Abstract
Background:
Tendon transfer surgery can restore elbow extension in approximately 70% of persons with tetraplegia and often results in antigravity elbow extension strength. However, we have noted an almost 15% rupture/attenuation rate.
Objective:
This investigation was conducted to analyze potential causes in adolescents/young adults with spinal cord injury (SCI) who experienced tendon rupture or attenuation after biceps-to-triceps transfer.
Methods:
Medical charts of young adults with SCI who underwent biceps-to-triceps transfer and experienced tendon rupture or attenuation were reviewed. Data collected by retrospective chart review included general demographics, surgical procedure(s), use and duration of antibiotic treatment, time from tendon transfer surgery to rupture/attenuation, and method of diagnosis.
Results:
Twelve subjects with tetraplegia (mean age, 19 years) who underwent biceps-to-triceps reconstruction with subsequent tendon rupture or attenuation were evaluated. Mean age at time of tendon transfer was 18 years (range, 14-21 years). A fluoroquinolone was prescribed for 42% (n=5) of subjects. Tendon rupture was noted in 67% (n=8), and attenuation was noted in 33% (n=4). Average length of time from surgery to tendon rupture/attenuation was 5.7 months (range, 3-10 months).
Conclusion:
Potential contributing causes of tendon rupture/attenuation after transfer include surgical technique, rehabilitation, co-contraction of the transfer, poor patient compliance, and medications. In this cohort, 5 subjects were prescribed fluoroquinolones that have a US Food and Drug Administration black box concerning tendon ruptures. Currently, all candidates for upper extremity tendon transfer reconstruction are counseled on the effects of fluoroquinolones and the potential risk for tendon rupture.
Keywords: adolescent, spinal cord injury, tendon rupture
The annual incidence of spinal cord injury (SCI) in the United States is approximately 40 cases per million population or 12,000 new cases each year. Of the annual cases reported each year, 50% result in either incomplete or complete tetraplegia.1 According to the Shriners Hospitals for Children Annual SCI Database Report, the median age at injury/diagnosis was 13 years, and 42% of all patients were between the ages of 15 and 21 years.2 Individuals with SCI face many challenges and are often dependent on others for many activities of daily living. Hanson and Franklin3 surveyed adult men with tetraplegia and found that most preferred restoration of hand function before restoration of bowel, bladder, or sexual function or walking ability. Seventy percent to 85% of individuals with tetraplegia may benefit from surgery of the upper extremity.4 Active elbow extension is lost in approximately 70% of persons sustaining cervical level SCI.5 Restoration of elbow extension is an essential part of the surgical intervention. Elbow extension can enhance mobility in bed, facilitate transfers, allow overhead reaching, augment weight shifting, and promote propelling a wheelchair.
Two surgical procedures are available for restoration of elbow extension. The posterior deltoid or the biceps may be used as a donor muscle to restore active elbow extension. At the authors’ institution, the preference is to use the biceps for transfer due to the avoidance of a free tendon graft, earlier time to mobilization, and superior elbow extension strength.6 However, we have noted an almost 15% rupture/attenuation rate.7
The fluoroquinolones were first introduced in the 1980s and have been used extensively to treat infections caused by gram-negative organisms.8 Fluoroquinolones have a number of therapeutic uses including the treatment of urinary tract infections (UTIs), lower respiratory tract infections, skin and skin structure infections, acute sinusitis, and community-acquired pneumonia.9-11 However, the use of fluoroquinolones has been associated with increased incidence of tendon ruptures.8,12 Fluoroquinolone-associated tendonitis most commonly involves the Achilles tendon, but effects on the quadriceps, peroneus brevis, extensor pollicis longus, the long head of the biceps, and the rotator cuff tendons have also been reported. Clinical manifestations of tendon rupture include severe and sudden onset of pain, tenderness on palpation, edema, and decreased movement of the affected area. Diagnosis is usually made by physical examination, ultrasonography, or MRI. Symptoms have been noted in patients as early as 2 weeks after starting the flouroquinolones. Early symptoms can begin a few hours after the initial dose, and symptoms have been reported 6 months after therapy has been stopped. Treatment interventions include discontinuation of the implicated flouroquinolone; nonsurgical intervention such as analgesia, physical therapy, or immobilization; and surgery for complete ruptures. Khaliq and Zhanel8 noted tendon recovery occurring in a mean of 59 to 101 days. Several mechanisms have been proposed regarding use of fluoroquinolones and the development of tendonitis or tendon rupture. Mechanisms include ischemia caused by decreased blood flow, toxicity to the collagen causing tendon necrosis, and reduced clearance of the drug in patients with renal impairment.13
The purpose of this study was to analyze potential causes in adolescents with SCI who underwent biceps-to-triceps transfer and experienced tendon rupture or attenuation.
