Abstract
The aim of this study was to develop a spray dried submicrometer powder formulation suitable for the excipient enhanced growth (EEG) application. Combination particles were prepared using the Buchi Nano spray dryer B-90. A number of spray drying and formulation variables were investigated with the aims of producing dry powder formulations that were readily dispersed upon aerosolization and maximizing the fraction of submicrometer particles. Albuterol sulfate, mannitol, L-leucine, and poloxamer 188 were selected as a model drug, hygroscopic excipient, dispersibility enhancer and surfactant, respectively. Formulations were assessed by scanning electron microscopy and aerosol performance following aerosolization using an Aerolizer® dry powder inhaler (DPI). In vitro drug deposition was studied using a realistic mouth-throat (MT) model. Based on the in vitro aerosolization results, the best performing submicrometer powder formulation consisted of albuterol sulfate, mannitol, L-leucine and poloxamer 188 in a ratio of 30:48:20:2, containing 0.5% solids in a water:ethanol (80:20% v/v) solution which was spray dried at 70 °C. The submicrometer particle fraction (FPF1μm/ED) of this final formulation was 28.3% with more than 80% of the capsule contents being emitted during aerosolization. This formulation also showed 4.1% MT deposition. The developed combination formulation delivered a powder aerosol developed for the EEG application with high dispersion efficiency and low MT deposition from a convenient DPI device platform.
Keywords: excipient enhanced growth (EEG), spray drying, vibrating mesh, hygroscopic aerosol, dry powder inhaler
1. Introduction
There has been extensive interest in the use of respiratory drug delivery technologies utilising dry powder inhaler (DPI) formulations for the treatment of local and systemic disorders by virtue of their propellant-free nature, high patient compliance and improved formulation stability (Ashurst et al., 2000; Prime et al., 1997; Timsina et al., 1994). While much effort has been expended in designing novel DPIs and formulations to achieve high drug deposition in central and peripheral regions of the lung, such novel inhaled products continue to exhibit suboptimum drug delivery performance due to high mouth-throat (MT) drug deposition (Geller et al., 2011; Newman et al., 2000). It has been reported that DPIs with typical aerodynamic diameters of 3 to 6 μm deposit in the MT region about 40–70% of the dose due to inertial impaction (Borgstrom et al., 1994; Brand et al., 2007; Geller et al., 2011; Newman et al., 2000).
Inhaled nanoparticle delivery systems have high potential to significantly reduce extrathoracic depositional drug losses since particles in the range of 40–900 nm are known to achieve near zero deposition in the mouth-throat (MT) region (Cheng, 2003; Xi and Longest, 2008). However, the direct use of nanoparticles for lung delivery is limited since individual nanoparticles do not possess sufficient inertia to deposit efficiently in the lung, which results in the exhalation of a majority of the inhaled dose (Jaques and Kim, 2000). In addition, cohesion and aggregation of nanoparticles makes them difficult to process into dry powder formulations. The complete dispersion of ultra-fine powders is difficult due to large inter-particle attractive forces (Geldart, 1973), namely Van der Waals, electrostatic and capillary forces, compared to typically weaker aerodynamic separating forces (Visser, 1989). Attempts to overcome these issues have led to most inhalation dry powder nanoparticle formulations being designed as micron-sized particles encapsulating nanoparticles or aggregated nanoparticles (Yang et al., 2008). However, as the nanoparticles are now presented as conventionally sized inhalation aerosols, most of the potential drug delivery advantages are negated and they have similar MT deposition losses (40–70% of the inhaled dose) as conventional inhaled products.
One solution proposed adopts a dynamic aerosol particle size approach rather than the conventional static particle size used for current DPIs. Excipient enhanced growth (EEG) is a newly proposed respiratory delivery strategy which delivers an inhaled submicrometer particle formulation to minimize MT depositional losses. The aerosol increases to micrometer size during inhalation in order to maximize lung retention (Hindle and Longest, 2012; Tian et al., 2011b). In initial studies of the EEG approach, combination drug and hygroscopic excipient dry powder particles were produced in the size range of 100–900 nm from aqueous aerosol spray generators (Respimat and the small particle aerosol generator (SPAG)). These aerosols were shown to minimize MT deposition during inhalation and then the natural humidity in the lungs causes the particles containing the hygroscopic excipient to accumulate water, increasing the size and weight of the particle. Increasing the aerodynamic particle size to 2–4 μm will then ensure near complete lung deposition. Longest and Hindle developed correlations for these spray aerosol generators based on an experimentally validated model to predict the size increase of initially submicrometer combination drug and hygroscopic excipient particles in the airways and demonstrated diameter growth ratios of up to 4.6 at excipient mass loadings of 50% and below (Tian et al., 2011b). Results reported by Longest et al. indicate less than 1% MT deposition using the EEG application in combination with the Respimat inhaler, which represents over an order of magnitude improvement in performance, based on in vitro experiments and CFD simulations (Longest et al., 2012a). The Respimat is a spray device that employs liquid-based formulations (Longest et al., 2012b).
The aim of this study is to design a dry powder formulation containing submicrometer combination drug and hygroscopic excipient particles that is suitable for the EEG application for respiratory drug delivery. Our previous work has employed liquid aerosol generation devices, such as the Respimat and the SPAG nebulizer (Hindle and Longest, 2012; Longest et al., 2012b). A DPI formulation option would add to the utility of the EEG concept. It is well known that the performance of a DPI is highly dependent on formulation and device design. Thus, in this study, we develop a novel submicrometer DPI formulation with improved aerodynamic properties. A number of spray drying and formulation variables will be varied to produce a carrier-free submicrometer dry powder formulation. Albuterol sulfate (AS) and mannitol (MN) were selected as a model drug and a hygroscopic excipient. To address the issue of dry powder dispersion, L-leucine, an essential branched chain amino acid that acts as a dispersion enhancing excipient, was incorporated into the formulations to promote deaggregation of the submicrometer particles (Raula et al., 2008; Raula et al., 2010). Finally, the utility of the developed powder as an EEG formulation will be assessed following aerosolization using an Aerolizer® into an in vitro airway model to determine its MT deposition.
2. Materials and Methods
2.1. Materials
Albuterol sulfate USP was purchased from Spectrum Chemical Co. (Gardena, CA). Pearlitol® PF-Mannitol was donated from Roquette Pharma (Lestrem, France). Poloxamer 188 (Leutrol F68) was donated from BASF Corporation (Florham Park, NJ). L-leucine and all other reagents were purchased from Sigma Chemical Co. (St. Louis, MO). Size 3 hydroxypropylmethyl cellulose (HPMC) capsules were donated from Capsugel (Peapack, NJ). The Salbulin powder formulation containing albuterol sulfate 100μg (Meda Pharmaceuticals, Bishops Stortford, UK) was obtained from a commercial pharmacy source. An Aerolizer™ (Novartis; Basel, Switzerland) was obtained from a commercial pharmacy source. Molykote®316 silicone release spray was purchased from Dow Corning Corporation (Midland, MI).
2.2. Preparation of EEG combination and drug only dry powder formulations
Combination drug-excipient dry powder formulations were prepared using a Büchi Nano spray dryer B-90 (Büchi Laboratory-Techniques, Flawil, Switzerland). AS, MN, L-leucine and poloxamer 188 were selected as model drug, hygroscopic excipient, dispersibility enhancer and surfactant, respectively. To produce powder formulations which were readily dispersed upon aerosolization with a large portion of submicrometer particles, the spray drying and formulation variables were investigated during the development studies as shown in Table 1. The variables were drying chamber length, spray mesh size, inlet drying temperature, % L-leucine content, % ethanol concentration in the spray drying vehicle, and % solids concentration. Each formulation contained 30%w/w AS and 2% w/w of poloxamer 188. The following conditions were used during spray drying: the drying airflow was 120 L/min, the liquid feed rate was set to 100%, and the spray nozzle was a vibrating mesh. As a control formulation, a drug only (D-AS) powder formulation was also prepared by spray drying using the conditions determined for the final developed combination formulation. The dried solid particles were collected from the electrostatic precipitator in the spray drier and stored in sealed capped amber vials. The vials containing powders were stored in a desiccator (approx RH <10%) at room temperature.
