Abstract
Like the whole organism, skin follows the process of aging during life-time. Additional to internal factors, several environmental factors, such as solar radiation, considerably contribute to this process. While fundamental mechanisms regarding skin aging are known, new aspects of anti-aging agents such as melatonin are introduced. Melatonin is a hormone produced in the glandula pinealis that follows a circadian light-dependent rhythm of secretion. It has been experimentally implicated in skin functions such as hair cycling and fur pigmentation, and melatonin receptors are expressed in many skin cell types including normal and malignant keratinocytes, melanocytes and fibroblasts. It possesses a wide range of endocrine properties as well as strong antioxidative activity. Regarding UV-induced solar damage, melatonin distinctly counteracts massive generation of reactive oxygen species, mitochondrial and DNA damage. Thus, there is considerable evidence for melatonin to be an effective anti-skin aging compound, and its various properties in this context are described in this review.
Keywords: melatonin, ultraviolet radiation, skin, antioxidative enzymes, oxidative stress, mitochondrial damage, apoptosis
Introduction
Melatonin (N1-acetyl-5-methoxytryptamine) was initially isolated from bovine pineal tissue.1 Subsequently, it was documented that in mammals the nocturnal increase in blood levels of melatonin is almost exclusively a result of its nighttime synthesis and secretion from the pineal gland.2
Considering chronobiological aspects of melatonin, it regulates the circadian day-night-rhythm and seasonal bio-rhythms,3,4 and independent of that, melatonin has been shown in the mammalian system to modulate immune defense responses,5,6 body weight and reproduction4 and to exert tumor growth-inhibitory and anti-jet lag effects.7-10 Additionally, melatonin serves as a direct, receptor-independent potent antioxidant,11-13 a chemotoxicity-reducing agent,14-16 a putative general anti-aging substance17,18 and an anti-cancer agent.19
For decades, investigations concerning occurrence of melatonin in different body compartments revealed that significantly high concentrations are found in the bile fluid,20 bone marrow,21 cerebrospinal fluid,22 ovary,23 eye,24 lymphocytes5 or skin25 and is differentially distributed in subcellular organelles.21,26-28 It was reported that melatonin levels in organs mentioned above may be 10- to 1000-fold higher than in the plasma.27,28 High concentrations of melatonin across different organs suggest an ubiquitous, biologically highly relevant existence of tissue-specific, local melatoninergic systems which have the biological role of counteracting specific tissue-related regional stressors exactly at the place where they occur.20,21,25,27 In the skin, a melatoninergic antioxidative system (MAS) has been recently discovered in a highly differentiated manner regulating skin homeostasis and—very importantly—having the potential to prevent the harmful consequences of UV solar skin damage, i.e., skin aging and skin cancer.25,29,30
Cutaneous Synthesis of Melatonin
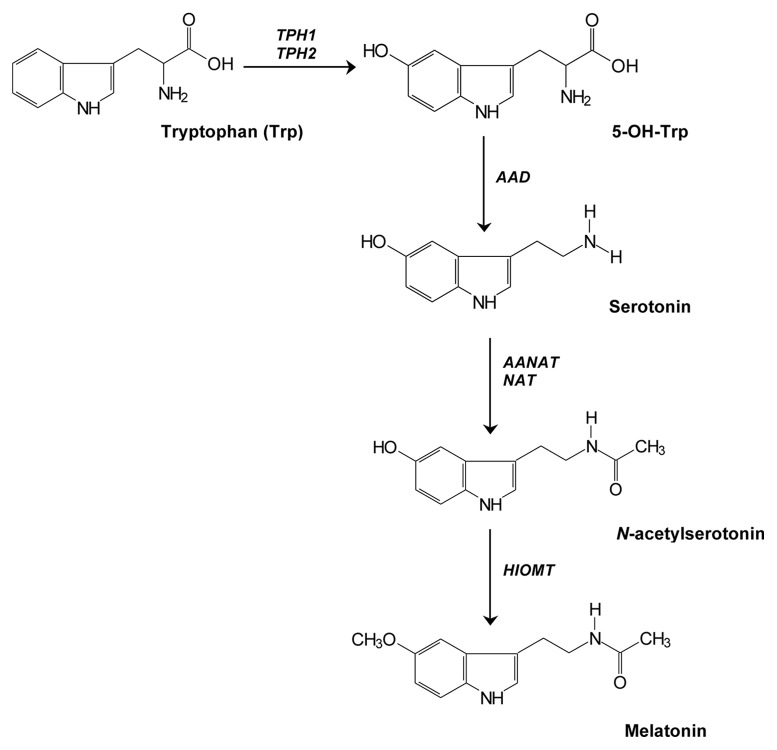
Most of investigations regarding the different aspects of melatonin confirm that, both, biosynthetic and biodegradative pathways of melatonin are observed in whole human and rodent skin and in the major cutaneous cell populations.31 The most important compound for intracutaneous synthesis of melatonin (Fig. 1) is an amino acid, tryptophan (Trp) which is converted by tryptophan hydroxylase (TPH1, TPH2) to 5-OH-Trp and further to serotonin by activity of aromatic amino acid decarboxylase (AAD). In fact, serotonin is essential in the melatonin biosynthesis pathway, nevertheless it has independent biological actions by itself and enters degradation independently of melatonin.32 Subsequently, occurring acetylation of serotonin mediates formation of N-acetylserotonin (NAS) catalyzed by either arylalkylamine N-acetyltransferase (AANAT) and/or arylamine N-acetyltransferase (NAT). Finally, NAS produced in the skin may be released into the circulation or stay in the cutaneous tissue and thereafter could be transformed into melatonin after active hydroxyindole-O-methyltransferase (HIOMT).32,33 Expression of these enzymes has been consistently demonstrated in human skin cells.32
Figure 1. Synthesis of melatonin in the skin. It is involved sequential transformation of tryptophan in a cascade of enzymatic reactions catalyzed by tryptophan hydroxylase (TPH1, TPH2), amino acid decarboxylase (AAD), arylalkylamine N-acetyltransferase (AANAT), arylamine N-acetyltransferase (NAT) and hydroxyindole-O-methyltransferase (HIOMT).
