Abstract
Background:
The reduction in physical activity that accompanies spinal cord injury (SCI) contributes to the development of secondary health concerns. Research has explored potential strategies to enhance the recovery of walking and lessen the impact of physical disability following SCI, but further work is needed to identify determinants of community walking activity in this population.
Objectives:
To quantify relationships among lower extremity strength (LES), preferred walking speed (PWS), and daily step activity (DSA) in adults with incomplete SCI (iSCI) and determine the extent to which LES and PWS predict DSA in persons with iSCI.
Methods:
Participants were 21 adults (age range, 21 to 62 years; AIS levels C and D) with iSCI. Maximal values of hip abduction, flexion, and extension, knee flexion and extension, and ankle dorsiflexion and plantar flexion were measured using handheld dynamometry and were summed to determine LES. PWS was calculated using a photoelectric cell-based timing system, and participants were fitted with activity monitors to measure DSA in a natural setting.
Results:
Statistically significant (P <; .05) correlations of moderate to high magnitude (.74 to .87) were observed among LES, PWS, and DSA. Multiple regression analysis revealed that LES and PWS accounted for 83% (adjusted R2) of the variation in DSA (P <; .001).
Conclusion:
A significant proportion of the explained variance in DSA can be predicted from knowledge of LES and PWS in adults with iSCI. These findings suggest that future efforts to improve community walking behavior following SCI should be directed toward increasing LES and PWS.
Key words: daily step activity, incomplete spinal cord injury, lower extremity strength, walking, walking speed
In designing rehabilitative strategies to lessen the decline in physical function observed in persons with incomplete spinal cord injury (iSCI), it is critical to identify key factors that promote effective ambulation in community settings. In this regard, 2 potential variables of interest are lower extremity strength and preferred walking speed, both of which decline following SCI.1 If walking bouts require greater leg strength than can be generated, or if a walking task cannot be completed in a reasonable time period, more efficient forms of mobility (eg, wheelchairs, motorized scooters) are often used to compensate for limitations in walking status. Although these compensatory strategies enable individuals with iSCI to become more functionally mobile, they also paradoxically contribute to a reduction in walking behavior.2
Increases in leg strength and walking speed have been associated with recovery of walking and fewer secondary health consequences in persons with SCI.3 However, the impact of lower extremity strength and speed deficits on locomotor function in this population has primarily been documented using measures such as the FIM-Locomotor subsection (FIM-L), the Walking Index for Spinal Cord Injury (WISCI-II), walking speed for 50 feet, and distance covered in a 6-minute walk test.4 Although these assessments provide valid clinical measures of walking capability, their ecological validity is limited because they do not reflect walking performance in real-life settings. In addition, use of the lower extremity motor score (LEMS), which features a graded strength assessment of lower limb muscle groups,5,6 may limit the ability to detect small but clinically meaningful differences in muscle strength between individuals with iSCI or reveal subtle changes in muscle force generation resulting from therapeutic interventions.
Consequently, the primary aim of this study was to quantify relationships among lower extremity strength, preferred walking speed, and community-based step activity in adults with iSCI. A secondary focus of this investigation was to document the extent to which lower extremity strength and preferred walking speed predict daily step activity in persons with iSCI. We hypothesized that significant associations would exist among lower extremity strength, preferred walking speed, and daily step activity in adults with iSCI and that knowledge of lower extremity strength and preferred walking speed would account for a large proportion of explained variance in the number of steps taken under free-living conditions.
Methods
Participants
Adults (males, n = 17; females, n = 4) with iSCI who were recruited through contacts with local clinicians and SCI community groups volunteered to participate in this study. Participants ranged in age from 21 to 62 years, were classified as either C or D on the American Spinal Cord Injury Association Impairment Scale (AIS), and displayed injury locations from C3 to T10. Participant characteristics are shown in Table 1. No participants exhibited complex comorbidity and all were at least 1 year post injury and capable of ambulating a minimum of 10 ft with or without an assistive device. The number of participants in the current study was similar to that found in other studies documenting leg strength and walking capacity in persons with iSCI.5,6 This project was approved by the university institutional review board and written informed consent was obtained before data collection commenced.
Table 1.