Table 1.
Spray drying and formulation variables used to produce combination particles for the EEG application
| Spray Drying Conditions | Spray Vehicle Composition | Formulation Excipients* | ||||||
|---|---|---|---|---|---|---|---|---|
| Experiment | Dryer length (cm) | Inlet temp. (°C) | Mesh size (μm) | Water (%, v/v) | Ethanol (%, v/v) | Solids conc. (%, w/v) | Mannitol (%, w/w) | Leucine (%, w/w) |
| 1 | 45 | 85 | 4 | 80 | 20 | 1 | 48 | 20 |
| 2 | 90 | 85 | 4 | 80 | 20 | 1 | 48 | 20 |
| 3 | 90 | 70 | 5.5 | 80 | 20 | 1 | 48 | 20 |
| 4 | 90 | 70 | 4 | 80 | 20 | 1 | 48 | 20 |
| 5 | 90 | 70 | 4 | 80 | 20 | 0.2 | 48 | 20 |
| 6 | 90 | 70 | 4 | 80 | 20 | 0.5 | 48 | 20 |
| 7 | 90 | 70 | 4 | 100 | 0 | 0.5 | 48 | 20 |
| 8 | 90 | 70 | 4 | 80 | 20 | 0.5 | 58 | 10 |
| 9 | 90 | 70 | 4 | 80 | 20 | 0.5 | 68 | 0 |
30 %w/v albuterol sulfate and 2 % w/v poloxamer were constant for each experiment
Albuterol sulfate drug content uniformity in the formulations was determined using a validated HPLC method (Section 2.8). Briefly, a solution of each sample was prepared by dissolving approximately 3 mg of powder, which was accurately weighed, in 10 mL of deionized water. For the combination particles, this solution was then injected directly into the HPLC for quantification. For the drug only particles, the solution was further diluted to produce an AS concentration of approximately 100 μg/mL.
2.3. Scanning electron microscopy (SEM)
The morphology of the powders was observed using an EVO 50 SEM (Carl Zeiss AG, Germany). Each sample was mounted separately onto SEM stubs using double-sided copper tape and then coated with gold using a sputter coater (Electron Microscopy Sciences, Hatfield, PA) for 2 minutes under vacuum at 0.2 mbar. The SEM was operated at high vacuum with accelerating voltage 15 kV and specimen working distance 8 mm.
2.4. Thermal analysis
Thermograms were measured using a differential scanning calorimetry (DSC), Model 7 (Perkin Elmer Inc., Waltham, MA). Dry nitrogen gas was used as the purge gas through the DSC cell at a flow rate of 20 mL/min. Samples (3 mg) were weighed into aluminum crimped pinhole pans. The mass of the empty sample pan was matched with that of the empty reference pan within ± 0.2 mg. Samples were heated at a rate of 10 °C/min from 30 to 250 °C. Thermogravimetric analysis (TGA) was conducted using a Pyris 1 system (Perkin Elmer Inc., Waltham, MA). Weight loss from 5 mg samples at a heating rate of 10 °C/min from 30 to 250 °C under nitrogen purge (40 mL/min) was recorded.
2.5. Particle size and powder density
Particle size distributions of the combination particles and the drug only particles were determined using a laser diffraction technique. This non-drug specific method assessed the particle geometric diameter based on volume fractions of the powders using a Spraytec® particle size analyzer equipped with an inhalation flow cell (Malvern Instruments, Ltd., Worcestershire, UK). The entire assembly operated in a closed system using the inhalation flow cell. Powders (approximately 2 mg) were filled into Size 3 HPMC capsules and loaded into an Aerolizer® DPI. An airflow rate of 80 L/min was drawn through the system to sample the powder from the Aerolizer® and deliver the powder to the measurement zone.
Skeletal density of the prepared powders was measured using an AccuPyc II 1340 gas pycnometer (Micrometritics Instrument Corporation, Norcross, GA) with a 1 cm3 volume capacity sample cup, and data was analyzed using V1.05 software.
Theoretical estimates of aerodynamic diameter (Dae) were derived from the Malvern determined volume median diameter (D50) and the skeletal density (ρ), according to Eq. 1 (Edwards et al., 1997).
| (1) |
2.6. Aerodynamic particle size characterization
A Next Generation Impactor (MSP Co., Shoreview, MN) was used to determine aerodynamic particle size characteristics of the drug in the combination particle formulations. A sample of each powder formulation (2 mg) was filled into size 3 HPMC capsules and placed into the Aerolizer® DPI prior to testing. The capsule was fired into a NGI through a pre-separator operating at an air flow rate of 80 L/min for 3 seconds under at ambient conditions (25 °C/45–55% RH). In order to assess the particle size distribution of the total dose of formulation, the USP induction port was omitted. The air flow rate of 80 L/min produced a pressure drop across the device of approximately 2 kPa. The flow rate was selected based upon the studies of Zanen et al., (Zanen et al., 1992), that showed 80 L/min provided good powder dispersion and would allow comparison of the developed powders under constant conditions. For each of the impactor experiments, the impactor collection stages and pre-separator were coated with Molykore®316 silicone spray to minimize particle re-entrainment and bounce. Albuterol sulfate remaining in the Aerolizer (including the capsule), deposited on the pre-separator, and on each impactor collections stages was determined by washing each item with 10 mL of deionized water to extract the drug for quantitative analysis. Collected samples were analyzed using a validated HPLC method (Section 2.8).
Drug emitted dose exiting the DPI was determined by subtracting the amount of AS remaining in the DPI from the initial mass of AS loaded. The initial mass loaded in the DPI was calculated from weight of combination formulation and the measured %AS content for each formulation. The drug fine particle fraction (FPF5μm/ED) and submicrometer particle fraction (FPF1μm/ED), defined as the total emitted dose of AS with aerodynamic diameters smaller than 5 μm and 1 μm, respectively, were calculated via interpolation from the cumulative mass versus the cutoff diameter of the respective stages of the NGI. Each measurement was repeated three times. The MMAD was determined at the 50th percentile on the % cumulative undersize (probability scale) versus logarithmic aerodynamic diameter plot.
2.7. EEG aerosol characterization in the realistic mouth-throat (MT) model
The in vitro MT deposition of AS emitted from the Aerolizer was determined in a realistic MT geometry (Figure 1) for the following formulations: the final developed submicrometer combination powder formulation (Expt 6), the micrometer size combination powder formulation (Expt 3), the submicrometer drug only formulation (D-AS), and a commercial albuterol sulfate dry powder formulation (Salbulin). The characteristic airway geometry consisted of a MT, details of which were previously described in the studies of Tian et al. (Tian et al., 2011a; Tian et al., 2011b) and Xi and Longest (Xi and Longest, 2007). A schematic diagram of experimental set up for the MT deposition study is shown in Figure 1 (Delvadia et al., 2012). The outlet of the MT model was connected to a low resistance glass fiber filter (Pulmoguard II, SDI Diagnostics, MA) capable of retaining all aerosolized drug that passed through the MT model. The filter was connected to a vacuum pump to draw a 4L of air across the setup. Airtight seals between the inhaler mouthpiece and the MT model were maintained in all cases. The internal surfaces of the MT model were coated with a silicone spray followed by solvent evaporation before each experiment. The dry powder aerosol was generated using the Aerolizer® DPI actuated using external ambient conditions (25 °C/45–55% RH). Each combination (2 mg; 27–28%w/w AS), drug only (2 mg; 93%w/w AS), and commercial (12.5 mg, 1.1%w/w AS) powder formulation was filled into size 3 HPMC capsules and placed into the Aerolizer® prior to test. The Aerolizer® was actuated using an air flow rate of 80 L/min for 3 seconds. Drug aerosol deposition in the device, MT and fiber filter were determined by washing each deposition site with 20–100 mL of deionized water. The collected samples were analyzed using a validated HPLC method (Section 2.8).