Melatonin Receptors
The hypothesis that all actions of melatonin are mediated via specific receptors in cellular membranes has also been markedly modified in recent years. Previous studies indicated that the receptors for melatonin were primarily located within cells in the suprachiasmatic nuclei (SCN) of the anterior hypothalamus.34 While the cells of the SCN contain large numbers of membrane receptors, they have also been found to be more widely distributed not only in the brain but in many other organs as well.35 This implies evidently that the actions of melatonin are extremely widespread. Phenotypic effects of melatonin can be mediated through interaction with the G protein-coupled membrane bound MT1 and MT2 receptors36 or with nuclear receptors of RZR/ROR subfamily of orphan receptors.37,38 The melatonin receptor type 3 (MT3) has been identified to be the enzyme quinone reductase II (NQO2)39,40 however, an alternative explanation of its role could be the function of melatonin as a co-factor or regulator of the enzyme NQO2.31 Expression of membrane-bound cell surface MT receptors in the skin is variable, depending on the species. For example, skin from the C57BL/6 mouse predominantly or exclusively expresses MT2,41 while human skin expresses both receptors, although with a strong bias toward MT1 (the predominant form found in both whole skin and cultured cells) (Table 1).42,43 Immunocytochemical studies on the human skin showed cell-type- and compartment-dependent expression of MT1 and MT2 proteins (Table 2).31
Table 1. Expression of membrane receptors for melatonin regarding tissue and cell type (adapted from Slominski, et al.42).
| Tissue/cell type | MT1 | MT2 |
|---|---|---|
| Brain (whole tissue) |
+ |
+ |
| Pituitary |
+ |
abberant |
| Adrenal gland |
+ |
- |
| Skin normal |
+ |
- |
| Skin with basal cell carcinoma |
+ |
- |
| Epidermal keratinocytes |
+ |
- |
| Hair follicles keratinocytes |
+ |
- |
| Neonatal keratinocytes |
+ |
+ |
| HaCaT keratinocytes |
- |
abberant |
| Epidermal melanocytes |
+ |
- |
| Hair follicles melanocytes |
- |
- |
| Dermal fibroblasts |
+ |
- |
| Hair follicles papilla fibroblasts | + | abberant |
+, positive; -, negative abberant, alternatively spliced isoform.
Table 2. Localization of membrane MT1 and MT2 receptors for melatonin in human scalp skin (adapted from Slominski, et al.31).
| Localization | MT1 | MT2 |
|---|---|---|
| Epidermis |
++ (Stratum granulosum) + (Stratum spinosum) |
- |
| Eccrine glands |
+++ |
+++ |
| Blood vessels |
+++ (Endothelium) |
++ (Endothelium) |
| Hair follicles | + (Upper outer root sheath) + (Inner root sheath) |
+ (Inner root sheath) |
+, weak; ++, moderate; +++, strong; -, negative.
The nuclear receptor RORα (retinoid-related orphan receptor α) contains at least four splicing variants: RORα1, RORα2, RORα3 and RZRα (RORα4).31,37,38,43 All of the tested skin cells expressed at least one of three RORα isoforms while RORα3 was consistently absent (Table 3).10,31
Table 3. Gene expression of cytosolic melatonin-binding site (MT3/NQO2) and nuclear receptors RORα (including selected isoforms RORα1 and RORα4/RZR that are relevant in normal skin cells and malignant melanoma cells (adapted from Fischer, et al.10; Slominski, et al.31).
| Cells | Species | Detection | Cytosolic melatonin- binding site |
Nuclear receptor |
Nuclear receptor splicing variants |
||
|---|---|---|---|---|---|---|---|
| MT3/NQO2 | RORα | RORα1 | RORα4 (RZRα) |
||||
|
Normal skin cells |
Adult epidermal keratinocytes |
Human |
RT-PCR |
+ |
+ |
- |
+ |
| Neonatal epidermal melanocytes |
RT-PCR |
+ |
+ |
- |
+ |
||
| Adult dermal fibroblasts |
RT-PCR |
+ |
+ |
+ |
+ |
||
| Melanoma cell lines | SKMEL-188 |
Human | RT-PCR |
- |
- |
- |
- |
| WM 164 |
RT-PCR |
+++ |
+ |
- |
+ |
||
| WM 98 |
RT-PCR |
++ |
+ |
- |
+ |
||
| SBCE2 | RT-PCR | + | + | - | + | ||
+, present; -, absent.
Melatonin as an Activity Enhancer of Antioxidative Enzymes
Melatonin was discovered to be a free radical scavenger two decades ago.11 However, the data documenting its ability to overcome oxidative stress has accumulated at a rapid pace and is now abundant.44-46 The efficacy of melatonin in functioning in this capacity relates to its direct free radical scavenging actions.44 The chemical formula of melatonin allows to interact with various forms of free radicals such as H2O2, •OH, singlet oxygen (1O2), superoxide anion (•O2−), peroxynitrite anion (ONOO−) and peroxyl radical (LOO•).12 It should be noted that melatonin’s antioxidant mechanism of action implies a free radical scavengers cascade in case of UV irradiation. Metabolites of melatonin degradation are formed such as N1-acetyl-5-methoxykynuramine (AMK) or N1-acetyl-N2-formyl-5-methoxykynuramine (AFMK), the main photoproducts and simultaneously potent antioxidants.25,47 Moreover, investigations using cell-free melatonin containing systems exposed to UV radiation (UVB: 60%, UVA: 30%) revealed four metabolites identified by HPLC and LC-MS: 2-OH-melatonin, 4-OH-melatonin, 6-OH-melatonin and AFMK.25 Since these metabolites are partly or fully potent antioxidants, this may suggests that melatonin metabolites, unlike classic antioxidants, do not induce prooxidant reactions.
Melatonin acts as a potent antioxidative agent also by indirect effects through enhancing activity of antioxidative enzymes.29 Of note, not only enzyme activity, but also gene transcription of antioxidant enzymes such as manganese superoxide dismutase (Mn-SOD), copper-zinc superoxide dismutase (Cu/Zn-SOD), GPx and gamma-glutamylcysteine synthetase (γ-GCS), the rate-limiting enzyme of glutathione (GSH) synthesis,48-50 was upregulated by melatonin during porphyrin-induced cell damage in rat brain cortex and in neuronal cell lines.48 This prolonged elevation suggests a possible involvement of membrane and/or nuclear melatonin receptor activation with signal transduction on transcriptional mRNA level to modify the regulation of antioxidant enzymes by melatonin following outer signals to stress.51,52
Currently, there are some proposals that melatonin-mediated expression of antioxidant enzymes is dependent of signal transduction pathways related to membrane, cytosolic and nuclear receptors,53 but this hypothesis still needs to be elucidated.
