Abstract
Objective
We investigated whether particular demographic, maternal psychosocial, and infant factors identified mothers of very preterm infants at risk for postpartum depression or anxiety at the time of discharge from a level III urban Neonatal Intensive Care Unit (NICU).
Study Design
A racially diverse cohort of mothers (N=73) of preterm infants (gestational age <30 weeks) completed a comprehensive questionnaire at discharge from the NICU assessing postpartum depression, anxiety, and psychosocial and demographic factors. Additionally, infants underwent brain magnetic resonance imaging prior to discharge.
Result
Twenty percent of mothers had clinically significant levels of depression while 43% had moderate-severe anxiety. Being married (p<.01), parental role alteration (p<.01) and prolonged ventilation (p<.05) were associated with increased depressive symptoms. No psychosocial, demographic, or infant factors, including severity of brain injury, were associated with state anxiety levels.
Conclusion
Maternal factors, such as marital status, stress from parental role alteration, and infant factors, such as prolonged ventilation, are associated with increased depression. However, clinically significant levels of anxiety are common in mothers of very preterm infants with few identifiable risk factors. These findings support the need for universal screening within the NICU.
Keywords: Risk Factors, Racial Differences, NICU
Introduction
Postpartum depression is a significant public health issue with rates reported between 10% and 15% in the general population.1 Mothers of preterm infants are at particular risk for poor postpartum functioning with rates of depression from 14% to 27%.2 Indeed, rates of clinically elevated depressive symptoms can be as high as 63% during the preterm infant’s hospitalization.3 More recently, increased levels of anxiety and acute stress among mothers of infants cared for in the Neonatal Intensive Care Unit (NICU) have been reported.4, 5 Maternal postpartum depression and anxiety affect child development with detrimental effects on cognitive6, 7 and social-emotional development7, 8 as well as parent-child interactions.9 Preterm infants appear more sensitive to the impact of poor maternal mental health as compared to full term infants.10, 11
The risk factors for postpartum depression in the general population include a prior history of depression, life stress, poor social support, marital discord, single marital status and low socioeconomic status.12 Another important factor, maternal smoking, is a risk factor for preterm delivery,13 as well as depressive symptoms during pregnancy14 and the postpartum period in mothers of both preterm and full-term infants.15,13 Prior research has identified risk factors for anxiety in mothers of very low birth weight (<1000 g) infants including marital status and social support,16 though this study measured trait anxiety reflecting mothers underlying propensity for anxiety rather than their current anxiety levels. Additional risk factors for postpartum depression and anxiety specific to the NICU setting include perception of the infant’s illness severity3, 17, poor coping skills, increased parenting stress, perceived parental role alteration18, length of ventilation11, 19 and length of stay in the NICU.11 In contrast to the general population, demographic risk factors, such as maternal education and age, have not been consistently associated with depressive symptoms among mothers of preterm infants though marital status was still an important risk factor.3
Ethnicity is another demographic factor that has not been consistently related to maternal postpartum functioning. It is well-established that African Americans are at the highest risk of preterm birth with rates at least twice that of Caucasians.20, 21 It is unclear, however, if they are at higher risk for postpartum depression and anxiety. Among the general population, African Americans are at increased risk of depression20, 22, 23 including during the postpartum period24 compared to non-Hispanic Caucasians. Among mothers of preterm infants, some report increased rates of postpartum depressive symptoms for African Americans25 while others do not.3 Different rates of risk factors between these samples may explain this discrepancy.
Identification of the risk factors predictive for poor postpartum functioning would assist in the recognition and referral of mothers at greatest risk prior to taking home their vulnerable infants. One study in mothers of infants born less than 35 weeks gestation reported that the interaction between maternal demographic characteristics conferred greater risk than the infant’s medical severity for mothers with elevated demographic risk, low social support and infants with very low birthweight.11 To date, however, the risk factors for poor postpartum functioning have not been well-studied in a sample that has both elevated demographic risk and medically fragile very preterm infants, representing the most vulnerable mother-infant dyads. To address this gap, the current study aims to assess which factors are most useful for identifying mothers at-risk for postpartum depression or anxiety at the time of discharge from the NICU by investigating the impact of demographic, maternal psychosocial and infant factors in a cohort of Caucasian and African American mothers of very preterm infants at a level III NICU.