Figure 1.
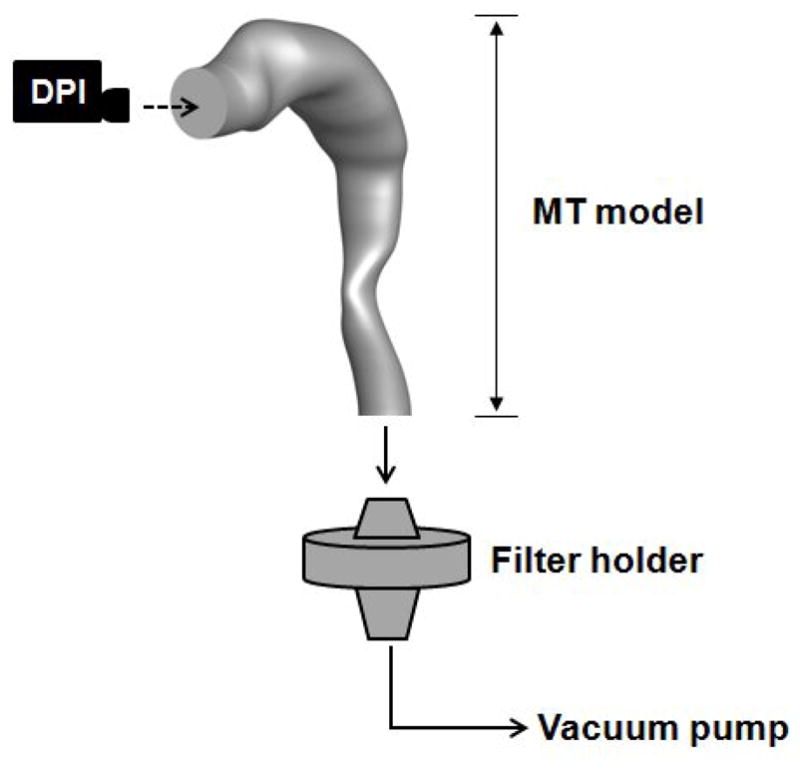
A schematic diagram of the experimental set up using a realistic MT geometry for evaluating the AS deposition in the model.
2.8. High-performance liquid chromatography (HPLC)
Albuterol sulfate quantification was performed using a validated HPLC method. A Waters 2690 separations module with a 2996 PDA detector (Waters Co., Milford, MA) was used. Chromatography was performed using a Restek Allure PFP 15 × 3.2 mm column (Bellefonte, PA). The mobile phase, consisting of methanol and ammonium formate buffer (20 mM, pH 3.4) in a ratio of 70:30, respectively, was eluted at a flow rate of 0.75 mL/min and the UV detector was set to a wavelength 276 nm. The column temperature was maintained at 25 °C, and the volume of each sample injected was 50 μL.
2.9. Statistical analysis
Data were expressed as the mean plus/minus standard deviation (SD). Statistical differences were studied by either analysis of variance or student’s t-test using Jump 9.0 software (SAS Institute Inc., Cary, NC). P values of less than 0.05 were considered as statistically significant. To identify the statistically significant differences between formulation and spray drying variables, the aerosolization properties of the combination powder formulations were analyzed using one-way analysis of variance (one-way ANOVA) followed by post hoc Dunnett’s test with a control. The significance level was 0.05.
3. Results
3.1. EEG dry powder formulation development
Combination drug-excipient powder formulations, consisting of an active pharmaceutical ingredient, a hygroscopic excipient, and a dispersibility enhancer, were prepared using a Buchi Nano spray dryer for the EEG application. As shown in Table 1, a total of 9 spray-dried powders were investigated with the aim of developing a powder formulation with the highest emitted dose and fine particle fraction. This was achieved by varying the spray drying and formulation parameters as shown in Table 1 to maximize the fraction of submicrometer particles in the DPI aerosol while maintaining a high emitted aerosol drug dose. Tables 2 and 3 show that AS content was very close to the nominal value of 30% w/w for all cases.
Table 2.
Effect of dryer length and mesh size on the aerosolization characteristics of AS in spray dried combination particles (values are mean (SD), n ≥ 3).
| Experiment | AS content (%) | ED (%) | MMAD (μm) | FPF5μm/ED (%) | FPF1μm/ED (%) |
|---|---|---|---|---|---|
| Effect of Dryer Length | |||||
| 1 (45cm) | 29.7 (0.7) | 82.1 (2.6)* | 3.4 (0.2)* | 66.2 (5.3)* | 2.8 (0.6)* |
| 2 (90 cm) | 27.8 (1.5) | 78.3 (0.8)* | 2.1 (0.1)* | 91.5 (2.4)* | 10.4 (2.2)* |
| Effect of Mesh Size | |||||
| 3 (5.5μm) | 29.0 (0.1) | 65.2 (1.2)** | 3.3 (0.0)** | 71.6 (0.8)** | 4.7 (0.7)** |
| 4 (4.0 μm) | 27.9 (0.6) | 76.9 (0.2)** | 1.8 (0.0)** | 94.4 (0.5)** | 14.5 (1.7)** |
Statistically significant effects on process variables were:
Length of drying chamber; ED, MMAD, FPF5μm/ED and FPF1μm/ED (Expt 1 vs Expt 2): t-test: P < 0.05
Nozzle mesh size; ED, MMAD, FPF5μm/ED and FPF1μm/ED (Expt 3 vs Expt 4): t-test: P < 0.05
Table 3.
Effect of % solids concentration and % ethanol concentration on the aerosolization characteristics of AS in spray dried combination particles (values are mean (SD), n ≥ 3).
| Experiment | AS content (%) | ED (%) | MMAD (μm) | FPF5μm/ED (%) | FPF1μm/ED (%) |
|---|---|---|---|---|---|
| Effect of % Solid Concentration | |||||
| 4 (1 %) | 27.9 (0.6) | 76.9 (0.2)# | 1.8 (0.0)# | 94.4 (0.5)# | 14.5 (1.7)# |
| 5 (0.2 %) | 27.4 (0.2) | 84.2 (0.6)# | 1.9 (0.3)# | 81.4 (7.4)# | 17.2 (6.0)# |
| 6 (0.5 %) | 27.3 (0.9)⧧ | 81.4 (2.0)# | 1.4 (0.1)# | 95.3 (1.1)# | 28.3 (3.1)# |
| Effect of % Ethanol Concentration | |||||
| 6 (20 %) | 27.3 (0.9)⧧ | 81.4 (2.0) | 1.4 (0.1)*** | 95.3 (1.1) | 28.3 (3.1)*** |
| 7 (0 %) | 27.6 (0.1) | 79.0 (0.7) | 1.7 (0.2)*** | 92.4 (4.5) | 17.6 (2.8)*** |
Values were average of 6 different batches.
Statistically significant effects on process variables were:
% solid concentration; ED, MMAD, FPF5μm/ED and FPF1μm/ED (Expt 4, Expt 5 and Expt 6): one-way ANOVA: P<0.05
Ethanol amount; FPF1μm/ED (Expt 6 vs Expt 7): t-test: P < 0.05
Tables 2 and 3 show that, overall, the prepared combination particle formulations exhibited excellent aerosolization properties using the Aerolizer®. With these carrier-free formulations, emitted doses were greater than 75% of the loaded dose and the fine particle fractions (FPF5μm/ED) were greater than 80% of the emitted dose, for the formulations generated using a spray dryer equipped with the 90 cm drying chamber and the 4μm spray mesh.
