INTRODUCTION
Because men who have sex with men (MSM) are disproportionately affected by HIV, understanding how risky sexual behaviors change as MSM age is an important aspect of the epidemiology in this population. HIV prevention efforts have traditionally focused on young MSM [1]. Due in part of ageism and homophobia, older MSM remain a marginal population in which HIV levels and sexual risk factors are less well known [2]. Contrary to the general belief that older MSM are not sexually active and are therefore not at risk for HIV, converging lines of research and data show otherwise. The Centers for Disease Control and Prevention estimates that 10 percent of all newly acquired infections are in adults over the age of 50, suggesting that older MSM are engaging in risk behaviors associated with HIV [3].
In a probability sample of older MSM living in four metropolitan cities, Dolcini and colleagues [4]reported an HIV prevalence of 19% among respondents over the age of 50. This HIV prevalence was even higher among African Americans, injection drug users, illicit drug users, and those who were more open about their sexual orientation. Other qualitative studies identified additional factors driving risky sexual behaviors among older MSM such as drinking in conjunction with sex, stigma related to sexual orientation and HIV, the perceived low risk for contracting the HIV virus, the perceived loss of attractiveness accompanied with aging, marginalization within the gay community, loneliness, and a desire to have sexual intimacy [5, 6].
Several historical issues must be considered when studying sexual behaviors in older MSM. With the advent of more effective treatments for HIV, a significant proportion of MSM are now living and aging with HIV. Some HIV-positive MSM continue to engage in high-risk sexual behavior after their diagnosis, placing themselves at risk for contracting secondary infections as well as transmitting HIV to others [7, 8]. Reduced concern due to highly active antiretroviral therapy and safer sex fatigue were also found to be associated with sexual risk-taking among HIV-positive MSM [9–11]. In addition, the development of phosphodiesterase type 5 (PDE-5) inhibitors, exemplified by Viagra, has enabled many older men to restore or enhance their sexual function. Recent work has demonstrated an association between the use of Viagra, by itself, or with other stimulant drugs, and increased rates of high-risk sexual behavior and HIV transmission in MSM [12]. This risk factor may be of special importance in the older MSM population.
It has become clear that older MSM are at risk for HIV acquisition and transmission, and the changes in patterns of risk behaviors in this population require further investigation. One of the most important risk behaviors for HIV acquisition and transmission among MSM involve multiple sexual partners [13–15]. Dolcini and colleagues [4]found that among older MSM, the median number of sexual partners per year decreases by one with every ten years of age. To our knowledge, only two published North American epidemiologic studies specifically investigated HIV risk behaviors among older MSM [4, 16]. The studies were, however, cross-sectional and could not elucidate the change of risk behavior such as number of sexual partners over time. Understanding sexual risk behaviors over time among older MSM is important because it will help identify who is at the highest risk, whether or not there are unique subgroups of MSM who are at higher risk than the others, and the factors associated with risk behaviors among aging MSM.
This exploratory study aims to identify subsets of trajectories with respect to the number of sexual partners among older HIV-negative and -positive MSM. We hypothesized that this group is not homogeneous and might be better characterized by subpopulations with specific attributes. This study tested this hypothesis relative to the number of sex partners over time. The secondary aim of the study is to investigate factors that may be associated with different trajectories.
METHODS
Study Population
We analyzed longitudinal data (n = 237) from the Pitt Men’s Study, an on-going cohort study of the natural history of HIV infection and progression among gay and bisexual men in Pittsburgh, PA. The Pitt Men’s Study is one of the four sites of the Multicenter AIDS Cohort Study (MACS). Enrollment of research subjects into the cohort has occurred three times: 1984–1985, 1987–1991, and 2001–2003. The inclusion criteria, recruitment and sampling strategies are described in greater details elsewhere [17, 18]. The participants in the Pitt Men’s Study comprise a convenience sample of men in Pittsburgh who reported having sexual activity with another man in the past seven years. Since 1984, participants in the study have been followed every six months with a detailed questionnaire-based interview, physical examination, and medical history review. The goal of the Pitt Men’s Study is to identify the barriers to risk reduction, and to create a program to reduce HIV risks for MSM in Pittsburgh. The sample size of the PMS was greatly expanded after the most recent enrollment, from 2001–2003. The sample of older men from the participants enrolled at earlier times was too small to permit meaningful statistical analyses. We selected data from visit 40 (Oct 1, 2003) to visit 50 (March 31, 2009) where sample size is greatest and data most complete. The period from Oct 1, 2003 to March 31, 2009 will be referred to as the study period in this paper. Since participants in the PMS were a convenience sample of MSM living in Pittsburgh and a majority of them had been followed for more than 20 years, this study may not be generalizable to the entire population of older MSM currently living in Pittsburgh.
