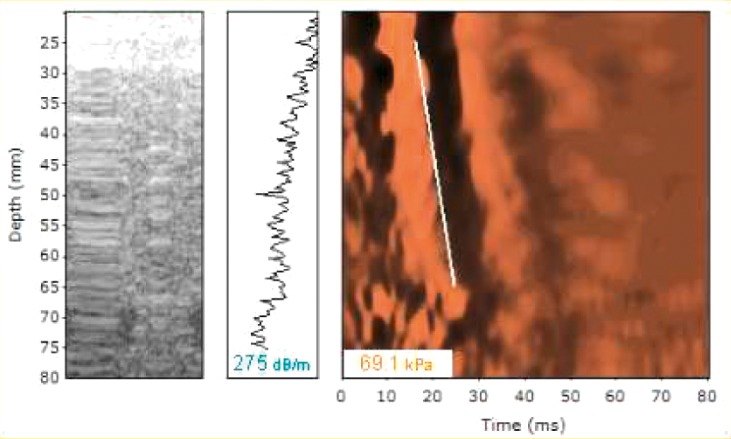
eFigure 1.
Transient elastography in cirrhosis: the measured liver stiffness of 69.1 kPa implies cirrhosis, while the CAP value of 275 dB/m implies steatosis of one-third to two-thirds of the hepatocytes
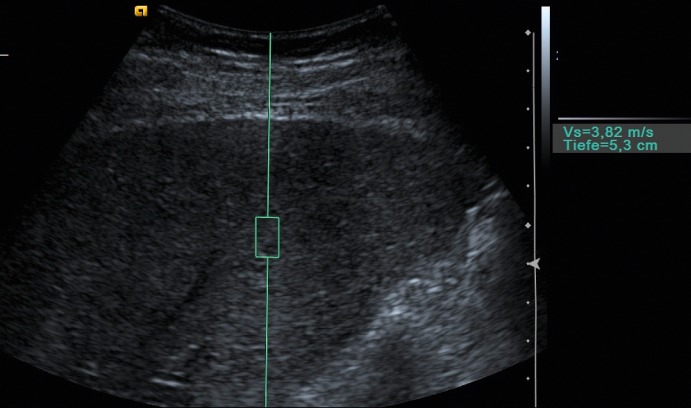
eFigure 2.
ARFI ultrasonography in cirrhosis: the measured value of 3.82 m/s implies cirrhosis
Footnotes
Conflict of interest statement
Prof. Berg has served as a paid consultant for Roche, Gilead, Janssen, BMS, and MSD and has received reimbursement of congress participation fees and travel and accommodation expenses from Roche, Gilead, Janssen, and MSD. He has received lecture honoraria and payment for the preparation of continuing medical education presentations from Roche, Gilead, Janssen, MSD, Bayer, Falk, Norgine, BMS, and Meduna. He has received payment for performing clinical trials on behalf of Roche, Gilead, BMS, Janssen, GSK, Abbott, Falk, Vertex, and MSD.
PD Dr. Wiegand has served as a paid consultant for Gilead. He has received reimbursement of congress participation fees and travel and accommodation expenses, as well as payment for the preparation of continuing medical education presentations, from Gilead, Bristol-Meyers Squibb, Roche, and MSD.