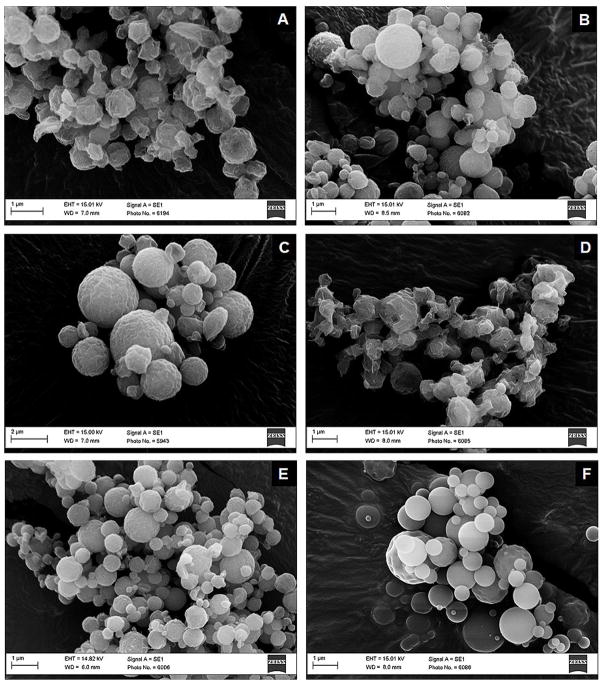
It was found that the aerosol characteristics of combination particle formulations were predominantly affected by the length of the drying chamber and the spray mesh size. The aerosolization properties of combination particle formulations were significantly improved by using a longer drying tubing (Expt 1 vs Expt 2) and a mesh with smaller pore size (Expt 3 vs Expt 4). Increasing the dryer length to 90 cm (Expt 2) resulted in a formulation, that despite a small but significant decrease in emitted dose, possessed a higher fine particle fraction (FPF5μm/ED) (P=0.0017), and a higher submicrometer particle fraction (FPF1μm/ED) (P=0.0046) compared to the 45 cm dryer chamber (Expt 1). The MMAD decreased from 3.4 μm to 2.1 μm as the dryer chamber length was increased (Table 2). Figure 2 (A) shows that the particles generated with the 45 cm drying chamber were partially bridged and had an apparent non-smooth surface. Comparing the powder formulations generated using the 4.0 μm and 5.5 μm mesh (Table 2), reducing the spray mesh size to 4 μm increased the drug fine particle fraction (FPF5μm/ED) (P<0.0001), and the submicrometer particle fraction (FPF1μm/ED) (P=0.007). The MMAD decreased from 3.3 μm to 1.8 μm when the mesh size was reduced. SEM images (Figure 2 (B) and (C)) also suggested that the spray mesh size had the greatest influence on the primary particle size; Figure 2 (B) illustrates smaller primary particles with the 4 μm mesh compared with Figure 2 (C) and the 5.5 μm mesh. Based on these results, all subsequent experiments in this study were performed exclusively using the 90 cm drying chamber and 4.0 μm mesh size. Decreasing the inlet drying temperature from 85 °C (Expt 2) to 70 °C (Expt 4), while maintaining all other conditions constant produced a small, but not statistically significant improvement in aerosol performance. The lower temperature was employed for the remaining experiments.
Figure 2.
SEM images of the spray dried formulations: (A) Expt 1, (B) Expt 4, (C) Expt 3, (D) Expt 5, (E) Expt 6 and (F) D-AS.
The solid concentration of spray solution which provided the best aerodynamic performance among three concentrations was 0.5 % w/v (Expt 6) (Table 3). The FPF1μm/ED for the 0.5% w/v formulation was significantly higher compared to that of the 0.2% w/v (Dunnett’s method: P=0.0089) and the 1.0% w/v (Dunnett’s method: P=0.0129) with a value of 28.3%. The MMAD for the 0.5% w/v formulation was 1.4 μm compared to 1.8 μm and 1.9 μm for the 1.0 %w/v and 0.2%w/v solutions, respectively (Table 3). The presence of ethanol in the carrier solvent was observed to be important to obtain powders with a high drug submicrometer particle fraction (Expt 6 vs Expt 7; FPF1μm/ED, P=0.005), although there is no significant difference in the other aerosolization properties (Table 3).
During the formulation development, it was observed that concentrations of greater than 20%w/w L-leucine were required for solid particle formation during the spray drying process and to aid dispersion during aerosolization. The sprayed formulations with less than 20%w/w L-leucine formed a thin film on the precipitator wall as the co-sprayed AS and MN formed a eutectic mixture.
The conditions for producing the best performing EEG combination particles, based on the in vitro aerosolization results, were identified as those used in Expt 6, and consisted of: 0.5%w/v solids concentration, consisting of AS, MN, L-leucine and poloxamer 188 in a ratio of 30/48/20/2 %w/w, respectively, in a water:ethanol (80:20% v/v) solution which was spray dried at 70 °C. The submicrometer particle fraction (FPF1μm/ED) of the developed formulation (Expt 6) was 28.3% with an emitted dose of over 80% and a fine particle fraction of 95.3% when aerosolized using the Aerolizer. It should be noted that this device was developed for the aerosolization of micrometer sized DPI formulations.
3.2. EEG dry powder formulation characterization
The physico-chemical properties of the best performing combination formulation (Expt 6) were assessed. In order to investigate the importance of the combination particle excipients on the particle size and aerosol performance characteristics of the combination powder formulation, a drug only control formulation (D-AS) was produced using the same spray drying conditions however without excipients. Figures 2 (E) and (F) show SEM images of the combination formulation (Expt 6) and the drug only formulation (D-AS), respectively. Individual particles from both powders appeared to be a similar size; however, the drug only particles did appear to possess a smoother surface.
As an alternative particle size screening method to cascade impaction, Table 4 shows the particle size distribution characteristics for the combination formulation (Expt 6) and the D-AS formulation determined using the Malvern Spraytec laser diffraction technique. The median particle size (D50) of the combination formulation was 2.0 μm. The skeletal density of this formulation was determined to be 1.33 g/cm3 (Table 4). The particle size data and density results were used to calculate a theoretical primary particle aerodynamic diameter (Dae) of 2.3 μm, which appeared to be significantly greater than the MMAD (1.4 μm) determined by cascade impaction (Table 3). It is important to recognize there can be significant differences between drug specific cascade impaction studies and laser diffraction methods.
Table 4.
Summary of the mean (SD) aerosol particle size characteristics of the final developed formulation (Expt 6) and a drug only formulation (D-AS), measured using the Malvern Spraytec® (n = 3)
| Experiment | D10 (μm) | D50 (μm) | D90 (μm) | Dae (μm) | Dae/MMAD |
|---|---|---|---|---|---|
| Expt 6 | 0.5 (0.0) | 2.0 (0.3) | 5.0 (0.5) | 2.3 | 1.6 |
| D-AS | 1.8 (1.5) | 29.2 (25.9) | 83.9 (53.9) | 33.3 | 17.5 |
For the drug only formulation (D-AS), the particle size distribution emitted from the inhaler appeared polydisperse with a median particle size (D50) of 29.2 μm. This contrasts with the SEM image in Figure 2 (F), which appears to show individual particles in the size range of 0.5 μm to 1.5 μm. It is believed that the increased particle size of the aerosol emitted from the inhaler for the drug only formulation reflects the formation of drug agglomerates within the capsule during aerosolization. Zhou et al., (Zhou et al., 2010) reported a similar observation using lactose as a model drug and showed particles with an initial size of 3.8 μm determined by SEM, while the particle size of the lactose emitted from the inhaler was between 12–16 μm. The degree of agglomeration will be dependent upon the initial particle size, the physic-chemical properties of the drug and the presence of excipient.