Participant characteristics
| Sex | Age | Level of lesion | AIS | Years post- injury | WISCI-II | Primary mode of locomotion | |
| 1 | M | 56 | T5 | C | 3 | 9 | Wheelchair |
| 2 | M | 21 | C5 | C | 2.5 | 6 | Wheelchair |
| 3 | M | 62 | T2 | D | 6 | 16 | Wheelchair |
| 4 | M | 28 | C4 | D | 3.5 | 10 | Ambulation |
| 5 | M | 43 | T8 | C | 2 | 9 | Wheelchair |
| 6 | M | 33 | T5 | D | 2 | 8 | Wheelchair |
| 7 | M | 23 | C6 | D | 1.5 | 16 | Wheelchair |
| 8 | F | 46 | T6 | C | 4.5 | 12 | Wheelchair |
| 9 | M | 50 | C4 | C | 1 | 11 | Wheelchair |
| 10 | M | 48 | T2 | D | 5 | 16 | Ambulation |
| 11 | M | 46 | T6 | C | 2 | 13 | Wheelchair |
| 12 | M | 31 | T7 | C | 3.5 | 12 | Wheelchair |
| 13 | M | 40 | T8 | D | 4.5 | 8 | Wheelchair |
| 14 | F | 51 | C3 | D | 3 | 10 | Ambulation |
| 15 | M | 41 | C6 | C | 10 | 18 | Wheelchair |
| 16 | M | 29 | T5 | C | 2 | 10 | Wheelchair |
| 17 | M | 28 | T8 | D | 28 | 18 | Wheelchair |
| 18 | F | 61 | C4 | C | 1 | 13 | Ambulation |
| 19 | M | 30 | T10 | C | 2.5 | 12 | Ambulation |
| 20 | M | 52 | T8 | D | 6 | 16 | Wheelchair |
| 21 | F | 40 | T6 | C | 3 | 9 | Wheelchair |
Note: M = male; F = female; AIS = American Spinal Injury Association Impairment Scale; WISCI-II = Walking Index for Spinal Cord Injury.
Lower extremity strength
Lower extremity strength was measured using a handheld dynamometer (J-Tech Medical, Salt Lake City, Utah). The use of handheld dynamometry to quantify muscle strength has been shown to be highly reliable (r > 0.91) when assessing persons with neurological disabilities.7 In addition, handheld dynamometers have been reported to demonstrate good validity in all force ranges, with validity and reliability increasing when stabilization techniques are used and trained examiners perform the strength measurements.8
Participants were securely positioned, with proximal stabilization provided to minimize muscle substitution and ensure appropriate force application by the muscle groups tested. Maximal isometric lower extremity strength was measured during flexion, extension, and abduction of the hip; knee flexion and extension; and ankle dorsiflexion and plantar flexion. These muscle groups were selected for evaluation because of their significant contributions to ambulation in persons with iSCI.5 Each joint was placed in as close to a 90º angle as possible, with the dynamometer placed at the distal end and perpendicular to the segment being tested. Exceptions to this procedure included hip abduction and ankle dorsiflexion and plantar flexion, which were measured from a neutral position. Joint angles were determined using a standard goniometer. A physical therapist experienced in the use of handheld dynamometry to assess leg strength in persons with disabilities performed all strength assessments.
A minimum of 3 trials were completed for each muscle group in both legs. Standardized verbal directions and physical prompts were provided to facilitate the appropriate direction of force application. During each trial, participants were instructed to press as hard as possible against the dynamometer, which was held in place by the tester (“make test”). When maximal effort appeared to have been given (~3 to 5 seconds), participants were instructed to relax. The highest strength values measured in the 7 muscle groups tested in both legs were summed to yield an overall lower extremity strength score. Body mass was determined using a calibrated wheelchair scale (Detecto-CR500; Cardinal Scale Manufacturing Co, Webb City, Missouri) to allow strength measures to be expressed relative to body mass.
Preferred walking speed
Walking speed was measured using a Brower Timing System (Brower Systems, Draper, Utah) as participants walked over a level indoor surface. Participants were instructed to walk at a comfortable pace for 3.048 m (10 ft). Preferred walking speed was calculated from the time (to 1/100 of a second) required to traverse a 2-m distance located in the middle of the walking course. Participants completed at least 3 walking trials, with adequate rest breaks between each trial. Mean preferred walking speed was calculated by averaging walking speeds performed at a pace described as normal by each participant during the first 3 trials.