References
- 1.Manns MP, Czaja AJ, Gorham JD, et al. Diagnosis and management of autoimmune hepatitis. Hepatology. 2010;51:2193–2213. doi: 10.1002/hep.23584. [DOI] [PubMed] [Google Scholar]
- 2.Chen CF, Lee WC, Yang HI, et al. Changes in serum levels of HBV DNA and alanine aminotransferase determine risk for hepatocellular carcinoma. Gastroenterology. 2011;141:1240–1248. doi: 10.1053/j.gastro.2011.06.036. [DOI] [PubMed] [Google Scholar]
- 3.Statistisches Bundesamt. Gesundheitsberichterstattung des Bundes. 2011. Todesursachenstatistik. [Google Scholar]
- 4.Neuschwander-Tetri BA, Caldwell SH. Nonalcoholic steatohepatitis: summary of an AASLD Single Topic Conference. Hepatology. 2003;37:1202–1219. doi: 10.1053/jhep.2003.50193. [DOI] [PubMed] [Google Scholar]
- 5.Robert-Koch-Institut. Virushepatitis B, C und D im Jahr 2010. Epid Bull. 2011;29:261–274. [Google Scholar]
- 6.Schuppan D, Afdhal NH. Liver cirrhosis. Lancet. 2008;371:838–851. doi: 10.1016/S0140-6736(08)60383-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Berg T. Diagnostik bei erhöhten Leberwerten. Der Gastroenterologe. 2009;4:557–572. [Google Scholar]
- 8.Tannapfel A, Dienes HP, Lohse AW. The indications for liver biopsy. Dtsch Arztebl Int. 2012;109(27-28):477–483. doi: 10.3238/arztebl.2012.0477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schirmacher P, Fleig WE, Tannapfel A, et al. Bioptic diagnosis of chronic hepatitis. Results of an evidence-based consensus conference of the German Society of Pathology, of the German Society for Digestive and Metabolic Diseases and of Compensated Hepatitis (HepNet) Pathologe. 2004;25:337–348. doi: 10.1007/s00292-004-0692-7. [DOI] [PubMed] [Google Scholar]
- 10.Castera L, Pinzani M. Biopsy and non-invasive methods for the diagnosis of liver fibrosis: does it take two to tango? Gut. 2010;59:861–866. doi: 10.1136/gut.2010.214650. [DOI] [PubMed] [Google Scholar]
- 11.Wai CT, Greenson JK, Fontana RJ, et al. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology. 2003;38:518–526. doi: 10.1053/jhep.2003.50346. [DOI] [PubMed] [Google Scholar]
- 12.Forns X, Ampurdanes S, Llovet JM, et al. Identification of chronic hepatitis C patients without hepatic fibrosis by a simple predictive model. Hepatology. 2002;36:986–992. doi: 10.1053/jhep.2002.36128. [DOI] [PubMed] [Google Scholar]
- 13.Vallet-Pichard A, Mallet V, Nalpas B, et al. FIB-4: an inexpensive and accurate marker of fibrosis in HCV infection comparison with liver biopsy and fibrotest. Hepatology. 2007;46:32–36. doi: 10.1002/hep.21669. [DOI] [PubMed] [Google Scholar]
- 14.Imbert-Bismut F, Ratziu V, Pieroni L, Charlotte F, Benhamou Y, Poynard T. Biochemical markers of liver fibrosis in patients with hepatitis C virus infection: a prospective study. Lancet. 2001;357:1069–1075. doi: 10.1016/S0140-6736(00)04258-6. [DOI] [PubMed] [Google Scholar]
- 15.Poynard T, Halfon P, Castera L, et al. Standardization of ROC curve areas for diagnostic evaluation of liver fibrosis markers based on prevalences of fibrosis stages. Clin Chem. 2007;53:1615–1622. doi: 10.1373/clinchem.2007.085795. [DOI] [PubMed] [Google Scholar]
- 16.Rosenberg WM, Voelker M, Thiel R, et al. Serum markers detect the presence of liver fibrosis: a cohort study. Gastroenterology. 2004;127:1704–1713. doi: 10.1053/j.gastro.2004.08.052. [DOI] [PubMed] [Google Scholar]