Participants were included in the analyses if they met all of the following criteria: (1) aged 50 and above by March 31, 2009; (2) between 50 and 59.5 years of age during the study period; (3) had at least one male sexual partner during the study period, and (4) had at least three visits during the study period (see Table 1). Of 693 subjects who came to the Pitt Men’s Study during the study period, 354 (51.1%) were 50 years or older on March 31, 2009. Since there were not sufficient cases for participants over the age 60, we limited the data to men who were between 50 to 59.5 years of age. This cut-off resulted in at least 30 cases at each age point. This restriction resulted in a analytic sample of 287 men. Analysis was further limited to men who had at least one male sex partner in the past 6 months if they reported that they were sexually active during the same period. Seventeen men did not have male sex partners when they were sexually active and were removed from the analysis. Finally, participants were required to have visited the study clinic at least three times during the study period, contributing three data points from which to estimate individual trajectories. The final sample included 237 men, accounting for 1,777 person-visits. The median number of observations per participant was 8 (range 3–11). Since the aim was to examine the age effect on the number of sexual partners, longitudinal data were restructured as a function of age rather than visit [19].
Table 1.
Socio-demographic, behavioral, and psychosocial characteristics of trajectory groups after the groups are identified from Nagin’s group-based modeling
| Low (N=46) | Medium (N=164) | High (N=27) | P | |
|---|---|---|---|---|
| White race % (n) | 80.4 (37) | 92.1 (151) | 100 (27) | 0.013a |
| HIV positive % (n) | 60.9 (28) | 38.4 (63) | 40.7 (11) | 0.024 |
| Cohort enrollment 2001–2003 (late)% (n) | 21.7 (10) | 14.0 (23) | 11.1 (3) | 0.367a |
| Education in years mean (sd) | 15.1 (2.8) | 15.3 (2.4) | 15.7 (2.5) | 0.641 |
| Any annual income <$20K % (n) | 47.8 (22) | 32.3 (53) | 25.9 (7) | 0.089 |
| Any current smoke % (n) | 30.4 (14) | 36.0 (59) | 22.2 (6) | 0.335 |
| Average no. of drinks per week mean (sd) | 2.9 (6.3) | 5.3 (10.1) | 4.4 (5.2) | 0.298 |
| Any binge drinking % (n) | 8.7 (4) | 17.1 (28) | 18.5 (5) | 0.344a |
| Any marijuana % (n) | 32.6 (15) | 38.4 (63) | 63.0 (17) | 0.028 |
| Any poppers % (n) | 6.5 (3) | 43.9 (72) | 55.6 (15) | <0.001 |
| Any crack cocaine % (n) | 0 (0) | 8.5 (14) | 14.8 (4) | 0.023a |
| Any other cocaine % (n) | 6.5 (3) | 11.0 (18) | 22.2 (6) | 0.132a |
| Any methamphetamine % (n) | 2.2 (1) | 3.7 (6) | 11.1 (3) | 0.154a |
| Any ecstasy % (n) | 0 (0) | 6.7 (11) | 3.7 (1) | 0.191a |
| Any Viagra % (n) | 6.5 (3) | 30.5 (5) | 66.7 (18) | <0.001 |
| Any CES-D ≥ 16 % (n) | 50.0 (23) | 48.2 (79) | 44.4 (12) | 0.900 |
| Any CES-D ≥ 22 % (n) | 34.8 (16) | 30.5 (50) | 33.3 (9) | 0.841 |
| Average NUAII mean (sd) | 0.0 (0.0) | 0.4 (0.6) | 2.1 (2.8) | <0.001 |
| Average NUARI Mean (sd) | 0.0 (0.0) | 0.3 (0.7) | 1.6 (2.5) | <0.001 |
NUAII= number of unprotected anal insertive intercourse in the past 6 months, NUARI=number of unprotected receptive intercourse partner in the past 6 months,
Fisher’s exact test
Measures
The number of sexual partners
In every biannual visit, participants were asked comprehensive questions regarding their sexual behaviors in the past six months. The participants were asked if they had “any sort of sexual activity with a man”, followed by a question about the number of oral and anal sex partners as well as sexual activities with partners that did not involve sexual intercourse. For the analysis, the number of male partners with whom participants had oral or anal intercourse in the past 6 months was used as the dependent variable. For brevity, the variable will be referred to as the number of sexual partners throughout the rest of the paper.
Sociodemographic characteristics
Participant age was calculated by using the date of each visit minus the date of birth for each participant. Since participants were interviewed at six-month intervals, age was then rounded off to the nearest half-year (e.g., 50.0; 50.5; 51.0, etc.). Self-reported race was categorized as Caucasian, African American, or other races. Years of education were recorded when the participants were enrolled to the study. The self-reported annual gross income in the past year was dichotomized as less than $20,000 or not. A summary variable was created to indicate if a participant has earned less than $20,000 at any age in the study period. This summary variable was an approximation of whether a participant experienced financial stress during the study period.
Individual risk behavior
Participants were asked if they were currently using the following drugs in the previous six months: 1) marijuana, 2) poppers or nitrite inhalants, 3) crack cocaine, 4) other forms of cocaine, 5) methamphetamines (“speed”, “meth“, or ice”), and 6) other recreational drugs such as “ecstasy” or MDA/MDMA (3,4-methylenedioxy-N-methylamphetamine), gammahydroxybutyrate (GHB), “speedball,” ethyl chloride, hallucinogens, “downers,” or heroin/opiates. Additionally, participants were asked if they had taken “Viagra, Cialis, Levitra or other drugs that were prescribed by a medical provider to treat erectile dysfunction”. Participants were considered currently smoking if they reported ‘yes’ to the question: “smoke cigarettes now? (as of one month ago)”. Binge drinking was defined as five or more drinks per occasion occurring at least monthly.
