Abstract
To address health problems that have a major impact on global health requires research designs that go beyond randomized controlled trials. One such design, the participant preference trial, provides additional information in an ecologically valid manner, once intervention efficacy has been demonstrated. The current study presents illustrative data from a participant preference trial of an Internet-based smoking cessation intervention. Participants (N = 7,763) from 124 countries accessed the intervention and were allowed to choose from nine different site components to aid their quit attempt. Of consenting participants, 36.7% completed at least one follow-up assessment. Individuals with depression were more likely to choose a mood management module and participants who smoked a higher number of cigarettes were more likely to choose a cigarette counter and a Nicotine Replacement Therapy guide. Furthermore, depressed participants selecting the mood management component were more likely to report at least one successful 7 day quit (37.2% vs. 22.2%) in the 12 months following the intervention. Thus, participants with depressive symptoms appear to make choices on the basis of their needs and to benefit from these decisions. This suggests that providing the ability to customize previously validated resources may be a successful way to widely disseminate interventions.
Keywords: Preferences, Internet Intervention, Smoking Cessation, Implementation, Dissemination, Spanish-speaking
1. Introduction
The Internet enables individuals to access up-to-date health information and resources comfortably and discretely from their own homes or mobile devices. In 2010, 80% of Internet users indicated searching for health care information online (Fox, 2011). But the Internet can go beyond providing health information. Full-scale Internet-based health interventions for various concerns have been evaluated and found successful, including those for anxiety (Carlbring et al., 2011), depression (Christensen, Griffiths, & Jorm, 2004), and smoking cessation (Muñoz et al., 2006; Muñoz et al., 2009). Internet interventions can complement face-to-face practices and act as stand alone, fully automated self-help interventions. Guided, therapist-assisted, Internet interventions can be as effective as face-to-face interventions at a lower cost (Kiropoulus et al., 2008). These interventions, however, still require the investment of professionals’ time. Fully automated interventions may be less effective for each user but still valuable from a societal perspective as they can provide a basic level of care for people around the world who lack access to other resources and are scalable at a level unmatched by guided techniques (Muñoz, 2010; but see also Rabius, Pike, Wiatrek, & McAlister, 2008 and Graham et al., 2011).
Beyond expanding access to resources for consumers, Internet interventions allow investigators to address questions that might be more difficult to study with face-to-face trials. Thus far, trials of Internet interventions have largely adopted traditional research designs to determine efficacy (e.g., randomized-controlled trials, RCTs). Ritterband and colleagues (2003) argued that randomized-controlled trials are the final step in the process of developing Internet interventions. However, other types of studies can provide additional information and delve deeper into questions of effectiveness and wide-scale implementation. This is especially relevant for Internet interventions, the fluidity of which permits rapid modifications of trial designs (Muñoz, Aguilera, Schueller, Leykin, & Pérez-Stable, 2012).
The current study draws data from a participant preference trial of an Internet-based smoking cessation intervention, previously tested in traditional RCTs (Muñoz et al., 2006; Muñoz et al., 2009). In this trial, users selected from nine possible intervention components validated in the previous RCTs. We examined whether participants chose components most relevant to their needs and whether such choices yielded higher quit rates.
Although participant choice models real-world application, it poses an important question: can participants pick practices that meet their needs? Despite some evidence demonstrating that participants benefit more when receiving a preferred treatment (Swift & Callahan, 2009) it might be that people would be better off following expert opinion or empirically determined recommendations.
An open trial of an Internet-delivered cognitive-behavioral intervention for anxiety disorders found that when participants chose which modules they received, rather than being assigned to them, they still experienced significant reduction in anxiety symptoms (Andersson et al., 2011). Some modules provided general techniques (e.g., cognitive restructuring, relaxation) whereas others targeted specific diagnoses (e.g., panic, agoraphobia). Although the general techniques were selected more often than the specific modules, the researchers did not examine whether choices of the specialized modules were related to specific diagnoses. More research needs to examine individual characteristics that influence choices and how these selections might relate to comparative efficacy of techniques.
The current study investigated the selection patterns of intervention components among participants visiting the “San Francisco Stop Smoking Site” an Internet based smoking cessation resource. Participants could select and access nine different intervention components from an online web portal. We report the choices that participants made and whether people selected components that addressed their specific needs. Further, we examine whether participants who chose the component that addressed a need had better quit rates than those who did not. We had two hypotheses.