- 17.Snyder N, Gajula L, Xiao SY, et al. APRI: an easy and validated predictor of hepatic fibrosis in chronic hepatitis C. J Clin Gastroenterol. 2006;40:535–542. doi: 10.1097/00004836-200607000-00013. [DOI] [PubMed] [Google Scholar]
- 18.Friedrich-Rust M, Ong MF, Martens S, et al. Performance of transient elastography for the staging of liver fibrosis: a meta-analysis. Gastroenterology. 2008;134:960–974. doi: 10.1053/j.gastro.2008.01.034. [DOI] [PubMed] [Google Scholar]
- 19.Friedrich-Rust M, Nierhoff J, Lupsor M, et al. Performance of Acoustic Radiation Force Impulse imaging for the staging of liver fibrosis: a pooled meta-analysis. J Viral Hepat. 2012;19:e212–e219. doi: 10.1111/j.1365-2893.2011.01537.x. [DOI] [PubMed] [Google Scholar]
- 20.Sebastiani G, Castera L, Halfon P, et al. The impact of liver disease aetiology and the stages of hepatic fibrosis on the performance of non-invasive fibrosis biomarkers: an international study of 2411 cases. Aliment Pharmacol Ther. 2011;34:1202–1216. doi: 10.1111/j.1365-2036.2011.04861.x. [DOI] [PubMed] [Google Scholar]
- 21.Argo CK, Northup PG, Al-Osaimi AM, Caldwell SH. Systematic review of risk factors for fibrosis progression in non-alcoholic steatohepatitis. J Hepatol. 2009;51:371–379. doi: 10.1016/j.jhep.2009.03.019. [DOI] [PubMed] [Google Scholar]
- 22.Romeo S, Kozlitina J, Xing C, et al. Genetic variation in PNPLA3 confers susceptibility to nonalcoholic fatty liver disease. Nat Genet. 2008;40:1461–1465. doi: 10.1038/ng.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stickel F, Buch S, Lau K, et al. Genetic variation in the PNPLA3 gene is associated with alcoholic liver injury in caucasians. Hepatology. 2011;53:86–95. doi: 10.1002/hep.24017. [DOI] [PubMed] [Google Scholar]
- 24.Sarrazin C, Berg T, Ross RS, et al. Prophylaxis, diagnosis and therapy of hepatitis C virus (HCV) infection: the German guidelines on the management of HCV infection. Z Gastroenterol. 2010;48:289–351. doi: 10.1055/s-0028-1110008. [DOI] [PubMed] [Google Scholar]
- 25.Cornberg M, Protzer U, Petersen J, et al. Prophylaxis, diagnosis and therapy of hepatitis B virus infection - the German guideline. Z Gastroenterol. 2011;49:871–930. doi: 10.1055/s-0031-1273462. [DOI] [PubMed] [Google Scholar]
- 26.European Association For The Study Of The Liver. EASL Clinical Practice Guidelines: Management of chronic hepatitis B virus infection. J Hepatol. 2012;57:167–185. doi: 10.1016/j.jhep.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 27.Wedemeyer H, Hofmann WP, Lueth S, et al. ALT screening for chronic liver diseases: scrutinizing the evidence. Z Gastroenterol. 2010;48:46–55. doi: 10.1055/s-0028-1109980. [DOI] [PubMed] [Google Scholar]
- 28.Breitling LP, Claessen H, Drath C, Arndt V, Brenner H. Gamma-glutamyltransferase, general and cause-specific mortality in 19,000 construction workers followed over 20 years. J Hepatol. 2011;55:594–601. doi: 10.1016/j.jhep.2010.12.029. [DOI] [PubMed] [Google Scholar]
- 29.Claessen H, Brenner H, Drath C, Arndt V. Gamma-glutamyltransferase and disability pension: a cohort study of construction workers in Germany. Hepatology. 2010;51:482–490. doi: 10.1002/hep.23324. [DOI] [PubMed] [Google Scholar]
- 30.Haring R, Wallaschofski H, Nauck M, Dorr M, Baumeister SE, Volzke H. Ultrasonographic hepatic steatosis increases prediction of mortality risk from elevated serum gamma-glutamyl transpeptidase levels. Hepatology. 2009;50:1403–1411. doi: 10.1002/hep.23135. [DOI] [PubMed] [Google Scholar]
