Abstract
Hepatitis E virus (HEV) causes an orofecal disease transmitted through poor hygiene environments, contaminated food (mainly pork products), or by contacts with infected animals. Very little data are currently available regarding the disease in the Southwestern Indian Ocean Islands. We report the first sero- and viro-survey for HEV in human and swine in Madagascar. A seroprevalence rate of 14.1% (60 of 427) was measured in slaughterhouse workers. Seroprevalence to HEV in pigs was estimated to 71.2% (178 of 250), strongly suggesting the existence of a zoonotic cycle. Three out of 250 pig livers (1.2%) tested HEV RNA-positive by quantitative polymerase chain reaction. Phylogenetic analyses based on 1-kb sequences of the ORF 2-3 identified these viruses as HEV genotype 3. Sequences clustered in a distinct Malagasy sub-clade, possibly representative of a new sub-genotype, for which the date of emergence was estimated around 1989. Further studies are needed to confirm other transmission routes of HEV to humans, especially through non-zoonotic cycles.
Introduction
Hepatitis E virus (HEV), the single member of the family Hepeviridae, genus Hepevirus, is a small non-enveloped virus with ∼7,200 nucleotide positive-sense, single-stranded RNA genome1; there are four major recognized and two putative genotypes of HEV according to previous sequence analyses. Genotype 1 and 2, restricted to humans, are associated with epidemics in developing countries with poor hygiene conditions (mainly genotype 1 in Asia and Africa and genotype 2 in Central America and Central Africa).2 Genotypes 3 and 4 infect swine and humans, the latter being infected by the consumption of contaminated food, resulting in sporadic cases of hepatitis E in both developing and industrialized countries.3–6 Genotype 3 infects the broadest spectrum of hosts (human, swine, wild boar, deer, rabbit, mongoose, etc.) and has the greatest genetic diversity, with 10 identified sub-genotypes (3a to 3j).7 Recently, new animal hepeviruses have been described in rats,8 poultry,9–11 and bats,12 however they are phylogenetically divergent and likely define new genera within the Hepeviridae family.
The HEV infection in swine occurs with elevated seroprevalences, sometimes higher than 95%, though it remains mainly asymptomatic.13 In France, HEV was reported to affect more than 30% of pigs and 65% of swine herds.14 In humans, hepatitis E has been reported worldwide.15–20 It is considered as an emerging viral disease of importance to public health and a significant cause of acute clinical hepatitis among adults in Asia, Middle East and Africa.2,21,22 High lethality rates have been reported in some developing countries, especially among pregnant women.23 In addition to the consumption of contaminated food, humans can be infected by HEV by direct exposure to swine or swine effluent or to infected swine blood,24 but there likely exist other important modes of viral transmission. People working in swine farms and slaughterhouses are known to be at higher risk of HEV infection.25,26
In the Southwestern Indian Ocean Islands, little information on HEV infection is available, essentially reported from the French overseas departments of La Réunion and Mayotte: a sporadic case of HEV, probably imported, was reported in Mayotte island, in the Comoros Archipelago.27 In Reunion Island, two human cases were reported in 2012, three human cases in 2008,28 and an imported hepatitis E case in 2003.29 No study has been carried out so far to determine the epidemiology of HEV infection in human population, nor the HEV status of the pig herds and risk factors associated with human contamination in these areas. Hence, the objectives of this study were 1) to assess HEV infection among humans in Madagascar by exploring the HEV seroprevalence in a high risk population, i.e., slaughterhouse workers; 2) to explore a possible pig-to-human zoonotic transmission cycle in Madagascar by assessing the HEV seroprevalence in swine herds; and 3) to identify the genotype of HEV circulating in pigs.
Material and Methods
Sampling description.
Human sera.
Human sera came from a serobank stored at Institut Pasteur in Madagascar that was collected between September 27, 2008 and May 27, 2009. Sera were collected during a national cross-sectional serologic survey among voluntary slaughterhouse workers within the administrative center of the district. We selected 427 sera from workers that lived in the same 18 districts and 11 regions from where the sampled pigs originated. The demographic characteristics of the workers included in the study are presented in Table 1.
Table 1.
Socio-demographic characteristics of slaughterhouse workers included in the study
| Characteristics of individuals | Number (%) |
|---|---|
| Gender | |
| Male | 338 (90.9%) |
| Female | 39 (9.1%) |
| Age group (years) | |
| < 20 | 28 (8.4%) |
| 20–30 | 133 (31.2%) |
| 30–40 | 128 (30.0%) |
| 40–50 | 82 (19.2%) |
| 50–60 | 48 (11.2%) |
| Duration of activity (years) | |
| < 5 | 57 (13.4%) |
| 5–10 | 223 (52.2%) |
| 10–20 | 79 (18.5%) |
| 20–30 | 68 (15.9%) |
| District (no) | |
| Ambalavao (1) | 31 (7.3%) |
| Ambato-Boina (2) | 5 (1.2%) |
| Ambatondrazaka (3) | 34 (8.0%) |
| Ambohimahasoa (4) | 18 (4.2%) |
| Ambositra (5) | 25 (5.9%) |
| Andramasina (6) | 32 (7.5%) |
| Arivonimamo (7) | 58 (13.6%) |
| Bealanana (8) | 19 (4.5%) |
| Befandriana-Nord (9) | 9 (2.1%) |
| Fianarantsoa Urban (10) | 33 (7.7%) |
| Maevatanana (11) | 13 (3.0%) |
| Manakara-Sud (12) | 18 (4.2%) |
| Marovoay (13) | 12 (2.8%) |
| Miarinarivo (14) | 18 (4.2%) |
| Morondava (15) | 29 (6.8%) |
| Port-Berger (16) | 19 (4.5%) |
| Soavinandriana (17) | 19 (4.5%) |
| Tsiroanomandidy (18) | 35 (8.2%) |
Samples from pigs.
A total of 20,000 pigs were estimated to be slaughtered at the four abattoirs of Antananarivo, the capital city of Madagascar, during the 3 months of surveys. To detect an estimated prevalence of HEV viral contamination of 2% in the swine population (with a confidence level at 99%), blood sera and liver samples were collected from 250 animals (M/F = 111/139) from November 2010 to January 2011. Animals were all more than 6 months of age at the date of slaughtering. Blood samples were collected at the bleeding post and a small piece of liver tissue was cut from the left medial lobe close to the gallbladder, as previously described14; all biological samples were transported in a cool box at 4°C, and then frozen and stored at −80°C. Because the absence of animal traceability in Madagascar excludes the possibility of the identification of an individual pig's farm at source, we considered the district and region of production as areas of origin. The sampled animals originated from 18 districts from 11 of 22 administrative regions.
Ethical considerations.
The human serobank used in this study was constituted under a human research protocol approved by the National Ethical Review Committee from the Malagasy Ministry of Public Health. (Authorization no. 228 – SANPFPS July 3, 2008) and amended for the current study (Authorization no. 039-SANPFPS June 4, 2012). The Malagasy Department of Veterinary Research and Husbandry does not, at this time, have a committee to review and approve scientific research protocols involving animals.
Serological analysis.
Detection of anti-HEV in human sera.
A commercial kit (EIAgen HEV Ab, Adaltis, Milano, Italy) was used, which detects immunoglobulin G (IgG) and IgM antibodies to the four HEV genotypes. The test was carried out according to the manufacturer's instructions. Samples were considered positive when the ratio between the OD450 values of the sample to that of the cutoff was higher than 1.1 (cutoff = mean of the negative control + 0.350).
