Abstract
Objective
To investigate the protective effects of c-Jun N-terminal kinase (JNK)–1 and -2 gene knockout (KO) on the corneal epithelial response to desiccating stress.
Methods
The C57BL/6, JNK1KO, and JNK2KO mice were subjected to desiccating stress (DS) for 5 days. The effects of DS on the corneal epithelium were evaluated by measuring corneal smoothness and permeability. Expression of matrix metalloproteinases (MMP)–1, MMP-9, and cornified envelope protein precursors (small prolinerich protein [SPRR]–1a, SPRR-2a, and involucrin) in the corneal epithelia was evaluated by immunostaining and real-time polymerase chain reaction. Collagenase and gelatinase activity in corneal sections as measured with in situ fluorescent assays.
Results
The JNK2KO mice had smoother corneal surfaces and less corneal barrier disruption in response to DS than JNK1KO mice and C57BL/6 wild-type control mice. The DS increased levels of MMP-1, MMP-9, SPRR-1a, SPRR-2a, involucrin immunoreactivity, and mRNA transcripts in the corneal epithelium of JNK1KO and C57BL/6 mice, but not in JNK2KO mice. Knockout of JNK2 prevented DS-induced increase in gelatinase and collagenase activity in the cornea.
Conclusion
The JNK2 protein appears to have an essential role in desiccation-induced corneal epithelial disease by stimulating production of MMP-1, MMP-9, and cornified envelope precursors.
Clinical Relevance
The JNK2 protein could be a novel therapeutic target in dry eye disease.
Dry eye is a common disease.1 The prevalence of dry eye increases with age,2 with a prevalence of 6% at 40 years of age, increasing to 15% to 25% in the population older than 65 years.3,4 Dry eye is accompanied by symptoms of eye irritation and blurred vision. Dry eye can have a significant effect on quality of life by decreasing functional vision and impairing the execution of daily tasks such as driving, reading, and watching television.5-8 Dry eye is often accompanied by pathologic changes in the ocular surface epithelium, with increased corneal permeability to fluorescein and conjunctival metaplasia and goblet cell loss.
We have previously found that dry eye and desiccating stress stimulate production of metalloproteinase (MMP)–9, as well as other MMPs, by the ocular surface epithelia.9-12 Metalloproteinase 9 was found to degrade the tight-junction protein occludin and to disrupt apical epithelial barrier function in the cornea.9 Furthermore, MMP-9 knockout mice were found to be resistant to the corneal ocular epithelial disease that develops in response to dry eye.9
We hypothesize that activation of mitogen-activated protein kinase (MAPK) intracellular signaling pathways by the desiccating and hyperosmolar stress of dry eye is another possible cause of the observed corneal epithelial pathology. The MAPK cascades are well-conserved signaling pathways that include 3 subtypes: the stress-responsive c-Jun N-terminal kinase/stress-activated protein kinases (JNK/SAPK), extracellular signal–regulated kinases and p38 MAPK. Extracellular signal–regulated kinase MAPKs have been reported to modulate barrier function, increasing transepithelial electrical resistance in human cultured epithelial cells.13 Other MAPKs, such as JNK, have been reported to stimulate production of cornified envelope proteins such as involucrin in the corneal epithelium.14 These kinase signaling pathways also regulate the expression of cytokines and MMPs (MMP-9, -1, -3, and -13).15-20
A hallmark of dry eye is poor wettability of the ocular surface and tear film instability. This may be due in part to reduced production of mucins by the ocular surface epithelia, but clinical and histological evidence suggests that this may be a shift toward a cornified envelope phenotype by the ocular surface epithelia.21
The purpose of this study was to determine if the corneal epithelial response to experimental desiccating stress (DS) would be ameliorated in mice genetically deficient in JNK SAPKs by evaluating corneal permeability and expression of MMPs and cornified envelope protein precursors.
METHODS
ANIMAL MODEL OF DRY EYE
This research protocol was approved by the Baylor College of Medicine Center for Comparative Medicine (Institutional Animal Care and Use Committe), and it conformed to the standards in the Association for Research in Vision and Ophthalmology Statement for the Use of Animals in Ophthalmic and Vision Research.
The JNK1 (B6.129S1-Mapk8tm1Flv/J) and JNK2 (B6.129S2-Mapk9tm1Flv/J) knockout (KO) mice in a C57BL/6 background and wild-type C57BL/6 mice were purchased from Jackson Laboratories (Bar Harbor, Maine) to establish breeding colonies. The genotype of JNK1KO and JNK2KO mice was confirmed according to the Jackson Laboratories protocol (data not shown). The C57BL/6 wild-type control mice were also purchased from Jackson Laboratories. Mice were used at 8 weeks of age.
Desiccating stress was induced by subcutaneous injection of scopolamine hydrobromide (0.5 mg/0.2 mL; Sigma-Aldrich, St Louis, Missouri) 4 times a day, alternating between the left and right flanks of the above 3 strains, as previously described, for 5 consecutive days (DS5).10,21-23 Mice were placed in modified cages with a perforated plastic screen on one side to allow airflow from a fan placed 6 in in front of them for 16 h/d. Room humidity was maintained at 30% to 35%. This model of dry eye disease has been used previously, with no discernible ill effects from the scopolamine treatment or low humidity.23,24 Control mice were kept in a nonstressed (NS) environment maintained at 50% to 75% relative humidity without exposure to forced air. Thirty-five animals per strain (JNK1KO, JNK2KO, and C57BL/6) per time point (NS and DS5) were used; 5 mice were used for histology sections, 10 for evaluation of corneal permeability, and 20 for gene analysis. Evaluation of corneal smoothness was performed on the same mice that were used for evaluating gene expression.