Materials and Methods
A descriptive retrospective research design was used (level 4 evidence). Medical charts of 12 individuals, aged 18 to 24 years, with SCI who underwent biceps-to-triceps tendon reconstruction and experienced tendon rupture or attenuation were reviewed. Institutional review board approval for this study was obtained. Data were numerically coded to protect subject anonymity and were kept in a secure location. Data collected by chart review included general demographics, surgical procedure(s), use of antibiotics, duration of antibiotic treatment, time from tendon transfer surgery to rupture/attenuation, and method of diagnosis. Data were analyzed by calculating the frequency, percentage, mean, and range.
Results
Patient demographics
Twelve male subjects with tetraplegia who underwent biceps-to-triceps tendon reconstruction and experienced tendon rupture or attenuation over a 4-year period were reviewed. Mean age was 19 years (range, 18-24 years). Five subjects had a C-5 level of injury, 5 subjects had a C-4 level of injury, and 2 subjects had a C-6 level of injury. Mean age at injury was 16 years (range, 12-18 years). Age at tendon transfer procedure ranged from 14 to 21 years (mean, 18 years).
Surgical technique
All surgery was performed by a single surgeon (S.H.K.). The biceps tendon is released from its insertion into the radial tuberosity. A large nonabsorbable polyester braided grasping suture is placed within the tendon. The biceps tendon and muscle are freed from the surrounding attachments until the biceps has adequate excursion to reach the olecranon. The biceps tendon is routed around the medial side of the humerus over the ulnar nerve, which is nonfunctional in persons with tetraplegia who require restoration of elbow extension. The biceps tendon is passed to the posterior aspect of the elbow. The elbow is placed in full extension and the biceps transfer is completed.
In 7 subjects (58%), the biceps tendon was passed through the triceps tendon and fixed into an osseous tunnel within the olecranon by using stout suture. In 3 subjects (25%), the biceps tendon was passed through the triceps tendon and secured within the olecranon with a biotenodesis screw (Accumed, Hillsboro, Oregon). In 2 subjects (17%), the biceps tendon was woven (tendon weave) through the triceps tendon without fixation into the olecranon (see Table 1).
Table 1.