Daily step activity
Home and community walking activity was documented using the Step Activity Monitor (SAM; OrthoCare, Oklahoma City, Oklahoma). The SAM is a lightweight, microprocessor-driven accelerometer that is worn on the ankle. Bowden and Behrmen9 have reported that the SAM is 97% accurate compared to hand-tallied step counts during 10-m and 6-minute walk tests when worn by individuals with iSCI. Each participant was fitted with a SAM to assess daily step activity at home and in the community. Initial calibration adjustments to the SAM were made for the expected sensitivity, cadence, threshold, and motion characteristics of each individual. Participants were then observed during overground walking to ensure that all step activity was captured. If step counts were missed, or if non-step activity was registered, further adjustments were made to the SAM until all valid step activity was recorded. The SAM devices were worn on the right ankle during waking hours (except when showering or bathing) for 7 consecutive days, beginning the day following laboratory testing. If participants wore an orthotic device on the right ankle, they were instructed to wear the SAM on the left ankle to increase the likelihood of recording all valid step activity.9 Step counts were recorded in 1-minute epochs, and the SAM automatically reset to a zero step count at the start of each new 24-hour cycle.
Following the 7-day monitoring period, the SAM was returned to allow stored activity data to be downloaded and processed. If step activity data were missing or incomplete, participants were asked to wear the SAM during the following week on the days for which step counts were missing to obtain activity data for 7 full days (5 weekdays and 2 weekend days). Step counts for all 7 days were averaged to derive a mean value for daily step activity. Because step count data from the SAM reflect activity from only one leg, the step activity of both legs can be calculated by doubling the step activity of the monitored leg.
Data analysis
Descriptive statistics were calculated using SPSS version 18 software (SPSS, Inc, Chicago, Illinois) and presented as means ± standard deviations. Pearson product-moment correlation analysis was performed to quantify relationships among lower extremity strength, preferred walking speed, and daily step activity. Multiple regression analysis was employed to determine the predictive value of lower extremity strength and preferred walking speed in estimating daily step activity. Trend analyses were also conducted to determine the pattern of distribution for lower extremity strength and preferred walking speed relative to daily step activity. A significance level of .05 was used for all statistical analyses.
Results
Descriptive statistics for maximal isometric lower extremity strength, preferred walking speed, and daily step activity of study participants are presented in Table 2. As shown in Table 3, significant (P < .05) correlations of moderate to high magnitude were observed among lower extremity strength, preferred walking speed, and daily step activity. Multiple regression analysis also indicated that lower extremity strength and preferred walking speed collectively accounted for 83% of the overall variation in daily step activity.
Table 2.
Leg strength, preferred walking speed, and daily step activity of study participants
| Variable | M | SD | Range |
| Leg strength (N•kg-1) | 10.30 | 3.62 | 4.63 – 15.84 |
| Preferred walking speed (m•s-1) | 0.43 | 0.21 | 0 – .77 |
| Daily step activity (right leg only) | 1167 | 770 | 10 – 2,149 |
Table 3.
Relationships among leg strength, preferred walking speed, and daily step activity
| Leg strength (N•kg-1) | Preferred walking speed (m·s-1) | Daily step activity (right leg only) | |
| Leg strength (N·kg-1) | – | .74* | .83* |
| Preferred walking speed (m•s-1) | – | .87* | |
| Daily step activity (right leg only) | – |
P < .05 (2-tailed).
Trend analyses illustrating the pattern of relationships between lower extremity strength and daily step activity and preferred walking speed and daily step activity are depicted in Figures 1 and 2, respectively. The association between lower extremity strength and daily step activity was best represented by a linear model (r = .83, P < .05), demonstrating that each unit of increase in leg strength was associated with a proportionate rise in daily step count. In contrast, a growth model best expressed the association between preferred walking speed and daily step activity (r = .87, P < .05), such that greater increases in daily step counts occurred at faster walking velocities than at slower walking velocities.
Figure 1.
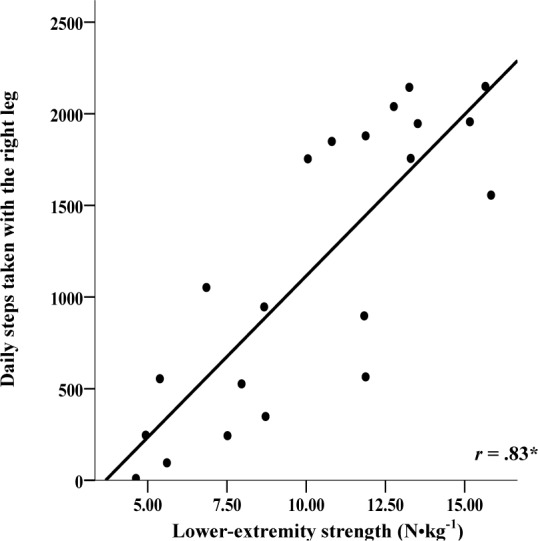
Trend analysis of the relationship between lower extremity strength and daily step activity. *P <.05.