Detection of antibodies to HEV in pig sera.
A commercial test validated for veterinary analysis was used: HEV ELISA 4.0v (MP Diagnostics, Illkirch, France). This test is a double sandwich ELISA detecting IgG, IgM, and IgA antibodies to a proprietary recombinant antigen, which is highly conserved between different HEV strains (genotypes 1 to 4). Analyses were performed according to the manufacturer's instructions except that 10 μL of sera were used.30 Samples were considered positive when the OD450 value of the sample was superior to the cutoff value (cutoff = mean of the negative control + 0.300).
Molecular detection of HEV in pig liver.
A small piece of liver tissue (∼1 mm3) was dissected on ice from the frozen samples and homogenized in DMEM medium using the TissueLyser (Qiagen GmbH, Hilden, France) and a 3 mm tungsten bead for 2 min at 25 Hz. Total nucleic acids were extracted from the mixture supernatant using the EZ1 Viral mini kit v2.0 and the EZ1 BioRobot (Qiagen), according to the manufacturer's recommendations. The complementary DNA (cDNA) was generated by GoScript Reverse Transcriptase using random hexamers (Promega Corporation, Madison, WI). TaqMan HEV quantitative polymerase chain reaction (qPCR) was conducted as described by Jothikumar and others,31 i.e., primers and probe targeting a portion of the open reading frame (ORF) 3 region of HEV genotypes 1 to 4 in animals and environmental samples.
Sequencing.
A sequence of 1,059 bp within the ORF 2-3 region was generated using a semi-nested PCR. The first round PCR was conducted on 5 μL of cDNA in a final volume of 25 μL containing 2X GoTaq Hot Start Mastermix, and 200 nM of primers JVHEV-F,31 and TqRev.32 Cycling conditions were as follows: 95°C for 2 min, and then 35 cycles of 95°C for 15 sec/60°C for 30 sec/72°C for 2 min followed by a final elongation step at 72°C for 7 min. Second round PCR was performed on 4 μL of primary PCR product in a final volume of 50 μL containing 200 nM of primers JVHEV-F and 3159N.33 Cycling conditions were the same as the first round PCR except that 40 cycles were performed. Positive amplifications were purified on a 1% (w/v) agarose gel electrophoresis with the QIAquick gel extraction kit (Qiagen), cloned in a pGEM-T Easy vector (Promega), and finally sequenced (GATC Biotech, Konstanz, Germany). Sequences were primers trimmed and assembled for analysis using the Geneious Pro 5.3.4 software package.34
Phylogenetic analyses.
All alignments were generated in Geneious Pro using the MUSCLE alignment method.35 The DNA substitution model that best fitted the data was performed by the software jModelTest 0.1.136 and was considered for all phylogenetic analyses. We selected different models of nucleotide substitution using the corrected Akaike information criterion.
Molecular evolutionary distances.
Evolutionary distances between sequences were calculated using MEGA 5,37 taking into account the best model of sequences evolution allowing correction of the estimates of evolutionary distance. Because MEGA does not contain the general time-reversible (GTR) model proposed, we used the Tajima-Nei correction,38 which is the nearest model to those proposed by jModelTest.
Genotyping and sub-typing.
For the determination of HEV genotype of the Malagasy strains, a total of 40 GenBank sequences of full-genome HEV were selected according to their origin (Asia, Europe, Africa, and America), their host (human, swine, rabbit, mongoose, and wild boar) and their genotype and sub-genotype. Avian HEV was defined as outgroup. Phylogenetic trees were constructed using the generated sequence of ∼1-kb by maximum likelihood (ML) within PhyML.39 Nodal support was evaluated by 1,000 bootstrap replicates. Bayesian phylogenetic inference (BI) was carried out using MrBayes,40 with two independent runs of four incrementally heated, Metropolis-coupled Markov chain Monte Carlo (MCMC) starting from a random tree. The MCMC were run for 1,000,000 iterations and associated model parameters being sampled every 200 generations. The initial 1,000 trees in each run were discarded as burning samples and the harmonic mean of the likelihood was calculated by combining the two independent runs.
To implement a maximum of sequences from the 10 HEV-3 sub-genotypes, phylogenies were restricted to a fragment of ∼300 bp inside the previous set of the ORF 2-3 region, as previously described by Lu and collaborators.7 A total of 233 sequences were used. The BI was conducted as previously described for genotyping analyses except that MCMC were run for 10,000,000 iterations, associated model parameters was sampled every 1,000 generations and the initial 100,000 trees in each run were discarded as burning samples.
Date estimations.
The same set of GenBank sequences as the one for sub-typing analyses was used, except that we retained only sequences for which the year of sampling was available (N = 65). The Bayesian MCMC analyses were performed using BEAST v. 1.6.1 (http://beast.bio.ed.ac.uk) under a strict molecular clock setting. GTR + I + Γ were used, as proposed by jModelTest. An exponential-growth coalescent model was chosen as a prior on the tree. We ran a chain length of 100,000,000 by sampling trees every 1,000 generations. Convergence, Bayes factors, and burning were assessed using Tracer v1.4.1b (http://tree.bio.ed.ac.uk/software/tracer). The maximum clade credibility phylogeny for analyzing the MCMC data set was annotated by TreeAnotator in the BEAST package. The tree was visualized using FigTree v1.2.2. (http://tree.bio.ed.ac.uk/software/figtree/).
Statistical and spatial analyses.
For serological data from pigs, statistical analyses were performed in R software version 2.14.1.41 The χ2 test was run to test the significance of the differences observed in seroprevalence repartition by gender and to compare the human and pig spatial seroprevalence distributions by district and region. Confidence intervals (CIs) based on these variables were also determined. For human serological data, same analyses were used to compare prevalence by age, sex, and duration of activity in slaughterhouses. The Mantel-Haenszel test was used to carry out adjustment for age when testing the association between duration of activity and serological status. The χ2 test and confidence intervals for human variables were performed on STATA/IC11.1 (StataCorp, College Station, TX). Human and pig data were geographically displayed with ArcGIS 10.0 (ESRI, Redlands, CA).
Results
Seroprevalence to HEV in slaughterhouse workers.
