Abstract
BACKGROUND AND PURPOSE
Patient-centered models of healthcare and patient derived criteria for success are becoming increasingly important. Research studies of such success criteria have not targeted facial pain (FP) or fibromyalgia (FM) individuals and little is known about the consistency across pain groups. This study examined patient-centered success criteria of individuals with FP and FM.
METHODS
Participants included 53 FP (46 women, 7 men) and 52 FM (49 women, 3 men) individuals who completed the Patient Centered Outcomes (PCO) Questionnaire. The PCO assesses four relevant domains of chronic pain: pain, fatigue, distress, and interference in daily activities. Participants rated their usual levels, expected levels, levels considered as successful improvements, and how important improvements were in each of the four domains following treatment.
RESULTS
Both groups of participants defined treatment success as a substantial decrease in their pain, fatigue, distress, and interference ratings (all approx. 60%). FM participants reported high levels of pain (M = 7.08, SD = 2.04), fatigue (M = 7.82, SD = 1.71), distress (M = 6.35, SD = 2.46), and interference (M = 7.35, SD = 2.21). FP participants’ ratings of these domains were significantly lower for pain (M = 5.62, SD = 2.38), fatigue (M = 5.28, SD = 2.64), distress (M = 4.34, SD = 2.78) and interference (M = 4.10, SD = 3.06).
INTERPRETATIONS
These results demonstrate the high expectations of individuals with chronic pain regarding treatments of their symptoms. Healthcare providers should incorporate these expectations into their treatment plans and discuss realistic treatment goals with their pain populations.
Keywords: facial pain, fibromyalgia, patient-centered care, treatment outcome, pain/psychology
Introduction
Chronic pain is one of the most frequent, costly, and disabling medical conditions in the United States, with estimates suggesting that 15% of adults experience some form of chronic pain. 1 Specifically, a significant number of these adults are affected by facial pain (FP) or fibromyalgia (FM). Whereas FP is a local pain syndrome, FM is defined by chronic widespread pain and tenderness. However, there is substantial overlap between both pain syndromes, and they seem to share relevant pain mechanisms. 2 Although FP is a heterogeneous syndrome that includes dental disorders, headaches, and neuropathic pain, most patients in this group have temporomandibular joint disorders. Recent estimates suggest that between 5% – 10% of adults and 30% – 50% of the elderly population are living with chronic and severe uncontrolled FP or FM. 3, 4 In fact, it has been estimated that more than 40% of individuals with FP or FM have experienced severe pain for over five years without finding effective means of achieving pain relief. 3 These clinical groups are difficult to treat because many individuals with chronic pain present with pain of an unknown etiology. Moreover, these populations are frequently misdiagnosed and given unsuccessful treatments, leading to patient frustration and multiple transitions between medical providers in an attempt to effectively control their pain. 3, 5
Traditionally, determinations regarding successful treatment for chronic pain treatment have been made predominantly by healthcare providers. However, this “medical-model” of treatment does not allow for the incorporation of patient perspectives of successful outcomes for any particular course of treatment. In contrast, adopting patient-centered models of treatment allows for healthcare providers and patients to work together to determine success criteria. 6 Researchers have recently begun investigating the patient-centered model of treatment outcomes and there is a large body of evidence showing the importance of a collaborative relationship between health care providers and their patients. 7, 8 In fact, Alamo, Moral, and Perula de Torres (2002) concluded that a patient-centered approach for the treatment of pain was more effective than a provider-centered approach. The former strategy led to improvements in most of the outcome measures during the one-year study period. 9 Though often reflecting high expectations, patient criteria of therapeutic success are variable throughout treatment. 10 Through interactions with their providers, chronic back and neck pain patients became less stringent in their success criteria during the course of treatment, and used these lenient criteria in making judgments about treatment success. 10
Due to the complex nature of chronic pain, many individuals report frustration with their healthcare providers related to multiple failed treatment attempts. Thus, individual expectations in the treatment of chronic pain appear to be extremely relevant for successful outcomes. 11, 12 Despite burgeoning interest, little is currently known regarding the specific factors that individuals with FP and FM consider important for successful treatment. Thus our study examined the treatment expectations in a sample of FP and FM participants.
The primary aim of this study was to define treatment success from the pain patient perspective across four domains (pain, fatigue, emotional distress, interference with daily activities) using the Patient Centered Outcomes (PCO) questionnaire.