Melatonin as a Protector Against UV-Induced Skin Aging
Because of its broad antioxidant and radical scavenger properties,12 melatonin may act as a protective agent against UV-mediated damage in the skin.25,29 Clinical studies indicated that melatonin is able to prevent sun damage only when it is administrated before UV irradiation to be present in relevant concentrations directly at the irradiation site upon UV exposure.55-57 These melatonin protective effects against UV-induced damage have strong experimental support from in vitro studies.58-63
Melatonin increased cell viability in UV-irradiated fibroblasts by counteracting the formation of polyamine levels,58 and accumulation of malondialdehyde while decreasing apoptosis cells.59 According to investigations performed by Ryoo et al.59 in UV-exposed fibroblasts, only 56% of the cells survived upon UV exposure (140 mJ/cm2), while cells preincubated with 1 nM melatonin revealed a cell survival rate of 92.50% which was paralleled by significant decrease of lipid peroxidation and cell death. Comparative experiments using UV-treated fibroblasts showed similar correlation in cell viability in presence of 100 nM melatonin.58
Moreover, human keratinocytes, the main target cell population in epidermal photodamage, irradiated at increasing doses (10, 25, 50 and 100 mJ/cm2) were investigated for proliferation, colony formation and induction of apoptosis (TUNEL positivity), respectively. Here, melatonin at 10−3 and 10−4 M significantly protected keratinocytes against UV-mediated apoptosis, thus ensuring cell survival.60 Melatonin was also determined as a crucial agent that downregulates expression of genes playing an important role in the execution of UV-induced skin photodamage: aldehyde dehydrogenase 3 type A1, interstitial collagenase (MMP-1), stromelysin 1 (MMP-3) or stromelysin 2 (MMP-10).31 Additionally, melatonin was described as an effective anti-apoptotic compound that inhibits mitochondria-dependent (intrinsic) apoptosis through inhibition of caspase 9 and caspase 3, but does not inhibit the receptor-dependent (extrinsic) pathway of apoptosis mediated by caspase 8.61 It reduces dissipation of mitochondrial transmembrane potential, cleavage of caspases or activation of poly(ADP-ribose) polymerase (PARP), a key DNA-repair-mediating enzyme.61 All these events are supposedly caused by UV-induced mitochondrial ROS (mROS) generation which are effectively reduced by melatonin at the concentrations of 10−6, 10−4 and 10−3 M.61 On a cellular level, melatonin also significantly reduced UV-induced detachment of keratinocytes in culture representative for apoptotic cells. These observations underline the direct and potent protective actions of melatonin in vitro related to molecular and cellular consequences of UV-induced apoptosis.29
Clinical investigations with patients were performed on 20 healthy volunteers who were treated with 0.6 mg/cm2 melatonin or vehicle either 15 min before or 1, 30 or 240 min after UV exposure.54 The irradiation was performed with solar spectrum, i.e., UVA and UVB light at a wavelength range 290–390 nm. UV-mediated erythema was assessed 24 h post-UV by visual score and chromametric method. It was reported that melatonin application 15 min prior to UV-irradiation significantly suppressed erythema compared to treatment with vehicle alone. Interestingly, treatment with melatonin at any time point after UV irradiation did not suppress UV erythema.54 Dose-response investigations revealed that 0.5% melatonin was the most potent suppressive concentration against UV-erythema.55
This observation was confirmed by another series of experiments showing that melatonin, but also other antioxidants (vitamin E and vitamin C) have no effect on UV-erythema when administered after UV-irradiation, irrespective of the time-course of application.57 Taking into account that the UV-induced free radical formation in the skin is an immediate event directly upon UV irradiation, the oxidative stress leading to all known consecutive damaging events in the skin can obviously only be antagonized by antioxidants such as melatonin that are already present at the target sites at the time point of UV-exposure.29,54-56,61
Besides, there is clear evidence that the protective effects of melatonin against photobiological disturbances are mediated by the strong antioxidative properties of this compound. It was shown that melatonin has a higher reduction potential (0.73 V) than vitamin C (0.23 V).62 Interestingly, formation of highly toxic hydroxyl radicals occurred in the presence of certain concentrations of vitamin C, while to date melatonin has not demonstrated such pro-oxidant properties. Considering that UV-induced ROS generation is tightly connected with photodamage, it was shown that melatonin is a significantly stronger scavenger of free radicals compared with vitamin C or Trolox, a vitamin E analog.63
UV-Enhanced Melatonin and Metabolites Production in Skin Cells
To date, the described protective effects of melatonin against UV induced solar skin damage were exclusively shown from investigations with exogenously added melatonin to skin cells. Since in 2002 Slominski et al.32 reported that skin cells of multiple types (normal and immortalized skin keratinocytes, hair follicle keratinocytes, fibroblasts from dermis and hair follicle dermal papilla, melanocytes, melanoma cells and squamous cell carcinoma cell lines) and cutaneous tissue samples from benign as well as malignant skin phenotypes (skin of basal cell carcinoma) express the essential enzymes for melatonin synthesis such as TPH, AANAT and HIOMT, it seemed very likely that melatonin can be produced in the skin as an extrapineal site of melatonin synthesis.32
Systematic investigations in keratinocytes under different experimental conditions of non-melatonin and melatonin supplemented keratinocyte cultures revealed time- and UV-dependent modifications of melatonin production or metabolization to specific melatonin degradants and — of note — definite melatonin detection in keratinocyte cell extracts at defined measurable levels.25 Specifically, it was shown by HPLC of keratinocyte cell extracts that “naïve” (i.e., non-melatonin pre-incubated) keratinocytes showed intracellular melatonin levels of 146.0 pmoles/3 × 106 cells, thus indicating autonomous melatonin synthesis by human keratinocytes at a level of approximately 11 fg per single keratinocyte. Given that the cell volume of a HaCaT keratinocyte is approximately 1.43 × 10−6 µl,64 the calculated intracellular melatonin concentration per keratinocyte, can be appreciated to be around 34 µM. Evaluation of melatonin levels after 24 h of keratinocyte proliferation in culture showed decrease of melatonin down to 65.0 pmoles/3 × 106 cells, while there was a time-parallel increase of the melatonin metabolites 2-hydroxymelatonin from 7.8 pmoles/3 × 106 to 20.4 pmoles/3 × 106 cells and AFMK from 17.4 pmoles/3 × 106 to 33.6 pmoles/3 × 106 cells, thus indicating a 24 h consumption of melatonin with metabolism to above mentioned melatonin metabolites.25 AFMK is also known to have anti-inflammatory properties, e.g., reduction of LPS-induced COX-2 upregulation, decrease of inducible nitric oxide synthase (iNOS) and prostaglandin E2 (PGE2).65 Moreover, AFMK inhibits 5-aminolevulinic acid-induced DNA damage66 and prevents protein destruction,67 therefore representing a potent antioxidative and anti-inflammatory agent against many different types of UV-induced solar damage.