CES-D score
Depressive symptoms were assessed by the 20-item CES-D, which was directly adapted from the instrument developed by Raldoff [20]. The participants recorded the frequency of each psychological symptom in the previous week by assigning a value as follows: 0 = “rarely or none of the time (<1 day per week),” 1 = “some of little of the time (1–2 day per week),” 2 = “occasionally or moderate amount of the time (3–4 days per week),” or 3 = “most or all of the time per week (5–7 days per week).” A threshold of 16 or more has been shown to be indicative of significant depressive symptoms and predictive of HIV morbidity and mortality among participants in the Multicenter AIDS Cohort Study [21]. A threshold of 22 has been used to approximate “major depression” in a previous study of depression among urban gay and bisexual men [22].
Men’s Personal Sexual Attitudes
Participants completed a 20-item survey including personal attitudes towards HAART and risk behaviors, sensation seeking, and safer sex fatigue. Respondents were asked to express disagreement or agreement with each statement on a 5-point Likert scale (from 1 ‘strongly disagree’ to 5 ‘strongly agree’). The five subscales are (1) reduced HIV concern(e.g., ‘Because of combination drug treatments for HIV, I am less concerned about becoming HIV positive or infecting someone’); (2) perception of HIV as a threat(e.g., ‘HIV is not longer the threat is used to be’); (3) safer sex fatigue(e.g., ‘I feel tired of always having to monitor my sexual behavior’); (4) viral load/transmission beliefs(e.g., ‘It would be more difficult for an HIV-positive person to infect a partner through unsafe sex if the HIV-positive person was taking combination drug treatments’); and (5) sexual sensation seeking (e.g., ‘I like wild “uninhibited” sexual encounters’). The Cronbach’s Alpha of the scales at visit 47, the latest visit where the instrument was administered, was 0.658.
Venues of seeking new partners
At visit 50, we examined the venues through which participants met new sexual partners in the past 6 months. These venues or means of meeting new partners include internet, party, advertisement in a newspaper, bar, bathhouse, park or outdoor public place, and others.
Statistical Analyses
First, we examined the distribution of the variable, ‘the number of sexual partners in the past 6 months’. Data for this variable range from 0 to 222, with sexual partners greater than 30 constituting the top 5th percentile of the data (range 31–222). When data of the top 5% percentile (31–222) were included in the model, unreliable, idiosyncratic trajectories were generated. Instead of discarding this 5% of data as potential outliers, we decided to keep the data but fixed the value to 30 sexual partners for all data outside the range 0–30. In a subanalysis, we found that the result did not change when the data for sexual partners greater than 30 were deleted from the analysis. Truncation of the number of sexual partners only applied for the trajectory analysis. Raw data were used to calculate the average numbers of sexual partners after the trajectory groups were identified.
A semi-parametric, group-based approach was used to identify various clusters of individual growth trajectories [23]. This group-based approach to analyzing longitudinal data has several advantages over traditional statistical methods. Instead of assuming a continuous distribution of trajectories within the population, group-based approach assumes that the population is composed of a mixture of distinct groups defined by the developmental pathways. In other words, group-based modeling can be used to identify trajectories of qualitatively different groups while standard growth modeling quantifies a change process in which common trajectory exists in the population. Previous research suggests that different classes (or groups) of sex partner trajectories may indeed exist among older MSM. This statistical approach provides a means to identify whether or not there are subgroups of trajectories, and if so, which subgroups are most at risk for having multiple sex partners. Trajectories were modeled as a function of age rather than visit. Trajectories were modeled using the SAS PROC TRAJ software available online at http://www.andrew.cmu.edu/user/bjones/index. Detailed information about the formulation and selection of group-based models have been described (Nagin 1999, 2005). Individuals with missing observations were included because PROC TRAJ uses all values available from each case to estimate an individual’s trajectory. A censored normal model was used to accommodate the possibility of clustering within the scale of 0 to 30. The optimal number of trajectory groups was selected based on Nagin’s criteria: (1) substantive theory (2) Bayesian Information Criteria (3) Average Posterior Probabilities (AvePP) and (4) group size. After the optimum number of trajectories was selected, the trend of each trajectory (linear, quadratic, cubic function of age) was determined. Further, chi-square tests and analysis of variance (ANOVA) were used to test group differences in demographic, behavioral, and psychosocial characteristics. To summarize results of the continuous variables, mean scores of the measures of interest (e.g. years of education and number of drinks per week) across the ages were calculated. For dichotomous behavioral and psychological measures (e.g. current smoker, recreational drug use, binge drinking), a new variable was created to denote if the participant had reported such characteristics at any age during the study period.