People’s choices will be related to their needs. Specifically, participants with higher levels of depressive symptoms and those who screened positive for a current depressive episode would be more likely to select the mood management component; participants smoking a greater number of cigarettes would be more likely to select a cigarette counter and a nicotine replacement therapy (NRT) guide. We predicted these components would be selected by those smoking a greater number of cigarettes because nicotine replacement is especially beneficial for those with moderate to high nicotine dependence (Fiore et al., 2008) and self-monitoring, an effective element of self-help smoking cessation programs (Foxx & Axelroth, 1983; Míquez & Becoña, 2007) has some evidence suggesting it may have a larger impact on those smoking a greater number of cigarettes (Shiffman, 2009).
Those who make choices that are consistent with their needs will report increased quit rates. That is, participants who are depressed will be more likely to quit if they select the mood management component; participants smoking a greater number of cigarettes will be more likely to quit if they select the cigarette counter or the NRT guide.
2. Method
The data we present are from an open participant preference trial of an Internet-based automated self-help smoking cessation. Details of the intervention and quit rates are described elsewhere (Muñoz et al., 2012). Here, we present aspects of the procedure relevant to the selection of differential intervention components.
2.1 Participant Recruitment
Google Adwords campaigns were the primary source of recruitment. Searching for smoking-related terms (e.g. “stop smoking” “how to quit smoking”) via the Google search engine triggered a “sponsored link” (an advertisement in a column to the right of the search result). Clicking on this link forwarded the user to the website. Other participants came to the sites via organic searches (regular search result), links from other websites, media stories, or word of mouth.
2.2 Procedure
The landing page informed visitors that the smoking cessation study contained therein was open to anyone 18 years of age or older, was designed to take about 8 weeks to finish, and that follow-up surveys would be sent out to participants at 1, 3, 6, and 12 months after enrollment. Interested participants clicking on the enrollment link were asked to complete a brief questionnaire containing basic demographic information. Eligible participants (those 18 years of age or older) were asked to provide their e-mail address. Email addresses were used to send consented participants their personalized password to enter the site, the invitations to complete the follow-up questionnaires, and Individually Timed Educational Messages (Lenert, Muñoz, Perez, & Banson, 2004; described below), if the participant chose this component.
After electronically signing the consent document, participants were presented a baseline questionnaire battery, which contained an extended demographics questionnaire, smoking patterns and history questionnaire, and depression measures. Participants could skip individual items but were provided a warning prior to moving on to the next page if any item was left blank. Participants were presented a list of nine components (described below) that they could select for their personalized website homepage. The list, offered in a fixed order to all participants contained a brief description of each component. Selecting a component required clicking on a checkbox next to a descriptive title of each component. Upon completing their selection, participants were forwarded to their personalized home page. The personalized home page contained a navigation bar providing access to the selected components. Consenting participants were automatically e-mailed invitations to complete online follow-up assessments at 1, 3, 6, and 12 months after the date of consent.
Intervention components
Participants could choose from among the following nine components:
The Stop Smoking Guide (Guía para dejar de fumar; henceforth – “Guía”) is an evidence-based intervention approved by the National Cancer Institute (2002). Originally developed for Spanish-speaking smokers, the Guía provides information about the effects of smoking and empirically validated methods for cessation.
Nicotine Replacement Therapy (NRT) Guide offered information regarding three options for nicotine substitutes (nicotine patch, nicotine gum, and nicotine inhaler) and antidepressant medication as quit aids and guidance regarding the appropriate times to consider such interventions.
The Cigarette Counter is a tool for participants to indicate the number of cigarettes smoked during the previous day. It has a graphic interface, and the results from previous entries are displayed as a graph.
The Pre-Quit Checklist listed 10 suggestions to prepare for the quit attempt, e.g., removing smoking-related cues from one’s environment, identifying situations that might lead to relapses, and dealing with those situations.
“Taking Control of Your Life” (Tomando Control de su Vida; henceforth – “Tomando Control”) is a downloadable document containing information useful for the quit attempt (e.g., keeping a daily log with activities, mood, and number of cigarettes smoked). This document had been found to significantly increase quit rates when administered via surface mail (Muñoz, VanOss Marin, Posner, & Pérez-Stable, 1997).
Mood Management is a brief cognitive-behavioral course to help participants improve their mood. It has been found effective at reducing symptoms of depression and increasing rates of quitting (Bränström, Penilla, Pérez-Stable, & Muñoz, 2010). It contains 8 lessons that highlight the link between thoughts, behaviors, and moods and how learning to gain more control over one’s mood without the use of cigarettes can promote quitting.
