Abstract
Background
Although health disparity research has investigated social structural, cultural, or psychological factors, the interrelations among these factors deserve greater attention.
Purpose
This study aims to examine cancer screening emotions and their relations to screening fatalism as determinants of breast cancer screening among women from diverse socioeconomic and ethnic backgrounds.
Methods
An integrative conceptual framework was used to test the multivariate relations among socioeconomic status, age, screening fatalism, screening emotions, and clinical breast exam compliance among 281 Latino and Anglo women, using multi-group structural equation causal modeling.
Results
Screening emotions and screening fatalism had a negative, direct influence on clinical breast exam compliance for both ethnic groups. Still, ethnicity moderated the indirect effect of screening fatalism on clinical breast exam compliance through screening emotions.
Conclusions
Integrative conceptual frameworks and multivariate methods may shed light on the complex relations among factors influencing health behaviors relevant to disparities. Future research and intervention must recognize this complexity when working with diverse populations.
Keywords: Emotions, Culture, Fatalism, Breast cancer screening, Health disparities
Introduction
In response to the US Preventive Services Task Force changes to mammography screening guidelines, the National Cancer Institute [1] recently suggested that women should consult with their healthcare professionals to discuss their individual benefits and risks prior to deciding when and how often they should have mammograms. These changes suggest that some patients may choose to forgo mammography and instead elect to have a clinical breast exam after consulting with their health professional. Therefore, understanding the factors that encourage or discourage women from consulting with their healthcare professionals and having a clinical breast exam may become more important than in the past. This may be particularly so in the case of Latin American (Latino)1 women in the USA, who already report lower rates of screening compared to non-Latino White (Anglo)2 women. In fact, disparities in breast cancer screening between Latino and Anglo women have increased during the last decade [3, 4]. Latino women were also more likely to present with breast cancer at stages III and IV [5, 6], and consistent with findings regarding socioeconomic status (SES)-related disparities, Latinas from lower as compared to higher income levels were more likely to be diagnosed at later stages [7].
Understanding health behaviors such as cancer screening within the context of a culturally diverse population requires that the interrelations among psychological, cultural, and social structural factors be considered [8]. Still, research in this area often focuses on either social structural, cultural, or psychological factors as determinants of breast cancer screening. Specifically, while some studies have focused on the role of emotions as motivators and/or deterrents of health behavior [9, 10], others have focused on the effects of access to care [11] or cultural beliefs [3, 12]. This represents an important limitation for understanding complex phenomena in this area, such as the potential role of culture in psychological processes (e.g., emotions), which may in turn impact health behavior. Such phenomena may actually explain why findings from research regarding the role of culture in cancer screening are mixed [3]. For instance, some studies have found that fatalistic beliefs predict lowered usage of self-breast exams, clinical breast exams, and Pap tests among Latino women [13, 14], whereas others have not found a direct relationship between fatalism and cancer screening [15]. Those that do not find direct relationships between aspects of culture and health behavior may conclude that culture does not influence behavior. However, this view may change when research considers the possibility that culture influences psychological processes, such as emotions, which may in turn influence health behavior. In fact, research suggests that variations in emotional response among Anglo and Latino women may account for differences in cancer screening [16].
Research has found that some ethnic minority populations such as Latinos [3] and African Americans [17] experience higher levels of negative cancer emotions compared to Anglo Americans, suggesting that the experience of emotions may differ as a function of ethnicity [18, 19]. However, research concerning the influence of emotions on cancer screening often times controls for ethnicity. Such research does not take into consideration the potential moderating role of ethnicity on the relations between cancer emotions and screening behavior. Furthermore, since cultural values and beliefs have been found to influence emotions [20], it is possible that ethnic variations in screening emotions may be in part a function of cultural factors.
The Structure of Relations Among Social, Cultural, and Psychological Factors Influencing Health Behavior: an Integrative Theoretical Framework
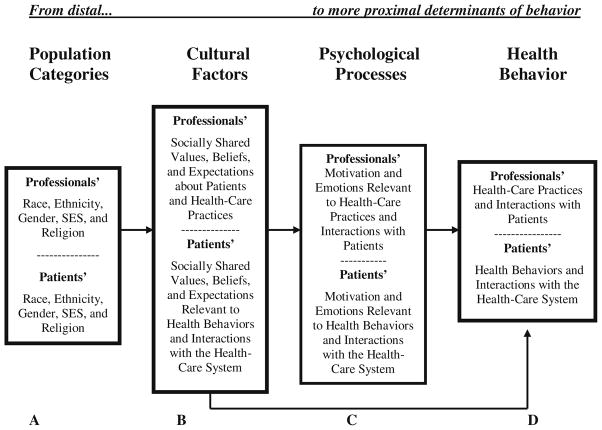
Gallo, Smith, and Cox [8] argue that in order to better understand the role of psychological and social determinants of health behaviors, an integrative theoretical framework is necessary. In fact, previous research in this area has suggested that theoretical models and multivariate methods are needed in order to account for the complexity of relations among psychological, social structural, and cultural determinants of health behaviors [3]. The present research is guided by a theoretical model (see Fig. 1) for the study of culture, psychological processes, and health behavior that provides a theoretical framework for understanding ethnic and socioeconomic health disparities [21, 22]. The model can be used to better understand the health behaviors of culturally diverse patients as well as their health professionals. In the present study, only the aspects of the model corresponding to the patients were examined.
Fig. 1.
Betancourt’s model of culture, psychological processes, and behavior adapted for the study of health behavior [21]
An important underlying principle of the model is that relations among the variables conceived as determinants of health behavior are structured from most distal to more proximal (moving from A to D), with proximity to behavior determining a greater impact. According to the model, health behavior (D) is a function of psychological processes such as emotions (C), which are experienced at the individual level. These psychological processes are the most proximal determinants and therefore have the greatest influence on behavior. Health behavior (D) is also associated with culture, which is defined here in terms of aspects such as value orientations, beliefs, and norms that are socially shared among individuals from a particular population or society (B). These aspects of culture (e.g., fatalistic beliefs) may be directly or indirectly associated with health behavior through psychological processes (C). Moving further away from behavior are social categories such as race, ethnicity, age, and SES (A), which represent sources of cultural variation. However, these social categories are more distal determinants and may not necessarily be directly associated with a particular health behavior.