Methods
Chronic Pain Participants
This study used a sample of 53 individuals evaluated at an orofacial pain clinic at the University of Florida (Table 1). This sample consisted of individuals who were heterogeneous with regard to orofacial pain complaint. Specifically, 42.6% of patients had jaw pain, 29.6% had FP localized to one side of the face, 13.0% had headaches, and 11.1% had pain related to teeth/gums. FP participants did not also meet criteria for FM. The average duration of pain was 93.4 months (SD = 111.6).
Table 1.
Demographic characteristics of samples
| Facial Pain Sample | Fibromyalgia Sample | |
|---|---|---|
| Sex | 46 women | 49 women |
| 7 men | 3 men | |
|
| ||
| Race | All Caucasian | 43 Caucasian |
| 3 African American | ||
| 1 Hispanic | ||
| 1 Pacific Islander | ||
|
| ||
| Age | Mean = 47.31 (SD = 15.15) | Mean = 46.48 (SD = 10.81) |
Our sample of FM participants was comprised of 52 individuals (Table 1). They were randomly selected from a pool of participants recruited from the Rheumatology clinic of one of the authors (R.S.) at the University of Florida or affiliated pain clinics. Chronic pain was reported on average for 110.3 months (SD = 57.5). All FM participants fulfilled the 1990 American College of Rheumatology Criteria (Wolfe et al. 1990). They reported chronic widespread musculoskeletal pain for more than 3 months and had at least 11 out of 18 tender points. None of the FM participants complained of facial pain during the office visit although 88% reported the presence of frequent headaches. All participants recruited had to be 18 years old or older, have the ability to read and write English, and have the ability to consent to participate.
Procedures
Participants were asked to complete a brief demographics questionnaire and a questionnaire about patient outcomes before their medical appointment. The Patient Centered Outcomes (PCO) questionnaire assesses four domains (pain, fatigue, emotional distress, and interference with daily activities) relevant to chronic pain populations on a numerical rating scale ranging from 0–10. For each domain the PCO Questionnaire asks participants to provide the following ratings: their usual levels of symptoms, the levels considered to be a successful treatment outcome, the levels they desire, the levels they expect following treatment, and how important improvement is for them in each of the four domains. The PCO Questionnaire has been shown to have acceptable test-retest reliability (r = .84 to r = .90, p<.001; for usual levels across domains) and concurrent validity with standardized measures of pain, mood, and disability. 13
Statistical Analyses
Descriptive statistics were generated for each domain and normality assumptions were tested for each measure. Repeated Measures Analyses of Variance (ANOVAS) were performed to determine whether differences existed across domains in the amount of change necessary for treatment to be deemed successful for FP participants. Subsequently, paired t tests were conducted to examine the specific differences in the amount of change necessary for treatment across domains. Repeated Measures Analyses of Variance were performed using participants’ PCO ratings for the amount of change (usual minus success) needed to meet success criterion for each of the four domains during treatment compared across the two pain groups.
Results
Descriptive FP and FM PCO Data
Descriptive information about participants’ ratings for usual levels, desired levels, expected levels, levels considered to be successful, and importance ratings for each of the four PCO domains (pain, fatigue, emotional distress, and interference with daily activities) are provided in Table 2. Participants’ success criteria for each domain were subtracted from their ratings for usual levels of each domain to determine the amount of change that was needed for treatment to be perceived as successful. Overall, for treatments to be considered successful, FP participants required a pain level of 2.19 (61.7% reduction), a fatigue level of 2.16 (59.3% reduction), a distress level of 1.92 (56% reduction), and an interference level of 1.56 (61.6% reduction). On the other hand, FM participants required a pain level of 3.13 (55.8% reduction), a fatigue level of 3.00 (61.6% reduction), a distress level of 2.62 (58.7% reduction), and an interference level of 2.69 (63.4% reduction).
Table 2.