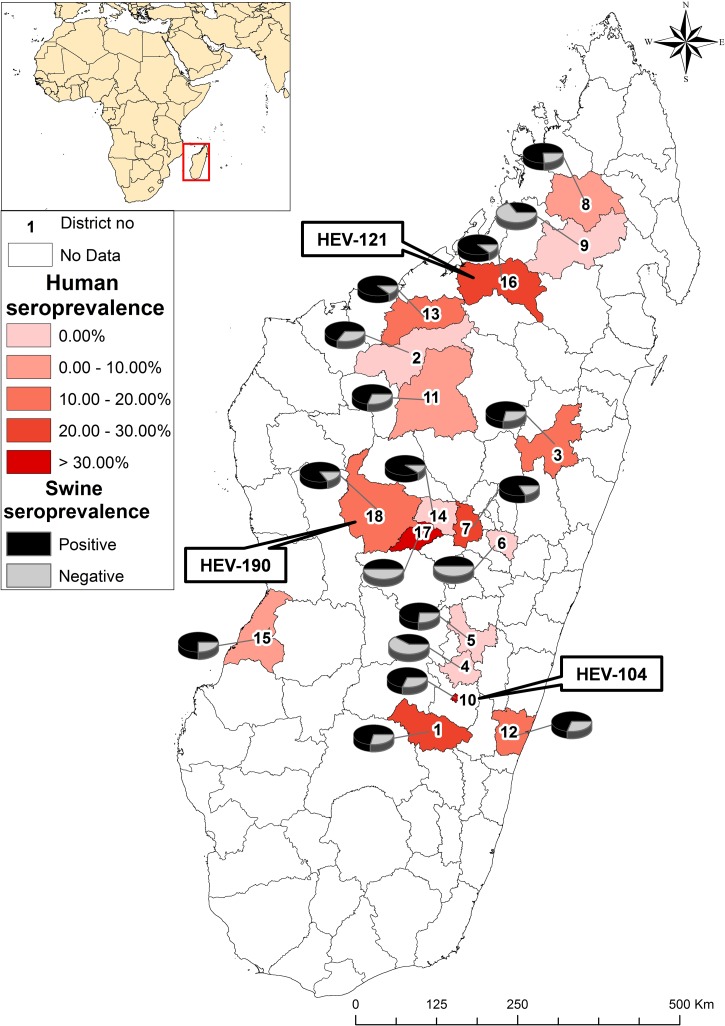
Of 427 human sera, 60 were positive for HEV, leading to a seroprevalence of 14.1%, (CI 95% [10.9–17.7]). There was no significant difference between age groups (22.2%, 10.5%, 14.1%, 15.9%, 14.6% in age groups < 20 years, 26–30 years, 30–40 years, 40–50 years, and 50–60 years, respectively, P value = 0.464) nor between males and females (13.4% and 20.5%, respectively, P value = 0.223). The seropositivity rates in slaughterhouse workers ranged from 5.3% (district of Bealanana, region of Sofia) to 31.4% (district of Fianarantsoa, region of Haute Matsiatra) (Table 2A, Figure 1). The duration of professional activity of workers in slaughterhouses before blood sampling was 11 years on average (CI 95% [1–56]). Seroprevalences are presented in Table 2B according to the age of workers and the duration of their professional activity. There was no significant difference between age groups for a given duration of activity (P value between 0.09 and 0.50). However, a significant difference was observed between people that worked for < 5 years, compared with those who worked for longer periods (P value = 0.03), suggesting a correlation between the time of exposure and the likelihood of infection irrespective of the workers age.
Table 2A.
Hepatitis E virus (HEV) seroprevalence among swine and slaughterhouse workers according to geographical repartition - HEV seroprevalence and confidence intervals (CI 95%) are expressed in percentage
| District (no) | Region | HEV seroprevalence according to district repartition (%) | HEV seroprevalence according to region repartition (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Human | Swine | Human | Swine | ||||||
| % | CI 95% | % | CI 95% | % | CI 95% | % | CI 95% | ||
| Ambatondrazaka (3) | Alaotra-Mangoro | 176 | 6.8–34.5 | 72.0 | 50.6–87.9 | 17.6 | 6.8–34.5 | 72.0 | 50.6–87.9 |
| Ambositra (5) | Amoron'i Mania | 0.0 | 0–13.7 | 73.7 | 48.8–90.9 | 0.0 | 0–13.7 | 73.7 | 48.8–90.9 |
| Andramasina (6) | Analamanga | 0.0 | 0–10.9 | 50.0 | 18.7–81.3 | 0.0 | 0–10.9 | 50.0 | 18.7–81.3 |
| Maevatanana (11) | Betsiboka | 7.7 | 0.2–36.0 | 70.0 | 34.8–93.3 | 7.7 | 0.2–36.0 | 70.0 | 34.8–93.3 |
| Ambato-Boina (2) | Boeny | 0.0 | 0–52.2 | 66.7 | 29.9–92.5 | 11.8 | 1.5–36.4 | 76.5 | 50.1–93.2 |
| Marovoay (13) | 16.7 | 2.1–48.4 | 87.5 | 47.3–99.7 | |||||
| Tsiroanomandidy (18) | Bongolava | 14.3 | 4.8–30.3 | 83.3 | 62.6–95.3 | 14.3 | 4.8–30.3 | 83.3 | 62.6–95.3 |
| Ambalavao (1) | Haute Matsiatra | 19.4 | 7.5–37.8 | 71.4 | 29.0–96.3 | 20.7 | 12.6–31.1 | 64.0 | 49.2–77.1 |
| Ambohimahasoa (4) | 0.0 | 0–18.5 | 40.0 | 12.2–73.8 | |||||
| Fianarantsoa Urban (10) | 33.3 | 18.0–51.9 | 69.7 | 51.3–84.4 | |||||
| Arivonimamo (7) | Itasy | 24.1 | 13.9–372 | 80.0 | 56.3–94.3 | 21.1 | 13.4–30.6 | 77.1 | 59.9–89.6 |
| Miarinarivo (14) | 0.0 | 0–18.5 | 88.9 | 51.8–99.7 | |||||
| Soavinandriana (17) | 31.6 | 19.2–74.9 | 50.0 | 11.8–88.2 | |||||
| Morondava (15) | Menabe | 6.9 | 0.8–22.8 | 75.0 | 34.9–96.8 | 6.9 | 0.8–22.8 | 75.0 | 34.9–36.8 |
| Bealanana (8) | Sofia | 5.3 | 13.3–26.0 | 76.0 | 54.9–90.6 | 10.6 | 3.5–23.1 | 69.0 | 52.9–82.4 |
| Befandriana-Nord (9) | 0.0 | 0–33.6 | 33.3 | 7.5–70.1 | |||||
| Port Berger (16) | 21.1 | 6.1–45.6 | 87.5 | 47.3–99.7 | |||||
| Manakara-Sud (12) | Vatovavy-Fitovinany | 11.1 | 1.4–34.7 | 70.0 | 34.8–93.3 | 11.1 | 1.4–34.7 | 70.0 | 34.8–93.3 |
Figure 1.
Geographical distribution of hepatitis E virus (HEV) seroprevalence in human and swine. Slaughterhouse workers HEV seroprevalence is displayed in red, and swine HEV seroprevalence with pie-charts. Location of virus-positive livers is mentioned in labels.
Table 2B.
Hepatitis E virus (HEV) seroprevalence among swine and slaughterhouse workers according to the duration of professional activity of workers
| Age of workers | Duration of activity | P value (a vs. b) | |
|---|---|---|---|
| < 5 years (a) | ≥ 5 years (b) | ||
| ≤ 20 | 14.29% (1/7) | 24.14% (7/29) | 0.503 |
| [20–35] | 3.70% (1/27) | 14.84% (27/182) | 0.091 |
| [35–50] | 5.56% (1/18) | 13.79% (16/116) | 0.294 |
| > 50 | 0.00% (0/5) | 16.28% (7/43) | 0.438 |
| Total | 5.26% (3/57) | 15.41% (57/370) | 0.03 |
Seroprevalence to HEV in swine populations.
Of 250 sera collected from pigs at the slaughterhouse, 178 tested positive for HEV. Seroprevalence was estimated at 71.2% (CI 95% [65.2–76.7]). There was no significant difference between male and female (72.1% and 70.5%, respectively, P value = 0.786). The highest seroprevalence in pigs was observed in the district of Mianarivo, region of Itasy (88.9% [51.8–99.7]), and the lowest in the district of Befandriana-Nord, region of Sofia (33.3% [7.5–70.1]) (Table 2A, Figure 1).
Spatial distribution of HEV seropositivity among swine and slaughterhouse workers.