Individually Timed Educational Messages (ITEMs) contain tips and encouragement to stop smoking. The emails are timed to the selected quit date and contained the link to the site; they have been shown to increase the likelihood of quitting successfully compared to a static online intervention that did not encourage participants to return (Lenert et al., 2004).
The Journal allows participants to enter notes regarding their progress (or anything else); previous entries are available for participants to review. Participants could also choose to post their journal entries on the virtual group bulletin board.
The Virtual Group is an asynchronous bulletin board where participants can post messages and respond to other user’s posts. It is intended to allow participants to obtain support and information from other individuals trying to quit smoking.
2.3 Measures
Demographic questionnaire – participants were asked about their age, gender, race/ethnicity, education, and country of residence.
The MDE Screener (Muñoz, 1998) – an instrument designed to screen for the presence of current and past major depressive episodes (MDEs). The MDE Screener assesses the presence of the 9 DSM-IV symptoms of depression during a two-week period, as well as for Criterion C (significant impairment in functioning). This instrument has been shown to have good agreement with structured (Muñoz, McQuaid, Gonzalez, Dimas, & Rosales, 1999) and clinician-administered interviews (Vázquez, Muñoz, Blanco, López, 2008). The current analysis defines depression as reporting a current major depressive episode on this measure at baseline.
Smoking questionnaire – participants were asked about their smoking history and current smoking behavior, including self-reported number of cigarettes smoked each day. We categorized smoking level as categorical variable dividing “light” (1–9 cigarettes/day), “moderate” 10–19 cigarettes/day, and “heavy” (20 or more cigarettes/day) smokers.
Outcome measure - The cessation outcome measure was self-reported 7-day point prevalence abstinence defined as a “no” response to the item “Have you smoked 1 or more cigarettes in the last 7 days?” This outcome is a point prevalence measure of abstinence and is widely used in smoking cessation trials (Hughes et al., 2003). We used this same outcome in the previously published RCTs (Muñoz et al., 2006; Muñoz et al., 2009). In this study, we were interested in those participants who made a successful quit attempt at any assessment and thus the main quit outcome was whether a participant responded “no” at the 1, 3, 6, or 12-month follow-up.
2.4 Analysis
We analyzed selection of components and how differential selection affected quit rates. Logistic regression models were constructed to predict selection of mood management, cigarette counter, and NRT guide. Predictors were: age, sex, education, language, current major depressive episode, and smoking level. Logistic regressions including interaction terms between predictors and selection of specific techniques were used to determine if individuals with hypothesized prescriptive variables who selected specific techniques would result in greater quit rates, for example if individuals with current depression who selected the mood management component would be more likely to quit and if individuals who smoked more cigarettes per day who selected the cigarette counter or NRT guide would be more likely to quit.
3. Results
3.1 Sample
Participants consisted of 7,763 people who visited our online smoking cessation website between September 18, 2008 and September 18, 2009 and consented to participate in a research study. This sample includes both visitors to an English (n = 1,825) and Spanish (n = 5,938) language version of the website. The average age of participants was 35.23 (SD = 10.80). The sample contained a slightly higher percentage of men (54.8%) than women. The website was available worldwide and 124 countries and territories were represented in the sample. As individuals could skip items on the baseline assessments, only those participants reporting all items on a questionnaire were included in baseline reports. Table 1 displays summary statistics of demographic and clinical measures with sample sizes corresponding to the number of participants who completed all relevant items. Outcome measures were available on 2,852 participants (36.7%) who completed at least one of the follow-up assessments.
Table 1.
Summary statistics for consenting participants who completed baseline.