Descriptive statistics from the PCO questionnaire
| Facial Pain Sample | Fibromyalgia Sample | |||
|---|---|---|---|---|
|
| ||||
| M | SD | M | SD | |
| Usual levels | ||||
| Pain | 5.62 | 2.38 | 7.08 | 2.04 |
| Fatigue | 5.28 | 2.64 | 7.82 | 1.71 |
| Distress | 4.34 | 2.78 | 6.35 | 2.46 |
| Interference | 4.10 | 3.06 | 7.35 | 2.21 |
|
| ||||
| Desired levels | ||||
| Pain | 0.81 | 1.34 | 1.35 | 1.99 |
| Fatigue | 0.93 | 1.33 | 1.14 | 1.95 |
| Distress | 0.85 | 1.20 | 1.15 | 1.65 |
| Interference | 0.52 | 1.17 | 1.02 | 1.90 |
|
| ||||
| Expected levels | ||||
| Pain | 2.01 | 1.89 | 3.48 | 2.32 |
| Fatigue | 1.94 | 1.81 | 3.50 | 2.34 |
| Distress | 1.79 | 1.79 | 2.85 | 2.29 |
| Interference | 1.38 | 1.60 | 3.21 | 2.35 |
|
| ||||
| Successful levels | ||||
| Pain | 2.19 | 1.42 | 3.13 | 1.50 |
| Fatigue | 2.16 | 1.54 | 3.00 | 1.64 |
| Distress | 1.92 | 1.33 | 2.62 | 1.71 |
| Interference | 1.56 | 1.45 | 2.69 | 1.62 |
|
| ||||
| Importance levels | ||||
| Pain | 8.90 | 2.49 | 9.17 | 1.32 |
| Fatigue | 7.87 | 2.94 | 8.87 | 1.31 |
| Distress | 7.08 | 3.67 | 7.54 | 1.88 |
| Interference | 7.69 | 3.54 | 8.54 | 1.54 |
|
| ||||
| Amount of Change Needed (Usual – Success) | ||||
| Pain | 3.43 | 2.03 | 3.94 | 1.67 |
| % reduction | 61.7 | 55.8 | ||
| Fatigue | 3.13 | 2.10 | 4.82 | 1.90 |
| % reduction | 59.3 | 61.6 | ||
| Distress | 2.42 | 2.20 | 3.73 | 2.35 |
| % reduction | 56.0 | 58.7 | ||
| Interference | 2.55 | 2.38 | 4.65 | 2.05 |
| % reduction | 61.6 | 63.4 | ||
Domain Analyses
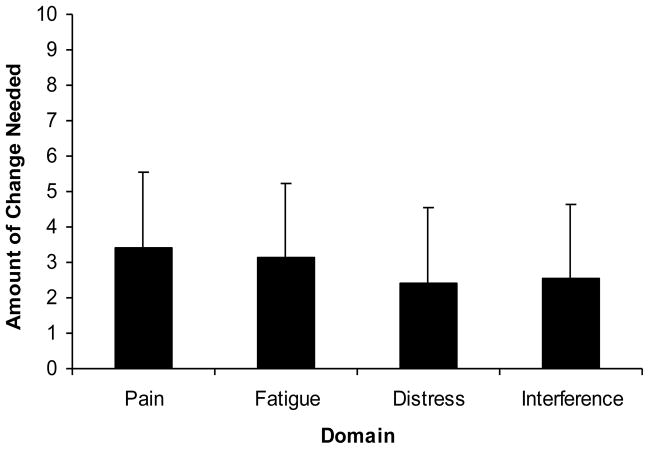
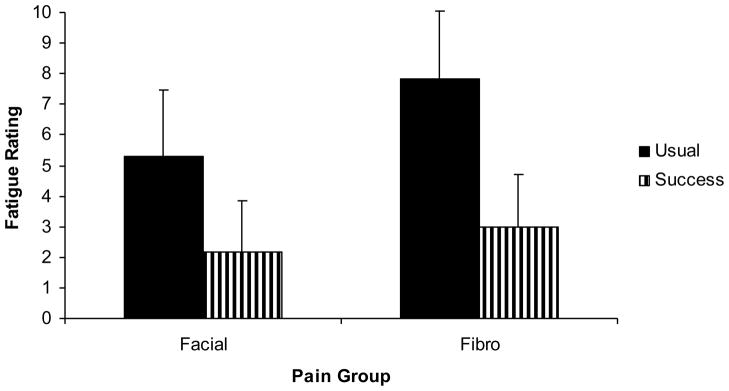
The repeated measures ANOVA yielded a significant effect for domain, F (3,156) = 5.15, p < .05, partial η2 = .09. Paired samples t tests revealed that FP participants would like a significantly greater reduction in pain compared to emotional distress, t (52) = 3.20, p = .002, in pain compared to interference, t (52) = 2.46, p = .017, and in fatigue compared to emotional distress, t (52) = 2.42, p = .019 (Figure 1).