RESULTS
Baseline Demographic and Behavioral Characteristics
Participants in the final sample (n=237) were primarily Caucasian (n=215; 90.7%), with a smaller proportion of African Americans (n=19, 8.0%), and other races (n=3, 1.3 %). In the later analysis, we combined African Americans and other races to “non-white” due to the small number of the racial minority category. Overall, participants were well-educated, with mean of 15.3 years of education (standard deviation=2.50, range 8–21 years). About 15% (n=36) of participants were recruited after 2001. At the end of the study period, a total of 135 participants (57.0%) were HIV-negative and 102 (43.0%) were HIV-positive. None of the men in the sample became infected with HIV during six year’s follow up. Among the men living with HIV (n=102), all of them were first diagnosed with HIV before 2003, 47 (46.1%)were first diagnosed with HIV before 1989.
Trajectory analyses
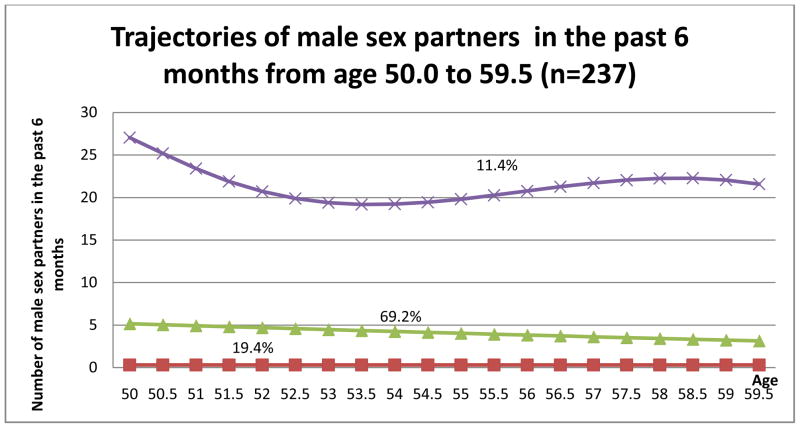
The three-group model was found to be the best model (Figure 1). Average posterior group membership probabilities (AvePP) for the three-group model ranged 0.930–0.999. These scores mean that 93–99% of individuals were correctly assigned to their groups. The first group, the “low group” (n = 46; 19.4% of the sample, AvePP = 0.930) had low or zero sex partners (mean = 0.2, median = 0, range 0–5) across middle age through early old age. The second group, the “medium group” (n = 164; 69.2% of the sample, AvePP = 0.984), consisted of participants who consistently had about two male sex partners (mean = 3.5, median = 2, range 0–56) over the age range of the study. Finally, the third group, “high group” (n = 27; 11.4% of the sample, AvePP = 0.999) had about 30 or more sexual partners at 50 years of age that appeared to decrease to about 20 sexual partners by 53 years of age and persisted till age 60 (mean = 28.8, median = 20, range 0–222).
Figure 1.
Trajectories with respect to number of male sexual partners in the past 6 months from age 50 to 59.9. Group 1, low group (n=46, 19.4%); group 2, medium group (n=164, 69.2%), group 3, high group (n=27, 11.4%); total n=237. As mentioned earlier, we based our model selection on several criteria: substantive theory, Bayesian Information Criteria, group size, and average posterior probabilities. As the number of group increased from three to four, the Bayesian Information Criteria became less negative (BIC for 3-group and 4-group model were −4522.25 and −4360.94, respectively). However, the four-group model yielded a prohibitively small trajectory group (5%, n=12). The theory of risky sexual behaviors among older MSM is not well-defined and we therefore based our model selection on parsimony and interpretability of the model. Hence, the three-group model was considered the best model. Therefore, the three-group model was considered the best model.
Statistical parameters of the trajectory groups with respect to multiple sex partners
Table 1 displays the sociodemographic, behavioral, and psychosocial characteristics of participants reported by each of the three trajectory groups. Because the proportion of other races was too small (about 1% of analytic sample) we combined African American and other races as “non-white”. The trajectory groups are statistically different in race (p = 0.013). All men in the high group were white, as compared to only 92.2% in the medium group, and 81.1% in the low group. The proportion of men reported earning less than $20,000 annually was highest in the low group, followed by the medium and high group but the difference in proportion did not achieve statistical significance (p = 0.089). There were no differences in the mean years of education among the men in the three trajectory groups. There were also no differences in the proportion of men from the late enrollment (2001–2003) among three trajectory groups (p = 0.367). However, the trajectory groups were significantly different in their HIV status. There was a greater proportion of HIV-positive men in the low group (60.9%) compared to the medium group (38.4 %) and the high group (40.7%) (p = 0.024). In a subanalysis, group-based modeling was run separately for HIV-positive men and HIV-negative men. The trajectories with respect to sexual partners in HIV-positive men and HIV-negative appeared to be similar to the trajectories of men combined. The high trajectory group of the HIV-positive men was unstable due to small sample size (n=10), we decided to not to separate the trajectory analysis by HIV status.