| All (n=7,763) | English (n = 1,825) | Spanish (n = 5,938) | |
|---|---|---|---|
| Sex | n = 7,724 | n = 1,820 | n = 5,904 |
| Men | 54.8 | 64.1 | 51.9 |
| Women | 45.2 | 35.9 | 48.1 |
| Age M(SD) | 35.23 (10.8) | 33.34 (10.8) | 35.81 (10.7) |
| 18–24 | 16.3 | 22.2 | 14.5 |
| 25–34 | 37.9 | 40.4 | 37.2 |
| 35–44 | 24.5 | 20.3 | 25.8 |
| 45–54 | 15.8 | 12.2 | 16.9 |
| 55–64 | 4.7 | 4.1 | 4.9 |
| 65+ | 0.7 | 0.8 | 0.7 |
| Education | n = 7,622 | n = 1,795 | n = 5,827 |
| High school or Less | 23.0 | 17.4 | 24.7 |
| Some college | 36.1 | 25.3 | 39.5 |
| College grad | 29.7 | 37.5 | 27.3 |
| Graduate degree | 11.2 | 19.8 | 8.5 |
| Depression variables | n = 7,712 | n = 1,799 | n = 5,913 |
| Major depressive episodes | |||
| No MDE history | 49.6 | 52.0 | 48.8 |
| Past MDE only | 32.2 | 32.6 | 32.1 |
| Current MDE | 18.2 | 15.4 | 19.1 |
| Smoking variables | n = 7,253 | n = 1,681 | n = 5,572 |
| Cigarettes per day M(SD) | 18.2 (12.0) | 16.8 (10.9) | 18.7 (12.3) |
| 1–9 cigarettes per day | 15.7 | 20.8 | 14.2 |
| 10–19 cigarettes per day | 34.5 | 35.5 | 34.2 |
| 20+ cigarettes per day | 49.8 | 43.7 | 51.6 |
Note: MDE = Major depressive episodes. Means and standard deviations are reported on continuous variables where indicated, all other values are percent of participants in each categorical variable.
3.2 Selection of Components
Table 2 displays the proportion of participants who chose each method. The Guía was chosen most often (93.0%) and the virtual group was chosen least often (53.3%). Table 3 displays how many people chose how many components. About one-third of the sample selected to have all components available to them.
Table 2.
Number and Percent of Individuals Selecting Each Component (N = 7,763)
| All (n = 7,763) | English (n = 1,825) | Spanish (n = 5,938) | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Number | Percent | Number | Percent | Number | Percent | |
| Guía | 7,221 | 93.0% | 1,703 | 93.3% | 5,518 | 92.9% |
| Pre-Quit Checklist | 6,080 | 78.3% | 1,423 | 78.0% | 4,657 | 78.4% |
| Mood Management Course | 5,923 | 76.3% | 1,323 | 72.5% | 4,600 | 77.5% |
| Cigarette Counter | 5,590 | 72.0% | 1,264 | 69.3% | 4,326 | 72.9% |
| Tomando Control | 5,537 | 71.3% | 1,327 | 72.7% | 4,210 | 70.9% |
| Email Reminders | 5,474 | 70.5% | 1,299 | 71.2% | 4,175 | 70.3% |
| Nicotine Replacement Therapy Guide | 4,743 | 61.1% | 987 | 54.1% | 3,756 | 63.3% |
| Journal | 4,384 | 56.5% | 926 | 50.7% | 3,458 | 58.2% |
| Virtual Group | 4,140 | 53.3% | 903 | 49.5% | 3,237 | 54.5% |
Table 3.
Number of People Selecting Different Number of Components (N = 7,763)
| Components Selected | All (n = 7,763) | English (n = 1,825) | Spanish (n = 5,938) | |||
|---|---|---|---|---|---|---|
|
| ||||||
| Number | Percent | Number | Percent | Number | Percent | |
| 1 | 642 | 8.3% | 153 | 8.4% | 489 | 8.2% |
| 2 | 331 | 4.3% | 84 | 4.6% | 247 | 4.2% |
| 3 | 486 | 6.3% | 114 | 6.2% | 372 | 6.3% |
| 4 | 595 | 7.7% | 158 | 8.7% | 437 | 7.4% |
| 5 | 639 | 8.2% | 176 | 9.6% | 463 | 7.8% |
| 6 | 779 | 10.0% | 215 | 11.8% | 564 | 9.5% |
| 7 | 781 | 10.1% | 199 | 10.9% | 582 | 9.8% |
| 8 | 948 | 12.2% | 229 | 12.5% | 719 | 12.1% |
| 9 | 2,562 | 33.0% | 497 | 27.2% | 2065 | 34.8% |
We were first interested in predictors of the number of components selected. Given the use of count data, we conducted a Poisson regression to analyze the relationship between demographic and mental health predictors and the number of items selected by participants at baseline (n = 7,483). The goodness-of-fit chi-squared test was not statistically significant (P = 0.24) indicating that the model fits the data reasonably well. Women, younger, more educated, visitors to the Spanish language site, current major depressive episode, and higher smoking level all predicted selecting more components.
