Abstract
Background:
To successfully prevent secondary health conditions (SHCs) and promote longevity after spinal cord injury (SCI), we must first understand the risk factors precipitating their occurrence and develop strategies to address these risk factors. Conceptual models may aid in identifying the nature of SHCs and guide research, clinical practice, and the development of prevention strategies.
Objective:
Our purpose is to review and refine an existing theoretical risk and prevention model (TRPM) as a means of classifying risk and protective factors for SHCs and mortality after SCI and for identifying points of intervention.
Methods:
We describe conceptual work within the field of SCI research and SHCs, including a description of the TRPM, a review of research using the TRPM, and conceptual enhancements to the TRPM based on previous research.
Conclusions:
The enhanced TRPM directs research to the timing and chronicity of the SHCs and their relationship with overall health and physiologic decline. Future research should identify differences in the nature of SHCs, the extent to which they relate to risk and protective factors, and the degree to which they may be prevented with appropriate research-based strategies.
Key words: health, longevity, mortality, risk, spinal cord injury, theoretical models
Spinal cord injury (SCI) is associated with a lifelong risk of secondary health conditions (SHCs) and results in diminished life expectancy. If we are to successfully prevent SHCs and promote longevity, we must first understand the risk factors precipitating their occurrence and develop strategies to address these risk factors. Conceptual models may aid in the development of prevention strategies by helping to identify the nature of SHCs and to guide research, clinical practice, and the development of prevention strategies.
Our purpose is to revisit a theoretical risk and prevention model (TRPM) we developed in 1996 as a means of classifying risk and protective factors for SHCs and mortality and for identifying points of intervention.1 To accomplish this, we describe conceptual work within the field, including a description of the TRPM. Our review of research using the TRPM and conceptual enhancements based on that research is discussed.
Recent Conceptual Developments
Two recent conceptual articles2,3 have helped define SHCs, one of which is specific to SCI. Jensen et al2 provided the following definition of SHCs: “physical or psychological health conditions for which the development or course is influenced directly or indirectly by the presence of a disability or impairment.”(pp374-375) They identified 3 necessary parameters: (1) temporality – causal agent (disability) precedes the development or worsening of the condition; (2) biological gradient – potency of the causal agent (greater disability or longer disability duration) leads to an increase in the frequency or severity of the condition; and (3) plausibility/coherence – a causal relationship is biologically or psychologically reasonable given the state of our scientific knowledge. The authors provide a general schematic, emphasizing the role of aging on secondary conditions, and they list a wide range of conditions that have been investigated as SHCs, including neurogenic bladder, neurogenic bowel, chronic pain, cardiovascular disease, spasticity, pressure ulcers, and urinary tract infection. No attempt is made to differentiate classes of SHCs based on common features.
A second conceptual scheme was developed by Rimmer et al3 who provide a decision tree for determining what constitutes SHCs after a disabling condition. To be considered an SHC, it must occur after disability onset (not be pre-existing), not be a direct result of the onset of the condition, be more prevalent after the disability, not be a consequence of treatment of the disability per se, and be a health or medical condition rather than a risk factor (poor hygiene or social isolation are provided as examples). The authors further provide examples of SHCs and a predictive model. The most basic predictors are nonmodifiable antecedents including socio-demographic factors, the nature of disability, pre-existing conditions, and associated conditions. They then propose modifiable risk factors, breaking them down into personal and environmental factors. Secondary conditions are the next stage of the model and consider the onset, progression, and the severity of the conditions. The relationship of SHCs with activities and participation is delineated, although mortality is not defined within the model.