Patients and Methods
Participants
This study was a prospective cohort design recruiting preterm infants born at less than 30 weeks gestation within the first 3 days of life over a three-year period. The study was approved by the institutional human ethics committee. Exclusion criteria included having a known congenital anomaly or being moribund with severe sepsis or respiratory failure in the first days of life. All infants whose parents gave informed consent for magnetic resonance imaging (MRI) were scanned during the NICU hospitalization. In addition, clinical information on the infant and mother were collected from the medical record, and each primary caregiver completed a comprehensive questionnaire at discharge from the NICU.
Measures
Maternal postpartum depression was measured with the Edinburgh Postnatal Depression Scale (EPDS). The EPDS is a 10-item self-report measure with good validity that assesses symptoms of postpartum depression among mothers over the last 7 days.27, 28 A score of 13 (range 0–30) or greater indicates a mother with clinically significant depression. The State-Trait Anxiety Inventory (STAI) is a widely used and reliable assessment of anxiety in adults and consists of two 20-item scales that differentiate between anxiety as a personality trait and conditional anxiety.29, 30 State anxiety was used as the outcome measure to reflect the anxiety that resulted from having a very preterm infant in the NICU. Moderate anxiety was defined by a score between 40 and 59 with severe anxiety between 60 and 80, as per published guidelines.29
Demographic Factors
Information on maternal age, race, education, and marital status were collected from the questionnaire by caregiver report. Insurance status, used as a proxy measure for socioeconomic status (SES), was obtained from the clinical record and dichotomized into public insurance or private insurance. Maternal education was dichotomized as those who attained the equivalent or less than high school degree or a college education or higher.
Maternal Psychosocial History
Data on prior history of depression or anxiety, smoking, stressful life events, and social support satisfaction were collected. Histories of depression and/or anxiety were obtained both by self-report in the discharge questionnaire as well as from the maternal clinical records. Maternal smoking was obtained by self-report and dichotomized into those who smoked at least 1 cigarette/day and non-smokers. Stressful life events were measured via the Life Stress subscale of the Parenting Stress Index (PSI),31 assessing stressful situational circumstances outside of parenting (e.g., death of a relative, loss of a job).32 Social support satisfaction was measured with the Social Support Questionnaire (SSQ) which rates satisfaction with self-identified sources of support.33 Parental role alteration was assessed using the parental role alteration subscale of the Parental Stressor Scale: Neonatal Intensive Care Unit (PSS)34, which has good reliability and internal consistency.35
Infant Factors
The following Infant factors were hypothesized a priori to impact maternal depression or anxiety: number of days of ventilation, length of stay, and extent of brain injury. The extent of brain injury was assessed from cranial ultrasound conducted at clinical discretion and from a study-related MRI conducted without sedation. MRI results were interpreted by a single, trained neurologist to determine the presence of focal white matter lesions, cystic periventricular leukomalacia (PVL), and cerebellar hemorrhage. Brain injury was dichotomized into no to mild abnormality or moderate to severe abnormality (IVH Grade III or IV; and/or moderate-severe white matter injury including multiple focal lesions and/or cystic PVL; and cerebellar hemorrhage). The results of the neuroimaging were communicated to the primary caregivers prior to completion of the discharge questionnaire, including estimated prognosis for motor and cognitive development for the infant, by a trained neonatologist and neurologist (TI).
For mothers of multiples, the infant with the most severe clinical presentation based on length of stay, length of ventilation, and degree of brain injury was chosen for the analysis in order to best assess the association between having a medically ill infant and maternal functioning.
Data Analysis
To assess the differential impact of the individual demographic (maternal age, race, education, marital status and insurance status), maternal psychosocial (prior history of depression or anxiety, smoking, stressful life events, parental role alteration, and social support satisfaction), and infant risk factors (number of days of ventilation, length of stay, and extent of brain injury) on depression and anxiety, each set of factors was entered into hierarchical linear regression models with EPDS and STAI-S scores as the outcome variables. The maternal psychosocial factors were entered in the first step, demographic factors entered in the second step and infant factors added in the final step. Maternal psychosocial factors were entered first based on the larger impact of these factors over demographic factors on depressive symptoms in the general population.12 Infant factors were added last as the literature has been mixed on the impact of infant health status on outcome. Within each step, the factors were entered with a stepwise procedure which retained variables with a p value <0.1. Possible disparities in the rates of risk factors between Caucasian and African American mothers were calculated using t-tests for continuous variables and chi-square analyses for categorical variables. Significant factors from the hierarchical regression model and factors more prevalent in one race (age, insurance status, and marital status) were evaluated for interactions with race by analysis of covariance.