CORNEAL PERMEABILITY
Corneal epithelial permeability to Oregon green dextran (OGD) (70 000 molecular weight [MW]; Invitrogen, Eugene, Oregon) was assessed in the NS and DS5 groups of the 3 strains (10 mice per group per experiment; 3 sets of experiments). Briefly, 0.5 μL of 50 μg/mL OGD was instilled onto the ocular surface 1 minute before euthanasia. Corneas were rinsed with phosphate-buffered saline and photographed with a stereoscopic zoom microscope (SMZ 1500; Nikon, Melville, New York) under fluorescence excitation at 470 nm. The severity of corneal OGD staining was graded in digital images in the 2-mm central corneal zone of each eye by 2 masked observers (C.S.D.P. and S.B.P.) using the MetaVue 6.24r software (Molecular Devices, Sunnyvale, California). The mean intensity measured inside this central zone, generated by the software, was transferred to a database, and the results were averaged within each group. Results are presented as mean(standard deviation) in gray levels.
EVALUATION OF CORNEAL SMOOTHNESS
Corneal smoothness was assessed in 30 eyes of the NS and DS5 of the 3 strains of mice in 3 sets of experiments, as previously described.21 Smoothness of images, taken by a stereoscopic zoom microscope fiber optic ring illuminator (SMZ 1500; Nikon), that were reflected off of the corneal surface was graded in digital images by 2 masked observers and averaged within each group. The reflected ring was divided into quadrants of 3 clock hours each. The corneal irregularity severity score was calculated using a 5-point scale based on the number of distorted quadrants in the reflected ring: 0, no distortion; 1, distortion in 1 quadrant of the ring (3 clock hours); 2, distortion in 2 quadrants (6 clock hours); 3, distortion in 3 quadrants (9 clock hours); 4, distortion in all 4 quadrants (12 clock hours); and 5, severe distortion, in which no ring could be recognized. Results are presented as mean(standard deviation).
IMMUNOFLUORESCENT STAINING AND LASER SCANNING CONFOCAL MICROSCOPY
Metalloproteinases 1 and 9, small proline-rich proteins 1a and 2a (SPRR-1a and SPRR-2a, respectively), and involucrin were evaluated by laser scanning confocal microscopy in tissue sections. The eyes and adnexa of mice from each strain per time point (n=5) were excised, embedded in optimal cutting temperature (OCT compound; VWR, Suwanee, Georgia), and flash frozen in liquid nitrogen. Sagittal 8-μm sections were cut with a cryostat (HM 500; Micron, Waldorf, Germany) and placed on glass slides that were stored at -80°C.
Cryosections stained for MMP-1, MMP-9 (1:100; Chemicon-Millipore, Billerica, Massachusetts), SPRR-1a (1:100; Abcam, Cambridge, Massachusetts), SPRR-2a (1:100, neat serum; Alexis Bio-chemicals, San Diego, California) and involucrin (1:20; Santa Cruz Biotechnology, Santa Cruz, California) were developed using appropriated Alexa-Fluor 488 conjugated IgG antibodies, as previously described.21,25 Negative controls were performed at the same time and consisted of sections incubated with an isotype control antibody or sections with omitted primary antibody. Cryosections digital images (512 × 512 pixels) were captured with a laser-scanning confocal microscope (LSM 510; Zeiss with kryptonargon and He-Ne laser; Carl Zeiss Meditec, Ltd, Thornwood, New York) with 488-excitation and 543-nm emission filters, LP505 and LP560, respectively. They were acquired with oil immersion (objective magnification, ×40/1.3). Images from DS5 and control corneas were captured with identical photomultiplier tube gain settings and images were processed the same way (LSM-PC software; Carl Zeiss Meditec, Inc).
IN SITU ZYMOGRAPHY AND COLLAGENASE ASSAYS
In situ zymography and collagenase assays were performed to localize the gelatinase/collagenase activity in corneal cryosections using a previously described method.10 Corneal sections were assayed individually either for gelatinases (MMP-2, MMP-9) or collagenase I (MMP-1) (n=5 per strain per assay). Sections were thawed and incubated overnight with reaction buffer, 0.05 M Tris-HCl, 0.15 M NaCl, 5 mM CaCl2, and 0.2 mM NaN3, pH 7.6, containing 40 μg/mL of either fluorescein isothiocyanate conjugate (FITC)–labeled dye-quenched (DQ) gelatin or FITC-labeled collagen I, which were available in a gelatinase/collagenase assay kit (EnzChek; Molecular Probes, Eugene, Oregon). As a negative control, 50 μM of 1,10-phenanthroline, a metalloproteinase inhibitor, was added to the reaction buffer before applying the FITC-labeled DQ/collagen I to frozen sections. Proteolysis of the FITC-labeled DQ gelatin or FITC-DQ collagen substrate yields cleaved FITC peptides that are fluorescent. The localization of fluorescence indicates the sites of net gelatinolytic/collagenase activity, and the intensity is proportional to the amount of activity in the tissue. After incubation, the sections were washed with phosphate-buffered saline and counterstained with propidium iodide (2 μg/mL in phosphate-buffered saline; Sigma, St Louis, Missouri) in an antifade Gel/Mount (Fisher, Atlanta, Georgia), and a coverslip was applied. Areas of gelatinolytic/collagenase activity of MMPs were viewed with a Nikon Eclipse E400 fluorescent microscope (Melville, New York), and images were captured by a Nikon DS-QiMc digital camera.