A number of factors such as race/ethnicity, access to care, education, income, age [11], and language barriers [23] have been identified as relevant to cancer screening disparities. According to the conceptual model represented in Fig. 1, these social structural factors are more likely to be associated with variations in aspects of culture rather than directly with health behavior. In fact, research indicates that ethnicity, income, age [24], and education [25] are all factors associated with fatalistic beliefs about cancer and cancer prevention.
Cultural variables such as fatalism have been examined in relation to health behavior in several studies [13–15, 25, 26]. Although the definitions vary [27], fatalism has been generally described as a cultural value orientation characterized by a set of beliefs around the view that life events are inevitable and that one’s destiny is not within one’s own hands [28]. Much of the research identifies this cultural belief with ethnicity. However, based on our definition of culture, beliefs, values, expectations, norms, and practices are considered cultural when they are socially shared. In fact, the category defining the population or group could be race, ethnicity, age, gender, or any other group for that matter. Moreover, many of these social structural categories often times overlap with one another (e.g., many ethnic minorities are overrepresented at lower SES levels). Therefore, fatalistic beliefs may be to a large extent a function of social structural barriers such as lower education and income rather than ethnicity per se [27]. Thus, research should test the role of education, income, and age along with ethnicity as sources of variation in fatalistic cultural beliefs rather than as direct determinants of screening behavior. In doing so, the relative impact of these variables as sources of cultural variation can be delineated and their relation to emotions and health behavior can be better understood.
Borrayo and Guarnaccia [29] indicate that a common problem in research methodology in this area is the failure to examine confounding relationships between social structural variables and cultural beliefs. In fact, variables such as SES and ethnicity are more likely to be controlled for rather than directly investigated to better understand their influence on health behaviors. Tov and Diener [30] argue that since these variables are associated with cultural beliefs, controlling for them actually results in the removal of cultural effects. As a result, when research controls for these social structural variables and predicts health behaviors based on cultural variables that had some of the cultural effects removed, results are likely to reveal less significant findings concerning the role of culture. Still, some studies have found significant effects for these cultural beliefs after controlling for social structural factors [24, 25], while others have not [15, 31]. These nonsignificant findings, however, may have more to do with research that does not employ methodological and statistical approaches that specifically investigate the interrelations among social structural categories, aspects of culture, psychological processes, and health behavior.
The Present Study
The purpose of this research was to examine the interrelations among screening emotions, screening fatalism, and related social structural factors as determinants of clinical breast exam compliance among culturally diverse women in Southern California. To ensure that the complexity of relations among these variables were properly understood, multi-group structural equation modeling was employed to test both the direct and indirect effects of the study variables on health behavior as well as the potential moderating role of ethnicity.
Consistent with the conceptual model guiding the research, it was hypothesized that clinical breast exam compliance would be a function of both screening emotions and screening fatalism for both Latino and Anglo women. Specifically, higher levels of screening emotions and screening fatalism were expected to negatively impact clinical breast exam compliance. It was also hypothesized that the effect of screening fatalism on clinical breast exam compliance was, at least in part indirect, through its effects on screening emotions. Higher levels of screening fatalism were expected to positively impact negative screening emotions, which would in turn negatively impact clinical breast exam compliance. Finally, consistent with research concerning the higher level of negative screening emotions among Latino women [3], it was expected that the role of screening emotions and screening fatalism as determinants of clinical breast exam compliance would be moderated by ethnicity.
Method
Participants and Procedures
Multi-stage, stratified sampling was conducted to obtain nearly equal proportions of Latino and Anglo women from varying demographic characteristics in Southern California. Using US Census tract data from the Federal Financial Institutions Examination Council, projections regarding ethnicity, SES, and age were anticipated for potential recruitment sites, including churches, markets, universities, free/low-cost health clinics, mobile home parks, and community settings. Once permission from key personnel at the selected sites was obtained, an English and/or Spanish recruitment flyer was posted describing the study, eligibility for participation, and the time and on-site location where interested women could go to participate.
Institutional Review Board approval for the study was granted prior to data collection. When interested women arrived at the noted settings, bilingual research assistants explained the purpose of the study and restated that women were eligible to participate if they were Latino or Anglo American, at least 20 years old, able to read English or Spanish, and had never been diagnosed with breast cancer. After participants provided written consent, they were administered an English or Spanish version of the instrument, which took approximately 30 to 45 min to complete. All participants were compensated $20 for their time. Once data were collected from a number of sites, the distributions of participants across demographics were examined and additional settings were identified to fulfill the particular demographic need. As a result, 326 self-identified Latino (n=173) or Anglo (n=153) women participated in the study.
Measures
Ethnicity
Ethnicity was self-reported by participants and included as a moderating variable in the structural equation models (SEM).
Social Structural Sources of Cultural Variation
An existing measure used in previous research with culturally diverse populations [3] was employed to assess income, education, and age. Participants indicated their age in years and annual household income based on five categories (see Table 1). Women also indicated their number of years of education, which was then coded into five categories to be consistent with the income categories.
Table 1.