Theoretical Risk and Prevention Model
In 1996, we developed the TRPM that was designed to categorize risk and protective factors for SHCs and mortality, establish theoretical links to describe the interrelationship of classes of factors and their relative importance with SHCs and mortality, and provide a model with explicit points of intervention.1 Unlike primary SCI complications, including sensory and motor impairment, SHCs are typically preventable to varying degrees, depending on the nature of the SHCs and the extent to which their occurrence is mediated by risk and protective factors that may become the focus of prevention strategies. Therefore, according to the model, SHCs are indirectly the result of the SCI. For example, pressure ulcers are partially the result of the loss of sensation and the ability to feel discomfort or pain, as well as the inability to move to shift weight and promote pressure relief. However, they are also related to a number of behavioral risk factors and are highly preventable with appropriate health maintenance behaviors and proper equipment.4,5 Preventing pressure ulcers is important due to their economic cost and their effect on overall health, quality of life, and longevity.6-10
As a first step in developing the TRPM, we sought to identify those factors that would explain variations in mortality above and beyond the known relationships of demographic and injury characteristics. We identified 3 additional levels of predictive variables and ordered them as to their relative importance with mortality. These included (1) psychological and socio-environmental factors, (2) behavioral factors, and (3) health factors and SHCs. Psychological and socio-environmental factors represent 2 different classes of predictors but were given relatively equal importance within the model. The fourth and most basic set of predictors relates to demographic and injury characteristics. We were guided by the following theoretical assumptions:
-
1.
Each set of factors was significantly predictive of mortality above and beyond the effects of demographic and injury characteristics. Therefore, considered by themselves with only demographic and injury characteristics as statistical controls, we would be able to identify at least one type of predictor from each set of factors that would be significantly related to mortality.
-
2.
The sets of factors would not be equally important, with some factors more proximal with mortality. We classified the model into 5 levels, with demographic and injury characteristics at the most basic level serving primarily as statistical controls due to their direct relationships with mortality. The next 3 levels, in order of importance, were psychological and environmental factors (2 sets of factors deemed to be of relatively equal importance), behavioral factors, and health factors. Mortality comprises the fifth layer of the model.
-
3.
The relationship between the factors with mortality is causal. Therefore, a series of mediational relationships was proposed to exist between the various levels in the model, with the more proximal factors mediating the relationships of more distal factors with mortality. For instance, health factors would mediate the observed relationships between behavioral characteristics and mortality, such that any observed relationships between behaviors and mortality would disappear after accounting for health factors. Similarly, the relationship of psychological and environmental factors with SHCs would be mediated by health behaviors, such that the effects of psychological and environmental variables would disappear after accounting for health behaviors.
The model was developed to both predict SHCs and mortality and to identify links in the causal chain that could become the focus of interventions. Therefore, SHCs are themselves treated as a predictor of mortality. However, the same model may be used to predict SHCs from the combination of the other sets of predictors, with the same assumptions regarding the importance of the predictive factors (ie, behavioral factors mediate the relationships between psychological and socio-environmental factors with SHCs).
Interventions can occur at multiple levels, depending on the nature of the predictive factor and where it appears within the causal chain. Interventions implemented earlier within the causal chain would have obvious benefits and be much more preventive in their focus. For instance, economic resources and access to health care are socio-environmental factors that are related to race/ethnicity.11-13 Disparities in economic resources are associated with differences in health behaviors that may in turn lead to a greater risk of morbidity (SHC) and mortality.14–17 The role of a potential intervention would be to create equal opportunities to improve economic status. If a pattern of differential access to economic opportunity is established, then an intervention may be directed further in the causal chain to prevent the differences in economic resources from resulting in high-risk behaviors and decreased protective behaviors. Once the behavioral pattern develops, then interventions may attempt to avert behavioral patterns from resulting in SHCs. Finally, once developed, only treatment can be applied to resolve the SHCs and prevent them from leading to mortality. The TRPM directs professionals at multiple levels and from multiple disciplines in the development of intervention strategies, with the goal of implementing strategies as early in the causal chain as possible.
Research Using the TRPM
Since the development of the TRPM, we have conducted a line of research by selecting factors from the model and applying them to this investigation of SHCs and mortality after SCI.18 Other research has classified risk and protective factors for mortality using the structure of the TRPM to guide the analysis and interpretation of the findings. In total, this research has supported the fundamental theoretical assumptions of the model, with some qualifications, and has led to the development of refined and expanded models. We review each of the assumptions from the TRPM in the following paragraphs, followed by a summary of conceptual enhancements.