Tendon transfer procedures and types of fixation
| Subject | Age at transfer, years | Procedure(s) | Fixation | Rupture or attenuation | FQ |
| 1 | 19 | Bilateral biceps to triceps | Tendon weave | Rupture | No |
| 2 | 15 | Left biceps to triceps; left split FPL; right biceps to triceps; right split FPL; right FCR tenotomy; right BR to ECRB | Biotenodesis screw | Attenuation | No |
| 3 | 17 | Bilateral biceps to triceps; bilateral BR to FPL; bilateral FPL; leftECRL to FDP | Osseous tunnel | Attenuation | Yes |
| 4 | 19 | Right BR to FPL; right split FPL; right biceps to triceps; left BR toECRB; left FPL; left biceps to triceps; left FCR lengthening | Tendon weave | Rupture | No |
| 5 | 19 | Left biceps to triceps; split FPL; BR to FPL; ECRL to FDP; right biceps to triceps; split FPL; BR to FPL | Biotenodesis screw | Rupture | Yes |
| 6 | 14 | Bilateral biceps to triceps; right BR to ECRB; right split FPL; rightFPL tenodesis; left BR to FPL; left split FPL; right MP arthrodesis | Biotenodesis screw | Rupture | Yes |
| 7 | 19 | Bilateral biceps to triceps; bilateral split FPL; right BR | Osseous tunnel | Rupture | Yes |
| 8 | 19 | Right biceps to triceps, CMC fusion; split FPL; BR to ECRB transfer | Osseous tunnel | Attenuation | Yes |
| 9 | 20 | Bilateral biceps to triceps; left BR to FPL; left split FPL | Osseous tunnel | Rupture | No |
| 10 | 18 | Bilateral biceps to triceps; bilateral BR to FPL; bilateral split FPL | Osseous tunnel | Rupture | No |
| 11 | 21 | Bilateral biceps to triceps; bilateral split FPL; bilateral CMC arthrodesis; bilateral BR to FPL; bilateral EPL tenodesis | Osseous tunnel | Rupture | No |
| 12 | 17 | Right biceps to triceps; BR to ECRB; FPL intrinsic plasty | Osseous tunnel | Attenuation | No |
Note: BR = brachioradialis; CMC = carpometacarpal; ECRB = extensor carpi radialis brevis; ECRL = extensor carpi radialis longus; EPL = extensor pollicis longus; FCR = flexor carpi radialis; ; FDP = flexor digitorum profundus; FPL = flexor pollicis longus; FQ = fluoroquinolones; MC = metacarpal.
After the transfer, the limb is maintained in full extension, and the subcutaneous tissue and skin are closed with absorbable sutures. The tourniquet is deflated, and dressings and a well-padded long arm cast are applied in the operating room. The wrist is included within the cast. The position of the hand depends on concomitant procedures performed for hand function.
Postoperative regimen
After surgery, the elbow is placed in a cast in full extension for 3 to 4 weeks. An elbow extension splint in full extension is then fabricated for nighttime use. A dial-hinge brace (eg, Bledso Brace Systems, Grand Prairie, Texas) is fitted for daytime use and acts as a flexion block at 15°. The brace is adjusted each week to allow an additional 15° of flexion. The brace is not advanced if an extension lag develops. The protocol for postoperative range and strengthening is also provided (see Table 2). Tendon transfer firing is started in an antigravity plane. The medially routed biceps can be palpated along the medial humerus during active elbow extension. Verbal prompting of active elbow flexion and active forearm supination facilitate motor learning. Additional modalities, such as biofeedback with surface electromyography, are provided for patients who have difficulty with firing. Biofeedback can be used with auditory or visual cues. A recording electrode is placed over the biceps muscle and elicits a noise or a visual on a screen when the muscle in contracting. This technique identifies activation and co-contraction, which facilitates muscle education.
Table 2.
Postoperative biceps to triceps mobilization protocol
| Immobilization phase | Patient is immobilized in long arm cast with elbow in full extension |
| 1 to 3 wk post-op | Precautions:
|
Therapeutic intervention:
|
|
| Mobilization phase 3 to 12 wk post-op | Cast removed |
Precautions:
|
|
Splint
|
|
Therapeutic intervention
|
|
| Functional training | |
| Light functional training or activities may begin in allowed elbow ranges (pending time frame and assessment of allowed amount of elbow flexion) only after the therapist is sure the transfer is firing with the activity. |
Functional activities of daily living are incorporated into therapy as elbow flexion increases each week. The dial-hinge brace is continued until 90° of elbow flexion is obtained without an extension lag. A nighttime extension splint is maintained until 12 weeks after surgery. Strengthening is started 3 months after surgery.