Sample demographics based on ethnicity
| Variable | Latino (n=144) | Anglo (n=137) |
|---|---|---|
| M (SD) | M (SD) | |
| Education* | 11.28 (4.01) | 14.49 (2.75) |
| Age in years* | 42.49 (12.03) | 47.20 (15.97) |
| n (%) | n (%) | |
| Income* | ||
| ≤$14,999 | 49 (34.03) | 28 (20.44) |
| $15–24,999 | 30 (20.83) | 17 (12.41) |
| $25–39,999 | 19 (13.19) | 24 (17.52) |
| $40–59,999 | 25 (17.36) | 21 (15.33) |
| ≥$60,000 | 21 (14.58) | 47 (34.31) |
| Marital status | ||
| Single | 27 (18.75) | 25 (18.25) |
| Married | 81 (56.25) | 74 (54.02) |
| Divorced | 23 (15.97) | 24 (17.52) |
| Widowed | 7 (4.86) | 11 (8.03) |
| Not specified | 6 (4.17) | 3 (2.19) |
| Place of birth* | ||
| Mexico | 64 (44.44) | 0 (0.00) |
| Central America/Caribbean | 5 (3.47) | 0 (0.00) |
| South America | 3 (2.08) | 0 (0.00) |
| Canada | 0 (0.00) | 2 (1.46) |
| Europe | 0 (0.00) | 3 (2.19) |
| Not specified | 9 (6.25) | 3 (2.19) |
| USA | 63 (43.75) | 129 (94.16) |
| Spanish survey language* | 63 (43.75) | 0 (0.00) |
| Health insurance coverage* | 107 (74.31) | 117 (85.40) |
| Access to healthcare clinic | 118 (81.94) | 124 (90.51) |
| Ever diagnosed with cancer | 8 (5.56) | 16 (11.68) |
| Know anyone diagnosed with breast cancer* | 90 (62.50) | 109 (79.56) |
| Family history of breast cancer* | 23 (16.00) | 54 (39.40) |
p<0.05
Screening Fatalism
A three-item subscale of the Cultural Cancer Screening Scale (CCSS; [3]) was used to assess breast cancer screening fatalism. The CCSS was developed with Latino and Anglo women based on the bottom-up methodological approach to the study of culture, which utilizes mixed methodologies. The approach begins with specific observations relevant to an area of research (e.g., cancer screening), which are derived through interviews from the populations of interest (e.g., Latinos and Anglos), and evolves from these observations to the development of quantitative instruments [3]. An advantage of this approach is that it allows for the identification of aspects of culture directly from individuals, rather than based on stereotypical views. Moreover, because efforts are taken to preserve the participants’ interview responses when developing the scale items and because the translation process is performed by Spanish–English speaking experts using the double back-translation [32] and decentering [33] procedures, measurement equivalence is more likely to be achieved.
The CCSS has demonstrated adequate reliability (Latino α=0.84; Anglo α=0.83), measurement equivalence (Tucker phi=0.98), and predictive validity with breast and cervical cancer screening behaviors [3]. The three items from the screening fatalism subscale include, “It is not necessary to screen regularly for breast cancer because everyone will eventually die of something anyway,” “It is not necessary to screen for breast cancer regularly because it is in God’s hand anyway,” and “If nothing is physically wrong, then you do not need to screen for breast cancer.” All items were based on a seven-point Likert scale from “strongly disagree” to “strongly agree.” The reliability for this subscale was good for both ethnic groups (Latino total α=0.782; Latino Spanish α= 0.739; Latino English α=0.781; Anglo α=0.814).
Negative Screening Emotions
Findings from interviews with Latino and Anglo women revealed that fear, anxiety, and embarrassment were the most frequently identified emotions associated with clinical breast exam screening [3]. Therefore, the three screening emotions included in the questionnaire were, “When I think about having a clinical breast exam I get very scared,” “Clinical breast exams are extremely embarrassing,” and “Thinking about having a clinical breast exam makes me terribly anxious.” Items were placed on a seven-point Likert scale from “strongly disagree” to “strongly agree.” The reliability of this scale was strong (Latino total α=0.927; Latino Spanish α=0.922; Latino English α=0.932; Anglo α=0.836).
Clinical Breast Exam Compliance
According to the American Cancer Society (ACS) [34], clinical breast exams are recommended for women in their 20–30s at least every 3 years and for women 40 and older every year. To assess clinical breast exam compliance, participants were provided with an illustration of a woman having a clinical breast exam and a brief description of the exam. Participants were then asked, “Have you ever had a clinical breast exam?” followed by, “If yes, how many have you had in the last 5 years?” Using similar methods employed by Kundadjie-Gyamfi and Magai [35], a screening compliance proportion was calculated based on the total number of clinical breast exam tests reported, divided by the maximum number that a woman of her age should have if they were fully compliant with screening guidelines (minimum compliance = 0; maximum compliance =1.0).
Covariates
Based on previous research [3], insurance status, knowledge about the availability of free/low-cost healthcare, country of birth, length of residence in the USA, language of the survey, diagnosis of cancer other than breast cancer, acquaintance with anyone diagnosed with breast cancer, and family history of breast cancer were assessed.
Statistical Analyses
All hypotheses were tested using Bentler’s structural equations program (EQS 6.1; [36]) with the ML method of estimation. In order to maintain a simplified model without using up model degrees of freedom [37], all relevant covariates were partitioned from the indicators of the noted outcomes prior to SEM analyses. Due to theoretical considerations, age, education, and income were included in the test of models as social structural sources of cultural variation. Adequacy of fit was assessed using the nonsignificant χ2 goodness-of-fit statistic, a ratio of less than 2.0 for the χ2/df [38], a Comparative Fit Index (CFI) of 0.95 or greater [36], and a root mean square error of approximation (RMSEA) of less than 0.05 [39]. Modifications of the hypothesized model were performed based on results from the Lagrange multiplier (LM) test and the Wald test in addition to theoretical considerations.
To test ethnicity-based differences in the magnitude of the relations among the study variables, multi-group structural equation modeling for Latino and Anglo women was also conducted. If the constrained structural model showed a decrement in fit based on a significant Δχ2 or ΔCFI of 0.01 or greater as compared to the reference model, the LM test of equality constraints was assessed for evidence of noninvariance [40]. Equality constraints were considered noninvariant and released in a sequential manner if doing so dramatically improved the model fit (LM χ2 ≥ 5.0 per df [41]). Since it is necessary in cross-cultural research to establish that differences observed between groups are not due to measurement artifacts [42], measurement equivalence was examined prior to invariance testing. Establishing measurement equivalence allows the researcher to more confidently assert that ethnic group differences are the result of the cultural factors being tested [43].
Results
Preliminary Analyses
As a result of multi-stage stratified sampling, the sample was well balanced between Latino and Anglo participants (n=173 and n=153, respectively). Cases with missing values on a manifest (e.g., measured) variable or more than half of the items on multi-item subscales were excluded from the analyses. There were some differences between the omitted and retained sample in regards to education (t(317)=1.97, p=0.05) and Spanish/English version of the survey (χ2(1)=14.10, p<0.001). The retained sample reported higher levels of education (M= 12.86, SD=3.81) compared to the omitted participants (M= 11.56, SD=4.72). Omission was also more likely among Latinos that completed the instrument in Spanish (25.88%, n=22) than English (9.54%, n=23). After imputing values for 26 cases using the expectation–maximization algorithm, data from 281 (144 Latino; 137 Anglo) women were available for analyses.