In 1997–1998, we implemented a prospective cohort study designed to measure factors from each component of the TRPM and test its assumptions. The first stage of the study included 1,386 participants with traumatic SCI, all of whom completed an instrument package sent by mail, with an overall response rate of 72%.6 Approximately 10 years after the collection of the initial data, we initiated a follow-up study (stage 2) with an expanded instrument package allowing for greater detail of assessment of each set of factors from the TRPM, with a particular emphasis on socio-environmental factors including access to care. Of the initial participants, 863 responded, which represents 81.6% of those who were known to be survivors (there were 312 deceased cases). In addition, a new cohort of 1,686 participants was identified, and the same instrument package was collected from these participants. Additional research will be conducted as a follow-up to selected outcomes within this study.19
Behavioral predictors of SHCs
As outlined in the original work,1 from a conceptual standpoint, risk and protective behaviors serve as distinct intersecting dimensions. Therefore, it is possible for an individual to fall within 1 of 4 quadrants based on their status on risk and protective behaviors: (1) high protective, low risk; (2) high protective, high risk; (3) low protective, low risk; (4) low protective, high risk.
Several behavioral characteristics have also been related to specific conditions. Because SCI often results from patterns of risk behaviors and the etiology of SCI is related to specific demographic patterns,20-22 we identified risk factors of subsequent injuries resulting in need for treatment in an outpatient or emergency room setting. Psychotropic prescription medication use was associated with greater risk of subsequent injury.23 Recurrent pressure ulcers were also associated with a pattern of risk behaviors including cigarette smoking and use of prescription medication for sleep. Several protective factors were identified, including employment, healthy lifestyle, healthy diet, and exercise; these were associated with decreased risk of recurrent pressure ulcers.24 Data from this stage were also used to look at the factor structure of behaviors, and a 7-factor solution was found: prescription medications, alcohol use, health nutrition, unhealthy nutrition, smoking, fitness, and SCI-specific activities.25
Studies of mortality
The primary analyses to test the assumptions from the TRPM used mortality as the outcome. A series of publications address the relationship of each set of predictive factors (SHCs, behavioral, psychological, and socio-environmental) with mortality after controlling for demographic and injury characteristics. In each of these publications, individual sets of predictive factors were assessed one at a time, in relation to mortality, while controlling for the demographic and injury factors.7,26-28 An overall model was then developed by entering the demographic and injury characteristics into the model followed by all of the predictors from the individual set of factors.6
These individual analyses supported the first assumption from the TRPM that each set of factors was significantly predictive of mortality above and beyond the effects of demographic and injury characteristics. The first analysis focused on the relationship of health outcomes and mortality; five health outcomes were related to mortality: probable major depression, surgeries to repair pressure ulcers, fractures and/or amputations, symptoms of infection, and days hospitalized in the past year.7 Several types of health behaviors were significantly related to mortality, including smoking, binge drinking, psychotropic prescription medication use (pain, spasticity, sleep, depression), and time spent out of bed.28 In an analysis of psychological characteristics,26 3 psychological factors were retained in the final model, including 2 personality scales (Impulsive Sensation Seeking, Neuroticism-Anxiety and the Purpose in Life Scale).29 A fourth analysis focused on the relationship of social support and socio-economic factors to mortality, and the model revealed 2 significant predictors of mortality: low income and general social support. In summary, each analysis clearly identified at least 1 characteristic from each of the 4 sets of risk and protective factors in relation to mortality, substantiating the importance of each set of factors when investigated without consideration of other types of factors from the TRPM except the most basic level of the model (ie, demographic and injury characteristics).
Simultaneous analysis of all sets of risk and protective factors from the TRPM in relation to mortality provided additional evidence for the second assumption that sets of factors would not be equally predictive of mortality, with some sets of factors more proximal to mortality. This assumption relates to the basic structure of the TRPM, with health factors being most proximal to mortality, followed by behavioral factors, and then psychological and socio-environmental factors (both of which receive equal weight). When considering all factors simultaneously, 4 health factors (days in the hospital, fracture/amputation, number of surgeries to repair pressure ulcers, probable major depression), 2 behavioral factors (prescription medication use, binge drinking), and 1 socio-environmental factor (income) were significantly related to mortality. These findings were consistent with the structure of the model as psychological factors, the most distal to mortality of all nondemographic and noninjury factors, were not predictive of mortality after considering other factors. Socio-environmental factors were also not highly significant; only income remained in the equation. These factors are treated with equal importance within the original TRPM. In contrast, the finding that 2 behavioral factors remained in the model was significant, as they are conceptually more important than psychological and socio-environmental factors. As expected, the majority of predictors were health factors. With each set of predictors included in the model, the pseudo-R increased; .121 for the base model, .136 after inclusion of psychological and socio-environmental factors, .161 after inclusion of behavioral factors, and .179 after inclusion of the health factors.