Results
There were a total of 83 Caucasian and African-American mothers of surviving infants enrolled in the study. 73 mother-infant dyads had complete data and were included in this analysis. Those with missing data had shorter lengths of stay (t=2.23, p=.03) compared to those included in the analysis. There were no other significant differences between those with missing data and those included in the analysis.
Maternal and infant characteristics are presented in Table 1. Significant differences in demographic factors were as follows: African American mothers were more likely to be unmarried (p<.001), be on public aid (p<.001), and be younger (p=.009). There was a trend for African American mothers to have less education (p=.09).
Table 1.
Maternal Characteristics
| TOTAL % /M (SD) N =73 |
CAUCASIAN % /M (SD) N= 36 |
AFRICAN AMERICAN % /M (SD) N= 37 |
|
|---|---|---|---|
| Demographics | |||
| Age | 27.2 (7.4) | 29.5 (8.2) | 25.0 (5.9)** |
| Education HS or less | 46.5% | 37.1% | 55.6% |
| Married | 42.5% | 73.5% | 10.8%** |
| Public Insurance | 69.0% | 50% | 86.5%** |
| First born | 34.3% | 34.% | 34.3% |
| Multiple birth | 15.1% | 19.4% | 10.8% |
| Psychosocial | |||
| Prior Dep/Anx | 17.8% | 16.7% | 18.9% |
| Social Support | 5.5 (1.0) | 5.6 (0.9) | 5.5 (1.0) |
| Parental Role | 3.1 (1.1) | 3.0 (1.0) | 3.0 (1.2) |
| Life Events | 3.0 (1.9) | 3.3 (1.7) | 2.6 (2.1) |
| Smoking | 12.3% | 11.1% | 13.5% |
| Dep/Anxiety | |||
| EPDS | 7.0 (6.0) | 7.9 (6.3) | 6.1 (5.7) |
| Clinical PPD | 20% | 22% | 18% |
| STAI-S | 38.7 (15.6) | 37.8 (15.2) | 39.6 (16.1) |
| Mod-sev Anx | 42.9% | 34.3% | 51.4% |
| Infant | |||
| #days on TPN, | 26.4 (22.7) | 24.0 (21.5) | 28.7 (23.9) |
| # of Vent days | 16.9 (31.8) | 13.1 (21.8) | 20.6 (39.1) |
| Crib Score | 4.2 (3.8) | 3.9 (3.3) | 4.5 (4.3) |
| Length of Stay | 90.5 (28.6) | 88.7 (24.9) | 92.3 (32.1) |
| GA | 26.5 (1.8) | 26.7 (2.0) | 26.2 (1.6) |
| Mod-Sev brain injury | 44.3% | 50% | 38.9% |
HS = High School, Dep = Depression, Anx = Anxiety, EPDS = Edinburgh Postnatal Depression Scale, PPD = Postpartum Depression, STAI-S= State Trait Anxiety Inventory-State, Mod-Sev = moderate to severe, TPN = Total Parenteral Nutrition, Vent= Ventilation, GA= Gestational Age
=p<.01
Depressive Symptoms
The results of the hierarchical regressions with the individual risk factors that were significant for each block for the EPDS are displayed in Table 2. The only psychosocial risk factor that remained in the model was parental role alteration. Among demographic risks, being married was the only significant factor in the second step. In the final step, the number of ventilation days was the only significant infant factor. The final model with all of three of these factors was significant (R2 =0.31 and p<.001).
Table 2.
Risk factors for EPDS scores
| β | 95 % CI | p | |
|---|---|---|---|
| Factor | |||
| Parental Role Alteration | .309 | 0.09 to 0.53 | .007 |
| Marital Status | .397 | 0.18 to 0.62 | .001 |
| # of Ventilation Days | .336 | 0.12 to 0.56 | .003 |
β is standardized estimate = number of standard deviations (SD) outcome will change with 1 SD change in predictor.