MEASUREMENT OF FLUORESCENCE INTENSITY IN CORNEA
Fluorescence intensity in the corneal sections used for either immunostaining (MMP-1, MMP-9, SPRR-1a, SPRR-2a, and involucrin) or in situ assays (zymography and collagenase I) were measured in digital images using NIS Elements Software (version 3.0, BR [basic research]; Nikon). At least 6 images per time point per strain were analyzed. The epithelial layer of the stained corneas was circumscribed by 2 masked observers. The fluorescence intensity was calculated by the software and entered into an Excel spreadsheet (Microsoft Corp, Redmond, Washington). Data are presented as mean(standard deviation) in gray levels.
RNA ISOLATION AND REAL-TIME POLYMERASE CHAIN REACTION
Total RNA from the corneal epithelium from the 3 strains per time point (NS and DS5) was extracted using an acid guanidium thiocyanate-phenol-chloroform method, as previously described.21 Four samples per strain per time point were used, and 1 sample consisted of pooled samples from 5 mice. Samples were treated with DNase to prevent genomic DNA contamination, according to the manufacturer’s instructions (Qiagen, Valencia, California).
First-strand complementary DNA was synthesized from 1 μg of total RNA using random hexamers and M-MuLV reverse transcriptase (Ready-To-Go You-Prime First-Strand Beads; GE Healthcare, Piscataway, New Jersey), as previously described.21 Realtime polymerase chain reaction was performed using gene expression assay primers and MGB probes specific for glyceraldehyde 3-phosphate dehydrogenase (GADPH), MMP-1, MMP-3, MMP-9, involucrin, SPRR-1a and SPRR-2a (assay identification numbers, Mm9999915, Mm00473493, Mn00440295, Mm00442991, Mm00515219, Mm01962902, and Mm00845122, respectively), and a TaqMan Universal PCR Master Mix AmpErase (Applied Biosystems, Foster City, California), in a commercial thermocycling system (Mx3005P QPCR System; Stratagene, La Jolla, California), according to the manufacturer’s recommendations. Assays were performed in duplicate, and there were 4 independent samples. A nontemplate control was included in all of the experiments to evaluate DNA contamination of the reagents used. The GAPDH gene was used as an endogenous reference for each reaction. The results of quantitative polymerase chain reaction were analyzed by the comparative cycle threshold (CT) method in which target change=2–ΔΔCt (User Bulletin, No. 2, P/N 4303859; Applied Biosystems). The CT was determined using the primary (fluorescent) signal as the cycle at which the signal crossed a user-defined threshold (the middle point of the amplification curve, usually 40% of the maximum fluorescence). The results were normalized by the CT value of GAPDH, and the mean CT of relative mRNA level in the NS group of each strain was used as the calibrator for the strain.
STATISTICAL ANALYSIS
The unpaired t test was used to compare the controls (NS vs DS5) with each mouse strain. P≤.05 was considered statistically significant. Analyses were performed using GraphPad Prism 4.0 software (GraphPad, San Diego, California).
RESULTS
RESISTANCE TO DESICCATION-INDUCED CORNEAL SURFACE ABNORMALITY
The results revealed that JNK2KO, but not JNK1KO, is resistant to desiccation-induced corneal surface abnormality.
Dry eye is often accompanied by an altered corneal epithelial barrier and corneal surface irregularity. Fluorescent dyes such as sodium fluorescein and OGD have been used with success to evaluate corneal barrier disruption.10,11,26 In humans, corneal regularity can be assessed by videokeratoscopy.27 Mice blink very infrequently, and it is not possible to assess the tear breakup time. Therefore, in mice, the regularity of the light ring reflected off the corneal surface has been used as a measure of corneal smoothness and compromise of tear film integrity.10
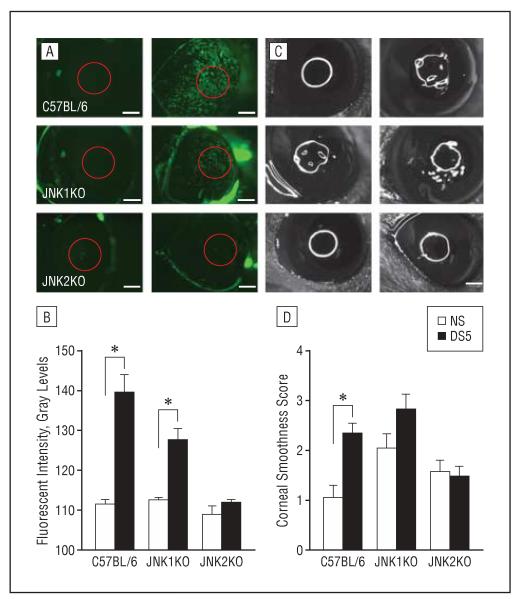
We evaluated the corneal permeability to OGD and corneal smoothness of the 3 mouse strains before and after experimental DS. The results are presented in Figure 1, A and B. The 3 strains had similar uptake of OGD by the corneal epithelium at baseline; however, DS induced significant corneal barrier disruption in C57BL/6 and JNK1KO mice, but not in the JNK2KO mice (Figure 1A). Of the 3 strains, wild-type C57BL/6 mice showed the greatest barrier disruption. A similar response pattern between strains was observed when evaluating corneal smoothness (Figure 1, C and D). The C57BL/6 and JNK1KO mice showed increased corneal irregularity after 5 days of desiccating stress, while JNK2KO DS5 mice maintained their corneal smoothness at baseline levels.