All 18 districts covered by the study were found positive for infection in swine, whereas only 12 of them had evidence of infection in humans. There were significant differences between the spatial distributions of human and swine HEV seroprevalences when tested at the district and the region levels (P value < 0.0001, Table 2A).
Molecular detection of HEV in pig liver.
A total of 250 livers were collected from the same pigs, which were serologically tested. Only three livers (1.2%) were found positive for HEV viral RNA, namely swHEV-MG-104, swHEV-MG-121, and swHEV-MG-190 (GenBank accessions nos.: JX507128–130). The three livers were sampled in December 2010 (one male and two female pigs). Two of these pigs originated from the Fianarantsoa and Mianarivo districts (located in the central highlands of Madagascar), and the third one from the Port-Berger district in the north-west (Figure 1). Interestingly, these regions had the highest seroprevalence rates to swine HEV and the highest rates to human HEV in slaughterhouse workers (district of Fianarantsoa), reflecting a probably active viral circulation in swine with an elevated risk of infection in humans. Of note, two animals detected positive for HEV viral RNA were concomitantly seropositive to HEV.
Genotyping, sub-typing and phylogenetic analysis of HEV in Malagasy pigs.
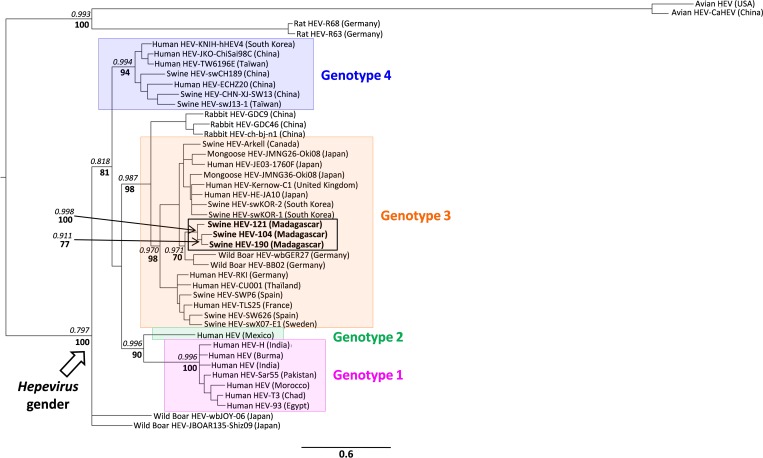
When compared with homologous sequences 2(ORF 2-3 sequences of 1-kb length) from human and swine HEV genotypes 1 to 4 deposited in the GenBank database the Malagasy HEV strains could be identified as genotype 3 (Figure 2). The three sequences branch together, forming a distinct group, with a high nodal support (posterior probability P = 0.998, ML bootstrap = 100). Within this group, swHEV-MG-104 and swHEV-MG-190 sequences fall into a sub-cluster supported by a high PP of 0.911 and a ML bootstra P value of 77 (Figure 2). Genetic distances between Malagasy HEV strains range between 7.4% (±0.97) and 9.8% (±1.09).
Figure 2.
Phylogenetic analysis of Malagasy hepatitis E virus (HEV) sequences based on a 1-kb fragment in the ORF 2-3. Bayesian analyses were used to fix tree topologies. Sequences are colored according their genotype (pink, green, orange, and blue for genotypes 1, 2, 3, and 4, respectively). Phylogenetic clusters containing Malagasy sequences are outlined. Only major nodal junctions are presented (at the origin of each genotype): Posterior probabilities (PP) in italic (P > 0.90) and, where nodes coincided, maximum likelihood bootstrap values (ML) in bold (ML > 70). Arrow marks established Hepevirus gender. Scale bar indicates the number of nucleotide substitution per site.
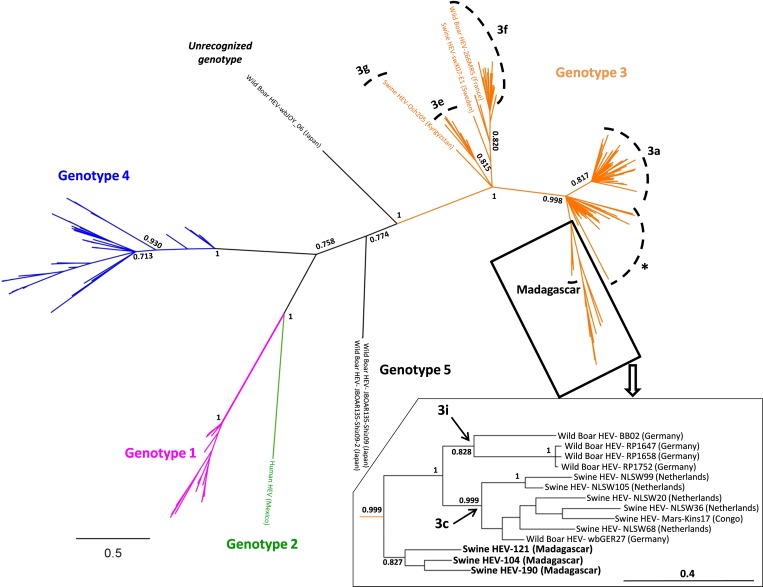
Sub-typing of the 3 HEV strains was performed by phylogenetic analysis of a small fragment (300 bp) of the ORF 2-3 region, as previously described.7 The Malagasy sequences also clustered in a distinct group, located at the root of clades formed by sub-genotypes 3c and 3i (Figure 3), with a strong nodal support (P = 0.827), suggesting a shared history between sub-genotypes 3c-, 3i-, and Malagasy-HEV. Table 3 shows the genetic distances between genotype 3 HEV sub-genotypes, as defined in Figure 3. Genetic distances between the Malagasy HEV clade and other sub-genotypes were in the same range as those observed between each other sub-type (15.6–22.4%), suggesting that the Malagasy HEV strains may form a distinct sub-genotype. It is most closely related to sub-type 3a (15.6%), and most distantly related to sub-type 3f (22.4%) according to the genetic distances.
Figure 3.
Bayesian phylogenetic analysis of Malagasy hepatitis E virus (HEV) sequences based on a 300 bp fragment in the ORF 2-3, as described by Lu and others.4 Sequences are colored according their genotype (pink, green, orange, and blue for genotypes 1, 2, 3, and 4, respectively). Phylogenetic clusters containing Malagasy sequences are outlined. Only major nodal junctions are presented: Posterior probabilities (PP) are noted in italic (P > 0.70). * Indicates a cluster with no clear sub-genotyping, including 3b- and 3d-HEV sequences. The HEV-3 sub-genotypes are mentioned in dashed lines. Inset: enlarged representation of Malagasy-, 3c- and 3i-HEV subtypes. Scale bar indicates the number of nucleotide substitution per site.
Table 3.
Estimates of evolutionary distances among hepatitis E virus (HEV)-3 sub-genotypes*
| 3a-HEV | 3c-HEV | 3e-HEV | 3f-HEV | 3g-HEV | 3i-HEV | Malagasy HEV | |
|---|---|---|---|---|---|---|---|
| 3a-HEV | – | 2.93% | 3.71% | 3.32% | 3.71% | 3.23% | 2.41% |
| 3c-HEV | 19.9% | – | 4.43% | 3.47% | 3.89% | 2.68% | 2.61% |
| 3e-HEV | 24.9% | 27.8% | – | 2.73% | 3.03% | 4.29% | 3.05% |
| 3f-HEV | 22.5% | 24.4% | 18.4% | – | 3.36% | 3.87% | 3.33% |
| 3g-HEV | 22.3% | 24.0% | 17.6% | 19.1% | – | 3.91% | 3.75% |
| 3i-HEV | 20.8% | 16.5% | 25.9% | 25.9% | 26.6% | – | 3.49% |
| Malagasy HEV | 15.6% | 17.1% | 20.3% | 22.4% | 22.0% | 19.3% | – |
Estimation of date of emergence of genotype 3 Malagasy HEV strains.