Next we investigated our hypotheses that selection of specific components would follow from individual needs. That is, participants with current major depressive episodes would be more likely to select the mood management component and participants with a higher smoking level would be more likely to select the NRT guide and the cigarette counter. We conducted a logistic regression to determine characteristics of participants (n = 7,483) that were linked to selection of the mood management component while controlling for age, gender, education, and language of the website visited. Individuals screening positive for current depression were more likely to select the mood management component (OR = 1.57, 95% CI 1.35–1.84, P < 0.001). Smoking level was not a significant predictor of selection of the mood management component. Women (OR = 1.44, 95% CI 1.28–1.61, P < 0.001), those with higher levels of education (OR = 1.08, 95% CI, 1.05–1.11, P < 0.001), and visitors to the Spanish version of the site (OR = 1.31, 95% CI, 1.15–1.50, P < 0.001) were all more likely to select the mood management component as well; 82.1% of individuals with current depression choose the mood management component compared to 75.2% of those without current depression.
We next considered selection of smoking related components. For the cigarette counter, we conducted a logistic regression using the same predictors (n = 7,483). Smoking a higher number of cigarettes was a significant predictor of selecting the cigarette counter (OR = 1.16, 95% CI 1.07–1.25, P < 0.001). Again, we controlled for demographic variables including age, gender, education, and language of the website visited. Younger participants, (OR = .98, 95% CI .97–.98, P < 0.001), women (OR = 1.19, 95% CI 1.07–1.33, P = 0.002), those with higher levels of education (OR = 1.04, 95% CI 1.01–1.07, P = 0.006), and visitors to the Spanish version of the site (OR = 1.21, 95% CI 1.06–1.37, P = 0.004) were all more likely to select the cigarette counter as well. Individuals with current depression also selected the cigarette counter at higher rates than individuals who were not currently depressed (OR = 1.15, 95% CI 1.00–1.33, P = 0.05). An additional logistic regression analyzed selection of the NRT guide (n = 7,483). Again, smoking a greater number of cigarettes corresponded to higher rates of selection (OR = 1.18, 95% CI 1.10–1.26, P < 0.001), as did screening positive for current depression (OR = 1.19, 95% CI 1.05–1.35, P = 0.007). Of the demographic predictors, age (OR = .99, 95% CI .98–.99, P = 0.003), education (OR = 1.04, 95% CI 1.01–1.07, P = 0.008), and Spanish language (OR = 1.43, 95% CI 1.27–1.60, P < 0.001) all predicted rates of selection of this component. Thus, whereas having higher level of addiction predicted selecting smoking-related components, but not mood management, screening positive for a current major depressive episode predicted the selection of both mood management and smoking components.
3.3 Selection of Components and Quit Rates
Lastly, we had predicted that individuals who select components that best meet their needs would be more likely to quit. Across the entire sample 45.0% of people completing follow-up measures reported a quit attempt during one of the follow-up assessments (45.7% for English, 44.8% for Spanish).
More detailed analysis of the quit rates are reported elsewhere (Muñoz et al., 2012). To analyze whether selection affected outcome, we were interested in interaction terms from the logistic regressions (n = 2,852) predicting those who reported a successful quit. We found a significant interaction between current major depressive episode status, selection of the mood management component, and success in quitting (P = 0.04) while controlling for number of components selected. Merely picking more components did not improve success in quitting as a greater number of components selected actually predicted reduced quit rates (P = 0.01). Figure 1 displays the quit rates across those choosing or not choosing the mood management component for both individuals with and without current major depressive episode. Specifically for those experiencing a current depressive episode, 37.2% of those who selected the mood management component reported a successful quit attempt whereas only 22.2% of people who did not select the mood management component reported quitting during at least one of the follow-up assessments (Fisher’s exact test P = 0.006).
Figure 1. Quit Rates Comparing Selection of Mood Management Component by Depression Status.
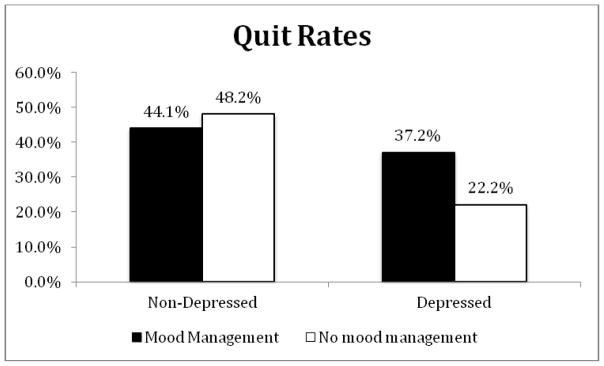
Note: A Fisher’s exact test was conduced to determine if observed quit rates (number reporting abstinence divided by number reporting smoking status) were equivalent amongst groups. Quit rates were not equally distributed amongst groups (P = 0.006).