The third assumption of the TRPM is similar to the second assumption in that it places differential importance on different sets of predictive factors, but it makes more stringent assumptions as it suggests the relationship between the factors with mortality is causal, such that a series of mediational relationships exist between the various levels in the model. Although the findings just noted regarding the importance of each set of factors indeed suggests that mediational relationships exist between the sets of factors, at least with mortality, the mediation has not been complete. In other words, if mediation was complete and the research fully accounted for the predictive factors for mortality, then we would anticipate that behavioral and socio-environmental factors would disappear altogether. The absence of complete mediation does not contraindicate a causal effect, nor can the causal effect be demonstrated completely. However, the evidence does suggest that the various factors may represent the differential importance that could be related to a causal series of events.
The major outlier within the research model is that income, a socio-environmental factor, remained important after the addition of all other factors. We sought to further investigate the relationship of income with mortality, as, conceptually, income cannot have a direct effect on mortality in the causal sense (ie, you cannot buy extra years of life). Therefore, it becomes important to identify factors that intervene or mediate the relationship of income with mortality. We conducted further analysis using the same data and structuring the analysis similar to that conducted in the general population. This analysis included self-rated health and severity of the injury as the 2 health predictors but included an expanded set of behaviors and socio-environmental predictors. Income remained significant, and its effect appeared to be more powerful than that observed within the general population. These findings clearly suggest the importance of economic factors in relation to mortality and are consistent with the theoretical stance that socio-economic status (SES) is a fundamental cause of disease within the general population.
Additional research has been conducted with data from the SCI Model Systems (SCIMS) to test various assumptions from the TRPM. The first study structured risk factors in accordance with the TRPM using data that was fit post hoc from the SCIMS. This type of secondary analysis of data is much less powerful than the prospective cohort design employed within the aforementioned longitudinal study, but it uses the strength of the SCIMS data – the number of participants available for study. The preliminary analyses conducted in this manner supported the overall TRPM in that at least 1 of the factors from each set of predictors was significantly related to mortality. Subsequent analyses isolated the effects of income on mortality, again finding highly significant effects. Consideration of additional socio-economic parameters, specifically employment status, substantiated these findings.
It is important to note that the absence of complete mediation may relate to different underlying relationships between the factors and mortality than initially proposed or to limitations in the data itself in terms of the scope of factors under study. In other words, the inclusion of additional factors could account for some relationships that currently do not appear to be fully mediated by other risk factors. Additional studies are needed to identify new mediators of both SHCs and mortality.
Model Refinements
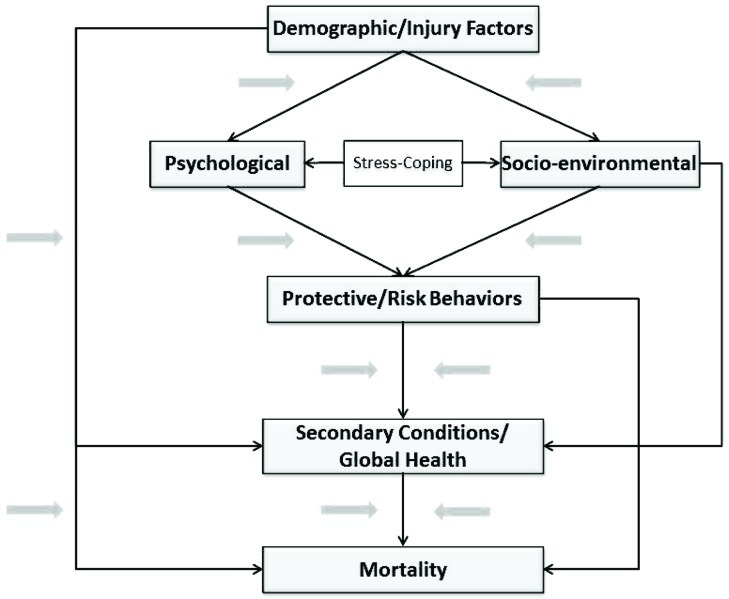
Modifications and enhancements have been made to the TRPM to accommodate research findings. Figure 1 displays the TRPM with the original model highlighted and shows enhancements that were added to the model. The enhancements account for the findings that suggest mediation is not complete. Therefore, direct paths between behaviors and mortality and SES and health outcomes have been added to the model. Krause et al published an expansion to the model introducing the idea of types of SES factors that could help explain the relationship of SES with SHCs and mortality. Tangible resources represent resources that could be purchased with increased SES, such as appropriate attendant care or a wheelchair, whereas intangible resources represent stress related to inadequate SES. Additionally, stress-coping, how an individual reacts to their environment, was added linking psychological and socio-environmental factors.37 The health behaviors and SHCs are broken down into factors based on previous work. The factor analysis of health behaviors was described previously. In assessing the factor structure of health outcomes, Krause et al37 found a 6-factor solution consisting of global health, treatment, pressure ulcers, symptoms of infections, orthopedic complications, and subsequent injuries.