Figure 1.
Corneal smoothness and permeability evaluation of the 3 strains of mice. A, Representative digital images of corneas in C57BL/6, c-Jun N-terminal kinase 1 knockout (JNK1KO), and JNK2KO mice (A) were used to score Oregon green dextran–488 permeability (B) after 5 days of desiccating stress (DS5). Gray levels of fluorescent intensity are shown on the y-axis (B). C, Representative digital images of the corneal surface in C57BL/6, JNK1KO, and JNK2KO mice were used to score corneal smoothness (D) after 5 days of desiccating stress. Data in graphs are mean(standard deviation). NS indicates nonstressed control; *P<.05 compared with NS in the same strain. Scale bars, 500 μm.
INCREASE IN GELATINASE AND COLLAGENASE LEVELS AND ACTIVITY BY DS
The results show that DS increases gelatinase and collagenase levels and activity in wild-type and JNK1KO mouse strains.
We have previously reported that MMPs are implicated in desiccation-induced disruption of barrier function, including cleavage of tight junction proteins such as occludin and zonula occludens 1.9-11 To better evaluate the role of JNK SAPK in corneal epithelial function, we performed immunostaining for the gelatinase MMP-9 and the collagenase MMP-1 and in situ gelatinase and collagenase activity assays in sequential corneal sections of the 3 strains. Our results are presented in Figure 2.
Figure 2.
Evaluation of metalloproteinase (MMP) expression and activity in corneal sections in the 3 strains of mice. Laser scanning immunofluorescent confocal microscopy of corneal sections stained for MMP-9 (A, green) or MMP-1 (E), with propidium iodide nuclear counterstaining (red) in nonstressed control conditions (NS) and after 5 days of desiccating stress (DS5) in C57BL/6, c-Jun N-terminal kinase knockout 1 (JNK1KO) and JNK2KO mice. B and F, Representative digital images of in situ zymography (B) and in situ collagenase assay (F). The fluorescence intensity is proportional to gelatinase or collagenase activity, respectively, within the tissue. Graphical data are the mean (standard deviation) of measured fluorescence levels of MMP-9 and MMP-1 immunofluorescent staining (C and G) and in situ assays (D and H). *P<.05 compared with NS in the same strain; **P<.001 compared with NS in the same strain. Scale bars, 50 μm (A, E, and F) and 100 μm (B).
Desiccating stress increased immunoreactivity of MMP-9 (Figure 2A) and MMP-1 (Figure 2E) in the corneal epithelium, notably in the most apical cell layers, in both C57BL/6 and JNK1KO mice. The MMP-9 and -1 fluorescent intensity levels were significantly higher in the DS5 than the NS sections from C57BL/6 and JNK1KO mice (Figure 2, C and G; P<.001, P<.001, P<.001, and P=.02, respectively). In situ gelatinase and collagenase activity increased significantly in DS5 corneal epithelium of C57BL/6 mice and showed a moderate, non–statistically significant increase in JNK1KO and no change in JNK2KO corneas. Analysis of MMP-9, -3, and -1 gene expression in the corneal epithelium is presented in the Table. Levels of MMP-9 mRNA transcripts significantly increased in C57BL/6, but decreased in both JNKKO strains at DS5. Levels of MMP-1 and -3 mRNA transcripts significantly increased in C57BL/6 and JNK1KO strains at DS5, while they showed a non–statistically significant decrease in JNK2KO mice. These findings suggest that the increased levels of MMP-9 protein observed by immunofluorescent staining at DS5 in the JNK1KO may occur at the posttranscriptional level.