These observations have also to be seen in the context of the study setting in which they were generated. While earlier studies had investigated melatonin metabolites only in UV wavelengths that are not essentially related to UV induced stress in cutaneous biology in naturam (300–575 nm, UV-visible light),68 the above mentioned and more recent studies have developed a human skin related approach by using relevant UV wavelengths within UVB/UVA range and also a mixed UV-source (UVB 60%; UVA 30%) that is closer to the naturally occurring solar irradiation.25
While earlier studies with detection of melatonin metabolites were performed in cell-free systems,69,70 the recent studies with melatonin provided the first evidence for UV-enhanced photolytic and/or enzymatic melatonin metabolism in cultured human keratinocytes.25 Therefore, it can be concluded with almost certainty, that human keratinocytes, and likely the skin and its appendages in vivo themselves as well, are not only targets for protective exogenous melatonin treatment, but also an extrapineal site of melatonin synthesis and of fully functioning local autonomous melatonin metabolism.25,32,42 Since cutaneous local synthesis and metabolism are inducible by UV-irradiation,25 it can be further postulated that the skin provides itself a self-regulated protective system that is switched on by environmental stressors such as UVR and ionizing radiation, and also by inflammation.54,55,57,60,70-74
The Melatoninergic Antioxidative System (MAS) of the Skin
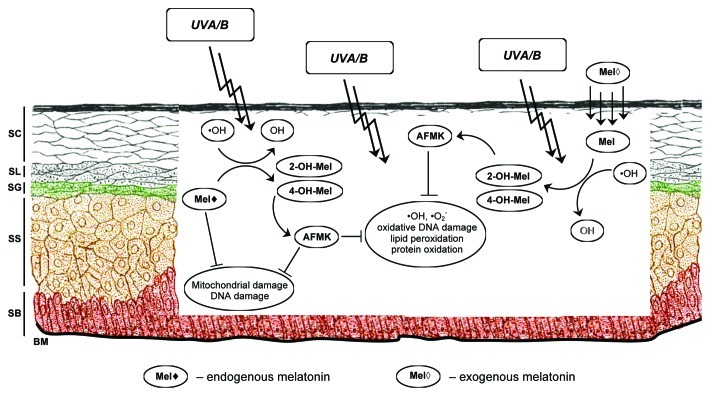
Melatonin is alleged as a major pineal hormone with activity of neurotransmitter, cytokine, antioxidant and global regulator of circadian clock.74 As mentioned before, synthesis of melatonin is not restricted to the pineal gland, but extends also to various other organs including the skin.5,20-25 Since UV-exposed skin mediates melatonin metabolism leading to the generation of antioxidant melatonin metabolites in human keratinocytes that exert strong antioxidative properties themselves, an antioxidative cascade can also be postulated for the skin in analogy to previously described melatonin-related antioxidative cascades in chemical or other tissue homogenate systems.47,69,75 This cascade has been defined as the melatoninergic antioxidative system (MAS) of the skin (Fig. 2) which would protect the skin as an important barrier organ against UV-induced oxidative stress-mediated damaging events on nuclear, subcellular, protein and cell morphology level.25 Regarding the chemical structure, melatonin as well as all metabolites are strongly lipophilic, an important fact which would render them able to diffuse easily in every skin and cell compartment, therefore extending the MAS beyond the epidermis, namely to the dermis and the hair follicle31,76,77 where it represents a defense mechanism against the multifaceted threats of environmental stress, especially UVR, to which the skin is life-long exposed.31,70,78,79
Figure 2. The melatoninergic antioxidative system in human skin. Parallel to directly scavenging UVB-induced reactive oxygen species (ROS), namely hydroxyl radicals, melatonin is transformed to 2-hydroxymelatonin, 4-hydroxymelatonin and consecutively to AFMK. All metabolites are strong antioxidants themselves creating a potent antioxidative cascade that reduces lipid peroxidation, protein oxidation, mitochondrial and DNA damage. SC, stratum corneum; SL, stratum lucida; SG, stratum granulosum; SS, stratum spinosum; SB, stratum basale; BM, basement membrane
One of the most reactive radicals, the hydroxyl radical, occurs under UV irradiation in the skin and reacts directly with melatonin.11,78,80,81 Melatonin is either autonomously produced in epidermal and/or hair follicle keratinocytes where it engages in intracrine signaling/interactions or is released into the extracellular space to regulate auto-, para- or endocrine signaling.25,76,82 The reaction of melatonin with hydroxyl radical induces the formation of 2-OH-melatonin and 4-OH-melatonin which are then further metabolized to AFMK and by arylamine formamidase or catalase to AMK.69,83 The effective scavenging of hydroxyl radicals indirectly or directly mediates the reduction of lipid peroxidation, protein oxidation, mitochondrial damage and DNA damage. This makes the melatoninergic antioxidative cascade very potent in reducing the extensive amounts of free radicals occurring under UV solar radiation and therefore represents a very promising strategy to protect the skin against this main environmental stressor and causative factor for skin aging and tumor promotion.
Conclusions
Aging of skin is a complex process, taking place over the many years of a human life-span. In addition to endogenous factors, several environmental factors contribute to this process and sometimes accelerate aging. Therefore, numerous investigations within dermatological science and especially dermato-endocrinology are having the aim to develop effective anti-aging agents and one of the very highly promising candidates is the indol melatonin. For years and in many investigations, great and convincing evidence revealed that melatonin with its strong antioxidative properties shows a tremendously wide spectrum of action such as bioregulatory as well as pluripotent and essential protective effects in many cells, tissues and compartments of unicells, animals and the human body.47 The predominant feature of melatonin therein is that of a potent cyto- and tissue-protective substance on multiple molecular and cellular damage levels and mechanisms, both in physiological and pharmacological concentrations.27,28,47,82