Figure 2.
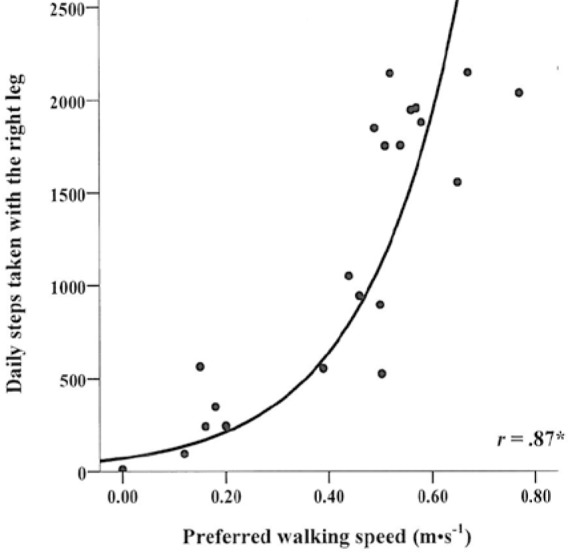
Trend analysis of the relationship between walking speed and daily step activity. *P <.05.
Discussion
The central aim of this investigation was to quantify relationships among lower extremity strength, preferred walking speed, and daily step activity in adults with iSCI. Previous research on this topic has been limited, and studies that have explored this topic have typically incorporated scale-based assessments to quantify muscle force5,6 and featured laboratory or clinical measures of walking performance such as the WISCI-II or 6-minute walk test.1,5,6 A secondary aim of our study was to evaluate the overall contribution of lower limb strength and walking speed to daily stepping activity in adults with iSCI. Knowledge gained from addressing both project aims could help inform clinical practice by highlighting the practical importance and potential unique impacts of strength and speed development on the daily walking behavior of persons who have experienced SCI.
Lower extremity strength
In persons with iSCI, strength assessment is typically quantified using the LEMS, which is a 0-to-5 rating scale based on the ability of muscles to resist gravity and external resistance. Using this scale-based assessment, scores for individual muscle groups are summed to produce an overall strength score.4 Although the LEMS has been used to provide a general classification of muscle strength in the iSCI population, modest changes in strength resulting from training or therapy may evade detection. To address this concern, Sara et al1 employed a quantitative assessment of maximal isometric volitional torque in adults with chronic motor iSCI. Similarly, handheld dynamometry, which has been employed in studies featuring neurologically impaired populations8,10 and shown to be valid at lower strength ranges,8 provided a direct measure of leg strength in our participant group. Because scale-based measures of leg muscle strength have been used in previous studies of persons with iSCI,4,11,12 it is difficult to compare our findings with those of other investigators. However, as depicted in Table 2, marked variability was present in the residual leg strength of our participants, such that the summed strength score of the strongest participant was 242% higher than that of the weakest participant. Although speculative, this disparity in total leg strength may be related to interindividual differences in the extent of neural sparing, as well as variation in intrinsic (eg, neural reorganization, neurogenesis) and extrinsic (eg, physical activity level) factors associated with recovery from iSCI.
Preferred walking speed
Published research suggests that a walking speed of 1.20 to 1.31 m•s-1 is required for independent community ambulation.13,14 The average walking speed for our sample was 0.43 ± 0.21 m•s1, which is similar to mean walking velocities of 0.36 m•s-1 and 0.31 m•s-1recorded in other studies of male and female adults with iSCI classified as AIS C and D.15,16 Viewed collectively, this trio of walking speeds falls below the threshold for independent community ambulation, thus setting the stage for an increased reliance on assistive mobility aids to facilitate locomotion. It has been suggested that the reduction in walking speed seen in persons with iSCI can be attributed to a reduction in gait cycle frequency caused by diminished neural processing speed.17 Hence, while stride length contributes to gait velocity, stride frequency appears to be the primary factor limiting speed of ambulation in persons with iSCI.17 Given this kinematic limitation, gait training following iSCI should include locomotor-based activities, such as assisted gait training,17 that facilitate rapid reciprocal patterns of stepping.