- 31.Roulot D, Costes JL, Buyck JF, et al. Transient elastography as a screening tool for liver fibrosis and cirrhosis in a community-based population aged over 45 years. Gut. 2011;60:977–984. doi: 10.1136/gut.2010.221382. [DOI] [PubMed] [Google Scholar]
- 32.Bell BP, Manos MM, Zaman A, et al. The epidemiology of newly diagnosed chronic liver disease in gastroenterology practices in the United States: results from population-based surveillance. Am J Gastroenterol. 2008;103:2727–2736. doi: 10.1111/j.1572-0241.2008.02071.x. [DOI] [PubMed] [Google Scholar]
- 33.Hofmann WP, Sarrazin C, Zeuzem S. Current standards in the treatment of chronic hepatitis C. Dtsch Arztebl Int. 2012;109(19):352–358. doi: 10.3238/arztebl.2012.0352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.EASL clinical practice guidelines for HFE hemochromatosis. J Hepatol. 2010;53:3–22. doi: 10.1016/j.jhep.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 35.EASL Clinical Practice Guidelines. Wilson’s disease. J Hepatol. 2012;56:671–685. doi: 10.1016/j.jhep.2011.11.007. [DOI] [PubMed] [Google Scholar]
- 36.O’Shea RS, Dasarathy S, McCullough AJ. Alcoholic liver disease. Hepatology. 2010;51:307–328. doi: 10.1002/hep.23258. [DOI] [PubMed] [Google Scholar]
- 37.Wittenburg H, Tennert U, Berg T. Complications of liver cirrhosis. Internist. 2011;52:1061–1070. doi: 10.1007/s00108-011-2853-0. [DOI] [PubMed] [Google Scholar]
- 38.Eckman MH, Kaiser TE, Sherman KE. The cost-effectiveness of screening for chronic hepatitis B infection in the United States. Clin Infect Dis. 2011;52:1294–1306. doi: 10.1093/cid/cir199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zein CO, Unalp A, Colvin R, Liu YC, McCullough AJ. Smoking and severity of hepatic fibrosis in nonalcoholic fatty liver disease. J Hepatol. 2011;54:753–759. doi: 10.1016/j.jhep.2010.07.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Modi AA, Feld JJ, Park Y, et al. Increased caffeine consumption is associated with reduced hepatic fibrosis. Hepatology. 2010;51:201–209. doi: 10.1002/hep.23279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e1.European Liver. 2012. Transplant Registry. [Google Scholar]
- e2.Lackner C, Struber G, Bankuti C, Bauer B, Stauber RE. Noninvasive diagnosis of cirrhosis in chronic hepatitis C based on standard laboratory tests. Hepatology. 2006;43:378–379. doi: 10.1002/hep.21037. [DOI] [PubMed] [Google Scholar]
- e3.Sofair AN, Barry V, Manos MM, et al. The epidemiology and clinical characteristics of patients with newly diagnosed alcohol-related liver disease: results from population-based surveillance. J Clin Gastroenterol. 2010;44:301–307. doi: 10.1097/MCG.0b013e3181b3f760. [DOI] [PubMed] [Google Scholar]
- e4.Julapalli VR, Kramer JR, El-Serag HB. Evaluation for liver transplantation: adherence to AASLD referral guidelines in a large Veterans Affairs center. Liver Transpl. 2005;11:1370–1378. doi: 10.1002/lt.20434. [DOI] [PubMed] [Google Scholar]
- e5.Sanyal A, Poklepovic A, Moyneur E, Barghout V. Population-based risk factors and resource utilization for HCC: US perspective. Curr Med Res Opin. 2010;26:2183–2191. doi: 10.1185/03007995.2010.506375. [DOI] [PubMed] [Google Scholar]
- e6.Marcellin P, Buti M, Gane E, et al. Five years of treatment with tenofovir DF (TDF) for chronic hepatitis B (CHB) infection is associated with sustained viral suppression and significant regression of histological fibrosis and cirrhosis. Hepatology. 2011;54 [Google Scholar]