In addition, aerodynamic particle sizing of the drug only formulation using the NGI impactor was performed. For the D-AS formulation, due to drug agglomeration and poor deaggregation of the drug only formulation, only 30.9 % of the formulation was deposited in the impactor for sizing, reflecting the larger particle size of the aerosol emitted from the device observed in the Malvern studies. The remainder of the dose was deposited in the device and preseparator. The high standard deviation observed during particle sizing was due to a combination of the powder agglomeration, poor powder dispersion and device emptying in the absence of the EEG excipients. The importance of the EEG excipients to prevent drug agglomeration and allow powder dispersion to the primary particles was demonstrated using the drug only formulation.
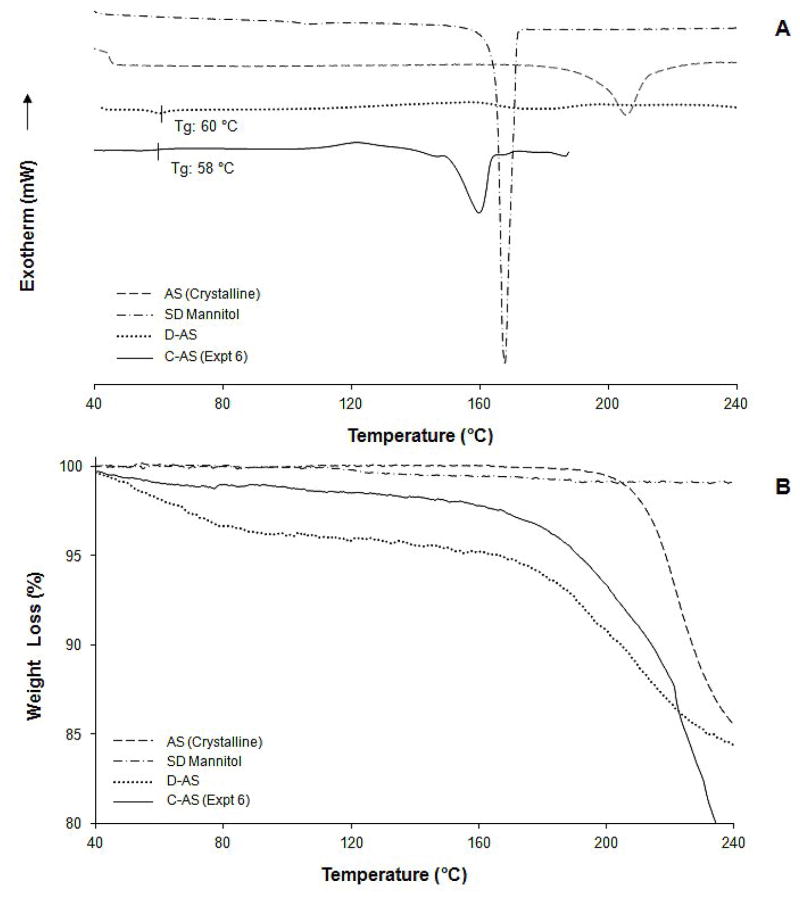
Differential scanning calorimetry (DSC) revealed that the AS in the combination formulation particles (C-AS; Expt 6) was present as an amorphous structure embedded in a crystalline MN matrix (Figure 3 (A)). A glass transition was observed at 58 °C, corresponding to the glass transition of AS. The amorphous AS in the combination particles recrystallized at about 120 °C followed by decomposition at 180 °C. Crystalline mannitol was observed to melt around 160 °C. From the TGA analysis (Figure 3 (B)), the total weight loss for the combination formulation was 1.5%w/w upon heating to 130 °C.
Figure 3.
DSC thermograms (A) and TGA results (B) for spray dried mannitol (SD Mannitol), crystalline AS, optimized combination particle formulation (Expt 6) and D-AS formulations.
The D-AS powder was also found to be amorphous. The DSC thermogram shows two endothermic processes associated with/without weight loss as seen in Figure 3 (A) and (B); the first one, at 60 °C, corresponds to the glass transition temperature and the second one, at 160 °C–200 °C, corresponds to decomposition of AS. TGA analysis of the D-AS formulation revealed the total weight loss of 4.1 %w/w upon heating to 130 °C.
3.3. EEG dry powder formulation aerosol characterization in the in vitro MT model
In order to gain an understanding of the relative importance of (i) particle size, and (ii) formulation excipients, the in vitro aerosolization performance in a MT model of the best performing submicrometer formulation (Expt 6) was compared with (i) a formulation with an identical composition and a micrometer particle size (Expt 3), (ii) a formulation with submicrometer particle size containing drug only (D-AS). To evaluate the influence of particle engineering process, which is known to be the key factor determining a particle deagglomeration, the MT deposition of commercial dry powder formulation (Salbulin), binary mixture of a micronized AS and course lactose carrier particles, was also compared.
Figure 4 shows that the commercial dry powder formulation was observed to exhibit the highest MT deposition as 80.4%/ED, indicating micronized AS particles were not fully detached from carrier particles upon aerosolization using the Aerolizer. The D-AS powder, which from SEM images had a similar particle size distribution to the combination formulation (Expt 6) without the addition of EEG excipients, showed about 40.1% AS deposition in the MT region. The lack of formulation excipients for this powder was perhaps responsible for the poor deaggregation of these submicrometer primary particles resulting in an unexpectedly high MT deposition. In comparison, the micrometer size combination particle formulation (Expt 3) had a MT deposition (20.8%) that was lower than the submicrometer drug only formulation despite its larger particle size, suggesting the importance of the excipients in obtaining good aerosolization properties. The combination of incorporating the formulation excipients into the submicrometer particles provided the lowest MT deposition in the submicrometer combination particle formulation (Expt 6; 4.1%).
Figure 4.
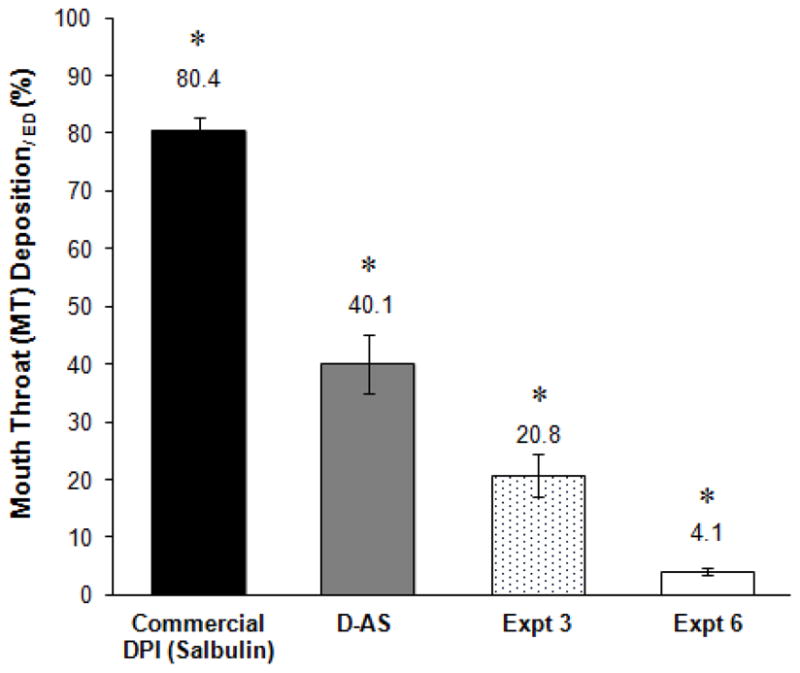
AS deposition in the MT geometry for aerosols emitted from the Aerolizer® (n ≥ 4).