Concerning risk behaviors, the trajectory groups were statistically significantly different in use of marijuana, poppers, crack cocaine, the number of unprotected anal insertive partners and the number of unprotected receptive partners. Participants in the high group were more likely to have reported using marijuana, poppers, crack cocaine, and Viagra at any age during the study period as compared to other trajectory groups. The proportions of men using marijuana in the previous visit at any age were 63.0%, 38.4%, and 32.6% among the high group, medium group, and low group respectively (p = 0.028). As high as 55.6% of the participants in the high group reported using poppers at any age, while significantly fewer participants in other trajectory groups reported using poppers at any age (43.9% for medium group, and 6.5% for low group, p < 0.001). Similarly, the proportions of men using crack cocaine were 14.8%, 8.5% and 0% among the high group, medium group, and low group respectively (p = 0.023). The proportions of men using Viagra were 66.7%, 30.5%, and 6.5% among the high group, medium group, and low group respectively (p <0.001).
Participants in the high group also reported significantly greater mean number of unprotected (i.e., no condom use) insertive anal sex partners in the past 6 months across ages (mean = 2.1) while the medium group reported a mean number of unprotected insertive anal sex partners of 0.4, and the men in low group reported zero unprotected insertive anal sex partners in the past 6 months across ages (p < 0.001). Similarly, the mean number of unprotected receptive anal sex partners for the high group, medium group, and low group are 1.6, 0.3, and 0, respectively (p < 0.001).
The trajectory groups are not statistically different in other risk behaviors such as number of drinks per week, binge drinking, other recreational drug use, as well as depressive symptoms. However, with respect to HIV-related attitudes, three of the five subscales of the HIV-related attitudes, namely ‘reduced HIV concern’, ‘safer sex fatigue’ and ‘sexual sensation-seeking’ were differentially associated with the trajectory groups (see Table 2). The men in the high group were most likely to report that they were less concerned with HIV, no longer interested in safer sex messages and were more likely to seek wild sex compared to men in the medium group and low group. Perception of HIV as a health threat, and viral load/transmission beliefs were not significantly different among the trajectory groups.
Table 2.
HIV-related Attitudes
| Low (N=46) | Medium (N=164) | High (N=27) | P | |
|---|---|---|---|---|
| Reduced HIV concern mean (sd) | 1.3 (0.8) | 1.2 (0.4) | 1.5 (0.6) | 0.012 |
| Perception of HIV as a threat mean (sd) | 1.9 (1.0) | 1.7 (0.8) | 1.8 (0.9) | 0.135 |
| Safer sex fatigue mean (sd) | 1.8 (0.9) | 2.0 (0.9) | 2.8 (1.0) | <0.001 |
| Viral load/transmission beliefs mean (sd) | 1.8 (1.1) | 1.5 (0.8) | 1.8 (0.8) | 0.193 |
| Sexual sensation-seeking, mean (sd) | 2.3 (1.3) | 2.7 (1.2) | 3.5 (1.2) | <0.001 |
In the high trajectory group, 21 participants were found to have met new partners in the past 6 months at visit 50. Among them, 9 (42.9%)were found to have met new partners via the Internet, 8 (38.1%) at the bathhouse, and 7 (33.3%) at the bathroom, bookstore, and other public indoor places.
DISCUSSION
The current study is novel in that it applied a longitudinal analytic approach to study sexual risk behaviors among older sexual minority populations. The study identified distinct trajectories with respect to the number of sexual partners in the past 6 months reported by MSM between the ages of 50 to 59.5. Specifically, we identified a group which reported no sexual partners across this age range (“low group”), a group with a median of two partners consistently across this age range (“medium group”), and a small group whose number of sexual partners started at 30 or more at the age 50 and declined to 20 by age 53 and persisted through age 60 (“high group”). Men in the high group were all Caucasian, reported higher use of marijuana, poppers, crack cocaine, and Viagra, and higher number of unprotected anal sex partners compared to the men in the low and medium group.
As one of the first studies to examine trajectories with respect to the number of sex partners in older MSM, this current study has no previous data with which to compare these findings. Although our sample lacks diversity in race and socioeconomics (over 90% of the sample were Caucasian with a median of 15 years of education), race was found to be associated with the trajectory groups.
As expected, the men in the “high partner group” were most likely to report ‘reduced concerns with HIV’, ‘safer sex fatigue’ and ‘sexual sensation seeking’ than the men in other trajectory groups. This finding is consistent with a previous substudy of the Multicenter AIDS Cohort Study which found association between ‘safer sex fatigue’ and unprotected anal intercourse [24]. Men classified in the high group were also found to have higher number of unprotected anal intercourse partners, both insertive and receptive, than men in the low and medium group. While marijuana and popper, and Viagra use were differentially associated with the trajectory groups, smoking, binge drinking, use of crack, cocaine, meth or ecstasy, and depressive symptoms were not differentially associated with trajectory groups.
The association of marijuana, popper use, and Viagra with sexual partner trajectories can be expected because of the intertwining of drugs and sex in the gay male population [25]. There is also convincing evidence that MSM maintain higher rates of recreational drugs in their later life when compared with their heterosexual counterparts [25]. However, the lack of association between depressive symptoms and the number of sexual partners was surprising. The finding is in contradiction of the co-occurrence of drug use, depression and risky sexual behaviors documented in previous research with urban gay and bisexual men [26]. Nevertheless, this finding is consistent with Cooperman’s study [27]of older high-risk men from New York City (n=624), which found a lack of association of depressive symptoms, also measured by CES-D, with risky sexual behaviors. Additionally, the result is consistent with our previous study which did not find the association between trajectories of depressive symptoms with risky sexual behavior in older gay and bisexual men in the Pitt Men’s Study [28].