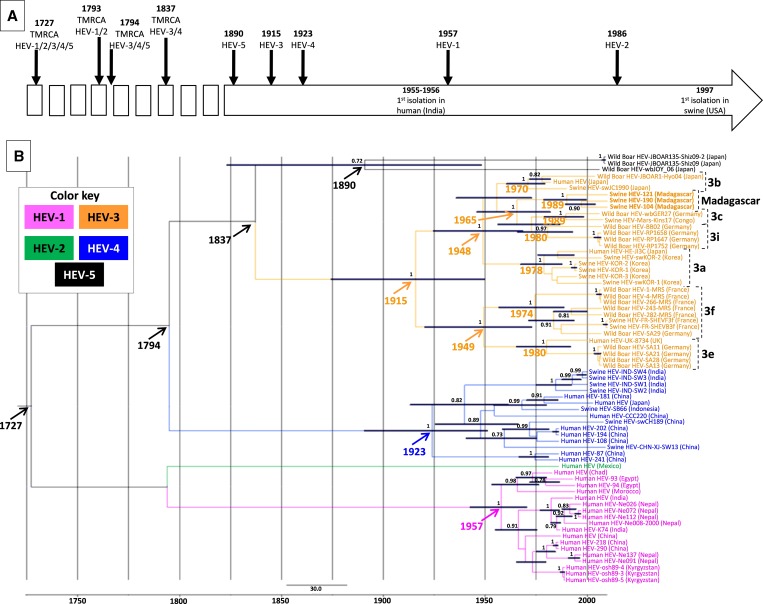
The Bayesian MCMC analysis estimates the time to the most recent common ancestor (TMRCA) of each genotype and sub-genotype, with a 95% highest probability density, and is presented in Figure 4. The resulting phylogenetic tree topology is the same as the one obtained by the Bayesian method for sub-typing (Figure 3). High posterior probabilities support the nodes defining each genotype and sub-type of HEV (P = 1.0 except for 3i-HEV for which P = 0.97). The TMRCA of HEV-3, HEV-4, HEV-1, and HEV-2 were estimated at 1915, 1923, 1957, and 1986, respectively. The estimated dates of emergence of the common ancestor of the Malagasy sub-type and the cluster formed by sub-types 3c and 3i was estimated to appear in 1965. The Malagasy HEV clade apparently diverged from the 3c-3i cluster around 1989. Interestingly, TMRCA of sub-type 3c is also estimated to emerge around 1989, suggesting that the common ancestor of sub-types 3c-, 3i-, and Malagasy-HEV had emerged in 1965, and then diversified in 3i-HEV around 1980 and in 3c- and Malagasy-HEV separate sub-types more recently, around 1989.
Figure 4.
Date estimations of hepatitis E virus (HEV) genotypes apparition and circulation. BEAST analysis is based on the fragment of 300 bp within ORF 2-3 of the 3 Malagasy HEV sequences and 65 globally representative GenBank sequences. Arrows indicate date positions. (A) Representation of the global diversification of HEV genotypes. Solid arrow represents the most recent common ancestor (TMRCA) for each defined genotype; dashed arrow represents TMRCA for non-distinct HEV genotype. (B) Sequences are colored by genotype (pink, green, orange, blue, and black for genotypes 1, 2, 3, 4, and 5, respectively). The HEV-3 sub-genotypes are mentioned in dashed lines. Standard deviation bars represent the 95% confidence interval of the mean estimated TMRCA. Scale bar indicates the number of years.
Discussion
Hepatitis E is widespread all over the world, both in human and swine populations. In industrialized countries, sporadic human infection mainly occurs by the consumption of contaminated food. In contrast, multiple routes of human contamination are operative in developing countries (such as Madagascar): poor hygiene environments, exposure to infected swine, or swine effluents.2,3 As humans may be infected by zoonotic or environmental routes, multiple HEV genotypes may circulate among human and swine populations.33,43,44 To investigate a possible swine-to-human route of infection, we report here the first sero- and viro-survey among slaughterhouse workers and swine populations in Madagascar.
Antibodies to HEV were detected in Malagasy slaughterhouse workers with a global prevalence of 14.1%. Previous studies have identified workers in slaughterhouses and pig handlers as populations at high risk of infection, because of their frequent contacts with organs, manure, and blood from animals.45,46 In Madagascar, we found that HEV seroprevalence among slaughterhouse workers reached 33.3% in the district of Fianarantsoa, but the average seropositivity (14.1%) could be considered as modest when compared with other studies. Indeed, studies in Spain,47 Germany,48 Switzerland,49 and in the United States24,50 have shown that HEV seroprevalence in exposed human populations, such as veterinarians and slaughterhouse workers, can reach more than 35%, whereas in non-exposed humans (i.e., blood donors) the seroprevalence is significantly lower. Further studies are needed to measure the seroprevalence of HEV in the Malagasy general population, and to determine if pig breeders are at higher risk of contamination. Indeed, in developing countries, several routes that are not linked to a direct contact with infected swine are commonly described for human contamination with HEV. In a resource-poor country, contamination of village water sources by HEV51 or human-to-human HEV transmission are possible routes, but in-depth analysis of the natural history of the disease and identification of associated risk factors are still lacking.
Our study shows that HEV circulates in Madagascar within the pig population, which strongly supports the role of an animal-to-human cycle in the country. A high seroprevalence rate of 71.2% on the average was found in pigs. Large differences were observed between districts (seroprevalences ranging from 33.3% to 88.9%) and regions (from 50.0% to 83.3%); however, because no traceability is operational in Madagascar to identify the individual pig farm at its source, no solid conclusion could be drawn with regard to the geographical distribution of HEV in the country, or the related on-farm risk factors. Hence, further studies targeting breeding areas are needed to more precisely measure the rates of infection and HEV burden in herds, and identify risks factors of contamination. Interestingly, because pigs fed on kitchen residue were recently reported to be more frequently infected than those fed on complete feed,52 on-farm practices, especially in animal feeding and hygiene management, need to be considered to promote biosecurity measures adapted to the Malagasy context.
In Madagascar, we found more than 70% of pigs sampled in slaughterhouses were seropositive for HEV, but that only 1.2% of livers were detected RNA virus positive. This relatively low level of ongoing viral infection in pigs may be caused by the age of swine at which the animals are slaughtered. In fact, pigs are usually infected during the early stages of the breeding (3–4 months of age), and the viral load in organs and feces are higher in younger animals, as previously reported.53,54 In Madagascar, pigs are usually slaughtered at older ages (6 to 12 months), and one may consider that only a few pigs remain infectious at that age.2 Therefore, pig farm breeders might be more exposed to HEV infection than slaughterhouse workers, as noted by Geng.55
Phylogenetic analyses revealed that genotype 3 HEV is circulating among swine populations in Madagascar. Recent studies21,56 have shown that HEV isolate TLS40 (GenBank accession no. EU495232) is at the root of sub-types 3c and 3i, as our Malagasy sequences. Unfortunately, we were not able to cluster this strain with the Malagasy HEV (data not shown), or to classify the Malagasy strains within an already known sub-genotype, probably caused by the shortness of the sequences used for this analysis. Full-genome analysis may allow us to determine whether the Malagasy HEV strains may form a new sub-type, and to better understand the origins of these strains.