*Statistical difference between three formulations groups (One-way ANOVA: P < 0.05)
4. Discussion
A spray dried submicrometer powder formulation containing drug and hygroscopic excipients was engineered to combine the high MT penetration efficiency of submicrometer aerosol particles with the deposition efficiency of micrometer sized particles by utilizing controlled condensational growth during the inhalation cycle. Based on the hygroscopic characteristics of a series of drug and hygroscopic excipients reported by Hindle and Longest (Hindle and Longest, 2012; Longest and Hindle, 2012; Longest et al., 2012b; Tian et al., 2011b), AS and MN were selected as a model drug and primary excipient for this first study to develop a dry powder formulation for the EEG approach. In these studies, the nominal AS concentration was 30%w/w which allowed delivery of therapeutically relevant doses (100–500 μg) using formulation masses of between 0.3–1.7 mg loaded into the DPI. MN as an excipient has been previously employed in the spray dried Exubera inhaled insulin formulation (Harper et al., 2007). A MN content of 48 %w/w was employed which was capable of providing stability under ambient conditions and sufficient hygroscopic growth in the simulated respiratory conditions. This is in part due to a combination of two properties, a strong propensity to crystallize and a high aqueous solubility (Lee et al., 2011b; You et al., 2007; Yu et al., 1998). Unlike most spray dried products spray dried MN tends to maintain its crystalline structure (Hulse et al., 2009). This minimizes moisture sorption under ambient conditions until it is exposed to saturated humidity conditions (Yu et al., 1998). The DSC thermograms (Figure 3 (A)) of spray dried MN and the combination particle formulation (Expt 6) show evidence of the MN crystalline form in both powders after spray drying with peaks at 160–167 °C corresponding to the melting of MN. The melting peak from the combination particle formulation was broad due to the glassy mixture embedded with the crystalline MN.
A new spray dryer was adopted for particle generation due to its reported capability of producing particles in the submicrometer size range at high yields (Lee et al., 2011a; Li et al., 2010; Schmid et al., 2010). Spray drying is a well established method to manufacture inhaled dry powder products (Chow et al., 2007; Vehring, 2008), however, the application of conventional spray dryers to design particles in the submicrometer size range is technically difficult due to limitations in atomization and powder collection techniques. The impact of process and formulation parameters (Table 1) on the resulting properties of the spray dried powders were evaluated. The properties of prepared formulations were characterized by SEM analysis (Figure 2) and aerosolization characterization (Tables 2 & 3). During the development studies, it was found that L-leucine content, the length of drying chamber, spray mesh size, % solids concentration and ethanol concentration in the carrier solvent were important factors affecting the properties of combination particles.
It was observed that combination particles required at least 20 %w/w L-leucine in order to generate solid particles. In the absence of L-leucine, the Tg of amorphous AS was lowered below the spray drier outlet temperature (about 40 °C) in the presence of MN. L-leucine, a glass forming agent with a high Tg (140 °C), was believed to increase the Tg of the amorphous mixture above the outlet temperature (Weers et al., 2007).
Increasing the length of the drying chamber and therefore increasing the particle drying time improved the aerosol performance of the combination formulation (Expt 1 vs Expt 2), as indicated by the drug FPF1μm/ED and FPF5μm/ED values. The FPF1μm/ED and FPF5μm/ED significantly increased from 2.8% and 66.2% with the 45 cm drying chamber to 10.4% and 91.5% using the 90 cm chamber, respectively (t-test: P=0.0046 and 0.0017 for the FPF1μm/ED and FPF5μm/ED). Unlike conventional bench top spray dryers which generate a cyclone (turbulent flow) to promote efficient drying, the nano spray dryer operates on a laminar flow principle, thus based on the aerosol performance data, the longer chamber appeared to provide complete drying for this particular aqueous formulation (Lee et al., 2011a). The laminar flow principle is particularly ideal for heat-sensitive materials since gentle heating of atomized particles is achievable with complete drying.
The pore size on the spray mesh surface was found to be a key factor determining the size of primary particle. The 5.5 μm spray mesh generated particle in the 3–4 micrometer range (Expt 3), whereas 4 μm spray mesh was able to prepare particles in the size range of 0.5 to 1.5 μm (Expt 4) for these aqueous formulations. This is attributed mainly to the vibrating mesh technology that the nano spray dryer utilizes for atomization. Unlike conventional spray nozzles, such as rotary atomizers, pressure nozzles and two-fluid nozzles, the vibrating mesh generates precisely sized droplets by extruding the liquid feed solution through the holes on the mesh surface utilizing a piezoelectric actuator (Lee et al., 2011a; Schmid et al., 2010). Schmid et al. reported a good correlation between the mesh size of 4 μm, 5.5 μm and 7 μm with the resulting droplet sizes prior to drying (D50) of 4.8 μm, 6 μm and 7.2 μm, respectively (Schmid et al., 2010).
A solid concentration of 0.5%w/v together with 4 μm spray mesh (Expt 6) produced a combination DPI formulation generating the largest submicrometer AS aerosol fraction of 28.3%. As expected, increasing the % solid concentration to 1% w/v (Expt 4) generated larger primary particles (Figure 2 (B)) and a lower AS FPF1μm/ED of 14.5% compared to the 0.5 %w/v formulation. It is widely known that the geometric diameter of spray dried particles is directly affected by changes in the solid concentration of the feed solution; generally, lower concentrations produce smaller dried particles. Lowering the solid concentration to 0.2 % w/v (Expt 5) produced particles without a well-defined individual structure (Figure 2 (D)). This was perhaps due to a lower solution ion concentration reducing the electrical conductivity of the solution, which was not sufficient to suppress the high electrostatic charge present in water. It has been reported that aerosols of pure water or non-electrolytes solution, generated by a vibrating mesh nebulizer, yielded a high electrostatic charge and therefore increased solution adhesion to the internal device surface (Deshpande et al., 2002; Ghazanfari et al., 2007; Rosell et al., 2000). Since the atomization mechanism of the vibrating mesh nozzle is similar to that of vibrating mesh nebulizer, it can be assumed that there are certain critical solution properties, such as ion concentration and electrical conductivity of feed solution, that are required to generate atomized liquid droplets from the vibrating mesh nozzle.
The addition of 20%v/v ethanol in aqueous carrier solvent was also observed to be important with respect to combination particle drug aerosol performance. In the absence of ethanol (Expt 7), the AS FPF1μm/ED was reduced to 17.6% compared to 28.3% when 20 %v/v ethanol (Expt 6) was added to the spray drying formulation. It was believed that ethanol accelerated the initial saturation of L-leucine on the atomized droplet surface by decreasing its solubility in the aqueous solution; the solubility of L-leucine in water is low, 22 mg/ml, and even lower in ethanol (Vehring, 2008).
It is widely recognized that dry powder inhaler formulations should be protected from the effects of ambient humidity in order to maintain aerosol performance. Prolonged exposure to elevated humidity can induce changes in crystallinity and affect powder dispersion (Ward and Schultz, 1995). In this present study, powders were stored a desiccator at < 10% prior to exposure to 45–55% RH during capsule filling. This is analogous to conditions used for a commercial capsule based DPI product that is filled under low humidity conditions and stored in humidity resistant packaging prior to exposure to ambient conditions during use by the patient. This is particularly important for the powder formulations produced in this study that were developed for their hygroscopic properties when exposed to the high humidity environments within the lungs. No attempt was made to investigate the effects of humidity exposure on the submicrometer formulations, however, it is expected that a similar decreased aerosol performance would be observed as reported by others if the powders were exposed (Hindle and Makinen, 1996; Young et al., 2007).