Interactions between race and significant factors (marital status, ventilation days, and parental role alteration) and between race and factors that differed between Caucasian and African American mothers (age, insurance status) were tested and were not significant (data not shown).
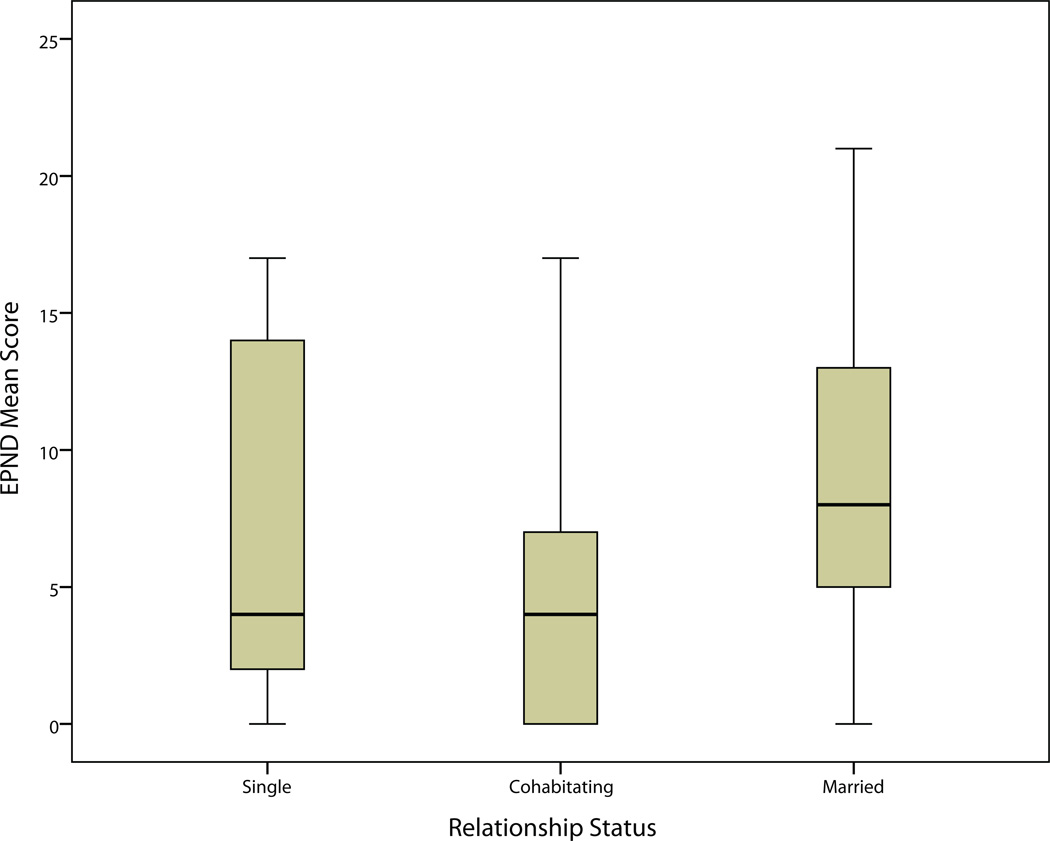
Given the unexpected finding that being married was associated with higher levels of depressive symptoms, we conducted exploratory analyses of this relationship. Comparing those that were married to those that were unmarried, married mothers had higher mean EPDS scores (t=−2.4, p=.02). Twenty-six percent of married mothers had clinical levels of depression compared to 15% of unmarried mothers (χ2 =1.2, p=.28). Married mothers had higher EPDS scores compared to unmarried mothers cohabitating (mean EPDS 8.9 vs. 4.3 respectively, F=2.9, p=.03) but not from single mothers (mean EPDS 6.7, Figure 1.). Other factors reported to be associated with depressive symptoms, notably receiving fertility treatments36 and marital separation used as a proxy for marital discord12 were evaluated. Use of fertility treatment was reported in only five participants, all of whom were married. Separation from their spouse was reported in three participants. Being married continued to be a predictor after adjusting for fertility treatment (β =.46, p=.002) or marital separation (β =.6, p<.001). Another potential confound, multiple births, noted to be associated with postpartum depression36 was also assessed. There was no difference in the rate of multiple births between married and unmarried mothers (χ2 = 0.77 p=.38). Additionally, there were no differences between the infant factors with reported impact on postpartum depression for married and unmarried mothers (ventilation days t=.83, p=.41; length of stay, t=.58, p=.57).