Nakano and others57 recently estimated the TMRCA of HEV genotypes and sub-genotypes. Our observations slightly differ from theirs, probably caused by different sequences used in the data set. We estimated the divergence of strictly human HEV (genotypes 1 and 2) and zoonotic HEV (genotypes 3, 4, and 5) to be in 1794. Then in 1837, genotype 4-HEV diverge from genotypes 3–5 clusters. Interestingly, genotype 4 is mainly found in Asian countries, and not in Old (Europe and Africa) or New World countries. We estimated the emergence of genotype 3-HEV around 1915 and that of the Malagasy HEV around 1989. Moreover, a clear diversification of genotype 3 seems to have occurred after the 70s (TMRCA of sub-types 3b, 3f, 3a, 3e, 3i, 3c estimated to appear in 1970, 1974, 1978, 1980, 1980, and 1989, respectively). The phylogenetic cluster formed by 3c-, 3i-, and Malagasy-HEV sub-types is composed by sequences originating from Europe and Africa. After 1965 (date of emergence of TMRCA of this cluster), a diversification occurred and resulted in a distinct European 3i-HEV sub-type, and two other groups formed by sequences both from Europe and Africa (3c-HEV and Malagasy-HEV). Because international commercial exchanges and importation of live animals have been regularly reported from Europe (France, Germany, Belgium) since the 60s, and because few animals were recently imported in Madagascar since the late 90s, our findings suggests that the HEV strains circulating in Madagascar may have a common history with European and African HEV strains.
Our study is the first reported so far on HEV infection in humans and swine in Madagascar, and the circulation of the virus in swine. The HEV strains circulating in Madagascar among pigs are of genotype 3 and may have a common history with European and African HEV strains. Further studies are in preparation to explore the role of environmental contamination, the role of other transmission routes, and the role of the wild fauna in the viral cycle.
ACKNOWLEDGMENTS
We deeply thank the technical staffs of the FOFIFA-DRZV, and especially Samuel Rakotonindrina, for their invaluable work in pig slaughterhouses. We are grateful to Jean Théophile Rafisandrantantsoa, Institute Pasteur of Madagascar, from the Virology Unit, for his involvement in the serological analysis. Equally, we thank warmly Elodie Barnaud, ANSES Maison-Alfort, for her technical assistance. We also thank D. A. Wilkinson for proofreading the text.
Footnotes
Financial support: The main financial support was provided by the Regional Council of La Réunion, the European Regional development Funds (ERDF) and French Government through the QualiREG research network in Indian Ocean (www.qualireg.org). We are grateful to Institut Pasteur in Madagascar for funding the human study component. We warmly thank the French Agency for Food, Environmental and Occupational Health & Safety (ANSES) for funding the serological analysis work in swine.
Authors' addresses: Sarah Temmam, Centre de Recherche et de Veille sur les Maladies Émergentes dans l'Océan Indien (CRVOI), Plateforme de Recherche CYROI, Sainte Clotilde, La Réunion, France, and CNRS, UMR5557 Ecologie Microbienne, Lyon, France, E-mail: s.temmam@cyroi.fr. Lydia Besnard, Coralie Foray, and Eric Cardinale, Centre de Recherche et de Veille sur les Maladies Émergentes dans l'Océan Indien (CRVOI), Plateforme de Recherche CYROI, Sainte Clotilde, La Réunion, France, and International Center for Agronomical Research for Development (CIRAD), UMR15 CMAEE, Saint Denis, La Réunion, France, E-mails: lydiabesnard@gmail.com, coralie.foray@cirad.fr, and eric.cardinale@cirad.fr. Soa Fy Andriamandimby and Jean-Michel Héraud, Institut Pasteur de Madagascar, Virology Unit, Antaananarivo, Madagascar, E-mails: soafy@pasteur.mg and jmheraud@pasteur.mg. Harentsoaniaina Rasamoelina-Andriamanivo, FOFIFA, Department of Veterinary and Husbandry Research, Ministry of Agriculture, Antananarivo, Madagascar, E-mail: harena23@yahoo.fr. Koussay Dellagi and Hervé Pascalis, Centre de Recherche et de Veille sur les Maladies Émergentes dans l'Océan Indien (CRVOI), Plateforme de Recherche CYROI, Sainte Clotilde, La Réunion, France, and Institut de Recherche pour le Développement (IRD), Saint Denis, La Réunion, France, E-mails: koussay.dellagi@ird.fr and herve.pascalis@ird.fr. Nicole Pavio, ANSES, Maisons-Alfort, France, E-mail: npavio@vet-alfort.fr. Vincent Porphyre, International Center for Agronomical Research for Development (CIRAD), UMR112 SELMET, Saint Pierre, La Réunion, France, E-mail: vincent.porphyre@cirad.fr.
References
- 1.Meng XJ, Anderson DA, Arankalle VA, Emerson SU, Harrison TJ, Jameel S, Okamoto H. Family Hepeviridae. In: King AM, Carstens EB, Lefkowitz EJ, editors. Virus Taxonomy: 9th Report of the International Committee on Taxonomy of Viruses. San Diego, CA: Elsevier; 2011. pp. 1021–1028. [Google Scholar]
- 2.Purcell RH, Emerson SU. Hidden danger: the raw facts about hepatitis. E virus. J Infect Dis. 2010;202:819–821. doi: 10.1086/655900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pavio N, Meng X-J, Renou C. Zoonotic hepatitis E: animal reservoirs and emerging risks. Vet Res. 2010;41:46. doi: 10.1051/vetres/2010018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang W, Shen Q, Hua X, Cui L. Novel hepatitis E virus genotype in Norway rats, Germany. Emerg Infect Dis. 2011;17:1981–1983. doi: 10.3201/eid1710.101399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cossaboom C, Córdoba L, Dryman B, Meng X-J. Hepatitis E virus in rabbits, Virginia, USA. Emerg Infect Dis. 2011;17:2047–2049. doi: 10.3201/eid1711.110428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Colson P, Borentain P, Queyriaux B, Kaba M, Moal V, Gallian P, Heyries L, Raoult D, Gerolami R. Pig liver sausage as a source of hepatitis E virus transmission to humans. J Infect Dis. 2010;202:825–834. doi: 10.1086/655898. [DOI] [PubMed] [Google Scholar]
- 7.Lu L, Li C, Hagedorn CH. Phylogenetic analysis of global hepatitis E virus sequences: genetic diversity, subtypes and zoonosis. Rev Med Virol. 2006;16:5–36. doi: 10.1002/rmv.482. [DOI] [PubMed] [Google Scholar]
- 8.Johne R, Heckel G, Plenge-Bönig A, Kindler E, Maresch C, Reetz J, Schielke A, Ulrich R. Novel hepatitis E virus genotype in Norway rats, Germany. Emerg Infect Dis. 2010;16:1452–1455. doi: 10.3201/eid1609.100444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Haqshenas G, Shivaprasad HL, Woolcock PR, Read DH, Meng X. Genetic identification and characterization of a novel virus related to human hepatitis E virus from chickens with hepatitis-splenomegaly syndrome in the United States. J Gen Virol. 2001;82:2449–2462. doi: 10.1099/0022-1317-82-10-2449. [DOI] [PubMed] [Google Scholar]