These studies have employed the combination of submicrometer particles and formulation excipients to significantly improve drug aerosol performance from a DPI platform using the EEG approach. The aerodynamic properties of the powder formulation are attributed to a combination of formulation excipients (mainly leucine), the submicrometer size of the particle and the dispersion mechanism of the DPI (Aerolizer) used to aerosolize the powder. A realistic MT model was used to compare the AS MT deposition of the developed submicrometer combination drug and excipient formulation (Expt 6) with a submicrometer drug only formulation (D-AS), a micrometer sized combination drug excipient formulation (Expt 3), and a commercial carrier-based dry powder formulation. It has been shown that using a realistic MT geometry (Figure 1) designed by Xi and Longest et al. (Xi and Longest, 2007) provides a good in vitro-in vivo correlation of MT deposition (Delvadia et al., 2012; Islam and Gladki, 2008). Figure 4 shows that the AS MT deposition was lowest (4.1%) for the submicrometer combination drug and excipient formulation (Expt 6). The submicrometer drug only formulation showed 10 times higher MT deposition when compared to the combination formulation (Expt 6), revealing the importance of the formulation excipients in producing an aerosolizable powder. Despite the submicrometer primary particle size, 40.1% of the drug aerosol was deposited in the MT region. Due to MT deposition and device drug retention, only 16% of the loaded AS dose was available for lung delivery, which was believed to be due to the presence of drug aggregates that were not easily dispersed during the DPI aerosolization process. In contrast, the incorporation of the formulation excipients into micrometer sized particles resulted in drug MT deposition of 20.8%, suggesting that despite the larger particle size, it was possible to produce low drug MT deposition using appropriate formulation excipients and micronization technique. This drug MT deposition for the spray dried EEG formulations is significantly better than that typically observed for conventional carrier-based DPI formulations (40–90%) (Newman and Busse, 2002; Zhang et al., 2007). We also observed about 80% MT drug deposition using the commercial lactose-based Salbulin DPI formulation. One of the major reasons for this high drug MT deposition is due to insufficient detachment/de-agglomeration of the micronized particles from either course carrier particles or particle agglomerates, which is mainly caused by strong interparticulate forces and poor formulation-device coordination. The submicrometer combination formulation performed well in a non-optimized commercially available DPI that was designed to aerosolize lactose carrier based formulations, with about 30% of submicrometer aerosol generation. It may be possible to significantly increase the submicrometer aerosol fraction by optimizing the inhaler device for use with this formulation. A formulation-device optimization study will be conducted with the submicrometer combination particles prepared in this study (Expt 6) to generate maximum amount of submicrometer aerosols. The hygroscopic growth of the submicrometer aerosols will also be assessed with a realistic lung model.
Conclusion
Spray dried combination drug and excipient particles were produced with a submicrometer primary particle size suitable for use in the EEG application. Spray drying and formulation variables were investigated to produce DPI aerosols with high emitted doses and fine particle fractions. The developed combination particle formulation exhibited excellent aerosolization properties with 28.3% of submicrometer fraction using a conventional DPI (Aerolizer®), with only 4.1% of MT deposition. The developed combination formulation delivered a powder aerosol developed for the EEG application with high dispersion efficiency and low MT deposition from a convenient DPI device platform.
Acknowledgments
This study was supported by Award Number R21 HL104319 and R01 HL107333 from the National Heart, Lung, and Blood Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health. Microscopy was performed at the VCU Department of Anatomy and Neurobiology Microscopy Facility, supported, in part, with funding from NIH-NINDS Center core grant (5P30NS047463-02).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ashurst I, Malton A, Prime D, Sumby B. Latest advances in the development of dry powder inhalers. Pharmaceutical Science & Technology Today. 2000;3:246–256. doi: 10.1016/s1461-5347(00)00275-3. [DOI] [PubMed] [Google Scholar]
- Borgstrom L, Bondesson E, Moren F, Trofast E, Newman SP. Lung deposition of budesonide inhaled via Turbuhaler - A comparision with terbutaline sulfate in normal subjects. European Respiratory Journal. 1994;7:69–73. doi: 10.1183/09031936.94.07010069. [DOI] [PubMed] [Google Scholar]
- Brand P, Meyer T, Weuthen T, Timmer W, Berkel E, Wallenstein G, Scheuch G. Lung deposition of radiolabeled tiotropium in healthy subjects and patients with chronic obstructive pulmonary disease. Journal of Clinical Pharmacology. 2007;47:1335–1341. doi: 10.1177/0091270006295788. [DOI] [PubMed] [Google Scholar]
- Cheng YS. Aerosol deposition in the extrathoracic region. Aerosol Science and Technology. 2003;37:659–671. doi: 10.1080/02786820300906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chow AHL, Tong HHY, Chattopadhyay P, Shekunov BY. Particle engineering for pulmonary drug delivery. Pharmaceutical Research. 2007;24:411–437. doi: 10.1007/s11095-006-9174-3. [DOI] [PubMed] [Google Scholar]
- Delvadia RR, Longest PW, Byron PR. In vitro tests for aerosol deposition. I: Scaling a physical model of the upper airways to predict drug deposition variation in normal humans. Journal of Aerosol Medicine and Pulmonary Drug Delivery. 2012;25:32–40. doi: 10.1089/jamp.2011.0905. [DOI] [PubMed] [Google Scholar]
- Deshpande D, Blanchard J, Srinivasan S, Fairbanks D, Fujimoto J, Sawa T, Wiener-Kronish J, Schreier H, Gonda I. Aerosolization of lipoplexes using AERx pulmonary delivery system. AAPS PharmSci. 2002;4:1–10. doi: 10.1208/ps040313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards DA, Hanes J, Caponetti G, Hrkach J, BenJebria A, Eskew ML, Mintzes J, Deaver D, Lotan N, Langer R. Large porous particles for pulmonary drug delivery. Science. 1997;276:1868–1871. doi: 10.1126/science.276.5320.1868. [DOI] [PubMed] [Google Scholar]
- Geldart D. Types of gas fluidization. Powder Technology. 1973;7:285–292. [Google Scholar]
- Geller DE, Weers J, Heuerding S. Development of an inhaled dry-powder formulation of tobramycin using PulmoSphere (TM) technology. Journal of Aerosol Medicine and Pulmonary Drug Delivery. 2011;24:175–182. doi: 10.1089/jamp.2010.0855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghazanfari T, Elhissi AMA, Ding Z, Taylor KMG. The influence of fluid physicochemical properties on vibrating-mesh nebulization. International Journal of Pharmaceutics. 2007;339:103–111. doi: 10.1016/j.ijpharm.2007.02.035. [DOI] [PubMed] [Google Scholar]
- Harper NJ, Gray S, De Groot J, Parker JM, Sadrzadeh N, Schuler C, Schumacher JD, Seshadri S, Smith AE, Steeno GS, Stevenson CL, Taniere R, Wang M, Bennett DB. The design and performance of the Exubera((R)) pulmonary insulin delivery system. Diabetes Technology & Therapeutics. 2007;9:S16–S27. doi: 10.1089/dia.2007.0222. [DOI] [PubMed] [Google Scholar]
- Hindle M, Longest PW. Condensational growth of combination drug-excipient submicrometer particles for targeted high-efficiency pulmonary delivery: evaluation of formulation and delivery device. Journal of Pharmacy and Phamacology. 2012;64:1254–1263. doi: 10.1111/j.2042-7158.2012.01476.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hindle M, Makinen G. Effects of humidity on the in-vitro aerosol performance and aerodynamic size distribution of cromolyn sodium for inhalation. European Journal of Pharmaceutical Sciences. 1996;4:142–142. [Google Scholar]