Although multi-stage stratified sampling efforts resulted in Latino and Anglo women represented across all levels of income, education, and age, the distribution of women within these categories was not equal. For instance, the Latino sample was overall younger, of lower income and education, and more likely to be uninsured. As expected, they were more likely to have been born outside the USA and complete the Spanish version of the survey (see Table 1).
Analysis of Covariates
Only one covariate was found to be statistically significant. For Latino participants, the negative screening emotion, “When I think about having a clinical breast exam I get very scared” was associated with a shorter period of residence in the USA (r=−0.251, p=0.020). The variance explained by this covariate was partialed from the indicator prior to SEM.
Descriptive Statistics and Correlations
Table 2 includes the means and standard deviations for the study variables. Approximately 58% of the total sample (62% Anglos, 55% Latinos) was fully adherent to ACS screening guidelines. Table 2 also reports the correlations among the study variables after adjustment of the covariate noted above. Fischer’s r-to-z test of difference revealed a number of significantly different bivariate correlations based on ethnicity, confirming the necessity for conducting a test of invariance.
Table 2.
Intercorrelations, means, and standard deviations as a function of ethnicity
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Education | – | |||||||||||
| 2. Income | 0.530*** (0.443***) | – | ||||||||||
| 3. Age | 0.136 (−0.316***) | 0.235** (0.031) | – | |||||||||
| 4. Screening fatalism | −0.416*** (−0.252**) | −0.369*** (−0.213*) | −0.089 (0.302***) | – | ||||||||
| 5. Nothing wrong | −0.299*** (−0.162*) | −0.265** (−0.137) | −0.064 (0.195*) | 0.718*** (0.644***) | – | |||||||
| 6. In God’s hands | −0.302*** (−0.228**) | −0.268** (−0.193*) | −0.064 (0.274**) | 0.727*** (0.906***) | 0.522*** (0.584***) | – | ||||||
| 7. Everyone will die | −0.318*** (−0.192*) | −0.283*** (−0.162) | −0.068 (0.230**) | 0.765*** (0.761***) | 0.550*** (0.490***) | 0.557*** (0.689***) | – | |||||
| 8. Screening emotions | −0.252** (−0.031) | −0.225** (−0.026) | −0.054 (0.026) | 0.170* (0.122) | 0.122 (0.079) | 0.124 (0.111) | 0.130 (0.093) | – | ||||
| 9. Embarrassment | −0.216** (−0.022) | −0.192* (−0.018) | −0.046 (0.033) | 0.145 (0.087) | 0.104 (0.056) | 0.105 (0.079) | 0.111 (0.066) | 0.851*** (0.709***) | – | |||
| 10. Anxiety | −0.248** (−0.027) | −0.220** (−0.023) | −0.053 (0.030) | 0.166* (0.109) | 0.119 (0.070) | 0.121 (0.099) | 0.127 (0.083) | 0.976*** (0.890***) | 0.830*** (0.631***) | – | ||
| 11. Scared | −0.221** (−0.025) | −0.196* (−0.021) | −0.047 (0.034) | 0.148 (0.099) | 0.106 (0.064) | 0.108 (0.090) | 0.113 (0.075) | 0.872*** (0.807***) | 0.742*** (0.572***) | 0.851*** (0.718***) | – | |
| 12. Clinical breast exam compliance | 0.169* (0.081) | 0.150 (0.070) | 0.036 (−0.097) | −0.275*** (−0.322***) | −0.197* (−0.208*) | −0.200* (−0.292***) | −0.210* (−0.245**) | −0.340*** (−0.178*) | −0.289*** (−0.126) | −0.331*** (−0.158) | −0.296*** (−0.144) | – |
| M | 11.27 (14.49) | 2.58 (3.31) | 42.49 (47.20) | 2.24 (1.54) | 2.46 (1.65) | 2.23 (1.55) | 2.04 (1.41) | 3.02 (2.44) | 2.98 (2.83) | 3.06 (2.45) | 3.03 (2.02) | 0.65 (0.76) |
| SD | 4.01 (2.75) | 1.47 (1.54) | 12.03 (15.97) | 1.70 (1.15) | 2.06 (1.38) | 2.01 (1.39) | 2.03 (1.28) | 2.14 (1.54) | 2.30 (1.94) | 2.32 (1.86) | 2.22 (1.50) | 0.37 (0.35) |
Intercorrelations, means, and standard deviations for Latino participants (n=144) are presented in upper portion of cell, and values in parentheses represent Anglo participants (n=137). Boldface indicates that groups differ significantly at p<0.05
p<0.05;
p<0.01;
p<0.001
Structural Equation Modeling
Test of the Hypothesized Model
Prior to conducting a test of the model for the Latino and Anglo samples independently, the data were screened revealing a violation of multivariate normality for both ethnic groups. Therefore, the ML robust test statistics, which corrects for non-normal data, are reported. The hypothesized model for Anglo women fit the data well (CFI=0.998, χ2 (30, n=137)=30.51, p=0.440, χ2/df=1.02, RMSEA=0.011). However, for Latinos, based on the Lagrange test and theoretical plausibility, the disturbance terms for screening fatalism and screening emotions were covaried (cov=−0.457, p=0.031), which resulted in an improvement in model fit (CFI=1.00, χ2(29, n=144)= 25.27, p=0.664, χ2/df=0.87, RMSEA=0.000). The factor structure, including the direction and significance of factor loadings, appeared similar for both groups. However, there were some differences in magnitude and significance of the associations between factors, which were further examined in multiple group analyses (Fig. 2).
Fig. 2.
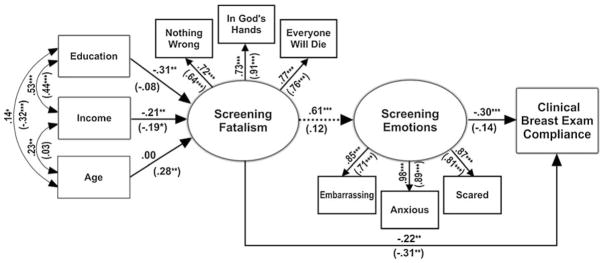
Final model with estimated path coefficients and factor loadings for Latino (Anglo) subgroups. *p<0.05; **p<0.01; ***p<0.001
Test of Configural Invariance (Model 1)
Testing for measurement equivalence began with the least restrictive model in which only the factor structure of the baseline model, namely the number of factors and the factor-loading pattern, was checked for equality across ethnic groups. The requirement for configural invariance suggests that the same items must be indictors of the same factor for Latinos and Anglos, yet differences in factor loadings are permitted across groups [44]. As shown in Table 3, the fit indices revealed an excellent fit to the data.