Figure 1.
Amount of change needed for each domain for facial pain patients.
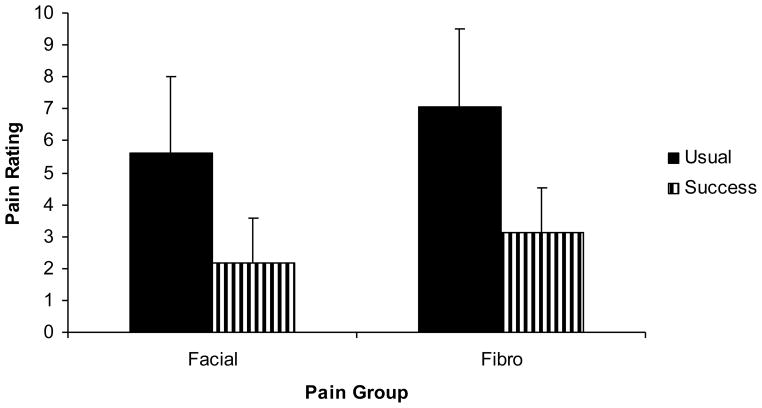
Pain Group Comparisons of PCO Data: Pain
For the pain groups, success was defined by significant decreases in their usual pain ratings, F(1, 103) = 411.64, p < .01, partial η2 = .80. There was a significant difference between the pain groups, F(1, 103) = 14.25, p < .01, partial η2 = .12. Specifically, FP participants had lower pain ratings than FM participants (p < .05). There was not a significant interaction between pain group and pain level (usual vs. success), suggesting that the pain groups defined success approximately equal for the pain domain (Figure 2).
Figure 2.
Usual and success pain ratings by pain group
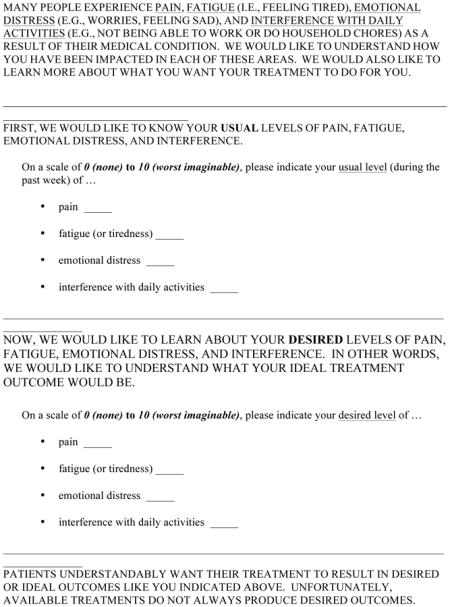
Pain Group Comparison of PCO Data: Fatigue
For the pain groups, success was defined by significant decreases in their usual fatigue ratings, F(1, 103) = 414.79, p < .01, partial η2 = .80. There was a significant difference between the pain groups, F(1, 103) = 27.31, p < .01, partial η2 = .21. Specifically, FP participants had lower fatigue ratings than FM participants (p < .05). There was a significant interaction between pain group and fatigue level (usual vs. success), F(1, 103) = 19.06, p < .01, partial η2 = .16 (Figure 3). FP participants required (for success) significantly less improvement in fatigue compared to FM participants (p < .05).
Figure 3.
Usual and success fatigue ratings by pain group
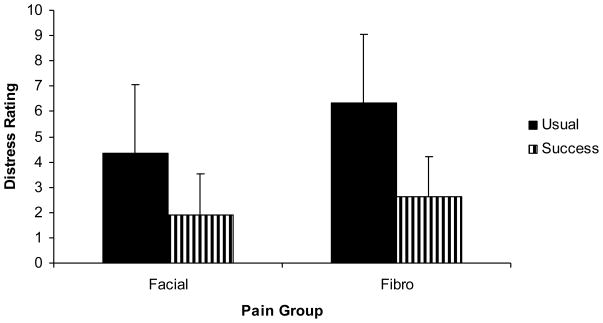
Pain Group Comparison of PCO Data: Emotional Distress
For the pain groups, success was defined by significant decreases in their usual distress ratings, F(1, 103) = 191.48, p < .01, partial η2 = .65. There was a significant difference between the pain groups, F(1, 103) = 14.50, p < .01, partial η2 = .12. Specifically, FP participants had lower distress ratings than FM participants (p < .05). There was a significant interaction between pain group and distress level (usual vs. success), F(1, 103) = 8.62, p < .05, partial η2 = .08 (Figure 4). FP participants required significantly less improvement in distress compared to FM participants (p < .05).