Daily step activity
Current evidence suggests that daily step activity of 6,000 to 7,000 steps is reflective of typical walking patterns for healthy adults (excluding sport and exercise participation), and values below this range are considered sedentary.18 Saraf and colleagues1 reported an average of 2,658 (±2,745) steps per day (for both legs) in a sample of persons with iSCI (AIS C, n = 15; AIS D, n = 35). This large standard deviation in step counts highlights the large variability in the daily step activity of persons with iSCI. Our sample of ambulatory persons with iSCI (AIS C, n = 12; AIS D, n = 9) displayed a mean step count of 1,167 (±770) steps per day (one leg only), a value that, when doubled, is reflective of the overall magnitude and variability in walking behavior reported by Saraf et al.1 The limited step activity exhibited by our participants is well below the threshold for sedentary persons identified by Tudor-Locke and Bassett18 and clearly highlights the need for greater physical activity in this population to enhance mobility and overall health.
Correlation and multiple regression analysis
Statistically significant relationships (.74 to .87) were observed among overall lower extremity strength, walking speed, and daily step activity in our sample of adults with iSCI. These findings, which confirm our first hypothesis, align with previous research demonstrating moderately strong correlations between walking speed and LEMS values (r = .64) and daily step activity and LEMS and knee extensor and hip extensor strength measures (r range, .62 to .73) in persons who have experienced iSCI.1,19 Validating our second hypothesis, multiple regression analysis also revealed that the combined influence of leg strength and walking speed accounted for a vast majority (83%) of the variation in daily step activity among our participants. In view of the association between daily physical activity and improved health in persons with SCI,20 our collective findings support the notion that rehabilitative and activity-oriented programs in this group should focus on improving lower extremity strength and speed of locomotion to enhance functional mobility, promote community-based walking opportunities, and reduce extended periods of sedentary behavior.
Trend analysis
Leg strength and walking speed were significant and substantial contributors to daily step frequency, but unique patterns of distribution for each variable relative to walking activity were observed. Trend analysis indicated that a linear model best expressed the relationship between leg strength and daily step activity, whereas the association between walking speed and daily step count was most accurately portrayed using a growth model. Specifically, visual inspection of Figure 2 suggests that a critical speed (~0.42 m•s-1) may exist, above which daily step activity in persons with iSCI rises in an accelerated fashion. This speed threshold is nearly identical to values reported for persons with myelomeningocele and stroke (0.42 m•s-1)21 and is at the lower end of the range of speeds (0.40 to 0.80 m•s-1) needed to attain limited ambulation following neurological impairment.22 Our data lend credence to the view that therapeutic interventions designed to increase community ambulation in persons with iSCI should aim to reach and eventually exceed this speed threshold by strengthening the lower limbs through resistance training, engaging in locomotor training, or regularly participating in other forms of weight-supported physical activity involving the legs.
Conclusion
Statistically significant relationships of moderate to strong magnitude were found among overall lower extremity strength, preferred walking speed, and community-based step activity in male and female adults with iSCI, and a substantial proportion of explained variance in daily step activity among our participants was predicted from knowledge of leg strength and normal walking speed. Moreover, in our group of adults with iSCI, a linear association was found to exist between lower extremity strength and daily step activity, whereas a curvilinear relationship between preferred walking speed and daily step activity was observed. Based on our results, future research and clinical interventions should be conducted to evaluate the impact of various lower body strength training regimens and gait retraining therapies on daily step activity and overall health in persons with iSCI.