Table 3.
Model summary for tests of configural, measurement, and structural invariance across ethnicity
| Model | S-B χ2 | df | CFI | RMSEA (90% CI) | ΔS-B χ2a | p | Δdf | ΔCFI |
|---|---|---|---|---|---|---|---|---|
| Model 1 configural | 56.28 | 59 | 1.00 | 0.000 (0.000, 0.034) | – | – | – | – |
| No constraints | ||||||||
| Model 2 measurement model (factor loadings constrained across ethnicity) | 59.91 | 63 | 1.00 | 0.000 (0.000, 0.033) | 3.68 | 0.451 | 4 | 0.00 |
| Model 3 structural model (constrained factor loadings and 6 structural paths) | 72.69 | 69 | 0.965 | 0.014 (0.000, 0.038) | 15.65 | 0.110 | 10 | −0.035 |
| Model 4 structural model (constrained factor loadings and 5 structural paths, released Fatalism→Screening emotions) | 67.56 | 68 | 1.00 | 0.000 (0.000, 0.035) | 10.97 | 0.278 | 9 | 0.00 |
S-B χ2 Satorra–Bentler scaled statistic, CFI robust CFI, RMSEA robust RMSEA, 90% CI 90% confidence interval
Corrected value
Test of Measurement Invariance (Table 3, Model 2)
In the second level of measurement equivalence, the factor loadings of the baseline model were constrained to be equal across ethnic groups, making these coefficients invariant between Latinos and Anglos. The fit of the constrained measurement model was also good, indicating that constraining factor loadings did not result in a significant decrement in model fit. Furthermore, a review of the LM test of equality constraints statistics showed no significant between-group differences in the paths of the measurement model. Because the measurement model operated similarly for both Latinos and Anglos, any group variations observed in the multi-group structural model could be interpreted as cross-cultural differences rather than the result of measurement artifacts (see [43]).
Test of Structural Invariance (Table 3, Model 3)
To test for differences in the magnitude of the paths among the study variables across ethnicity, constraints were imposed on all structural paths. Specifically, invariance tests for path coefficients were used to test whether the effect of one variable on another variable differed as a function of ethnicity. In comparison with the configural model (model 1, Table 3), the constrained structural model showed a decrement in fit based on the change in CFI greater than 0.01 (ΔCFI=−0.035). The chi-square difference test (ΔS-B χ2(10)=15.65, p=0.110) also revealed a similar trend. A review of the LM test of equality constraints statistics confirmed significant between-group differences in the path from screening fatalism to screening emotions (LM χ2(1)=6.13, p=0.013).
Test of Partial Structural Invariance (Table 3, Model 4)
After releasing the path constraint from screening fatalism to screening emotions (Latino: β=0.61, p=0.004; Anglo: β= 0.12, p=0.311), the fit of the model improved. The fit shown in the final test of invariance was comparable to the configural model, indicating that no additional paths should be released.
Test of Research Hypotheses
The proposed structure of relations among SES, age, screening fatalism, screening emotions, and clinical breast exam compliance explained the data well for both Latino and Anglo women. As expected, ethnicity was found to significantly impact the magnitudes of some structural paths resulting in different combinations of significant direct and indirect effects for the Latino and Anglo models.
The first hypothesis concerning the direct effects of screening emotions and screening fatalism on clinical breast exam compliance was confirmed for Latino women and partially confirmed for Anglo women. For both ethnic groups, screening fatalism exerted a direct and negative impact on clinical breast exam compliance (Latinos: β=−0.22, p= 0.019; Anglos: β=−0.31, p=0.006). While the negative effect of screening emotions on clinical breast exam compliance was significant for Latino women (β=−0.30, p<0.001), it was not for Anglo women.
The second hypothesis concerning the indirect effect of screening fatalism on clinical breast exam compliance through screening emotions was also partially confirmed. For Latino women, screening fatalism significantly influenced compliance indirectly through screening emotions (βindirect =−0.184, p =0.015). Specifically, higher levels of screening fatalism positively impacted screening emotions (β=0.61, p=0.004), and as already indicated in the first hypothesis, screening emotions in turn negatively influenced clinical breast exam compliance (β=−0.30, p< 0.001). For Anglo women, however, this indirect effect was not significant.
The third hypothesis, which predicted that the influence of screening emotions and screening fatalism on clinical breast exam compliance would be moderated by ethnicity, was also confirmed. The test of invariance revealed that the influence of screening fatalism on screening emotions was stronger for the Latino sample (β=0.61, p=0.004; Anglos: β=0.12, p=0.311). Regarding the influence of screening emotions on clinical breast exam compliance, though the effect was only significant for the Latino sample (Latinos: β=−0.30, p<0.001; Anglos: β=−0.14, p=0.151), the test of invariance did not reveal a significant difference in the effect between Latinos and Anglos. To further examine the moderating role of ethnicity on the indirect effect of screening fatalism on clinical breast exam compliance through screening emotions, MacKinnon’s [45] procedures for contrasting indirect effects were employed. The indirect effects were shown to be statistically different between Latinos and Anglos (t=2.00, p=0.046), indicating that ethnicity significantly moderated the indirect effect of screening fatalism on clinical breast exam compliance through screening emotions.
In addition to the noted hypotheses, age, education, and income were found to be social structural sources of variation in the cultural factor screening fatalism. However, the relative influence of these social structural categories varied for Latino and Anglo women. For instance, among Latino women, lower education and income was associated with higher levels of screening fatalism (β=−0.31, p= 0.003; β=−0.21, p=0.008, respectively), but age was not. On the other hand, among Anglos, greater age and lower income was associated with higher levels of screening fatalism (β=0.28, p=0.010; β=−0.19, p=0.028, respectively), but education was not found to be a strong social structural source of cultural variation in screening fatalism. Interestingly, the LaGrange test statistic, which provides recommendations for adding parameters not hypothesized in the causal model, did not recommend that any direct paths be added from these social structural factors in relation to clinical breast exam compliance.