- 10.Marek A, Bilic I, Prokofieva I, Hess M. Phylogenetic analysis of avian hepatitis E virus samples from European and Australian chicken flocks supports the existence of a different genus within the Hepeviridae comprising at least three different genotypes. Vet Microbiol. 2010;145:54–61. doi: 10.1016/j.vetmic.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 11.Zhao Q, Zhou EM, Dong SW, Qiu HK, Zhang L, Hu SB, Zhao FF, Jiang SJ, Sun YN. Analysis of avian hepatitis E virus from chickens, China. Emerg Infect Dis. 2010;16:1469–1472. doi: 10.3201/eid1609.100626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Drexler JF, Seelen A, Corman VM, Fumie Tateno A, Cottontail V, Melim Zerbinati R, Gloza-Rausch F, Klose SM, Adu-Sarkodie Y, Oppong SK, Kalko EK, Osterman A, Rasche A, Adam A, Müller MA, Ulrich RG, Leroy EM, Lukashev AN, Drosten C. Bats worldwide carry hepatitis E-related viruses that form a putative novel genus within the family Hepeviridae. J Virol. 2012;86:9134–9147. doi: 10.1128/JVI.00800-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Satou K, Nishiura H. Transmission dynamics of hepatitis E among swine: potential impact upon human infection. BMC Vet Res. 2007;3:9. doi: 10.1186/1746-6148-3-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rose N, Lunazzi A, Dorenlor V, Merbah T, Eono F, Eloit M, Madec F, Pavio N. High prevalence of Hepatitis E virus in French domestic pigs. Comp Immunol Microbiol Infect Dis. 2011;34:419–427. doi: 10.1016/j.cimid.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 15.Montalvo Villalba M, Lay L, Chandra V, Bello Corredor M, Frometa S, Moreno A, Jameel SM. Hepatitis E virus genotype 1, Cuba. Emerg Infect Dis. 2008;14:1320–1322. doi: 10.3201/eid1408.080049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Despierres L-A, Kaphan E, Attarian S, Cohen-Bacrie S, Pelletier J, Pouget J, Motte A, Charrel R, Gerolami R, Colson P. Neurologic disorders and hepatitis E, France. Emerg Infect Dis. 2010;17:1510–1512. doi: 10.3201/eid1708.102028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Escribà J, Nakoune E, Recio C, Massamba P-M, Matsika-Claquin M, Goumba C, Rose AM, Nicand E, García E, Leklegban C, Koffi B. Hepatitis E, Central African Republic. Emerg Infect Dis. 2008;14:681–683. doi: 10.3201/eid1404.070833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lewis H, Boisson S, Ijaz S, Hewitt K, Ngui S, Boxall E, Teo CG, Morgan D. Hepatitis E in England and Wales. Emerg Infect Dis. 2008;14:165–167. doi: 10.3201/eid1401.070307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li R-C, Ge S-X, Li Y-P, Zheng Y-J, Nong Y, Guo Q-S, Zhang J, Ng M, Xia N. Seroprevalence of hepatitis E virus infection, rural southern People's Republic of China. Emerg Infect Dis. 2006;12:1682–1688. doi: 10.3201/eid1211.060332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rutjes S, Lodder W, Lodder-Verschoor F, van den Berg H, Vennema H, Duizer E, Koopmans M, de Roda Husman AM. Sources of hepatitis E virus genotype 3 in the Netherlands. Emerg Infect Dis. 2009;15:381–387. doi: 10.3201/eid1503.071472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Legrand-Abravanel F, Mansuy JM, Dubois M, Kamar N, Peron JM, Rostaing L, Izopet J. Hepatitis E virus genotype 3 diversity, France. Emerg Infect Dis. 2009;15:110–114. doi: 10.3201/eid1501.080296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Purcell RH, Emerson SU. Hepatitis E: an emerging awareness of an old disease. J Hepatol. 2008;48:494–503. doi: 10.1016/j.jhep.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 23.Boccia D, Guthmann J, Klovstad H, Hamid N, Tatay M, Ciglenecki I, Nizou J, Nicand E, Guerin P. High mortality associated with an outbreak of hepatitis E among displaced persons in Darfur, Sudan. Clin Infect Dis. 2006;42:1679–1684. doi: 10.1086/504322. [DOI] [PubMed] [Google Scholar]
- 24.Meng XJ, Wiseman B, Elvinger F, Guenette DK, Toth TE, Engle RE, Emerson SU, Purcell RH. Prevalence of antibodies to hepatitis E virus in veterinarians working with swine and in normal blood donors in the United States and other countries. J Clin Microbiol. 2002;40:117–122. doi: 10.1128/JCM.40.1.117-122.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pérez-Gracia M, Mateos M, Galiana C, Fernández-Barredo S, García A, Gómez M, Moreira V. Autochthonous hepatitis E infection in a slaughterhouse worker. Am J Trop Med Hyg. 2007;77:893–896. [PubMed] [Google Scholar]
- 26.Di Martino B, Di Profio F, Martella V, Di Felice E, Di Francesco C, Ceci C, Marsilio F. Detection of hepatitis E virus in slaughtered pigs in Italy. Arch Virol. 2010;155:103–106. doi: 10.1007/s00705-009-0544-0. [DOI] [PubMed] [Google Scholar]
- 27.Epelboin L, Nicand E, Roussin C, Lernout T, Pettinelli M-E, Tesse S, Ali R, Aubry P. A sporadic case of genotype 3f hepatitis E in Mayotte. Med Mal Infect. 2011;41:392–394. doi: 10.1016/j.medmal.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 28.Nicand É, Bigaillon C, Tessé S. Hepatitis E in France: surveillance data for human cases, 2006–2008. Bull Épidémiol Hebd. 2009;31–32:337–342. [Google Scholar]
- 29.Milon A. Hépatite E à la Réunion. Bull Soc Pathol Exot. 2004;96:149–150. [Google Scholar]
- 30.Barnaud E, Rogee S, Garry P, Rose N, Pavio N. Thermal inactivation of infectious hepatitis e virus in experimentally contaminated food. Appl Environ Microbiol. 2012;78:5153–5159. doi: 10.1128/AEM.00436-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jothikumar N, Cromeans TL, Robertson BH, Meng XJ, Hill VR. A broadly reactive one-step real-time RT-PCR assay for rapid and sensitive detection of hepatitis E virus. J Virol Methods. 2006;131:65–71. doi: 10.1016/j.jviromet.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 32.Gyarmati P, Mohammed N, Norder H, Blomberg J, Belák S, Widén F. Universal detection of hepatitis E virus by two real-time PCR assays: TaqMan and Primer-Probe Energy Transfer. J Virol Methods. 2007;146:226–235. doi: 10.1016/j.jviromet.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 33.Cooper K, Huang FF, Batista L, Rayo CD, Bezanilla JC, Toth TE, Meng XJ. Identification of genotype 3 hepatitis E virus (HEV) in serum and fecal samples from pigs in Thailand and Mexico, where genotype 1 and 2 HEV strains are prevalent in the respective human populations. J Clin Microbiol. 