Figure 1.
Theoretical risk and prevention model.
Synthesis of Existing Work
The TRPM was designed to guide research on risk and protective factors for SHCs, rather than define SHCs themselves. Whereas Jensen et al2 suggested SHCs result “directly or indirectly by the presence of a disability or impairment,” within the TRPM, SHCs are indirectly related to the SCI (as outlined earlier). This is more similar to the decision tree provided by Rimmer et al, who exclude conditions that are a direct result of the onset of the condition. Therefore, conditions such as neurogenic bladder and neurogenic bowel are not considered SHCs within the TRPM or by Rimmer et al,3 but they are considered SHCs according to Jensen’s scheme.2 Rimmer et al3 classifies such conditions as nonmodifiable antecedents.
Jensen et al2 also suggest SHCs are related to a biological gradient, such as greater disability or longer disability duration. Some, but not all, SHCs follow this pattern. Clearly, some conditions are progressive and may develop over time after SCI onset. For instance, orthopedic complications, such as contractures or curvature of the spine, are related to years post injury.38 Other conditions, such as pressure ulcers, may occur intermittently at different times after SCI onset. Skin integrity may decline with aging, an underlying condition that may elevate risk of pressure ulcers. Other complications related to behavioral factors, such as injuries, may actually occur more frequently at younger ages.23
Rimmer et al3 provide both the decision tree for identifying what constitutes an SHC, as well as a predictive model. As with the TRPM, the most basic factors within the model are nonmodifiable antecedents (described in the TRPM as demographic and injury characteristics). Rimmer et al3 include pre-existing and associated conditions within this category, as well as socio-demographic factors and the nature of disability. Additional similarities with the TRPM include a breakdown of predictive factors into personal and environmental characteristics, followed by SHCs. The TRPM essentially breaks personal characteristics down into psychological and behavioral characteristics, with behavioral characteristics more proximal and therefore more efficient predictors of SHCs (ie, later in the causal chain). The models then diverge in terms of focus; Rimmer et al3 focus more closely on participation and quality of life, whereas the TRPM is primarily concerned with the next stage in the model – mortality. It is noteworthy that participation is viewed from the behavioral perspective in the TRPM and quality of life is treated as an associated outcome, as defined in an elaboration of the original model.36 With the exception of the distinction between conditions directly resulting from the injury (eg, neurogenic bladder, neurogenic bowel), none of the models attempt to differentiate classes of SHCs according to their antecedents.
Implications for the Future
The conceptual and empirical work summarized in this article reflects the ongoing effort to better describe, classify, predict, and prevent SHCs after SCI. Given the focus on prevention, future research should identify the antecedent conditions for SHCs, as well as more general indicators of health and health decline. Understanding the timing of SHCs in relation to SCI onset will allow persons planning preventive efforts to target the most appropriate interventions at critical points within their development.