Table. Levels of MMP-9, MMP-1, MMP-3, SPRR-1a, SPRR-2a, and Involucrin mRNA Transcripts in the Corneal Epithelia of the 3 Strains Before and After Desiccating Stress for 5 Days.
| Transcript by Mouse Type |
Mean (SD) |
P Value |
|
|---|---|---|---|
| NS | DS5 | ||
| MMP-9 | |||
| C57BL/6 | 1.00 (0.33) | 1.76 (0.46) | .009 |
| JNK1KO | 1.00 (0.22) | 0.44 (0.17) | <.001 |
| JNK2KO | 1.00 (0.38) | 0.45 (0.42) | <.001 |
| MMP-1 | |||
| C57BL/6 | 1.00 (0.77) | 2.97 (0.62) | <.001 |
| JNK1KO | 1.00 (0.36) | 1.85 (0.50) | .007 |
| JNK2KO | 1.00 (0.32) | 0.39 (0.43) | .11 |
| MMP-3 | |||
| C57BL/6 | 1.00 (0.30) | 2.58 (0.34) | <.001 |
| JNK1KO | 1.00 (0.20) | 1.32 (0.17) | .01 |
| JNK2KO | 1.00 (0.42) | 0.44 (0.26) | .17 |
| SPRR-1a | |||
| C57BL/6 | 1.00 (0.32) | 2.72 (0.23) | <.001 |
| JNK1KO | 1.00 (0.21) | 1.72 (0.10) | <.001 |
| JNK2KO | 1.00 (0.37) | 1.63 (0.35) | .01 |
| SPRR-2a | |||
| C57BL/6 | 1.00 (0.33) | 1.60 (0.43) | .008 |
| JNK1KO | 1.00 (0.30) | 1.24 (0.23) | .15 |
| JNK2KO | 1.00 (0.74) | 0.67 (0.29) | .33 |
| Involucrin | |||
| C57BL/6 | 1.00 (0.26) | 1.87 (0.28) | <.001 |
| JNK1KO | 1.00 (0.52) | 2.38 (0.14) | <.001 |
| JNK2KO | 1.00 (0.29) | 0.48 (0.36) | .002 |
Abbreviations: DS5, desiccating stress for 5 days; JNK1KO, c-Jun N-terminal kinase knockout 1; JNK2KO, c-Jun N-terminal kinase knockout 2; MMP, metalloproteinase; NS, nonstressed condition (before DS5); SPRR, small proline-rich protein.
LEVELS OF CORNIFIED ENVELOPE PROTEIN PRECURSOR TRANSCRIPTS
High levels of cornified envelope protein precursor transcripts were observed in JNK1KO, but not JNK2KO mice.
We have previously demonstrated that DS increased expression of cornified envelope precursor proteins.21 To further investigate the role of JNK SAPK pathway in this stress response, we examined the expression of the cornified envelope precursors SPRR-1a, SPRR-2a, and involucrin in the corneal epithelium by immunostaining and real-time polymerase chain reaction.
Our immunofluorescent staining results are presented in Figure 3. The intensity of SPRR-1a and SPRR-2a was similar for the 3 strains in the NS control group. Increased staining intensity for involucrin was noted in the basal epithelium of the JNK1KO and JNK2KO corneas at baseline compared with C57BL/6; however, this was not statistically significant.
Figure 3.
Evaluation of cornified envelope protein precursors in the corneal sections of the 3 strains of mice. Laser scanning immunofluorescent confocal microscopy of corneal sections stained for small proline-rich protein (SPRR)–1a (A, green), SPRR-2a (B, green), or involucrin (C, green) with propidium iodide nuclear counterstaining (red) in nonstressed control conditions (NS) and after 5 days of desiccating stress (DS5) in C57BL/6, c-Jun N-terminal kinase knockout 1 (JNK1KO), and JNK2KO mice. Graphical data are the mean (standard deviation) of measured fluorescence levels for each protein. *P<.05 compared with NS in the same strain; **P<.01 compared with NS in the same strain; and ***P<.001 compared with NS in the same strain. Scale bars=50 μm.
Immunoreactivity of SPRR-1a, SPRR-2a, and involucrin significantly increased in the corneas of DS5 C57BL/6 and JNK1KO, while no change in immunoreactivity was observed in JNK2KO mice (Figures 3, A-C).
The levels of mRNA transcripts for these cornified envelope precursors are presented in the Table. Levels of SPRR-1a transcripts increased in all 3 strains following 5 days of DS, with the greatest relative increase from baseline in the C57BL/6 strain. The C57BL/6 mice also had a significant increase in SPRR-2a and involucrin transcripts. Involucrin transcripts also increased in JNK1KO, while there was no change in SPRR-2a and a statistically significant decrease in involucrin transcripts in the JNK2KO mice.
COMMENT
Our model of DS has previously been noted to induce activation of JNK SAPK in the corneal and conjunctival epithelium, with the greatest increase noted for JNK2.12 We hypothesized that SAPK signaling pathways are activated by the ocular surface desiccation and hypertonic extracellular environment that results from decreased tear production in our model. Consistent with this theory, we found increased levels of active phosphorylated JNK1 and JNK2 (JNK2 > JNK1) in ocular surface epithelia treated with hypertonic saline in vivo and in cultured human corneal epithelial cells exposed to hyperosmolar media.20,23 Because there are no specific inhibitors for each JNK isoform, we opted to evaluate mice deficient in either JNK1 or JNK2 to better dissect the specific contribution of each JNK isoform to the epithelial response of dry eye.
Activation of the JNK pathway has been implicated in the increased production of MMPs and cornified envelope precursor proteins that has been observed in the corneal epithelium following desiccating or hyperosmotic stress.10,12,20,28 The activation of MAPK p38 alone has been shown to induce expression of MMP-1 and -3 in an activator protein 1–independent manner by stabilizing the corresponding mRNAs in human skin fibroblasts.29 To confirm the relative roles of JNK1 and JNK2 in the corneal epithelial stress response in vivo, we compared corneal epithelial barrier function and smoothness, as well as production of MMPs and cornified envelope precursors, following 5 days of experimental desiccation in JNK1 and JNK2 gene–deficient and wild-type C57BL/6 strains.