The fact that the essential enzymes for melatonin synthesis are expressed in skin cells and cutaneous tissue at a great variety, and that skin cells are able to produce autonomously melatonin and to develop metabolism with the generation of metabolites with strong antioxidative properties, renders the skin a major extrapineal site of melatonin production and activity.25,32,42 Moreover, solar UV irradiation is one of the main environmental skin stressors and it is significantly counteracted or modulated by melatonin in the context of a complex intracutaneous melatoninergic antioxidative system of the skin.25,29,30,60,61
Regarding clinical application, exogenous melatonin should rather be used topically than orally, since orally administered melatonin appears in rather low levels in the blood due to prominent first-pass degradation in the liver, thus limiting skin access.84 Topical application might be meaningful, since melatonin can penetrate into the stratum corneum and build there a depot due to its distinct lipophilic chemical structure.85 Therefore, endogenous intracutaneous melatonin production, together with topically applied exogenous melatonin or metabolites can be expected to represent one of the most potent antioxidative defense systems against UV-induced skin aging.25,29-31
Acknowledgments
The authors wish to acknowledge the funding agencies that have supported some of the original work cited in this review: German Academy of Natural Scientists Leopoldina, Halle and Federal Ministry of Education and Research” BMBF-LPD 9901/8-113 (T.W.F.), Foundation “Rene Touraine” Short-Term International Fellowship, France (T.W.F.), Aaron B. Lerner scholarship from the Friedrich-Schiller-University, Jena, Germany (T.W.F.) and University of Tennessee Cancer Center Pilot Grant (T.W.F.). The senior author (T.W.F.) is also grateful to Prof. Andrzej Slominski, who has been the mentor and host of T.W.F. during his research stay at the Department of Pathology and Laboratory Medicine at the University of Tennessee Health Science Center, Memphis, TN USA.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Footnotes
Previously published online: www.landesbioscience.com/journals/dermatoendocrinology/article/22344
References
- 1.Lerner AB, Case JD, Takahashi Y, Lee TH, Mori W. Isolation of melatonin, a pineal factor that lightens melanocytes. J Am Chem Soc. 1958;80:2587. doi: 10.1021/ja01543a060. [DOI] [Google Scholar]
- 2.Reiter RJ. Melatonin: the chemical expression of darkness. Mol Cell Endocrinol. 1991;79:C153–8. doi: 10.1016/0303-7207(91)90087-9. [DOI] [PubMed] [Google Scholar]
- 3.Bubenik GA, Smith PS. Circadian and circannual rhythms of melatonin in plasma of male white-tailed deer and the effect of oral administration of melatonin. J Exp Zool. 1987;241:81–9. doi: 10.1002/jez.1402410110. [DOI] [PubMed] [Google Scholar]
- 4.Lerchl A, Schlatt S. Influence of photoperiod on pineal melatonin synthesis, fur color, body weight, and reproductive function in the female Djungarian hamster, Phodopus sungorus. Neuroendocrinology. 1993;57:359–64. doi: 10.1159/000126380. [DOI] [PubMed] [Google Scholar]
- 5.Carrillo-Vico A, Calvo JR, Abreu P, Lardone PJ, García-Mauriño S, Reiter RJ, et al. Evidence of melatonin synthesis by human lymphocytes and its physiological significance: possible role as intracrine, autocrine, and/or paracrine substance. FASEB J. 2004;18:537–9. doi: 10.1096/fj.03-0694fje. [DOI] [PubMed] [Google Scholar]
- 6.Guerrero JM, Reiter RJ. Melatonin-immune system relationships. Curr Top Med Chem. 2002;2:167–79. doi: 10.2174/1568026023394335. [DOI] [PubMed] [Google Scholar]
- 7.Hu DN, Roberts JE. Melatonin inhibits growth of cultured human uveal melanoma cells. Melanoma Res. 1997;7:27–31. doi: 10.1097/00008390-199702000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Waterhouse J, Reilly T, Atkinson G, Edwards B. Jet lag: trends and coping strategies. Lancet. 2007;369:1117–29. doi: 10.1016/S0140-6736(07)60529-7. [DOI] [PubMed] [Google Scholar]
- 9.Bartsch C, Bartsch H, Karasek M. Melatonin in clinical oncology. Neuro Endocrinol Lett. 2002;23(Suppl 1):30–8. [PubMed] [Google Scholar]
- 10.Fischer TW, Zmijewski MA, Zbytek B, Sweatman TW, Slominski RM, Wortsman J, et al. Oncostatic effects of the indole melatonin and expression of its cytosolic and nuclear receptors in cultured human melanoma cell lines. Int J Oncol. 2006;29:665–72. doi: 10.3892/ijo.29.3.665. [DOI] [PubMed] [Google Scholar]
- 11.Tan DX, Chen LD, Poeggeler B, Manchester LC, Reiter RJ. Melatonin: a potent, endogenous hydroxyl radical scavenger. Endocr J. 1993;1:57–60. [Google Scholar]
- 12.Tan DX, Reiter RJ, Manchester LC, Yan MT, El-Sawi M, Sainz RM, et al. Chemical and physical properties and potential mechanisms: melatonin as a broad spectrum antioxidant and free radical scavenger. Curr Top Med Chem. 2002;2:181–97. doi: 10.2174/1568026023394443. [DOI] [PubMed] [Google Scholar]
- 13.Reiter RJ, Tan DX, Poeggeler B, Menendez-Pelaez A, Chen LD, Saarela S. Melatonin as a free radical scavenger: implications for aging and age-related diseases. Ann N Y Acad Sci. 1994;719:1–12. doi: 10.1111/j.1749-6632.1994.tb56817.x. [DOI] [PubMed] [Google Scholar]
- 14.Reiter RJ, Tan DX, Sainz RM, Mayo JC, Lopez-Burillo S. Melatonin: reducing the toxicity and increasing the efficacy of drugs. J Pharm Pharmacol. 2002;54:1299–321. doi: 10.1211/002235702760345374. [DOI] [PubMed] [Google Scholar]
- 15.Oz E, Erbaş D, Sürücü HS, Düzgün E. Prevention of doxorubicin-induced cardiotoxicity by melatonin. Mol Cell Biochem. 2006;282:31–7. doi: 10.1007/s11010-006-1153-9. [DOI] [PubMed] [Google Scholar]
- 16.Parlakpinar H, Ozer MK, Sahna E, Vardi N, Cigremis Y, Acet A. Amikacin-induced acute renal injury in rats: protective role of melatonin. J Pineal Res. 2003;35:85–90. doi: 10.1034/j.1600-079X.2003.00059.x. [DOI] [PubMed] [Google Scholar]