Figure 1.
Comparison of EPND scores of single, unmarried cohabitating, and married mothers.
Anxiety symptoms
None of the psychosocial, demographic, or infant risk factors significantly predicted STAI state (STAI-S) scores. Post hoc analyses found no correlation between the number of children and STAI-S scores (r=.11 p=.23) nor any difference in mean STAI-S scores between those who did or did not have children previously (t =.10, p=.92). Parenting confidence was also assessed by maternal rating of their parenting skills. There was no association between parenting confidence and STAI-S scores. In addition, the anxiety traits of the cohort were explored. The mean STAI trait score was 33.8 with 27% of mothers having moderate trait anxiety and none having severe trait anxiety. There was a modest correlation between the STAI state and STAI trait scores (r=.4, p=.001).
Discussion
In this study of Caucasian and African American mothers of very preterm infants, there were specific factors that were associated with postpartum depressive symptoms at the time of discharge. In contrast, none of the risk factors analyzed were associated with anxiety at NICU discharge. Approximately 20% of mothers had clinical levels of depression, similar to previous reports.2 There was no difference in the rate of postpartum depression between Caucasian and African American mothers. While modest levels of anxiety are reasonably anticipated upon discharge from the NICU, rates of moderate to severe state anxiety were found in 43% of mothers in this cohort, present at the time of discharge often many months after the initial admission. Indeed, the cohorts mean anxiety score was similar to means reported at much earlier time points in the NICU hospitalization.37, 38 The modest association between trait and state anxiety suggests that the elevated state anxiety was not due to an over-representation of temperamentally anxious mothers. The rates of moderate-severe anxiety did not differ between Caucasian and African American mothers.
We found that being married, experiencing parental role alteration, and increased length of ventilation were the only risk factors associated with elevated postpartum depressive symptoms. It was a surprising finding that being married was associated with postpartum depression, given unmarried status has been previously associated with postpartum depression.3, 12 This discrepancy was accounted for by unmarried, cohabitating mothers having the lowest EPDS scores. Evidence has shown that it is poor relationship quality, and not marital status per se, that is related to increased postpartum depression.39 The infants in this study had a much longer NICU hospitalization than similar research that found marriage protective3 which may have increased the stress on married couples. It is also possible that more married couples compared to cohabiting couples had planned or intended pregnancies and thus, preterm delivery and this prolonged NICU stay may have had a greater impact on married mothers’ emotional well-being. Information on relationship quality and pregnancy intention were not captured in the current study.
Experiencing parental role alteration and the length of ventilation have been previously reported as risk factors.11, 18, 19 Both factors relate to the disruption in the typical maternal-infant connectedness that occurs when an infant is in the NICU. Prolonged ventilation likely indicates not only greater medical severity but also prolonged physical separation. Thus, both of these factors may identify dyads at greatest risk for poor attachment which is detrimental to both maternal functioning and infant development.
Another unexpected finding was that a prior history of depression and anxiety was not related to current symptoms of depression and anxiety. One possible explanation is that mothers underreported their prior histories of symptoms and this may have been better assessed with a clinical interview rather than by self-report. Nevertheless, while a history of depression/anxiety has been noted to be predictive in other studies in the general population, this has not been confirmed in prior cohorts of preterm infants.40 Unfortunately, prior research with mothers of preterm infants with racially diverse samples did not evaluate the impact of a history of prior depression on postpartum depression symptoms3.
The most unexpected result was the lack of significant predictors for state anxiety. Prior research had found risk factors for trait anxiety, a different construct, with a sample that was less racially diverse, had less social disadvantage and had infants with an older mean gestational age. It is particularly notable that there was no relationship between the severity of the medical course or the presence of brain injury with maternal anxiety. While there may be other unmeasured risk factors for anxiety, this finding suggests that a large proportion of mothers of very preterm infants are at elevated risk for significant and impairing levels of anxiety even after the infant’s medical condition has stabilized. This highlights the importance of surveillance of mothers of very preterm infants for impairing levels of anxiety at discharge from the NICU, at postpartum visits and well baby check-ups. It also highlights how challenging it may be for the clinical team to identify the mother at greatest risk as the majority of clinical teams would assign risk based on demographic, psychosocial history and/or severity of infant illness.