Conditions whose onset is immediately after SCI onset and whose course is stable over time represent the more direct consequences of the SCI and may be difficult to prevent. Other conditions, such as orthopedic complications, may take some time to develop after SCI and have a progressive course, which requires strategies to limit their progression. Yet others may have a more variable onset with multiple new episodes over time. For example, pressure ulcers have been found to occur in a portion of individuals only shortly after injury, whereas they occur first years after SCI onset for others and have variable patterns of intermittent reoccurrence or rather continuous occurrence in yet other individuals.24
In addition to preventing specific SHCs, it is important to evaluate changes in general health indicators that may result from, or be indicative of, health status and health decline. Previous factor analytic work of health outcomes identified 2 types of global health indicators, one of which represented a treatment factor (nonroutine physician visits and hospitalizations) and the other of which represented global health ratings, days in poor health, and depressive symptomatology. 37 Clinical research may better detail the role of biomarkers in health change and decline, as acknowledged in the previous model enhancement.39
For instance, the allostatic load model, a biologic theory of stress, proposes that the stress response is influenced by a number of factors and that the accumulation of allostatic load can have adverse effects systemwide, contributing to morbidity and mortality.40-43 The cumulative effects of the elevated stress levels inherent to SCI and the social determinants of health related to poor economics may lead to greater allostatic load, which may be a mediator of mortality. Similarly, telomeres are protective caps at the ends of eukaryotic chromosomes made up by repeating DNA sequences (TTAGGG), and telomerase is the enzyme that adds the DNA sequence to the ends of the chromosomes. Telomere length is a marker of biological aging, influenced by both genetics and oxidative stress. Shortened telomeres are associated with morbidity,45 mortality,46 and disability in older populations.47 The conceptual link between telomerase and telomere length with SCI is similar to that with allostatic load in that the stressors associated with SCI may ultimately lead to significant biologic change, increasing the risk of mortality. These are topics for future research.
Future research should be directed at identifying differences in the nature of SHCs and the extent to which they can be related to risk and protective factors from the model and the degree to which they may be prevented with appropriate research-based strategies. Establishing the connections between SHCs and biomarkers as indicators of physiologic decline will further determine the cumulative effects of SHCs on overall health status. Identifying specific risk and protective factors for different SHCs will allow for more targeted interventions.
Ultimately, the value of the TRPM will depend on how successfully it is implemented to guide research and intervention strategies to reduce SHCs, improve health, and enhance longevity after serious traumatic injury.
Acknowledgments
The contents of this presentation were developed under grants from the Department of Education (NIDRR H133B090005) and the National Institutes of Health (1R01 NS 48117). However, those contents do not necessarily represent the policy of the Department of Education or NIH, and endorsement by the Federal Government should not be assumed.
References
- 1. Krause JS. Secondary conditions and spinal cord injury: a model for prediction and prevention. Top Spinal Cord Inj Rehabil. 1996;2(2):217–227. [Google Scholar]
- 2. Jensen MP, Molton IR, Groah SL, et al. Secondary health conditions in individuals aging with SCI: terminology, concepts and analytic approaches. Spinal Cord. 2012;50(5):373–378. [DOI] [PubMed] [Google Scholar]
- 3. Rimmer JH, Chen MD, Hsieh K. A conceptual model for identifying, preventing, and managing secondary conditions in people with disabilities. Phys Ther. 2011;91(12):1728–1739. [DOI] [PubMed] [Google Scholar]
- 4. Krause JS, Vines CL, Farley TL, Sniezek J, Coker J. An exploratory study of pressure ulcers after spinal cord injury: relationship to protective behaviors and risk factors. Arch Phys Med Rehabil. 2001;82(1):107–113. [DOI] [PubMed] [Google Scholar]