Discussion
Overall, this research reveals that psychological processes, such as screening emotions, and cultural beliefs, such as those related to fatalism, are factors relevant to disparities in health behaviors such as clinical breast exam compliance. Findings concerning the interrelations among social structural, cultural, and psychological phenomena demonstrate the importance of models that can guide the investigation of complex relations among multiple determinants of health behavior. Specifically, consistent with the conceptual model guiding the research, screening emotions and screening fatalism were found to influence compliance for both ethnic groups. These findings not only point to the interrelations among cultural beliefs, emotions, and breast cancer screening, as proposed by the model, but also point to the moderating role of ethnicity on these relations, which has conceptual as well as practical implications.
The fact that the structure of relations specified by the model is supported by the results strengthens its value as a foundation for both research and theory. Still, findings concerning the moderating role of ethnicity represent both a contribution to a better understanding of the relations among social structural, cultural, and psychological antecedents of behavior as well as a challenge to the linear representation of the relations specified in Fig. 1. In general terms, this finding is not inconsistent with the conceptual foundations of the model [21, 22, 46], in that ethnicity is thought to represent more than socially shared beliefs. Specifically, it is conceivable that aspects associated with ethnicity, other than those relevant to the measured cultural factor, can make a difference in how individuals of different ethnic backgrounds behave in a particular situation, which could explain in part a moderating effect like the one observed. In sum, while it sheds light on the nature of the culture-behavior link within the context of a multiethnic society, the observed moderating effect is expected to stimulate further conceptual work and research.
From a methodological perspective, these results confirm the importance of employing statistical techniques that take into account the role of ethnicity such as multi-group structural equation modeling. For instance, in the present study, Latino women reported significantly higher levels of anxiety and fear about clinical breast exam screening as compared to Anglo women, which in turn impacted clinical breast exam compliance to a greater degree for the Latino as compared to the Anglo sample. If these data were not analyzed separately for Latino and Anglo women, but rather controlled for ethnicity, the complexity of these relations might not have been recognized. These results are consistent with Consedine and associates’ [47] suggestion that the lower screening behaviors of African American women may be more influenced by fear, due to finding that this population is more afraid of cancer [48]. In fact, similar results have been reported for Latino and Anglo women regarding the influence of emotions on health behavior as a result of perceptions of healthcare mistreatment [16].
Concerning the proposed influence of socially shared fatalistic beliefs on screening emotions and clinical breast exam compliance, the role of ethnicity is interesting, particularly when considering the indirect influence of those cultural beliefs. Consistent with the model for the study of culture, screening fatalism was strongly and directly related to clinical breast exam compliance for both Latino and Anglo women. For Latinas, screening fatalism also exerted a significant indirect effect through screening emotions. These findings suggest that for Latino women, both screening fatalism as well as screening emotions are important determinants of cancer screening. However, for Anglo women, screening fatalism mainly exerted a direct effect on clinical breast exam compliance as the indirect effect through emotions was not significant. Future research should perhaps examine the role of screening fatalism in relation to cognitive processes, such as perception of control and causal attributions. It is possible that among Anglo women, these cognitive variables may be more directly influenced by culture than are emotions.
In addition to supporting the hypothesized structure of relations among cultural and psychological variables associated with clinical breast exam compliance, results also shed light on the role of SES and age as social structural sources of variation in cultural beliefs. While a significant amount of research in the health disparities literature has examined factors such as ethnicity, SES, age, and access to care, most research in this area typically controls for such social structural variables or test their direct effects on health behavior. Consistent with the model, these social structural factors are postulated to be sources of cultural variation and are believed to influence health behavior indirectly through psychological processes. Although in some cases income and access to care may be directly related to health behavior due to the instrumental importance of resources, this direct relation may not have been observed because California provides free breast and cervical cancer screening exams to underserved women. In fact, the present research revealed that age, education, and income did influence clinical breast exam compliance but only through their effects on screening fatalism. Similar results have been reported by Murguia and Zea [49] revealing that Latino cultural health beliefs were better predictors of healthcare utilization as compared to SES and acculturation.
Despite the significance of the study findings, some limitations of the research should be considered. For instance, the Latino sample of this study reflected the demographic reality of Southern California, which is predominantly of a Mexican cultural background. Therefore, it is unclear whether the results would be the same with Latinos from regions of the country that represent other national origins. The sample also included both immigrant and US born Latinos, which was expected to contribute to more variance in the cultural factor. Future research could include samples of Latinos that would make it possible to examine generation status and other potential sources of cultural variation, which may provide more targeted information. In addition, while the theoretical model on which the hypothesized relations were based provided a meaningful conceptual foundation for SEM models, the cross-sectional design of this study limits the test of temporal relations. Future work could employ longitudinal data in order to examine such relations in a more definitive manner.
The findings of the research have important implications for interventions with culturally diverse patients. First, results concerning the indirect effects of culture on clinical breast exam compliance for the two ethnic groups suggest that efforts designed to improve clinical breast exam compliance among culturally diverse populations may have to emphasize different variables highlighted in the model. For instance, on the one hand, in order to be effective with Anglo patients, health professionals may have to recognize cultural beliefs. On the other hand, when working with Latino patients, health professionals may be better off paying attention to not only their cultural beliefs but also emotions such as those related to the screening process. In fact, research with women in Korea has indicated that interventions that focus on both cognitions and emotions, such as shame, embarrassment, and worry related to Pap smear screening, are particularly successful [50]. All things considered, intervention efforts that address both screening fatalism as well as emotions may prove effective at enhancing screening and reducing the noted health disparities between Latino and Anglo women.
Acknowledgments
This research was supported by a NIH grant 1R21CA101867-01A2 to H. Betancourt, PI, through the National Cancer Institute and the Office of Research on Women’s Health and by grant PFT-08-014-01-CPPB to P. Flynn, PI, through the American Cancer Society.
Footnotes
The term Latino refers to the individuals or populations of the USA who came originally from Latin America or a region of the USA that was once part of Latin America.
Anglo American refers to non-Latino White individuals or populations of the USA who came originally from the UK or other European backgrounds, who share the English language and Anglo American cultural heritage [2].