This study has several strengths including the racial and socioeconomic diversity of the cohort as well as a more comprehensive set of risk factors including a prior history of depression/anxiety and severity of brain injury. Limitations include that we report on findings at only one time point so it is unclear if these factors continue to confer risk over time. This cohort is part of a longitudinal study and subsequent investigation of the persistence of maternal postpartum symptoms during infancy and childhood as well the impact of these early risk factors will be undertaken. Nevertheless, early attachment with infants is important for promoting development and elevated depressive or anxiety symptoms at discharge may increase the risk of attachment difficulties and impact the care of these infants when they are still medically fragile. Another possible limitation is that this cohort was recruited from an urban level III NICU, and thus, these results may not be generalizable to all mothers of VPT infants, nor to all Caucasian and African American mothers.
Conclusion
The findings from this study confirm the common nature of maternal postpartum depression and anxiety disorders in mothers of very preterm infants at the time of discharge from the NICU. Identification of risk factors (marital state/satisfaction, parental role alteration, and length of ventilation) may assist physician and other team members to screen for this disorder. In contrast, anxiety is commoner and had no identifiable risk factors. Universal screening for anxiety in the NICU would be required to identify mothers with moderate-severe anxiety. Future research is needed to study the relationship between the identified risk factors and the duration of depression and anxiety in this population and to determine whether targeting interventions early in the NICU hospitalization to mothers identified as at-risk reduces symptoms prior to discharge.
Acknowledgments
Sources of Support: This study was funded by the National Institutes of Health under NICHD R01 HD057098-01, NIAAA T32 5T32AA007580, NCRR/NCATS UL1 RR024992, and the Doris Duke Charitable Foundation.
Footnotes
Financial Disclosures: Drs. Rogers, Kidokoro, Wallendorf, and Inder report no biomedical financial interests or potential conflicts of interest.
References
- 1.O’Hara MW, Swain AM. Rates and risk of postpartum depression—a meta-analysis. International Review of Psychiatry. 1996;8(1):37–54. [Google Scholar]
- 2.Anon Prevalence of self-reported postpartum depressive symptoms--17 states, 2004–2005. MMWR Morb. Mortal. Wkly. Rep. 2008;57(14):361–366. [PubMed] [Google Scholar]
- 3.Miles MS, Holditch-Davis D, Schwartz TA, Scher M. Depressive symptoms in mothers of prematurely born infants. J Dev Behav Pediatr. 2007;28(1):36–44. doi: 10.1097/01.DBP.0000257517.52459.7a. [DOI] [PubMed] [Google Scholar]
- 4.Carter JD, Mulder RT, Bartram AF, Darlow BA. Infants in a neonatal intensive care unit: parental response. Arch. Dis. Child. Fetal Neonatal Ed. 2005;90(2):F109–F113. doi: 10.1136/adc.2003.031641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vanderbilt D, Bushley T, Young R, Frank DA. Acute posttraumatic stress symptoms among urban mothers with newborns in the neonatal intensive care unit: a preliminary study. J Dev Behav Pediatr. 2009;30(1):50–56. doi: 10.1097/DBP.0b013e318196b0de. [DOI] [PubMed] [Google Scholar]
- 6.Hay DF, Pawlby S, Waters CS, Sharp D. Antepartum and postpartum exposure to maternal depression: different effects on different adolescent outcomes. J Child Psychol Psychiatry. 2008;49(10):1079–1088. doi: 10.1111/j.1469-7610.2008.01959.x. [DOI] [PubMed] [Google Scholar]
- 7.Zelkowitz P, Na S, Wang T, Bardin C, Papageorgiou A. Early maternal anxiety predicts cognitive and behavioural outcomes of VLBW children at 24 months corrected age. Acta Paediatr. 2011 doi: 10.1111/j.1651-2227.2010.02128.x. Available at: http://www.ncbi.nlm.nih.gov/pubmed/21214883. [DOI] [PubMed]