- 17.Karasek M, Reiter RJ. Melatonin and aging. Neuro Endocrinol Lett. 2002;23(Suppl 1):14–6. [PubMed] [Google Scholar]
- 18.Reiter RJ, Tan DX, Manchester LC, El-Sawi MR. Melatonin reduces oxidant damage and promotes mitochondrial respiration: implications for aging. Ann N Y Acad Sci. 2002;959:238–50. doi: 10.1111/j.1749-6632.2002.tb02096.x. [DOI] [PubMed] [Google Scholar]
- 19.Karbownik M. Potential anticarcinogenic action of melatonin and other antioxidants mediated by antioxidative mechanisms. Neuro Endocrinol Lett. 2002;23(Suppl 1):39–44. [PubMed] [Google Scholar]
- 20.Tan D, Manchester LC, Reiter RJ, Qi W, Hanes MA, Farley NJ. High physiological levels of melatonin in the bile of mammals. Life Sci. 1999;65:2523–9. doi: 10.1016/S0024-3205(99)00519-6. [DOI] [PubMed] [Google Scholar]
- 21.Tan DX, Manchester LC, Reiter RJ, Qi WB, Zhang M, Weintraub ST, et al. Identification of highly elevated levels of melatonin in bone marrow: its origin and significance. Biochim Biophys Acta. 1999;1472:206–14. doi: 10.1016/S0304-4165(99)00125-7. [DOI] [PubMed] [Google Scholar]
- 22.Skinner DC, Malpaux B. High melatonin concentrations in third ventricular cerebrospinal fluid are not due to Galen vein blood recirculating through the choroid plexus. Endocrinology. 1999;140:4399–405. doi: 10.1210/en.140.10.4399. [DOI] [PubMed] [Google Scholar]
- 23.Itoh MT, Ishizuka B, Kuribayashi Y, Amemiya A, Sumi Y. Melatonin, its precursors, and synthesizing enzyme activities in the human ovary. Mol Hum Reprod. 1999;5:402–8. doi: 10.1093/molehr/5.5.402. [DOI] [PubMed] [Google Scholar]
- 24.Cahill GM, Besharse JC. Light-sensitive melatonin synthesis by Xenopus photoreceptors after destruction of the inner retina. Vis Neurosci. 1992;8:487–90. doi: 10.1017/S0952523800005009. [DOI] [PubMed] [Google Scholar]
- 25.Fischer TW, Sweatman TW, Semak I, Sayre RM, Wortsman J, Slominski A. Constitutive and UV-induced metabolism of melatonin in keratinocytes and cell-free systems. FASEB J. 2006;20:1564–6. doi: 10.1096/fj.05-5227fje. [DOI] [PubMed] [Google Scholar]
- 26.Menendez-Pelaez A, Reiter RJ. Distribution of melatonin in mammalian tissues: the relative importance of nuclear versus cytosolic localization. J Pineal Res. 1993;15:59–69. doi: 10.1111/j.1600-079X.1993.tb00511.x. [DOI] [PubMed] [Google Scholar]
- 27.Reiter RJ, Tan DX. What constitutes a physiological concentration of melatonin? J Pineal Res. 2003;34:79–80. doi: 10.1034/j.1600-079X.2003.2e114.x. [DOI] [PubMed] [Google Scholar]
- 28.Reiter RJ, Tan DX, Maldonado MD. Melatonin as an antioxidant: physiology versus pharmacology. J Pineal Res. 2005;39:215–6. doi: 10.1111/j.1600-079X.2005.00261.x. [DOI] [PubMed] [Google Scholar]
- 29.Fischer TW, Slominski A, Zmijewski MA, Reiter RJ, Paus R. Melatonin as a major skin protectant: from free radical scavenging to DNA damage repair. Exp Dermatol. 2008;17:713–30. doi: 10.1111/j.1600-0625.2008.00767.x. [DOI] [PubMed] [Google Scholar]
- 30.Slominski A, Wortsman J, Tobin DJ. The cutaneous serotoninergic/melatoninergic system: securing a place under the sun. FASEB J. 2005;19:176–94. doi: 10.1096/fj.04-2079rev. [DOI] [PubMed] [Google Scholar]
- 31.Slominski A, Fischer TW, Zmijewski MA, Wortsman J, Semak I, Zbytek B, et al. On the role of melatonin in skin physiology and pathology. Endocrine. 2005;27:137–48. doi: 10.1385/ENDO:27:2:137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Slominski A, Pisarchik A, Semak I, Sweatman T, Wortsman J, Szczesniewski A, et al. Serotoninergic and melatoninergic systems are fully expressed in human skin. FASEB J. 2002;16:896–8. doi: 10.1096/fj.01-0952fje. [DOI] [PubMed] [Google Scholar]
- 33.Conti A, Conconi S, Hertens E, Skwarlo-Sonta K, Markowska M, Maestroni JM. Evidence for melatonin synthesis in mouse and human bone marrow cells. J Pineal Res. 2000;28:193–202. doi: 10.1034/j.1600-079X.2000.280401.x. [DOI] [PubMed] [Google Scholar]
- 34.Reppert SM, Weaver DR, Ebisawa T. Cloning and characterization of a mammalian melatonin receptor that mediates reproductive and circadian responses. Neuron. 1994;13:1177–85. doi: 10.1016/0896-6273(94)90055-8. [DOI] [PubMed] [Google Scholar]
- 35.Witt-Enderby PA, Radio NM, Doctor JS, Davis VL. Therapeutic treatments potentially mediated by melatonin receptors: potential clinical uses in the prevention of osteoporosis, cancer and as an adjuvant therapy. J Pineal Res. 2006;41:297–305. doi: 10.1111/j.1600-079X.2006.00369.x. [DOI] [PubMed] [Google Scholar]
- 36.Dubocovich ML, Rivera-Bermudez MA, Gerdin MJ, Masana MI. Molecular pharmacology, regulation and function of mammalian melatonin receptors. Front Biosci. 2003;8:d1093–108. doi: 10.2741/1089. [DOI] [PubMed] [Google Scholar]
- 37.Becker-André M, Wiesenberg I, Schaeren-Wiemers N, André E, Missbach M, Saurat JH, et al. Pineal gland hormone melatonin binds and activates an orphan of the nuclear receptor superfamily. J Biol Chem. 1994;269:28531–4. [PubMed] [Google Scholar]
- 38.Carlberg C, Hooft van Huijsduijnen R, Staple JK, DeLamarter JF, Becker-André M. RZRs, a new family of retinoid-related orphan receptors that function as both monomers and homodimers. Mol Endocrinol. 1994;8:757–70. doi: 10.1210/me.8.6.757. [DOI] [PubMed] [Google Scholar]
- 39.Nosjean O, Ferro M, Coge F, Beauverger P, Henlin JM, Lefoulon F, et al. Identification of the melatonin-binding site MT3 as the quinone reductase 2. J Biol Chem. 2000;275:31311–7. doi: 10.1074/jbc.M005141200. [DOI] [PubMed] [Google Scholar]
- 40.Nosjean O, Nicolas JP, Klupsch F, Delagrange P, Canet E, Boutin JA. Comparative pharmacological studies of melatonin receptors: MT1, MT2 and MT3/QR2. Tissue distribution of MT3/QR2. Biochem Pharmacol. 2001;61:1369–79. doi: 10.1016/S0006-2952(01)00615-3. [DOI] [PubMed] [Google Scholar]