We also investigated three-way interactions including both gender and language to determine if either men or women were better at selecting components that met their needs or if this was different in the visitors to different language versions of the websites. None of these variables produced significant interaction terms. Although women and Spanish speakers selected the mood management component more often, this did not relate to increased quit rates.
We conducted similar analyses investigating whether those who smoked higher number of cigarettes per day who selected the cigarette counter and the NRT guide were more likely to quit. Neither of these regressions found significant main effects nor interactions between cigarettes per day and either condition.
4. Discussion
In this report, we investigated choices participants made for specific intervention components in an Internet-based smoking cessation study. Participants could choose among nine different intervention components. We found that screening positive for major depressive episode and higher number of self-reported cigarettes smoked per day were related to selection of more components. Consistent with our hypotheses, participants screening positive for current depression were more likely to select a mood management intervention. Furthermore, participants meeting criteria for a current major depressive episode who selected the mood management component were more likely to report quitting compared to those individuals who met criteria for a current depressive episode but did not select the mood management component. These results indicate that participants in general are able to identify components that would be useful for them and tend to benefit differentially from these selections.
Although most participants were interested in learning about the mood management component, a slightly greater (82.1% vs. 75.2%) percent of those with current depression selected it as an option. This was not simply related to greater distress as smoking level was not related to higher rates of selection of that component. This suggests that individuals with depressive symptoms can accurately identify what they need. For the addiction severity analysis, smoking level did predict higher selection of the NRT guide and cigarette counter but with less specificity than the mood management findings, as current depression also predicted selection of the NRT guide and the cigarette counter. We did not find, however, that selection of these components then led to increased quit rates. It could be in this study that the mood management component was more of a unique feature (designed specifically to address mood problems) and was indicated for those who experienced current mood symptoms and had a desire to quit. Given that all of the resources were designed with smoking cessation in mind, it could be that receiving any component adequately addressed the needs of those who were highly dependent.
Participants in this trial selected more components if they experienced greater symptom severity (as indicated by current depression or greater cigarettes smoked per day). The most common pattern, however, was that participants selected all of the components available. The most popular component was the Guía, a psychoeducation pamphlet that included information and empirically supported techniques for stopping smoking.
As predicted, individuals select components on the basis of their needs. In this sample, participants screening positive for major depressive episodes were more likely to select a cognitive-behavioral based mood management intervention and heavier smokers selected the NRT guide and the cigarette counter. These findings provide support for wide dissemination of evidence-based self-help materials. Participants seem able to identify the best individual components for them. If so, unguided, automated interventions, much like this one, can be a very effective technique for meeting their needs. In this study, very few smokers (only 1 out of 3) had used other smoking cessation aids prior to coming to the San Francisco Stop Smoking site. For example, only 3.3% had consulted with a physician or nurse and 1.7% had attended a smoking cessation group (Muñoz et al., 2012). Making self-help resources available is one way to overcome this massive gap in utilizing needed services.
Our findings are consistent with past research that has demonstrated that participants with lower initial levels of positive affect are more successful at quitting if they receive a mood management component (Bränström et al., 2010). People often use smoking as a stress management strategy and, for those participants who need additional help to manage their moods, their quit attempts may be unsuccessful without additional help in this regard. The current study shows that people who report depressive symptoms quit at higher rates when they select a mood management component.
We found no evidence for differential interactions between gender or language. Although there was a main effect such that women and Spanish speakers picked the mood management component more frequently, this did not correspond to higher quit rates for either group. This suggests that evidence-based Internet interventions may work similarly well across gender and cultural groups. Although it appears that individuals with current depression benefit more when this is addressed, we may not need to change components for different genders or language groups.
This trial has several limitations. First, it recruited participants and conducted the trial entirely online, with no human interaction. Thus, it may not generalize to non-Internet interventions. As a consequence, the retention rate of 36.73% is low, however, this is consistent with other trials of Internet interventions (Eysenbach, 2005). Nevertheless, even with low retention rates, the accessibility and reach of Internet interventions allows large populations to benefit (Muñoz et al., 2012). Second, participants selected components at the beginning of the intervention and may not have fully understood the nature of some of the components before making their selection. It is possible that providing participants with a brief preview of each component may increase appropriate selection of components. Another option would be to examine what people use not just what they select. Future research, especially using Internet interventions, should include metrics of usage of techniques to determine if people use what they select and how usage might relate to outcomes. Lastly, in this trial the cost of selection was very low hence the most common choice was to choose everything. This does not mirror the real world where people make trade offs when choosing between options, e.g., choosing one often means not receiving the other or investing time in one means less time devoted to another. Future trials might consider limiting the number of components participants can choose to determine if this affects selections or outcome.