We observed that JNK2KO mice were resistant to corneal epithelial barrier disruption and maintained a regular corneal surface in response to desiccation, whereas JNK1KO mice behaved like wild-type control mice, with significant disruption of barrier and a non–statistically significant increase in surface regularity. Consistent with the lack of worsening of clinical parameters of dry eye, JNK2KO mice showed no change in immunoreactivity to MMP-9 and -1 and no increase in gelatinase or collagenase activity in their corneal epithelium. Furthermore, levels of MMP-3, a physiological activator of MMP-9,30 remained constant in JNK2KO mice. Previously, MMP-9 has been found to have a role in corneal barrier disruption in dry eye by degrading tight junction proteins in the apical corneal epithelium and accelerating apical cell desquamation. We observed that tear MMP-9 activity increased with severity of corneal epithelial disease in dry eye and positively correlated with corneal fluorescein staining scores and inversely correlated with low-contrast visual acuity.31 To distinguish proteolytic activation of MMP by JNK2 from synthesis of new MMP in cultured corneal epithelial cells, a drug such as cycloheximide, which inhibits protein synthesis, could be used in the future. The JNK pathway may also upregulate expression of cytokines capable of regulating MMP production (ie, interleukin 1 and tumor necrosis factor α), so it is reasonable to say that the consequential effect of MMP upregulation may be a direct or indirect effect of JNK.
Cornified envelope precursor proteins are usually expressed in low levels in the wet ocular surface mucosal epithelia, as opposed to differentiated skin epidermal cells, which have a thick cornified envelope that functions to maintain barrier function.32 This and previous studies suggest that the corneal epithelium responds to desiccating or osmotic stress by producing cornified envelope precursor proteins, perhaps as a mechanism to form an alternative skinlike protective barrier.21,28,33 Certain cornified envelope precursor genes such as involucrin and SPRR-2a have been noted to be regulated by JNK14,28; however, there are no studies showing any specificity for JNK2 over JNK1 in the promoter-binding sites of SPRR and MMP genes. Similar to MMPs, the production of these factors, particularly SPRR-2a and involucrin, was also attenuated in JNK2KO mice.
Our findings suggest that certain aspects of the regulated response of the corneal epithelium to desiccating stress are modulated by the JNK2 signaling pathway. This implies that JNK2 inhibitors may have therapeutic potential for treatment of the corneal epithelial disease that develops in dry eye. Indeed, clinical studies have found that corticosteroids, which inhibit activator protein 1 gene transcription, have improved corneal epithelial disease.34 Furthermore, doxycycline, a tetracycline antibiotic with JNK inhibitory properties, has been reported to significantly improve corneal barrier function and smoothness in our murine model of dry eye.10,20,21
Taken together, our results demonstrate clearly different roles for JNK2 and JNK1 in the pathogenesis of corneal epithelial disease (Figure 4) and that inhibiting JNK2 could be a novel therapeutic target in dry eye disease.
Figure 4.
Schematic showing the proposed sequence of events after exposure of ocular surface tissue to desiccating stress. JNK indicates c-Jun N-terminal kinase. Smaller font of JNK1 indicates its possible smaller role.
Acknowledgments
Funding/Support: This study was supported by National Eye Institute grants EY11915 (Dr Pflugfelder) and EY07001-29 (Dr De Paiva); an unrestricted grant from Research to Prevent Blindness; the Oshman Foundation; The William Stamps Farish Fund; and an unrestricted grant from Allergan, Inc.
Footnotes
Financial Disclosure: None reported.
Contributor Information
Dr Cintia S. De Paiva, Ocular Surface Center, Department of Ophthalmology, Cullen Eye Institute, Baylor College of Medicine, Houston, Texas.
Dr Solherny B. Pangelinan, Ocular Surface Center, Department of Ophthalmology, Cullen Eye Institute, Baylor College of Medicine, Houston, Texas.
Dr Emmanuel Chang, Ocular Surface Center, Department of Ophthalmology, Cullen Eye Institute, Baylor College of Medicine, Houston, Texas.
Dr K.-C. Yoon, Department of Ophthalmology, Chonnam National University Medical School, Dong-Gu, Gwangju, South Korea.
Dr William J. Farley, Ocular Surface Center, Department of Ophthalmology, Cullen Eye Institute, Baylor College of Medicine, Houston, Texas.
Dr De-Quan Li, Ocular Surface Center, Department of Ophthalmology, Cullen Eye Institute, Baylor College of Medicine, Houston, Texas.
Dr Stephen C. Pflugfelder, Ocular Surface Center, Department of Ophthalmology, Cullen Eye Institute, Baylor College of Medicine, Houston, Texas.