- 41.Slominski A, Pisarchik A, Wortsman J. Expression of genes coding melatonin and serotonin receptors in rodent skin. Biochim Biophys Acta. 2004;1680:67–70. doi: 10.1016/j.bbaexp.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 42.Slominski A, Pisarchik A, Zbytek B, Tobin DJ, Kauser S, Wortsman J. Functional activity of serotoninergic and melatoninergic systems expressed in the skin. J Cell Physiol. 2003;196:144–53. doi: 10.1002/jcp.10287. [DOI] [PubMed] [Google Scholar]
- 43.Pozo D, García-Mauriño S, Guerrero JM, Calvo JR. mRNA expression of nuclear receptor RZR/RORalpha, melatonin membrane receptor MT, and hydroxindole-O-methyltransferase in different populations of human immune cells. J Pineal Res. 2004;37:48–54. doi: 10.1111/j.1600-079X.2004.00135.x. [DOI] [PubMed] [Google Scholar]
- 44.Allegra M, Reiter RJ, Tan DX, Gentile C, Tesoriere L, Livrea MA. The chemistry of melatonin’s interaction with reactive species. J Pineal Res. 2003;34:1–10. doi: 10.1034/j.1600-079X.2003.02112.x. [DOI] [PubMed] [Google Scholar]
- 45.Hardeland R, Coto-Montes A, Poeggeler B. Circadian rhythms, oxidative stress, and antioxidative defense mechanisms. Chronobiol Int. 2003;20:921–62. doi: 10.1081/CBI-120025245. [DOI] [PubMed] [Google Scholar]
- 46.Hardeland R, Pandi Perumal SR. Melatonin, a potent agent in antioxidative defense: actions as a natural food contaminant, gastrointestinal factor, drug and prodrug. Nutr Metab. 2005;2:22. doi: 10.1186/1743-7075-2-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tan DX, Manchester LC, Terron MP, Flores LJ, Reiter RJ. One molecule, many derivatives: a never-ending interaction of melatonin with reactive oxygen and nitrogen species? J Pineal Res. 2007;42:28–42. doi: 10.1111/j.1600-079X.2006.00407.x. [DOI] [PubMed] [Google Scholar]
- 48.Antolín I, Rodríguez C, Saínz RM, Mayo JC, Uría H, Kotler ML, et al. Neurohormone melatonin prevents cell damage: effect on gene expression for antioxidant enzymes. FASEB J. 1996;10:882–90. doi: 10.1096/fasebj.10.8.8666165. [DOI] [PubMed] [Google Scholar]
- 49.Kotler M, Rodríguez C, Sáinz RM, Antolín I, Menéndez-Peláez A. Melatonin increases gene expression for antioxidant enzymes in rat brain cortex. J Pineal Res. 1998;24:83–9. doi: 10.1111/j.1600-079X.1998.tb00371.x. [DOI] [PubMed] [Google Scholar]
- 50.Urata Y, Honma S, Goto S, Todoroki S, Iida T, Cho S, et al. Melatonin induces gamma-glutamylcysteine synthetase mediated by activator protein-1 in human vascular endothelial cells. Free Radic Biol Med. 1999;27:838–47. doi: 10.1016/S0891-5849(99)00131-8. [DOI] [PubMed] [Google Scholar]
- 51.Rodriguez C, Mayo JC, Sainz RM, Antolín I, Herrera F, Martín V, et al. Regulation of antioxidant enzymes: a significant role for melatonin. J Pineal Res. 2004;36:1–9. doi: 10.1046/j.1600-079X.2003.00092.x. [DOI] [PubMed] [Google Scholar]
- 52.Martín V, Sainz RM, Antolín I, Mayo JC, Herrera F, Rodríguez C. Several antioxidant pathways are involved in astrocyte protection by melatonin. J Pineal Res. 2002;33:204–12. doi: 10.1034/j.1600-079X.2002.02113.x. [DOI] [PubMed] [Google Scholar]
- 53.Tomás-Zapico C, Antonio Boga J, Caballero B, Vega-Naredo I, Sierra V, Alvarez-García O, et al. Coexpression of MT1 and RORalpha1 melatonin receptors in the Syrian hamster Harderian gland. J Pineal Res. 2005;39:21–6. doi: 10.1111/j.1600-079X.2005.00210.x. [DOI] [PubMed] [Google Scholar]
- 54.Bangha E, Elsner P, Kistler GS. Suppression of UV-induced erythema by topical treatment with melatonin (N-acetyl-5-methoxytryptamine). Influence of the application time point. Dermatology. 1997;195:248–52. doi: 10.1159/000245953. [DOI] [PubMed] [Google Scholar]
- 55.Bangha E, Elsner P, Kistler GS. Suppression of UV-induced erythema by topical treatment with melatonin (N-acetyl-5-methoxytryptamine). A dose response study. Arch Dermatol Res. 1996;288:522–6. doi: 10.1007/BF02505248. [DOI] [PubMed] [Google Scholar]
- 56.Dreher F, Denig N, Gabard B, Schwindt DA, Maibach HI. Effect of topical antioxidants on UV-induced erythema formation when administered after exposure. Dermatology. 1999;198:52–5. doi: 10.1159/000018064. [DOI] [PubMed] [Google Scholar]
- 57.Dreher F, Gabard B, Schwindt DA, Maibach HI. Topical melatonin in combination with vitamins E and C protects skin from ultraviolet-induced erythema: a human study in vivo. Br J Dermatol. 1998;139:332–9. doi: 10.1046/j.1365-2133.1998.02447.x. [DOI] [PubMed] [Google Scholar]
- 58.Lee KS, Lee WS, Suh SI, Kim SP, Lee SR, Ryoo YW, et al. Melatonin reduces ultraviolet-B induced cell damages and polyamine levels in human skin fibroblasts in culture. Exp Mol Med. 2003;35:263–8. doi: 10.1038/emm.2003.35. [DOI] [PubMed] [Google Scholar]
- 59.Ryoo YW, Suh SI, Mun KC, Kim BC, Lee KS. The effects of the melatonin on ultraviolet-B irradiated cultured dermal fibroblasts. J Dermatol Sci. 2001;27:162–9. doi: 10.1016/S0923-1811(01)00133-5. [DOI] [PubMed] [Google Scholar]
- 60.Fischer TW, Zbytek B, Sayre RM, Apostolov EO, Basnakian AG, Sweatman TW, et al. Melatonin increases survival of HaCaT keratinocytes by suppressing UV-induced apoptosis. J Pineal Res. 2006;40:18–26. doi: 10.1111/j.1600-079X.2005.00273.x. [DOI] [PubMed] [Google Scholar]
- 61.Fischer TW, Zmijewski MA, Wortsman J, Slominski A. Melatonin maintains mitochondrial membrane potential and attenuates activation of initiator (casp-9) and effector caspases (casp-3/casp-7) and PARP in UVR-exposed HaCaT keratinocytes. J Pineal Res. 2008;44:397–407. doi: 10.1111/j.1600-079X.2007.00542.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Fischer TW, Scholz G, Knöll B, Hipler UC, Elsner P. Melatonin suppresses reactive oxygen species induced by UV irradiation in leukocytes. J Pineal Res. 2004;37:107–12. doi: 10.1111/j.1600-079X.2004.00142.x. [DOI] [PubMed] [Google Scholar]