- 5. Gelis A, Dupeyron A, Legros P, Benaim C, Pelissier J, Fattal C. Pressure ulcer risk factors in persons with spinal cord injury part 2: the chronic stage. Spinal Cord. 2009;47(9):651–661. [DOI] [PubMed] [Google Scholar]
- 6. Krause JS, Zhai Y, Saunders LL, Carter RE. Risk of mortality after spinal cord injury: an 8-year prospective study. Arch Phys Med Rehabil. 2009;90(10):1708–1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Krause JS, Carter RE, Pickelsimer E, Wilson D. A prospective study of health and risk of mortality after spinal cord injury. Arch Phys Med Rehabil. 2008;89(8):1482–1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Thein HH, Gomes T, Krahn MD, Wodchis WP. Health status utilities and the impact of pressure ulcers in long-term care residents in Ontario. Qual Life Res. 2010;19(1):81–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Paker N, Soy D, Kesiktas N, et al. Reasons for rehospitalization in patients with spinal cord injury: 5 years’ experience. Int J Rehabil Res. 2006;29(1):71–76. [DOI] [PubMed] [Google Scholar]
- 10. Javitz HS, Ward MM, Martens L. Major costs associated with pressure sores. J Wound Care. 1998;7(6):286–290. [DOI] [PubMed] [Google Scholar]
- 11. Hayward MD, Crimmins EM, Miles TP, Yu Y. The significance of socioeconomic status in explaining the racial gap in chronic health conditions. Amer Sociol Rev. 2000;65(6):910–930. [Google Scholar]
- 12. House JS, Williams DR. Understanding and reducing socioeconomic and racial/ethnic disparities in health. In: Smedley BD, Syme SL, eds. Promoting Health: Intervention Strategies From Social and Behavioral Research. Washington, DC: National Academy Press; 2000:81–125. [PubMed] [Google Scholar]
- 13. Fiscella K, Franks P, Gold MR, Clancy CM. Inequality in quality: addressing socioeconomic, racial, and ethnic disparities in health care. JAMA. 2000;283(19):2579–2584. [DOI] [PubMed] [Google Scholar]
- 14. Lantz PM, Golberstein E, House JS, Morenoff J. Socioeconomic and behavioral risk factors for mortality in a national 19-year prospective study of U.S. adults. Soc Sci Med. 2010;70(10):1558–1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lantz PM, Lynch JW, House JS, et al. Socioeconomic disparities in health change in a longitudinal study of US adults: the role of health-risk behaviors. Soc Sci Med. 2001;53:29–40. [DOI] [PubMed] [Google Scholar]
- 16. Stringhini S, Dugravot A, Shipley M, et al. Health behaviours, socioeconomic status, and mortality: further analyses of the British Whitehall II and the French GAZEL prospective cohorts. PLoS Med. 2011;8(2):e1000419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Stringhini S, Sabia S, Shipley M, et al. Association of socioeconomic position with health behaviors and mortality. JAMA. 2010;303(12):1159–1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Krause JS, Saunders LL. Risk and protective factors for secondary conditions: a 15-year longitudinal study. Top Spinal Cord Inj Rehabil. 2010;16(2):22–29. [Google Scholar]
- 19. Saunders LL, Krause JS, Selassie AW. Association of health services with secondary conditions: use of a population-based cohort of persons with SCI in South Carolina. Top Spinal Cord Inj Rehabil. 2010;16(2):30–39. [Google Scholar]
- 20. Jackson AB, Dijkers M, Devivo MJ, Poczatek RB. A demographic profile of new traumatic spinal cord injuries: change and stability over 30 years. Arch Phys Med Rehabil. 2004;85(11):1740–1748. [DOI] [PubMed] [Google Scholar]
- 21. Ho CH, Wuermser, Priebe MM, Chiodo AE, Scelza WM, Kirshblum SC. Spinal cord injury medicine. 1. Epidemiology and classification. Arch Phys Med Rehabil. 2007;88(3 Suppl 1):S49–54. [DOI] [PubMed] [Google Scholar]
- 22. Chen Y, Tang Y, Vogel L, DeVivo MJ. Causes of spinal cord injury. Top Spinal Cord Inj Rehabil. 2013;19(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Krause JS. Factors associated with risk for subsequent injuries after the onset of traumatic spinal cord injury. Arch Phys Med Rehabil. 2004;85:1503–1508. [DOI] [PubMed] [Google Scholar]
- 24. Krause JS, Broderick L. Patterns of recurrent pressure ulcers after spinal cord injury: identification of risk and protective factors 5 or more years after onset. Arch Phys Med Rehabil. 2004;85:1257–1264. [DOI] [PubMed] [Google Scholar]