Conflict of Interest The authors have no conflict of interest to disclose.
Contributor Information
Patricia M. Flynn, Email: pflynn@llu.edu, Department of Psychology, Loma Linda University, Loma Linda, CA 92354, USA
Hector Betancourt, Department of Psychology, Loma Linda University, Loma Linda, CA 92354, USA. Universidad de La Frontera, Temuco, Chile
Sarah R. Ormseth, Department of Psychology, Loma Linda University, Loma Linda, CA 92354, USA
References
- 1.National Cancer Institute. [Accessibility verified December 16, 2009];NCI statement on breast cancer screening. Available at http://www.cancer.gov/newscenter/pressreleases/BreastScreen2009.
- 2.Betancourt H, Fuentes JL. Culture and Latino issues in health psychology. In: Kazarian S, Evans D, editors. Handbook of Cultural Health Psychology. San Diego: Academic; 2001. pp. 205–221. [Google Scholar]
- 3.Betancourt H, Flynn PM, Riggs M, Garberoglio C. A cultural research approach to instrument development: The case of breast and cervical cancer screening among Latino and Anglo women. Health Educ Res. 2010;25:991–1007. doi: 10.1093/her/cyq052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ries LA, Melbert D, Krapcho M, et al. SEER cancer statistics review, 1975–2005. Bethesda: National Cancer Institute; 2008. [Google Scholar]
- 5.Li IC, Malone EK, Dailing RJ. Differences in breast cancer stage, treatment, and survival by race and ethnicity. Arch Intern Med. 2003;163:49–56. doi: 10.1001/archinte.163.1.49. [DOI] [PubMed] [Google Scholar]
- 6.Biffl WL, Myers A, Franciose RJ, Gonzalez RJ, Darnell D. Is breast cancer in young Latinas a different disease? Am J Surg. 2001;182:596–600. doi: 10.1016/s0002-9610(01)00789-9. [DOI] [PubMed] [Google Scholar]
- 7.Howe HL, Wu X, Ries LAG, et al. Annual report to the nation on the status of cancer, 1975–2003, featuring cancer among U.S. Hispanic/Latino populations. Cancer. 2006;107:1711–1742. doi: 10.1002/cncr.22193. [DOI] [PubMed] [Google Scholar]
- 8.Gallo LC, Smith TW, Cox CM. Socioeconomic status, psychosocial processes, and perceived health: An interpersonal perspective. Ann Behav Med. 2006;31:109–119. doi: 10.1207/s15324796abm3102_2. [DOI] [PubMed] [Google Scholar]
- 9.Diefenbach MA, Miller SM, Daly MB. Specific worry about breast cancer predicts mammography use in women at risk for breast and ovarian cancer. Health Psychol. 1999;18:532–536. doi: 10.1037//0278-6133.18.5.532. [DOI] [PubMed] [Google Scholar]
- 10.Lindberg NM, Wellisch D. Anxiety and compliance among women at risk for breast cancer. Ann Behav Med. 2001;23:298–303. doi: 10.1207/S15324796ABM2304_9. [DOI] [PubMed] [Google Scholar]
- 11.Strzelczky J, Dignan M. Disparities in adherence to recommended follow-up on screening mammography: Interaction of sociodemographic factors. Ethnic Dis. 2002;12:77–86. [PubMed] [Google Scholar]
- 12.Borrayo EA, Gonzalez P, Swaim R, Marcus AL, Flores E, Espinoza P. The Latina Breast Cancer Screening Scale: Beliefs about breast cancer and breast cancer screening. J Health Psychol. 2009;14:944–955. doi: 10.1177/1359105309341203. [DOI] [PubMed] [Google Scholar]
- 13.Suarez L, Roche L, Nichols D, Simpson D. Knowledge, behavior, and fears concerning breast and cervical cancer among older low-income Mexican-American women. Am J Prev Med. 1997;13:137–424. [PubMed] [Google Scholar]
- 14.Lobell M, Bay RC, Rhoads KVL, Keske B. Barriers to cancer screening in Mexican-American women. Mayo Clin Proc. 1998;73:301–308. doi: 10.1016/S0025-6196(11)63694-X. [DOI] [PubMed] [Google Scholar]
- 15.Dettenborn L, DuHamel K, Butts G, Thompson H, Jandorf L. Cancer fatalism and its demographic correlates among African American and Hispanic women: Effects on adherence to cancer screening. J Psychosoc Oncol. 2004;22:47–60. [Google Scholar]
- 16.Betancourt H, Flynn PM, Ormseth SR. Healthcare mistreatment and continuity of cancer screening among Latino and Anglo American women in Southern California. Women & Health. 2011;51(1):1–24. doi: 10.1080/03630242.2011.541853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Friedman LC, Webb JA, Weinberg AD, Lane M, Cooper HP, Woodruff A. Breast cancer screening: Racial/ethnic differences in behaviors and beliefs. J Cancer Educ. 1995;10:213–216. doi: 10.1080/08858199509528376. [DOI] [PubMed] [Google Scholar]
- 18.Consedine NS, Magai C. The uncharted waters of emotion: Ethnicity, trait emotion and emotion expression in older adults. Cross-Cult Geront. 2002;17:71–100. doi: 10.1023/a:1014838920556. [DOI] [PubMed] [Google Scholar]
- 19.Matsumoto D. Ethnic differences in affect intensity, emotion judgments, display rule attitudes, and self-reported emotional expression in an American sample. Motiv Emotion. 1993;17:107–123. [Google Scholar]
- 20.Wong S, Bond MH, Mosquera PM. The influence of cultural value orientations on self-reported emotional expression across cultures. Cross-Cult Psychol. 2008;39:224–229. [Google Scholar]
- 21.Betancourt H, Flynn PM. The psychology of health: Physical health and the role of culture in behavior. In: Villarruel FA, Carlo G, Contreras Grau JM, et al., editors. Handbook of US Latino psychology. Thousand Oaks: Sage; 2009. pp. 347–61. [Google Scholar]
- 22.Betancourt H, Lopez SR. The study of culture, ethnicity, and race in American psychology. Am Psychol. 1993;48:629–37. [Google Scholar]