- 8.Carter AS, Garrity-Rokous FE, Chazan-Cohen R, Little C, Briggs-Gowan MJ. Maternal depression and comorbidity: predicting early parenting, attachment security, and toddler social-emotional problems and competencies. J Am Acad Child Adolesc Psychiatry. 2001;40(1):18–26. doi: 10.1097/00004583-200101000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Nicol-Harper R, Harvey AG, Stein A. Interactions between mothers and infants: impact of maternal anxiety. Infant Behav Dev. 2007;30(1):161–167. doi: 10.1016/j.infbeh.2006.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bugental DB, Beaulieu D, Schwartz A. Hormonal sensitivity of preterm versus full-term infants to the effects of maternal depression. Infant Behav Dev. 2008;31(1):51–61. doi: 10.1016/j.infbeh.2007.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Poehlmann J, Fiese BH. The interaction of maternal and infant vulnerabilities on developing attachment relationships. Dev. Psychopathol. 2001;13(1):1–11. doi: 10.1017/s0954579401001018. [DOI] [PubMed] [Google Scholar]
- 12.Beck CT. Predictors of postpartum depression: an update. Nurs Res. 2001;50(5):275–285. doi: 10.1097/00006199-200109000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Yuan W, Duffner AM, Chen L, et al. Analysis of preterm deliveries below 35 weeks’ gestation in a tertiary referral hospital in the UK. A case-control survey. BMC Res Notes. 2010;3:119. doi: 10.1186/1756-0500-3-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lancaster CA, Gold KJ, Flynn HA, et al. Risk factors for depressive symptoms during pregnancy: a systematic review. Am. J. Obstet. Gynecol. 2010;202(1):5–14. doi: 10.1016/j.ajog.2009.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McCoy SJB, Beal JM, Shipman SBM, Payton ME, Watson GH. Risk factors for postpartum depression: a retrospective investigation at 4-weeks postnatal and a review of the literature. J Am Osteopath Assoc. 2006;106(4):193–198. [PubMed] [Google Scholar]
- 16.Zelkowitz P, Bardin C, Papageorgiou A. Anxiety affects the relationship between parents and their very low birth weight infants. Infant Ment. Health J. 2007;28(3):296–313. doi: 10.1002/imhj.20137. [DOI] [PubMed] [Google Scholar]
- 17.Shields-Poë D, Pinelli J. Variables associated with parental stress in neonatal intensive care units. Neonatal Netw. 1997;16(1):29–37. [PubMed] [Google Scholar]
- 18.Spear ML, Leef K, Epps S, Locke R. Family reactions during infants’ hospitalization in the neonatal intensive care unit. Am J Perinatol. 2002;19(4):205–213. doi: 10.1055/s-2002-28484. [DOI] [PubMed] [Google Scholar]
- 19.Poehlmann J, Schwichtenberg AJM, Bolt D, Dilworth-Bart J. Predictors of depressive symptom trajectories in mothers of preterm or low birth weight infants. J Fam Psychol. 2009;23(5):690–704. doi: 10.1037/a0016117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mew AM, Holditch-Davis D, Belyea M, Miles MS, Fishel A. Correlates of depressive symptoms in mothers of preterm infants. Neonatal Netw. 2003;22(5):51–60. doi: 10.1891/0730-0832.22.5.51. [DOI] [PubMed] [Google Scholar]
- 21.Gavin AR, Chae DH, Mustillo S, Kiefe CI. Prepregnancy depressive mood and preterm birth in black and white women: findings from the CARDIA Study. J Womens Health (Larchmt) 2009;18(6):803–811. doi: 10.1089/jwh.2008.0984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.U.S. Department of Health and Human Services, Administration on Children, Youth and Families. Child Maltreatment 2007. Washington, DC: U.S. Government Printing Office; 2009. [Google Scholar]
- 23.McLennan JD, Kotelchuck M, Cho H. Prevalence, persistence, and correlates of depressive symptoms in a national sample of mothers of toddlers. J Am Acad Child Adolesc Psychiatry. 2001;40(11):1316–1323. doi: 10.1097/00004583-200111000-00012. [DOI] [PubMed] [Google Scholar]