- Hulse WL, Forbes RT, Bonner MC, Getrost M. The characterization and comparison of spray-dried mannitol samples. Drug Development and Industrial Pharmacy. 2009;35:712–718. doi: 10.1080/03639040802516491. [DOI] [PubMed] [Google Scholar]
- Islam N, Gladki E. Dry powder inhalers (DPIs) - A review of device reliability and innovation. International Journal of Pharmaceutics. 2008;360:1–11. doi: 10.1016/j.ijpharm.2008.04.044. [DOI] [PubMed] [Google Scholar]
- Jaques PA, Kim CS. Measurement of total lung deposition of inhaled ultrafine particles in healthy men and women. Inhalation Toxicology. 2000;12:715–731. doi: 10.1080/08958370050085156. [DOI] [PubMed] [Google Scholar]
- Lee SH, Heng D, Ng WK, Chan HK, Tan RBH. Nano spray drying: A novel method for preparing protein nanoparticles for protein therapy. International Journal of Pharmaceutics. 2011a;403:192–200. doi: 10.1016/j.ijpharm.2010.10.012. [DOI] [PubMed] [Google Scholar]
- Lee YY, Wu JX, Yang M, Young PM, van den Berg F, Rantanen J. Particle size dependence of polymorphism in spray-dried mannitol. European Journal of Pharmaceutical Sciences. 2011b;44:41–48. doi: 10.1016/j.ejps.2011.06.002. [DOI] [PubMed] [Google Scholar]
- Li XA, Anton N, Arpagaus C, Belleteix F, Vandanune TF. Nanoparticles by spray drying using innovative new technology: The Buchi Nano Spray Dryer B-90. Journal of Controlled Release. 2010;147:304–310. doi: 10.1016/j.jconrel.2010.07.113. [DOI] [PubMed] [Google Scholar]
- Longest PW, Hindle M. Condensational growth of combination drug-excipient submicrometer particles for targeted high efficiency pulmonary delivery: comparison of CFD predictions with experimental results. Pharmaceutical Research. 2012;29:707–721. doi: 10.1007/s11095-011-0596-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longest PW, Tian G, Li X, Son Y-J, Hindle M. Performance of combination drug and hygroscopic excipient submicrometer particles from a softmist inhaler in a characteristic model of the airways. Annals of Biomedical Engineering. 2012a doi: 10.1007/s10439-10012-06160-10432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longest PW, Tian G, Son Y-J, Li X, Hindle M. Respiratory Drug Delivery 2012. Davis Healthcare International; River Grove, IL: 2012b. Engineered drug targeting to the lungs: Ensuring growth and deposition of submicrometer aerosols through device design and formulations; pp. 61–69. [Google Scholar]
- Newman SP, Busse WW. Evolution of dry powder inhaler design, formulation, and performance. Respiratory Medicine. 2002;96:293–304. doi: 10.1053/rmed.2001.1276. [DOI] [PubMed] [Google Scholar]
- Newman SP, Pitcairn GR, Hirst PH, Bacon RE, O’Keefe E, Reiners M, Hermann R. Scintigraphic comparison of budesonide deposition from two dry powder inhalers. European Respiratory Journal. 2000;16:178–183. doi: 10.1034/j.1399-3003.2000.16a29.x. [DOI] [PubMed] [Google Scholar]
- Prime D, Atkins PJ, Slater A, Sumby B. Review of dry powder inhalers. Advanced Drug Delivery Reviews. 1997;26:51–58. doi: 10.1016/s0169-409x(97)00510-3. [DOI] [PubMed] [Google Scholar]
- Raula J, Laehde A, Kauppinen EI. A novel gas phase method for the combined synthesis and coating of pharmaceutical particles. Pharmaceutical Research. 2008;25:242–245. doi: 10.1007/s11095-007-9464-4. [DOI] [PubMed] [Google Scholar]
- Raula J, Thielmann F, Naderi M, Lehto VP, Kauppinen EI. Investigations on particle surface characteristics vs. dispersion behaviour of L-leucine coated carrier-free inhalable powders. International Journal of Pharmaceutics. 2010;385:79–85. doi: 10.1016/j.ijpharm.2009.10.036. [DOI] [PubMed] [Google Scholar]
- Rosell J, Schuster J, Gonda I, Liu K. Electrostatic charge in AERx aerosols. Drug Delivery to the Lungs. 2000:64–67. [Google Scholar]
- Schmid K, Arpagaus C, Friess W. Evaluation of the nano spray dryer B-90 for pharmaceutical applications. Pharmaceutical Development and Technology. 2010;16:287–294. doi: 10.3109/10837450.2010.485320. [DOI] [PubMed] [Google Scholar]
- Tian G, Longest PW, Su G, Hindle M. Characterization of respiratory drug delivery with enhanced condensational growth using an individual path model of the entire tracheobronchial airways. Annals of Biomedical Engineering. 2011a;39:1136–1153. doi: 10.1007/s10439-010-0223-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian G, Longest PW, Su G, Walenga RL, Hindle M. Development of a stochastic individual path (SIP) model for predicting the tracheobronchial deposition of pharmaceutical aerosols: Effects of transient inhalation and sampling the airways. Journal of Aerosol Science. 2011b;42:781–799. [Google Scholar]
- Timsina MP, Martin GP, Marriott C, Ganderton D, Yianneskis M. Drug-delivery to the respiratory-tract using dry powder inhalers. International Journal of Pharmaceutics. 1994;101:1–13. [Google Scholar]
- Vehring R. Pharmaceutical particle engineering via spray drying. Pharmaceutical Research. 2008;25:999–1022. doi: 10.1007/s11095-007-9475-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser J. Van der Waals and other cohesive forces affecting powder fluidization. Powder Technology. 1989;58:1–10. [Google Scholar]
- Ward GH, Schultz RK. Process-induced crystallinity changes in albuterol sulfate and its effect on powder physical stability. Pharm Res. 1995;12:773–779. doi: 10.1023/a:1016232230638. [DOI] [PubMed] [Google Scholar]
- Weers JG, Tarara TE, Clark AR. Design of fine particles for pulmonary drug delivery. Expert Opinions on Drug Delivery. 2007;4:297–313. doi: 10.1517/17425247.4.3.297. [DOI] [PubMed] [Google Scholar]
- Xi J, Longest PW. Transport and deposition of micro-aerosols in realistic and simplified models of the oral airway. Annals of Biomedical Engineering. 2007;35:560–581. doi: 10.1007/s10439-006-9245-y. [DOI] [PubMed] [Google Scholar]
- Xi J, Longest PW. Effects of oral airway geometry characteristics on the diffusional deposition of inhaled nanoparticles. Journal of Biomechanical Engineering. 2008;130:011008. doi: 10.1115/1.2838039. [DOI] [PubMed] [Google Scholar]
- Yang W, Peters JI, Williams RO., III Inhaled nanoparticles - A current review. International Journal of Pharmaceutics. 2008;356:239–247. doi: 10.1016/j.ijpharm.2008.02.011. [DOI] [PubMed] [Google Scholar]
- You Y, Zhao M, Liu G, Tang X. Physical characteristics and aerosolization performance of insulin dry powders for inhalation prepared by a spray drying method. Journal of Pharmacy and Pharmacology. 2007;59:927–934. doi: 10.1211/jpp.59.7.0003. [DOI] [PubMed] [Google Scholar]
- Young PM, Sung A, Traini D, Kwok P, Chiou H, Chan HK. Influence of humidity on the electrostatic charge and aerosol performance of dry powder inhaler carrier based systems. Pharm Res. 2007;24:963–970. doi: 10.1007/s11095-006-9218-8. [DOI] [PubMed] [Google Scholar]
- Yu L, Mishra DS, Rigsbee DR. Determination of the glass properties of D-mannitol using sorbitol as an impurity. Journal of Pharmaceutical Sciences. 1998;87:774–777. doi: 10.1021/js970224o. [DOI] [PubMed] [Google Scholar]
- Zanen P, van Spiegel PI, van der Kolk H, Tushuizen E, Enthoven R. The effect of the inhalation flow on the performance of a dry powder inhalation system. International Journal of Pharmaceutics. 1992;81:199–203. [Google Scholar]
- Zhang Y, Gilbertson K, Finlay WH. In vivo-in vitro comparison of deposition in three mouth-throat models with Qvar (R) and Turbuhaler (R) inhalers. Journal of Aerosol Medicine-Deposition Clearance and Effects in the Lung. 2007;20:227–235. doi: 10.1089/jam.2007.0584. [DOI] [PubMed] [Google Scholar]
- Zhou QT, Armstrong B, Larson I, Stewart PJ, Morton DAV. Understanding the influence of powder flowability, fluidization and de-agglomeration characteristics on the aerosolization of pharmaceutical model powders. European Journal of Pharmaceutical Sciences. 2010;40:412–421. doi: 10.1016/j.ejps.2010.04.012. [DOI] [PubMed] [Google Scholar]