2005;43:1684–1688. doi: 10.1128/JCM.43.4.1684-1688.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kearse M, Moir R, Wilson A, Stones-Havas S, Cheung M, Sturrock S, Buxton S, Cooper A, Markowitz S, Duran C, Thierer T, Ashton B, Meintjes P, Drummond A. Geneious basic: an integrated and extendable desktop software platform for the organization and analysis of sequence data. Bioinformatics. 2012;28:1647–1649. doi: 10.1093/bioinformatics/bts199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Edgar RC. MUSCLE: a multiple sequence alignment method with reduced time and space complexity. BMC Bioinformatics. 2004;5:113. doi: 10.1186/1471-2105-5-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Posada D. jModelTest: phylogenetic model averaging. Mol Biol Evol. 2008;25:1253–1256. doi: 10.1093/molbev/msn083. [DOI] [PubMed] [Google Scholar]
- 37.Tamura K, Peterson D, Peterson N, Stecher G, Nei M, Kumar S. MEGA5: molecular evolutionary genetics analysis using maximum likelihood, evolutionary distance, and maximum parsimony methods. Mol Biol Evol. 2011;28:2731–2739. doi: 10.1093/molbev/msr121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tajima F, Nei M. Estimation of evolutionary distance between nucleotide sequences. Mol Biol Evol. 1984;1:269–285. doi: 10.1093/oxfordjournals.molbev.a040317. [DOI] [PubMed] [Google Scholar]
- 39.Guindon S, Gascuel O. A simple, fast, and accurate algorithm to estimate large phylogenies by maximum likelihood. Syst Biol. 2003;52:696–704. doi: 10.1080/10635150390235520. [DOI] [PubMed] [Google Scholar]
- 40.Ronquist F, Huelsenbeck JP. MrBayes 3: Bayesian phylogenetic inference under mixed models. Bioinformatics. 2003;19:1572–1574. doi: 10.1093/bioinformatics/btg180. [DOI] [PubMed] [Google Scholar]
- 41.R Development Core Team . Vienna: 2008. R: a language and environment for statistical computing.http://www.r-project.org Available at. Accessed January 22, 2012. [Google Scholar]
- 42.Tajima F, Nei M. Estimation of evolutionary distance between nucleotide sequences. Mol Biol Evol. 1984;1:269–285. doi: 10.1093/oxfordjournals.molbev.a040317. [DOI] [PubMed] [Google Scholar]
- 43.Vivek R, Kang G. Hepatitis E virus infections in swine and swine handlers in Vellore, southern India. Am J Trop Med Hyg. 2011;84:647–649. doi: 10.4269/ajtmh.2011.10-0456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang W, Yang S, Ren L, Shen Q, Cui L, Fan K, Huang F, Kang Y, Shan T, Wei J, Xiu H, Lou Y, Liu J, Yang Z, Zhu J, Hua X. Hepatitis E virus infection in central China reveals no evidence of cross-species transmission between human and swine in this area. PLoS ONE. 2009;4:e8156. doi: 10.1371/journal.pone.0008156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Perez-Gracia MT, Mateos ML, Galiana C, Fernandez-Barredo S, Garcia A, Gomez MT, Moreira V. Autochthonous hepatitis E infection in a slaughterhouse worker. Am J Trop Med Hyg. 2007;77:893–896. [PubMed] [Google Scholar]
- 46.Adjei AA, Aviyase JT, Tettey Y, Adu-Gyamfi C, Mingle JA, Ayeh-Kumi PF, Adiku TK, Gyasi RK. Hepatitis E virus infection among pig handlers in Accra, Ghana. East Afr Med J. 2009;86:359–363. doi: 10.4314/eamj.v86i8.54155. [DOI] [PubMed] [Google Scholar]
- 47.Galiana C, Fernandez-Barredo S, Garcia A, Gomez MT, Perez-Gracia MT. Occupational exposure to hepatitis E virus (HEV) in swine workers. Am J Trop Med Hyg. 2008;78:1012–1015. [PubMed] [Google Scholar]
- 48.Krumbholz A, Mohn U, Lange J, Motz M, Wenzel JJ, Jilg W, Walther M, Straube E, Wutzler P, Zell R. Prevalence of hepatitis E virus-specific antibodies in humans with occupational exposure to pigs. Med Microbiol Immunol (Berl) 2012;201:239–244. doi: 10.1007/s00430-011-0210-5. [DOI] [PubMed] [Google Scholar]
- 49.Kaufmann A, Kenfak-Foguena A, Andre C, Canellini G, Burgisser P, Moradpour D, Darling KE, Cavassini M. Hepatitis E virus seroprevalence among blood donors in southwest Switzerland. PLoS ONE. 2011;6:e21150. doi: 10.1371/journal.pone.0021150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Withers MR, Correa MT, Morrow M, Stebbins ME, Seriwatana J, Webster WD, Boak MB, Vaughn DW. Antibody levels to hepatitis E virus in North Carolina swine workers, non-swine workers, swine, and murids. Am J Trop Med Hyg. 2002;66:384–388. doi: 10.4269/ajtmh.2002.66.384. [DOI] [PubMed] [Google Scholar]
- 51.Toole MJ, Claridge F, Anderson DA, Zhuang H, Morgan C, Otto B, Stewart T. Hepatitis E virus infection as a marker for contaminated community drinking water sources in Tibetan villages. Am J Trop Med Hyg. 2006;74:250–254. [PubMed] [Google Scholar]
- 52.Xiao P, Li R, She R, Yin J, Li W, Mao J, Sun Q. Prevalence of hepatitis E virus in swine fed on kitchen residue. PLoS ONE. 2012;7:e33480. doi: 10.1371/journal.pone.0033480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Di Bartolo I, Martelli F, Inglese N, Pourshaban M, Caprioli A, Ostanello F, Ruggeri FM. Widespread diffusion of genotype 3 hepatitis E virus among farming swine in Northern Italy. Vet Microbiol. 2008;132:47–55. doi: 10.1016/j.vetmic.2008.04.028. [DOI] [PubMed] [Google Scholar]
- 54.Nakai I, Kato K, Miyazaki A, Yoshii M, Li TC, Takeda N, Tsunemitsu H, Ikeda H. Different fecal shedding patterns of two common strains of hepatitis E virus at three Japanese swine farms. Am J Trop Med Hyg. 2006;75:1171–1177. [PubMed] [Google Scholar]
- 55.Geng J, Wang L, Wang X, Fu H, Bu Q, Liu P, Zhu Y, Wang M, Sui Y, Zhuang H. Potential risk of zoonotic transmission from young swine to human: seroepidemiological and genetic characterization of hepatitis E virus in human and various animals in Beijing, China. J Viral Hepat. 2011;18:583–590. doi: 10.1111/j.1365-2893.2011.01472.x. [DOI] [PubMed] [Google Scholar]
- 56.Adlhoch C, Wolf A, Meisel H, Kaiser M, Ellerbrok H, Pauli G. High HEV presence in four different wild boar populations in East and West Germany. Vet Microbiol. 2009;139:270–278. doi: 10.1016/j.vetmic.2009.06.032. [DOI] [PubMed] [Google Scholar]
- 57.Nakano T, Takahashi K, Pybus OG, Hashimoto N, Kato H, Okano H, Kobayashi M, Fujita N, Shiraki K, Takei Y, Ayada M, Arai M, Okamoto H, Mishiro S. New findings regarding the epidemic history and population dynamics of Japan-indigenous genotype 3 hepatitis E virus inferred by molecular evolution. Liver Int. 2012;32:675–688. doi: 10.1111/j.1478-3231.2011.02728.x. [DOI] [PubMed] [Google Scholar]