References
- 1.Saraf P, Rafferty M, Moore J, et al. Daily stepping in individuals with motor incomplete spinal cord injury. Phys Ther. 2010;90(2):224–240 [DOI] [PubMed] [Google Scholar]
- 2.Botos M, Gericke C.Ambulatory capacity in cerebral palsy: prognostic criteria and consequences for intervention. Dev Med Child Neurol. 2003;45:786–790 [DOI] [PubMed] [Google Scholar]
- 3.Lavis T, Scelza W, Bockenek W.Cardiovascular health and fitness in persons with spinal cord injury. Phys Med Rehabil Clin North Am. 2007;18:317–331 [DOI] [PubMed] [Google Scholar]
- 4.Ditunno J, Scivoletto G.Clinical relevance of gait research applied to clinical trials in spinal cord injury. Brain Res Bull. 2009;78:35–42 [DOI] [PubMed] [Google Scholar]
- 5.Shah P, Stevens J, Gregory C, et al. Lower-extremity muscle cross-sectional area after incomplete spinal cord injury. Arch Phys Med Rehabil. 2006;87(6):772–778 [DOI] [PubMed] [Google Scholar]
- 6.Kim C, Eng J, Whittaker M.Level walking and ambulatory capacity in persons with incomplete spinal cord injury: relationship with muscle strength. Spinal Cord. 2004;42:156–162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Riddle D, Finucaine S, Rothstein J, Walker M.Intrasession and intersession reliability of hand-held dynamometer measurements taken on brain damaged patients. Phys Ther. 1989;69:182–194 [DOI] [PubMed] [Google Scholar]
- 8.Nollet F, Beelen A.Strength assessment in postpolio syndrome: validity of a hand-held dynamometer in detecting change. Arch Phys Med Rehabil. 1999;80(10):1316–1323 [DOI] [PubMed] [Google Scholar]
- 9.Bowden M, Behrman A.Step activity monitor: accuracy and test-retest reliability in persons with incomplete spinal cord injury. J Rehabil Res Dev. 2007;44(3):355–362 [DOI] [PubMed] [Google Scholar]
- 10.Wiley M, Damiano D.Lower-extremity strength profiles in spastic cerebral palsy. Dev Med Child Neurol. 1998;40:100–107 [DOI] [PubMed] [Google Scholar]
- 11.Dobkin B, Apple D, Barbeau H, et al. Weight-supported treadmill vs over-ground training for walking after acute incomplete spinal cord injury. Neurology. 2006;66(2):484–493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Geisler F, Dorsey F, Coleman W.Recovery of motor function after spinal cord injury – a randomized placebo-controlled trail with GM-1 ganglioside. New Engl J Med. 1991;324(26):1829–1838 [DOI] [PubMed] [Google Scholar]
- 13.Lapointe R, Lajoie Y, Serresse O, Barbeau H.Functional community ambulation requirements in incomplete spinal cord injured subjects. Spinal Cord. 2001;39:327–335 [DOI] [PubMed] [Google Scholar]
- 14.van Hedel H, Tomatis L, Muller R.Modulation of leg muscle activity and gait kinematics by walking speed and bodyweight unloading. Gait Posture. 2006;4:35–45 [DOI] [PubMed] [Google Scholar]
- 15.Wirz M, Zemon D, Rupp R, et al. Effectiveness of automated locomotor training in patients with chronic incomplete spinal cord injury: a multicenter trial. Arch Phys Med Rehabil. 2005;86:672–680 [DOI] [PubMed] [Google Scholar]
- 16.Winchester P, Smith P, Foreman N, et al. A prediction model for determining over ground walking speed after locomotor training in persons with motor incomplete spinal cord injury. J Spinal Cord Med. 2009;32(1):63–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pepin A, Ladouceur M, Barbeau H.Treadmill walking in incomplete spinal-cord-injured subjects: 2. Factors limiting maximal walking speed. Spinal Cord. 2003;41: 271–279 [DOI] [PubMed] [Google Scholar]
- 18.Tudor-Locke C, Bassett D.How many steps/day are enough? Preliminary pedometer indices for public health. Sports Med. 2004;34(1):1–8 [DOI] [PubMed] [Google Scholar]
- 19.Dobkin B, Barbeau H, Deforge D, et al. The evolution of walking-related outcomes over the first twelve weeks of rehabilitation for incomplete traumatic spinal cord injury: the multicenter randomized spinal cord injury locomotor trial. Neurorehabil Neural Repair. 2007;21(1):25–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Myers J, Lee M, Kiratli J.Cardiovascular disease in spinal cord injury. Am J Phys Med Rehabil. 2007;86(2):142–152 [DOI] [PubMed] [Google Scholar]
- 21.Schmid A, Duncan P, Studenski S, et al. Improvements in speed-based gait classifications are meaningful. Stroke. 2007;38:2096–2100 [DOI] [PubMed] [Google Scholar]
- 22.Perry J, Garrett M, Gronley J, Mulroy S.Classification of walking handicap in the stroke population. Stroke. 1995;26:982–989 [DOI] [PubMed] [Google Scholar]