This study has implications for researchers interested in the dissemination of interventions. This study took advantage of the fact that an Internet intervention developed for previous RCTs could quickly and efficiently be turned into a participant preference trial to allow for an investigation of different questions, including what people select when provided choice and how these choices relate to observed quit rates. By using a research design other than an RCT (which had already been conducted with this intervention), we were able to gain new insight into how people might select and benefit from these techniques when disseminated widely. We encourage other researchers to build upon their initial outcome trials by using additional designs and recommend routine implementation of open participant preference trials after Internet RCTs are completed.
An unanswered question is whether these findings can guide prescribed dissemination of treatment components. It is worth knowing if allowing users to choose components is different than assigning components based on baseline assessments (e.g., participants with current depression being assigned the mood management component). Participants may be more motivated to use components that they choose and thus the act of choosing may impact engagement or efficacy. Controlled investigations of prescribed versus self-selected treatment content could shed light on whether choice plays an important role or is merely one avenue to getting people what they need.
This study demonstrates that allowing participant choice is a desirable method of disseminating efficacious intervention components. Many individuals (e.g., depressed smokers) are capable of making reasonable choices and benefited from their decisions. Online web resources provide a ready method for researchers to further investigate how well people access what most benefits them.
Acknowledgments
This research program was supported by the Tobacco Related Disease Research Program, the University of California, Office of the President, the Google Adwords Grants Program, and the Brin Wojcicki Foundation (Muñoz, P.I.), the National Cancer Institute (NCI) for Redes en Acción (U01CA86117) (Pérez-Stable, P.I.) and by NIMH grants F32MH095345 (Schueller, P.I.) and -5K08MH091501 (Leykin, P.I.). We would also like to thank the Center for Health and Community at UCSF, the Information Services Unit, Leslie Lenert, Carlos Penilla, Eduardo Ballesteros, Thomas Manley, and Veronica Pitbladdo for their contributions to this line of research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Andersson G, Estling F, Jakobsson E, Cuijpers P, Carlbring P. Can the patient decide which modules to endorse? An open trial of tailored Internet treatment of anxiety disorders. Cognitive Behaviour Therapy. 2011;40:57–64. doi: 10.1080/16506073.2010.529457. [DOI] [PubMed] [Google Scholar]
- Bränström B, Penilla C, Pérez-Stable EJ, Muñoz RF. Positive affect and mood management in successful smoking cessation. American Journal of Health Behavior. 2010;34:553–562. [PubMed] [Google Scholar]
- Carlbring P, Maurin L, Törngren C, Linna E, Eriksson T, Sparthan E, Strååt M, Marquez von Hage C, Bergman-Nordgren L, Andersson G. Individually-tailored, internet-based treatment for anxiety disorders: A randomized controlled trial. Behaviour Research and Therapy. 2011;49:18–24. doi: 10.1016/j.brat.2010.10.002. [DOI] [PubMed] [Google Scholar]
- Christensen H, Griffiths KM, Jorm AF. Delivering interventions for depression using the internet: Randomised controlled trial. British Medical Journal. 2004;328:265–270. doi: 10.1136/bmj.37945.566632.EE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenbach G. The law of attrition. Journal of Medical Internet Research. 2005;7:e11. doi: 10.2196/jmir.7.1.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiore MC, Jaén CR, Baker TB, et al. Clinical practice guideline. Rockville, MD: U.S. Department of Health and Human Services; 2008. Treating tobacco use and dependence: 2008 update. [Google Scholar]
- Fox S. The social life of health information. 2011 Retrieved from http://pewinternet.org/Reports/2011/Social-Life-of-Health-Info.aspx.