REFERENCES
- 1.de Paiva CS, Pflugfelder SC. Diagnostic approaches to lacrimal keratoconjunctivitis. In: Pflugfelder SC, Beuerman RW, Stern ME, editors. Dry Eye and Ocular Surface Disorders. Marcel Dekker Inc; New York, NY: 2004. pp. 269–308. [Google Scholar]
- 2.Moss SE, Klein R, Klein BE. Incidence of dry eye in an older population. Arch Ophthalmol. 2004;122(3):369–373. doi: 10.1001/archopht.122.3.369. [DOI] [PubMed] [Google Scholar]
- 3.Schein OD, Munoz B, Tielsch JM, Bandeen-Roche K, West S. Prevalence of dry eye among the elderly. Am J Ophthalmol. 1997;124(6):723–728. doi: 10.1016/s0002-9394(14)71688-5. [DOI] [PubMed] [Google Scholar]
- 4.Bandeen-Roche K, Munoz B, Tielsch JM, West SK, Schein OD. Self-reported assessment of dry eye in a population-based setting. Invest Ophthalmol Vis Sci. 1997;38(12):2469–2475. [PubMed] [Google Scholar]
- 5.Goto E, Yagi Y, Matsumoto Y, Tsubota K. Impaired functional visual acuity of dry eye patients. Am J Ophthalmol. 2002;133(2):181–186. doi: 10.1016/s0002-9394(01)01365-4. [DOI] [PubMed] [Google Scholar]
- 6.Ishida R, Kojima T, Dogru M, et al. The application of a new continuous functional visual acuity measurement system in dry eye syndromes. Am J Ophthalmol. 2005;139(2):253–258. doi: 10.1016/j.ajo.2004.08.075. [DOI] [PubMed] [Google Scholar]
- 7.Kaido M, Dogru M, Ishida R, Tsubota K. Concept of functional visual acuity and its applications. Cornea. 2007;26((9)(suppl 1)):S29–S35. doi: 10.1097/ICO.0b013e31812f6913. [DOI] [PubMed] [Google Scholar]
- 8.Miljanović B, Dana R, Sullivan DA, Schaumberg DA. Impact of dry eye syndrome on vision-related quality of life. Am J Ophthalmol. 2007;143(3):409–415. doi: 10.1016/j.ajo.2006.11.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pflugfelder SC, Farley W, Luo L, et al. Matrix metalloproteinase-9 knockout confers resistance to corneal epithelial barrier disruption in experimental dry eye. Am J Pathol. 2005;166(1):61–71. doi: 10.1016/S0002-9440(10)62232-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.De Paiva CS, Corrales RM, Villarreal AL, et al. Corticosteroid and doxycycline suppress MMP-9 and inflammatory cytokine expression, MAPK activation in the corneal epithelium in experimental dry eye. Exp Eye Res. 2006;83(3):526–535. doi: 10.1016/j.exer.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 11.Corrales RM, Stern ME, de Paiva CS, Welch J, Li DQ, Pflugfelder SC. Desiccating stress stimulates expression of matrix metalloproteinases by the corneal epithelium. Invest Ophthalmol Vis Sci. 2006;47(8):3293–3302. doi: 10.1167/iovs.05-1382. [DOI] [PubMed] [Google Scholar]
- 12.Luo L, Li DQ, Corrales RM, Pflugfelder SC. Hyperosmolar saline is a proinflammatory stress on the mouse ocular surface. Eye Contact Lens. 2005;31(5):186–193. doi: 10.1097/01.icl.0000162759.79740.46. [DOI] [PubMed] [Google Scholar]
- 13.Wang Y, Zhang J, Yi XJ, Yu FS. Activation of ERK1/2 MAP kinase pathway induces tight junction disruption in human corneal epithelial cells. Exp Eye Res. 2004;78(1):125–136. doi: 10.1016/j.exer.2003.09.002. [DOI] [PubMed] [Google Scholar]
- 14.Adhikary G, Crish J, Lass J, Eckert RL. Regulation of involucrin expression in normal human corneal epithelial cells: a role for activator protein one. Invest Ophthalmol Vis Sci. 2004;45(4):1080–1087. doi: 10.1167/iovs.03-1180. [DOI] [PubMed] [Google Scholar]
- 15.Zeigler ME, Chi Y, Schmidt T, Varani J. Role of ERK and JNK pathways in regulating cell motility and matrix metalloproteinase 9 production in growth factor-stimulated human epidermal keratinocytes. J Cell Physiol. 1999;180(2):271–284. doi: 10.1002/(SICI)1097-4652(199908)180:2<271::AID-JCP15>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 16.Reunanen N, Li SP, Ahonen M, Foschi M, Han J, Kahari VM. Activation of p38a mitogen-activated protein kinase enhances collagenase-1 (MMP-1) and stromelysin-1 (MMP-3) expression by mRNA stabilization [published online ahead of print June 11, 2002] J Biol Chem. 2002;277(35):32360–32368. doi: 10.1074/jbc.M204296200. [DOI] [PubMed] [Google Scholar]
- 17.Liacini A, Sylvester J, Li WQ, Zafarullah M. Inhibition of interleukin-1-stimulated MAP kinases, activating protein-1 (AP-1) and nuclear factor kappa B (NF-kappaB) transcription factors down-regulates matrix metalloproteinase gene expression in articular chondrocytes. Matrix Biol. 2002;21(3):251–262. doi: 10.1016/s0945-053x(02)00007-0. [DOI] [PubMed] [Google Scholar]