Figure 4.
Usual and success distress ratings by pain group
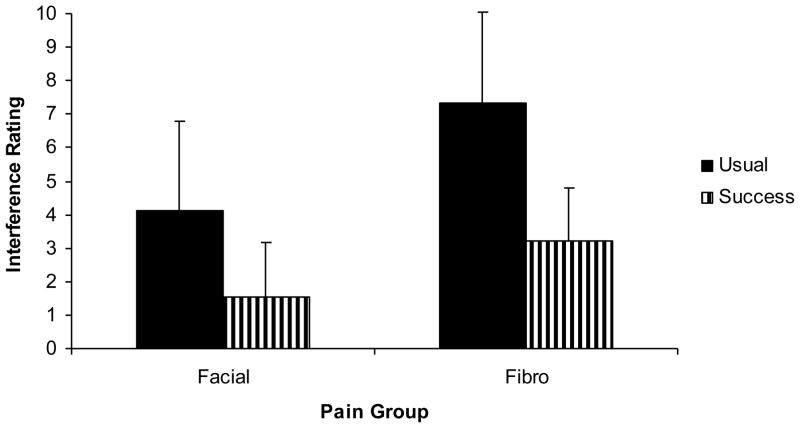
Pain Group Comparison of PCO Data: Interference
For the pain groups, success was defined by significant decreases in their usual interference ratings, F(1, 103) = 275.20, p < .01, partial η2 = .73. There was a significant difference between the pain groups, F(1, 103) = 35.68, p < .01, partial η2 = ..26. Specifically, FP participants had lower interference ratings than FM participants (p < .05). There was a significant interaction between pain group and interference level (usual vs. success), F(1, 103) = 23.55, p < .01, partial η2 = .19 (Figure 5). FP participants also required significantly less improvement in interference compared to FM participants (p < .05).
Figure 5.
Usual and success interference ratings by pain group
Discussion
FP and FM individuals require approximately 60% reductions in pain, fatigue, emotional distress, and interference with daily activities in order for treatment to be deemed successful. The present study also found that FP and FM individuals desired significantly greater reductions in pain compared to distress and interference and significantly greater reductions in fatigue compared to distress. In addition, these results indicate that chronic pain populations also highly value improvements in their emotional and behavioral well-being.
For all study participants, success was defined by large improvements in their usual pain, fatigue, emotional distress, and interference with daily activities. These endpoints are also consistent with the multi-dimensional features of pain and supported by prior research. 14 Interestingly, though, participants did not expect total pain elimination for treatments to be successful. This finding suggests that participants accept the more realistic scenario that they may experience some level of pain regardless of the treatment, even though their desired levels are lower (i.e., all pain groups had an average desired level of pain of less than 2 on an 11-point scale). Similarly, participants from both groups rated the importance levels for improvement in each domain an average of 7 or greater. These findings all suggest that patient-centered outcomes are critical to be considered by all health care providers.
The amount of pain reduction considered success by FP participants is similar with those reported in our previous study of chronic pain patients (2005). The current study showed that individuals with FP want pain to be reduced by an average 3.43 points (61.7% reduction) similar to our previous study (2005) which found that individuals with chronic back pain want pain to be reduced by an average of 3.4 points (56% reduction). These studies are in disagreement with a recent meta-analysis, which found that individuals with pain consider a decrease in pain by 2.0 (30% reduction) as clinically meaningful. 15 An important caveat to note, however, is that the results of this meta-analysis were based on a different measure of treatment success, namely “patient global impression of change.”
This study also demonstrated that FP participants had overall lower pain, fatigue, distress, and interference ratings than FM participants and that they required significantly less improvement in fatigue and distress than FM participants. It is likely that this difference between groups is due to the difference in perceived severity of the different disorders. For example, individuals with FM often experience significant global impairments in physical functioning and emotional distress. 16 Moreover, FM is defined by the person reporting widespread pain (involving all 4 limbs and the trunk) and tenderness to digital palpation in at least 11 of 18 pre-determined body areas called tender points. 17 Individuals with FP typically have pain localized to one part of their body, however. Perhaps having a more localized pain condition results in a decreased need for as much of a symptom reduction in multiple domains compared to individuals with widespread pain conditions.18 One important caveat to note here is that individuals with FP had overall lower values than individuals with FM; therefore, the smaller need for improvement could also be a function of lower initial values.