With respect to HIV status, men in the high group have a lower prevalence of HIV (40.7%) as compared to the low group (60.9 %) but higher as compared to the medium group (38.4 %). Medical and psychosocial reasons can explain why older HIV-positive MSM may reduce their sexual activity and, consequently, risky sexual behaviors. Cooperman et al. (2007) found that HIV-positive men reported significantly less sexual activity and risky sexual behaviors in the past 6 months compared to their HIV-negative counterparts. This is because men living with HIV, in general, have more co-morbid conditions which can compromise their sexual functions and reduce their sexual desires. They are also known to have higher prevalence of erectile dysfunction because of the side effects of antiretroviral therapy. In this study, the majority of men in the low sex partners group are HIV+ and yet they seemed to use less Viagra compared to men in the medium group and the high group. (This suggests off-label use of Viagra in the high group, or at least the use was not due to ED from being HIV positive). Other psychosocial factors such as perceived reduced desirability and fear of rejection may make older MSM living with HIV to self-censor and reduce their sexual opportunity, which, in turns, reduce their sexual activity and sexual partners [29].
The limitations of the current study are the ones common in secondary data analysis. The Pitt Men’s Study was not an age-cohort study in which all participants of the same age were recruited at the beginning of the study. Therefore, the age range of the sample was wide. We were able to compensate for that by using a ‘cohort sequential design’ so that we can model the trajectories according to age instead of visit [19]. The age range was arbitrarily limited to 50 to 59.5 years because data were sufficient only in this age range. Nagin’s group-based modeling has been criticized for the potential to overly extract trajectory groups, which may not be true subgroups in the population [30]. Furthermore, Nagin warns against reification of the subgroups and emphasizes that the results should be used as a heuristic tool [31]. We noted that there was significant variability within the trajectory (the range of the number of sex partners in the high trajectory is wide), and that the trajectories are certainly more complex in the real world.
Second, our dependent variable, number of male sexual intercourse partners, involve both oral and anal sex partners. Although the transmission risk by oral sex is considerably smaller, we did not separate anal sex from oral sex because the number of anal sex partners was too small for meaningful longitudinal data analysis. Omission of several potentially important variables, particularly concerning partner-related factors, is also a limitation of the study. Where HIV risk is concerned, distinction of long-term, regular sexual partners from casual, newly acquired sexual partners is important. Unfortunately, the type of partnerships of multiple sexual partners could not be ascertained from the Pitt Men’s Study. In the similar vein, our data could not distinguish serial monogamy and concurrency, which could place older MSM at higher risk for HIV infections.
In the sub-analysis, for men in the high group who reported meeting new partners in the past 6 months, the Internet, bathhouses, bathrooms, and bookstores were the most often mentioned venues where they met new partners. The social, interpersonal, physical and attitudinal contexts involved in the use of these venues require further investigation. For example, sex tourism may be an important social context for older MSM to acquire greater risk for HIV [32]. A study in Key West, a gay resort for older MSM, shows that MSM who attended gay resorts encountered multiple anal sex partners over a brief period, which might have elevated their risks for HIV and STD infection [33].
Additionally, expectation of monogamy and sexual exclusivity in a gay couple relationship may be important for this population. For example, some gay men reported that they could disassociate love from sex and, because of a partner’s discrepant sexual desires, they sought sex partners outside of long-term committed relationship [34]. Moreover, intergenerational relationship among gay men [35] and preference for older gay men by certain ethnic gay men[36]have been reported. A psychological context for older men and sensation seeking is the need to hold onto youth or to prove that “I still have it” [37]. This context may be a key to driving some older men to have sex with higher numbers of sex partners. Other psychosocial variables, such as loneliness [5], social marginalization within and without the gay community [5], a sense of self [38], as well as the desire for intimacy [6]should also be considered in future research when examining trajectories of multiple sexual partners in this population.
This study found that the medium trajectory group has the lowest proportion of HIV-positive men (37%) compared to the low (58.5%) and high group (42.5%). Men in the high group reported more unprotected anal intercourse partners than men in the low and medium groups. This is particularly worrisome because it means that men who acquired high number of sexual partners did not use a condom while having anal sex. The men in the high group may be those for whom further public health interventions might be most beneficial. While many evidence-based interventions have been designed to target young MSM, none specifically target older MSM. Certainly, current interventions should be tailored to target older men and this study suggests that the differences among members of this population need to be addressed. In this study, the men engaging in sex with the highest numbers male sex partners were more likely to use illicit drugs and to have reduced concern with HIV, to experience safer sex fatigue and to seek sexual sensation. More research is needed to ascertain whether different trajectories can be found among MSM of racial and ethnic minority background and to identify behaviors and attitudes associated with higher numbers of partners so that prevention interventions can be appropriately developed and delivered.
We look forward to the replication of this study by using similar methods to examine the trajectories of sex partners among MSM older than 60 as well as older MSM of racial or ethnic minorities. Only when we can identify and understand the interactions of the aforementioned risk factors can appropriate public health intervention be designed to reach these men.