- 18.Mengshol JA, Vincenti MP, Brinckerhoff CE. IL-1 induces collagenase-3 (MMP-13) promoter activity in stably transfected chondrocytic cells: requirement for Runx-2 and activation by p38 MAPK and JNK pathways. Nucleic Acids Res. 2001;29(21):4361–4372. doi: 10.1093/nar/29.21.4361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Woodgett JR, Avruch J, Kyriakis JM. Regulation of nuclear transcription factors by stress signals. Clin Exp Pharmacol Physiol. 1995;22(4):281–283. doi: 10.1111/j.1440-1681.1995.tb01995.x. [DOI] [PubMed] [Google Scholar]
- 20.Li DQ, Chen Z, Song XJ, Luo L, Pflugfelder SC. Stimulation of matrix metalloproteinases by hyperosmolarity via a JNK pathway in human corneal epithelial cells. Invest Ophthalmol Vis Sci. 2004;45(12):4302–4311. doi: 10.1167/iovs.04-0299. [DOI] [PubMed] [Google Scholar]
- 21.De Paiva CS, Corrales RM, Villarreal AL, et al. Apical corneal barrier disruption in experimental murine dry eye is abrogated by methylprednisolone and doxycycline. Invest Ophthalmol Vis Sci. 2006;47(7):2847–2856. doi: 10.1167/iovs.05-1281. [DOI] [PubMed] [Google Scholar]
- 22.Niederkorn JY, Stern ME, Pflugfelder SC, et al. Desiccating stress induces T cell-mediated Sjogren’s syndrome-like lacrimal keratoconjunctivitis. J Immunol. 2006;176(7):3950–3957. doi: 10.4049/jimmunol.176.7.3950. [DOI] [PubMed] [Google Scholar]
- 23.Luo L, Li DQ, Doshi A, Farley W, Corrales RM, Pflugfelder SC. Experimental dry eye stimulates production of inflammatory cytokines and MMP-9 and activates MAPK signaling pathways on the ocular surface. Invest Ophthalmol Vis Sci. 2004;45(12):4293–4301. doi: 10.1167/iovs.03-1145. [DOI] [PubMed] [Google Scholar]
- 24.Yeh S, Song XJ, Farley W, Li DQ, Stern ME. Pflugfelder SC. Apoptosis of ocular surface cells in experimentally induced dry eye. Invest Ophthalmol Vis Sci. 2003;44(1):124–129. doi: 10.1167/iovs.02-0581. [DOI] [PubMed] [Google Scholar]
- 25.de Paiva CS, Villarreal AL, Corrales RM, et al. IFN-γ promotes goblet cell loss in response to desiccating ocular stress. Invest Ophthalmol Vis Sci. 2006;47 E-Abstract 5579. [Google Scholar]
- 26.De Paiva CS, Chotikavanich S, Pangelinan SB, et al. IL-17 disrupts corneal barrier following desiccating stress [published online ahead of print February 25, 2009] Mucosal Immunol. 2009;2(3):243–253. doi: 10.1038/mi.2009.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.de Paiva CS, Lindsey JL, Pflugfelder SC. Assessing the severity of keratitis sicca with videokeratoscopic indices. Ophthalmology. 2003;110(6):1102–1109. doi: 10.1016/s0161-6420(03)00245-8. [DOI] [PubMed] [Google Scholar]
- 28.Chen Z, Tong L, Li Z, et al. Hyperosmolarity-induced cornification of human corneal epithelial cells is regulated by JNK MAPK. Invest Ophthalmol Vis Sci. 2008;49(2):539–549. doi: 10.1167/iovs.07-0569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Capoulade C, Mir LM, Carlier K, et al. Apoptosis of tumoral and nontumoral lymphoid cells is induced by both mdm2 and p53 antisense oligodeoxynucleotides. Blood. 2001;97(4):1043–1049. doi: 10.1182/blood.v97.4.1043. [DOI] [PubMed] [Google Scholar]
- 30.Ogata Y, Enghild JJ, Nagase H. Matrix metalloproteinase 3 (stromelysin) activates the precursor for the human matrix metalloproteinase 9. J Biol Chem. 1992;267(6):3581–3584. [PubMed] [Google Scholar]
- 31.Chotikavanich S, de Paiva CS, Lee D-Q, et al. Production and activity of matrix metalloproteinase-9 on the ocular surface increase in dysfunctional tear syndrome [published online ahead of print February 28, 2009] Invest Ophthalmol Vis Sci. 2009;50:3203–3209. doi: 10.1167/iovs.08-2476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Segre J. Complex redundancy to build a simple epidermal permeability barrier. Curr Opin Cell Biol. 2003;15(6):776–782. doi: 10.1016/j.ceb.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 33.Li S, Nikulina K, DeVoss J, et al. Small proline-rich protein 1B (SPRR1B) is a biomarker for squamous metaplasia in dry eye disease. Invest Ophthalmol Vis Sci. 2008;49(1):34–41. doi: 10.1167/iovs.07-0685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Newton R, Holden NS. Separating transrepression and transactivation: a distressing divorce for the glucocorticoid receptor? Mol Pharmacol. 2007;72(4):799–809. doi: 10.1124/mol.107.038794. [DOI] [PubMed] [Google Scholar]