- 63.Fischer TW, Scholz G, Knöll B, Hipler UC, Elsner P. Melatonin suppresses reactive oxygen species in UV-irradiated leukocytes more than vitamin C and trolox. Skin Pharmacol Appl Skin Physiol. 2002;15:367–73. doi: 10.1159/000064543. [DOI] [PubMed] [Google Scholar]
- 64.Watt FM, Jordan PW, O’Neill CH. Cell shape controls terminal differentiation of human epidermal keratinocytes. Proc Natl Acad Sci U S A. 1988;85:5576–80. doi: 10.1073/pnas.85.15.5576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mayo JC, Sainz RM, Tan DX, Hardeland R, Leon J, Rodriguez C, et al. Anti-inflammatory actions of melatonin and its metabolites, N1-acetyl-N2-formyl-5-methoxykynuramine (AFMK) and N1-acetyl-5-methoxykynuramine (AMK), in macrophages. J Neuroimmunol. 2005;165:139–49. doi: 10.1016/j.jneuroim.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 66.Onuki J, Almeida EA, Medeiros MH, Di Mascio P. Inhibition of 5-aminolevulinic acid-induced DNA damage by melatonin, N1-acetyl-N2-formyl-5-methoxykynuramine, quercetin or resveratrol. J Pineal Res. 2005;38:107–15. doi: 10.1111/j.1600-079X.2004.00180.x. [DOI] [PubMed] [Google Scholar]
- 67.Ressmeyer AR, Mayo JC, Zelosko V, Sáinz RM, Tan DX, Poeggeler B, et al. Antioxidant properties of the melatonin metabolite N1-acetyl-5-methoxykynuramine (AMK): scavenging of free radicals and prevention of protein destruction. Redox Rep. 2003;8:205–13. doi: 10.1179/135100003225002709. [DOI] [PubMed] [Google Scholar]
- 68.Maharaj DS, Anoopkumar-Dukie S, Glass BD, Antunes EM, Lack B, Walker RB, et al. The identification of the UV degradants of melatonin and their ability to scavenge free radicals. J Pineal Res. 2002;32:257–61. doi: 10.1034/j.1600-079X.2002.01866.x. [DOI] [PubMed] [Google Scholar]
- 69.Tan DX, Manchester LC, Burkhardt S, Sainz RM, Mayo JC, Kohen R, et al. N1-acetyl-N2-formyl-5-methoxykynuramine, a biogenic amine and melatonin metabolite, functions as a potent antioxidant. FASEB J. 2001;15:2294–6. doi: 10.1096/fj.01-0309fje. [DOI] [PubMed] [Google Scholar]
- 70.Fischer TW, Elsner P. The antioxidative potential of melatonin in the skin. Curr Probl Dermatol. 2001;29:165–74. doi: 10.1159/000060665. [DOI] [PubMed] [Google Scholar]
- 71.Wiesenberg I, Missbach M, Carlberg C. The potential role of the transcription factor RZR/ROR as a mediator of nuclear melatonin signaling. Restor Neurol Neurosci. 1998;12:143–50. [PubMed] [Google Scholar]
- 72.Kim BC, Shon BS, Ryoo YW, Kim SP, Lee KS. Melatonin reduces X-ray irradiation-induced oxidative damages in cultured human skin fibroblasts. J Dermatol Sci. 2001;26:194–200. doi: 10.1016/S0923-1811(01)00088-3. [DOI] [PubMed] [Google Scholar]
- 73.Slominski A, Chassalevris N, Mazurkiewicz J, Maurer M, Paus R. Murine skin as a target for melatonin bioregulation. Exp Dermatol. 1994;3:45–50. doi: 10.1111/j.1600-0625.1994.tb00265.x. [DOI] [PubMed] [Google Scholar]
- 74.Kleszczyński K, Hardkop LH, Fischer TW. Differential effects of melatonin as a broad range UV-damage preventive dermato-endocrine regulator. Dermatoendocrinol. 2011;3:27–31. doi: 10.4161/derm.3.1.14842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tan DX, Manchester LC, Reiter RJ, Qi WB, Karbownik M, Calvo JR. Significance of melatonin in antioxidative defense system: reactions and products. Biol Signals Recept. 2000;9:137–59. doi: 10.1159/000014635. [DOI] [PubMed] [Google Scholar]
- 76.Kobayashi H, Kromminga A, Dunlop TW, Tychsen B, Conrad F, Suzuki N, et al. A role of melatonin in neuroectodermal-mesodermal interactions: the hair follicle synthesizes melatonin and expresses functional melatonin receptors. FASEB J. 2005;19:1710–2. doi: 10.1096/fj.04-2293fje. [DOI] [PubMed] [Google Scholar]
- 77.Fischer TW, Slominski A, Tobin DJ, Paus R. Melatonin and the hair follicle. J Pineal Res. 2008;44:1–15. doi: 10.1111/j.1600-079X.2007.00512.x. [DOI] [PubMed] [Google Scholar]
- 78.Scharffetter-Kochanek K, Wlaschek M, Brenneisen P, Schauen M, Blaudschun R, Wenk J. UV-induced reactive oxygen species in photocarcinogenesis and photoaging. Biol Chem. 1997;378:1247–57. [PubMed] [Google Scholar]
- 79.Scharffetter-Kochanek K, Wlaschek M, Briviba K, Sies H. Singlet oxygen induces collagenase expression in human skin fibroblasts. FEBS Lett. 1993;331:304–6. doi: 10.1016/0014-5793(93)80357-Z. [DOI] [PubMed] [Google Scholar]
- 80.Krutmann J, Grewe M. Involvement of cytokines, DNA damage, and reactive oxygen intermediates in ultraviolet radiation-induced modulation of intercellular adhesion molecule-1 expression. J Invest Dermatol. 1995;105(Suppl):67S–70S. doi: 10.1038/jid.1995.14. [DOI] [PubMed] [Google Scholar]
- 81.Berneburg M, Grether-Beck S, Kürten V, Ruzicka T, Briviba K, Sies H, et al. Singlet oxygen mediates the UVA-induced generation of the photoaging-associated mitochondrial common deletion. J Biol Chem. 1999;274:15345–9. doi: 10.1074/jbc.274.22.15345. [DOI] [PubMed] [Google Scholar]
- 82.Tan DX, Manchester LC, Hardeland R, Lopez-Burillo S, Mayo JC, Sainz RM, et al. Melatonin: a hormone, a tissue factor, an autocoid, a paracoid, and an antioxidant vitamin. J Pineal Res. 2003;34:75–8. doi: 10.1034/j.1600-079X.2003.02111.x. [DOI] [PubMed] [Google Scholar]
- 83.Hardeland R, Reiter RJ, Poeggeler B, Tan DX. The significance of the metabolism of the neurohormone melatonin: antioxidative protection and formation of bioactive substances. Neurosci Biobehav Rev. 1993;17:347–57. doi: 10.1016/S0149-7634(05)80016-8. [DOI] [PubMed] [Google Scholar]
- 84.Arendt J. Melatonin. Clin Endocrinol (Oxf) 1988;29:205–29. doi: 10.1111/j.1365-2265.1988.tb00263.x. [DOI] [PubMed] [Google Scholar]
- 85.Fischer TW, Greif C, Fluhr JW, Wigger-Alberti W, Elsner P. Percutaneous penetration of topically applied melatonin in a cream and an alcoholic solution. Skin Pharmacol Physiol. 2004;17:190–4. doi: 10.1159/000078822. [DOI] [PubMed] [Google Scholar]