Acknowledgments
The authors are grateful to the participants in the Pitt Men’s Study as well as the staff members of the Pitt Men’s Study. We would like to especially thank Ms. Carol Perfetti for her assistance in data preparation. This paper was completed as part of SH Lim’s dissertation in the Department of Epidemiology, Graduate School of Public Health of the University of Pittsburgh.
References
- 1.Mansergh G, Marks G. Age and risk of HIV infection in men who have sex with men. AIDS. 1998;12(10):1119–28. doi: 10.1097/00002030-199810000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Grossman AH. At risk, infected, and invisible: older gay men and HIV/AIDS. J Assoc Nurses AIDS Care. 1995;6(6):13–9. doi: 10.1016/S1055-3290(05)80010-X. [DOI] [PubMed] [Google Scholar]
- 3.CDC. Fact Sheet, Estimates of new HIV infections in the United States. Centers for Disease Control and Prevention; Atlanta, GA: 2008. [Google Scholar]
- 4.Dolcini MM, Catania JA, Stall RD, Pollack L. The HIV epidemic among older men who have sex with men. J Acquir Immune Defic Syndr. 2003;33:S115–S121. doi: 10.1097/00126334-200306012-00008. [DOI] [PubMed] [Google Scholar]
- 5.Murray J, Adam BD. Aging, sexuality, and HIV issues among older gay men. Can J Hum Sex. 2001;10(3–4):75–90. [Google Scholar]
- 6.Wierzalis EA, Barret B, Pope M, Rankins M. Gay men and aging: sex and intimacy. In: Kimmel D, Rose T, David S, editors. Lesbian, gay, bisexual, and transgender aging: research and clinical perspectives. New York: Columbia University Press; 2006. [Google Scholar]
- 7.Crepaz N, Marks G. Towards an understanding of sexual risk behavior in people living with HIV: a review of social, psychological, and medical findings. AIDS. 2002;16(2):135–49. doi: 10.1097/00002030-200201250-00002. [DOI] [PubMed] [Google Scholar]
- 8.van Kesteren NM, Hospers HJ, Kok G. Sexual risk behavior among HIV-positive men who have sex with men: a literature review. Patient Educ Couns. 2007;65(1):5–20. doi: 10.1016/j.pec.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 9.Brennan DJ, Welles SL, Miner MH, Ross MW, Rosser BR. HIV treatment optimism and unsafe anal intercourse among HIV-positive men who have sex with men: findings from the positive connections study. AIDS Educ Prev. 2010;22(2):126–37. doi: 10.1521/aeap.2010.22.2.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hart GJ, Elford J. Sexual risk behaviour of men who have sex with men: emerging patterns and new challenges. Curr Opin Infect Dis. 2010;23(1):39–44. doi: 10.1097/QCO.0b013e328334feb1. [DOI] [PubMed] [Google Scholar]
- 11.Ostrow DG, Fox KJ, Chmiel JS, et al. Attitudes towards highly active antiretroviral therapy are associated with sexual risk taking among HIV-infected and uninfected homosexual men. AIDS. 2002;16(5):775–780. doi: 10.1097/00002030-200203290-00013. [DOI] [PubMed] [Google Scholar]
- 12.Ostrow DG, Plankey MW, Cox C, et al. Specific sex drug combinations contribute to the majority of recent HIV seroconversions among MSM in the MACS. J Acquir Immune Defic Syndr. 2009;51(3):349–355. doi: 10.1097/QAI.0b013e3181a24b20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Finer LB, Darroch JE, Singh S. Sexual partnership patterns as a behavioral risk factor for sexually transmitted diseases. Fam Plann Perspect. 1999;31(5):228–36. [PubMed] [Google Scholar]
- 14.Hughes G, Brady AR, Catchpole MA, et al. Characteristics of those who repeatedly acquire sexually transmitted infections: a retrospective cohort study of attendees at three urban sexually transmitted disease clinics in England. Sex Transm Dis. 2001;28(7):379–86. doi: 10.1097/00007435-200107000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Parazzini F, Cavalieri D’oro L, Naldi L, et al. Number of sexual partners, condom use and risk of human immunodeficiency virus infection. Int J Epidemiol. 1995;24(6):1197–203. doi: 10.1093/ije/24.6.1197. [DOI] [PubMed] [Google Scholar]
- 16.Jacobs RJ, Fernandez MI, Ownby RL, Bowen GS, Hardigan PC, Kane MN. Factors associated with risk for unprotected receptive and insertive anal intercourse in men aged 40 and older who have sex with men. AIDS Care. 2010:1–8. doi: 10.1080/09540121003615137. [DOI] [PubMed] [Google Scholar]
- 17.Silvestre AJ, Lyter DW, Rinaldo CR, Jr, Kingsley LA, Forrester R, Huggins J. Marketing strategies for recruiting gay men into AIDS research and education projects. J Community Health. 1986;11(4):222–32. doi: 10.1007/BF01325118. [DOI] [PubMed] [Google Scholar]