Antibiotics
All subjects received perioperative prophylactic antibiotics, most commonly a cephalosporin. Five subjects (42%) were prescribed fluoroquinolones during their inpatient stays after tendon transfer. Four of the 5 subjects (75%) were prescribed fluoroquinolones for treatment of a symptomatic UTI, and 1 subject was prescribed a fluoroquinolone for treatment of osteomyelitis (see Table 3). Of the 5 subjects who received fluoroquinolones postoperatively, none recalled previously taking a fluoroquinolone. Subjects were also noted to be on several other medications during initial tendon transfer postoperative recovery and rehabilitation periods (see Table 4).
Table 3.
Fluoroquinolone prescription and indications
| Subject | Courses of FQ | No. of doses | Indication | Time from primary tendon transfer surgery to FQ prescribed | Time from primary tendon transfer surgery to diagnosis |
| 3 | 2 | 40 | UTI | 10 days | 3 months |
| 5 | 1 | 300 | Osteomyelitis | 2 months | 4 months |
| 6 | 1 | 14 | UTI | 42 days | 10 months |
| 7 | 1 | 20 | UTI | 16 days | 9 months |
| 8 | 1 | 20 | UTI | 34 days | 7 months |
Note:FQ = fluoroquinolone; UTI = urinary
Table 4.
Other prescribed medications
| Medication type | n (%) |
| Anticholinergics | 10 (83) |
| Stool softeners/bowel agents | 9 (75) |
| Gastrointestinal | 9 (75) |
| Antispasticity | 11 (91) |
| Antidepressants | 6 (50) |
| Pain | 11 (91) |
| Over the counter | 5 (27) |
Diagnosis of tendon rupture/attenuation
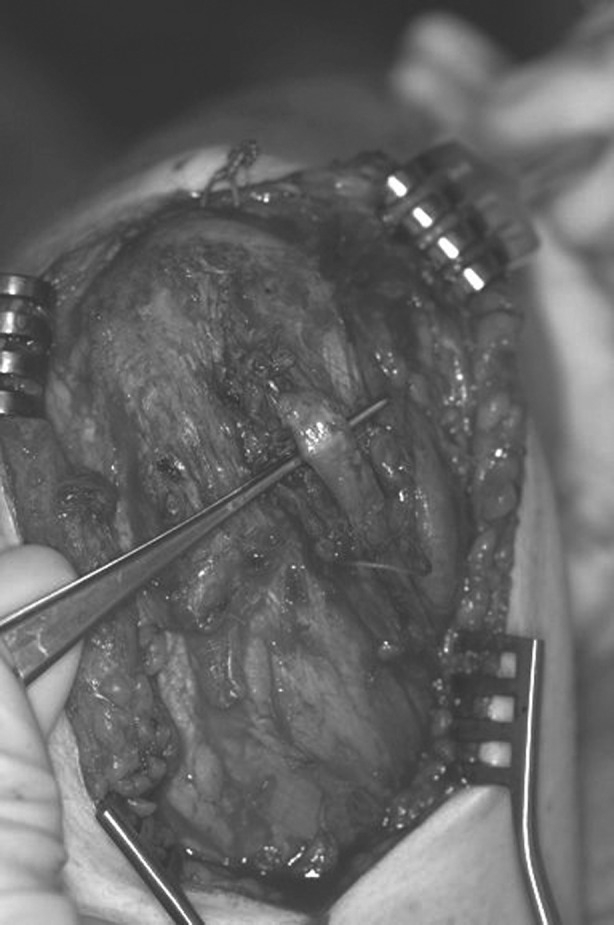
Diagnosis was made by means of physical examination. Overt tendon rupture was noted in 8 (67%) subjects with complete loss of active elbow extension (Figures 1A and 1B). Tendon attenuation was confirmed in 4 (33%) subjects by the development of a substantial extension lag. The length of time from tendon transfer surgery to tendon rupture or attenuation ranged from 3 to 10 months (mean, 5.7 months). These ruptures were noted to occur relatively later in the recovery period and during variable activities, all within the home environment. Revision surgery has been performed on a few subjects, and outcomes are pending (Figure 2). No biopsies of the tendon were performed at the time of revision.
Figure 1. (A) Subject 10 demonstrating inability to actively extend elbow. (B) Elbow extension possible with passive motion only; diagnosis of tendon rupture.