Furthermore, chronic pain populations have been shown to be heterogeneous such that there are individuals who place a higher importance on certain domains. 19 In fact, Robinson and colleagues (2005) performed a cluster analysis on a chronic pain population and found three subgroups: the Pain-Focused group, which places greater importance on pain reduction; the Multifocused-High group, which rates improvement in all domains as extremely important; and the Multifocused-Moderate group, which reports moderate importance ratings across domains. 13 These results suggest that treatment should be tailored to meet patients’ expectations but should also aim for multidimensional treatment success. 20 Therefore the PCO can provide important clinical information and may be used to determine types and focus of treatments for the different pain groups. Future studies will be necessary to further investigate the nature of these differences.
Several limitations of the study should be considered. The sample of the current study consisted predominantly of Caucasian individuals and may have limited the generalizability of findings to a more diverse population. The facial pain sample consisted of heterogeneous facial pain concerns; therefore, there could be individual differences between subsets of the facial pain population (e.g., individuals with migraines versus individuals with temporomandibular joint pain). In addition, detailed information about prior treatments of the patients of this study was not collected. Although beyond the scope of this study, such treatment may have affected PCO ratings and therefore, there may be differences between participants who received prior treatment for their pain condition and those who did not. However, the long duration of their illness (more than 8 years) makes it very unlikely that the majority of FM and FP participants had not received any pain treatments in the past. Furthermore, the PCO questionnaire was completed by participants prior to any defined treatment endpoint, although most patients and healthcare providers would not consider a complete resolution of symptoms (cure) impossible. Thus it was impossible to determine whether participants adjust their ratings in response to treatment modalities and strategies. A longitudinal design in future studies would help elucidate the effect of treatment strategies on PCO ratings.
Conclusions
FM and FP individuals expect more symptom relief from their health care providers than previously known. Reductions of approximately 60% for pain, fatigue, distress, and interference with daily activities are necessary to satisfy their success criteria. Importantly, for FM and FP individuals alike, reductions in pain and fatigue rank higher than improved distress or function. Careful assessments of these important outcome measures are needed to tailor the comprehensive care that most individuals with chronic pain will require. Future research should examine the clinical relevance of differences in pain-related ratings across chronic pain groups, predictors of change, and the presence of further subgroups.
Appendix. Patient-Centered Outcomes Questionnaire
Contributor Information
Lauren A. Stutts, Email: lstutts@phhp.ufl.edu, Center for Pain Research and Behavioral Health, PO Box 100165, Gainesville, FL 32610-0165, Phone: 352.273.5221, Fax: 352.273.6156
Michael E. Robinson, Center for Pain Research and Behavioral Health, PO Box 100165, Gainesville, FL 32610-0165
Robert C. McCulloch, Center for Pain Research and Behavioral Health, PO Box 100165, Gainesville, FL 32610-0165
Evangelia Banou, Center for Pain Research and Behavioral Health, PO Box 100165, Gainesville, FL 32610-0165
Henry A. Gremillion, Department of Oral and Maxillofacial Surgery, PO Box 100437, Gainesville, FL 32610-0437
Lori B. Waxenberg, Center for Pain Research and Behavioral Health, PO Box 100165, Gainesville, FL 32610-0165
Roland Staud, Department of Medicine, PO Box 100221, Gainesville, FL 32610-0221
References
- 1.Verhaak PF, Kerssens JJ, Dekker J, Sorbi MJ, Bensing JM. Prevalence of chronic benign pain disorder among adults: a review of the literature. Pain. 1998;77(3):231–239. doi: 10.1016/S0304-3959(98)00117-1. [DOI] [PubMed] [Google Scholar]