- Foxx RM, Axelroth E. Nicotine fading, self-monitoring and cigarette fading to produce cigarette abstinence or controlled smoking. Behaviour Research and Therapy. 1983;21:17–27. doi: 10.1016/0005-7967(83)90122-5. [DOI] [PubMed] [Google Scholar]
- Graham AL, Cobb NK, Papandonatos GD, Moreno JL, Kang H, Tinkelman DG, Bock BC, Niaura RS, Abrams DB. A randomized trial of Internet and telephone treatment for smoking cessation. Archives of Internal Medicine. 2011;10:46–53. doi: 10.1001/archinternmed.2010.451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes JR, Keely JP, Niaura S, Ossip-Klein DJ, Richmond RL, Swan GE. Measures of abstinence in clinical trials: Issues and recommendations. Nicotine & Tobacco Research. 2003;5:13–25. [PubMed] [Google Scholar]
- Kiropoulous LA, Klein B, Austin DW, Gilson K, Pier C, Mitchell J, Ciechomski L. Is internet-based CBT for panic disorder and agoraphobia as effective as face-to-face CBT? Journal of Anxiety Disorders. 2008;22:1273–1284. doi: 10.1016/j.janxdis.2008.01.008. [DOI] [PubMed] [Google Scholar]
- Lenert L, Muñoz RF, Perez J, Banson A. Automated e-mail messaging as a tool for improving quit rates in an Internet smoking cessation intervention. Journal of the American Medical Informatics Association. 2004;11:235–240. doi: 10.1197/jamia.M1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Míguez MC, Becoña E. Evaluating the effectiveness of a single telephone contact as an adjunct to a self-help intervention for smoking cessation in a randomized controlled trial. Nicotine & Tobacco Research. 2007;10:129–135. doi: 10.1080/14622200701767746. [DOI] [PubMed] [Google Scholar]
- Muñoz RF. Preventing major depression by promoting emotion regulation: A conceptual framework and some practical tools. International Journal of Mental Health Promotion. 1998;1:23–40. [Google Scholar]
- Muñoz RF. Using evidence-based Internet interventions to reduce health disparities worldwide. Journal of Medical Internet Research. 2010;12:e60. doi: 10.2196/jmir.1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muñoz RF, Aguilera A, Schueller SM, Leykin Y, Pérez-Stable EJ. From online randomized controlled trials to participant preference studies: Morphing the San Francisco stop smoking site into a worldwide smoking cessation resource. Journal of Medical Internet Research. 2012;14:e64. doi: 10.2196/jmir.1852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muñoz RF, Barrera AZ, Delucchi K, Penilla C, Torres LD, Pérez-Stable EJ. International Spanish/English Internet smoking cessation trials yields 20% abstinence rates at 1 year. Nicotine & Tobacco Research. 2009;11:1025–1034. doi: 10.1093/ntr/ntp090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muñoz RF, Lenert LL, Delucchi K, Stoddard J, Perez JE, Penilla C, Pérez-Stable EJ. Toward evidence-based Internet interventions: A Spanish/English web site for international smoking cessation trials. Nicotine & Tobacco Research. 2006;8:77–87. doi: 10.1080/14622200500431940. [DOI] [PubMed] [Google Scholar]
- Muñoz RF, McQuaid JR, Gonzalez GM, Dimas J, Rosales VA. Depression screening in a women’s clinic: Using automated Spanish-and English-language voice recognition. Journal of Consulting and Clinical Psychology. 1999;67:502–510. doi: 10.1037//0022-006x.67.4.502. [DOI] [PubMed] [Google Scholar]
- Muñoz RF, VanOss Marín B, Posner SF, Pérez-Stable EJ. Mood management mail intervention increases abstinence rates for Spanish-speaking Latino smokers. American Journal of Community Psychology. 1997;25:325–343. doi: 10.1023/a:1024676626955. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute. NIH Publication No 02–3001. Washington, DC: U.S. Government Printing Office; 2002. Guía para dejar de fumar [Guide for quitting smoking] Retrieved August 1, 2011, from http://dccps.cancer.gov/tcrb/No_FumarC.pdf. [Google Scholar]
- Rabius V, Pike KJ, Wiatrek D, McAlister AL. Comparing assistance for smoking cessation: 13-month follow-up of a six-arm randomized controlled trial. Journal of Medical Internet Research. 2008;10:e45. doi: 10.2196/jmir.1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritterband LM, Gonder-Frederick LA, Cox DJ, Clifton AD, West RW, Borowitz SM. Internet interventions: In review, in use, and into the future. Professional Psychology: Research and Practice. 2003;34:527–534. [Google Scholar]
- Shiffman S. How many cigarettes did you smoke? Assessing cigarette consumption by global report, time-line follow-back, and ecological momentary assessment. Health Psychology. 2009;28:519–526. doi: 10.1037/a0015197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swift JK, Callahan JL. The impact of client treatment preferences on outcome: A meta- analysis. Journal of Clinical Psychology. 2009;65:368–381. doi: 10.1002/jclp.20553. [DOI] [PubMed] [Google Scholar]
- Vázquez FL, Muñoz RF, Blanco V, López M. Validation of Muñoz’s mood screener in a nonclinical Spanish population. European Journal of Psychological Assessment. 2008;24:57–64. [Google Scholar]