Figure 2. Biceps tendon rupture on intraoperative exploration.
Discussion
Elbow extension is crucial for overhead activities, transfers, and weight shifting, and it enhances wheelchair propulsion. Moreover, the ability to extend the hand in space an additional 12 in. increases workspace of the hand by 800%.14
The biceps-to-triceps transfer can result in functional antigravity strength approximately 75% of the time. However, the surgery and rehabilitation process are demanding and arduous. The patient is immobilized in a long arm cast or casts and loses considerable independence during the rehabilitation process. The patient becomes dependent on others for all activities of daily living, such as eating, writing, and turning in bed. Subsequently, graduated therapy is necessary with slow increases in the allowable elbow flexion. Incremental increases in elbow flexion are required to protect the tendon transfer from sudden stretch. Therapeutic strategies also focus on facilitating motor learning of the transfer.
Rupture or attenuation of the tendon is a devastating complication for the patient, surgeon, and therapist. The length of time from tendon transfer surgery to tendon rupture or attenuation ranges from 3 to 10 months. This time frame infers substantial commitment and effort from the time of surgery until the sentinel event. Potential contributing causes include the surgical technique, rehabilitation, co-contraction of the transfer, patient compliance, and medications. The surgical technique was similar in all cases, except for the method of fixation, which was variable. We could not equate technique with rupture or attenuation in this cohort. Similar rates of rupture are not found with hand/forearm transfers (eg, active pinch and grasp); most likely, these transfers experience less force during use.
Rehabilitation is also a consideration because advancing elbow flexion too quickly could result in gap formation, which has deleterious effects on tendon healing.15 We used a dial-hinge brace, which is only advanced 15° each week, and the brace was not progressed if an extension lag developed.
Regarding co-contraction of the transfer, Hutchinson et al16 have shown that the biceps muscle achieves phasic reversal over time with activity during extension and quiescence during flexion. This “learning” may be subject and time dependent. Inadvertent biceps contraction before phasic reversal could cause early gap formation, insufficient healing of the transfer, and, ultimately, rupture or attenuation.16
Patient compliance is another concern; however, all subjects in this study underwent their initial rehabilitation as inpatients under supervision by an experienced therapist. In addition, patients are often implicated as the origin for surgical complications. We do not believe that subject noncompliance played a role in subsequent tendon rupture or attenuation
The effect of medications on tendon healing is an interesting issue. Persons with SCI take many medications for a variety of reasons. Perioperative administration of cephalosporins is common practice for surgical prophylaxis at the authors’ institution. Similar cases of tendon injury have not been reported with the use of cephalosporins. Cephalosporins are in a different class of antibiotic compounds (beta lactams) than fluoroquinolones. Five subjects (42%) were prescribed fluoroquinolones during their inpatient stays after tendon reconstruction. Because UTIs are the most common type of infection in patients with SCI, the use of fluoroquinolones is commonplace. Factors that predispose this population to UTIs include bladder catheterization and urinary stasis. In 2008, the US Food and Drug Administration (FDA) added a black box warning for fluoroquinolones, which contains information about the increased risk of tendonitis and tendon rupture. Tendon disorders associated with fluoroquinolones have been estimated to occur at a rate of approximately 15 to 20 per 100,000 patients. Proposed mechanisms regarding treatment with fluoroquinolones and the development of tendonitis or tendon rupture include ischemia caused by decreased blood flow and toxicity to the collagen, which causes tendon necrosis.8,12,13
We attempted to survey all our subjects who underwent tendon transfer and their use of antibiotics. However, their initial injury was so dramatic and their acute rehabilitation so difficult that subjects and their families were unable to recall specific medications. This information would be invaluable for providing a denominator for calculation of true incidence. Nonetheless, we believe that the evidence is compelling with reference to the relationship between fluoroquinolones and tendon rupture.