- 18.Silvestre AJ, Hylton JB, Johnson LM, et al. Recruiting minority men who have sex with men for HIV research: results from a 4-city campaign. Am J Public Health. 2006;96(6):1020–7. doi: 10.2105/AJPH.2005.072801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mehta PD, West SG. Putting the individual back into individual growth curves. Psychol Methods. 2000;5(1):23–43. doi: 10.1037/1082-989x.5.1.23. [DOI] [PubMed] [Google Scholar]
- 20.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 21.Farinpour R, Miller EN, Satz P, et al. Psychosocial Risk Factors of HIV Morbidity and Mortality: Findings from the Multicenter AIDS Cohort Study (MACS) J Clin Exp Neuropsychol. 2003;25(5):654–670. doi: 10.1076/jcen.25.5.654.14577. [DOI] [PubMed] [Google Scholar]
- 22.Mills TC, Paul J, Stall R, et al. Distress and depression in men who have sex with men: the Urban Men’s Health Study. Am J Psychiatry. 2004;161(2):278–85. doi: 10.1176/appi.ajp.161.2.278. [DOI] [PubMed] [Google Scholar]
- 23.Nagin D. Analyzing developmental trajectories: a semi-parametric group-based approach. Psychol Methods. 1999;4:139–157. doi: 10.1037/1082-989x.6.1.18. [DOI] [PubMed] [Google Scholar]
- 24.Ostrow DE, Fox KJ, Chmiel JS, et al. Attitudes towards highly active antiretroviral therapy are associated with sexual risk taking among HIV-infected and uninfected homosexual men. AIDS. 2002;16(5):775–80. doi: 10.1097/00002030-200203290-00013. [DOI] [PubMed] [Google Scholar]
- 25.Ostrow DG, Stall R. Alcohol, tobacco and drug use among gay and bisexual men. In: Woltiski RJ, Stall R, Valdiserri RO, editors. Unequal opportunity: health disparities affecting gay and bisexual men in the United States. New York: Oxford University Press; 2008. [Google Scholar]
- 26.Stall R, Mills TC, Williamson J, et al. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am J Public Health. 2003;93(6):939–42. doi: 10.2105/ajph.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cooperman NA, Arnsten JH, Klein RS. Current sexual activity and risky sexual behavior in older men with or at risk for HIV infection. AIDS Educ Prev. 2007;19(4):321–33. doi: 10.1521/aeap.2007.19.4.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lim SH, Spencer SM, Kim K, Markovic N, Stall R, Silvestre AJ. Changing trajectories of depressive symptoms among a cohort of middle-aged and older men who have sex with men. J Gerontol B Psychol Sci Soc Sci. 2010 (under review) [Google Scholar]
- 29.Siegel K, Schrimshaw EW. Reasons for the adoption of celibacy among older men and women living with HIV/AIDS. J Sex Res. 2003;40(2):189–200. doi: 10.1080/00224490309552180. [DOI] [PubMed] [Google Scholar]
- 30.Bauer DJ, Curran PJ. Distribution assumptions for growth mixture models: Implications for overextraction of latent trajectory classes. Psychol Methods. 2003;8(3):338–363. doi: 10.1037/1082-989X.8.3.338. [DOI] [PubMed] [Google Scholar]
- 31.Nagin DS, Tremblay RE. Developmental trajectory groups: Fact or a useful statistical fiction? Criminology. 2005;43(4):873–904. [Google Scholar]
- 32.Wright ER. Travel, tourism, and HIV risk among older adults. J Acquir Immune Defic Syndr. 2003;33:S233–S237. doi: 10.1097/00126334-200306012-00023. [DOI] [PubMed] [Google Scholar]
- 33.Benotsch EG, Mikytuck JJ, Ragsdale K, Pinkerton SD. Sexual risk and HIV acquisition among men who have sex with men travelers to Key West, Florida: A mathematical modeling analysis. AIDS Patient Care STDS. 2006;20(8):549–56. doi: 10.1089/apc.2006.20.549. [DOI] [PubMed] [Google Scholar]
- 34.Shernoff M. Negotiated nonmonogamy and male couples. Fam Process. 2006;45(4):407–418. doi: 10.1111/j.1545-5300.2006.00179.x. [DOI] [PubMed] [Google Scholar]
- 35.Steinman R. Social exchanges between older and younger gay male partners. J Homosex. 1991;20:179–206. doi: 10.1300/j082v20n03_12. [DOI] [PubMed] [Google Scholar]
- 36.Ellen JM, Brown BA, Chung SE, et al. Impact of sexual networks on risk for gonorrhea and chlamydia among low-income urban African American adolescents. J Pediatr. 2005;146(4):518–22. doi: 10.1016/j.jpeds.2004.11.023. [DOI] [PubMed] [Google Scholar]
- 37.Rubin R. Men talking about Viagra. Men Masc. 2004;7(1):22–30. [Google Scholar]
- 38.van Kesteren NM, Hospers HJ, van Empelen P, van Breukelen G, Kok G. Sexual decision-making in HIV-positive men who have sex with men: How moral concerns and sexual motives guide intended condom use with steady and casual sex partners. Arch Sex Behav. 2007;36(3):437–49. doi: 10.1007/s10508-006-9125-4. [DOI] [PMC free article] [PubMed] [Google Scholar]