- 24.Gazmararian JA, James SA, Lepkowski JM. Depression in black and white women. The role of marriage and socioeconomic status. Ann Epidemiol. 1995;5(6):455–463. doi: 10.1016/1047-2797(95)00061-5. [DOI] [PubMed] [Google Scholar]
- 25.Howell EA, Mora PA, Horowitz CR, Leventhal H. Racial and ethnic differences in factors associated with early postpartum depressive symptoms. Obstet Gynecol. 2005;105(6):1442–1450. doi: 10.1097/01.AOG.0000164050.34126.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Poehlmann J, Schwichtenberg AM, Bolt D, Dilworth-Bart J. Predictors of depressive symptom trajectories in mothers of preterm or low birth weight infants. Journal of Family Psychology. 2009;23(5):690–704. doi: 10.1037/a0016117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 28.Cox JL, Chapman G, Murray D, Jones P. Validation of the Edinburgh Postnatal Depression Scale (EPDS) in non-postnatal women. J Affect Disord. 1996;39(3):185–189. doi: 10.1016/0165-0327(96)00008-0. [DOI] [PubMed] [Google Scholar]
- 29.Spielberger CD. State-Trait Anxiety Inventory (Form Y) Manual. California, USA: Mind Garden, Inc.; 1983. [Google Scholar]
- 30.Spielberger C. Assessment of state and trait anxiety: Conceptual and methodologicalissues. The Southern Psychologist. 2:6–16. [Google Scholar]
- 31.Loyd BH, Abidin RR. Revision of the Parenting Stress Index. J Pediatr Psychol. 1985;10(2):169–177. doi: 10.1093/jpepsy/10.2.169. [DOI] [PubMed] [Google Scholar]
- 32.Abidin RR. Parenting Stress Index Professional Manual. USA: Psychological Assessment Resources, Inc; 1995. [Google Scholar]
- 33.Sarason IG, Levine HM, Basham RB, Sarason BR. Assessing social support: The Social Support Questionnaire. Journal of Personality and Social Psychology. 1983;44(1):127–139. [Google Scholar]
- 34.Miles MS, Funk SG, Carlson J. Parental Stressor Scale: neonatal intensive care unit. Nurs Res. 1993;42(3):148–152. [PubMed] [Google Scholar]
- 35.Shields-Poë D, Pinelli J. Variables associated with parental stress in neonatal intensive care units. Neonatal Netw. 1997;16(1):29–37. [PubMed] [Google Scholar]
- 36.Monti F, Agostini F, Fagandini P, La Sala GB, Blickstein I. Depressive symptoms during late pregnancy and early parenthood following assisted reproductive technology. Fertil. Steril. 2009;91(3):851–857. doi: 10.1016/j.fertnstert.2008.01.021. [DOI] [PubMed] [Google Scholar]
- 37.Ross LE, McQueen K, Vigod S, Dennis C-L. Risk for postpartum depression associated with assisted reproductive technologies and multiple births: a systematic review. Hum. Reprod. Update. 2011;17(1):96–106. doi: 10.1093/humupd/dmq025. [DOI] [PubMed] [Google Scholar]
- 38.Melnyk BM, Feinstein NF, Alpert-Gillis L, et al. Reducing premature infants’ length of stay and improving parents’ mental health outcomes with the Creating Opportunities for Parent Empowerment (COPE) neonatal intensive care unit program: a randomized, controlled trial. Pediatrics. 2006;118(5):e1414–e1427. doi: 10.1542/peds.2005-2580. [DOI] [PubMed] [Google Scholar]
- 39.Erdem Y. Anxiety levels of mothers whose infants have been cared for in unit level-I of a neonatal intensive care unit in Turkey. J Clin Nurs. 2010;19(11–12):1738–1747. doi: 10.1111/j.1365-2702.2009.03115.x. [DOI] [PubMed] [Google Scholar]
- 40.Akincigil A, Munch S, Niemczyk KC. Predictors of Maternal Depression in the First Year Postpartum: Marital Status and Mediating Role of Relationship Quality. Social Work in Health Care. 2010;49(3):227–244. doi: 10.1080/00981380903213055. [DOI] [PubMed] [Google Scholar]
- 41.Davis L, Edwards H, Mohay H, Wollin J. The impact of very premature birth on the psychological health of mothers. Early Hum. Dev. 2003;73(1–2):61–70. doi: 10.1016/s0378-3782(03)00073-2. [DOI] [PubMed] [Google Scholar]