Conclusion
Although there are several potential contributing causes for tendon rupture, all patients at the authors’ institution who are currently candidates for upper extremity tendon transfer reconstruction are counseled on the effects of fluoroquinolones and the potential risk for tendon rupture. In addition, we prescribe alternative antibiotics for symptomatic UTIs in patients with SCI who may undergo tendon transfer. We are currently evaluating our cases of tendon rupture to further identify contributing causes.
Acknowledgments
Lisa Merenda is a Clinical Research Nurse who currently oversees coordination of multicenter projects at Shriners Hospitals for Children in Philadelphia. Dr. Scott Kozin, upper extremity surgeon and co-author, provided his mentorship, input, and expertise on this article.
References
- 1.The National Spinal Cord Injury Statistical Center. Facts and figures at a glance April 1, 2009. https://www.nscisc.uab.edu/PublicDocuments Accessed July6, 2009.
- 2.Shriners Hospitals for Children. Spinal Cord Injury Annual Statistical Report. Tampa, FL; 2008 [Google Scholar]
- 3.Hanson RW, Franklin MR.Sexual loss in relation to other functional losses for spinal cord injured males. Arch Phys Med Rehabil. 1976;57 (6): 291–293 [PubMed] [Google Scholar]
- 4.Moberg E.Possible surgical rehabilitation of highlevel tetraplegia In: Tubiana R, ed. The Hand. Philadelphia: WB Saunders; 1991: 541–547 [Google Scholar]
- 5.James M.Treatment of the upper extremity: indications, patient assessment, and procedures In: Betz RR, Mulcahey MJ, eds. The Child With a Spinal Cord Injury. Rosemont, IL: American Academy of Orthpaedic Surgeons; 1996: 393–404 [Google Scholar]
- 6.Kuz JE, Van Heest AE, House JH.Biceps-to-triceps transfer in tetraplegic patients: report of the medial routing technique and follow-up of three cases. J Hand Surg Am. 1999;24 (1): 161–172 [DOI] [PubMed] [Google Scholar]
- 7.Kozin SH, D’Adessi L, Chaftetz RS, Ashworth S, Mulcahey MJ.Biceps-to-triceps transfer for elbow extension in persons with tetraplegia. J Hand Surg. 2010;35A:968–975 [DOI] [PubMed] [Google Scholar]
- 8.Khaliq Y, Zhanel GG.Fluoroquinolone-associated tendinopathy: a critical review of the literature. Clin Infect Dis. 2003;36 (11): 1404–1410 [DOI] [PubMed] [Google Scholar]
- 9.Cipro [prescribing information] Bayer; October 2007. Updated April 2009. http://www.univgraph.com/bayer/inserts/ciprotab.pdf Accessed July6, 2009
- 10. Avelox [prescribing information]. Bayer; October 2007. Accessed November6, 2008
- 11. Levaquin [prescribing information]. Ortho-McNeil; 2010. Accessed November6, 2008
- 12.Khaliq Y, Zhanel GG.Musculoskeletal injury associated with fluoroquinolone antibiotics. Clin Plast Surg. 2005;32 (4): 495–502, vi. [DOI] [PubMed] [Google Scholar]
- 13.Belavic JM.Fluoroquinolone-induced tendinopathy. Nurse Pract. 2009;34 (1): 17–18 [DOI] [PubMed] [Google Scholar]
- 14.Hentz VR, Leclerq C.Surgical Rehabilitation of the Upper Limb in Tetraplegia. New York: WB Saunders; 2009 [Google Scholar]
- 15.Kim HM, Nelson G, Thomopoulos S, Silva MJ, Das R, Gelberman RH. Technical and biological modifications for enhanced flexor tendon repair. J Hand Surg. 2010;35A:1031–1037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hutchinson D, Kozin SH, Mayer N, Mulcahey MJ, Duffy T, Gaughan JP.Dynamic electromyographic evaluation of adolescents with traumatic cervical injury after biceps to triceps transfer: the role of phasic contraction. J Hand Surg Am. 2008;33: 1331–1336 [DOI] [PubMed] [Google Scholar]