- 2.Rhodus NL, Fricton J, Carlson P, Messner R. Oral symptoms associated with fibromyalgia syndrome. J Rheumatol. 2003;30(8):1841–1845. [PubMed] [Google Scholar]
- 3.Talley RL, Fricton JR, Okeson JP. Broad support evident for the emerging specialty of orofacial pain. J Okla Dent Assoc. 2000;91(1):14–17. [PubMed] [Google Scholar]
- 4.Madland G, Newton-John T, Feinmann C. Chronic idiopathic orofacial pain: I: What is the evidence base? Br Dent J. 2001;191(1):22–24. doi: 10.1038/sj.bdj.4801081. [DOI] [PubMed] [Google Scholar]
- 5.Okeson JP. Nonodontogenic toothache. Tex Dent J Jul. 2000;117(7):64–74. [PubMed] [Google Scholar]
- 6.Laine C, Davidoff F. Patient-centered medicine. A professional evolution Jama. 1996;275(2):152–156. [PubMed] [Google Scholar]
- 7.Hirsh AT, Atchison JW, Berger JJ, et al. Patient satisfaction with treatment for chronic pain: predictors and relationship to compliance. Clin J Pain. 2005;21(4):302–310. doi: 10.1097/01.ajp.0000113057.92184.90. [DOI] [PubMed] [Google Scholar]
- 8.Masi AT, White KP, Pilcher JJ. Person-centered approach to care, teaching, and research in fibromyalgia syndrome: justification from biopsychosocial perspectives in populations. Semin Arthritis Rheum. 2002;32(2):71–93. doi: 10.1053/sarh.2002.33717. [DOI] [PubMed] [Google Scholar]
- 9.Alamo MM, Moral RR, Perula de Torres LA. Evaluation of a patient-centred approach in generalized musculoskeletal chronic pain/fibromyalgia patients in primary care. Patient Educ Couns. 2002;48(1):23–31. doi: 10.1016/s0738-3991(02)00095-2. [DOI] [PubMed] [Google Scholar]
- 10.Brown JL, Edwards PS, Atchison JW, Lafayette-Lucey A, Wittmer V, Robinson ME. Defining patient-centered multidimensional success criteria for treatment of chronic spine pain [published online ahead of print August 28 2007] Pain Med. 2007 doi: 10.1111/j.1526-4637.2007.00357.x. [DOI] [PubMed] [Google Scholar]
- 11.Newsome PR, McGrath C. Patient-centred measures in dental practice: 3. Patient satisfaction. Dent Update. 2007;34(2):87–88. 90. doi: 10.12968/denu.2007.34.2.87. [DOI] [PubMed] [Google Scholar]
- 12.McGrath C, Newsome PR. Patient-centred measures in dental practice: 2. Quality of life. Dent Update. 2007;34(1):41–42. 44. doi: 10.12968/denu.2007.34.1.41. [DOI] [PubMed] [Google Scholar]
- 13.Robinson ME, Brown JL, George SZ, et al. Multidimensional success criteria and expectations for treatment of chronic pain: the patient perspective. Pain Med. 2005;6(5):336–345. doi: 10.1111/j.1526-4637.2005.00059.x. [DOI] [PubMed] [Google Scholar]
- 14.Casarett D, Karlawish J, Sankar P, Hirschman K, Asch DA. Designing pain research from the patient’s perspective: what trial end points are important to patients with chronic pain? Pain Med. 2001;2(4):309–316. doi: 10.1046/j.1526-4637.2001.01041.x. [DOI] [PubMed] [Google Scholar]
- 15.Farrar JT, Young JP, Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–158. doi: 10.1016/S0304-3959(01)00349-9. [DOI] [PubMed] [Google Scholar]
- 16.Wolfe F. Fibromyalgia. Rheum Dis Clin North Am. 1990;16(3):681–698. [PubMed] [Google Scholar]
- 17.Wolfe F, Smythe HA, Yunus MB, et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum. 1990;33(2):160–172. doi: 10.1002/art.1780330203. [DOI] [PubMed] [Google Scholar]
- 18.Staud R, Price DD, Robinson ME, Vierck CJ., Jr Body pain area and pain-related negative affect predict clinical pain intensity in patients with fibromyalgia. J Pain. 2004;5(6):338–343. doi: 10.1016/j.jpain.2004.05.007. [DOI] [PubMed] [Google Scholar]
- 19.Riley JL, 3rd, Robinson ME, Geisser ME, Wittmer VT. Multivariate cluster analysis of the MMPI-2 in chronic low-back pain patients. Clin J Pain. 1993;9(4):248–252. doi: 10.1097/00002508-199312000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Turner JA, Jensen MP, Warms CA, Cardenas DD. Blinding effectiveness and association of pretreatment expectations with pain improvement in a double-blind randomized controlled trial. Pain. 2002;99(1–2):91–99. doi: 10.1016/s0304-3959(02)00060-x. [DOI] [PubMed] [Google Scholar]