- 25. Krause JS, McArdle JJ, Pickelsimer E, Reed KS. A latent variable structural path model of health behaviors after spinal cord injury. J Spinal Cord Med. 2009;32:162–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Krause JS, Carter R, Zhai Y, Reed K. Psychologic factors and risk of mortality after spinal cord injury. Arch Phys Med Rehabil. 2009;90(4):628–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Krause JS, Carter RE. Risk of mortality after spinal cord injury: relationship with social support, education, and income. Spinal Cord. 2009;47(8):592–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Krause JS, Carter RE, Pickelsimer E. Behavioral risk factors of mortality after spinal cord injury. Arch Phys Med Rehabil. 2009;90(1):95–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Crumbaugh JC, Maholick LT. Manual of Instructions for the Purpose in Life Test. Saratoga, CA: Institute of Logotherapy;1981. [Google Scholar]
- 30. Krause JS, Saunders LL. Socioeconomic and behavioral risk factors for mortality: Do risk factors observed after spinal cord injury parallel those from the general USA population? Spinal Cord. 2012;50(8):609–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995;35(extra issue):80–94. [PubMed] [Google Scholar]
- 32. Krause JS, DeVivo MJ, Jackson AB. Health status, community integration, and economic risk factors for mortality after spinal cord injury. Arch Phys Med Rehabil. 2004;85(11):1764–1773. [DOI] [PubMed] [Google Scholar]
- 33. Krause JS, Saunders LL, DeVivo MJ. Income and risk of mortality after spinal cord injury. Arch Phys Med Rehabil. 2011;92(3):339–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Krause JS, Saunders LL, Acuna J. Gainful employment and risk of mortality after spinal cord injury: effects beyond that of demographic, injury and socioeconomic factors. Spinal Cord. 2012;50(10):784–788. [DOI] [PubMed] [Google Scholar]
- 35. Krause JS, Saunders LL. Life expectancy estimates in the life care plan: accounting for economic factors. J Life Care Plan. 2010;9(2):15–28. [PMC free article] [PubMed] [Google Scholar]
- 36. Krause JS, Newman S. Clinical outcomes after spinal cord injury. In: Lajtha A, ed. Handbook of Neurochemistry and Molecular Neurobiology: Central Nervous System Injuries and Disorders (Vol 24, 3rd ed). New York: Springer; 2009:615–632. [Google Scholar]
- 37. Krause JS, Reed KS, McArdle JJ. A structural analysis of health outcomes after spinal cord injury. J Spinal Cord Med. 2010;33(1):22–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Krause JS. Intercorrelations between secondary conditions and life adjustment among people with spinal cord injuries. SCI Psychosocial Process. 1998;11:3–7. [Google Scholar]
- 39. Krause JS, Newman S, Brotherton S. Clinical considerations in translational research with chronic spinal cord injury: intervention readiness and intervention impact. In: Lajtha A, ed. Handbook of Neurochemistry and Molecular Neurobiology: Central Nervous System Injuries and Disorders (Vol 24, 3rd ed). New York: Springer; 2009:563–580. [Google Scholar]
- 40. McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338(3):171–179. [DOI] [PubMed] [Google Scholar]
- 41. Seeman TE, Singer BH, Rowe JW, Horwitz RI, McEwen BS. Price of adaptation--allostatic load and its health consequences. MacArthur studies of successful aging. Arch Intern Med. 1997;157(19):2259–2268. [PubMed] [Google Scholar]
- 42. Seeman TE, McEwen BS, Rowe JW, Singer BH. Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proc Natl Acad Sci USA. 2001;98(8):4770–4775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Karlamangla AS, Singer BH, Seeman TE. Reduction in allostatic load in older adults is associated with lower all-cause mortality risk: MacArthur studies of successful aging. Psychosom Med. 2006;68(3):500–507. [DOI] [PubMed] [Google Scholar]
- 44. Blackburn EH. Structure and function of telomeres. Nature. 1991;350(6319):569–573. [DOI] [PubMed] [Google Scholar]
- 45. Calado RT, Young NS. Telomere diseases. N Engl J Med. 2009;361(24):2353–2365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Cawthon RM, Smith KR, O’Brien E, Sivatchenko A, Kerber RA. Association between telomere length in blood and mortality in people aged 60 years or older. Lancet. 2003;361(9355):393–395. [DOI] [PubMed] [Google Scholar]
- 47. Risques RA, Arbeev KG, Yashin AI, et al. Leukocyte telomere length is associated with disability in older U.S. population. J Am Geriatr Soc. 2010;58(7):1289–1298. [DOI] [PMC free article] [PubMed] [Google Scholar]