- 23.Jacobs EA, Karavolos K, Rathouz PJ, Ferris TG, Powell LH. Limited English proficiency and breast and cervical cancer screening in a multiethnic population. Am J Public Health. 2005;95:1410–1416. doi: 10.2105/AJPH.2004.041418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Powe BD. Cancer fatalism among elderly African American women: Predictors of the intensity of the perceptions. J Psychosoc Oncol. 2001;19:85–95. [Google Scholar]
- 25.Niederdeppe J, Levy AG. Fatalistic beliefs about cancer prevention and three prevention behaviors. Cancer Epidem Biomar. 2007;16:998–1003. doi: 10.1158/1055-9965.EPI-06-0608. [DOI] [PubMed] [Google Scholar]
- 26.Chavez L, Hubbell F, Mishra S, Valdez R. The influence of fatalism on self-reported use of Papanicolaou smears. Am J Prev Med. 1997;31:418–424. [PubMed] [Google Scholar]
- 27.Abraido-Lanza AF, Viladrich A, Florez KR, Cespedes A, Aguirre AN, De La Cruz AA. Commentary: Fatalismo reconsidered: A cautionary note for health-related research and practice with Latino populations. Ethnic Dis. 2007;17:153–158. [PMC free article] [PubMed] [Google Scholar]
- 28.Perez-Stable E, Sabogal F, Otero-Sabogal R, Hiatt R, McPhee S. Misconceptions about cancer among Latino and Anglos. J Amer Med Assoc. 1992;268:3219–3223. doi: 10.1001/jama.1992.03490220063029. [DOI] [PubMed] [Google Scholar]
- 29.Borrayo EA, Guarnaccia CA. Differences in Mexican-born and U.S. born women of Mexican descent regarding factors related to breast cancer screening behaviors. Health Care Women I. 2000;21:599–613. doi: 10.1080/07399330050151842. [DOI] [PubMed] [Google Scholar]
- 30.Tov W, Diener E. Culture and subjective well-being. In: Kitayama S, Cohen D, editors. Handbook of cultural psychology. New York: Guilford; 2007. pp. 691–713. [Google Scholar]
- 31.Mayo RM, Ureda JR, Parker VG. Importance of fatalism in understanding mammography in rural elderly women. J Women Aging. 2001;13:57–72. doi: 10.1300/J074v13n01_05. [DOI] [PubMed] [Google Scholar]
- 32.Knight GP, Roosa MW, Umana-Taylor AJ. Studying ethnic minority and economically disadvantaged populations. Washington, DC: American Psychological Association; 2009. [Google Scholar]
- 33.Prieto AJ. A method for translation of instruments to other languages. Adult Educ Quart. 1992;43:1–14. [Google Scholar]
- 34.Smith RA, Cokkinides V, Eyre HJ. American Cancer Society guidelines for the early detection of cancer, 2006. CA Cancer J Clin. 2006;56:11–25. doi: 10.3322/canjclin.56.1.11. [DOI] [PubMed] [Google Scholar]
- 35.Kudadjie-Gyamfi E, Magai C. The influence of coping styles on mammography screening in a multiethnic sample. Cult Diver and Ethn Min. 2008;14:183–192. doi: 10.1037/1099-9809.14.3.183. [DOI] [PubMed] [Google Scholar]
- 36.Bentler PM. EQS 6 structural equations program. Encino: Multivariate Software; 2005. [Google Scholar]
- 37.Kammeyer-Mueller JD, Wanberg CR. Unwrapping the organizational process: Disentangling multiple antecedents and their pathways to adjustment. J Appl Psychol. 2003;88:779–794. doi: 10.1037/0021-9010.88.5.779. [DOI] [PubMed] [Google Scholar]
- 38.Tabachnick BG, Fidell LS. Using multivariate statistics. New York: Harper Collins; 2001. [Google Scholar]
- 39.Browne M, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Thousand Oaks: Sage; 1993. [Google Scholar]
- 40.Cheung GW, Rensvold RB. Evaluating goodness-of-fit indexes for testing measurement invariance. Struct Equ Modeling. 2002;9:233–255. [Google Scholar]
- 41.Scott-Lennox JA, Lennox RD. Sex-race differences in social support and depression among older low-income adults. In: Hoyle RH, editor. Structural equation modeling: Concepts, issues, and applications. Thousand Oaks: Sage; 1995. pp. 199–216. [Google Scholar]
- 42.van de Vijver FJR, Leung K. Methods and data analysis for cross-cultural research. Thousand Oaks: Sage; 1997. [Google Scholar]
- 43.Chen FF. What happens if we compare chopsticks with forks? The impact of inappropriate comparisons in cross-cultural research. J Pers Soc Psycho. 2008;95:1005–1018. doi: 10.1037/a0013193. [DOI] [PubMed] [Google Scholar]
- 44.Byrne BM. Structural equation modeling with EQS. Mahwah: Lawrence Erlbaum Associates; 2006. [Google Scholar]
- 45.Mackinnon DP. Introduction to statistical mediation analysis. New York: Taylor and Francis; 2008. [Google Scholar]
- 46.Betancourt H, Hardin C, Manzi J. Beliefs, value orientation, and culture in attribution processes and healing behavior. J Cross Cultur Psychol. 1992;23:179–195. [Google Scholar]
- 47.Consedine NS, Magai C, Neugut AI. The contribution of emotional characteristics to breast cancer screening among women from six ethnic groups. Prev Med. 2004;38:64–77. doi: 10.1016/j.ypmed.2003.09.030. [DOI] [PubMed] [Google Scholar]
- 48.Miller LY, Hailey BJ. Cancer anxiety and breast cancer screening in African-American women: A preliminary study. Womens Health Iss. 1994;4:170–174. doi: 10.1016/s1049-3867(05)80058-1. [DOI] [PubMed] [Google Scholar]
- 49.Murguia A, Zea MC. The development of the Cultural Health Attributions Questionnaire (CHAQ) Cult Diver and Ethn Min. 2000;6:268–283. doi: 10.1037/1099-9809.6.3.268. [DOI] [PubMed] [Google Scholar]
- 50.Park S, Chang S, Chung C. Effects of a cognition-emotion focused program to increase public participation in Papanicolaou smear screening. Public Health Nurs. 2005;22:289–298. doi: 10.1111/j.0737-1209.2005.220404.x. [DOI] [PubMed] [Google Scholar]